Abstract
Background:
Considering the lengthy recovery and high recurrence risk after a hamstring injury, effective rehabilitation and accurate prognosis are fundamental to timely and safe return to play (RTP) for athletes.
Purpose:
To analyze methods of rehabilitation for acute proximal and muscular hamstring injuries and summarize prognostic factors associated with RTP.
Study Design:
Systematic review; Level of evidence, 4.
Methods:
In August 2020, MEDLINE, CINAHL, Cochrane Central Register of Controlled Trials, and SPORTDiscus were queried for studies examining management and factors affecting RTP after acute hamstring injury. Included were randomized controlled trials, cohort studies, case-control studies, and case series appraising treatment effects on RTP, reinjury rate, strength, flexibility, hamstrings-to-quadriceps ratio, or functional assessment, as well as studies associating clinical and magnetic resonance imaging factors with RTP. Risk of bias was assessed using the Cochrane Risk-of-Bias Tool for Randomized Trials or the Methodological Index for Non-Randomized Studies (MINORS).
Results:
Of 1289 identified articles, 75 were included. The comparative and noncomparative studies earned MINORS scores of 18.8 ± 1.3 and 11.4 ± 3.4, respectively, and 12 of the 17 randomized controlled trials exhibited low risk of bias. Collectively, studies of muscular injury included younger patients and a greater proportion of male athletes compared with studies of proximal injury. Surgery for proximal hamstring ruptures achieved superior outcomes to nonoperative treatment, whereas physiotherapy incorporating eccentric training, progressive agility, and trunk stabilization restored function and hastened RTP after muscular injuries. Platelet-rich plasma injection for muscular injury yielded inconsistent results. The following initial clinical findings were associated with delayed RTP: greater passive knee extension of the uninjured leg, greater knee extension peak torque angle, biceps femoris injury, greater pain at injury and initial examination, “popping” sound, bruising, and pain on resisted knee flexion. Imaging factors associated with delayed RTP included magnetic resonance imaging-positive injury, longer lesion relative to patient height, greater muscle/tendon involvement, complete central tendon or myotendinous junction rupture, and greater number of muscles injured.
Conclusion:
Surgery enabled earlier RTP and improved strength and flexibility for proximal hamstring injuries, while muscular injuries were effectively managed nonoperatively. Rehabilitation and athlete expectations may be managed by considering several suitable prognostic factors derived from initial clinical and imaging examination.
Keywords: hamstring injury, imaging, rehabilitation, return to play
Hamstring injury is one of the most common injuries among athletes. 31 Athletes involved in activities requiring high-speed running 6,10 or stretching to extreme muscle lengths 7,8 are particularly subject to hamstring injury, which is classified according to location within the muscle complex, specific muscle(s) affected, severity, and chronicity. Because of the complex anatomic and biomechanical properties necessary to facilitate movement at both the hip and the knee, however, uniform assessment of hamstring injury epidemiology is challenging. 22 Determining whether the injury affects the proximal origin or muscle belly is an important first step to elucidating injury epidemiology, understanding clinical presentation, and identifying potential complications. Proximal hamstring injuries occur predominantly in middle-aged patients and are often more severe, 43 usually associated with prolonged convalescence and carrying greater risk for complications such as postoperative weakness and sciatic nerve injury. 13,81 Conversely, muscular injuries occur more commonly in younger male athletes with risk factors such as strength or flexibility deficits, and although initially milder than proximal injuries, there exists substantial risk for recurrent injury of greater severity. 32,67
Consideration of injury location is also important when determining clinical management. Although approach to rehabilitation is tailored according to injury location, severity, and patient goals of therapy, management generally includes physiotherapy ∥ with possible concomitant surgical intervention ¶ or injections of platelet-rich plasma (PRP). # Despite extensive research investigating methods of rehabilitation and advances in therapeutic techniques designed to return athletes to competition quickly while minimizing reinjury risk, 61,74 acute hamstring injury continues to account for significant absence from sports, and little consensus has been reached regarding optimal management strategies. Accurate prediction of time to return to play (RTP) is necessary to guide activity progression and manage patient expectations for recovery. Although clinicians often rely on clinical and structural factors gleaned from initial examination and magnetic resonance imaging (MRI) scans to inform their prognosis, whether these adequately correlate with recovery time remains a topic of debate.
The purpose of this study was to systematically review the literature concerning evidence-based management of acute proximal and muscular hamstring injuries in athletes and to report the baseline clinical and MRI factors associated with RTP.
Methods
Research Framework
The design and reporting of this systematic review are compliant with the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines. 60
Eligibility Criteria
English-language articles examining management and factors affecting RTP after acute hamstring injury were considered for eligibility, and those meeting each of the following criteria were included: (1) the article employed a randomized controlled trial (RCT), cohort, case-control, or case series design; (2) patients had sustained acute proximal or muscular hamstring injury, defined as <6 weeks between injury and initial evaluation; (3) the authors investigated the effects of a well-described intervention on hamstring rehabilitation or associated baseline clinical or MRI assessment findings with RTP; and (4) outcome measures included time to RTP, reinjury rate, hamstring strength, hamstring range of motion (ROM), hamstrings-to-quadriceps (H:Q) ratio, or results of standardized functional assessment. Studies limited to only chronic tendinopathy or only recurrent hamstring injuries were excluded.
Information Sources and Search
Searches of MEDLINE (1966 to present), CINAHL (1981 to present), Cochrane Central Register of Controlled Trials (1996 to present), and SPORTDiscus (1949 to present) were conducted in August 2020. To identify articles pertinent to acute hamstring injury management and prognosis, a comprehensive search strategy was developed using applicable Medical Subject Headings terms and keywords (see Appendix Table A1). Subsequent manual inspection of included article reference lists ascertained any additional relevant articles not found via the computerized search.
Study Selection
Two reviewers (S.S.R. and M.P.K.)independently screened all articles on the basis of title and abstract using a specialized systematic review software (Covidence systematic review software; Veritas Health Innovation). Potentially eligible articles underwent full-text review prior to final determination of study inclusion. Any disagreements between reviewers were resolved via discussion.
Data Collection
Based on the Cochrane Handbook for Systematic Reviews of Interventions recommendations for data extraction, 28 a custom data extraction form was developed to collect information on study design; methods; population; intervention(s); and outcome measures, including time to RTP, reinjury rate, hamstring strength, hamstring ROM, H:Q ratio, and/or standardized functional assessment. All data were extracted by a single reviewer (S.S.R.) and verified by a second reviewer (M.P.K.).
Risk-of-Bias and Quality Assessment
A risk-of-bias assessment was performed for all included studies. RCTs were assessed using the Revised Cochrane Risk-of-Bias Tool for Randomized Trials, which appraises studies based on patient randomization, assignment to intervention, availability of outcome data, outcome measurement, and selection of reported results. 80 Overall risk of bias for each RCT was judged as “low,” “some concerns,” or “high.” Nonrandomized studies were assessed using the Methodological Index for Non-Randomized Studies (MINORS) tool. 79 The MINORS tool represents a 12-item assessment of methodological value, with 8 criteria indicated for noncomparative studies and an additional 4 criteria indicated for comparative studies. Each criterion was scored from 0 to 2, with higher overall scores indicating higher quality of evidence.
Statistical Analysis
Patient characteristics were quantified using descriptive statistics, calculated as weighted means and standard deviations across included studies. We used t tests to identify any differences in characteristics between patients with acute proximal and muscular hamstring injuries. A P value < .05 was used to determine statistical significance. Stata (Version 13.1; StataCorp) software was used for all statistical analyses.
Results
Study Selection
The database search retrieved 1704 articles, with an additional 22 identified via manual search as potentially relevant. After removing duplicates, 1289 articles were screened on the basis of title and abstract. A total of 126 articles were retained for full-text review, of which 51 were excluded for failure to satisfy the inclusion criteria, and 75 were included (Figure 1).
Figure 1.
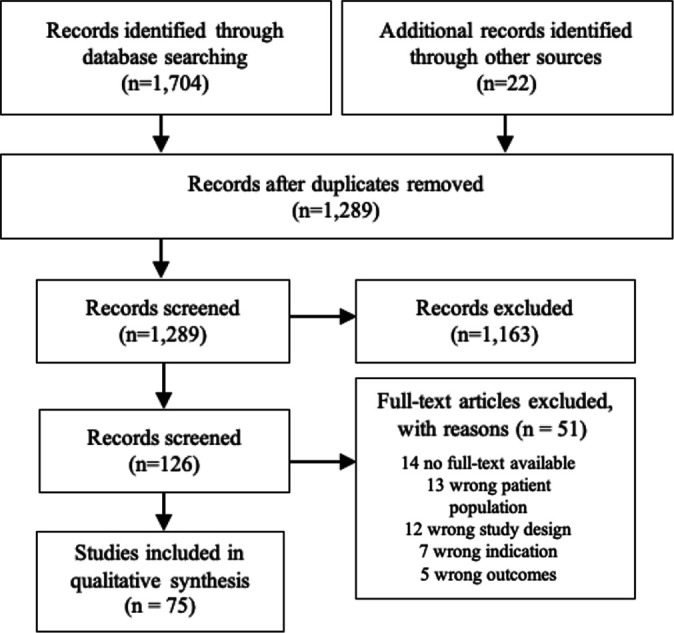
Study flowchart.
