Abstract
The study of premature deaths from causes that are generally preventable given the current availability of healthcare – called amenable deaths due to healthcare – provides information on the quality of services. However, they are not only impacted by healthcare characteristics: other factors are also likely to influence. Therefore, identifying the association between amenable deaths due to healthcare and health determinants, such as education, might be the key to preventing these deaths in the future. Still unclear however, is how this works and how amenable deaths due to healthcare are distributed and evolve within the European Union (EU) below the national level. We therefore studied the geographical and temporal patterns of amenable deaths due to healthcare in the 259 EU regions from 1999 to 2016, including the 2007–2008 financial crisis and the post-2008 economic downturn, and identified whether any association with education exists.
A cross-sectional ecological study was carried out. Using a hierarchical Bayesian model, we estimated the average smoothed Standardized Mortality Ratios (sSMR). A regression model was also applied to measure the relative risks (RR) at 95% credible intervals for cause-specific mortality association with education.
Results show that amenable deaths due to healthcare decreased globally. Nevertheless, the decrease is not the same across all regions, and inequalities within countries do persist, with lower mortality ratios seen in regions from Central European countries and higher mortality ratios in regions from Eastern European countries. Also, the evolution trend reveals that after the financial crisis, the number of these deaths increased in regions across almost all EU countries. Moreover, educational disparities in mortality emerged, and a statistical association was found between amenable deaths due to healthcare and early exit from education and training.
These results confirm that identifying and understanding the background of regional differences may lead to a better understanding of the amenable deaths due to healthcare and allow for the application of more effective policies.
Keywords: Amenable deaths due to healthcare, Health determinants, Education, European Union regions, NUTS 2, Spatial inequalities, Bayesian model, Relative risk
Highlights
-
•
Amenable deaths due to healthcare decreased within the EU regions.
-
•
The change did not occur equally as relative inequalities within countries remain.
-
•
Amenable deaths increased in regions from 17 EU countries after 2011–2013.
-
•
A 1% increase in school dropout is linked to a 2% increase in amenable deaths.
1. Introduction
European population health has improved in recent decades, yet progress has varied between countries and significant inequalities are notable within member states (Bambra, 2019; Costa, Santana, et al., 2019; Mackenbach et al., 2016; Marmot, 2013; Rydland, Solheim, & Eikemo, 2020; Santana et al., 2017). Thus health inequalities remain, even in the highly developed welfare states of Europe (Leão et al., 2018; Nelson & Tøge, 2017). Therefore, it remains important to draw the attention of policymakers to the wider social circumstances in which people live their lives and particularly those aspects that more or less indirectly affect their health (Bergqvist et al., 2013). Looking at avoidable deaths, and specifically amenable deaths due to healthcare, is one way to achieve this.
Avoidable mortality is a “sentinel indicator” used as a proxy to analyse geographical disparities in population health and to help identify potential shortfalls (Hoffmann et al., 2014; Nolte & McKee, 2004; Plug et al., 2012). It originates from the pioneering work of Rustein and colleagues (1976) that introduced the notion of conditions leading to unnecessary/untimely deaths and that, later on, Charlton et al. (1983) named avoidable mortality. Since the beginning, the concept of avoidable deaths has been modified with researchers not reaching a consensus regarding its precise definition, the causes of death classified as avoidable or the age limits established to separate avoidable from unavoidable deaths (Charlton et al., 1983; Holland, 1990; Mackenbach et al., 1988; Nolte et al., 2002; Nolte & McKee, 2004).
According to the EUROSTAT′ Task Force, avoidable mortality are deaths that, «in the light of medical knowledge and technology or in the light of understanding of the determinants of health at the time of death, all or most deaths from that cause (subject to age limits if appropriate) could be avoided through good quality healthcare or by public health interventions in the broadest sense» (EUROSTAT, 2014, p. 1). In 2014, based on the work of the UK's Office for National Statistics, EUROSTAT divided avoidable deaths into two groups: amenable deaths due to healthcare and preventable deaths. The former are deaths that, «in the light of medical knowledge and technology at the time of death, all or most deaths from that cause could be avoided through good quality healthcare». The latter are deaths that, «in the light of understanding of the determinants of health at the time of death, all or most deaths from that cause (subject to age limits if appropriate) could be avoided by public health interventions in the broadest sense» (EUROSTAT, 2014, p. 1). Still, some causes of death were both considered amenable and preventable as they can be amenable by appropriate healthcare and preventable by health behaviours (Gavurova & Vagasova, 2017). This is the case for ischaemic heart disease, cerebrovascular diseases or diabetes mellitus.
Literature reveals that good quality healthcare is not the only determinant impacting amenable deaths due to healthcare (Karanikolos & Nolte, 2018; Rosella et al., 2019). Other factors related to the likelihood of individuals to contract a disease or to seek medical advice – education, social class, health beliefs, levels of concern – are likely to influence the amount of amenable and preventable deaths (McMinn et al., 2020; Nagy et al., 2012; Nolte & McKee, 2004; Plug et al., 2012; Tobias & Yeh, 2009).
Education is among the social determinants highlighted in the Whitehead and Dahlgren’ social determinants model (Popham & Iannelli, 2021; von dem Knesebeck et al., 2006; Witkam et al., 2021). According to the literature, education is among the most relevant determinants and prominent in shaping health outcomes because it relates more directly to knowledge and skills than other socioeconomic indicators (Laaksonen et al., 2005; Popham & Iannelli, 2021; Sauerberg, 2021; Witkam et al., 2021). In a study designed to appraise population health in a wide range of health domains in Europe, education was considered the second most relevant dimension, confirming what is widely stated in the literature (Santana, Freitas, Costa, et al., 2020).
The interrelationship between education and mortality, and specifically with amenable deaths due to healthcare, is explained through numerous pathways. Education generates benefits regarding occupational prospects, income, job satisfaction, stress reduction, better decision making and better living conditions, which are closely related with higher health literacy, increased likelihood of having health insurance, more informed decisions affecting health, better access to health technologies, improved health status, ability to avoid risky health behaviours, higher life expectancy, lower reliance on health services and higher social value attributed to health (Brunello & Paola, 2014; Clench-Aas & Holte, 2017; Kaplan, 2012; Lochner, 2011; Mackenbach, 2012; Phelan et al., 2010). On the contrary, those with lower levels of education have a higher risk of mortality, especially premature, a higher prevalence of chronic diseases, mental health problems and poor self-reported health (Leão et al., 2018; Mackenbach et al., 2008; von dem Knesebeck et al., 2006). Looking specifically to the causes of death amenable to healthcare, previous studies found that a lower educational level is associated with higher mortality (Plug et al., 2012; Stirbu et al., 2010) and that the mortality for amenable causes of death declined faster among the highly educated (Mackenbach et al., 2017; Rydland et al., 2020; Stirbu et al., 2010).
An important aspect that has affected both education, income and access to healthcare in Europe in recent decades, was the financial crisis in 2007–2008 and the post-2008 economic downturn, popularly referred to as the ‘great recession’ (Doetsch et al., 2017; Leão et al., 2018; Nelson & Tøge, 2017). According to the literature, this crisis created huge issues for health, social and economic structures. During this period, most European countries faced low economic growth and began suffering from increased deficits and costs of sales which impacted the availability of resources for public spending, including education and health (Kaplan, 2012; Leão et al., 2018; Reeves et al., 2013). This had an immediate impact on levels of benefits, unemployment, job insecurity, migration, purchasing power, and could, potentially, affect how people accessed healthcare (Legido-Quigley et al., 2016). It also imposed financial constraints on some healthy behaviours and affected living conditions and other factors associated with financial and material disadvantage (Laaksonen et al., 2005). In the healthcare sector, per capita public spending on health fell in several countries which impacted the provision of health services and access to care, with large increases in unmet medical needs during and after the crisis (Arora et al., 2015; Cylus & Pearson, 2015; Reeves et al., 2014). These changes affected the way the population access healthcare, particularly with regards to the timing of access, leading to an increase of causes of death that could have been avoided if the quality of healthcare services was the same as before the crisis, and especially the case in Southern European countries (Bacigalupe et al., 2016; Costa & Santana, 2021). Karanikolos et al. (2018) demonstrated an increase of amenable deaths due to healthcare following the financial crisis in countries such as Greece, Estonia and Slovakia while the remaining ones appeared to be unaffected by the crisis. Furthermore, some studies found an increase in amenable deaths due to healthcare during or after the crisis within deprived areas of countries such as Portugal (Costa & Santana, 2021) and Spain (Pereyra-Zamora et al., 2020).
Finally, national level measures of mortality often hide the increase of mortality within-country differentials that are worth revealing. Previous studies regarding amenable deaths due to healthcare identify that there are significant differences within countries (Rican et al., 2017; Santana, 2002; Santana et al., 2017) and conclude that a deeper analysis is needed (Karanikolos et al., 2018) and that further research is required (Plug et al., 2012). Within the EU, the Nomenclature of Territorial Units for Statistics (NUTS) provides a common and hierarchical standard for data collection (Costa, Freitas, et al., 2019). The NUTS 2 level, commonly referred to as regions, was formulated by the European Commission for the application of regional policies that might positively contribute to tackle health determinants (Santana, Freitas, Costa, et al., 2020). Therefore, the NUTS 2 level is fundamental to better understanding of the challenges and opportunities of each region within the EU (Becker et al., 2010; Santana, Freitas, Costa, et al., 2020).
Our hypothesis is that, although amenable deaths due to healthcare are decreasing in European Countries and the temporal trend appears not to be affected by the crisis, this might not be true at sub-national level. Therefore, the objectives of this study are: i) to discuss the geographical and temporal patterns of amenable deaths due to healthcare at a sub-national scale with a focus on the years of the financial crisis, and ii) to determine the extent to which there is an association with education.
2. Data and methods
2.1. Design and sources of information
This study follows an ecological design based on EUROSTAT data for mortality, population and education indicators.
