Abstract
Gastrointestinal stromal tumors (GISTs) arising from the rectum are rare. We report the case of an aggressive rectal gastrointestinal stromal tumor (GIST) in a 60-year-old female that presented for symptoms of constipation and lower gastrointestinal bleeding. Upon rectal examination, a hard mass was found at 6cm from the anal marge. An MRI was indicated that shows a well-demarcated lesion originates from the distal rectum with exophytic growth and central necrosis. The diagnosis of rectal gist was confirmed by colonoscopy with biopsy and immunohistochemical analyses of bioptic material. Liver metastases were seen on computerized tomography (CT). She was referred for palliative chemotherapy. The patient had suffered from intestinal obstruction three weeks after his initial presentation and passed away shortly thereafter. We aimed to report this case as an aggressive and rare GIST localization.
Keywords: Rectum, GIST, MRI
Introduction
GIST in the rectum is extremely rare. It represents less than 5% of all gastrointestinal stromal tumors and 0.1% of all colorectal tumors.
We present a case of an aggressive rectal GIST tumor that was not amenable to resection, resulting in intestinal obstruction and liver metastasis.
Case report
A 60-year-old male patient with symptoms of constipation and lower gastrointestinal bleeding. She also described abdominal pain located in the right upper quadrant of the abdomen.
Physical exam revealed a palpable mass on rectal exam located at 6 centimeters from anal marge visualized on rectoscopy evocative of anorectal carcinoma.
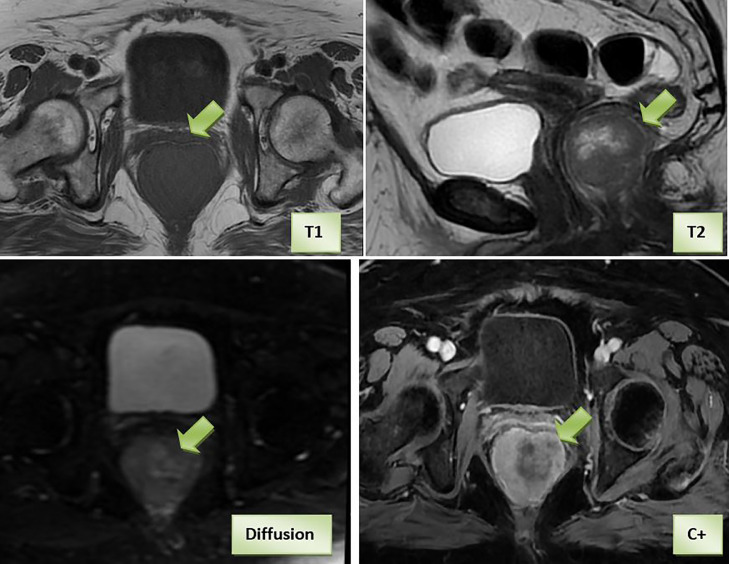
Pelvic MRI was performed for determining the exact tumor origin and delineating the spatial relation to adjacent structures. It reveals a well-demarcated mass originates from the distal rectum with exophytic growth, central necrosis by T2-weighted imaging of high signal, and heterogeneous enhancement suggestive of GIST (Fig. 1). We noticed close contact with the posterior vaginal wall and bilateral levator ani. Her colonoscopy-guided biopsy and immunohistochemical examination confirmed the diagnosis of rectal GIST with high mitotic activity.
Fig. 1.
Pelvic MRI shows a Well-demarcated mass originates from the distal rectum with exophytic growth and central necrosis on T2-weighted image, T1-weighted image, sagittal T2–weighted image, Diffusion, and contrast enhancement
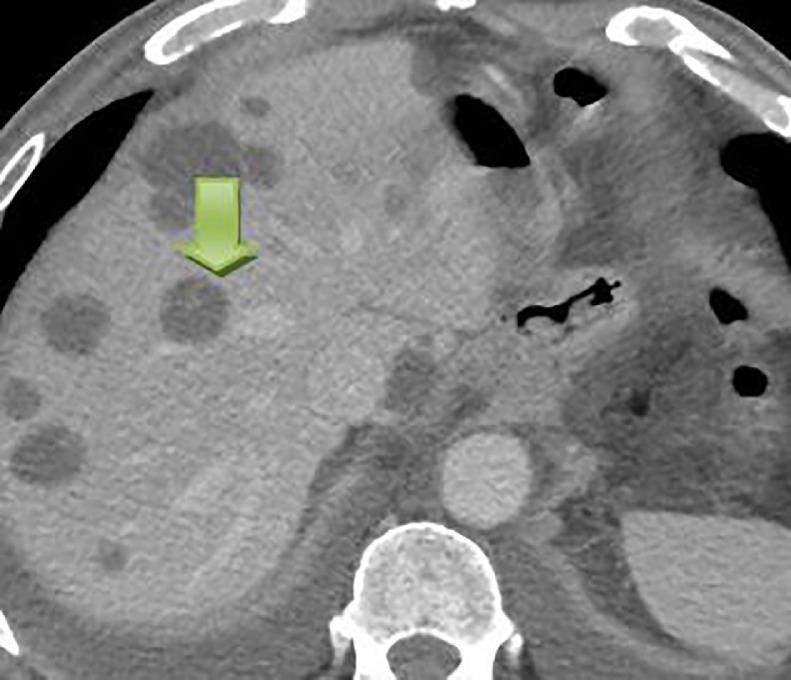
Contrast-enhanced CT of the chest and abdomen, for staging revealed metastatic lesions of the liver (Fig. 2). She was determined to be a non-surgical candidate due to metastatic liver disease and was referred to an oncology department for palliative chemotherapy (Imatinib). She presented to the emergency department three weeks later with abdominal pain, nausea, and vomiting. Her abdomen and imaging from the outside hospital revealed an intestinal obstruction. The patient refused surgery as she wished to be discharged home and be with her family. She passed away two weeks later.
