Abstract
Background:
Model 3 of Medicare’s Bundled Payments for Care Improvement (BPCI) was a voluntary alternative payment model that held participating skilled nursing facilities (SNFs) accountable for 90-day costs of care. Its overall impact on Medicare spending and clinical outcomes is unknown.
Methods:
Retrospective cohort study using Medicare claims from 2012–2017. We used an interrupted time series design to compare participating versus matched control SNFs on total 90-day Medicare payments and payment components (initial SNF stay, readmissions, and outpatient/clinician), case mix (volume, proportion Medicaid, proportion Black, number of comorbidities), and clinical outcomes (90 day readmission, mortality and healthy days at home, and length of initial SNF stay), overall and among key subgroups with frailty or dementia, for 47 of the 48 conditions in the program (excluding major lower extremity joint replacement).
Results:
Our sample included 1,001 participating and 3,873 matched control SNFs. At baseline, total Medicare institutional payments were increasing at BPCI SNFs at a rate of $121 per episode per quarter; during the intervention period, payments decreased at a rate of −$398/episode/quarter. Among controls, payments were stable in the baseline period (+$17/episode/quarter) but decreased at −$424/episode/quarter during the intervention period, yielding a nonsignificant difference in slope changes of −$79/episode/quarter (95% confidence interval [CI] −$188, $31, p=0.16). However, among patients with frailty, spending declined by $620/episode/quarter in the BPCI group, compared with $330/episode/quarter in the non-BPCI group, for a difference in slope changes of −$289 (95% CI −$482, −$96, p=0.003). There were no differences in the change in slopes in case selection or clinical outcomes overall or in any clinical subgroup.
Conclusions:
SNF participation in BPCI was associated with no overall differential change in total Medicare payments per episode, case selection, or clinical outcomes. Exploratory analyses revealed a decrease in Medicare payments in patients with frailty that may warrant further study.
Keywords: Medicare, payment models, skilled nursing facilities, frailty, dementia
INTRODUCTION
Post-acute care (PAC) after a hospitalization helps patients make a successful transition to home. The Centers for Medicare and Medicaid Services (CMS) spends roughly $60 billion annually on PAC, and about a quarter of hospitalizations in Medicare are followed by a skilled nursing facility (SNF) stay.1,2 However, evidence demonstrates wide geographic, provider, and payer-related variability in PAC use, and suggests that SNFs may be used more than clinically necessary.3–7 Consequently, PAC spending has been a major target for policymakers looking to reduce health care costs.
One way in which policymakers have targeted high PAC costs is through experimental payment models. One such model is the Bundled Payments for Care Improvement (BPCI) program, a voluntary initiative that started in 2013. “Model 3” of this program was a track for PAC providers, including SNFs, home health agencies, and long-term care facilities. The rationale was that PAC providers would be most able to decrease unnecessary post-acute spending; it was particularly novel because no major payment experiment had previously enrolled these groups nationally and at such a scale. PAC providers that elected to join could participate for one or more of 48 hospital discharge diagnoses included in the program, including medical and surgical conditions. Participants assumed responsibility for the entire cost of post-hospital care including PAC, readmissions, emergency care, and outpatient visits, starting on the day of admission to the PAC facility and continuing for 30, 60 or 90 days. The BPCI Model 3 track, which ended in September 2018, had 1,143 participants, of which 76% were SNFs.
Bundled payments provide incentives to better coordinate services around care transitions and redesign in-facility care. These changes could be especially helpful for vulnerable older adults such as those with Alzheimer’s or other forms of dementia or those who are frail, populations with high needs and for whom clinical innovations are generally lacking. On the other hand, such programs could induce providers to avoid higher-risk patients or reduce the amount or intensity of care provided in a deleterious way. Yet the impact of this major experiment on health care spending, and even more importantly, on patient outcomes, has not previously been examined. One prior study showed that SNFs participating in BPCI Model 3 reduced Medicare spending for patients with joint replacement,8 but did not include other conditions. Federal contractors performed condition-by-condition analyses on an annual basis,9–12 but there has been no summative evaluation of the program. Unlike the other major track within BPCI, Model 3 was not extended, and CMS has not definitively disclosed why this is the case, though concern for adverse selection may have played a role.12 It is therefore crucial that there be a broad independent examination of the program.
Further, findings on the impact of this payment model have implications for post-acute value-based and alternative payment models more broadly, which are a priority area for both traditional Medicare and Medicare Advantage programs given PAC’s large and variable contribution to Medicare spending. If novel PAC payment models are cost-saving or outcome-enhancing, designing a new PAC-focused payment model could be a significant policy priority. On the other hand, if this model is associated with higher costs, or worse patient outcomes, the concept of applying cost targets to the PAC setting and patient population may need to be substantially revised. In this study we aimed to fill this gap by examining changes in Medicare payments, patient selection, and clinical outcomes under BPCI’s Model 3.
METHODS
Overview of BPCI Model 3 and Participants
In BPCI Model 3, PAC facilities were paid fee-for-service rates, but payments were retrospectively reconciled against targets on a quarterly basis. Target prices for the 30-, 60-, or 90-day episode were set based on each facility’s historical costs, minus a discount of 2–3% depending on the episode length chosen by the participant.13
We obtained publicly available data from CMMI listing BPCI Model 3 participants and their start and end dates. We limited our sample to SNFs, because they made up over three-quarters of Model 3 participants. SNFs could enroll in the program on a quarterly basis between 10/1/13 and the end of enrollment in 12/30/15; the program ended 9/30/2018. However, SNFs primarily enrolled in two major waves, one group on 1/1/14 and then another set of groups over a year later (4/1/15, 7/1/15, and 10/1/15, Supplementary Table S1). Based on prior work demonstrating that early joiners in the hospital version of BPCI accrued savings in longer-term follow-up,14,15 we a priori decided to examine early and late joiners separately; we categorized these groups as Wave 1 and Wave 2, respectively. We included SNFs that enrolled for 47 of the 48 BPCI conditions; we did not include lower extremity joint replacement because it has been examined previously,8 and because of evidence from the hospital track of BPCI that it may follow different patterns than other conditions under the program.16,17 We included all SNFs that enrolled in BPCI, regardless of whether they terminated participation in the program before its end (Supplementary Figure S1).
Participation data were linked to the Certification and Survey Provider Enhanced Reports (CASPER) dataset18 and Nursing Home Compare19 for SNF characteristics, and the Area Health Resources File for market characteristics. Market share was calculated as the proportion of admissions in a county for the condition of interest to each SNF, and market competitiveness was calculated using the Herfindahl-Hirschman Index20.
Control SNFs
To identify control SNFs, we used a matching approach used in prior studies of BPCI.8,21 Using propensity scores based on SNF and market characteristics as well as pre-intervention trends in readmission, mortality, and costs,22 each BPCI SNF-condition pair was matched without replacement with up to 5 controls within the same state and same volume group (average of 1–5, 6–10, or 10+ admissions for a BPCI condition in 2013). Matching was restricted to SNF-condition pairs with a log odds propensity score absolute difference below 0.2.23 Each control SNF could contribute multiple SNF-condition pairs for matching, but SNFs that participated in BPCI for any condition were excluded from being in the control group for other conditions.