Study Characteristics
A total 45 of the included studies pertained to injury management,** 25 defined factors associated with RTP, †† and 5 integrated both. 1,9,10,45,76 Studies investigated 3 to 360 male and female athletes engaged in various sports of all competitive levels with a mean age of 14 to 58 years. Of the studies pertaining to injury management, 22 ‡‡ concerned injuries to the proximal origin, and 28 §§ were specific to muscular injuries. A variety of techniques and programs were assessed according to recovery time, reinjury risk, and degree of functional improvement, including surgical and nonsurgical treatment, ∥∥ PRP injection, ¶¶ and physiotherapeutic interventions. ## There was a lack of uniformity across studies regarding diagnostic methods, criteria for RTP, and assessment of outcomes. Prognostic studies determined whether baseline findings were correlated with time to RTP by conducting clinical and/or MRI assessment shortly after injury.
Of note, study samples were duplicated in a few articles. 5 –7,39,40,44,83,85 Specifically, injuries to the 18 sprinters and 15 dancers described in Askling et al 5 were also investigated separately in 2 other studies by the same authors. 6,7 Hamilton et al, 40 Jacobsen et al, 44 van der Made et al, 83 and Wangensteen et al 85 additionally shared considerable overlap in patient populations due to their use of pooled data from a prior RCT. 39
Risk-of-Bias Assessment
Seventeen RCTs were included, of which 12 were determined to present low risk of bias, a and 5 were judged to raise some concerns. 9,10,46,49,70 Nonrandomized studies comprised 11 comparative b and 47 noncomparative c designs with average scores of 18.8 ± 1.3 and 11.4 ± 3.4 on MINORS assessment, respectively.
Synthesis of Results
Patient Characteristics
Acute hamstring injuries were classified according to location within the muscle complex. Collectively, 775 patients with proximal hamstring injury and 1057 patients with muscular hamstring injury were assessed by the included studies. Studies investigating methods of proximal injury management generally included younger patients and a greater proportion of male patients compared with studies of proximal hamstring injury rehabilitation (Table 1).
TABLE 1.
Comparison of Patient Characteristics Between Studies of Proximal Versus Muscular Hamstring Injury a
| Studies of Proximal Hamstring Injury Management | Studies of Muscular Hamstring Injury Management | |
|---|---|---|
| No. of patients | 775 | 1057 |
| Patient age, y, mean ± SD | 42.4 ± 10.5 | 26.2 ± 6.5 |
| Patient sex, % male | 57.2 | 87.6 |
a Bold values were statistically significantly different between groups (P < .05).
Management
Management of hamstring injury was also dependent upon localization to the proximal origin or muscle belly. Time to RTP and reinjury rate at final follow-up are listed according to intervention in Tables 2 to 4. Because of extensive variation in the methods of measuring and reporting hamstring strength, ROM, H:Q ratio, and functional assessment, individual study results for these outcomes are discussed in the text only and not presented in the tables.
TABLE 2.
Summary of Studies on Management of Acute Injuries to the Proximal Hamstring a
| Additional Outcomes | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Lead Author (Year) | Risk of Bias b | Injury Type | Intervention | N | Mean ± SD Time to RTP, d | Reinjury Rate, % | Mean Follow-up, mo | Hamstring Strength | Hamstring ROM | H:Q Ratio | Functional Assessment |
| Arner (2019) 4 | 9 (16) | Partial proximal hamstring avulsion | Surgical | 64 | 333 (range, 150-1440) | — | 78 | X | |||
| Ayuob (2020) 11 | 12 (16) | Complete proximal semimembranosus rupture | Surgical | 20 | 83.3 ± 39.9 | 0.0 | 35 | X | X | X | |
| Ayuob (2020) 12 | 12 (16) | Partial/complete tear of proximal MTJ of long head of biceps | Surgical | 64 | 93.8 ± 35.7 | — | 24 | X | X | X | |
| Barnett (2015) 13 | 10 (16) | Partial/complete proximal hamstring avulsion | Surgical | 38 | — | — | 54 | X | |||
| Best (2019) 15 | 9 (16) | Complete proximal hamstring avulsion | Surgical | 49 | — | — | 28 | X | |||
| Biedert (2015) 17 | 9 (16) | Avulsion fracture of ischial tuberosity | Surgical | 3 | — | — | 24 | X | |||
| Birmingham (2011) 18 | 11 (16) | Complete proximal hamstring avulsion | Surgical | 23 | 294 (range, 90-1080) | — | 43 | X | X | ||
| Blakeney (2017) 19 | 15 (16) | Partial/complete proximal hamstring avulsion | Surgical | 96 | — | — | 34 | X | |||
| Bowman (2013) 20 | 10 (16) | Partial proximal hamstring avulsion | Surgical | 17 | — | — | 32 | X | |||
| Chahal (2012) 23 | 9 (16) | Complete proximal hamstring avulsion | Surgical | 13 | — | — | 24 | X | X | ||
| Hofmann (2014) 42 | 9 (16) | Complete proximal hamstring avulsion | Nonoperative | 17 | — | — | 31 | X | X | ||
| Klingele (2002) 47 | 10 (16) | Complete proximal hamstring avulsion | Surgical | 11 | 180 (range, 90-300) | — | 34 | X | |||
| Konan (2010) 48 | 12 (16) | Complete proximal hamstring avulsion | Surgical | 10 | 175 (range, 126-455) | — | 12 | X | X | ||
| Lefevre (2013) 51 | 18 (24) | Partial/complete proximal hamstring avulsion | Surgical | 34 | 171 ± 48 | — | 27 | X | X | X | |
| Léger-St-Jean (2019) 52 | 12 (16) | Complete proximal hamstring avulsion | Surgical | 22 | 120 (IQR, 60-240) | — | 6 | X | |||
| Lempainen (2006) 54 | 10 (16) | Partial proximal hamstring avulsion | Surgical | 48 | 150 (range, 30-360) | — | 36 | ||||
| Piposar (2017) 62 | 18 (24) | Partial/complete proximal hamstring avulsion | (1) Surgical (2) Nonoperative |
15 10 |
— | — | 30 35 |
X | X | ||
| Sandmann (2016) 68 | 11 (16) | Complete proximal hamstring avulsion | Surgical | 16 | 180 (range, 120-270) | — | 56 | X | X | X | |
| Shambaugh (2017) 72 | 17 (24) | Complete proximal hamstring avulsion | (1) Surgical (2) Nonoperative |
14 11 |
— | — | 43 30 |
X | X | ||
| Skaara (2013) 77 | 9 (16) | Partial proximal hamstring avulsion | Surgical | 31 | — | — | 30 | X | X | X | |
| Subbu (2014) 81 | 12 (16) | Complete proximal hamstring avulsion | Surgical | 78 | 112 (range, 84-224) | 0.0 | 24 | ||||
| Willinger (2020) 87 | 11 (16) | Partial/complete proximal hamstring avulsion | Surgical | 71 | — | — | 56 | X | |||
a Dashes indicate data not reported. H:Q, hamstrings-to-quadriceps ratio; IQR, interquartile range; MTJ, myotendinous junction; ROM, range of motion; RTP, return to play; X, outcome(s) reported.
b Reported as Methodological Index for Non-Randomized Studies score (maximum score).
TABLE 4.
