Abstract
Background
Ischemic heart disease (IHD) imposes the greatest disease burden globally, especially in low‐ and middle‐income countries (LMICs). We aim to examine the population‐attributable fraction and risk‐attributable death and disability‐adjusted life years (DALYs) for IHD in 137 low‐ and middle‐income countries.
Methods and Results
Using comparative risk assessment framework from the 2019 Global Burden of Disease study, the population‐attributable fraction and IHD burden (death and DALYs) attributable to risk factors in low‐income countries, lower‐middle‐income countries (LMCs), and upper‐middle‐income countries were assessed from 2000 to 2019. In 2019, the population‐attributable fraction (%) of IHD deaths in relation to all modifiable risk factors combined was highest in lower‐middle‐income countries (94.2; 95% uncertainty interval, 91.9–96.2), followed by upper‐middle‐income countries (93.5; 90.4–95.8) and low‐income countries (92.5; 90.0–94.7). There was a >13‐fold difference between Peru and Uzbekistan in age‐standardized rates (per 100 000) of attributable death (44.3 versus 660.4) and DALYs (786.7 versus 10506.1). Dietary risks accounted for the largest proportion of IHD’s behavioral burden in low‐ and middle‐income countries, primarily attributable to diets low in whole grains. High systolic blood pressure and high low‐density lipoprotein cholesterol remained the 2 leading causes of DALYs, with the former topping the list in 116 countries, while the latter led in 21 of the 137 countries. Compared with 2000 to 2010, the increases in risk‐attributable deaths and DALYs among upper‐middle income countries were slower from 2010 to 2019, while the trends in low‐income countries and lower‐middle income countries were opposite.
Conclusions
IHD’s attributable burden remains high in low‐ and middle‐income countries. Considerable heterogeneity was observed among different income‐classified regions and countries.
Keywords: death, disability‐adjusted life years, ischemic heart disease, low‐ and middle‐income countries, risk factors
Subject Categories: Cardiovascular Disease, Epidemiology, Risk Factors
Nonstandard Abbreviations and Acronyms
- DALYs
disability‐adjusted life years
- GBD
Global Burden of Disease
- IHD
ischemic heart disease
- LICs
low‐income countries
- LMCs
lower‐middle‐income countries
- LMICs
low‐ and middle‐income countries
- MICs
middle‐income countries
- PAF
population‐attributable fraction
- PURE
Prospective Urban Rural Epidemiology
- TMREL
theoretical minimum risk exposure level
- UMCs
upper‐middle‐income countries
Clinical Perspective
What Is New?
Using the updated comparative risk assessment framework from the 2019 Global Burden of Disease study, we provided the first income‐classified region‐, country‐, sex‐, and age‐specific assessment of ischemic heart disease (IHD) burden attributable to risk clusters and risk factors among 137 low‐ and middle‐income countries from 2000 to 2019.
Most global risk‐attributable deaths and DALYs for IHD occurred in low‐ and middle‐income countries, with a substantial geographic discrepancy observed across the 137 individual countries.
A diverging trend in IHD burden between middle‐income countries and low‐income countries during the 2010 to 2019 period compared with 2000 to 2010.
What Are the Clinical Implications?
Preventive interventions reducing behavioral and metabolic risks will be more effective in managing IHD burden for middle‐income countries, while interventions to reduce environmental risks should be implemented in low‐income countries.
More investments in managing preventable IHD burden are needed considering the substantial geographical income discrepancies across the 137 low‐ and middle‐income countries.