Patient Identification
We used Medicare inpatient files from January 1, 2012 to September 30, 2017 to identify index admissions for the BPCI conditions using diagnosis-related group (DRG) codes. We included beneficiaries that were continuously enrolled in Parts A and B during their episode of care as well as the year prior and excluded those with end-stage renal disease (Supplementary Figure S2).
For each index SNF admission, standardized Medicare-allowed episode payments for the initial SNF stay plus 90 days following admission to the SNF (hereafter referred to as Medicare payments, see Supplementary Methods) were calculated on a quarterly basis. Standardized payments following CMS specification remove differences in payment based on wage index and other special payments. Payments were calculated from 100% SNF, inpatient (including long-term hospitals and inpatient rehabilitation), home health, and durable medical equipment claims for 2013 to 2017. Outpatient and clinician claims were examined for a 20% random sample of patients due to data availability. Similarly, one year of baseline data (2012) for the 52 of 1043 SNFs that joined in Wave 1 was limited to a 20% sample. Per BPCI rules, total payments were Winsorized at the 95th percentile of national episode payments annually and adjusted for inflation to prices in 2017. Because the majority of SNFs chose 90-day episodes, we focused on this length.21
We had two patient subpopulations of particular interest: those with frailty and those with Alzheimer’s or other dementias. We identified patients with frailty using a modification of a validated claims-based frailty index (Supplementary Methods).24 Although the original index includes all Medicare claims files, due to data availability our frailty index was calculated from claims that appeared in each patient’s inpatient records only in the year prior to their index SNF admission. To test this modification, we conducted analyses among a 20% sample of patients comparing the frailty index calculated across all files to the index calculated using only inpatient claims and found their correlation to be 0.84. We also calculated payments and outcomes for quintiles of this index (Supplementary Figure S3). For analyses, we considered the top tertile frail. We identified patients with Alzheimer’s and other dementias using chronic condition warehouse (CCW) codes for these conditions.
Study Period
For Wave 1, the baseline period was 1/1/12 through 12/31/13, and the intervention period was 1/1/14 through 9/30/17. For Wave 2, the baseline period was 1/1/13 to each SNF’s official program start date (4/1/15, 7/1/15, or 10/1/15), and the intervention period was the start date through 9/30/17.
Outcomes
Our primary outcome was change in Medicare payments per episode, overall and by wave, defined as any payments to hospitals, SNFs, inpatient rehabilitation facilities, long-term care hospitals, home health agencies, and durable medical equipment. Secondary outcomes included the proportion enrolled in Medicaid, proportion Black, proportion with high frailty; and average number of comorbidities. Additional cost and clinical outcomes included changes in payment components (index SNF stay, readmissions, outpatient/clinician payments), 90-day readmissions and mortality, and 90-day healthy days at home (defined as days without hospitalization, SNF stay, or emergency department visit).25
Analyses
We compared SNF and market characteristics between BPCI SNFs and their matched controls using standardized mean differences with <0.10 signifying good balance. We used an interrupted time-series design to compare slope changes in each group from the baseline to intervention period. Analyses were run at the patient level, with each outcome in a separate segmented linear regression model. We assumed that responding to the BPCI program would be an evolving process and therefore the model allowed for a slope change but no intercept change. For each SNF and its matched controls, time zero was set as the initiation of participation and the Time variable was an indicator for quarter, which ranged from negative 11 to positive 15. A separate variable indicating time that had elapsed in the intervention period was set at the quarterly level, equal to zero prior to program participation, and 1 to a maximum of 15 thereafter. The significance of an interaction term between BPCI participation and the intervention time variable determined whether there had been a greater change in slope in patients at BPCI compared to control SNFs. A marginal, generalized equation approach to modeling (the GENMOD procedure in the SAS statistical package) was used to account for the clustering of patients within SNFs, along with fixed effects for match groups. We included indicator variables for index-hospitalization DRGs, and controlled for age, sex, race, dual enrollment in Medicaid, and patient comorbidities using individual CCW comorbidities. We ran separate analyses for the outpatient and clinician payments since these were only available for 20% of patients. We repeated each of these analyses among Wave 1 and Wave 2 hospitals separately, for patients in the highest and lowest tertile of frailty, and for those with and without dementia.
For our primary outcome, the differential change in total Medicare payments per episode in the overall sample and in the two waves independently for participants compared to controls, a Bonferroni adjustment was pre-specified to account for multiple comparisons, so that a traditionally calculated p<0.0167 was required for significance. Secondary endpoints and analyses should be considered exploratory. Analyses were performed using SAS 9.4 (Cary, NC).
RESULTS
SNF, Market, and Patient Characteristics
Across 47 conditions, there were 1,043 SNFs that participated in BPCI Model 3 and 13,512 SNFs that did not (see Supplementary Table S2 for conditions chosen). Of these, 1,001 BPCI SNFs were matched to 3,873 controls (Table 1). Although BPCI SNFs were larger, more often for-profit, urban, and part of a chain than non-participating SNFs prior to matching (Supplementary Table S3), BPCI SNFs and their controls had similar observable characteristics after matching.