Summary of Studies Managing Acute Injuries to Hamstring Muscle With Physiotherapy a
| Additional Outcomes | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Lead Author (Year) | Risk of Bias b | Injury Type | Intervention(s) | N | Mean ± SD Time to RTP, d | Reinjury Rate, % | Mean Follow-up, d | Hamstring Strength | Hamstring ROM | H:Q Ratio | Functional Assessment |
| Albertin (2020) 3 | 10 (16) | Grade 2 | Primal Reflex Release Technique | 6 | — | — | — | X | X | ||
| Askling (2013) 10 | Some concerns | Sprinting or stretching | (1) L-protocol (2) C-protocol |
37 38 |
28 ± 15
c
51 ± 21 c |
0.0 2.6 |
12 | ||||
| Askling (2014) 9 | Some concerns | Sprinting or stretching | (1) L-protocol (2) C-protocol |
28 28 |
49 ± 26
c
86 ± 34 c |
0.0 7.1 |
12 | ||||
| Bayer (2018) 14 | Low | Munich type 3-4 | (1) Early rehab (2) Delayed rehab |
20 22 |
62.5 (IQR, 48.8-77.8)
d
83.0 (IQR, 64.5-97.3) d |
9.1 0.0 |
12 | X | X | ||
| Hickey (2020) 41 | Low | Grade 1-2 | (1) Pain-threshold rehab (2) Pain-free rehab |
21 22 |
17 (95% CI, 11-24) 15 (95% CI, 13-17) |
9.5 9.1 |
6 | X | |||
| Kilcoyne (2011) 45 | 10 (16) | Grade 1-2 | Early, progressive rehab | 48 | 11.9 (range, 5-23) | 6.3 | 6 | ||||
| Kim (2018) 46 | Some concerns | Grade 2 | Stretching and ROM-based rehab | 13 | — | — | 2 | X | X | ||
| Kornberg (1989) 49 | Some concerns | Grade 1 | (1) Slump stretching (2) Standard rehab |
12 16 |
1 absent >1 game
c
16 absent >1 game c |
— | — | ||||
| Malliaropoulos (2004) 56 | Low | Grade 2 | (1) 1× daily stretching (2) 4× daily stretching |
40 40 |
15.1 ± 0.8
c
13.3 ± 0.7 c |
— | — | X | |||
| Medeiros (2020) 57 | Low | Grade 1-2 | (1) LLLT protocol (2) Standard rehab |
11 11 |
23.1 ± 9.1 23.8 ± 12.6 |
0.0 0.0 |
6 | X | X | ||
| Mendiguchia (2017) 58 | Low | Grade 1 | (1) Rehab algorithm (2) Rehab protocol |
24 24 |
25.5 ± 7.8 23.2 ± 11.7 |
4.2
d
25.0 d |
6 | ||||
| Sefiddhashti (2018) 70 | Some concerns | Grade 1-2 | (1) Cryotherapy with stretching (2) Cryotherapy alone |
18 19 |
— | — | 0.25 | X | X | ||
| Sherry (2004) 73 | Low | Grade 1-2 | (1) STST protocol (2) PATS protocol |
11 13 |
37.4 ± 27.6 22.2 ± 8.3 |
70.0
c
7.7 c |
12 | ||||
| Silder (2013) 76 | Low | Grade 1-2 | (1) PATS protocol (2) PRES protocol |
13 12 |
28.8 ± 11.4 25.2 ± 6.3 |
16.7 23.1 |
12 | X | |||
| Tyler (2017) 82 | 11 (16) | Grade 1-3 | Eccentric strength protocol | 50 | 77 ± 70 | 8.0 | 24 | X | |||
a Dashes indicate data not reported. C-protocol, conventional protocol; H:Q, hamstrings-to-quadriceps ratio; IQR, interquartile range; L-protocol, lengthening protocol; LLLT, low-level laser therapy; PATS, progressive agility and trunk stabilization; PRES, progressive running and eccentric strengthening; rehab, rehabilitation; ROM, range of motion; RTP, return to play; STST, stretching and strengthening; X, outcome(s) reported.
b Reported as Methodological Index for Non-Randomized Studies score (maximum score) for nonrandomized studies or Cochrane Risk-of-Bias Tool for Randomized Trials.
c Significant difference between interventions (P < .001).
d Significant difference between interventions (P < .05).
Proximal Injuries
To determine optimal treatment for acute proximal hamstring injuries, 22 studies investigated the efficacy of surgical and nonsurgical intervention ‡‡ (Table 2). When supplemented with postoperative rehabilitation, surgical repair for partial avulsion was associated with a high rate of RTP 13,51,87 and low levels of pain and functional limitation. 4,20,54,77 Piposar et al 62 found no differences in objective outcomes between operative and nonoperative management, although subjective results were superior after surgery. Satisfactory operative results were also observed in the context of complete avulsion, regardless of tendon retraction 19,48,52,81 or ischial tuberosity fracture. 17 Mean hamstring strength recovered to 78.0% to 94.6% within 12 months of surgery, and the rate of RTP surpassed 75%, 11,18,47,81 although up to 45% of patients reported decreased level of activity. 23,87 Two studies measuring hamstring ROM demonstrated >90% recovery within 12 months of surgical repair. 11,12 Functional outcomes did not differ by sex in any study except that by Chahal et al, 23 in which all 4 patients experiencing poor outcomes were female. Comparatively, nonoperative management of complete proximal avulsion resulted in noticeable strength deficits and lower functional scores. 42
Muscular Injuries
Management of acute muscular hamstring injury was the focus of 28 studies. Eleven studies evaluated the efficacy of autologous PRP d or autologous conditioned serum 88 injection using various injection volumes, locations, and frequencies (Table 3). Although 3 studies found patients receiving PRP achieved earlier RTP than controls by 10 to 15 days, 1,16,33 5 studies showed no such effect. 21,37,39,65,66 Despite finding no relationships between PRP injection and days or practices missed because of hamstring injury in National Football League athletes, Bradley et al 21 reported PRP injection to be associated with fewer games missed. Zanon et al 89 noted a decreased reinjury rate in patients receiving PRP in the short term; however, the long-term rate was not different from that of controls. None observed strength differences associated with PRP injection 1,39,66 except Gaballah et al, 33 who demonstrated a transient increase in strength 4 weeks after injection relative to controls that dissipated by week 8. Only Reurink et al 66 measured hamstring ROM and elucidated no effect of PRP injection on straight-leg raise or active knee extension ROM. None of the included studies concerning PRP or autologous conditioned serum injection reported the H:Q ratio or standardized functional assessment.
TABLE 3.
Summary of Studies Managing Acute Muscular Hamstring Injury Using PRP or Autologous Conditioned Serum a
| Additional Outcomes | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Lead Author (Year) | Risk of Bias b | Injury Type | Intervention | N | Mean ± SD Time to RTP, d | Reinjury Rate, % | Mean Follow-up, mo | Hamstring Strength | Hamstring ROM |
| A Hamid (2014) 1 | Low | Grade 1 | (1) PRP (1 × 3-mL direct injection 5 d postinjury (2) No injection |
14 14 |
26.7 ± 7.0
c
42.5 ± 20.6 c |
— | — | X | |
| Bezuglov (2019) 16 | Low | BAMIC 2a/2b | (1) PRP (1 × 8-mL direct injection <48 h postinjury) (2) Saline (1 × 8-mL direct injection <48 h postinjury) |
20 20 |
11.4 ± 1.2
c
21.3 ± 2.7 c |
0.0 0.0 |
6 | ||
| Bradley (2020) 21 | 18 (24) | Cohen grade 2 | (1) PRP (1-3 × 2- to 5-mL direct injections 1 wk apart) (2) No injection |
30 39 |
22.5 ± 20.1 25.7 ± 20.6 |
3.3 2.6 |
— | ||
| Gaballah (2018) 33 | Low | Grade 2 | (1) PRP (1 × 3-mL direct injection, 5-7 d postinjury) (2) No injection |
8 9 |
Maximum, 27
c
Maximum, 43 c |
— | — | X | |
| Guillodo (2015) 37 | 19 (24) | Grade 3 | (1) PRP (1 × 3-mL direct injection <8 d postinjury) (2) No injection |
15 19 |
50.9 ± 10.7 52.8 ± 15.7 |
— | — | ||
| Hamilton (2015) 39 | Low | Grade 1-2 | (1) PRP (3 × 1-mL injections 1 cm apart, <5 d postinjury) (2) PPP (3 × 1-mL injections 1 cm apart, <5 d postinjury) (3) No injection |
30 30 30 |
21 (95% CI, 18-24)
c
27 (95% CI, 21-33) c 25 (95% CI, 22-29) |
7.7 10.7 10.3 |
6 | X | |
| Lee (2020) 50 | 12 (16) | Grade 1-3 | PRP (single injection) | 8 | 49 (range, 10-112) | — | — | ||
| Rettig (2013) 65 | 18 (24) | Grade 1-2 | (1) PRP (1 × 9-mL direct injection <48 h postinjury) (2) No injection |
5 5 |
20 (range, 16-30) 17 (range, 8-81) |
— | — | ||
| Reurink (2015) 66 | Low | Grade 1-2 | (1) PRP (3 × 1-mL injections 1 cm apart at 5 and 10 d postinjury) (2) Saline (3 × 1-mL injections 1 cm apart at 5 and 10 d postinjury) |
41 39 |
42 (IQR, 30-58) 42 (IQR, 37-56) |
27.0 29.7 |
12 | X | X |
| Wright-Carpenter (2004) 88 | 19 (24) | Grade 2 | (1) Autologous conditioned serum (5 × 1-mL injections over area of injury every 2nd day [mean, 5.4 injections]) (2) Actovegin/Traumeel therapy (5 × 1-mL injections over area of injury every second day [mean, 8.3 injections]) |
6 5 |
16.3 ± 3.1
c
21.8 ± 4.8 c |
— | — | ||
| Zanon (2016) 89 | 12 (16) | Grade 2 | PRP (2-3 × 3-mL injections at 72 h and 7 d postinjury) | 25 | 35.1 ± 18.9 | 12.0 | 37 | ||
a Dashes indicate data not reported. BAMIC, British Athletics Muscle Injury Classification; IQR, interquartile range; PPP, platelet-poor plasma; PRP, platelet-rich plasma; ROM, range of motion; RTP, return to play; X, outcome(s) reported.
b Reported as Methodological Index for Non-Randomized Studies score (maximum score) for nonrandomized studies or Cochrane Risk-of-Bias Tool for Randomized Trials.
c Significant difference between interventions (P < .05).