Fig. 2.
Contrast-enhanced showing multiples hypodense lesions related to metastatic disease
Discussion
Rectal GISTs account for approximately 2% of all gist tumors and 0.1% of all colorectal tumors [1]. The majority of GISTs have a benign course, in some rare cases, it can exhibit an aggressive course, such as the case in our patient.
The aggressiveness of a GIST tumor is related to tumor size and histological findings [2]. In a tumor larger than 5 cm with a mitotic count higher than ten per fifty high-power field HPF, the risk of aggressive clinical behavior is considered to be high.
The median age is around 60–65 years old, with a similar clinical presentation to rectal adenocarcinoma including rectal bleeding, constipation, abdominal and pelvic discomfort. However intestinal obstruction due to rectal GIST is uncommon [3]. For this reason, we aimed to report this case.
The majority of rectal GISTs arise from the muscularis propria of the intestinal wall. They usually have an exophytic growth pattern with the epicenter located well outside the rectum [4].
MRI is the best modality to determine the origin of the tumor. It allows an appropriate assessment of the surgical pelvic floor, the involvement of adjacent organs, and the exact distance from the anal verge. It may be superior to CT in detecting the internal component.
Rectal GISTs appear as isointense to skeletal muscle on T1-weighted images and hyperintense on T2-weighted images, and moderately or mildly enhanced. An heterogeneous pattern of enhancement is common as in our case. It corresponds to intralesional necrosis or hemorrhage considered as poor prognostic factors [5].
Contrast-enhanced CT is more dedicated to assess the presence or absence of metastatic disease.
Accurate diagnosis relies on pathologic, cytologic, and immunohistochemical analysis of the tumor cells. Through immunocytochemical stain, the tumor cells for c-kit and CD34 showed diffusely positive in both smear specimens and paraffin sections [6].
GIST tumors including rectal localization are typically managed with surgical resection. The liver is the first metastatic site, Lymph node involvement, lung and bone metastasis are rare with GISTs.If the tumor presents with metastases or local advancement to the point where surgical treatment may not be effective, the patient is treated with tyrosine kinase inhibitor imatinib mesylate [7].
As with other GIST tumors, adjuvant chemotherapy with imatinib mesylate is effective in the treatment of rectal GISTs. Our patient didn't have the chance to start her Imatinib mesylatechemotherapy as she presented intestinal obstruction.
Intestinal obstruction in rectal gists is an unusual situation [8].
The overall survival rate for a patient with a rectal GIST varies based on its tumor grade [8]. The most common cause of death is distant metastasis and involvement of the liver is a frequent event.
In our case, the intestinal obstruction complicates, even more, the outcome.
Conclusion
Rectal GISTs, need to be approached earlier and with caution due to their unpredictable character of aggressiveness. Imatinib should be introduced earlier for unresectable and metastatic diseases. A high-risk rectal GIST based on mitotic power and size of the tumor is associated with aggressive metastatic dissemination to the liver and evocative of poor survival.
Provisional title of the case report:
Metastatic Rectal Gastrointestinal Stromal Tumor with intestinal obstruction: A rare Case Report
I, GAAMOUCH FATIMA have been diagnosed by Dr RAMI AMAL and Dr KASSIMI MARIAM
My mail address is GAAMOUCH.FATIMA@gmail.com
I confirm that I: (please check the box to confirm)
X am legally entitled to give this consent
In signing this consent form, I authorize this practitioner and other co-authors to write a case report about my treatment. I understand the following:
I will not directly benefit from participating in this case report. The information that can be shared with other health care professionals, however, may improve the care that is received by others in the future.