The unit of analysis corresponds to the NUTS 2 level (Nomenclature of Territorial Units for Statistics) of the European Union, 2013 version (excluding the outermost regions and autonomous cities), which is the lowest level with data available for all the EU. Due to the lack of mortality data at NUTS 2 level for Denmark and Croatia, these two countries were also excluded from the study. Therefore, 259 regions were considered for this study, with a population ranging from 30,000 inhabitants in Aland, Finland, to more than 12 million in Ile de France, France (in 2016).
The temporal trend takes into account the six 3-year periods available on the EUROSTAT database: 1999–2001, 2002–2004, 2005–2007, 2008–2010, 2011–2013 and 2014–2016. 1999 and 2016 are the first and the last year with data for almost all the EU regions.
2.2. Indicators
2.2.1. Mortality data
The Standardized Mortality Ratio (SMR) is the mortality indicator used for this analysis. The indicator amenable deaths due to healthcare is based on the list defined by the EUROSTAT Task Force on “Satellite Lists for Causes of Deaths (COD)” and considers those available on the European shortlist of causes of death (Table 1). The number of deaths from these causes were collected for the same age groups as specified on the EUROSTAT amenable deaths indicator and for all NUTS 2 of the 26 EU countries. The indicator collected from the EUROSTAT database was the 3-year mean number of deaths by cause of death.
Table 1.
Correspondence table between the EUROSTAT list of amenable deaths due to healthcare and the European causes of death shortlist by age group.
| EUROSTAT amenable deaths due to healthcare and ICD10 code | European causes of death shortlist and ICD10 code | Age group |
|---|---|---|
|
Infections | ||
| Tuberculosis [A15-A19, B90] | Tuberculosis [A15-A19, B90] | 0–74 |
| Selected invasive bacterial and protozoal infections [A38-A41, A46, A48.1, B50– B54, G00, G03, J02, L03] | n.a. | 0–74 |
| Hepatitis C [B17.1, B18.2] | Hepatitis [B15–B19, B942] | 0–74 |
| HIV/AIDS [B20–B24] | AIDS-HIV [B20–B24] | All |
|
Neoplasms | ||
| Malignant neoplasm of colon and rectum [C18–C21] | Colorectal [C18–C21] | 0–74 |
| Malignant melanoma of skin [C43] | Skin [C43] | 0–74 |
| Malignant neoplasm of breast [C50] | Breast [C50] | 0–74 |
| Malignant neoplasm of cervix uteri [C53] | Cervix [C53] | 0–74 |
| Malignant neoplasm of bladder [C67] | Bladder [C67] | 0–74 |
| Malignant neoplasm of thyroid gland [C73] | Thyroid Gland [C73] | 0–74 |
| Hodgkin's disease [C81] | Lymphatic/haematopoietic Tissue [C81–C85] | 0–74 |
| Leukaemia [C91, C92.0] | Leukaemia [C91–C95] | 0–74 |
| Benign neoplasms [D10-D36] | n.a. | 0–74 |
|
Nutritional, endocrine and metabolic | ||
| Diabetes mellitus [E10-E14] | Diabetes [E10-E14] | 0–49 |
|
Neurological disorders | ||
| Epilepsy and status epilepticus [G40-G41] | n.a. | 0–74 |
|
Cardiovascular diseases | ||
| Rheumatic and other valvular heart disease [I01–I09] | n.a. | 0–74 |
| Hypertensive diseases [I10–I15] | n.a. | 0–74 |
| Ischaemic heart disease [I20–I25] | Ischaemic heart disease [I20–I25] | 0–74 |
| Cerebrovascular diseases [I60–I69] | Cerebrovascular disease [I60–I69] | 0–74 |
|
Respiratory diseases | ||
| Influenza (including swine flu) [J09-J11] | Influenza [J09-J11] | 0–74 |
| Pneumonia [J12-J18] | Pneumonia [J12-J18] | 0–74 |
| Asthma [J45-J46] | Asthma [J45-J46] | 0–74 |
|
Digestive disorders | ||
| Gastric and duodenal ulcer [K25–K28] | Ulcers [K25–K28] | 0–74 |
| Acute abdomen, appendicitis, intestinal obstruction, cholecystitis/lithiasis, pancreatitis, hernia [K35–K38, K40–K46, K80–K83, K85, K86.1-K86.9, K91.5] | n.a. | 0–74 |
|
Genitourinary disorders | ||
| Nephritis and nephrosis [N00–N07, N17–N19, N25–N27] | Diseases of kidney and ureter [N00–N29] | 0–74 |
| Obstructive uropathy and prostatic hyperplasia [N13, N20–N21, N35, N40, N99.1] | n.a. | 0–74 |
|
Maternal and infant | ||
| Complications of perinatal period [P00–P96, A33] | Certain conditions originating in the perinatal period [P00–P96] | All |
| Congenital malformations, deformations and chromosomal anomalies [Q00-Q99] | Congenital malformations [Q00-Q99] | 0–74 |
|
Intentional injuries | ||
| Misadventures to patients during surgical and medical care [Y60–Y69, Y83–Y84] | n.a. | All |
n.a. = Cause of death not available on the European causes of death shortlist.
The mortality data were disaggregated into four-year age groups (except the first, corresponding to less than one year) in order to comply with data confidentiality rules.
The study population consisted of residents in EU regions between 1999 and 2016, stratified by the same age groups as the mortality data.
2.2.2. Education
Education characteristics of the regions considered for this study were those that researchers and stakeholders within the EURO-HEALTHY project identified as relevant for measuring educational inequalities in health between EU regions: Population aged 25–64 with lower secondary education attainment (%), and Early leavers from education and training (%) (Freitas et al., 2018). Both indicators were provided by EUROSTAT and collected for the midpoint year in each of the six periods.
A preliminary assessment detected missing data (e.g., region without data for a year), which was overcome by applying the protocol for missing data defined by Costa and colleagues (2019a) .
2.3. Data analysis
The analysis is based on the outcomes from the hierarchical Bayesian model proposed by Besag, York and Mollié (BYM) (1991) to overcome issues with population size and obtain smoothed Standardized Mortality Ratios (sSMR). This spatial disease mapping model is widely used for the analysis of registry data, such as mortality, and it is used in epidemiology on a standard basis (Schrödle & Held, 2011). The model allows us to produce smoothed estimates of amenable deaths due to healthcare, minimizing potential bias with well-established rigour while presenting a valid spatial pattern for mortality inequalities and a robust approach regarding the association with health determinants (Borrell et al., 2019; Eksler et al., 2008; Middleton et al., 2006; Palència et al., 2020; Santana et al., 2015).
The sSMR was estimated by using the following (model 1):
Where, for each region i, reveals the observed cases of death and the relative risk. represents the intercept, the spatial random effect and the heterogeneous effect. The expected number of deaths in each region was calculated by indirect standardization taking as reference the mortality rate by age group in EU26 and using the European Standard Population (2012 version).
This model takes into account two types of random effects – spatial and heterogeneous - for clustering and overdispersion. The spatial effect takes into account the spatial structure of the data so an intrinsic conditional autoregressive prior distribution was assigned. The heterogeneous effect deals with non-structural (non-spatial) variability and is represented using an independent normal distribution (Hoffmann et al., 2014). A half-normal distribution was assigned to the standard deviations and a vague prior distribution was assigned to the explanatory variables.
To investigate the association of the two education indicators as an explanatory variable of amenable deaths due to healthcare, a so-called ecological regression model was formulated as follows (model 2):
Where denotes the relative risk of mortality by a one-unit change in the explanatory indicator. Relative risk (RR) estimates were obtained based on their posterior means, along with the corresponding 95% credible intervals (95%CI). A RR will be considered significantly higher or lower than 1 if its 95%CI does not include 1. This model was implemented for each indicator - Population aged 25–64 with lower secondary education attainment, and Early leavers from education and training - and year-period - 1999–2001, 2002–2004, 2005–2007, 2008–2010, 2011–2013 and 2014–2016 - separately.
For both models, the Bayesian inference was obtained through the Integrated nested Laplace Approximation (INLA) library that runs in R statistical package (Schrödle & Held, 2011).
The sSMR value allows comparison between each region and the EU pattern, represented by the value 100. The geographical distribution of sSMR was represented using the following fixed categories: ]<50]; ]50–70]; ]70–90]; ]90–110]; ]110–130]; ]130–150] and ]>150]. It was also represented by comparing the region where the capital of each country is located with the remaining ones within the country. The share of population by the risk of mortality considers people living in both the first and the last categories, this is 1) regions where the mortality ratio is lower than 50, meaning that the mortality risk is less than half than what was expected according to the EU pattern; and 2) regions where the mortality ratio is higher than 150, meaning that the mortality risk is 1.5 times higher than the EU pattern.
Two other methods were applied: the Indirectly Standardized Mortality Rate (ISMR) and the Gini Coefficient. The first was utilized to identify the evolution of amenable deaths due to health care throughout the periods. It was calculated by multiplying the crude rate in the region by the crude rate in the standard population. The latter was tested to identify whether the magnitude of inequalities between all the EU regions had changed over time. It was calculated by ranking the regions in decreasing order based on the amenable deaths due to healthcare indicator; following the approach developed by Deaton (1997). G-value ranges from 0 to 1, where 0 expresses perfect equality and 1 expresses maximal inequality across regions.