Physiotherapeutic programs for acute hamstring muscular injuries were assessed in 15 studies e (Table 4). Eccentric training enabled faster RTP for elite soccer 10 and track and field 9 athletes compared with conventional training regardless of whether the injury was of sprinting or stretching type. Reinjury rate did not differ between eccentric and conventional rehabilitation protocols. 9,10 However, athletes fully compliant with an eccentric training program experienced fewer reinjuries and reduced strength deficits compared with noncompliant patients. 82 Reinjury risk was further reduced via an individualized rehabilitation algorithm designed to address risk factors, although this approach resulted in possibly slower RTP. 58
Kim et al 46 found stretching and ROM exercises were effective in restoring passive ROM and reducing pain in athletes with grade 2 injury, but active ROM and strength were not improved. 46 Active ROM was increased by increasing the frequency of stretching from 1 to 4 daily sessions, however, as patients were quicker to normalize flexibility between injured and uninjured limbs and RTP. 56 Stretching after icing (“cryostretching”) yielded greater increases in active knee extension and lower extremity functional scale scores compared with icing alone. 70 A stretching and strengthening (STST) intervention was compared with progressive agility and trunk stabilization (PATS) by Sherry and Best, 73 who reported similar time to RTP between groups but a significantly greater reinjury rate in the 12 months after STST. Silder et al 76 compared a progressive running and eccentric strengthening program with PATS and found no benefit in RTP, reinjury risk, strength, or ROM. Notably, all 25 athletes in this study displayed residual injury markers on MRI scans at RTP, and half of those who experienced reinjury did so within 2 weeks.
Two studies demonstrated the benefit of early intervention. 45,14 After 24 hours of immobilization, a progressive rehabilitation program developed by Kilcoyne et al 45 returned patients with grade 1 to 2 injury to activity in an average of <2 weeks with a 6-month reinjury rate of 6.3%. Athletes who began physiotherapy 2 days after grade 3 to 4 injury achieved faster RTP than athletes beginning at 9 days, with no difference in reinjury rate within 1 year. 14 Peak hamstring strength was increased in the early group 13 weeks after injury, but this difference disappeared by 26 weeks. Both early and late groups exhibited decreased H:Q ratios compared with the uninjured leg. Hickey et al 41 determined that pain threshold—based rehabilitation failed to accelerate RTP or influence reinjury rate relative to pain-free therapy. However, isometric hamstring strength was 15% greater after 2 months of training in the pain-threshold group. The Primal Reflex Release Technique, a method of downregulating the autonomic nervous system to reset reflexes via reciprocal inhibition, was shown to significantly increase active and passive ROM as well as functional scores. 3 A neurologically based approach was also examined by Kornberg and Lew, 49 who reported that slump stretching resulted in fewer games missed after grade 2 injury in Australian Rules football players. Last, an RCT by Medeiros et al 57 investigating low-level laser therapy revealed no effect in any reported outcome measure.
Surgical intervention for muscular injury was examined in 2 studies. Lempainen et al 53 (MINORS score, 10/16) assessed outcomes of surgical repair for muscular injury with concomitant complete rupture of the central hamstring tendon, reporting RTP within 4 months and no reinjuries by 1 year for the 2 patients with nonrecurrent injury included in the study. In addition, Cooper and Conway 26 (MINORS score, 18/24) compared surgical and nonoperative treatments for complete distal semitendinosus rupture and found no difference in time to RTP. However, 42% of patients treated nonoperatively did not achieve acceptable results and required subsequent surgical intervention.
Prognostic Factors
Characteristics and findings of studies correlating baseline clinical and/or MRI findings with time to RTP are summarized in Tables 5 and 6.
TABLE 5.
Summary of Studies Assessing Prognostic Value of Baseline Assessment a
| Assessment | ||||
|---|---|---|---|---|
| Lead Author (Year) | Risk of Bias b | N | Clinical | MRI |
| A Hamid (2014) 1 | Low | 28 | X | |
| A Hamid (2013) 2 | 10 (16) | 360 | X | |
| Askling (2006) 5 | 12 (16) | 33 | X | |
| Askling (2007) 6 | 14 (16) | 15 | X | X |
| Askling (2007) 7 | 14 (16) | 18 | X | X |
| Askling (2008) 8 | 11 (16) | 30 | X | X |
| Askling (2014) 9 | Some concerns | 56 | X | X |
| Askling (2013) 10 | Some concerns | 75 | X | X |
| Cohen (2011) 24 | 14 (16) | 38 | X | |
| Comin (2013) 25 | 20 (24) | 62 | X | |
| Crema (2018) 27 | 11 (16) | 22 | X | |
| Ekstrand (2012) 29 | 12 (16) | 207 | X | |
| Ekstrand (2016) 30 | 12 (16) | 255 | X | |
| Gibbs (2004) 33 | 12 (16) | 31 | X | |
| Guillodo (2014) 36 | 12 (16) | 128 | X | |
| Hallen (2014) 37 | 13 (16) | 386 | X | |
| Hamilton (2018) 40 | 13 (16) | 110 | X | |
| Jacobsen (2016) 44 | 14 (16) | 90 | X | X |
| Kilcoyne (2011) 45 | 10 (16) | 48 | X | |
| Malliaropoulos (2010) 55 | 21 (24) | 165 | X | |
| Moen (2014) 59 | 13 (16) | 74 | X | X |
| Pollock (2016) 63 | 11 (16) | 44 | X | |
| Pomeranz (1993) 64 | 10 (16) | 14 | X | |
| Schneider-Kolsky (2006) 69 | 21 (24) | 58 | X | X |
| Silder (2013) 76 | Low | 25 | X | |
| Slavotinek (2002) 75 | 12 (16) | 30 | X | |
| van der Made (2018) 80 | 14 (16) | 70 | X | |
| Verrall (2003) 81 | 12 (16) | 83 | X | X |
| Wangensteen (2015) 82 | 11 (16) | 180 | X | X |
| Warren (2010) 83 | 13 (16) | 59 | X | |
a MRI, magnetic resonance imaging; X, outcome(s) reported.
b Reported as Methodological Index for Non-Randomized Studies score (maximum score) for nonrandomized studies or Cochrane Risk-of-Bias Tool for Randomized Trials.
TABLE 6.
