Abstract
Objective:
In the United States, people of color (POC) are disproportionately affected by various sources of stress and prevalent mental and physical health issues that may benefit from Mindfulness-based Interventions (MBIs). However, effects of MBIs for POC are unclear. This meta-analysis examines the efficacy of MBIs through randomized controlled trials (RCTs) that included predominately POC (≥75% of the sample).
Method:
Random effects models were used to synthesize effect sizes. A total of 24 RCT samples were analyzed.
Results:
Samples were on average 94.4% POC and predominantly from low-income backgrounds (total N = 2,156). At post-treatment, MBIs yielded small but statistically superior outcomes to active controls (Hedges’ g = 0.11) and inactive controls (g = 0.26). Compared to active controls, MBIs’ effects on well-being were smaller than their effects on other outcome types. Compared to inactive controls, MBIs that focused on non-clinical populations and had higher proportion of POC had larger effect sizes. Attrition rates of MBIs did not differ from other active conditions in outpatient settings.
Conclusion:
Findings provide modest, preliminary empirical support for MBIs among POC. We discuss main findings, limitations, and implications for future MBI research for health promotion among POC.
Keywords: mindfulness, meta-analysis, racial/ethnic minorities, evidence-based treatments
People of color (POC)1 in the United States (U.S.) are disproportionately affected by various structural inequalities such as mass incarceration (Wildeman & Wang, 2017), racism (Bailey et al., 2017), and housing and economic difficulties (Zimmerman & Anderson, 2019). Cumulatively, such adversities harm the well-being of POC (Bailey et al., 2017; Wildeman & Wang, 2017; Zimmerman & Anderson, 2019). POC show high rates of psychological and physical health issues, such as depressive symptomology (Bailey, Mokonogho, & Kumar, 2019), risk of trauma exposure and Post-Traumatic Stress Disorder (PTSD) (Asnaani & Hall-Clark, 2017), hypertension and cardiovascular disease (Balfour, Rodriguez, & Ferdinand, 2015), and HIV/AIDS (Millett et al., 2012). Further, racial disparities exist in mental health treatment and healthcare: POC are less likely to utilize and more likely to prematurely withdraw from services (Cooper & Conklin, 2015; McClendon, Dean, & Galovski, 2020), resulting in limited benefits of usual care and more persistent conditions (e.g., depression chronicity) (Bailey et al., 2019). Various factors contribute to this reduced health service utilization, such as mistrust of providers and health systems; negative attitudes (e.g., stigma) toward seeking professional psychological help; and the lack of affordable, culturally competent services (Atdjian & Vega, 2005; Sun, Hoyt, Brockberg, Lam, & Tiwari, 2016).
Recent decades have witnessed the rapid growth of research in mindfulness (Goldberg, Riordan, Sun, & Davidson, 2021), which can be defined as “paying attention in a particular way, on purpose, in the present moment, and nonjudgmentally” (Kabat-Zinn, 1994, p. 4). Mindfulness-based interventions (MBIs), such as Mindfulness-based Stress Reduction (MBSR) (Kabat-Zinn, 1990) and Mindfulness-based Cognitive Therapy (MBCT) (Teasdale et al., 2000), often utilize a group format and employ an experiential learning approach to foster mindfulness. Meta-analyses have demonstrated MBIs’ efficacy in improving health outcomes among conditions that are prevalent among POC, such as psychiatric symptoms (Galante et al., 2021; Goldberg et al., 2018), HIV/AIDS (Scott-Sheldon et al., 2018), cardiovascular conditions (Abbott et al., 2014) and hypertension (Lee et al., 2020). Thus, MBIs could potentially offer transdiagnostic efficacy and benefits to POC.
However, POC have been underrepresented in MBI research. A systematic review of demographic characteristics in 69 RCTs of MBSR and MBCT in the U.S. found that among the 45 studies that reported data on race and income, 76% participants identified as non-Hispanic White and most studies had more than half of participants making over $40,000 annually (Waldron, Hong, Moskowitz, & Burnett-Zeigler, 2018). These demographics contrast the racial/ethnic and socioeconomic diversity in the general U.S. population (60.4% non-Hispanic White, per capita 12-month income of $32,621; Unites States Census Bureau, 2019). Thus, the efficacy of MBIs among POC is unclear, in part due to limited research.
Further, extent literature suggests mixed findings regarding the acceptability of MBIs to POC. Some scholars have argued that certain aspects of MBIs are especially culturally relevant to POC including attention to overall health and well-being; emphasis on resilience rather than psychopathology; and the group-based, communal delivery formats (LoParo, Mack, Patterson, Negi, & Kaslow, 2018; Woods-Giscombé & Gaylord, 2014). Therefore, although not designed to address provider- or systemic- level factors such as institutional racism or health policy, as a patient/client-level intervention, MBIs may provide a feasible, relevant, and efficacious approach to ameliorate the burden of health disparities and enhance health outcomes among POC (e.g., Woods-Giscombé & Gaylord, 2014). However, evidence on acceptability has been mixed. Using the National Health Interview Survey data, Olano et al. (2015) found lower engagement in mindfulness practices among non-Hispanic Blacks and Hispanics relative to non-Hispanic Whites (Olano et al., 2015). In contrast, a recent study found Hispanic veterans were more likely to report using meditation in the past year compared to non-Hispanic White veterans (Goldberg et al., 2019). If acceptability of MBIs is low among POC, adaptation to improve MBIs’ fit and cultural relevancy may be needed to achieve their full potential.
The dearth of research and mixed findings of MBIs among POC limits our understanding of the utility and efficacy of MBIs for this population. While prior reviews have clarified the relative lack of representation of POC within MBI research (Waldron et al., 2018) and few instances of cultural adaptation (DeLuca, Kelman, & Waelde, 2018), no review has actually evaluated the efficacy and acceptability of MBIs among POC. A quantitative synthesis of research in this area can help clarify the empirical promise of this intervention approach.
Present Study
The current systematic review and meta-analysis was conducted to characterize the efficacy of MBIs in POC in the United States. As with any evidence-based intervention (American Psychological Association, 2006), understanding the efficacy of MBIs in specific populations, particularly marginalized and underserved populations (who tend to engage less in conventional, evidence-based treatment, Alegría, Alvarez, Ishikawa, DiMarzio, & McPeck, 2016), is crucial to broaden the application of MBIs and evaluate their potential for improving population health. Thus, the primary aim of the study was to systematically review available RCTs testing MBIs for POC and conduct a meta-analysis examining the efficacy of MBIs for POC. Acceptability of MBIs compared to other active controls was also evaluated. In addition, we aimed to explore study characteristics that may moderate treatment effects to inform future intervention trials (e.g., sample and intervention characteristics, outcome type).
Method
This meta-analysis was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement (Moher, Liberati, Tetzlaff, Altman, & the PRISMA Group, 2009). The study was registered in a public systematic review registry (PROSPERO; CRD42019124968).
Eligibility Criteria
To be included, studies needed to (a) be written in English, (b) take place in the U.S., (c) include an RCT that had an intervention and a control condition, and (d) include at least 75% POC in the full sample. The 75% threshold was selected for two main reasons. First, social science research shows that the “tipping point” of a majority representation is 75% for the group to remain relatively homogenous in terms of culture and social norms (Centola, Becker, Brackbill, & Baronchelli, 2018). Second, previous review regarding mindfulness for POC used this cutoff (DeLuca et al., 2018), which allows comparison between the current study and prior work in this area. In addition, eligible studies need to include a mindfulness-based intervention, which is defined in consistence with previous meta-analyses on MBIs (e.g., Goldberg et al., 2018; Dunning et al., 2019) and the conceptual definition of mindfulness-based programs (Crane et al., 2017). Specifically, eligible studies needed to (e) include mindfulness meditation as a core component of the intervention condition (Crane et al., 2017) and (f) include MBIs of at least two sessions so that participants had an opportunity to engage in home practice of mindfulness-based meditation (e.g., brief inductions were excluded). Treatments that emphasized the attitudinal stance of mindfulness (e.g., Acceptance and Commitment Therapy) or incorporated mindfulness as one the several treatment components (e.g., Dialectical Behavioral Therapy) were excluded. Compassion-based interventions that did not use mindfulness as a major component of the treatment were also excluded. In addition, eligible studies also needed to (g) use a randomized controlled design, (h) have a non-mindfulness control group, and (i) report data necessarily for computing for effect sizes (e.g., means and standard deviations, t- or F-statistics).