Table 1:
Baseline Skilled Nursing Facility, Market, and Patient Characteristics
| SNF Characteristicsa | BPCI SNFs (n=1,001) | Matched Control SNFs (n=3,873) | SMD |
|---|---|---|---|
| Baseline Volume (admissions), mean (SD) | 111.8 (95.2) | 102.3 (90.4) | 0.10 |
| N of conditions joined | 9.8 (12.2) | n/a | |
| Quarters of follow-up during intervention | 9.5 (1.5) | n/a | |
| Profit Status: For Profit | 859 (85.8%) | 3,175 (82.0%) | 0.10 |
| Profit Status: Non-Profit | 118 (11.8%) | 537 (13.9%) | 0.06 |
| Profit Status: Government | 24 (2.4%) | 161 (4.2%) | 0.09 |
| Urban | 834 (83.3%) | 3182 (82.2%) | 0.03 |
| Number of Federally Certified Beds, mean (SD) | 118.1 (53.9) | 115.9 (55.7) | 0.04 |
| SNF in chain | 861 (86.0%) | 3,182 (82.2%) | 0.10 |
| SNF hospital based | 7 (0.7%) | 34 (0.9%) | 0.02 |
| Region: Northeast | 245 (24.5%) | 798 (20.6%) | 0.10 |
| Region: Midwest | 266 (26.6%) | 1,193 (30.8%) | 0.09 |
| Region: South | 336 (33.6%) | 1,307 (33.8%) | 0.00 |
| Region: West | 153 (15.3%) | 575 (14.8%) | 0.01 |
| Overall Star Rating, mean (SD) | 3.27 (1.40) | 3.30 (1.37) | 0.02 |
| County Characteristics b | |||
| Population 65+ in county , mean (SD) | 104,996 (154,249) | 100,750 (161,628) | 0.03 |
| Median Household Income, $ | 53,445 | 52,602 | 0.06 |
| % Medicare Advantage, mean (SD) | 28.9 (13.1) | 29.1 (13.6) | 0.01 |
| SNF beds Per 10,000 in county, mean (SD) | 414.4 (192.3) | 425.4 (183.5) | 0.06 |
| SNF market share,c mean (SD) | 0.1 (0.2) | 0.1 (0.2) | 0.01 |
| Market competitiveness (HHI),d mean (SD) | 0.0 (0.0) | 0.0 (0.0) | 0.01 |
| Patient Characteristics | |||
| Episodes, N | 183,897 | 188,420 | |
| Age 64 and under | 12,011 (6.5%) | 11,867 (6.3%) | 0.01 |
| Age 65–79 | 61,016 (33.2%) | 60,963 (32.4%) | 0.02 |
| Age 80+ | 110,870 (60.3%) | 115,590 (61.3%) | 0.02 |
| Female | 116,305 (63.2%) | 119,025 (63.2%) | 0.00 |
| Dual Enrollment in Medicaid | 49,699 (27.0%) | 51,856 (27.5%) | 0.01 |
| Disabled without ESRD | 36,936 (20.1%) | 37,342 (19.8%) | 0.01 |
| Frailty | |||
| Highest tertile e | 59,951 (32.6%) | 62,943 (33.4%) | 0.02 |
| Medium tertile | 61,260 (33.3%) | 63,718 (33.8%) | 0.01 |
| Lowest tertile | 62,686 (34.1%) | 61,759 (32.8%) | 0.03 |
| Dementia | 57,891 (31.5%) | 60,796 (32.3%) | 0.02 |
| Race | |||
| White | 158,818 (86.4%) | 165,609 (87.9%) | 0.05 |
| Black | 19,405 (10.6%) | 16,159 (8.6%) | 0.07 |
| Hispanic | 1,754 (1.0%) | 2,450 (1.3%) | 0.03 |
| Unknown/other | 3,920 (2.1%) | 4,202 (2.2%) | 0.01 |
| Comorbidity score, mean (SD) | 6.6 (3.4) | 6.6 (3.4) | 0.02 |
| Level of complexity | |||
| DRG with MCC | 85,097 (46.3%) | 87,487 (46.4%) | 0.00 |
| DRG with CC | 49,461 (26.9%) | 50,131 (26.6%) | 0.01 |
| DRG without CC | 49,339 (26.8%) | 50,802 (27.0%) | 0.00 |
Abbreviations: BPCI, Bundled Payments for Care Improvement; CC, complication or comorbidity; DRG, diagnosis-related group; ESRD, end-stage renal disease; HHI, Herfindahl-Hirschman index; MCC, major complication or comorbidity; SMD, standardized mean difference; SNF, skilled nursing facility.
Both BPCI SNFs and their matched controls could participate in more than one clinical condition. This table shows a SNF-level comparison, even though some SNFs will contribute more patients to the analysis than others as a result.
All county level characteristics are from 2013, other than the number of rehabilitation hospitals which is from 2012.
Markets are defined using counties.
HHI is defined as the sum of the squares of each provider’s market share, such that a perfectly competitive market has an HHI near zero, and a completely concentrated market has an HHI of one.
Tertiles of frailty were calculated based on levels of frailty in the overall Medicare population, and therefore are not symmetrically distributed among the study population. Since ours is a population comprised of individuals requiring SNF care, they are more frail than Medicare beneficiaries on average.
52 SNFs joined in Wave 1 and 949 in Wave 2. Wave 1 SNFs were larger, more often non-profit and urban, and more concentrated in the Northeast and Midwest than Wave 2 SNFs. They had higher readmission rates, lower mortality rates, higher costs, and participated in a mean of 23.7 conditions compared to 8.7 conditions for Wave 2 SNFs (Supplementary Table S4).
There were 183,897 patients in the study cohort from BPCI SNFs and 188,413 from non-BPCI SNFs. Patient characteristics were similar between groups, with more than 60% of episodes among individuals over the age of 80 and women, and over a quarter among individuals dually enrolled in Medicare and Medicaid (Table 1).
Changes in Medicare Payments
In the first quarter of 2012, total unadjusted payments in the BPCI group overall were $28,931 per episode, and total unadjusted payments in the control group were $28,057 per episode (Figure 1, Panel A); adjusted baseline payments were $28,503 and $29,483, respectively (Table 2). During the baseline period, payments were increasing at BPCI SNFs at $121 per episode per quarter (p<0.001); during the intervention, payments decreased at −$398/episode/quarter (p<0.001, Table 2). Among controls, payments were stable in the baseline period (change +$17/episode/quarter, p=0.52) but decreased at −$424/episode/quarter during the intervention (p<0.001), yielding a nonsignificant difference in slope changes of −$79/episode/quarter (95% confidence interval [CI] −$188, $31, p=0.16). There were no differences in the change in slopes in payments for the initial SNF stay or readmissions, or for outpatient/clinician payments.