Baseline Assessment Findings and Prognostic Relationships With RTP Times a
| Clinical Factors | MRI Factors |
|---|---|
| RTP Prognosis: Accelerated | |
| Pain during outer-range strength test 42 | BAMIC grade 0 61 |
| Midrange strength as % of uninjured leg 42 | Shorter radiologist-predicted time to RTP 66 |
| SLR flexibility of uninjured leg 42 | Shorter length of lesion 66 |
| Greater physiotherapy attendance 42 | Smaller injury CSA 66 |
| Shorter clinician-predicted time to RTP 66 | MRI-negative injury 9,10,33,37,62 |
| Lower grade of injury 66 | Single muscle/tendon involvement 23 |
| Sprinting-type vs stretching-type injury 10 | Lower % of muscle/tendon involvement 23 |
| Lower radiologic grade of injury 23,29 | |
| Lower Cohen MRI score 23 | |
| Injuries not involving proximal tendon 9 | |
| RTP Prognosis: No Effect | |
| Sex 43 | Craniocaudal length of injury 6,7,8,26,42,57 |
| Dominant vs nondominant limb 2,42,43 | Mediolateral width of injury 6,7,42 |
| Sudden vs gradual pain onset 42 | Depth of injury 7,30 |
| Injury during game vs training 42 | Volume of edema 7,26,57 |
| Forced to cease activity within 5 min 42 | Tendon involvement 30,42 |
| Ability to walk/jog pain-free 42 | Myofascial involvement 30,42 |
| No. of days to walk pain-free 42,57 | Muscle (most) involved 24,29,30,37,42,57,61,75,82 |
| No. of days to ascend stairs pain-free 83 | Injury CSA as % of total muscle CSA 26,42,57 |
| Mechanism of injury 2,42,57,82,83 | Distance of injury from ischium 7,8,42,57,82 |
| History of low back pain 42,82 | Intra- or intermuscular hemorrhage 66 |
| History of lower limb injury 42 | Site of injury within the muscle 23,30,61,75 |
| History of lower limb surgery 42 | Grade 1 vs grade 2 injury 29,61 |
| Pain on 1- or 2-leg squat 42 | MRI grade of injury 57 |
| Pain on palpation of injured area 35,42 | Presence of extramuscular fluid 57 |
| Craniocaudal length of palpated pain 1,6,7,42,57 | Partial disruption of the central tendon 80 |
| Mediolateral width of palpated pain 42 | Amount of central tendon retraction 80 |
| Distance of palpated pain from ischium 35,42,57 | BAMIC type a vs b 61 |
| Location of point of highest palpated pain 7,8 | |
| Site of injury within the muscle 43,55,81,83 | |
| No. of muscles injured 2 | |
| Positive vs negative slump test 82,83 | |
| Frequency of physiotherapy 2 | |
| Grade of injury 2,43 | |
| Level of play/intensity of sport 2,57 | |
| Delay in seeking physiotherapy 1 | |
| Active knee extension deficit 1,57,83 | |
| Pain upon active knee extension 57 | |
| Pain upon PKE 35 | |
| Pain on passive SLR 57 | |
| Pain upon isometric contraction 35,83 | |
| Previous ACL graft harvesting 57 | |
| Isometric knee flexion strength 5,57 | |
| Hip ROM 5,83 | |
| Use of NSAIDs within 72 h of injury 83 | |
| RTP Prognosis: Delayed | |
| Female sex 2 | Volume of injury 6,42,75 |
| Greater PKE range of uninjured leg 42 | Greater craniocaudal length of injury 9,10,23,30,66,73 |
| Greater peak torque angle in knee extension 42 | Greater width of edema 30 |
| Higher grade of injury 66 | Greater length of lesion as % of height 33 |
| Injury to biceps femoris 66 | Greater depth of injury 6 |
| Shorter distance of pain to ischium 7,9,10 | Longer radiologist-predicted time to RTP 66 |
| Stretching-type vs sprinting-type injury 5,10 | Larger injury CSA 6,33,62,66,75 |
| Greater maximum pain at time of injury 42,82 | Involvement of proximal tendon 6,10 |
| Worst VAS pain score >6 35 | Proximal vs distal injuries 6 |
| Higher VAS pain score at initial examination 81 | Shorter distance of injury to ischium 6,9,10 |
| “Popping” sound at time of injury 35 | Higher Cohen MRI score 23 /score >10 39 |
| Bruising 35 | MRI-positive injury 81 |
| Greater deficit in passive SLR 57 | Greater % of muscle/tendon involvement 23 |
| Longer clinician-predicted time to RTP 66,81 | Complete tendinous/myotendinous rupture 62 |
| Forced to cease activity within 5 min 82 | Complete central tendon disruption 24,80 |
| Greater length of palpated pain 82 | Presence of central tendon waviness 80 |
| Pain on resisted knee flexion 82 | Greater central tendon retraction 23 |
| >1 wk to initial consultation 2 | Higher radiologic grade of injury 23,29,30,37,61,82 |
| Recurrent muscle injury 2 | Greater No. of muscles involved 39 |
| Greater active knee ROM deficit 35,53 | Distal tendinous or myotendinous injury 62 |
| Longer self-predicted time to RTP 57 | Peritendinous fluid collection 62 |
| Lower level of sport 8 | |
| >1 d to walk pain-free 83 | |
a ACL, anterior cruciate ligament; BAMIC, British Athletics Muscle Injury Classification; CSA, cross-sectional area; MRI, magnetic resonance imaging; NSAID, nonsteroidal anti-inflammatory drug; PKE, passive knee extension; ROM, range of motion; RTP, return to play; SLR, straight-leg raise; VAS, visual analog scale.
Clinical Factors
Seventeen studies investigated relationships between clinical assessment findings and time to RTP f . Pain during outer-range strength testing, 44 greater midrange strength as a percentage of uninjured leg strength, 44 and shorter clinician-predicted recovery 69 were associated with accelerated RTP. In contrast, factors associated with delayed RTP included greater passive knee extension of the uninjured leg, 44 greater peak torque angle in knee extension, 44 injury to the biceps femoris, 69 greater maximum pain at injury, 44,85 worst visual analog scale (VAS) pain score >6, 36 higher VAS pain score at initial examination, 84 popping sound at injury, 36 bruising, 36 pain on resisted knee flexion, 85 and longer clinician- 69,84 and self-predicted time to RTP. 59 Several examined factors had contradictory results across studies. Two studies by Askling et al 5,10 noted stretching-type injuries took longer to recover than did sprinting-type ones, while others found injury mechanism to have no effect on recovery time. 2,44,59,85,86 There was no consensus regarding the effect on time to RTP for sex, 2,45 injury grade, 2,45,69 physiotherapy attendance, 1,2,44 hip ROM, 5,44,59,86 number of days to walk pain-free, 44,59,86 history of ipsilateral or contralateral lower limb injury, 1,2,44,45,59,85,86 craniocaudal length of pain, 1,6,7,44,59,85 need to cease activity within 5 minutes of injury, 44,85 level of play, 2,8,59 or active knee extension deficit. 1,36,55,59,86
MRI Factors
Twenty-three studies evaluated the role of MRI in predicting time to RTP. g Accelerated RTP was associated with MRI-negative injury, 9,10,34,38,64 lower percentage of muscle/tendon involvement, 24 and shorter radiologist-predicted recovery. 69 Conversely, the following were associated with prolonged recovery time: MRI-positive injury, 84 greater normalized length of lesion, 34 greater percentage of muscle/tendon involvement, 24 complete tendinous/myotendinous rupture, 63,64 complete central tendon disruption, 25,83 central tendon waviness, 83 greater number of muscles involved, 40 and longer radiologist-predicted recovery. 69 Studies reported conflicting results for injury grade, 24,29,30,38,59,63,85 length, h width, 6,7,30,44 depth, 6,7,30 cross-sectional area, 6,27,34,44,59,64,69,78 volume, 6,7,27,44,59,78 tendon involvement, 6,9,10,24,30,44 amount of tendon retraction, 24,83 site of injury within the muscle, 6,24,30,63,64,78 presence of extramuscular fluid, 59,64 distance from ischium, 6 –10,44,59,85 and the Cohen MRI score. 24,40 Of note, the Cohen MRI score refers to an assessment tool designed to evaluate hamstring injuries on the basis of patient age, muscles involved, injury location, extent of injury, and retraction. 24
Discussion
This review assessed management of acute proximal and muscular hamstring injuries by reviewing interventions and prognostic factors associated with RTP. According to the literature, patients undergoing surgical treatment for partial or complete proximal hamstring ruptures achieved consistently better outcomes compared with those managed nonoperatively. 11,12,15,19,68 For patients with acute muscular injuries, physiotherapy incorporating eccentric training 9,10,82 and PATS 73,76 attained favorable outcomes in time to RTP, reinjury rate, and restoration of strength. Stretching-based protocols increased ROM but failed to reduce reinjury risk or improve strength. 46,56,73 Supported by findings that rehabilitation with pain-threshold limits does not predispose to adverse effects, 41 early initiation of rehabilitation enabled faster RTP. 14,45 Slump stretching 49 and reflexive release techniques 3 also offered functional benefit by addressing neurological components of hamstring strain. Regarding the efficacy of PRP injection, results were inconclusive, confounded by a lack of standardization in PRP formulation and injection protocol. Similar inconsistencies have been reported in recent meta-analyses, 35,61,71,75 emphasizing the need to determine the optimal injection protocol for standard use in future research investigating the effect of PRP on time to RTP. Overall, although the quality of evidence of included studies varied, the diverse methods and predictive factors examined warrant consideration by clinicians seeking to optimize injury recovery.
Studies quantifying the prognostic value of baseline assessments have indicated that certain clinical and MRI findings are correlated with time to RTP. Clinical factors associated with accelerated RTP included lesser deficit in strength of the injured leg relative to the uninjured leg 44 and shorter physician-predicted recovery time, 69 whereas prolonged time to RTP was observed in patients with greater pain, 36,44,84,85 injury to the biceps femoris, 69 and longer physician- 69,84 and self-predicted 59 recovery times. It is possible that patients with greater strength and decreased pain in the injured leg at baseline may be able to begin physiotherapeutic activity and facilitate rehabilitation sooner after injury, resulting in earlier RTP. On MRI scans, findings indicating greater injury severity at initial presentation, such as greater lesion size, 24,34,84 tendinous/myotendinous rupture, 25,63,64,83 and greater number of muscles affected, 40 were correlated with prolonged RTP. Despite associations of initial examination and MRI findings with time to RTP, accurate prognostication of recovery time remains difficult. In a multivariate analysis of 180 patients, Wangensteen et al 85 determined that a single clinical examination at initial presentation accounted for 29% of variance in time to RTP, whereas supplementation with MRI findings explained only an additional 2.8%. Jacobsen et al 44 likewise reported that 59.0% and 8.6% of variance in RTP was accounted for by clinical and MRI examination, respectively, suggesting the added benefit of MRI findings in prognosticating RTP is less pronounced.