Information Sources
We identified studies by conducting searches on PsycINFO, ProQuest, PubMed, and ProQuest Dissertations and Theses to find published or unpublished English-language studies that reported data based on RCTs. A clinical trials register (www.clinicaltrials.gov) was also searched to detect potential completed trials that had not yet been published.
Search
We completed the search in January 2021 using search terms “mindfulness” and “randomized”, combined with “racial minority” or “ethnic minority” or “African American” or “Black” or “Asian” or “Latino/a/x” or “Hispanic” or “Mexican American” or “Native American” or “Pacific Islander.” Search terms in each dataset are reported in Supplemental Table 1.
Study Selection
The first and second authors independently completed coding of potential eligible studies for inclusion. Both individuals are PhD-level psychologists with previous experience conducting meta-analyses. Disagreements were discussed until a consensus was reached.
Data Collection Process
The first author developed a coding manual to extract study-level data as potential moderators, as described below. Coding was completed separately by the first and second authors. Interrater agreement was assessed for study inclusion and the coding of other study data. Inter-rater reliabilities were in the good to excellent range (i.e., kappas and ICCs > .60; Cicchetti, 1994). Discrepancy were resolved through discussion until agreement was reached.
Data Items
Data necessary for computing standardized effect sizes were extracted (i.e., means, standard deviations, etc.). In addition, the following data items were coded:
Control type.
Consistent with prior meta-analyses of MBIs (Goldberg et al., 2018; Khoury et al., 2013) and psychological interventions generally (Wampold et al., 1997), control conditions were coded based whether or not they were intended to be therapeutic (i.e., promote positive psychological or behavioral health change; Wampold et al., 1997). Active control conditions involved engagement of participants in interventions intended to create or facilitate change (i.e., evidence-based treatment, Leonard et al., 2013; skills training, Lyons, Womack, Cantrell, & Kenemore, 2018; social support group, Palta et al., 2012; health education, Sibinga et al., 2013). Inactive controls did not involve treatment that was intended to be therapeutic (e.g., waitlist, Fung et al., 2019; treatment-as-usual [TAU] conditions in which both the MBI and non-MBI arm received ongoing TAU, Zhang & Emory, 2015).
Population characteristics.
Study population characteristics coded included race/ethnicity, mean age, gender (percent female), and income. Income was coded as low-income, not low-income, or not reported based on each study’s description of the sample or population from which the sample was recruited (e.g., 86.1% sample had annual income < $15,000, Alegría et al., 2019).
Mindfulness intervention characteristics.
We coded MBI duration and dosage along with whether or not the MBI was adapted. Given the meta-analytic sample engaged POC largely from lower socioeconomic backgrounds and that many participants had other disadvantaged social positions (e.g., incarcerated) and health conditions (e.g., HIV+, hypertensive), intervention adaptation was rated separately on the following two criteria (1 = Yes, 0 = No): (1) was any adaptation conducted for the population, (2) was any cultural adaptation conducted for POC, which was defined as systematic modifications of the treatment “to consider language, culture, and context in such a way that is compatible with the client’s cultural patterns, meanings, and values” (Bernal, Jiménez-Chafey, & Domenech Rodríguez, 2009, p. 362), such as using cultural metaphors, incorporating cultural-specific elements in intervention.
Study setting.
Study setting was a potential moderator of interest that may reflect differential efficacy across subpopulations (Zoogman, Goldberg, Hoyt, & Miller, 2015). We first qualitatively coded the description of study setting (e.g., “an alternative high school for high-risk adolescents”). Then, we categorized study setting in three types: (1) school, (2) correctional/ residential facilities, and (3) community-based settings.
Outcome type.
To investigate if MBIs are more efficacious for POC on certain outcomes, we coded outcome type (see Supplemental Materials Table 2). Within each study, outcomes were categorized into one of the following types: (1) psychological symptoms (e.g., anxiety, depression, PTSD, perceived stress), (2) psychosomatic health (e.g., self-reported somatic symptoms/health); (3) biomarkers (non-self-reported biological markers, such as cortisol level, blood pressure, CD4+), (4) cognitive outcomes (e.g., ADHD symptoms, cognitive task performance), (5) mindfulness (including self-reported mindfulness and self-compassion), (6) coping skills, and (7) well-being (e.g., quality of life, subjective well-being).
Risk of Bias in Individual Studies
The methodological quality of each study was independently assessed by the first two authors using a modified Jadad’s criteria (Jadad et al., 1996) that has been used in previous MBI research (Piet & Hougaard, 2011). The following criteria were applied (1 = Present; 0 = Absent; range = [0, 5]): (1) participants were randomized through an adequate randomization procedure, (2) outcome assessment was blinded (e.g., assessed by blinded clinician or non-self-report measure), (3) study groups were similar with regard to baseline demographic and psychosocial characteristics or adjustments were made to correct for baseline imbalance, (4) the description of drop-outs was provided, and (5) intent-to-treat analysis was used.
Synthesis of Results
Effect size calculation.
Our primary effect size measure was the standardized mean difference (Hedges’ g). Hedges’ g is a variation of Cohen’s d that is corrected for small sample bias (Hedges & Olkin, 1985). Analyses were conducted using R statistical software and the ‘metafor’ and ‘MAd’ packages (Del Re & Hoyt, 2010; R Core Team, 2016; Viechtbauer, 2010). Random effects models were computed, with effects weighted based on the inverse of their variance. Consistent with prior meta-analyses of psychological interventions (Wampold et al., 1997) and MBIs (Galante et al., 2021; Goldberg et al., 2021, 2018), efficacy analyses were conducted separately for MBIs in comparison to active controls and inactive controls since they represent differed meanings (i.e., the efficacy of MBIs relative to another intervention intended to be therapeutic vs. passage of time).
Effect sizes were calculated based on pre- and post-intervention means and standard deviations (SD), when available. Other reported statistics (e.g., t- or F-statistics, p-values, odds ratios) were used as needed in accordance with standard meta-analytic methods (Cooper, Hedges, & Valentine, 2009). Hedges’ g was calculated first for each measured outcome within every study in following steps (Hedges & Olkin, 1985). First, Cohen’s dwithin was calculated within intervention and control groups separately, from pre- to post-intervention (or pre- to follow-up), when pre-intervention data was available (and post-intervention data was used when pre-intervention outcomes were not reported). Second, the between-group difference was calculated using to calculate Cohen’s dbetween. Third, Hedges’ g was calculated by multiplying Cohen’s dbetween by a correction (Hedges & Olkin, 1985).
Variance was calculated using Becker’s (1988) statistical technique. Prior to aggregation across studies, data were first aggregated within studies. In cases where separate subscales reflected a larger, more global construct (e.g., nine subscales of the Symptoms Checklist-90; Derogatis & Unger, 2010), subscales were first aggregated within a given measure using the ‘agg’ function in the ‘MAd’ package (Del Re & Hoyt, 2010), followed by aggregation across measures within studies (for analyses involving the overall effect). Then, between-study effect sizes were aggregated, using restricted maximum likelihood random effects analyses (Cooper et al., 2009). Summary statistics were computed in Hedges’ g units along with corresponding 95% confidence intervals. Hedges’ g can be interpreted according to Cohen’s (1988) conventions as small (0.20), medium (0.50), and large (0.80). Following omnibus test, false discovery rate (FDR) correction was made using the Benjamini-Hochberg procedure. Heterogeneity was assessed using the I2 (the ratio of true heterogeneity to observed variation) and Q-statistic (evaluating whether between-study heterogeneity exceeded that expected by chance) (Higgins, Thompson, Deeks, & Altman, 2003).
Attrition.
We computed odds ratio of dropout from MBIs relative to control to estimate differential attrition (Cooper et al., 2009). Differential attrition was only calculated for studies that (a) utilized an active control to compare MBI to another condition that also intended to be therapeutic and (b) in a setting where participants can freely withdrawal (i.e., outpatient).
Exploratory moderator analyses.