3. Results
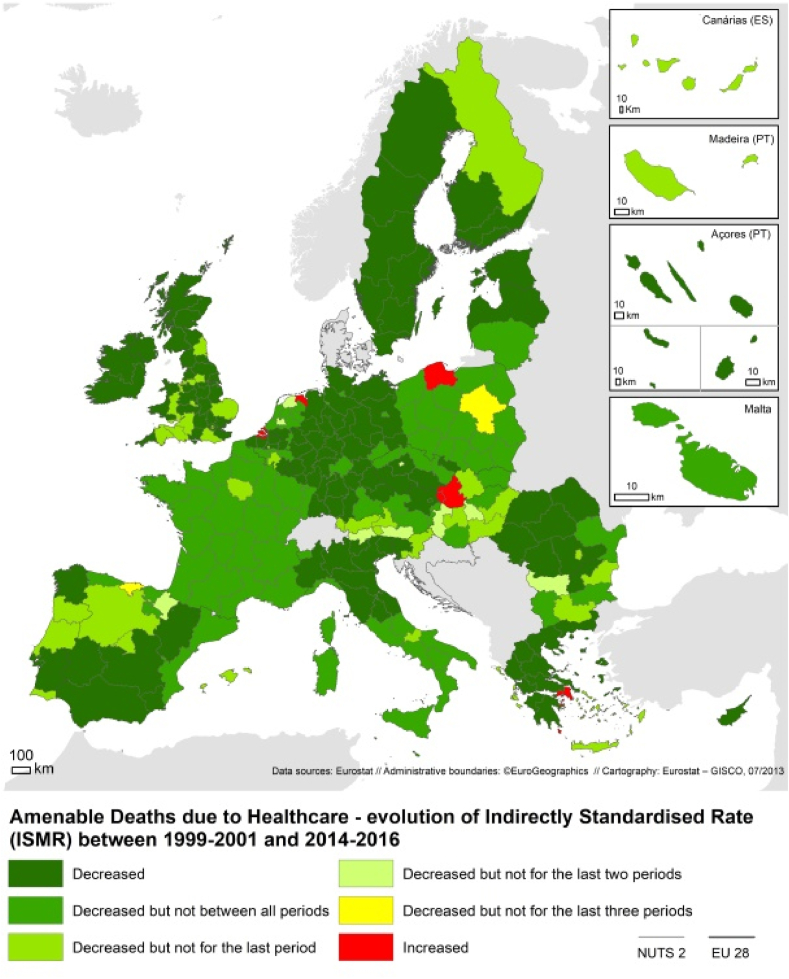
Fig. 1 shows that amenable mortality due to healthcare has declined in almost all the 259 EU regions over the last 20 years. However, the magnitude of the decrease – measured through the comparison of the ISMR in the first and last period, differs between regions and some even reveal an increase in these causes of death, namely in some regions of Greece, Poland, Netherlands and Slovakia. This phenomenon is even more visible between 2011-2013 and 2014–2016: 18.6% of the EU population were living in regions where amenable causes of death due to healthcare increased between those two periods. These regions are spread across 17 of the 26 EU countries and are highly diverse as they comprise both very dense and very rural regions.
Fig. 1.
Evolution of amenable deaths due to healthcare by region (ISMR) from 1999 to 2001 to 2014–2016. Note: Green represents the regions where treatable deaths decreased from 1999 to 2016. Lighter green means that the ISMR is not decreasing anymore. Red represents the regions revealing an increase. (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
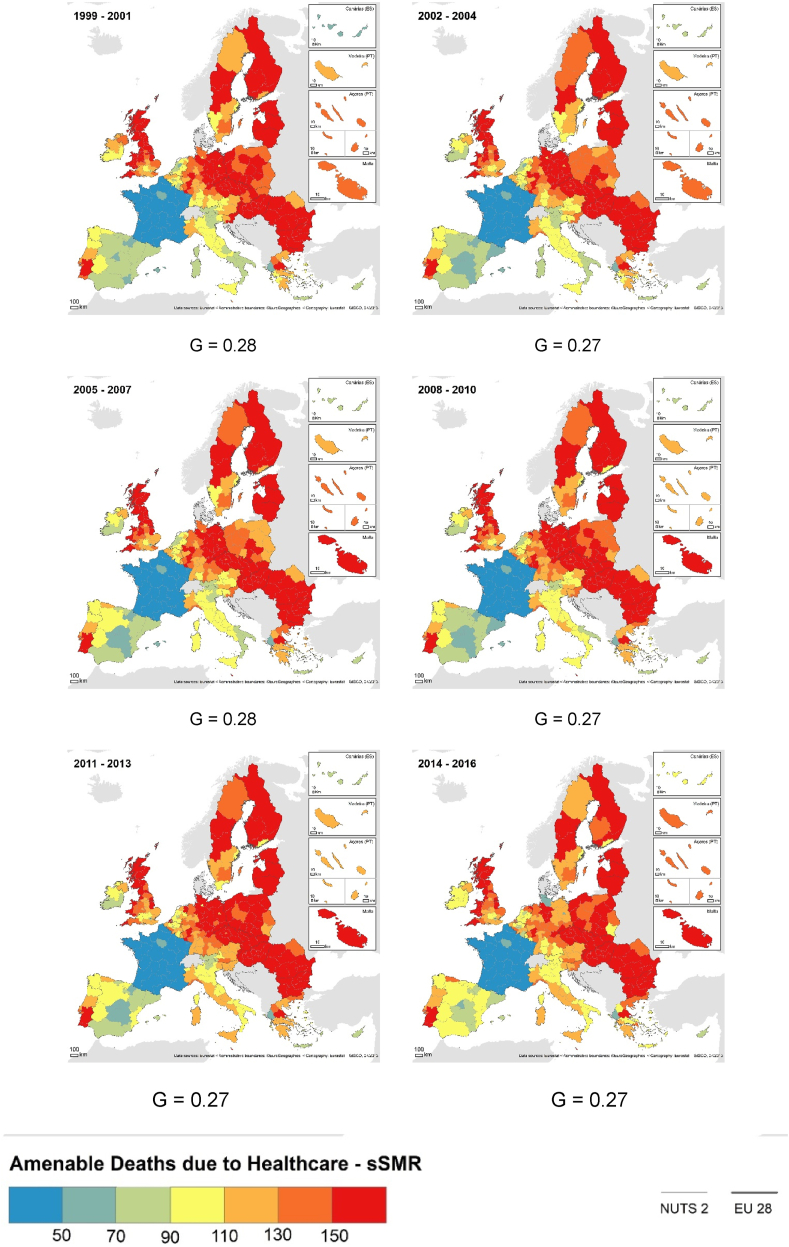
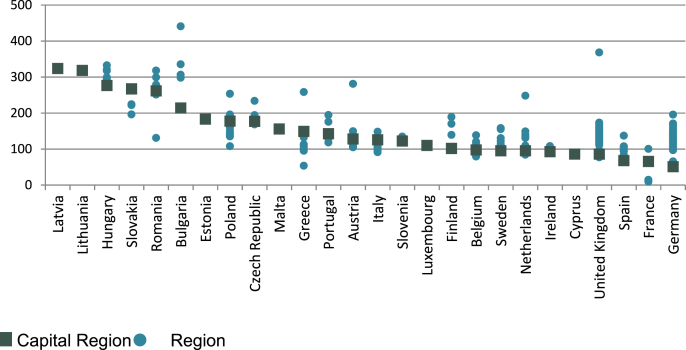
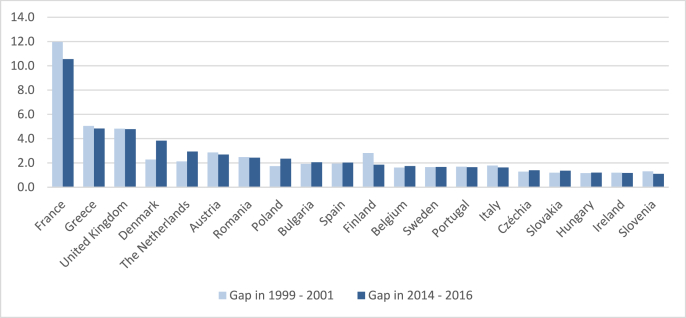
The Gini Coefficient reveals that the inequalities of sSMR at the EU level are moderate and relatively stable for these 6 periods (Fig. 2). However, a geographical pattern of sSMR is observed: a Central-Periphery contrast, with lower values in the Central European regions, especially in France, and higher values in peripheral regions, mainly in Eastern Northern and Southern Europe. Within each country, capital regions often present lower sSMR (Fig. 3). However, the countries presenting the highest ratio between regions, recording the lowest and highest sSMR, are France (10.6), United Kingdom (4.8) and Greece (4.8) (Fig. 4). In 1999–2001 those were also the countries revealing a higher differential between regions.
Fig. 2.
sSMR by causes of death amenable to the healthcare, at the regional level and Gini Coefficient (G), between 1999-2001 and 2014–2014. Note: Blue colours represent the regions where sSMR is below 100. Red colours represent the regions with sSMR above 100. G reveals the Gini Coefficient of each year. (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
Fig. 3.
Regional disparity in sSMR by causes of death amenable to the healthcare by Capital Region and other regions within each country, 2014–2016. Note: Some countries only have one NUTS 2 level region. Note: Green squares represent the sSMR of the capital region in each country. Blue dots represent the remaining regions. Countries are organized by the sSMR of the capital region. Some countries only have one NUTS 2 level region. (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
Fig. 4.
Amenable deaths due to healthcare (sSMR): Gap between regions within each country in 1999–2001 and 2014–2016. Note: only countries with more than one region are represented on the Figure. Note: The bars represent the gap between the region with the lowest sSMR and the one with the highest sSMR by country. The lighter bar represents the gap in 1999–2001. The darker gap represents the gap in 2014–2016.
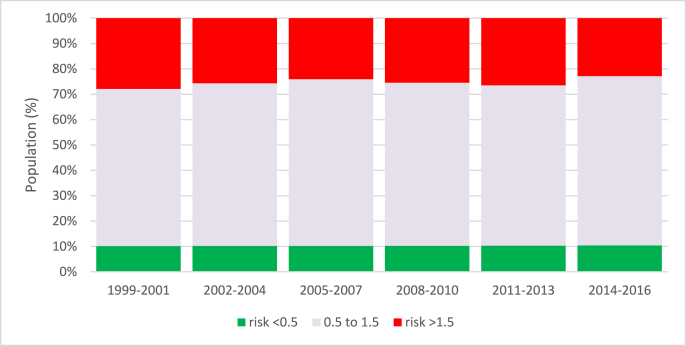
Fig. 5 shows that the share of population living in regions with very high risk of mortality due to a cause of death amenable to healthcare (mortality ratio higher than 1.5) has been decreasing over the last 20 years. In 1999–2001, 27.8% of the population was living in these regions, whereas in 2014–2016 the rate fell to 22.9%. During the financial crisis, however, there was a slight increase (1%) in the share of population living in these areas, i.e., the share of people living in regions with 1.5 times higher risk of dying from an amenable cause of death was larger in 2011–2013 than the period before.