This study has several important limitations. First, the strength of any systematic review is dependent upon the quality of evidence of included studies. This review included 17 RCTs, of which 5 were determined as raising “some concerns” on risk-of-bias assessment. The remaining 58 studies consisted of cohort, case-control, and case series study designs included in an effort to be comprehensive in evaluating rehabilitative techniques. When critically appraised, comparative nonrandomized studies achieved a mean MINORS score of 18.8 ± 1.3, and noncomparative nonrandomized studies achieved a score of 11.4 ± 3.4. These scores indicate a reasonable risk of bias and are mainly attributable to a lack of prospective data collection, blinding, and/or prospective calculation of sample size. Differences in study design, patient population, and outcome measures limited direct comparisons between studies and precluded data pooling for meta-analyses, making it difficult to draw concrete conclusions in circumstances of conflicting results. This was particularly apparent when analyzing the efficacy of PRP injection for treatment of hamstring muscular injury, as studies varied in terms of volume, location, and number of injections. With regard to studies examining the prognostic value of clinical and MRI examination, the majority conducted only univariate analyses correlating baseline findings with RTP. Furthermore, criteria for RTP and methods of functional assessment were inconsistent, likely explaining some of the variance in time to RTP across studies. Future large-scale research using standardized RTP criteria and outcome measures are required to determine reliable associations between baseline findings and RTP prognosis via multivariate analysis.
Conclusion
Surgical intervention offers substantial benefits over nonoperative care for treatment of acute partial and complete proximal hamstring ruptures, while muscular injuries are effectively treated with physiotherapy encompassing eccentric training and PATS. The efficacy of PRP, however, remains controversial. Prognostication of RTP is of great importance, and the ability to accurately predict recovery time can be improved with a thorough clinical examination shortly after injury. Although the added benefit may be limited, structural factors observed on MRI scans can also inform RTP prognosis. Future high-quality research evaluating novel therapeutic protocols and prognostic determinants of RTP is needed to further enhance rehabilitation and better predict recovery timelines for athletes with acute hamstring injury.
APPENDIX
TABLE A1.
Search Strategy
| MEDLINE (Ovid) |
|
| CINAHL (EBSCO) |
|
| Cochrane Central Register for Controlled Trials (EBSCO) |
|
| SPORTDiscus (EBSCO) |
|
References 3, 4, 11 –21, 23, 26, 33, 37, 39, 41, 42, 46 –54, 56 –58, 62, 65, 66, 68, 70, 72, 73, 77, 81, 82, 87 –89.
References 1, 3, 9, 10, 14, 16, 21, 26, 33, 37, 39, 41, 45, 46, 49, 50, 53, 56 –58, 65, 66, 70, 73, 76, 82, 88, 89.
Footnotes
Final revision submitted July 5, 2021; accepted August 10, 2021.
One or more of the authors has declared the following potential conflict of interest or source of funding: Funding was provided by the Conine Family Fund for Joint Preservation. S.D.M. has received education payments from Kairos Surgical and honoraria from Allergan. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
References
- 1. A Hamid MS, Mohamed Ali MR, Yusof A, George J, Lee LPC. Platelet-rich plasma injections for the treatment of hamstring injuries: a randomized controlled trial. Am J Sports Med. 2014;42(10):2410–2418. [DOI] [PubMed] [Google Scholar]
- 2. A Hamid MS, Yusof A, Mohamed Ali MR. Pattern of muscle injuries and predictors of return-to-play duration among Malaysian athletes. Singapore Med J. 2013;54(10):587–591. [DOI] [PubMed] [Google Scholar]
- 3. Albertin ES, Walters M, May J, Baker RT, Nasypany A, Cheatham S. An exploratory case series analysis of the use of Primal Reflex Release Technique™ to improve signs and symptoms of hamstring strain. Int J Sports Phys Ther. 2020;15(2):263–273. [PMC free article] [PubMed] [Google Scholar]
- 4. Arner JW, Freiman H, Mauro CS, Bradley JP. Functional results and outcomes after repair of partial proximal hamstring avulsions at midterm follow-up. Am J Sports Med. 2019;47(14):3436–3443. [DOI] [PubMed] [Google Scholar]
- 5. Askling C, Saartok T, Thorstensson A. Type of acute hamstring strain affects flexibility, strength, and time to return to pre-injury level. Br J Sports Med. 2006;40(1):40–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Askling CM, Tengvar M, Saartok T, Thorstensson A. Acute first-time hamstring strains during high-speed running: a longitudinal study including clinical and magnetic resonance imaging findings. Am J Sports Med. 2007;35(2):197–206. [DOI] [PubMed] [Google Scholar]
- 7. Askling CM, Tengvar M, Saartok T, Thorstensson A. Acute first-time hamstring strains during slow-speed stretching: clinical, magnetic resonance imaging, and recovery characteristics. Am J Sports Med. 2007;35(10):1716–1724. [DOI] [PubMed] [Google Scholar]
- 8. Askling CM, Tengvar M, Saartok T, Thorstensson A. Proximal hamstring strains of stretching type in different sports. Am J Sports Med. 2008;36(9):1799–1804. [DOI] [PubMed] [Google Scholar]
- 9. Askling CM, Tengvar M, Tarassova O, Thorstensson A. Acute hamstring injuries in Swedish elite sprinters and jumpers: a prospective randomised controlled clinical trial comparing two rehabilitation protocols. Br J Sports Med. 2014;48(7):532–539. [DOI] [PubMed] [Google Scholar]
- 10. Askling CM, Tengvar M, Thorstensson A. Acute hamstring injuries in Swedish elite football: a prospective randomised controlled clinical trial comparing two rehabilitation protocols. Br J Sports Med. 2013;47(15):953–959. [DOI] [PubMed] [Google Scholar]
- 11. Ayuob A, Kayani B, Haddad FS. Acute surgical repair of complete, nonavulsion proximal semimembranosus injuries in professional athletes. Am J Sports Med. 2020;48(9):2170–2177. [DOI] [PubMed] [Google Scholar]
- 12. Ayuob A, Kayani B, Haddad FS. Musculotendinous junction injuries of the proximal biceps femoris: a prospective study of 64 patients treated surgically. Am J Sports Med. 2020;48(8):1974–1982. [DOI] [PubMed] [Google Scholar]
- 13. Barnett AJ, Negus JJ, Barton T, Wood DG. Reattachment of the proximal hamstring origin: outcome in patients with partial and complete tears. Knee Surg Sports Traumatol Arthrosc. 2015;23(7):2130–2135. [DOI] [PubMed] [Google Scholar]
- 14. Bayer ML, Hoegberget-Kalisz M, Jensen MH, et al. Role of tissue perfusion, muscle strength recovery, and pain in rehabilitation after acute muscle strain injury: a randomized controlled trial comparing early and delayed rehabilitation. Scand J Med Sci Sports. 2018;28(12):2579–2591. [DOI] [PubMed] [Google Scholar]
- 15. Best R, Eberle J, Beck F, Beckmann J, Becker U. Functional impairment after successful surgical reconstruction for proximal hamstring avulsion. Int Orthop. 2019;43(10):2341–2347. [DOI] [PubMed] [Google Scholar]
- 16. Bezuglov E, Maffulli N, Tokareva A, Achkasov E. Platelet-rich plasma in hamstring muscle injuries in professional soccer players: a pilot study. Muscles Ligaments Tendons J. 2019;9(1):112–118. [Google Scholar]
- 17. Biedert RM. Surgical management of traumatic avulsion of the ischial tuberosity in young athletes. Clin J Sport Med. 2015;25(1):67–72. [DOI] [PubMed] [Google Scholar]
- 18. Birmingham P, Muller M, Wickiewicz T, Cavanaugh J, Rodeo S, Warren R. Functional outcome after repair of proximal hamstring avulsions. J Bone Joint Surg Am. 2011;93(19):1819–1826. [DOI] [PubMed] [Google Scholar]
- 19. Blakeney WG, Zilko SR, Edmonston SJ, Schupp NE, Annear PT. A prospective evaluation of proximal hamstring tendon avulsions: improved functional outcomes following surgical repair. Knee Surg Sports Traumatol Arthrosc. 2017;25(6):1943–1950. [DOI] [PubMed] [Google Scholar]
- 20. Bowman KF, Cohen SB, Bradley JP. Operative management of partial-thickness tears of the proximal hamstring muscles in athletes. Am J Sports Med. 2013;41(6):1363–1371. [DOI] [PubMed] [Google Scholar]