Following the methodological criteria and recommendations for assessment of moderators in systematic reviews of randomized controlled trials (RCTs) (Pincus et al., 2011), moderator analyses are necessary to inform future clinical trials. As there is limited prior meta-analytic research and theory regarding the use of MBIs for POC, moderator analyses were exploratory rather than based on a priori hypothesis. We followed Fu et al.’s (2011) recommendation to require k ≥ 4 studies within each subcategory for categorical moderator tests (e.g., study setting). Thus, some moderator tests were not conducted due to the limited number of studies. Analyses were conducted within each control type (i.e., active, inactive) and completed using the ‘rma’ function in the ‘metafor’ package (Viechtbauer, 2010). We tested both categorial (e.g., study setting) and continuous (e.g., mean age) moderators. For key subcategories of interest (i.e., study setting, outcome type), sub-analyses were also conducted for descriptive purposes when k ≥ 2 studies were available.
Risk of Bias across Studies
We assessed publication bias by visually inspecting funnel plots for asymmetry disaggregated by control condition (i.e., active, inactive). Models were also re-estimated using trim-and-fill methods that account for the asymmetric distribution of studies around an omnibus effect (Duval & Tweedie, 2000). In addition, we also examined study quality (i.e., modified Jadad scores) as a moderator of treatment effects within each control type.
Results
Study Selection
The search produced 550 citations. After removing duplicates, titles and abstracts were reviewed, resulting in a total of 84 for full text review. After applying the exclusion criteria, we retained 26 studies. Among them, four studies did not report sufficient data for estimating effect sizes, even after contacting authors of the original studies. Therefore, a total of 22 studies were included in the meta-analysis, and among them, two studies compared an MBI to both an active and an inactive control, yielding 24 comparisons. Thus, the final sample included 16 studies that compared an MBI to an active control and 8 studies that compared an MBI to an inactive control. Among them, all reported post-treatment assessments with two also reporting follow-up data. The PRISMA flow diagram is shown in Supplemental Material Figure 1.
Study Characteristics
Study characteristics are reported for each study in Supplemental Material Table 3. The sample had a total of 2,156 participants and was 94.4% POC (range = [77.5%, 100%]). Average sample size was 98 (SD = 96.9, range = [19, 341]) participants per study. The sample was on average 23.2 years old (range = [7.9, 72.9]), with approximately half being male (50.8%, range = [0%, 100%]). The majority of studies focused on African Americans (k = 14, 63.6%), three studies included a combination of Asian American and Latinx/Hispanic participants (13.6%), two studies focused primarily on Latinx/Hispanic participants (9.1%), two studies included participants with a mix of racial/ethnic minority backgrounds (9.1%), and one had a mix of Latinx and African American participants (4.5%). Among the 17 studies that reported participants’ income level, 14 studies (82.4%) indicated the sample was predominately low-income (see Supplemental Material Table 3). Most study samples (k = 14, 63.6%) had a clinical diagnosis (medical and/or psychiatric), elevated symptoms, or legal status that distinguish them from the general population (e.g., incarcerated with substance use disorder). The average duration of MBIs in all studies was 9 weeks (range = [4, 12] weeks). The majority of the interventions (k = 14; 63.6%) were derived from Mindfulness-based Stress Reduction (MBSR) (k = 12; 54.5%) or Mindfulness-based Cognitive Therapy (MBCT) (k = 2; 9.1%). Most common outcome was psychological in included trials (reported in 17 out of 22 RCTs, 77.3%).
Risk of Bias within Studies
All included studies used randomized designs. Two studies included both an active and inactive control arm (i.e., three-armed design). A total of 16 studies (72.7%) included an active control and 8 studies (36.4%) included an inactive control. A total of 13 studies (59.1%) used at least one blinded outcome assessment (i.e., non-self-report measure). The majority of studies (k = 15; 68.2%) compared MBIs and control groups at baseline and made adjustments if a significant difference was detected. A total of 19 studies (86.4%) reported drop-out rates. Half of the studies (k = 11, 50.0%) used intent-to-treat analysis. The average Jadad quality score among studies was 3.68 (SD = 0.99, range = [2, 5]; Supplemental Materials Table 4). More than half of studies (k = 13; 59.1%) received a ≥4 or higher quality score (maximum score = 5).
Results of Individual Studies
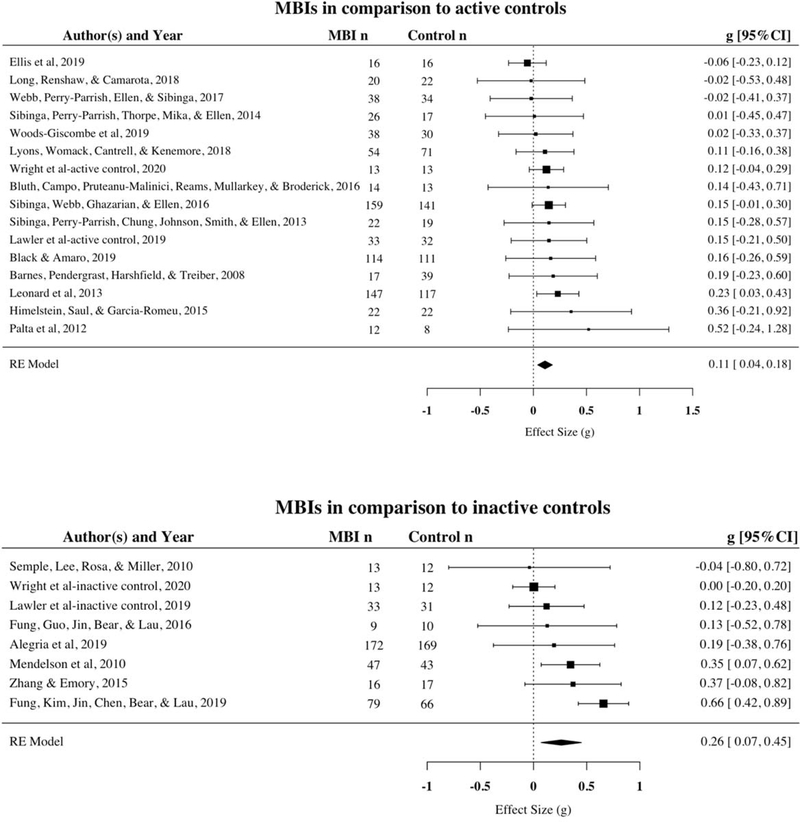
Effect sizes reflecting the impact of MBIs for each included study are shown in Figure 1 and Supplemental Materials Table 5.
Figure 1.
Forest plot of MBIs for POC by control type
Synthesis of Results
Efficacy.
When aggregated across all outcomes, MBIs were shown to be overall modestly superior to active control conditions (k = 16, g = 0.11, 95%CI = [0.04, 0.18], p = .002) as well as inactive control conditions (k = 8, g = 0.26, 95%CI = [0.07, 0.45], p = .007). Results remained significant after FDR correction (p values adjusted as .004 and .007, correspondingly). Heterogeneity was low for studies using active controls (I2 = 0.00%, 95%CI = [0.00%, 17.94%]) and moderate for studies using inactive controls (I2 = 54.03%, 95%CI = [8.55%, 85.50%]).
Attrition.
Differential attrition were calculated in studies that included an active control that received an intervention and where individuals could freely withdraw (i.e., outpatient, k = 8). Rates of attrition varied considerably, range = [0, 71.4%] in MBIs (weighted M = 22.0%) and range = [0, 78.6%] in controls (weighted M = 19.7%). Rates of attrition between MBI and control group were highly correlated, r = .98. Participants randomized to MBIs were no more likely to drop out than the control group (OR = 0.97, 95%CI = [0.57, 1.64], p = .91). Heterogeneity was low across studies (Q [6] = 2.38, I2 = 0.00%, 95%CI = [0.00%, 33.23%]).
Risk of Bias across Studies
Asymmetric funnel plots suggested evidence for publication bias for MBIs versus active and inactive controls (see Supplemental Materials Figures 2 & 3), with one study missing from the left side of the omnibus effect for active control comparisons and studies missing from the right side of the omnibus effect for inactive control comparisons. Based on a trim-and-fill analysis, MBIs continued to show significantly superiority to active controls with the addition of one imputed study and the omnibus effect size adjusted, g = 0.11, 95%CI = [0.04, 0.18], p = .003, as well as to inactive controls with the addition of four imputed studies and adjusted omnibus effect size, g = 0.45, 95%CI = [0.24, 0.65], p < .001.