Ischemic heart disease (IHD) is the leading contributor to deaths and disability‐adjusted life years (DALYs) globally, especially in low‐ and middle‐income countries (LMICs); most deaths and DALYs are attributable to potentially modifiable risk factors. 1 IHD is projected to remain a serious threat, because widespread drivers including demographic shifts, environmental risks, and harmful lifestyles, steadily present challenges to its control and prevention. 2 , 3 Evidence has indicated that rising income inequality accelerates health disparities between countries. 4 , 5 Tracking discrepancies in attributable burden (death and DALYs) across income‐classified regions and countries at varying economic levels is necessary to prioritize resource allocation and devise tailored regulations in concordance with the Sustainable Development Goals’ target 3, which advocates for context‐specific initiatives to reduce premature mortality caused by IHD and diminish related risks. 6
A critical starting point is to quantify the magnitude of avoidable IHD burden associated with modifiable risks across LMICs, where limited economic development may decrease the availability of health services. However, previous studies regarding the attributable IHD burden were restricted to single countries with small populations, 7 , 8 , 9 limited time frames lacking temporal trends, 5 incomprehensive analyses containing a small number of risk factors, 5 , 10 , 11 and inconsistent methods. 8 , 12 Moreover, most studies have paid disproportionately little attention to LMICs 13 , 14 and have failed to provide systematic estimates that account for economic disparities among countries. The Global Burden of Diseases (GBD) 1 study can fill the above gaps, as it provides the most up‐to‐date estimates on metrics of multiple diseases associated with specific risks. However, detailed data on the IHD burden resulting from specific risk factors remain inadequate.
Understanding the modifiable risk factors that drive disease is a necessary global priority to prevent health loss. Our study is an attempt to provide such detailed data. In order to document the burden of IHD that results from modifiable risk factors, we regionally and nationally monitored the disparities in population‐attributable fraction (PAF), as well as the burden of IHD attributable to both risk clusters and 27 individual risk factors from 2000 to 2019. In response to the Sustainable Development Goals’ target to “leave no one behind by 2030,” 6 this study’s results will help inform governments of tailored strategies to mitigate preventable IHD burden in 137 LMICs.
Methods
The data that support the findings of this study are publicly available via the Global Health Data Exchange website (http://www.healthdata.org). We conformed to Guidelines for Accurate and Transparent Health Estimates Reporting recommendations to ensure the transparency and reproducibility of results (Data S1). Ethics approval and consent to participate were not applicable to this study.
Overview
The 2019 GBD study provided age‐sex‐specific mortality, years lived with disability, years of life lost, and DALYs for 369 diseases and injuries, and 87 risk factors in 204 countries and territories from 1990 to 2019. 1 , 15 , 16 , 17 To quantify the epidemiologic transitions for individual risk factors and risk clusters by income‐classified region, country, sex, age, cause, and year, the updated comparative risk assessment framework was established as a causal web of modifiable risk factors leading to health outcomes. 1 Compared with previous GBD studies, 18 , 19 the 2019 GBD study developed new approaches to better estimate the exposure to risk factors by integrating globally accessible data from multiple epidemiologic studies, which included updated high‐quality meta‐analyses, randomized controlled trials, cohort studies, case‐control studies, and other observational studies, providing major updates about dietary and metabolic risks. 1 The GBD study used unified and standard methods to ensure the results were comparable and regionally and nationally representative. The detailed methodology of the risk assessments has been provided elsewhere. 1
All data obtained in the present study were publicly available at the Institute for Health Metrics and Evaluation website and can be accessed with open online tools (http://www.healthdata.org/results/data‐visualizations; http://ghdx.healthdata.org/gbd‐resultstool). 20 IHD is defined as per the International Classification of Diseases, Tenth Revision (ICD‐10) with diagnosis codes I20–I25. 17
Modifiable Risk Factors for IHD
According to the GBD study criteria, IHD‐related individual risk factors and risk clusters were classified into 5 hierarchical levels (0–4). All potentially modifiable risk factors combined were defined as level 0. In level 1, clusters of behavioral, environmental, and metabolic risk factors were assessed. Detailed clusters of risks (ie, air pollution, other environmental risks, tobacco, and dietary risks) were included in level 2. Twenty‐seven risk‐IHD pairs in causal relationships were established in level 4, where deaths and DALY‐based PAFs for individual risk factors were ranked. These risk factors include ambient particulate matter pollution, household air pollution from solid fuels, lead exposure, smoking, secondhand smoke, diets low in fruits/vegetables/legumes/whole grains/nuts and seeds/fiber/seafood‐derived omega‐3 fatty acids/polyunsaturated fatty acids, diets high in red meat/processed meat/sugar‐sweetened beverages/trans fatty acids/sodium, low physical activity, high systolic blood pressure, high low‐density lipoprotein (LDL) cholesterol, high fasting plasma glucose, high body mass index, impaired kidney function, high temperature, and low temperature. There were 1 cluster (particulate matter pollution) and 19 individual risk factors at level 3. 1
Statistical Analysis
The Bayesian meta‐regression model DisMod‐MR 2.1 was used as the main method to estimate the prevalence of nonfatal diseases, and the Cause of Death Ensemble Model was used to appraise cause‐specific mortality. 16 , 17 To explore potential trends of specific risk factors, improved spatiotemporal Gaussian process regression was applied to synthesize all available data. 1 DALYs are the sum of years lived with disability, which is based on cause‐specific prevalence and disability weight, and years of life lost attributable to premature mortality, which is calculated by multiplying age‐sex–specific deaths by global standard life expectancy. 15 The detailed methodology for estimating disease burden in the above metrics was published previously. 15 , 16 , 17 To characterize the temporal trends across income‐classified regions and countries, age‐standardized rates (per 100 000) were computed using the global age‐standard population constructed by the World Health Organization.