- 21. Bradley JP, Lawyer TJ, Ruef S, Towers JD, Arner JW. Platelet-rich plasma shortens return to play in National Football League players with acute hamstring injuries. Orthop J Sports Med. 2020;8(4):2325967120911731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Carlson C. The natural history and management of hamstring injuries. Curr Rev Musculoskelet Med. 2008;1(2):120–123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Chahal J, Bush-Joseph CA, Chow A, et al. Clinical and magnetic resonance imaging outcomes after surgical repair of complete proximal hamstring ruptures: does the tendon heal? Am J Sports Med. 2012;40(10):2325–2330. [DOI] [PubMed] [Google Scholar]
- 24. Cohen SB, Towers JD, Zoga A, et al. Hamstring injuries in professional football players: magnetic resonance imaging correlation with return to play. Sports Health. 2011;3(5):423–430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Comin J, Malliaras P, Baquie P, Barbour T, Connell D. Return to competitive play after hamstring injuries involving disruption of the central tendon. Am J Sports Med. 2013;41(1):111–115. [DOI] [PubMed] [Google Scholar]
- 26. Cooper DE, Conway JE. Distal semitendinosus ruptures in elite-level athletes. Am J Sports Med. 2010;38(6):1174–1178. [DOI] [PubMed] [Google Scholar]
- 27. Crema MD, Godoy IRB, Abdalla RJ, de Aquino JS, Ingham SJM, Skaf AY. Hamstring injuries in professional soccer players: extent of MRI-detected edema and the time to return to play. Sports Health. 2018;10(1):75–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Cumpston M, Li T, Page MJ, et al. Updated guidance for trusted systematic reviews: a new edition of the Cochrane Handbook for Systematic Reviews of Interventions. Cochrane Database Syst Rev. 2019;10:ED000142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Ekstrand J, Healy JC, Waldén M, Lee JC, English B, Hägglund M. Hamstring muscle injuries in professional football: the correlation of MRI findings with return to play. Br J Sports Med. 2012;46(2):112–117. [DOI] [PubMed] [Google Scholar]
- 30. Ekstrand J, Lee JC, Healy JC. MRI findings and return to play in football: a prospective analysis of 255 hamstring injuries in the UEFA Elite Club Injury Study. Br J Sports Med. 2016;50(12):738–743. [DOI] [PubMed] [Google Scholar]
- 31. Ekstrand J, Waldén M, Hägglund M. Hamstring injuries have increased by 4% annually in men’s professional football, since 2001: a 13-year longitudinal analysis of the UEFA Elite Club Injury Study. Br J Sports Med. 2016;50(12):731–737. [DOI] [PubMed] [Google Scholar]
- 32. Engebretsen AH, Myklebust G, Holme I, Engebretsen L, Bahr R. Intrinsic risk factors for hamstring injuries among male soccer players: a prospective cohort study. Am J Sports Med. 2010;38(6):1147–1153. [DOI] [PubMed] [Google Scholar]
- 33. Gaballah A, Elgeidi A, Bressel E, Shakrah N, Abd-Alghany A. Rehabilitation of hamstring strains: does a single injection of platelet-rich plasma improve outcomes? (Clinical study). Sport Sci Health. 2018;14(2):439–447. [Google Scholar]
- 34. Gibbs NJ, Cross TM, Cameron M, Houang MT. The accuracy of MRI in predicting recovery and recurrence of acute grade one hamstring muscle strains within the same season in Australian Rules football players. J Sci Med Sport. 2004;7(2):248–258. [DOI] [PubMed] [Google Scholar]
- 35. Grassi A, Napoli F, Romandini I, et al. Is platelet-rich plasma (PRP) effective in the treatment of acute muscle injuries? A systematic review and meta-analysis. Sports Med. 2018;48(4):971–989. [DOI] [PubMed] [Google Scholar]
- 36. Guillodo Y, Here-Dorignac C, Thoribé B, et al. Clinical predictors of time to return to competition following hamstring injuries. Muscles Ligaments Tendons J. 2014;4(3):386–390. [PMC free article] [PubMed] [Google Scholar]
- 37. Guillodo Y, Madouas G, Simon T, Le Dauphin H, Saraux A. Platelet-rich plasma (PRP) treatment of sports-related severe acute hamstring injuries. Muscles Ligaments Tendons J . 2015;5(4):284–288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Hallén A, Ekstrand J. Return to play following muscle injuries in professional footballers. J Sports Sci. 2014;32(13):1229–1236. [DOI] [PubMed] [Google Scholar]
- 39. Hamilton B, Tol JL, Almusa E, et al. Platelet-rich plasma does not enhance return to play in hamstring injuries: a randomised controlled trial. Br J Sports Med. 2015;49(14):943–950. [DOI] [PubMed] [Google Scholar]
- 40. Hamilton B, Wangensteen A, Whiteley R, et al. Cohen’s MRI scoring system has limited value in predicting return to play. Knee Surg Sports Traumatol Arthrosc. 2018;26(4):1288–1294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Hickey JT, Timmins RG, Maniar N, et al. Pain-free versus pain-threshold rehabilitation following acute hamstring strain injury: a randomized controlled trial. J Orthop Sports Phys Ther. 2020;50(2):91–103. [DOI] [PubMed] [Google Scholar]
- 42. Hofmann KJ, Paggi A, Connors D, Miller SL. Complete avulsion of the proximal hamstring insertion: functional outcomes after nonsurgical treatment. J Bone Joint Surg Am. 2014;96(12):1022–1025. [DOI] [PubMed] [Google Scholar]
- 43. Irger M, Willinger L, Lacheta L, Pogorzelski J, Imhoff AB, Feucht MJ. Proximal hamstring tendon avulsion injuries occur predominately in middle-aged patients with distinct gender differences: epidemiologic analysis of 263 surgically treated cases. Knee Surg Sports Traumatol Arthrosc. 2020;28(4):1221–1229. [DOI] [PubMed] [Google Scholar]
- 44. Jacobsen P, Witvrouw E, Muxart P, Tol JL, Whiteley R. A combination of initial and follow-up physiotherapist examination predicts physician-determined time to return to play after hamstring injury, with no added value of MRI. Br J Sports Med. 2016;50(7):431–439. [DOI] [PubMed] [Google Scholar]
- 45. Kilcoyne KG, Dickens JF, Keblish D, Rue J-P, Chronister R. Outcome of grade I and II hamstring injuries in intercollegiate athletes: a novel rehabilitation protocol. Sports Health. 2011;3(6):528–533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Kim G, Kim H, Kim WK, Kim J. Effect of stretching-based rehabilitation on pain, flexibility and muscle strength in dancers with hamstring injury: a single-blind, prospective, randomized clinical trial. J Sports Med Phys Fitness. 2018;58(9):1287–1295. [DOI] [PubMed] [Google Scholar]
- 47. Klingele KE, Sallay PI. Surgical repair of complete proximal hamstring tendon rupture. Am J Sports Med. 2002;30(5):742–747. [DOI] [PubMed] [Google Scholar]
- 48. Konan S, Haddad F. Successful return to high level sports following early surgical repair of complete tears of the proximal hamstring tendons. Int Orthop. 2010;34(1):119–123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Kornberg C, Lew P. The effect of stretching neural structures on grade one hamstring injuries. J Orthop Sports Phys Ther. 1989;10(12):481–487. [DOI] [PubMed] [Google Scholar]
- 50. Lee KY, Baker HP, Hanaoka CM, Tjong VK, Terry MA. Treatment of patellar and hamstring tendinopathy with platelet-rich plasma in varsity collegiate athletes: a case series. J Orthop. 2020;18:91–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Lefevre N, Bohu Y, Naouri J, Klouche S, Herman S. Returning to sports after surgical repair of acute proximal hamstring ruptures. Knee Surg Sports Traumatol Arthrosc. 2013;21(3):534–539. [DOI] [PubMed] [Google Scholar]
- 52. Léger-St-Jean B, Gorica Z, Magnussen RA, Vasileff WK, Kaeding CC. Accelerated rehabilitation results in good outcomes following acute repair of proximal hamstring ruptures. Knee Surg Sports Traumatol Arthrosc. 2019;27(10):3121–3124. [DOI] [PubMed] [Google Scholar]
- 53. Lempainen L, Kosola J, Pruna R, et al. Central tendon injuries of hamstring muscles: case series of operative treatment. Orthop J Sports Med. 2018;6(2):2325967118755992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Lempainen L, Sarimo J, Heikkila J, Mattila K, Orava S. Surgical treatment of partial tears of the proximal origin of the hamstring muscles. Br J Sports Med. 2006;40(8):688–691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Malliaropoulos N, Papacostas E, Kiritsi O, Papalada A, Gougoulias N, Maffulli N. Posterior thigh muscle injuries in elite track and field athletes. Am J Sports Med. 2010;38(9):1813–1819. [DOI] [PubMed] [Google Scholar]