Exploratory Moderator Analyses
Moderator analyses were conducted separately for active and inactive comparisons.
Sample characteristics.
Sample characteristics tested as potential moderators of treatment effects included mean age and age group (i.e., youth vs. adult), percentage female, income level, proportion of POC, and proportion of each racial minority group (African American, Asian American, Latinx/Hispanic, and Multiracial). Among studies that used active controls, none of these characteristics emerged as significant moderators (see Supplemental Materials Table 6). Among studies that used inactive controls, two significant moderators were found: comparisons using a clinical population showed significantly smaller effects for MBIs than those targeted a general population (B = −0.45, 95%CI = [−0.70, −0.20], Q[1] = 12.47, p < .001), and studies with higher proportion of POC had larger effect sizes in favor of MBIs (B = 0.06, 95%CI = [0.02, 0.09], Q[1] = 11.20, p < .001; see Supplemental Materials Table 6).
Intervention characteristics.
Intervention duration, dosage (number of weeks, number of minutes per week, total time engaged in treatment), adaptation, and study quality were not significant moderators of treatment effects (see Supplemental Materials Table 7). While most studies used an intervention adapted for their target population (k = 17 in active control, 94.4% and k = 5 in inactive control, 83.3%), these adaptations involved non-cultural elements (e.g., Lyons, Womack, Cantrell, & Kenemore, 2018). Only two studies employed cultural adaptation (k = 1 in active control, Black & Amaro, 2019 and k = 1 in inactive control, Alegría et al., 2019).
Study setting.
Only studies using active controls had a sufficient number (i.e., k ≥ 4; Fu et al., 2011) to allow formal moderator testing. Effects did not differ significantly across settings (k = 16, Q[2] = 2.85, p = .240; see Supplemental Material Table 8). Effect size aggregation was performed for each setting for descriptive purpose. In comparison to active controls, MBIs yielded better outcomes in school (k = 5, g = 0.14, 95%CI = [0.01, 0.27], p = .038) and correctional/residential settings (k = 4, g = 0.20, 95%CI = [0.05, 0.34], p = .008), but did not differ from controls in community-based settings (k = 7, g = 0.05, 95%CI = [−0.05, 0.16], p = .333). In comparison to inactive controls, MBIs were superior in school settings (k =3, g = 0.46, 95%CI = [0.18, 0.73], p = .001) but not in community-based settings (k = 5, g = 0.08, 95%CI = [−0.07, 0.23], p = .310). No study in correctional/residential settings used an inactive control. Supplemental Material Figure 4 presents forest plot separated by study settings.
Outcome type.
For moderator analysis, sufficient studies were available for four outcome types in studies with active controls (ks = 12, 8, 6, 6, 6, and 4, for psychological, mindfulness, biomarkers, coping, behavioral, and well-being outcome types, respectively). Outcome type was not a significant moderator (Q[4] = 7.36, p = .118). However, inspection of the subgroup omnibus analyses for the various outcome types suggested well-being outcomes may differ from other types. A post hoc test evaluating this possibility with outcomes coded as well-being or non-well-being indicated that effects were indeed statistically small when well-being outcomes were assessed in studies using active controls (Q[1] = 4.06, I2 = 40.56%, 95%CI = [3.45%, 64.38%], p = .044). MBIs yielded significantly smaller effects in well-being than other outcomes when compared to active controls (B = −0.33, 95%CI = [- .65, - .01]; Supplemental Materials Table 8). Among studies that used inactive controls, only psychological outcomes met the threshold (k ≥ 4). Thus, moderator analysis was not conducted in this subsample.
Effects of MBIs were examined within seven outcome domains and separately for active and inactive comparisons for descriptive purposes when k ≥2 (also see Supplemental Material Figure 5). Among studies that utilized an active control, MBIs were superior in reducing psychological symptoms (g = 0.13, 95%CI = [0.02, 0.24]) and improving psychosomatic health (g = 0.26, 95%CI = [0.06, 0.46]). MBIs did not differ from other active controls in the following domains: biomarkers (g = 0.07, 95%CI = [−0.20, 0.34]), cognitive outcomes (g = 0.45, 95%CI = [−0.12, 1.01]), mindfulness (g = 0.12, 95%CI = [−0.09, .33]), coping skills (g = 0.15, 95%CI = [−0.07, 0.37]), well-being (g = −0.23, 95%CI = [−0.51, 0.04]), and behavioral outcomes (g = −0.08, 95%CI = [−0.21, 0.04]). Among studies that included an inactive control, MBIs were superior on improving cognitive outcomes (g = 0.25, 95%CI = [0.02, 0.48]), mindfulness (g = 0.63, 95%CI = [0.04, 1.21]), and coping (g = 0.52, 95%CI = [0.10, 0.93]), but MBIs did not differ from inactive controls in psychological (g = 0.16, 95%CI = [−0.28, 0.60]), biomarkers (g = 0.05, 95%CI = [−0.32, 0.43]), and behavioral outcomes (g = 0.11, 95%CI = [−0.13, 0.36]).
Discussion
This is the first meta-analysis to examine the effects of MBIs specifically for POC. In an overall sample of 2,156 participants (94.4% POC) drawn from 22 RCTs with 24 comparisons, results provide an empirical synthesis on the utility of MBIs in this population. Based on Cohen’s (1988) guidelines, an effect size below small (g = 0.11) was detected in comparison to active controls and a small effect size (g = 0.26) was detected in comparison to inactive controls. Effects remained significant after accounting for publication bias in trim-and-fill analyses.
Although these effects mirror the statistical significance seen in previous large-scale meta-analyses of MBI RCTs, the current effect size are smaller in magnitude compared to findings in other populations. In psychiatric and medical populations, meta-analyses reported the relative efficacy of MBIs to be gs = 0.23 (Goldberg et al., 2018) and 0.33 (Khoury et al., 2013) compared to active controls and gs = 0.53 (Khoury et al., 2013) and 0.55 (Goldberg et al., 2018) compared to inactive controls. In healthy adults, Khoury et al. (2015) found g = 0.53 comparing to largely inactive controls (waitlist). Among youth, Dunning et al. (2019) reported ds = 0.26 and 0.38 for comparisons with active and inactive controls, respectively. At present, the reason for smaller effects in the current meta-analysis is unclear. Outside of MBIs, a meta-analytic review of Cognitive Behavioral Therapy (CBT) for substance use found that its longitudinal effect was stronger in non-Hispanic White than Black and Hispanic samples, suggesting potential racial disparity in treatment (Windsor, Jemal, & Alessi, 2015). It is possible that structural challenges (e.g., socioeconomic status, neighborhood violence) that disproportionately affect POC may pose additional barriers for MBIs to achieving higher efficacy. The overall smaller effects of MBIs among POC compared to other populations suggests the need for improvement.
Dropout rate is an important metric of intervention acceptability, and it’s been consistently documented that POC are more likely to prematurely terminate treatment (Cooper & Conklin, 2015; McClendon et al., 2020). Our synthesis on attrition suggests that MBIs did not differ from other active controls in acceptability in outpatient settings. This may be good news – MBIs did not perform worse – but also indicates room for improvement (i.e., MBIs could be adapted to increase acceptability relative to other interventions). Given that all samples were predominately POC, it is intriguing that only two employed cultural adaptation (Alegría et al., 2019; Black & Amaro, 2019). This is particularly surprising given robust meta-analytic evidence suggesting that cultural adaptation improves treatment engagement and outcomes (Hall, Ibaraki, Huang, Marti, & Stice, 2016). Given that the majority of included studies involved some adaptation, it is possible that the lack of cultural adaptation was due to study samples having other demographic and clinical features that might have been more in the forefront of adaptation consideration. Another possibility is that the lack of cultural adaptation reflects limited recognition among treatment developers and clinical trialists about the potential benefits of these modifications. Indeed, culturally-adapted MBIs may represent an important future opportunity for MBI research to fully achieve the potential of MBIs in minority health promotion.