Fig. 5.
Causes of death amenable to healthcare: Share of population living in the NUTS 2 level EU regions by risk of mortality from 1999 to 2001 to 2014–2016. Note: The green bar represents the share of people from EU-26 that live in regions where mortality risk is halve (lower than 0.5). The red bar represents the share of people from EU-26 that live in regions with a 1.5 higher risk of dying from a treatable cause of death. The grey bar represents the people living in the remained regions. (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
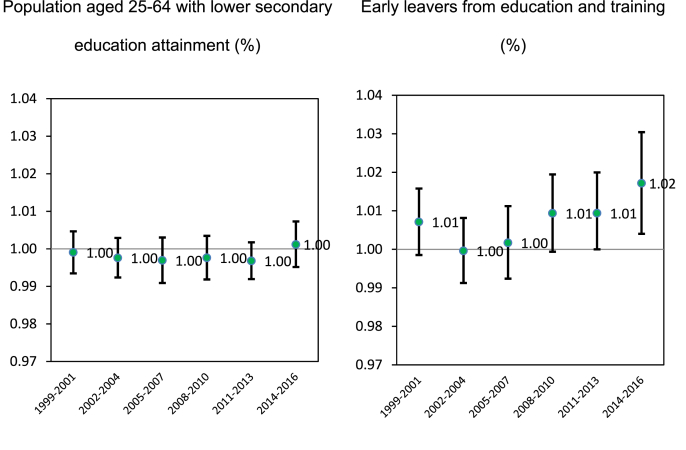
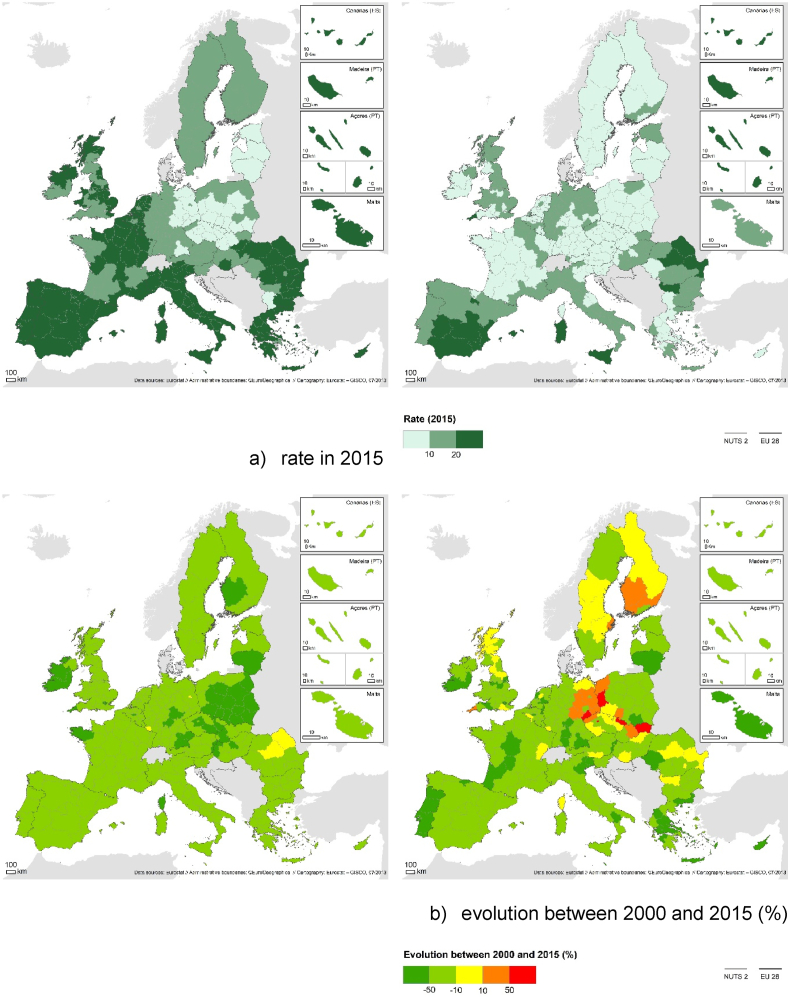
Finally, Fig. 6 provides evidence regarding the association between sSMR due to amenable causes of death due to healthcare and the two education indicators selected for this study. A statistical association was only found for the share of early leavers from education and training, which has been increasing since 2002–2004. This association became significant after the financial crisis and, for the last period of analysis, the relative risk was already 1.02, meaning that a 1% increase in early leavers is associated with a 2% increase in amenable deaths due to healthcare. However, the credible intervals of the risk ratios do not indicate a significant increase over the observed time periods. The regions with high share of early leavers from education and training often register high rates of people actively employed with lower rates of education. Yet, unlike the lower educated workers, the number of early leavers is increasing, especially in regions closer to the border with neighbouring countries (Fig. 7).
Fig. 6.
Relative risk of mortality due to a cause of death amenable to healthcare (RR) in the EU26 in the last 20 years. Note: The dot represents the relative risk. The bars represent the 95% credible interval. Population aged 25–64 with lower secondary education attainment (%) and Early leavers from education and training (%).
Fig. 7.
Geographical pattern and Temporal evaluation of the Education indicators. Note: The two maps on a) represent the share of population aged 25–64 with lower secondary education attainment (map on the left) and the share of early leavers from education and training (map on the right). Darker green represent higher rates. The two maps on b) represent the evolution of the indicators between 2000 and 2015. The map on the left side represents the percentage of evolution on population aged 25–64 with lower secondary education attainment. The map on the right side represents the percentage of evolution on early leavers from education and training. Green colour indicates that the indicator decreased. Red colours indicators that the indicator increased. (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
4. Discussion
Amenable deaths due to healthcare in the EU decreased between 1999 and 2016: the total number of deaths decreased −25.6%, meaning an average decrease of −1.2% of amenable deaths due to healthcare per year, and the share of amenable deaths due to healthcare in total mortality decreased from 35.4% to 32.7%. Nonetheless, the change did not occur equally for the 259 EU regions, as relative inequalities within countries remain, and some regions experienced an increase after the great recession (2011–2013). Also, an association between those deaths and the school dropout rate was identified, revealing that a 1% increase in early leavers from education or training is associated with a 2% increase in amenable deaths due to healthcare.
First, the results point to a substantive decrease in amenable deaths due to healthcare in almost all EU regions between 1999-2001 and 2014–2016 and to a slowdown in the share of people living in regions with a very high risk of mortality due to an amenable cause of death. According to Mackenbach et al. (2016), the decline in amenable deaths due to healthcare was responsible for the decline in absolute inequalities between lower and higher socioeconomic groups, although there is considerable variation across welfare regimes (Leão et al., 2018). However, in this research, in the last study period (2014–2016), almost one quarter of the EU population were living in regions with a mortality ratio higher than 150, that is, 1.5 times higher than the EU pattern. Regions from Eastern countries, as well as those from the United Kingdom and Portugal reveal regions with mortality ratios higher than expected. Finally, a border effect is observed near France, Czechia, Slovakia and Hungary. These regional patterns which highlight the geographical discrepancies within the EU have also been discussed by other researchers, although at country level (Karanikolos et al., 2018; Kossarova et al., 2013; Nagy et al., 2012). Also, a study regarding amenable mortality in Europe in 2011–2013 found that the national context explains 40% of the subnational variation (Rican et al., 2017). Nonetheless, those studies also masked relevant patterns. For example, in this study, some regions from the Netherlands revealed an increase between 1999 and 2016, yet according to Gavurová and Vagasová (Gavurová & Vagašová, 2015), this country was one of the Member States revealing the lowest values in the EU and also recording a significant decrease in amenable deaths due to healthcare in recent decades. Therefore, lowering the geographical scale of analysis is an important tool for delivering insights into regional mortality differences (Deboosere & Gadeyne, 2002).
Second, although amenable death due to healthcare has declined overall, relative inequalities between regions and within countries remain stable through the study period: the countries revealing a higher gap between regions with higher and lower mortality ratio in 1999–2001 are the same in 2014–2016, and the magnitude of inequalities between all EU regions remains stable. Regions in France reveal the lowest amenable deaths due to healthcare ratios during the entire period and, at the same time, the highest gap between the regions with the lowest and the highest ratio. Greece and the United Kingdom also reveal a fourfold gap between regions. This result is in line with that of Mackenbach et al. (2016), albeit at country level, providing evidence that absolute inequalities in mortality between lower and higher socioeconomic groups are declining but relative inequalities have increased overall.
Third, although amenable death due to healthcare has declined overall, some regions located in 17 out of 26 EU countries appeared to experience reversals after 2008–2013. The first regions revealing a significant increase in 2008–2013 were mainly rural, with low population density. In 2011–2013 this pattern was no longer clear. For Belgium, Czechia, Greece, France, Romania and Slovakia, the capital region was the only one revealing an increase. For the United Kingdom, Poland and Hungary, the capital region and other densely populated regions also revealed an increase. Austria and Italy only revealed an increase in regions with low population density (below 100 inhabitants/km2). Also, countries like Germany, the Netherlands and Poland, revealed an increase in relative inequalities between the regions with the lowest and the highest mortality ratio. This reveals a different pattern when compared with previous studies at the country level where researchers only identified increases in amenable mortality due to healthcare following the global financial crisis in Estonia, Slovenia and Greece (Karanikolos et al., 2018) and so concluded that trends in mortality appeared to be unaffected by the crisis in most EU countries (Nelson & Tøge, 2017). Notice that the impact of the economic crisis has been asymmetric between regions within the same country, as well as their capacity to recover (Ballas et al., 2017; Cuadrado-Roura et al., 2016). During the economic crisis, unemployment rose first in regions with labour markets specialized in the construction or manufacturing sectors and the implementation of austerity policies created higher tension in regions with higher dependency on transfers from central governments to provide public amenities like healthcare, social care and education (Giannakis & Bruggeman, 2017, pp. 1394–1415). This deterioration of the quality of life conditions and sudden loss of resources in these regions triggered a rise in social exclusion and poverty rates, increasing the likelihood of having a preventable condition or dying from it (Mackenbach, 2017; Zapata Moya et al., 2015). Thus, the higher the deterioration of the social fabric, the higher the time needed to recover from the crisis.