- 56. Malliaropoulos N, Papalexandris S, Papalada A, Papacostas E. The role of stretching in rehabilitation of hamstring injuries: 80 athletes follow-up. Med Sci Sports Exerc. 2004;36(5):756–759. [DOI] [PubMed] [Google Scholar]
- 57. Medeiros DM, Aimi M, Vaz MA, Baroni BM. Effects of low-level laser therapy on hamstring strain injury rehabilitation: a randomized controlled trial. Phys Ther Sport. 2020;42:124–130. [DOI] [PubMed] [Google Scholar]
- 58. Mendiguchia J, Martinez-Ruiz E, Edouard P, et al. A multifactorial, criteria-based progressive algorithm for hamstring injury treatment. Med Sci Sports Exerc. 2017;49(7):1482–1492. [DOI] [PubMed] [Google Scholar]
- 59. Moen MH, Reurink G, Weir A, Tol JL, Maas M, Goudswaard GJ. Predicting return to play after hamstring injuries. Br J Sports Med. 2014;48(18):1358–1363. [DOI] [PubMed] [Google Scholar]
- 60. Moher D, Liberati A, Tetzlaff J, Altman DG; the PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Pas HI, Reurink G, Tol JL, Weir A, Winters M, Moen MH. Efficacy of rehabilitation (lengthening) exercises, platelet-rich plasma injections, and other conservative interventions in acute hamstring injuries: an updated systematic review and meta-analysis. Br J Sports Med. 2015;49(18):1197–1205. [DOI] [PubMed] [Google Scholar]
- 62. Piposar JR, Vinod AV, Olsen JR, Lacerte E, Miller SL. High-grade partial and retracted (<2 cm) proximal hamstring ruptures. Orthop J Sports Med. 2017;5(2):2325967117692507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Pollock N, Patel A, Chakraverty J, Suokas A, James SL, Chakraverty R. Time to return to full training is delayed and recurrence rate is higher in intratendinous (“c”) acute hamstring injury in elite track and field athletes: clinical application of the British Athletics Muscle Injury Classification. Br J Sports Med. 2016;50(5):305–310. [DOI] [PubMed] [Google Scholar]
- 64. Pomeranz SJ, Heidt RS., Jr MR imaging in the prognostication of hamstring injury: work in progress. Radiology. 1993;189(3):897–900. [DOI] [PubMed] [Google Scholar]
- 65. Rettig AC, Meyer S, Bhadra AK. Platelet-rich plasma in addition to rehabilitation for acute hamstring injuries in NFL players: clinical effects and time to return to play. Orthop J Sports Med. 2013;1(1):2325967113494354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Reurink G, Goudswaard GJ, Moen MH, et al. Rationale, secondary outcome scores and 1-year follow-up of a randomised trial of platelet-rich plasma injections in acute hamstring muscle injury: the Dutch Hamstring Injection Therapy study. Br J Sports Med. 2015;49(18):1206–1212. [DOI] [PubMed] [Google Scholar]
- 67. Ribeiro-Alvares JB, Marques VB, Vaz MA, Baroni BM. Four weeks of Nordic hamstring exercise reduce muscle injury risk factors in young adults. J Strength Cond Res. 2018;32(5):1254–1262. [DOI] [PubMed] [Google Scholar]
- 68. Sandmann GH, Hahn D, Amereller M, et al. Mid-term functional outcome and return to sports after proximal hamstring tendon repair. Int J Sports Med. 2016;37(7):570–576. [DOI] [PubMed] [Google Scholar]
- 69. Schneider-Kolsky ME, Hoving JL, Warren P, Connell DA. A comparison between clinical assessment and magnetic resonance imaging of acute hamstring injuries. Am J Sports Med. 2006;34(6):1008–1015. [DOI] [PubMed] [Google Scholar]
- 70. Sefiddashti L, Ghotbi N, Salavati M, Farhadi A, Mazaheri M. The effects of cryotherapy versus cryostretching on clinical and functional outcomes in athletes with acute hamstring strain. J Bodyw Mov Ther. 2018;22(3):805–809. [DOI] [PubMed] [Google Scholar]
- 71. Seow D, Shimozono Y, Tengku Yusof TNB, Yasui Y, Massey A, Kennedy JG. Platelet-rich plasma injection for the treatment of hamstring injuries: a systematic review and meta-analysis with best-worst case analysis. Am J Sports Med. 2021;49(2):529–537. [DOI] [PubMed] [Google Scholar]
- 72. Shambaugh BC, Olsen J, Kellum EL, Lacerte E, Miller SL. A comparison of nonoperative and operative treatment of complete proximal hamstring ruptures. Orthop J Sports Med. 2017;5(11):2325967117738551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Sherry MA, Best TM. A comparison of 2 rehabilitation programs in the treatment of acute hamstring strains. J Orthop Sports Phys Ther. 2004;34(3):116–125. [DOI] [PubMed] [Google Scholar]
- 74. Sherry MA, Johnston TS, Heiderscheit BC. Rehabilitation of acute hamstring strain injuries. Clin Sports Med. 2015;34(2):263–284. [DOI] [PubMed] [Google Scholar]
- 75. Sheth U, Dwyer T, Smith I, et al. Does platelet-rich plasma lead to earlier return to sport when compared with conservative treatment in acute muscle injuries? A systematic review and meta-analysis. Arthroscopy. 2018;34(1):281–288.e281. [DOI] [PubMed] [Google Scholar]
- 76. Silder A, Sherry MA, Sanfilippo J, Tuite M, Hetzel SJ, Heiderscheit BC. Clinical and morphological changes following 2 rehabilitation programs for acute hamstring strain injuries: a randomized clinical trial. J Orthop Sports Phys Ther. 2013;43(5):284–299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Skaara HE, Moksnes H, Frihagen F, Stuge B. Self-reported and performance-based functional outcomes after surgical repair of proximal hamstring avulsions. Am J Sports Med. 2013;41(11):2577–2584. [DOI] [PubMed] [Google Scholar]
- 78. Slavotinek JP, Verrall GM, Fon GT. Hamstring injury in athletes: using MR imaging measurements to compare extent of muscle injury with amount of time lost from competition. AJR Am J Roentgenol. 2002;179(6):1621–1628. [DOI] [PubMed] [Google Scholar]
- 79. Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological Index for Non-Randomized Studies (MINORS): development and validation of a new instrument. ANZ J Surg. 2003;73(9):712–716. [DOI] [PubMed] [Google Scholar]
- 80. Sterne JAC, Savovic J, Page MJ, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898. [DOI] [PubMed] [Google Scholar]
- 81. Subbu R, Benjamin-Laing H, Haddad F. Timing of surgery for complete proximal hamstring avulsion injuries: successful clinical outcomes at 6 weeks, 6 months, and after 6 months of injury. Am J Sports Med. 2015;43(2):385–391. [DOI] [PubMed] [Google Scholar]
- 82. Tyler TF, Schmitt BM, Nicholas SJ, McHugh MP. Rehabilitation after hamstring-strain injury emphasizing eccentric strengthening at long muscle lengths: results of long-term follow-up. J Sport Rehabil. 2017;26(2):131–140. [DOI] [PubMed] [Google Scholar]
- 83. van der Made AD, Almusa E, Whiteley R, et al. Intramuscular tendon involvement on MRI has limited value for predicting time to return to play following acute hamstring injury. Br J Sports Med. 2018;52(2):83–88. [DOI] [PubMed] [Google Scholar]
- 84. Verrall GM, Slavotinek JP, Barnes PG, Fon GT. Diagnostic and prognostic value of clinical findings in 83 athletes with posterior thigh injury: comparison of clinical findings with magnetic resonance imaging documentation of hamstring muscle strain. Am J Sports Med. 2003;31(6):969–973. [DOI] [PubMed] [Google Scholar]
- 85. Wangensteen A, Almusa E, Boukarroum S, et al. MRI does not add value over and above patient history and clinical examination in predicting time to return to sport after acute hamstring injuries: a prospective cohort of 180 male athletes. Br J Sports Med. 2015;49(24):1579–1587. [DOI] [PubMed] [Google Scholar]
- 86. Warren P, Gabbe BJ, Schneider-Kolsky M, Bennell KL. Clinical predictors of time to return to competition and of recurrence following hamstring strain in elite Australian footballers. Br J Sports Med. 2010;44(6):415–419. [DOI] [PubMed] [Google Scholar]
- 87. Willinger L, Siebenlist S, Lacheta L, et al. Excellent clinical outcome and low complication rate after proximal hamstring tendon repair at mid-term follow up. Knee Surg Sports Traumatol Arthrosc. 2020;28(4):1230–1235. [DOI] [PubMed] [Google Scholar]
- 88. Wright-Carpenter T, Klein P, Schaferhoff P, Appell HJ, Mir LM, Wehling P. Treatment of muscle injuries by local administration of autologous conditioned serum: a pilot study on sportsmen with muscle strains. Int J Sports Med. 2004;25(8):588–593. [DOI] [PubMed] [Google Scholar]
- 89. Zanon G, Combi F, Combi A, Perticarini L, Sammarchi L, Benazzo F. Platelet-rich plasma in the treatment of acute hamstring injuries in professional football players. Joints. 2016;4(1):17–23. [DOI] [PMC free article] [PubMed] [Google Scholar]