Moderator analyses were exploratory in nature and likely underpowered (Hedges & Pigott, 2004). Thus, findings should be interpreted with caution and as potential indications for clinically meaningful directions. Compared to inactive controls, MBIs were also more effective for studies with higher rather than lower proportions of POC, although this effect did not appear for comparisons with active controls. Potentially, a more homogenous POC group may promote comfort, trust and group cohesion (Kivlighan, Drinane, Tao, Owen, & Liu, 2019), leading to higher efficacy. Contrary to previous reports of meta-analyses noting that MBIs often have a larger effect size for clinical rather than non-clinical populations (Galante et al., 2021; Zoogman et al., 2015), MBIs for POC were more effective in non-clinical compared to clinical samples (e.g., psychiatric, medical) among RCTs utilizing inactive controls (although, again, this did not appear for active controls). Given the meta-analytic sample largely encompassed POC often with other sociodemographic advertises (e.g., low-income, trauma history), relatively brief MBIs alone may not be sufficient and more intensive interventions may be necessary to support change for POC with clinical conditions. It is also intriguing that among studies employing active controls, MBIs had smaller effects on well-being compared to other domains of intervention outcomes. This is consistent with a previous meta-analysis on the effects of mindfulness meditation programs which showed stronger evidence in support of reduced distress (i.e., anxiety and depression) than increased well-being (i.e., quality of life Goyal et al., 2014). It is also possible that as there are various vulnerability factors at multiple levels that disproportionately affect the health of POC (e.g., housing, unemployment, neighborhood violence) (Nazroo, 2003; Smedley, 2012), MBI as an individual-level intervention may have limited effects in achieving optimal well-being.
Limitations
Study findings should be interpreted in the context of several limitations. First, included study samples were predominately from low-income backgrounds and many study participants had other intersecting adversities (e.g., incarceration, exposure to neighborhood violence). Such sample characteristics perhaps reflects the multiple systemic issues that disproportionately affect POC, yet also limits the generalizability of findings to POC without these adversities. This confounding between POC status and intersecting adversities in the included studies makes it challenging to disentangle effects on either characteristic alone. A second and related limitation is the heterogeneity of sample characteristics other than race/ethnicity such as mean age, setting, and clinical features. Given the early stage of MBI research for POC and limited numbers of studies for subgroups of POC, we caution the claim that MBIs are equally effective across POC subgroups (despite these features failing to predict variation in effect sizes in the current study). In a related vein, given the included sample was relatively young (M = 18.6), study findings may not be generalizable to older POC. Third, although the majority of studies used active controls (k = 16), most used non-evidence-based treatments (e.g., health education, support group). Hence, though MBIs were found to be superior to active controls, the effects of MBIs in comparison to other evidence-based treatments for POC is still unknown. Fourth, only two of the studies included follow-up assessment, precluding estimation of long-term effects. Fifth, exploratory moderator tests may have produced false positives (Type I error). These tests were also likely underpowered, as is commonly the case (Hedges & Pigott, 2004). Other errors such as confounding between moderators and ecological fallacy may also have affected results (e.g., individuals and groups with one characteristic may tend to share other characteristics).
Implications for Future Research and Clinical Practice
Based on meta-analytic findings, we provide the following recommendations for future MBI research with POC. First, more trials, particularly rigorous, large-scale RCTs with robust control conditions are needed. As the majority of studies in the current meta-analysis focused on African American and/or Latinx/Hispanic participants, more research on Native Americans and Asian Americans are warranted. It would be valuable to include follow-up assessment to index the degree to which benefits persist. It would also be helpful to consistently report assessments of intervention quality (e.g., treatment integrity). These features are rarely reported (Goldberg et al., 2017), but in theory may impact MBI outcomes, particularly when delivered in less resourced settings. Another method for evaluating efficacy among racial/ethnic minority participants would be examining the proportion of samples that are racial/ethnic minority participants as a moderator of effects within the full MBI literature.
Second, cultural adaptations of MBIs may be beneficial to address the needs of POC. Qualitative, formative research is well-suited to guide intervention development and targeted sample recruitment through a community-centered approach (Hwang, 2009). Adaptations may consider the clinical characteristics of the target population (e.g., depressive symptomology, hypertension) as well as the lived experiences of POC (e.g., structural racism, economic difficulty) that may contribute to these health outcomes. It may be also valuable for treatment developers to determine what target populations may traditionally believe causes relevant symptoms or difficulties and what ways of healthy coping already exist within their communities. Adaptation may therefore seek to find a balance between fidelity to the essence of MBIs (Crane et al., 2017) and the unique cultural needs and preferences of a specific POC population. Future RCTs (and eventually meta-analyses) could evaluate whether culturally-adapted MBIs yield superior outcomes in comparison to non-culturally adapted MBIs for POC in terms of recruitment, engagement, retention, and efficacy (Biggers et al., 2020).
In a related vein, MBI researchers may consider including culturally-relevant and culturally-validated outcome measures that attend to the experience of POC. Candidate constructs may include acculturation/enculturation, mistrust, racial/ethnic identity, racial trauma, experiences of discrimination and other forms of minority stress (Hall, 2001; Pascoe & Richman, 2009; Sun et al., 2016; Whaley, 2001). As evidence-based MBIs (e.g., MBSR) undergo adaptation to meet the needs of POC, recording and reporting of treatment fidelity will also be informative for continued assessment of the intervention’s adherence to and preservation of the principles of mindfulness-based interventions (Crane et al., 2017) as well as the role of treatment fidelity in culturally adapted MBIs (Chu & Leino, 2017).
Third, it may be important to address structural components in future interventions. It is possible that for certain minority groups (e.g., those with unstable housing, community violence exposure), MBIs might be most effective as part of a multi-level intervention that addresses factors affecting the well-being of POC on individual, interpersonal, and community levels. In addition, considering that many POC subgroups experience multiple adversities, future research may want to examine if extended interventions (e.g., beyond the typical 8-week length) may be ideal to facilitate health promotion.
Findings of this systematic review also provide several implications for clinical practice of mindfulness with POC. First, as indicated by sample characteristics, it may be beneficial for mindfulness practitioners working with POC to attend to various intersecting identities and social positions (e.g., socioeconomic status, history of incarceration, neighborhood factors) as well as larger systemic and sociohistorical factors that may have affect their clients’ psychological health and coping. Second, given the high prevalence of trauma exposure among POC (Alegria et al., 2013), a trauma-sensitive approach to teaching mindfulness (Treleaven, 2018) may also be beneficial. Finally, it is worth considering if and when MBIs may be a preferred approach. Given the modest effect sizes observed here, coupled with the possibility that effects in the MBI literature are inflated (e.g., due to researcher allegiance; Goldberg & Tucker, 2020), it is important to consider MBIs as one of many evidence-based approaches that may help remediate the adverse impacts of structural inequalities and promote population health among POC.
Supplementary Material
Clinical or methodological significance of this article:
This is the first meta-analysis that examines the efficacy of mindfulness-based interventions (MBIs) for POC, a population affected by various mental and physical health disparities. MBIs had significant, yet small effects compared to inactive controls and active controls. Results provide modest, preliminary support for the potential utility of MBIs for health promotion among POC.
Acknowledgement:
This research was supported by the National Center for Complementary and Integrative Health Grant K23AT011173 (Shufang Sun) and Grant K23AT010879 (Simon B. Goldberg). Funders had no role in study design, data collection, analysis, manuscript writing, and decision on publication.
Footnotes
Conflict of Interest: Authors declare no conflict of interest.
POC is an umbrella term to represent people in the U.S. with historical or ancestral heritage in African, Asian, Latinx, American Indian/Alaska Native, and Polynesian American communities. Consistent with the Race and Ethnicity Guidelines in Psychology (APA, 2019), we opted to use the term “POC” instead of “racial and ethnic minorities,” given the changing demographics in some regions of the U.S.
References
References marked with an asterisk indicate studies included in the meta-analysis.