Signing this consent form does not remove my rights to privacy. My name and protected health information (PHI) will not be shared, unless my authorship is requested and consented, however, I understand that complete anonymity cannot be guaranteed. It is possible that somebody somewhere - for example, somebody who looked after me or a relative - may recognize me.
My information being used for this case report includes relevant to this case disease history, laboratory findings, photographs and prescribed treatment protocols.
A summary of my treatment will be presented for evaluation by a panel of experts and researchers and may be published in a medical journal under open access license (everybody can see and read such publication freely online) and/or presented at a medical conference, and I give permission for such publication or presentation. The summary of my treatment and the case report will not contain any personal data. If any personal data are affected they will be published in anonymized form.
Allowing my information to be used in this case report will not involve any additional costs to me. I will not receive any compensation.
My participation is entirely voluntary, and I may withdraw permission to participate in this case report at any time. All my personal data submitted to Heel will be deleted after notification received from the treating practitioner. However, once the case report is written and published (containing any personal data in anonymized form), it will not be possible for me to withdraw it. My decision will not result in any penalty or loss of benefits to which I am entitled including the quality of care I receive. The withdrawal can be sent to the treating practitioner (please see contact data above).
I may be asked to contribute a “patient's perspective” on the treatment that I have received. I can voluntarily decide to provide this perspective or decline.
By signing this form, I confirm that:
-
•
The case report has been fully explained to me and all of my questions have been answered to my satisfaction
-
•
I have been informed of the risks and benefits, if any, of allowing my information to be used in this case report
-
•
I have been informed that I do not have to participate in this case report
-
•
I have read each page of this form
-
•
I authorize access to my personal health information (medical record) as explained in this form
-
•
I have agreed to participate in this case report
-
•
I have seen a version of a case report to be submitted or published (including photographs) and I agree to it
|
To sign for the patient or legally entitled caregiver |
To sign for the treating practitioner, who has explained and administered the form to the patient |
|
Date 19/7/2021 Place CASABLANCA Print name EL GAAMOUCH FATIMA Signature |
Date 19/7/2021 Place CASABLANCA Print name MARIAM KASSIMI Signature |
Footnotes
Funding: This study was not funded.
Conflicts of interest: The authors declare that they have no conflict of interest.
Availability of data and material: Data available within the article.
References
- 1.Puckett Y, Aryaie A. Case report of diffusely metastatic rectal GIST. Int J Surg Case Rep. 2017;37:4–9. doi: 10.1016/j.ijscr.2017.05.033. Epub 2017 Jun 1. PMID: 28605620; PMCID: PMC5470555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jiang ZX, Zhang SJ, Peng WJ, Yu BH. Rectal gastrointestinal stromal tumors: imaging features with clinical and pathological correlation. World J Gastroenterol. 2013;19(20):3108–3116. doi: 10.3748/wjg.v19.i20.3108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dickhoff C, Leguit RJ, Slors JF, Vervenne WL, Bemelman WA. Giant rectal gastrointestinal stromal tumors: a report of two cases. Case Rep Gastroenterol. 2008;2:54–69. doi: 10.1159/000119317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Manouras A, Pappas A, Katergiannakis V, Filis K, Chrysikos J, Pattas M, et al. Gastrointestinal stromal tumors of the rectum: report of five cases. Acta Gastroenterol Belg. 2009;72:257–261. [PubMed] [Google Scholar]
- 5.Iwa N, Shiozaki K, Izawa H, Baba M, Kanai T, Kobayashi Y, et al. Gastrointestinal stromal tumor arising from anorectum: correlation of imprint cytology and radiologic imaging. Ann Diagn Pathol. 2007:212–216. doi: 10.1016/j.anndiagpath.2006.08.002. [DOI] [PubMed] [Google Scholar]
- 6.Kane WJ, Friel CM. Diagnosis and treatment of rectal gastrointestinal stromal tumors. Dis Colon Rectum. 2019;62(5):537–540. doi: 10.1097/DCR.0000000000001376. PMID: 30964792. [DOI] [PubMed] [Google Scholar]
- 7.Karla Uribe Rivera Ana, Andres Guevara Jabiles, Ivan Chavez Passiuri, Elica Garcia Leon, Melvy Guerrero Quiroga, Renier Cruz Baca, et al. Gastrointestinal stromal tumour of the rectum and intestinal obstruction. Case Rep Ecancer. 2020;14:1139. doi: 10.3332/ecancer.2020.1139. [DOI] [PMC free article] [PubMed] [Google Scholar]