Estimation of the Attributable Burden
The relative risks for risk‐IHD pairs were determined by multinational prospective studies. 1 Under the comparative risk assessment framework, counterfactual analysis was employed to estimate the theoretical minimum risk exposure level (TMREL) that represented the optimal level of risk factor exposure (Table S1). PAF was the avoidable proportion of the IHD burden that may occur if the exposure to a specific risk factor could be reduced to the TMREL in a general population. PAF was estimated using incorporated data of relative risks for risk‐IHD pairs, the exposure level of the risk factor, and the TMREL. 11 The PAF for each individual risk factor was calculated either directly or with mediation adjustments, and calculations for risk clusters took into consideration the interaction between risk factors. The negative values of PAF imply a beneficial effect of risk exposure (alcohol use) on IHD risks. Further details of the PAF calculation methodology are specified in Data S2.
Based on the following formula, the attributable burden for IHD in a given year, age, sex, and location was calculated by multiplying the burden metric (such as absolute deaths and DALYs) by the corresponding PAF:
where AB is the attributable burden (deaths and DALYs) for risk factor i in a given population. The detailed calculation process for the risk‐attributable IHD burden is demonstrated in the analytical flowchart in Figure S1.
Geographic Estimation
Based on income levels categorized by the World Bank, a total of 137 LMICs were stratified into 3 groups, with 31, 47, and 59 countries classified as low‐income countries (LICs), lower‐middle‐income countries (LMCs), and upper‐middle‐income countries (UMCs), respectively (Table S2).
Uncertainty Interval
For deaths and DALYs, the corresponding 95% uncertainty intervals were calculated using the 2.5th and 97.5th estimates in posterior simulation of 1000 ordered draws, with the aim of examining uncertain distributions deriving from random and systematic errors.
Results
PAF and IHD Attributable Burden in 2019
Overall Modifiable Risk Factors
Income‐Classified Region
In 2019, the PAF (%) of deaths for all modifiable risk factors was highest in LMCs (94.2; 95% uncertainty interval, 91.9–96.2), followed by LICs (92.5; 90.0–94.7) and UMCs (93.5; 90.4–95.8); the risk‐attributable proportion for DALYs ranged from 93.0% in LICs to 94.7% in LMCs. A total of 8.54 (7.81–9.14) million deaths from IHD were attributable to potentially modifiable risk factors globally, with 3.42 (3.07–3.71) million, 3.19 (2.89–3.48) million, and 0.28 (0.24–0.33) million in UMCs, LMCs, and LICs, respectively (Table 1). There were wide variations in age‐standardized risk‐attributable death and DALY rates for IHD across income‐classified regions (Figure 1A and 1C; Tables S3 and S4).
Table 1.