- Abbott RA, Whear R, Rodgers LR, Bethel A, Thompson Coon J, Kuyken W, … Dickens C (2014). Effectiveness of mindfulness-based stress reduction and mindfulness based cognitive therapy in vascular disease: A systematic review and meta-analysis of randomised controlled trials. Journal of Psychosomatic Research, 76(5), 341–351. doi: 10.1016/j.jpsychores.2014.02.012 [DOI] [PubMed] [Google Scholar]
- Alegría M, Alvarez K, Ishikawa RZ, DiMarzio K, & McPeck S (2016). Removing obstacles to eliminating racial and ethnic disparities in behavioral health care. Health Affairs, 35(6), 991–999. doi: 10.1377/hlthaff.2016.0029 *
- Alegría M, Falgas-Bague I, Collazos F, Carmona Camacho R, Lapatin Markle S, Wang Y, … Shrout PE (2019). Evaluation of the Integrated Intervention for Dual Problems and Early Action Among Latino Immigrants With Co-occurring Mental Health and Substance Misuse Symptoms: A Randomized Clinical Trial. JAMA Network Open, 2(1), e186927. doi: 10.1001/jamanetworkopen.2018.6927 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alegria M, Fortuna LR, Lin JY, Norris LF, Gao S, Takeuchi DT, … Valentine A (2013). Prevalence, risk, and correlates of posttraumatic stress disorder across ethnic and racial minority groups in the U.S. Medical Care, 51(12), 1114–1123. doi: 10.1097/MLR.0000000000000007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychological Association. (2006). Evidence-based practice in psychology. The American Psychologist, 61(4), 271–85. doi: 10.1037/0003-066X.61.4.271 [DOI] [PubMed] [Google Scholar]
- Asnaani A, & Hall-Clark B (2017). Recent developments in understanding ethnocultural and race differences in trauma exposure and PTSD. Current Opinion in Psychology, 14, 96–101. doi: 10.1016/j.copsyc.2016.12.005 [DOI] [PubMed] [Google Scholar]
- Atdjian S, & Vega WA (2005). Disparities in mental health treatment in U.S. racial and ethnic minority groups: Implications for psychiatrists. Psychiatric Services, 56(12), 1600–1602. doi: 10.1176/appi.ps.56.12.1600 [DOI] [PubMed] [Google Scholar]
- Bailey, Mokonogho J, & Kumar A (2019). Racial and ethnic differences in depression: Current perspectives. Neuropsychiatric Disease and Treatment, 15, 603–609. doi: 10.2147/NDT.S128584 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bailey ZD, Krieger N, Agénor M, Graves J, Linos N, & Bassett MT (2017). Structural racism and health inequalities in the USA: Evidence and interventions. The Lancet, 389(10077), 1453–1463. doi: 10.1016/S0140-6736(17)30569-X [DOI] [PubMed] [Google Scholar]
- Balfour PC, Rodriguez CJ, & Ferdinand KC (2015). The role of hypertension in race-ethnic disparities in cardiovascular disease. Current Cardiovascular Risk Reports, 9(4). doi: 10.1007/s12170-015-0446-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnes VA, Pendergrast RA, Harshfield GA, & Treiber FA (2008). Impact of breathing awareness meditation on ambulatory blood pressure and sodium handling in prehypertensive African American adolescents. Ethnicity and Disease, 18(1), 1–5. *
- Becker BJ (1988). Synthesizing standardized mean-change measures. British Journal of Mathematical and Statistical Psychology, 41, 257–278. [Google Scholar]
- Bernal G, Jiménez-Chafey MI, & Domenech Rodríguez MM (2009). Cultural adaptation of treatments: A resource for considering culture in evidence-based practice. Professional Psychology: Research and Practice, 40(4), 361–368. doi: 10.1037/a0016401 [DOI] [Google Scholar]
- Biggers A, Spears CA, Sanders K, Ong J, Sharp LK, & Gerber BS (2020). Promoting Mindfulness in African American Communities. Mindfulness. doi: 10.1007/s12671-020-01480-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- Black DS, & Amaro H (2019). Moment-by-Moment in Women’s Recovery (MMWR): Mindfulness-based intervention effects on residential substance use disorder treatment retention in a randomized controlled trial. Behaviour Research and Therapy, 120, 103437. doi: 10.1016/j.brat.2019.103437 *
- Bluth K, Campo RA, Pruteanu-Malinici S, Reams A, Mullarkey M, & Broderick PC (2016). A school-based mindfulness pilot study for ethnically diverse at-risk adolescents. Mindfulness, 7(1), 90–104. doi: 10.1007/s12671-014-0376-1. *
- Centola D, Becker J, Brackbill D, & Baronchelli A (2018). Experimental evidence for tipping points in social convention. Science, 1119(June), 1116–1119. [DOI] [PubMed] [Google Scholar]
- Chu J, & Leino A (2017). Advancement in the maturing science of cultural adaptations of evidence-based interventions. Journal of Consulting and Clinical Psychology, 85(1), 45–57. doi: 10.1037/ccp0000145 [DOI] [PubMed] [Google Scholar]
- Cicchetti DV (1994). Guidelines, criteria, and rules of thumb for evaluating normed and standardized assessment instruments in psychology. Psychological Assessment, 6(4), 284–290. doi: 10.1037/1040-3590.6.4.284 [DOI] [Google Scholar]
- Cohen J (1988). Statistical power analysis for the behavioral sciences (2nd ed.). Hillsdale, NJ: Lawrence Erlbaum Associates Publishers. [Google Scholar]
- Cooper, & Conklin LR (2015). Dropout from individual psychotherapy for major depression: A meta-analysis of randomized clinical trials. Clinical Psychology Review, 40, 57–65. doi: 10.1016/j.cpr.2015.05.001 [DOI] [PubMed] [Google Scholar]
- Cooper HM, Hedges LV, & Valentine JC (2009). The handbook of research synthesis and mean-analysis (2nd ed.). New York: Russell Sage Foundation. [Google Scholar]
- Crane RS, Brewer J, Feldman C, Kabat-Zinn J, Santorelli S, Williams JMG, & Kuyken W (2017). What defines mindfulness-based programs? the warp and the weft. Psychological Medicine, 47(6), 990–999. doi: 10.1017/S0033291716003317 [DOI] [PubMed] [Google Scholar]
- Del Re AC, & Hoyt WT (2010). MAd: Meta-analysis with mean differences (R package).