Finally, amenable deaths due to healthcare are associated with the share of early leavers from education or training. Our results confirm that the relative risk of mortality of amenable causes of death increases 2% for each 1% increase in school dropout rates, and that this association became statistically significant after the crisis (2014–2016), although the credible intervals do not indicate a significant increase over the observed time periods. The education sector also faced, directly and indirectly, the impact of the financial crisis. Thus, the cuts on social benefits and the rise of unemployment decreased families’ capacity to support further education and access to student loans (Barakat et al., 2010). According to human capital theory, an individual invests in education if the expected future stream of benefits exceeds the total costs to acquire education (Pompei & Selezneva, 2019), so, although education helps to escape inactivity, if confidence levels in the future are low, the likelihood of dropping out will be higher (Brunello & Paola, 2014; De Witte et al., 2013). In spite of that, education is the central component of regional development and the key determinant to resilience in an economic crisis, so, to reduce inequalities and enhance spatial homogeneity between regions, it is important to increase educational attainment and maintain a relatively equal educational distribution (Crescenzi et al., 2016; Giannakis & Bruggeman, 2017; OECD, 2015; Panori & Psycharis, 2019). Although these results do not provide insight into the mechanisms underlying the relationship between the economic crisis and education with amenable deaths due to healthcare, some studies shed light on the potential mechanisms that might explain this association.
Regarding the association of amenable deaths due to healthcare with the economic crisis, there are several pathways. First, the decrease on per capita public spending on health impacted upon the provision of health services and created barriers to accessing care and an increase in waiting times, leading to a deterioration in services and large increases in unmet medical need (Karanikolos et al., 2013; Reeves et al., 2014). Second, the increase in the proportion of EU citizens who incurred a rise in out-of-pocket expenditures, or experienced catastrophic expenditures, has consequences for health, namely delaying care which impacts health outcomes, especially for the most vulnerable living in disadvantaged areas (Legido-Quigley et al., 2016; Palladino et al., 2016). Thus, cost constituted one major barrier during the recession period, leading several patients with chronic diseases to cut down on use of medication and adherence to treatments (Sakellarides et al., 2014). Both pathways explain the increase of amenable death due to healthcare in the long-term (Correia et al., 2015; Costa & Santana, 2021; Karanikolos et al., 2013; Legido-Quigley et al., 2016; Perelman et al., 2015). As Karanikolos et al. (2018) state, crisis in itself can pose real threats to health, particularly for vulnerable people through unemployment and loss of income, but the austerity measures applied to the health system exacerbate the issue and further limit access to, and quality of, healthcare services. Research is still in progress, with the pro-cyclical and counter-cyclical effects of the economic crisis yet to be revealed.
Regarding the association of amenable deaths due to healthcare with education, literature offers several explanations. First, the decline in mortality is faster among the more highly educated than among the lesser educated (Mackenbach et al., 2017; Shkolnikov et al., 2012; Strand et al., 2010). Second, countries demonstrating an excess of mortality due to healthcare services also presented large educational inequalities in health in previous studies (Stirbu et al., 2010; von dem Knesebeck et al., 2006). Third, the relative size of the less educated group has diminished over time, whereas that of the more highly educated group has increased (Mackenbach et al., 2016). It is likely that this has led to changes in the composition of these groups; for example, the less educated group has become more homogeneous and/or more extreme in terms of socioeconomic disadvantage (Mackenbach, 2012) and the more highly educated has become more heterogeneous in terms of, for example, the socioeconomic status of their family of origin (Mackenbach et al., 2017). Four, educational gaps are higher among highly preventable health conditions than less preventable ones because the highly educated have better access to new developments and treatments of a health condition classified as highly preventable (Rydland, Solheim, & Eikemo, 2020; Zapata Moya et al., 2015). Finally, the steady increase in the association between education and amenable deaths due to healthcare, especially since 2011–2013, suggests that the financial crisis might have exposed systemic problems which eventually led to the worsening of amenable mortality in some EU regions (Costa & Santana, 2021; Schwandt et al., 2021). Thus, the crisis may have a stronger impact on less-educated people as they are more vulnerable to crisis consequences and have fewer possibilities to access resources that harness indirect health benefits (Mackenbach et al., 2015; Zapata Moya et al., 2015).
Early school dropout is a fundamental factor that significantly increases difficulties in adulthood, namely through a higher risk of unemployment, poverty, sustained dependence on public assistance and social exclusion later in life (De Witte et al., 2013; Mackenbach, 2012; Plenty et al., 2021). Therefore, early leavers are more prone to poor physical and mental health, self-rated health and functional limitations, and more likely to engage in criminal and violent activities (Brunello & Paola, 2014; Smyth & Esri, 2009). According to recent studies, health inequalities between early school leavers and other educational groups are larger in societies with more comprehensive schooling systems as compared to societies with rigidly tracked schooling systems (Delaruelle et al., 2019).
According to Smeyers and Depaepe (2006), school dropout is not the problem itself but an indication and origin of fundamental inequities. As a multi-faceted and complex problem, it is caused by a cumulative process of disengagement, resulting from personal, social, economic, geographical, educational or family-related reasons (OECD, 2012); therefore it requires the identification of causal links and an holistic answer to the problem that often goes beyond health and includes a range of health determinants outside the healthcare sector (De Witte et al., 2013; Santana, Freitas, Costa, et al., 2020).
The Cohesion Funds granted by the European Commission provide a chance to support targeted interventions to health determinants, especially in disadvantaged areas (European Commission Regional Policy, 2014; Santana, Freitas, Costa, et al., 2020). They aim to stimulate, strengthen and support consistent development of EU regions by reducing the existing economic, social, and territorial inequalities through the allocation of funds to disadvantaged areas and sectors (European Commission Regional Policy, 2014). Thus, by allocating funds to the regions where education is lagging behind, cohesion funds may reduce regional inequalities and act as a major driver of health equity (Cuadrado-Roura et al., 2016; Panori & Psycharis, 2019; Santana, Freitas, Costa, et al., 2020).
4.1. Strengths and weaknesses of the study
This paper brings novelty by looking to amenable deaths due to healthcare at subnational level. Previous research identified a general decrease and a weak association with the crisis. This research provides evidence that national level monitoring concealed the struggle of several regions within almost all EU countries regarding the economic crisis that hit Europe, which had consequences for mortality.
This is even more relevant since the COVID-19 pandemic. The disease reveals higher mortality among disadvantaged population groups that already faced issues accessing health and, at the same time, severely compromised all healthcare services. Its long-term impact will be greater than at its outbreak, therefore the availability of a reliable monitoring system at subnational level will be crucial to responding with adequate measures in a timely manner and further decrease amenable deaths due to healthcare in the future.
According to Loney and Nagelkerke (2014), there is no such thing as a perfect ecological study, and all research designs have both strengths and weaknesses. Therefore, several limitations of this study need to be considered.
First, it is not possible to conclude a causal relationship between educational inequalities and amenable deaths due to healthcare since spurious correlations produced by unstudied confounding effects may be present. Caution is also advised due to the ecological fallacy of making individual inferences from aggregate data (Loney & Nagelkerke, 2014). Moreover, results are sensitive to the assumptions of the statistical model (Wu et al., 2020).
Second, it is possible that we are dealing with a modifiable areal unit problem since the spatial unit influences the statistical results and consequent conclusions.
Third, the mortality data is routinely collected through national death registries so there might be issues of comparability between countries (Plug et al., 2012; Stirbu et al., 2010) and this might compromise the results over time and place (Barber et al., 2017; Mackenbach et al., 2016; Nolte & McKee, 2004). The data released by EUROSTAT has a very good level of availability overall. However, a lack of harmonization is evident with many causes of death not available at NUTS2 level or not available for the same periods (Costa et al., 2019a).
Fourth, to some extent, the selection of the causes of death are, time and space specific (Gavurova & Vagasova, 2017; Plug et al., 2012). The causes of death considered for this study provide a set of conditions for which there is a reasonable consensus indicating that personal healthcare has a major effect. However, this does not include all possible causes for which healthcare can improve survival and, by setting the age limit at 75 years to minimize issues with the coding of multi-morbidity, might exclude some potentially amenable deaths in older people, thus reducing the potential of detecting significant changes when low levels have been achieved. It also increases chances of random year-on-year fluctuations in specific amenable causes of deaths due to small numbers. Therefore, comparability with other studies must always take into consideration that the causes of death underlying each study might not be the same.
Fifth, it is possible that other factors explain the geographical pattern of amenable deaths due to healthcare and even its noted association with education, such as public and private health expenditure, geographical accessibility to healthcare, family socioeconomic status or material conditions. Moreover, our results are sensitive to the indicator selected to measure education. Education is a multidimensional theoretical construct that covers a variety of social and financial circumstances and each indicator only partially-captures the full range (Laaksonen et al., 2005). Thus, there might be important cultural differences between countries that influence both education and amenable deaths due to healthcare narrowing the evidence based on cross-country comparisons. For instance, being an early leaver from education in a meritocratic society might have a lower impact on health than in a society with less social mobility (Dibben & Popham, 2011).