Deaths and DALYs for IHD Attributable to Modifiable Risk Factors, and PAF Both Globally and in Low‐ and Middle‐Income Countries in 2019
| Low‐income | Lower‐middle | Upper‐middle | Globally | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Attributable number (in thousand) (95% UI*) |
PAF (%) (95% UI) | Rank |
Attributable number (in thousand) (95% UI*) |
PAF (%) (95% UI) | Rank |
Attributable number (in thousand) (95% UI*) |
PAF (%) (95% UI) | Rank |
Attributable number (in thousand) (95% UI*) |
PAF (%) (95% UI) | Rank | |
| Death | ||||||||||||
| Environmental/occupational risks |
128.5 (106.9 to 153.0) |
41.7 (38.1 to 45.9) |
1192.8 (1040.6 to 1350.6) |
35.2 (32.0 to 38.2) |
1017.8 (865.2 to 1181.2) |
27.8 (24.7 to 31.0) |
2615.8 (2296.2 to 2939.7) |
28.6 (25.8 to 31.6) |
||||
| Air pollution |
106.5 (87.8 to 127.6) |
34.6 (31.2 to 39.0) |
928.0 (804.2 to 1049.6) |
27.4 (25.0 to 30.0) |
689.5 (580.2 to 802.0) |
18.8 (16.6 to 21.1) |
1843.2 (1605.7 to 2080.5) |
20.2 (17.9 to 22.4) |
||||
| Particulate matter pollution |
106.5 (87.8 to 127.6) |
34.6 (31.2 to 39.0) |
928.0 (804.2 to 1049.6) |
27.4 (25.0 to 30.0) |
689.5 (580.2 to 802.0) |
18.8 (16.6 to 21.1) |
1843.2 (1605.7 to 2080.5) |
20.2 (17.9 to 22.4) |
||||
| Ambient particulate matter pollution |
22.6 (13.1 to 35.2) |
7.4 (4.2 to 11.2) |
11 |
612.9 (483.3 to 737.3) |
18.1 (14.8 to 21.2) |
4 |
580.2 (477.3 to 686.4) |
15.8 (13.5 to 18.0) |
7 |
1332.0 1086.9 to 1557.2) |
14.6 (12.2 to 16.7) |
7 |
| Household air pollution from solid fuels |
83.9 (63.4 to 108.2) |
27.2 (21.8 to 33.6) |
3 |
315.1 (211.8 to 440.1) |
9.3 (6.4 to 12.8) |
10 |
109.2 (55.5 to 186.3) |
3.0 (1.5 to 5.1) |
21 |
511.2 (348.4 to 714.6) |
5.6 (3.8 to 7.8) |
14 |
| Suboptimal temperature |
16.5 (9.4 to 22.5) |
5.4 (2.9 to 7.1) |
173.9 (88.0 to 234.8) |
5.1 (2.7 to 6.8) |
269.6 (186.8 to 364.4) |
7.4 (5.2 to 9.9) |
596.8 (414.3 to 763.3) |
6.5 (4.6 to 8.3) |
||||
| High temperature |
2.1 (−4.2 to 4.6) |
0.7 (−1.3 to 1.5) |
26 |
29.2 (−39.0 to 70.9) |
0.9 (−1.2 to 2.1) |
26 |
8.8 (−3.4 to 17.9) |
0.2 (−0.1 to 0.5) |
26 |
43.3 (−42.1 to 95.3) |
0.5 (−0.5 to 1.0) |
26 |
| Low temperature |
14.5 (9.6 to 19.8) |
4.7 (3.2 to 6.2) |
18 |
145.8 (94.9 to 195.6) |
4.3 (2.8 to 5.7) |
21 |
261.5 (176.8 to 358.7) |
7.1 (4.9 to 9.6) |
11 |
555.5 (391.6 to 721.3) |
6.1 (4.4 to 7.9) |
12 |
| Other environmental risks |
18.2 (11.4 to 26.5) |
5.9 (3.8 to 8.3) |
207.1 (133.2 to 292.4) |
6.1 (4.1 to 8.3) |
153.2 (87.3 to 235.9) |
4.2 (2.4 to 6.3) |
413.0 (242.8 to 615.7) |
4.5 (2.7 to 6.6) |
||||
| Lead exposure |
18.2 (11.4 to 26.5) |
5.9 (3.8 to 8.3) |