Figure 1:
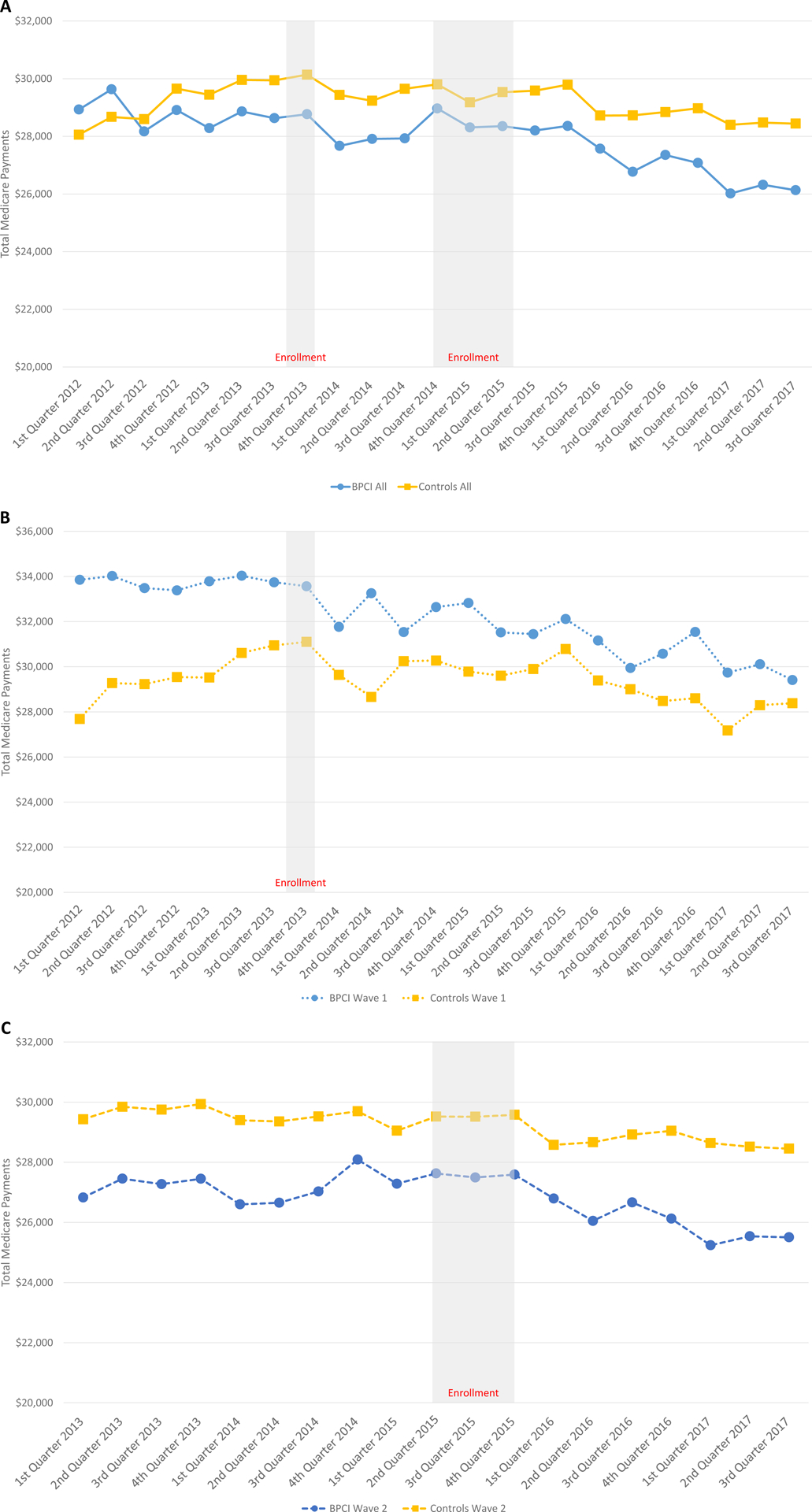
Changes in Total Payments by Wave. (A) Wave 1 and Wave 2 SNFs. (B) Wave 1 SNFs (joined 10/1/13). (C) Wave 2 SNFs (joined 4/1/15–10/1/15). Abbreviations: BPCI, Bundled Payments for Care Improvement; SNF, skilled nursing facility.
Table 2:
Differences in Changes in Quarterly Slopes in Medicare Payments per Episode, Overall and by Clinical Subgroup
| Cost | BPCI Status | First Quarter | Baseline slope | Intervention slope | Change | Lower CI | Upper CI | p |
|---|---|---|---|---|---|---|---|---|
| OVERALL | ||||||||
| Total Payments | BPCI | $28,503 | $121 | −$398 | −$519 | −$598 | −$440 | <0.001 |
| Non-BPCI | $29,483 | $17 | −$424 | −$440 | −$516 | −$365 | <0.001 | |
| Difference | $104 | $25 | −$79 | −$188 | $31 | 0.160 | ||
| Initial SNF stay | BPCI | $13,977 | −$3 | −$236 | −$233 | −$293 | −$173 | <0.001 |
| Non-BPCI | $15,202 | $51 | −$242 | −$293 | −$356 | −$231 | <0.001 | |
| Difference | −$54 | $7 | $61 | −$25 | $146 | 0.167 | ||
| Readmission | BPCI | $7,335 | $17 | −$32 | −$50 | −$71 | −$29 | <0.001 |
| Non-BPCI | $7,455 | −$33 | −$60 | −$27 | −$47 | −$7 | 0.009 | |
| Difference | $51 | $28 | −$23 | −$52 | $6 | 0.122 | ||
| Outpatient/Clinician | BPCI | $4,975 | $63 | $5 | −$58 | −$72 | −$44 | <0.001 |
| Non-BPCI | $4,762 | $53 | $5 | −$49 | −$63 | −$34 | <0.001 | |
| Difference | $9 | $0 | −$10 | −$30 | $11 | 0.350 | ||
| FRAIL | ||||||||
| Total Payments | BPCI | $32,755 | $170 | −$450 | −$620 | −$754 | −$485 | <0.001 |
| Non-BPCI | $32,362 | −$65 | −$395 | −$330 | −$467 | −$193 | <0.001 | |
| Difference | $235 | −$55 | −$289 | −$482 | −$96 | 0.003 | ||
| Initial SNF stay | BPCI | $13,485 | −$22 | −$212 | −$190 | −$274 | −$107 | <0.001 |
| Non-BPCI | $14,201 | $31 | −$197 | −$228 | −$300 | −$156 | <0.001 | |
| Difference | −$53 | −$15 | $38 | −$72 | $147 | 0.500 | ||
| Readmission | BPCI | $8,968 | $19 | −$36 | −$55 | −$99 | −$10 | 0.016 |
| Non-BPCI | $8,912 | −$47 | −$66 | −$19 | −$61 | $22 | 0.364 | |
| Difference | $66 | $30 | −$35 | −$96 | $25 | 0.254 | ||
| Outpatient/Clinician | BPCI | $6,043 | $82 | $4 | −$78 | −$105 | −$52 | <0.001 |
| Non-BPCI | $5,787 | $60 | $9 | −$52 | −$75 | −$28 | <0.001 | |
| Difference | $22 | −$5 | −$27 | −$62 | $9 | 0.140 | ||
| NON-FRAIL | ||||||||
| Total Payments | BPCI | $24,626 | $77 | −$360 | −$437 | −$529 | −$345 | <0.001 |
| Non-BPCI | $26,296 | $102 | −$426 | −$528 | −$616 | −$440 | <0.001 | |
| Difference | −$25 | $66 | $91 | −$35 | $217 | 0.158 | ||
| Initial SNF stay | BPCI | $14,246 | $27 | −$273 | −$299 | −$378 | −$221 | <0.001 |
| Non-BPCI | $15,741 | $74 | −$305 | −$379 | −$462 | −$296 | <0.001 | |
| Difference | −$47 | $33 | $80 | −$34 | $193 | 0.170 | ||
| Readmission | BPCI | $5,820 | $10 | −$19 | −$29 | −$49 | −$9 | 0.005 |
| Non-BPCI | $5,970 | −$16 | −$41 | −$25 | −$44 | −$6 | 0.010 | |
| Difference | $26 | $22 | −$4 | −$32 | $24 | 0.775 | ||
| Outpatient/Clinician | BPCI | $4,025 | $55 | −$1 | −$56 | −$79 | −$34 | <0.001 |
| Non-BPCI | $4,005 | $54 | −$6 | −$60 | −$81 | −$38 | <0.001 | |
| Difference | . | $1 | $4 | $3 | −$28 | $34 | 0.847 |
Abbreviations: BPCI, Bundled Payments for Care Improvement; CI, confidence interval; Q1, quarter one; SNF, skilled nursing facility.
Payments are adjusted using patient-level comorbidities from Medicare’s chronic conditions warehouse (CCW) data.