- DeLuca SM, Kelman AR, & Waelde LC (2018). A systematic review of ethnoracial representation and cultural adaptation of mindfulness- and meditation-based interventions. Psychological Studies, 63(2), 117–129. doi: 10.1007/s12646-018-0452-z [DOI] [Google Scholar]
- Derogatis LR, & Unger R (2010). Symptom Checklist-90-Revised. In The Corsini Encyclopedia of Psychology. [Google Scholar]
- Dunning DL, Griffiths K, Kuyken W, Crane C, Foulkes L, Parker J, & Dalgleish T (2019). Research review: The effects of mindfulness-based interventions on cognition and mental health in children and adolescents – a meta-analysis of randomized controlled trials. Journal of Child Psychology and Psychiatry, 60(3), 244–258. doi: 10.1111/jcpp.12980 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duval S, & Tweedie R (2000). Trim and fill: A simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics, 56(2), 455–463. [DOI] [PubMed] [Google Scholar]
- Ellis DA, Carcone AI, Slatcher R, Naar-King S, Hains A, Graham A, & Sibinga E (2019). Efficacy of mindfulness-based stress reduction in emerging adults with poorly controlled, type 1 diabetes: A pilot randomized controlled trial. Pediatric Diabetes, 20(2), 226–234. doi: 10.1111/pedi.12807 *
- Fu R, Gartlehner G, Grant M, Shamliyan T, Sedrakyan A, Wilt TJ, … Trikalinos TA (2011). Conducting quantitative synthesis when comparing medical interventions: AHRQ and the Effective Health Care Program. Journal of Clinical Epidemiology, 64(11), 1187–1197. doi: 10.1016/j.jclinepi.2010.08.010 [DOI] [PubMed] [Google Scholar]
- Fung J, Guo S, Jin J, Bear L, & Lau A (2016). A pilot randomized trial evaluating a school-based mindfulness intervention for ethnic minority youth. Mindfulness, 7, 819–828. doi: 10.1007/s12671-016-0519-7 *
- Fung J, Kim JJ, Jin J, Chen G, Bear L, & Lau AS (2019). A randomized trial evaluating school-based mindfulness intervention for ethnic minority youth: Exploring mediators and moderators of intervention effects. Journal of Abnormal Child Psychology, 47, 1–19. doi: 10.1007/s10802-018-0425-7 *
- Galante J, Friedrich C, Dawson AF, Modrego-Alarcón M, Gebbing P, Delgado-Suárez I, … Jones PB (2021). Mindfulness-based programmes for mental health promotion in adults in nonclinical settings: A systematic review and meta-analysis of randomised controlled trials. PLoS Medicine, 18(1), 1–40. doi: 10.1371/journal.pmed.1003481 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldberg SB, Riordan KM, Sun S, & Davidson RJ (2021). The empirical status of mindfulness-based interventions: A systematic review of 44 meta-analyses of randomized controlled trials. Perspectives on Psychological Science. doi: 10.1177/174569162096877 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldberg SB, & Tucker RP (2020). Allegiance effects in mindfulness-based interventions for psychiatric disorders: A meta-re-analysis. Psychotherapy Research, 30(6), 753–762. doi: 10.1080/10503307.2019.1664783 [DOI] [PubMed] [Google Scholar]
- Goldberg SB, Tucker RP, Greene PA, Davidson RJ, Wampold BE, Kearney DJ, & Simpson TL (2018). Mindfulness-based interventions for psychiatric disorders: A systematic review and meta-analysis. Clinical Psychology Review, 59, 52–60. doi: 10.1016/j.cpr.2017.10.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldberg SB, Tucker RP, Greene PA, Simpson TL, Kearney DJ, & Davidson RJ (2017). Is mindfulness research methodology improving over time? A systematic review. PLoS ONE, 12(10), 1–16. doi: 10.1371/journal.pone.0187298 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldberg SB, Zeliadt SB, Hoggatt KJ, Simpson TL, Fortney JC, & Taylor SL (2019). Mindfulness meditation in veterans: Results from a national survey. Mindfulness, 10, 2596–2605. doi: 10.1007/s12671-019-01214-7 [DOI] [Google Scholar]
- Goyal M, Singh S, Sibinga EM, Gould NF, Rowland-Seymour A, Sharma R, … Haythornthwaite JA (2014). Meditation programs for psychological stress and well-being: A systematic review and meta-analysis. JAMA Internal Medicine, 174(3), 357–368. doi: 10.1001/jamainternmed.2013.13018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall GCN (2001). Psychotherapy research with ethnic minorities: Empirical, ethical, and conceptual issues. Journal of Consulting and Clinical Psychology, 69(3), 502–510. doi: 10.1037/0022-006X.69.3.502 [DOI] [PubMed] [Google Scholar]
- Hall GCN, Ibaraki AY, Huang ER, Marti CN, & Stice E (2016). A Meta-Analysis of Cultural Adaptations of Psychological Interventions. Behavior Therapy, 47(6), 993–1014. doi: 10.1016/j.beth.2016.09.005 [DOI] [PubMed] [Google Scholar]
- Hedges LV, & Olkin I (1985). Statistical methods for meta-analysis. San Diego, CA: Academic Press. [Google Scholar]
- Hedges LV, & Pigott TD (2004). The power of statistical tests for moderators in meta-analysis. Psychological Methods, 9(4), 426–445. doi: 10.1037/1082-989X.9.4.426 [DOI] [PubMed] [Google Scholar]
- Higgins JP, Thompson SG, Deeks JJ, & Altman DG (2003). Measuring inconsistency in meta-analysis. BMJ, 327(7414), 557–560. doi: 10.1136/bmj.327.7414.557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Himelstein S, Saul S, & Garcia-Romeu A (2015). Does mindfulness meditation increase effectiveness of substance abuse treatment with incarcerated youth ? A pilot randomized controlled trial. Mindfulness, 6, 1472–1480. doi: 10.1007/s12671-015-0431-6 *
- Hwang W-C (2009). The Formative Method for Adapting Psychotherapy (FMAP): A community-based developmental approach to culturally adapting therapy. Professional Psychology, Research and Practice, 40(4), 369–377. doi: 10.1037/a0016240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJM, Gavaghan DJ, & McQuay HJ (1996). Assessing the quality of randomized controlled trials: Is blinding necessary? Controlled Clinical Trials, 17(January 1995), 1–12. [DOI] [PubMed] [Google Scholar]
- Kabat-Zinn J (1990). Full catastrophe living: Using the wisdom of your body and mind to face stress, pain, and illness. New York, NY: Delta Book. [Google Scholar]
- Kabat-Zinn J (1994). Wherever you go, there you are: Mindfulness meditation in everyday life. New York, NY: Hyperion. [Google Scholar]
- Khoury B, Lecomte T, Fortin G, Masse M, Therien P, Bouchard V, … Hofmann SG (2013). Mindfulness-based therapy: A comprehensive meta-analysis. Clinical Psychology Review, 33(6), 763–771. doi: 10.1016/j.cpr.2013.05.005 [DOI] [PubMed] [Google Scholar]
- Khoury B, Sharma M, Rush SE, & Fournier C (2015). Mindfulness-based stress reduction for healthy individuals: A meta-analysis. Journal of Psychosomatic Research, 78(6), 519–528. doi: 10.1016/j.jpsychores.2015.03.009 [DOI] [PubMed] [Google Scholar]
- Kivlighan DM, Drinane JM, Tao KW, Owen J, & Liu WM (2019). The Detrimental Effect of Fragile Groups: Examining the Role of Cultural Comfort for Group Therapy Members of Color. Journal of Counseling Psychology, 66(6), 763–770. doi: 10.1037/cou0000352 [DOI] [PubMed] [Google Scholar]
- Lawler JM, Esposito EA, Doyle CM, & Gunnar MR (2019). A Preliminary, Randomized-Controlled Trial of Mindfulness and Game-Based Executive Function Trainings to Promote Self-Regulation in Internationally-Adopted Children. Development and Psychopathology, 1–13. doi: 10.1017/s0954579418001190 *
- Lee EKP, Yeung NCY, Xu Z, Zhang D, Yu CP, & Wong SYS (2020). Effect and Acceptability of Mindfulness-Based Stress Reduction Program on Patients with Elevated Blood Pressure or Hypertension: A Meta-Analysis of Randomized Controlled Trials. Hypertension, 1992–2001. doi: 10.1161/HYPERTENSIONAHA.120.16160 [DOI] [PubMed] [Google Scholar]
- Leonard NR, Jha AP, Casarjian B, Goolsarran M, Garcia C, Cleland CM, … Massey Z (2013). Mindfulness training improves attentional task performance in incarcerated youth : a group randomized controlled intervention trial. Frontiers in Psychology, 4, 1–10. doi: 10.3389/fpsyg.2013.00792 *
- Long ACJ, Renshaw TL, & Camarota D (2018). Classroom Management in an Urban, Alternative School: a Comparison of Mindfulness and Behavioral Approaches. Contemporary School Psychology, 22(3), 233–248. doi: 10.1007/s40688-018-0177-y *
- LoParo D, Mack SA, Patterson B, Negi LT, & Kaslow NJ (2018). The efficacy of cognitively-based compassion training for African American suicide attempters. Mindfulness. doi: 10.1007/s12671-018-0940-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lyons T, Womack VY, Cantrell WD, & Kenemore T (2018). Mindfulness-based relapse prevention in a jail drug treatment program. Substance Use and Misuse, 1–8. doi: 10.1080/10826084.2018.1491054 *