Finally, the influence of the economic crisis was not statistically tested so all the assumptions in this paper are based on observational trends. Moreover, the definition of the ‘crisis’ is problematic given how the range of possible economic indicators varied across countries and how the financial crisis impacted on mortality (Karanikolos et al., 2018; Palència et al., 2020).
Despite these limitations, their influence on the outcomes of this study was limited and we were able to give both a comprehensive overview of health inequalities across the EU regions and demonstrate how the education-based gap is related to this pattern. More research is required to understand the potential pathways through which educational measures might influence healthcare utilization and, consequently, amenable deaths due to healthcare.
5. Conclusion
Our results indicate that amenable mortality due to healthcare is decreasing in the European regions. However, inequalities within countries remain and even increased in most countries during the great recession. Moreover, a rise in the association between school dropout rates and amenable deaths due to healthcare becomes apparent throughout the study period.
The evidence of both the geographical pattern and temporal trend, as well as the association with education and the economic crisis, reveals the sensitivity of these causes of death to the contextual determinants and its relevance as a sentinel indicator. Therefore, we need to strengthen monitoring through regular tracking, analysis and reporting on amenable deaths due to healthcare. This will enable detection of regions which are of concern and the recommendation of operational strategies to tackle educational inequalities and further decrease amenable deaths due to healthcare in the future.
Credit author statement
Claudia Costa was responsible for Conceptualization; Data curation; Formal analysis; Funding acquisition; Investigation; Methodology; Roles/Writing - original draft; Writing - review & editing. Paula Santana was responsible for Conceptualization; Formal analysis; Funding acquisition; Investigation; Supervision; Validation; Writing - review & editing.
Declaration of competing interest
None.
Acknowledgments
This research was supported by a Research fellow from the Portuguese Science and Technology Foundation (SFRH/BD/132218/2017) - supported by the budget from the Portuguese Republic, Portugal 2020 and POR_CENTRO programmes and the European Social Fund - and received support from the Centre of Studies in Geography and Spatial Planning (CEGOT), funded by national funds through the Foundation for Science and Technology (FCT) under the reference UIDB/04084/2020.
The authors would like to acknowledge the reviewers for important suggestions that improved this paper, Adriana Loureiro and Ângela Freitas for the insightful comments during the writing of this paper, Tiago Girão and Cátia Leal for giving support to the data collection, Scott Culp and Linda Naughton for English review services and all the researchers from the EURO-HEALTHY project.
Contributor Information
Claudia Costa, Email: claudiampcosta@uc.pt.
Paula Santana, Email: paulasantana@uc.pt.
References
- Arora V.S., Karanikolos M., Clair A., Reeves A., Stuckler D., McKee M. Data resource profile: The European union statistics on income and living conditions (EU-SILC) International Journal of Epidemiology. 2015 doi: 10.1093/ije/dyv069. [DOI] [PubMed] [Google Scholar]
- Bacigalupe A., Esnaola S., Martín U. The impact of the Great Recession on mental health and its inequalities: The case of a Southern European region, 1997-2013. International Journal for Equity in Health. 2016 doi: 10.1186/s12939-015-0283-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ballas D., Dorling D., Hennig B. A human cartographic perspective. Vol. 51. 2017. 2017. Analysing the regional geography of poverty, austerity and inequality in Europe. [Google Scholar]
- Bambra C. In: Hurrelmann K., Shaikh M., Wendt C., editors. Oxford University Press; 2019. Governing health inequalities; pp. 5–66. (The governance report 2019). [Google Scholar]
- Barakat B., Holler J., Prettner K., Schuster J. Pap; Work: 2010. The impact of the economic crisis on labour and education in Europe. [Google Scholar]
- Barber R.M., Fullman N., Sorensen R.J.D., et al. Healthcare access and quality index based on mortality from causes amenable to personal health care in 195 countries and territories, 1990-2015: A novel analysis from the global burden of disease study 2015. Lancet. 2017;390:231–266. doi: 10.1016/S0140-6736(17)30818-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becker S., Egger P., von Ehrlich M. Going NUTS: The effect of EU structural funds on regional performance. Journal of Public Economics. 2010;94:578–590. doi: 10.1016/j.jpubeco.2010.06.006. 2009. [DOI] [Google Scholar]
- Bergqvist K., Yngwe M.Å., Lundberg O. Understanding the role of welfare state characteristics for health and inequalities - an analytical review. BMC Public Health. 2013 doi: 10.1186/1471-2458-13-1234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Besag J., York J., Mollié A., Molli A. Bayesian image restoration, with two applications in spatial statistics. Annals of the Institute of Statistical Mathematics. 1991;43:1–20. doi: 10.1007/BF00116466. [DOI] [Google Scholar]
- Borrell C., Palència L., Marí Dell'Olmo M., Morrisson J., Deboosere P., Gotsens M., Dzurova D., Costa C., Lustigova M., Burstrom B., Rodríguez-Sanz M., Bosakova L., Zengarini N., Katsouyanni K., Santana P. Socioeconomic inequalities in suicide mortality in European urban areas before and during the economic recession. The European Journal of Public Health. 2019 doi: 10.1093/eurpub/ckz125. [DOI] [PubMed] [Google Scholar]
- Brunello G., Paola M. De. The costs of early school leaving in Europe. IZA Journal of Labor Policy. 2014 doi: 10.1186/2193-9004-3-22. [DOI] [Google Scholar]
- Charlton J., Silver R., Hartley R.M., Holland W.W. Geographical variation in mortality from conditions amenable to medical intervention in England and Wales. Lancet. 1983;321:691–696. doi: 10.1016/S0140-6736(83)91981-5. [DOI] [PubMed] [Google Scholar]
- Clench-Aas J., Holte A. The financial crisis in Europe: Impact on satisfaction with life. Scandinavian Journal of Public Health. 2017 doi: 10.1177/1403494817718692. [DOI] [PubMed] [Google Scholar]
- Correia T., Dussault G., Pontes C. Health Policy; New. York: 2015. The impact of the financial crisis on human resources for health policies in three southern-Europe countries. [DOI] [PubMed] [Google Scholar]
- Costa C., Freitas Â., Stefanik I., Krafft T., Pilot E., Morrison J., Santana P. Evaluation of data availability on population health indicators at the regional level across the European Union. Population Health Metrics. 2019;17:11. doi: 10.1186/s12963-019-0188-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costa C.C., Santana P. Gender and age differences in socioeconomic inequalities in total and avoidable mortality in Portugal: A trend analysis. Journal of Fiscal Studies. 2021;42:123–145. doi: 10.1111/1475-5890.12264. [DOI] [Google Scholar]
- Costa C., Santana P., Dimitroulopoulou S., Burstrom B., Borrell C., Schweikart J., Dzurova D., Zangarini N., Katsouyanni K., Deboseree P., Freitas Â., Mitsakou C., Samoli E., Vardoulakis S., Dell'Olmo M.M., Gotsens M., Lustigova M., Corman D., Costa G. Population health inequalities across and within european metropolitan areas through the lens of the euro-healthy population health index. International Journal of Environmental Research and Public Health. 2019;16 doi: 10.3390/ijerph16050836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crescenzi R., Luca D., Milio S. The geography of the economic crisis in Europe: National macroeconomic conditions, regional structural factors and short-term economic performance. Cambridge Journal of Regions, Economy and Society. 2016;9:13–32. doi: 10.1093/CJRES/RSV031. [DOI] [Google Scholar]
- Cuadrado-Roura J.R., Martin R., Rodríguez-Pose A. The economic crisis in Europe: Urban and regional consequences. Cambridge Journal of Regions, Economy and Society. 2016;9:3–11. doi: 10.1093/CJRES/RSV036. [DOI] [Google Scholar]
- Cylus J., Pearson M. In: Thomson S., Figueras J., Evetovits T., Mladovsky P., Maresso A., Cylus J., Karanikolos M., Kluge H., editors. 2015. The crisis and its implications for household financial security, government resources and health expenditure. (Economic crisis, health systems and health in Europe. European observatory on health systems and policies). [PubMed] [Google Scholar]
- De Witte K., Cabus S., Thyssen G., Groot W., Van Den Brink H.M. A critical review of the literature on school dropout. Educational Research Review. 2013 doi: 10.1016/j.edurev.2013.05.002. [DOI] [Google Scholar]
- Deaton A. John Hopkins University Press; Baltimore MD: 1997. Analysis of household surveys. [Google Scholar]
- Deboosere P., Gadeyne S. Can regional patterns of mortality in Belgium be explained by individual socio-economic characteristics. Reflets Perspect. la Vie Econ. 2002 doi: 10.3917/rpve.414.0087. [DOI] [Google Scholar]
- Delaruelle K., van de Werfhorst H., Bracke P. Do comprehensive school reforms impact the health of early school leavers? Results of a comparative difference-in-difference design. Social Science & Medicine. 2019;239:112542. doi: 10.1016/j.socscimed.2019.112542. [DOI] [PubMed] [Google Scholar]
- Dibben C., Popham F. Are socio-economic groupings the most appropriate method for judging health equity between countries? Journal of Epidemiology & Community Health. 2011 doi: 10.1136/jech.2009.102491. [DOI] [PubMed] [Google Scholar]