In exploratory analyses, among patients with frailty, spending declined by $620/episode/quarter in the BPCI group, compared with $330/episode/quarter in the non-BPCI group, for a difference in slope changes of −$289 (95% CI −$482, −$96, p=0.003, Table 2), but there were no differential changes in patients without frailty. There were no decreases in spending among patients either with or without dementia (Supplementary Table S5).
Patterns also differed by wave (Figure 1, Panels B and C). For the 52 SNFs in Wave 1, there was no detectable impact of BPCI on the change in trend in total payments (Table 2). Among the 949 Wave 2 BPCI SNFs, Medicare payments were increasing at $119/episode/quarter at baseline (p<0.001) but decreasing at −$480/episode/quarter during the intervention (p<0.001). Among controls, payments were increasing in the baseline period (change $55/episode/quarter, p=0.03) but decreased at −$405/episode/quarter during the intervention (p<0.001), yielding a difference in slope changes of −$138/episode/quarter (95% CI −$260, −$17, p=0.03, Supplementary Table S5) that was not statistically significant given our correction for multiple comparisons, requiring p<0.0167 for the three components of the primary outcome.
Changes in Volume, Case Mix, and Clinical Outcomes
At the BPCI SNFs and their controls, patient volume per quarter for the conditions included in BPCI increased to a similar degree over time (Table 3). There was a small increase in those dually enrolled in Medicaid in both groups. There were no differential changes in the mean comorbidity score between groups. These patterns were similar among Wave 1 and Wave 2 SNFs and among patients with frailty or dementia (Supplementary Table S6).
Table 3:
Differences in Changes in Quarterly Slopes in Volume and Case Mix, Overall and by Clinical Subgroup
| BPCI Status | First Quarter | Baseline slope | Intervention slope | Change | Lower CI | Upper CI | p | |
|---|---|---|---|---|---|---|---|---|
| OVERALL | ||||||||
| Admissions/quarter | BPCI | 12.5 | 0.09 | 0.00 | −0.09 | −0.22 | 0.05 | 0.198 |
| Non-BPCI | 5.9 | −0.06 | −0.04 | 0.02 | −0.07 | 0.11 | 0.643 | |
| Difference | 0.14 | 0.04 | −0.11 | −0.28 | 0.06 | 0.217 | ||
| % Medicaid | BPCI | 25.0% | 0.0% | 0.0% | 0.0% | 0.0% | 1.0% | <0.001 |
| Non-BPCI | 25.0% | 0.0% | 0.0% | 0.0% | 0.0% | 1.0% | <0.001 | |
| Difference | 0.0% | 0.0% | 0.0% | 0.0% | 0.0% | 0.895 | ||
| % Black | BPCI | 11.0% | 0.0% | 0.0% | 0.0% | 0.0% | 0.0% | 0.009 |
| Non-BPCI | 8.0% | 0.0% | 0.0% | 0.0% | 0.0% | 0.0% | 0.919 | |
| Difference | 0.0% | 0.0% | 0.0% | 0.0% | 0.0% | 0.101 | ||
| N of comorbidities | BPCI | 6.4 | 0.00 | 0.01 | 0.01 | 0.00 | 0.03 | 0.088 |
| Non-BPCI | 6.4 | −0.01 | 0.01 | 0.02 | 0.01 | 0.04 | 0.002 | |
| Difference | 0.01 | 0.00 | −0.01 | −0.03 | 0.01 | 0.286 | ||
| FRAIL | ||||||||
| Admissions/quarter | BPCI | 5.2 | 0.05 | 0.00 | −0.05 | −0.13 | 0.03 | 0.207 |
| Non-BPCI | 3.4 | −0.04 | −0.03 | 0.01 | −0.05 | 0.07 | 0.670 | |
| Difference | 0.09 | 0.02 | −0.07 | −0.17 | 0.04 | 0.215 | ||
| % Medicaid | BPCI | 31.0% | 0.0% | 0.0% | 0.0% | 0.0% | 1.0% | 0.013 |
| Non-BPCI | 30.0% | 0.0% | 0.0% | 1.0% | 0.0% | 1.0% | 0.004 | |
| Difference | 0.0% | 0.0% | 0.0% | −1.0% | 0.0% | 0.919 | ||
| % Black | BPCI | 13.0% | 0.0% | 0.0% | 0.0% | 0.0% | 0.0% | 0.099 |
| Non-BPCI | 10.0% | 0.0% | 0.0% | 0.0% | 0.0% | 0.0% | 0.597 | |
| Difference | 0.0% | 1.0% | 0.0% | 0.0% | 1.0% | 0.121 | ||
| N of comorbidities | BPCI | 7.7 | 0.00 | 0.01 | 0.01 | −0.01 | 0.04 | 0.261 |
| Non-BPCI | 7.7 | 0.00 | 0.02 | 0.02 | −0.01 | 0.04 | 0.126 | |
| Difference | 0.00 | 0.00 | 0.00 | −0.04 | 0.03 | 0.841 | ||
| NON-FRAIL | ||||||||
| Admissions/quarter | BPCI | 5.6 | 0.02 | −0.07 | −0.09 | −0.15 | −0.04 | 0.001 |
| Non-BPCI | 3.4 | −0.01 | 0.00 | 0.00 | −0.05 | 0.05 | 0.990 | |
| Difference | 0.03 | −0.06 | −0.09 | −0.17 | −0.02 | 0.018 | ||
| % Medicaid | BPCI | 20.0% | 0.0% | 0.2% | 0.3% | 0.0% | 0.5% | 0.056 |
| Non-BPCI | 18.9% | −0.2% | 0.1% | 0.3% | 0.1% | 0.6% | 0.011 | |
| Difference | 0.2% | 0.1% | −0.1% | −0.4% | 0.3% | 0.699 | ||
| % Black | BPCI | 7.8% | 0.1% | 0.3% | 0.2% | 0.0% | 0.3% | 0.049 |
| Non-BPCI | 7.0% | −0.2% | 0.0% | 0.1% | 0.0% | 0.3% | 0.124 | |
| Difference | 0.3% | 0.3% | 0.0% | −0.2% | 0.2% | 0.919 | ||
| N of comorbidities | BPCI | 5.2 | 0.00 | 0.00 | 0.00 | −0.02 | 0.02 | 0.989 |
| Non-BPCI | 5.0 | −0.02 | 0.01 | 0.03 | 0.01 | 0.05 | 0.001 | |
| Difference | 0.02 | −0.01 | −0.03 | −0.06 | −0.01 | 0.015 |
Abbreviations: BPCI, Bundled Payments for Care Improvement; CI, confidence interval; Q1, quarter one; SNF, skilled nursing facility.
Beneficiaries in BPCI SNFs had no differential changes in 30- or 90-day readmission or mortality rates, healthy days at home, or length of initial SNF stay. These patterns were similar among Wave 1 and Wave 2 SNFs and among subgroups of patients with frailty or dementia (Supplementary Table S7).
DISCUSSION
SNF participation in episode-based payment under BPCI Model 3 was associated with no significant overall differences in total Medicare payments, volume, case mix, or clinical outcomes. Among patients with frailty, and among later-joining SNFs, there were small reductions in spending that should be considered hypothesis-generating.