- McClendon J, Dean KE, & Galovski T (2020). Addressing Diversity in PTSD Treatment: Disparities in Treatment Engagement and Outcome Among Patients of Color. Current Treatment Options in Psychiatry, 7, 275–290. [Google Scholar]
- Mendelson T, Greenberg MT, Dariotis JK, Gould LF, Rhoades BL, & Leaf PJ (2010). Feasibility and preliminary outcomes of a school-based mindfulness intervention for urban youth. Journal of Abnormal Child Psychology, 38(7), 985–994. doi: 10.1007/s10802-010-9418-x *
- Millett GA, Peterson JL, Flores SA, Hart TA, Jeffries IV WL, Wilson PA, … Remis RS (2012). Comparisons of disparities and risks of HIV infection in black and other men who have sex with men in Canada, UK, and USA: A meta-analysis. The Lancet, 380(9839), 341–348. doi: 10.1016/S0140-6736(12)60899-X [DOI] [PubMed] [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, Altman DG, & the PRISMA Group. (2009). Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Annals of Internal Medicine, 151(4), 264–269. [DOI] [PubMed] [Google Scholar]
- Nazroo JY (2003). The structuring of ethnic inequalities in health: Economic position, racial discrimination, and racism. American Journal of Public Health, 93(2), 277–284. doi: 10.2105/AJPH.93.2.277 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olano HA, Kachan D, Tannenbaum SL, Mehta A, Annane D, & Lee DJ (2015). Engagement in mindfulness practices by U.S. adults: Sociodemographic barriers. Journal of Alternative and Complementary Medicine, 21(2), 100–102. doi: 10.1089/acm.2014.0269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palta P, Page G, Piferi RL, Gill JM, Hayat MJ, Connolly AB, & Szanton SL (2012). Evaluation of a mindfulness-based intervention program to decrease blood pressure in low-income African-American older adults. Journal of Urban Health, 89(2), 308–316. doi: 10.1007/s11524-011-9654-6 *
- Pascoe EA, & Richman LS (2009). Perceived discrimination and health: A meta-analytic review. Psychological Bulletin, 135(4), 531–554. doi: 10.1037/a0016059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piet J, & Hougaard E (2011). The effect of mindfulness-based cognitive therapy for prevention of relapse in recurrent major depressive disorder: A systematic review and meta-analysis. Clinical Psychology Review, 31(6), 1032–1040. doi: 10.1016/j.cpr.2011.05.002 [DOI] [PubMed] [Google Scholar]
- Pincus T, Miles C, Froud R, Underwood M, Carnes D, & Taylor SJ (2011). Methodological criteria for the assessment of moderators in systematic reviews of randomised controlled trials: A consensus study. BMC Medical Research Methodology, 11(1), 14. doi: 10.1186/1471-2288-11-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- R Core Team. (2016). R Development Core Team. R: A Language and Environment for Statistical Computing. Retrieved from https://www.r-project.org/
- Scott-Sheldon LAJ, Balletto BL, Donahue ML, Feulner MM, Cruess DG, Salmoirago-Blotcher E, … Carey MP (2018). Mindfulness-Based Interventions for Adults Living with HIV/AIDS: A Systematic Review and Meta-analysis. AIDS and Behavior, 23(1), 60–75. doi: 10.1007/s10461-018-2236-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Semple RJ, Lee J, Rosa D, & Miller LF (2010). A randomized trial of mindfulness-based cognitive therapy for children: Promoting mindful attention to enhance social-emotional resiliency in children. Journal of Child and Family Studies, 19(2), 218–229. doi: 10.1007/s10826-009-9301-y *
- Sibinga EMS, Perry-parrish C, Chung S, Johnson SB, Smith M, & Ellen JM (2013). School-based mindfulness instruction for urban male youth : A small randomized controlled trial. Preventive Medicine, 57(6), 799–801. doi: 10.1016/j.ypmed.2013.08.027 *
- Sibinga EMS, Perry-Parrish C, Thorpe K, Mika M, & Ellen JM (2014). A small mixed-method RCT of mindfulness instruction for urban youth. Explore: The Journal of Science and Healing, 10(3), 180–186. doi: 10.1016/j.explore.2014.02.006 *
- Sibinga EMS, Webb L, Ghazarian SR, & Ellen JM (2015). School-based mindfulness instruction: An RCT. Pediatrics, 137(1), e20152532. doi: 10.1542/peds.2015-2532 *
- Smedley BD (2012). The lived experience of race and its health consequences. American Journal of Public Health, 102(5), 933–935. doi: 10.2105/AJPH.2011.300643 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun S, Hoyt WT, Brockberg D, Lam J, & Tiwari D (2016). Acculturation and enculturation as predictors of psychological help-seeking attitudes (HSAs) among racial and ethnic minorities: A meta-analytic investigation. Journal of Counseling Psychology, 63(6), 617–632. doi: 10.1037/cou0000172 [DOI] [PubMed] [Google Scholar]
- Teasdale JD, Segal ZV, Williams JM, Ridgeway VA, Soulsby JM, & Lau MA (2000). Prevention of relapse/recurrence in major depression by mindfulness-based cognitive therapy. Journal of Consulting and Clinical Psychology, 68(4), 615–623. doi: 10.1037//0022-006x.68.4.615 [DOI] [PubMed] [Google Scholar]
- Treleaven DA (2018). Trauma-sensitive mindfulness: Practices for safe and transformative healing. WW Norton & Company. [Google Scholar]
- Unites States Census Bureau. (2019). United States Census Quick Facts, 2018. Retrieved from https://www.census.gov/quickfacts/fact/table/US/PST045219
- Viechtbauer W (2010). Conducting meta-analyses in R with the Metafor package. Journal of Statistical Software, 36(3), 1–49. [Google Scholar]
- Waldron EM, Hong S, Moskowitz JT, & Burnett-Zeigler I (2018). A systematic review of the demographic characteristics of participants in US-based randomized controlled trials of mindfulness-based interventions. Mindfulness, 9(6), 1671–1692. doi: 10.1007/s12671-018-0920-5 [DOI] [Google Scholar]
- Wampold BE, Mondin GW, Moody M, Stich F, Benson K, & Ahn HN (1997). A meta-analysis of outcome studies comparing bona fide psychotherapies: Empirically, “all must have prizes.” Psychological Bulletin, 122(3), 203–215. [Google Scholar]
- Webb L, Perry-parrish C, Ellen J, & Sibinga E (2018). Mindfulness instruction for HIV-infected youth: A randomized controlled trial. AIDS Care, 30(6), 688–695. doi: 10.1080/09540121.2017.1394434 *
- Whaley AL (2001). Cultural mistrust: An important psychological construct for diagnosis and treatment of African Americans. Professional Psychology: Research and Practice, 32(6), 555–562. doi: 10.1037/0735-7028.32.6.555 [DOI] [Google Scholar]
- Wildeman C, & Wang EA (2017). Mass incarceration, public health, and widening inequality in the USA. The Lancet, 389(10077), 1464–1474. doi: 10.1016/S0140-6736(17)30259-3 [DOI] [PubMed] [Google Scholar]
- Windsor LC, Jemal A, & Alessi EJ (2015). Cognitive behavioral therapy: A meta-analysis of race and substance use outcomes. Cultural Diversity & Ethnic Minority Psychology, 21(2), 300–313. doi: 10.1037/a0037929 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woods-Giscombé CL, & Gaylord SA (2014). The cultural relevance of mindfulness meditation as a health intervention for African Americans: Implications for reducing stress-related health disparities. Journal of Holistic Nursing, 32, 147–160. doi: 10.1177/0898010113519010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woods-Giscombe CL, Gaylord SA, Li Y, Brintz CE, Bangdiwala SI, Buse JB, … Faurot K (2019). A mixed-methods, randomized clinical trial to examine feasibility of a mindfulness-based stress management and diabetes risk reduction intervention for African Americans with prediabetes. Evidence-Based Complementary and Alternative Medicine, 1–16. doi: 10.1155/2019/3962623 *
- Wright KD, Klatt MD, Adams IR, Nguyen CM, Mion LC, Tan A, … Scharre DW (2020). Mindfulness in Motion and Dietary Approaches to Stop Hypertension (DASH) in Hypertensive African Americans. Journal of the American Geriatrics Society, 1–6. doi: 10.1111/jgs.16947 *
- Zhang H, & Emory EK (2015). A Mindfulness-based intervention for pregnant African-American women. Mindfulness, 6, 663–674. doi: 10.1007/s12671-014-0304-4 *
- Zimmerman FJ, & Anderson NW (2019). Trends in Health Equity in the United States by Race/Ethnicity, Sex, and Income, 1993–2017. JAMA Network Open, 1–10. doi: 10.1001/jamanetworkopen.2019.6386 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zoogman S, Goldberg SB, Hoyt WT, & Miller L (2015). Mindfulness interventions with youth: A meta-analysis. Mindfulness, 6(2), 290–302. doi: 10.1007/s12671-013-0260-4 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.