- Doetsch J., Pilot E., Santana P., Krafft T. Potential barriers in healthcare access of the elderly population influenced by the economic crisis and the troika agreement: A qualitative case study in Lisbon, Portugal. International Journal for Equity in Health. 2017;16 doi: 10.1186/s12939-017-0679-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eksler V., Lassarre S., Thomas I. Regional analysis of road mortality in Europe. Public Health. 2008;122:826–837. doi: 10.1016/j.puhe.2007.10.003. [DOI] [PubMed] [Google Scholar]
- European Commission Regional Policy . 2014. Making Europe's regions and cities more competitive, fostering growth and creating jobs. Brussels. [Google Scholar]
- EUROSTAT . 2014. Specifications of the public health theme tables (hlth_cd_pbt) [Google Scholar]
- Freitas Â., Santana P., Oliveira M.D., Almendra R., Bana E Costa J.C., Bana E Costa C.A. Indicators for evaluating European population health: A Delphi selection process. BMC Public Health. 2018;18:557. doi: 10.1186/s12889-018-5463-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gavurová B., Vagašová T. The significance of amenable mortality quantification for financing the health system in Slovakia. Procedia Economics and Finance. 2015;32:77–86. doi: 10.1016/s2212-5671(15)01367-2. [DOI] [Google Scholar]
- Gavurova B., Vagasova T. Advances in health management. 2017. Assessment of avoidable mortality concepts in the European union countries, their benefits and limitations. [DOI] [Google Scholar]
- Giannakis E., Bruggeman A. Determinants of regional resilience to economic crisis. A European perspective. 2017;25:1394–1415. doi: 10.1080/09654313.2017.1319464. [DOI] [Google Scholar]
- Hoffmann R., Borsboom G., Saez M., Mari Dell'Olmo M., Burström B., Corman D., Costa C., Deboosere P., Domínguez-Berjón M.F., Dzúrová D., Gandarillas A., Gotsens M., Kovács K., Mackenbach J., Martikainen P., Maynou L., Morrison J., Palència L., Pérez G.…Borrell C. Social differences in avoidable mortality between small areas of 15 European cities: An ecological study. International Journal of Health Geographics. 2014;13 doi: 10.1186/1476-072X-13-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holland W. Avoidable death as a measure of quality. International Journal for Quality in Health Care. 1990 doi: 10.1093/intqhc/2.3-4.227. [DOI] [PubMed] [Google Scholar]
- Kaplan G.A. Economic crises: Some thoughts on why, when and where they (might) matter for health-A tale of three countries. Social Science & Medicine. 2012 doi: 10.1016/j.socscimed.2011.12.013. [DOI] [PubMed] [Google Scholar]
- Karanikolos M., Mackenbach J.P., Nolte E., Stuckler D., McKee M. Amenable mortality in the EU—has the crisis changed its course? The European Journal of Public Health. 2018;28:864–869. doi: 10.1093/eurpub/cky116. [DOI] [PubMed] [Google Scholar]
- Karanikolos M., Mladovsky P., Cylus J., Thomson S., Basu S., Stuckler D., MacKenbach J.P., McKee M. Financial crisis, austerity, and health in Europe. Lancet. 2013 doi: 10.1016/S0140-6736(13)60102-6. [DOI] [PubMed] [Google Scholar]
- Karanikolos M., Nolte E. Interpreting health systems performance indicators: More complex than it looks? Lancet Public Health. 2018;3:E207–E208. doi: 10.1016/S2468-2667(18)30076-8. [DOI] [PubMed] [Google Scholar]
- von dem Knesebeck O., Verde P.E., Dragano N. Education and health in 22 European countries. Social Science & Medicine. 2006;63:1344–1351. doi: 10.1016/j.socscimed.2006.03.043. [DOI] [PubMed] [Google Scholar]
- Kossarova L., Holland W., Mossialos E. “Avoidable” mortality: A measure of health system performance in the Czech Republic and Slovakia between 1971 and 2008. Health Policy and Planning. 2013;28:508–525. doi: 10.1093/heapol/czs093. [DOI] [PubMed] [Google Scholar]
- Laaksonen M., Rahkonen O., Martikainen P., Lahelma E. Socioeconomic position and self-rated health: The contribution of childhood socioeconomic circumstances, adult socioeconomic status, and material resources. American Journal of Public Health. 2005;95:1403–1409. doi: 10.2105/AJPH.2004.047969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leão T., Campos-Matos I., Bambra C., Russo G., Perelman J. Welfare states, the Great Recession and health: Trends in educational inequalities in self-reported health in 26 European countries. PLoS One. 2018 doi: 10.1371/journal.pone.0193165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Legido-Quigley H., Karanikolos M., Hernandez-Plaza S., de Freitas C., Bernardo L., Padilla B., Sá Machado R., Diaz-Ordaz K., Stuckler D., McKee M. Health Policy; New. York: 2016. Effects of the financial crisis and Troika austerity measures on health and health care access in Portugal. [DOI] [PubMed] [Google Scholar]
- Lochner L. Handbook of the economics of education. 2011. Non-production benefits of education : Crime, health, and good citizenship. [Google Scholar]
- Loney T., Nagelkerke N.J. The individualistic fallacy, ecological studies and instrumental variables: A causal interpretation. Emerging Themes in Epidemiology. 2014 doi: 10.1186/1742-7622-11-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mackenbach J.P. The persistence of health inequalities in modern welfare states: The explanation of a paradox. Social Science & Medicine. 2012 doi: 10.1016/j.socscimed.2012.02.031. [DOI] [PubMed] [Google Scholar]
- Mackenbach J.P. Nordic paradox, southern miracle, Eastern disaster: Persistence of inequalities in mortality in Europe. The European Journal of Public Health. 2017;27:14–17. doi: 10.1093/EURPUB/CKX160. [DOI] [PubMed] [Google Scholar]
- Mackenbach J.P., Kulhánová I., Artnik B., Bopp M., Borrell C., Clemens T., Costa G., Dibben C., Kalediene R., Lundberg O., Martikainen P., Menvielle G., Östergren O., Prochorskas R., Rodríguez-Sanz M., Strand B.H., Looman C.W.N., De Gelder R. Changes in mortality inequalities over two decades: Register based study of European countries. BMJ. 2016 doi: 10.1136/bmj.i1732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mackenbach J.P., Kulhánová I., Bopp M., Deboosere P., Eikemo T.A., Hoffmann R., Kulik M.C., Leinsalu M., Martikainen P., Menvielle G., Regidor E., Wojtyniak B., Östergren O., Lundberg O., EURO-GBD-SE Consortium Variations in the relation between education and cause-specific mortality in 19 European populations: A test of the “fundamental causes” theory of social inequalities in health. Social Science & Medicine. 2015;127:51–62. doi: 10.1016/j.socscimed.2014.05.021. [DOI] [PubMed] [Google Scholar]
- Mackenbach J.P., Looman C.W.N., Artnik B., Bopp M., Deboosere P., Dibben C., Kalediene R., Kovács K., Leinsalu M., Martikainen P., Regidor E., Rychtaříková J., de Gelder R. ‘Fundamental causes’ of inequalities in mortality: An empirical test of the theory in 20 European populations. Sociology of Health & Illness. 2017;39:1117–1133. doi: 10.1111/1467-9566.12562. [DOI] [PubMed] [Google Scholar]
- Mackenbach J.P., Looman C.W.N., Kunst A.E., Habbema J.D.F., van der Maas P.J. Post-1950 mortality trends and medical care: Gains in life expectancy due to declines in mortality from conditions amenable to medical intervention in The Netherlands. Social Science & Medicine. 1988 doi: 10.1016/0277-9536(88)90278-X. [DOI] [PubMed] [Google Scholar]
- Mackenbach J.P., Stirbu I., Roskam A.-J.R., Schaap M.M., Menvielle G., Leinsalu M., Kunst A.E. Socioeconomic inequalities in health in 22 European countries. New England Journal of Medicine. 2008;358:2468–2481. doi: 10.1056/nejmsa0707519. [DOI] [PubMed] [Google Scholar]
- Marmot M. Health inequalities in the EU - final report of a consortium. 2013. [DOI]
- McMinn M.A., Seaman R., Dundas R., Pell J.P., Leyland A.H. 2020. Socio-economic inequalities in rates of amenable mortality in Scotland: Analyses of the fundamental causes using the Scottish Longitudinal Study, 1991–2010. (Population, space and place). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Middleton N., Sterne J.A.C., Gunnell D. The geography of despair among 15-44-year-old men in England and wales: Putting suicide on the map. Journal of Epidemiology & Community Health. 2006;60:1040–1047. doi: 10.1136/jech.2005.045302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nagy C., Juhasz A., Beale L., Paldy A. Mortality amenable to health care and its relation to socio-economic status in Hungary, 2004-08. The European Journal of Public Health. 2012;22:620–624. doi: 10.1093/eurpub/ckr143. [DOI] [PubMed] [Google Scholar]
- Nelson K., Tøge A.G. Health trends in the wake of the financial crisis - increasing inequalities? Scandinavian Journal of Public Health. 2017 doi: 10.1177/1403494817707088. [DOI] [PubMed] [Google Scholar]
- Nolte E., McKee M. The Nuffield Trust; 2004. Does healthcare save lives ? avoidable mortality revisited. [Google Scholar]
- Nolte E., Scholz R., Shkolnikov V., McKee M. The contribution of medical care to changing life expectancy in Germany and Poland. Social Science & Medicine. 2002 doi: 10.1016/S0277-9536(01)00320-3. [DOI] [PubMed] [Google Scholar]
- OECD . 2012. Equity and quality in education. Supporting disadvantaged students and schools. [DOI] [Google Scholar]
- OECD . OECD Publishing; Paris: 2015. In it together: Why less inequality benefits all. (It together: Why less inequality benefits all). [DOI] [Google Scholar]
- Palència L., Gotsens M., Marí-Dell’Olmo M., Bosakova L., Burström B., Costa C., Deboosere P., Dzurova D., Lustigova M., Morrison J., Santana P., Borrell C. Effect of the recent economic crisis on socioeconomic inequalities in mortality in nine urban areas in Europe. Gaceta Sanitaria. 2020;34 doi: 10.1016/j.gaceta.2019.11.001. [DOI] [PubMed] [Google Scholar]
- Palladino R., Lee J.T., Hone T., Filippidis F., Millett C. The great recession and increased cost sharing in European health systems. Health Affairs. 2016;35:1204–1213. doi: 10.1377/hlthaff.2015.1170. [DOI] [PubMed] [Google Scholar]