Our findings are in contrast to findings suggesting that BPCI Model 3 was associated with reductions in Medicare payments for patients with joint replacement.8 As in studies of the BPCI program that focused on hospitals, joint replacement may follow a different paradigm than medical and surgical conditions more broadly. Joint replacement patients are carefully selected (at least among elective procedures), and follow specific care pathways before, during, and after their procedures. Patients with more variable disease courses, such as those with heart failure, sepsis, or cardiac surgery, may represent a more difficult population for care redesign, and indeed in studies of the hospital track of BPCI, savings were smaller and later to emerge for medical conditions.14–16
It is also possible that the lack of major savings in Model 3 is because of the way the program is designed. In the hospital track for BPCI, most hospitals saved money by decreasing PAC, thus reducing someone else’s revenue rather than their own. Expecting PAC providers to reduce PAC use may be unrealistic, or the rewards for doing so may not have been strong enough. Our findings may also explain in part why CMS did not choose to move forward with BPCI Model 3 when they renewed the program for hospitals and physician groups, and have implications for other payers, both in the US and internationally, seeking to reduce PAC spending.
Where savings did accrue, it seemed to be among later-joining SNFs and patients with frailty, though these should only be considered hypothesis-generating. Frail patients are much more costly than non-frail ones, so it may not be surprising that savings were seen within this group, and it is encouraging that the savings were not accompanied by obvious changes in patient selection or worsening clinical outcomes like readmission rates or healthy days at home. However, our metrics are likely too blunt to pick up small changes in functional status or long-term care needs that could occur if care were inappropriately withheld from this vulnerable group, and warrants ongoing study.
There have been prior studies examining BPCI, though most have focused on hospitals.15,16,21,26–29 There is only one study in the peer-reviewed literature on Model 3 to our knowledge, which demonstrated savings for total joint replacement.8 There have been four annual federal reports that evaluated individual conditions under Model 3, though they did not examine the program as a whole.9–12 Among the 11 individual conditions included in year 5 of the program evaluation (of the 48 from which participants could choose), payment reductions for 5 conditions reached significance at p<0.05, with savings of $1,849 to $2,991 per episode.12 They also reported potential evidence of adverse selection in 5 conditions, which we did not find in the broader sample. Differences between our findings and theirs could be because of the different number of conditions in the analyses, or because their analysis only included SNFs that remained in the program while ours took an intent-to-treat approach.
In this context, our findings have significant policy implications. First, the lack of savings in the program overall suggests that new approaches to alternative payment models may be needed in the PAC setting. Coupled with modest impacts of the value-based payment program aimed at SNFs,30,31 policymakers may need to reconsider where the most effective touchpoints are in encouraging SNFs to operate efficiently. Similarly, Medicare Advantage programs focused on individuals in PAC or long-term care settings (for example, institutional special needs plans) may need novel approaches to reduce costs. Focusing on quality improvement rather than costs may have potential, given emerging studies on interventions to reduce unnecessary hospital transfer among SNF and LTC residents32 – a marker of quality for which we did not observe improvement in this intervention.
Limitations
There are limitations to our findings. While we considered changes in case mix to represent adverse selection, it is possible that changes reflect more appropriate matching of patients to PAC capabilities, for example patients with higher care needs going to long-term acute care hospitals rather than SNFs. We examined a large number of conditions, beneath which there is likely significant heterogeneity indicating conditions or patients for which bundling may be best suited; this represents an important area for future work. BPCI is a voluntary program and our findings may not generalize to SNFs more broadly. We do not know whether any SNFs had financial relationships with hospitals participating in other BPCI models, which could impact our findings. Although we used propensity score matching to account for observable differences between BPCI participants and controls, other approaches to identifying a control group may have yielded different results. We focused on SNF participants; though these comprise the majority of Model 3 participants,13 patterns may differ for home health agencies or inpatient rehabilitation facilities. We only had a 20% sample for outpatient/clinician fees, and thus could not include those in total payment calculations. Because Medicare has not released data on target pricing nor on SNFs’ savings or losses under the program, we could only evaluate BPCI’s impact on patients and their outcomes and could not determine whether SNFs received bonuses or penalties as a result. We had a limited follow-up period for our later joiners, and longer-term follow-up may be necessary to fully evaluate how care evolves in this group,33 though among the group of SNFs with the longest follow-up, no savings were seen.
In conclusion, SNF participation in BPCI was associated with no overall differential change in total Medicare payments per episode, case selection, or 90-day clinical outcomes. Among patients with frailty, and among later-joining SNFs, there were small reductions in spending that should be considered hypothesis-generating.
Supplementary Material
Supplementary Methods
Supplementary Table S1: Enrollment of Skilled Nursing Facilities in BPCI
Supplementary Figure S1: Flowchart of SNF Inclusion and Exclusion
Supplementary Figure S2: Flowchart of Patient Inclusion and Exclusion
Supplementary Table S2: Conditions Selected by Skilled Nursing Facilities in BPCI
Supplementary Figure S3: Outcomes and Total Medicare Payments of Skilled Nursing Facility Patients by Frailty Quintile
Supplementary Table S3: Baseline Skilled Nursing Facility and Market Characteristics, Before Matching
Supplementary Table S4: Baseline Skilled Nursing Facility and Market Characteristics, BPCI Wave 1 versus Wave 2
Supplementary Table S5: Differences in Changes in Quarterly Slopes in Medicare Payments per Episode by Wave and Dementia Subgroup
Supplementary Table S6: Differences in Changes in Quarterly Slopes in Volume and Case Mix by Wave and Dementia Subgroup
Supplementary Table S7: Differences in Changes in Quarterly Slopes in Clinical Outcomes by Wave and Dementia Subgroup
Table 4:
Differences in Changes in Quarterly Slopes in Clinical Outcomes, Overall and by Clinical Subgroup
| BPCI Status | First Quarter | Baseline slope | Intervention slope | Change | Lower CI | Upper CI | p | |
|---|---|---|---|---|---|---|---|---|
| OVERALL | ||||||||
| 90-day Readmission | BPCI | 37.1% | 0.3% | −0.4% | −0.7% | −0.9% | −0.5% | <0.001 |
| Non-BPCI | 38.0% | 0.1% | −0.5% | −0.6% | −0.8% | −0.5% | <0.001 | |
| Difference | 0.2% | 0.2% | −0.1% | −0.3% | 0.2% | 0.522 | ||
| 90-day Mortality | BPCI | 15.2% | −0.2% | −0.2% | 0.0% | −0.2% | 0.2% | 0.924 |
| Non-BPCI | 15.6% | −0.3% | −0.1% | 0.1% | 0.0% | 0.3% | 0.120 | |
| Difference | 0.1% | −0.1% | −0.1% | −0.3% | 0.1% | 0.323 | ||
| HDAH | BPCI | 42.7 | 0.0 | 0.9 | 0.9 | 0.7 | 1.0 | <0.001 |
| Non-BPCI | 40.1 | 0.2 | 0.9 | 0.7 | 0.6 | 0.9 | <0.001 | |
| Difference | −0.2 | 0.0 | 0.1 | −0.1 | 0.3 | 0.253 | ||
| Initial SNF Days | BPCI | 26.5 | −0.1 | −0.5 | −0.4 | −0.5 | −0.2 | <0.001 |
| Non-BPCI | 29.1 | −0.1 | −0.6 | −0.5 | −0.7 | −0.3 | <0.001 | |
| Difference | 0.0 | 0.1 | 0.1 | −0.1 | 0.4 | 0.183 | ||
| FRAIL | ||||||||
| 90-day Readmission | BPCI | 53.4% | 0.3% | −0.3% | −0.6% | −0.9% | −0.3% | <0.001 |
| Non-BPCI | 54.8% | 0.1% | −0.6% | −0.7% | −0.9% | −0.4% | <0.001 | |
| Difference | 0.2% | 0.2% | 0.0% | −0.3% | 0.4% | 0.802 | ||
| 90-day Mortality | BPCI | 19.2% | −0.3% | −0.1% | 0.2% | −0.1% | 0.5% | 0.106 |
| Non-BPCI | 20.1% | −0.1% | −0.2% | 0.0% | −0.3% | 0.3% | 0.841 | |
| Difference | −0.2% | 0.1% | 0.3% | −0.1% | 0.7% | 0.194 | ||
| HDAH | BPCI | 33.9 | 0.0 | 0.9 | 0.9 | 0.6 | 1.1 | <0.001 |
| Non-BPCI | 32.7 | 0.2 | 0.8 | 0.6 | 0.4 | 0.8 | <0.001 | |
| Difference | −0.2 | 0.0 | 0.2 | −0.1 | 0.6 | 0.145 | ||
| Initial SNF Days | BPCI | 27.3 | −0.1 | −0.5 | −0.4 | −0.6 | −0.1 | 0.001 |
| Non-BPCI | 29.7 | −0.1 | −0.5 | −0.4 | −0.7 | −0.2 | <0.001 | |
| Difference | 0.0 | 0.1 | 0.1 | −0.2 | 0.4 | 0.569 | ||
| NON-FRAIL | ||||||||
| 90-day Readmission | BPCI | 20.6% | 0.3% | −0.3% | −0.5% | −0.8% | −0.3% | <0.001 |
| Non-BPCI | 21.3% | 0.2% | −0.3% | −0.5% | −0.8% | −0.3% | <0.001 | |
| Difference | 0.1% | 0.1% | 0.0% | −0.3% | 0.3% | 0.953 | ||
| 90-day Mortality | BPCI | 8.2% | −0.2% | −0.3% | −0.1% | −0.3% | 0.1% | 0.458 |
| Non-BPCI | 10.6% | −0.3% | −0.2% | 0.1% | −0.1% | 0.3% | 0.425 | |
| Difference | 0.1% | −0.1% | −0.1% | −0.4% | 0.1% | 0.277 | ||
| HDAH | BPCI | 52.9 | 0.0 | 0.8 | 0.8 | 0.6 | 1.0 | <0.001 |
| Non-BPCI | 48.4 | 0.0 | 0.9 | 0.8 | 0.6 | 1.0 | <0.001 | |
| Difference | 0.0 | 0.0 | 0.0 | −0.3 | 0.2 | 0.804 | ||
| Initial SNF Days | BPCI | 25.9 | −0.1 | −0.5 | −0.4 | −0.5 | −0.2 | <0.001 |
| Non-BPCI | 28.5 | −0.1 | −0.6 | −0.5 | −0.7 | −0.4 | <0.001 | |
| Difference | 0.0 | 0.1 | 0.1 | −0.1 | 0.4 | 0.211 |
Abbreviations: BPCI, Bundled Payments for Care Improvement; CI, confidence interval; HDAH, healthy days at home; Q1, quarter one; SNF, skilled nursing facility.
Key Points:
SNF participation in Medicare’s Bundled Payments for Care Improvement program was not associated with changes in spending or clinical outcomes, though decreases in spending were seen for frail patients.
Why does this matter? Different approaches may be needed to improve care and reduce costs in the post-acute setting.
ACKNOWLEDGEMENTS
Conflict of Interest:
Dr. Joynt Maddox receives research support from the National Heart, Lung, and Blood Institute (R01HL143421) and National Institute on Aging (R01AG060935, R01AG063759, and R21AG065526), and previously did contract work for the US Department of Health and Human Services. She also serves on the Health Policy Advisory Council for the Centene Corporation (St. Louis, MO). The other authors have no conflicts.
Sponsor’s Role:
This study was funded by the National Institute on Aging (R01AG060935 and K23AG058806). The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; or the decision to submit the manuscript for publication.
Footnotes
Meetings: ASHECon 2020 and AcademyHealth 2020 Annual Research Meeting.
REFERENCES
- 1.Medicare Payment Advisory Commission. Report to Congress: Medicare Payment Policy - Chapter 8: Skilled nursing facility services. Washington, DC2019. [Google Scholar]
- 2.Health at a Glance 2019. 2019.
- 3.Barnett ML, Mehrotra A, Grabowski DC. Postacute Care - The Piggy Bank for Savings in Alternative Payment Models? N Engl J Med. 2019;381(4):302–303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Burke RE, Jones CD, Coleman EA, Falvey JR, Stevens-Lapsley JE, Ginde AA. Use of post-acute care after hospital discharge in urban and rural hospitals. Am J Accountable Care. 2017;5(1):16–22. [PMC free article] [PubMed] [Google Scholar]
- 5.Werner RM, Coe NB, Qi M, Konetzka RT. Patient Outcomes After Hospital Discharge to Home With Home Health Care vs to a Skilled Nursing Facility. JAMA Intern Med. 2019;179(5):617–623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Werner RM, Konetzka RT. Trends in Post-Acute Care Use Among Medicare Beneficiaries: 2000 to 2015. JAMA. 2018;319(15):1616–1617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kosar CM, Loomer L, Ferdows NB, Trivedi AN, Panagiotou OA, Rahman M. Assessment of Rural-Urban Differences in Postacute Care Utilization and Outcomes Among Older US Adults. JAMA network open. 2020;3(1):e1918738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Barnett ML, Joynt Maddox KE, Orav EJ, Grabowski DC, Epstein AM. Association of Skilled Nursing Facility Participation in a Bundled Payment Model With Institutional Spending for Joint Replacement Surgery. Jama. 2020;324(18):1869–1877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dummit L, Marrufo G, Marshall J, et al. CMS Bundled Payments for Care Improvement Initiative Models 2–4: Year 2 Evaluation & Monitoring Annual Report. Falls Church, VA: The Lewin Group; August 2016. [Google Scholar]
- 10.Dummit L, Marrufo G, Marshall J, et al. CMS Bundled Payments for Care Improvement Initiative Models 2–4: Year 3 Evaluation & Monitoring Annual Report. Falls Church, VA: The Lewin Group; October 2017. [Google Scholar]
- 11.Dummit L, Marrufo G, Marshall J, et al. CMS Bundled Payments for Care Improvement Initiative Models 2–4: Year 4 Evaluation & Monitoring Annual Report. Falls Church, VA: The Lewin Group; June 2018. [Google Scholar]
- 12.Dummit L, Marrufo G, Marshall J, et al. CMS Bundled Payments for Care Improvement Initiative Models 2–4: Year 5 Evaluation & Monitoring Annual Report. Falls Church, VA: The Lewin Group; October 2018. [Google Scholar]
- 13.Centers for Medicare and Medicaid Services. Bundled Payments for Care Improvement (BPCI) Initiative: General Information http://innovation.cms.gov/initiatives/bundled-payments/. Published 2017. Accessed May 8, 2017.