- Panori A., Psycharis Y. Exploring the links between education and income inequality at the municipal level in Greece. Applied Spatial Analysis and Policy. 2019;12:101–126. doi: 10.1007/S12061-017-9234-6/TABLES/6. [DOI] [Google Scholar]
- Perelman J., Felix S., Santana R. Health Policy; New. York: 2015. The Great Recession in Portugal: Impact on hospital care use. [DOI] [PubMed] [Google Scholar]
- Pereyra-Zamora P., Copete J.M., Oliva-Arocas A., Caballero P., Moncho J., Vergara-Hernández C., Nolasco A. Changes in socioeconomic inequalities in amenable mortality after the economic crisis in cities of the Spanish Mediterranean coast. International Journal of Environmental Research and Public Health. 2020;17 doi: 10.3390/ijerph17186489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phelan J.C., Link B.G., Tehranifar P. Social conditions as fundamental causes of health inequalities: Theory, evidence, and policy implications. Journal of Health and Social Behavior. 2010 doi: 10.1177/0022146510383498. [DOI] [PubMed] [Google Scholar]
- Plenty S., Magnusson C., Laftman S.B. Internalising and externalising problems during adolescence and the subsequent likelihood of being Not in Employment, Education or Training (NEET) among males and females: The mediating role of school performance. Social Science Medicine - Popul. Heal. 2021;12 doi: 10.1016/j.ssmph.2021.100873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Plug I., Hoffmann R., Artnik B., Bopp M., Borrell C., Costa G., Deboosere P., Esnaola S., Kalediene R., Leinsalu M., Lundberg O., Martikainen P., Regidor E., Rychtarikova J., Strand B.H., Wojtyniak B., Mackenbach J.P. Socioeconomic inequalities in mortality from conditions amenable to medical interventions: Do they reflect inequalities in access or quality of health care? BMC Public Health. 2012;12:346. doi: 10.1186/1471-2458-12-346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pompei F., Selezneva E. Unemployment and education mismatch in the EU before and after the financial crisis. Journal of Policy Modeling. 2019 doi: 10.1016/j.jpolmod.2019.09.009. [DOI] [Google Scholar]
- Popham F., Iannelli C. Does comprehensive education reduce health inequalities? Social Science Medicine - Popul. Heal. 2021;15 doi: 10.1016/j.ssmph.2021.100834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reeves A., Basu S., McKee M., Marmot M., Stuckler D. Austere or not? UK coalition government budgets and health inequalities. Journal of the Royal Society of Medicine. 2013 doi: 10.1177/0141076813501101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reeves A., McKee M., Basu S., Stuckler D. The political economy of austerity and healthcare: Cross-national analysis of expenditure changes in 27 European nations 1995–2011. Health Policy (New. York) 2014;115:1–8. doi: 10.1016/j.healthpol.2013.11.008. [DOI] [PubMed] [Google Scholar]
- Rican S., Tenailleau Q., Squiban C., Costa C. In: Santana P., editor. Coimbra University Press; Coimbra: 2017. Healthcare access and avoidable mortality; pp. 53–59. (Promoting population health and equity in Europe. From evidence to policy). [DOI] [Google Scholar]
- Rosella L., Kornas K., Huang A., Grant L., Bornbaum C., Henry D. Population risk and burden of health behavioralerelated all-cause,premature, and amenable deaths in Ontario, Canada: Canadian Community health survey linked mortality files. Annals of Epidemiology. 2019;32:49–57. doi: 10.1016/j.annepidem.2019.01.009. [DOI] [PubMed] [Google Scholar]
- Rutstein D.D., Berenberg W., Chalmers T.C., Child C.G., Fishman A.P., Perrin E.B., Feldman J.J., Leaverton P.E., Lane J.M., Sencer D.J., Rutstein D.D. Measuring the quality of medical care: A clinical method. New England Journal of Medicine. 1976 doi: 10.1056/NEJM197603112941104. [DOI] [PubMed] [Google Scholar]
- Rydland H.T., Fjaer E.L., Eikemo T.A., Huijts T., Bambra C., Wendt C., Kulhánová I., Martikainen P., Dibben C., Kalèdiené R., Borrell C., Leinsalu M., Bopp M., Mackenbach J.P. Educational inequalities in mortality amenable to healthcare. A comparison of European healthcare systems. PLoS One. 2020;15 doi: 10.1371/journal.pone.0234135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rydland H.T., Solheim E.F., Eikemo T.A. Educational inequalities in high- vs. low-preventable health conditions: Exploring the fundamental cause theory. Social Science & Medicine. 2020;267 doi: 10.1016/J.SOCSCIMED.2020.113145. [DOI] [PubMed] [Google Scholar]
- Sakellarides C., Castelo-Branco L., Barbosa P., Azevedo H. Europea Observatory on Health systems and Policies. 2014. The impact of the financial crisis on the health system and health in Portugal. [Google Scholar]
- Santana P. A mortalidade evitável em Portugal continental, 1989 a 1993. Rev Cent Estud Demograficos. 2002:107–145. [Google Scholar]
- Santana P., Costa C., Freitas Â., Stefanik I., Quintal C., Bana e Costa C., Borrell C., et al. In: Imprensa d., editor. 2017. Atlas of population health in European Union regions. (Imprensa da Universidade de Coimbra). Coimbra. [DOI] [Google Scholar]
- Santana P., Costa C., Marí-Dell’Olmo M., Gotsens M., Borrell C. Mortality, material deprivation and urbanization: Exploring the social patterns of a metropolitan area. International Journal for Equity in Health. 2015;14 doi: 10.1186/s12939-015-0182-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santana P., Freitas Â., Costa C., Stefanik I., Santinha G., Krafft T., Pilot E. The role of cohesion policy funds in decreasing the health gaps measured by the euro-healthy population health index. International Journal of Environmental Research and Public Health. 2020;17 doi: 10.3390/ijerph17051567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santana P., Freitas Â., Stefanik I., Costa C., Oliveira M., Rodrigues T.C.T.C., Vieira A., Ferreira P.L.P.L., Borrell C., Dimitroulopoulou S., Rican S., Mitsakou C., Marí-Dell’Olmo M., Schweikart J., Corman D., Bana E Costa C.A.C.A., Quintal C., Malva J., Cunha L.…Zengarini N. Advancing tools to promote health equity across European Union regions: The EURO-HEALTHY project. Health Research Policy and Systems. 2020;18:18. doi: 10.1186/s12961-020-0526-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sauerberg M. The impact of population's educational composition on Healthy Life Years: An empirical illustration of 16 European countries. Social Science Medicine - Popul. Heal. 2021;15 doi: 10.1016/j.ssmph.2021.100857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schrödle B., Held L. A primer on disease mapping and ecological regression using INLA. Computational Statistics. 2011 doi: 10.1007/s00180-010-0208-2. [DOI] [Google Scholar]
- Schwandt H., Currie J., Bar M., Banks J., Bertoli P., Butikofer A., Cattan S., Zong-Ying Chao B., Costa C., Gonzalez L., Grembi V., Huttunen K., Lombardi S., Redler P., Riumallo-Herl C., Rodríguez-González A., Salvanes K., Santana P., Thuilliez J.…Wuppermann A. Inequality in mortality between black and white Americans by age, place, and cause, and in comparison to Europe, 1990-2018. Proceedings of the National Academy of Sciences of the United States of America. 2021;118 doi: 10.1073/pnas.2104684118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shkolnikov V.M., Andreev E.M., Jdanov D.A., Jasilionis D., Kravdal Ø., Vågerö D., Valkonen T. Increasing absolute mortality disparities by education in Finland, Norway and Sweden, 1971-2000. Journal of Epidemiology & Community Health. 2012 doi: 10.1136/jech.2009.104786. [DOI] [PubMed] [Google Scholar]
- Smeyers P., Depaepe M. Educ. Res. Why ’What Work. Doesn’t Work. 2006. Introduction: On the rhetoric of “what works” contextualizing educational research and the picture of performativity. [DOI] [Google Scholar]
- Smyth E., Esri S.M. Investing in education: Combating educational disadvantage. ESRI. 2009 [Google Scholar]
- Stirbu I., Kunst A.E., Bopp M., Leinsalu M., Regidor E., Esnaola S., Costa G., Martikainen P., Borrell C., Deboosere P., Kalediene R., Rychtarikova J., Artnik B., Mackenbach J.P. Educational inequalities in avoidable mortality in Europe. Journal of Epidemiology & Community Health. 2010;64:913–920. doi: 10.1136/jech.2008.081737. [DOI] [PubMed] [Google Scholar]
- Strand B.H., Grøholt E.K., Steingrímsdóttir Ó.A., Blakely T., Graff-Iversen S., Næss Ø. Educational inequalities in mortality over four decades in Norway: Prospective study of middle aged men and women followed for cause specific mortality, 1960-2000. BMJ. 2010 doi: 10.1136/bmj.c654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tobias M., Yeh L.-C. How much does health care contribute to health gain and to health inequality? Trends in amenable mortality in New Zealand 1981-2004. Australian & New Zealand Journal of Public Health. 2009;33:70–78. doi: 10.1111/j.1753-6405.2009.00342.x. [DOI] [PubMed] [Google Scholar]
- Witkam R., Gwinnutt J., Humphreys J., Gandrup J., Cooper R., Vestappen S. Do associations between education and obesity vary depending on the measure of obesity used? A systematic literature review and meta-analysis. Social Science Medicine - Popul. Heal. 2021;15 doi: 10.1016/j.ssmph.2021.100884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu X., Nethery R.C., Sabath M.B., Braun D., Dominici F. Air pollution and COVID-19 mortality in the United States: Strengths and limitations of an ecological regression analysis. Science Advances. 2020 doi: 10.1126/SCIADV.ABD4049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zapata Moya A.R., Buffel V., Navarro Yáñez C.J., Bracke P. Social inequality in morbidity, framed within the current economic crisis in Spain. International Journal for Equity in Health. 2015;14:1–20. doi: 10.1186/S12939-015-0217-4/TABLES/7. [DOI] [PMC free article] [PubMed] [Google Scholar]