- 14.Joynt Maddox KE, Orav EJ, Zheng J, Epstein AM. Learning and the “Early Joiner” Effect for Medical Conditions in Medicare’s Bundled Payments for Care Improvement Program: Retrospective Cohort Study. Med Care. 2020. [DOI] [PubMed] [Google Scholar]
- 15.Rolnick JA, Liao JM, Emanuel EJ, et al. Spending and quality after three years of Medicare’s bundled payments for medical conditions: quasi-experimental difference-in-differences study. BMJ (Clinical research ed). 2020;369:m1780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Joynt Maddox KE, Orav EJ, Zheng J, Epstein AM. Evaluation of Medicare’s Bundled Payments Initiative for Medical Conditions. N Engl J Med. 2018;379(3):260–269. [DOI] [PubMed] [Google Scholar]
- 17.Navathe AS, Emanuel EJ, Venkataramani AS, et al. Spending And Quality After Three Years Of Medicare’s Voluntary Bundled Payment For Joint Replacement Surgery. Health Aff (Millwood). 2020;39(1):58–66. [DOI] [PubMed] [Google Scholar]
- 18.Cowles Research Group. CASPER & OSCAR. Cowles Research Group https://www.longtermcareinfo.com/data/casper-and-oscar.php. Published 2020. Accessed June 25, 2020.
- 19.U.S. Department of Health & Human Services. Nursing Home Compare. United States Department of Health and Human Services https://www.medicare.gov/nursinghomecompare/search.html. Accessed June 25, 2020.
- 20.Antitrust Division of the United States Department of Justice. Herfindahl-Hirschman Index. United States Department of Justice https://www.justice.gov/atr/herfindahl-hirschman-index. Published 2015. Accessed May 2, 2018.
- 21.Dummit LA, Kahvecioglu D, Marrufo G, et al. Association Between Hospital Participation in a Medicare Bundled Payment Initiative and Payments and Quality Outcomes for Lower Extremity Joint Replacement Episodes. JAMA. 2016;316(12):1267–1278. [DOI] [PubMed] [Google Scholar]
- 22.Daw JR, Hatfield LA. Matching and Regression to the Mean in Difference-in-Differences Analysis. Health Serv Res. 2018;53(6):4138–4156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Austin PC. Optimal caliper widths for propensity-score matching when estimating differences in means and differences in proportions in observational studies. Pharmaceutical statistics. 2011;10(2):150–161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kim DH, Schneeweiss S, Glynn RJ, Lipsitz LA, Rockwood K, Avorn J. Measuring Frailty in Medicare Data: Development and Validation of a Claims-Based Frailty Index. J Gerontol A Biol Sci Med Sci. 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Burke LG, Orav EJ, Zheng J, Jha AK. Healthy Days at home: A novel population-based outcome measure. Healthc (Amst). 2020;8(1):100378. [DOI] [PubMed] [Google Scholar]
- 26.Bhatt SP, Wells JM, Iyer AS, et al. Results of a Medicare Bundled Payments for Care Improvement Initiative for Chronic Obstructive Pulmonary Disease Readmissions. Ann Am Thorac Soc. 2017;14(5):643–648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Navathe AS, Troxel AB, Liao JM, et al. Cost of Joint Replacement Using Bundled Payment Models. JAMA Intern Med. 2017;177(2):214–222. [DOI] [PubMed] [Google Scholar]
- 28.Iorio R, Clair AJ, Inneh IA, Slover JD, Bosco JA, Zuckerman JD. Early Results of Medicare’s Bundled Payment Initiative for a 90-Day Total Joint Arthroplasty Episode of Care. The Journal of arthroplasty. 2016;31(2):343–350. [DOI] [PubMed] [Google Scholar]
- 29.Joynt Maddox KE, Orav EJ, Zheng J, Epstein AM. Post-Acute Care After Joint Replacement in Medicare’s Bundled Payments for Care Improvement Initiative. Journal of the American Geriatrics Society. 2019. [DOI] [PubMed] [Google Scholar]
- 30.Hefele JG, Wang XJ, Lim E. Fewer Bonuses, More Penalties At Skilled Nursing Facilities Serving Vulnerable Populations. Health Aff (Millwood). 2019;38(7):1127–1131. [DOI] [PubMed] [Google Scholar]
- 31.Qi AC, Luke AA, Crecelius C, Joynt Maddox KE. Performance and Penalties in Year 1 of the Skilled Nursing Facility Value-Based Purchasing Program. Journal of the American Geriatrics Society. 2020;68(4):826–834. [DOI] [PubMed] [Google Scholar]
- 32.Blackburn J, Stump TE, Carnahan JL, et al. Reducing the Risk of Hospitalization for Nursing Home Residents: Effects and Facility Variation From OPTIMISTIC. Journal of the American Medical Directors Association. 2020;21(4):545–549.e541. [DOI] [PubMed] [Google Scholar]
- 33.Dundon JM, Bosco J, Slover J, Yu S, Sayeed Y, Iorio R. Improvement in Total Joint Replacement Quality Metrics: Year One Versus Year Three of the Bundled Payments for Care Improvement Initiative. The Journal of bone and joint surgery American volume. 2016;98(23):1949–1953. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Methods
Supplementary Table S1: Enrollment of Skilled Nursing Facilities in BPCI
Supplementary Figure S1: Flowchart of SNF Inclusion and Exclusion
Supplementary Figure S2: Flowchart of Patient Inclusion and Exclusion
Supplementary Table S2: Conditions Selected by Skilled Nursing Facilities in BPCI
Supplementary Figure S3: Outcomes and Total Medicare Payments of Skilled Nursing Facility Patients by Frailty Quintile
Supplementary Table S3: Baseline Skilled Nursing Facility and Market Characteristics, Before Matching
Supplementary Table S4: Baseline Skilled Nursing Facility and Market Characteristics, BPCI Wave 1 versus Wave 2
Supplementary Table S5: Differences in Changes in Quarterly Slopes in Medicare Payments per Episode by Wave and Dementia Subgroup
Supplementary Table S6: Differences in Changes in Quarterly Slopes in Volume and Case Mix by Wave and Dementia Subgroup
Supplementary Table S7: Differences in Changes in Quarterly Slopes in Clinical Outcomes by Wave and Dementia Subgroup