14 |
207.1 (133.2 to 292.4) |
6.1 (4.1 to 8.3) |
15 |
153.2 (87.3 to 235.9) |
4.2 (2.4 to 6.3) |
17 |
413.0 (242.8 to 615.7) |
4.5 (2.7 to 6.6) |
17 |
| Behavioral risks |
189.2 (154.9 to 228.1) |
61.5 (54.1 to 68.1) |
2215.5 (1932.4 to 2499.4) |
65.4 (58.7 to 71.0) |
2383.8 (2049.0 to 2701.1) |
65.1 (58.5 to 71.1) |
5896.9 (5170.3 to 6632.0) |
64.5 (57.8 to 70.6) |
||||
| Tobacco |
48.6 (41.1 to 57.0) |
15.8 (14.6 to 17.1) |
734.7 (656.5 to 807.9) |
21.7 (20.5 to 22.9) |
887.2 (795.7 to 988.6) |
24.2 (22.8 to 25.8) |
1998.2 (1840.4 to 2155.8) |
21.9 (20.8. 23.1) |
||||
| Smoking |
39.4 (33.4 to 46.3) |
12.8 (11.8 to 13.9) |
7 |
597.7 (537.0 to 658.1) |
17.7 (16.7 to 18.7) |
6 |
748.4 (670.6 to 831.6) |
20.4 (19.1 to 21.9) |
4 |
1682.0 (1558.4 to 1805.3) |
18.4 (17.5 to 19.5) |
4 |
| Secondhand smoke |
10.9 (8.4 to 13.8) |
3.6 (2.9 to 4.3) |
21 |
166.5 (134.0 to 201.7) |
4.9 (4.0 to 5.9) |
18 |
178.1 (141.4 to 217.5) |
4.9 (4.0 to 5.8) |
16 |
397.4 (319.9 to 477.6) |
4.3 (3.6 to 5.2) |
18 |
| Alcohol use |
−5.4 (−9.4 to −1.5) |
−1.8 (−3.0 to −0.5) |
27 |
−30.8 (−65.3 to 5.5) |
−0.9 (−2.0 to 0.2) |
27 |
−34.9 (−98.1 to 27.1) |
−1.0 (−2.6 to 0.7) |
27 |
−108.0 (−252.6 to 36.5) |
−1.2 (−2.8 to 0.4) |
27 |
| Dietary risks |
166.6 (130.2 to 206.4) |
54.1 (45.0 to 62.4) |
1857.1 (1523.7 to 2170.3) |
54.9 (45.7 to 62.4) |
1925.4 (1547.2 to 2307.2) |
52.6 (43.3 to 60.9) |
4877.1 (3990.6 to 5749.3) |
53.4 (44.2 to 61.2) |
||||
| Diet low in fruits |
19.2 (7.7 to 29.4) |
6.2 (2.6 to 9.0) |
13 |
222.4 (98.5 to 323.8) |
6.6 (2.9 to 9.4) |
13 |
131.3 (45.3 to 210.1) |
3.6 (1.2 to 5.6) |
19 |
436.5 (179.4 to 659.3) |
4.8 (1.9 to 7.1) |
16 |
| Diet low in vegetables |
26.9 (16.5 to 37.6) |
8.7 (5.5 to 11.9) |
10 |
192.7 (106.2 to 277.2) |
5.7 (3.2 to 8.0) |
16 |
75.5 (38.5 to 108.4) |
2.1 (1.1 to 3.0) |
24 |
358.3 (195.9 to 513.6) |
3.9 (2.1 to 5.6) |
19 |
| Diet low in legumes |
36.6 (8.4 to 61.9) |
11.9 (2.8 to 19.3) |
8 |
441.0 (99.5 to 723.4) |
13.0 (3.0 to 21.0) |
8 |
410.6 (85.8 to 660.6) |
11.2 (2.3 to 18.1) |
10 |
1116.4 (252.0 to 1815.3) |
12.2 (2.8 to 19.7) |
9 |
| Diet low in whole grains |
50.2 (19.2 to 67.9) |
16.3 (6.2 to 21.5) |
5 |
540.9 (213.2 to 711.1) |
16.0 (6.2 to 20.9) |
7 |
594.3 (219.6 to 781.5) |
16.2 (5.9 to 21.1) |
6 |
1459.1 (550.8 to 1908.0) |
16.0 (6.0 to 20.8) |
6 |
| Diet low in nuts and seeds |
16.4 (8.7 to 23.2) |
5.3 (2.8 to 7.3) |
16 |
263.3 (149.3 to 352.0) |
7.8 (4.4 to 10.3) |
12 |
189.9 (83.7 to 278.7) |
5.2 (2.3 to 7.5) |
14 |
546.6 (279.3 to 757.4) |
6.0 (3.1 to 8.2) |
13 |
| Diet high in processed meat |
3.8 (0.7 to 10.8) |
1.2 (0.2 to 3.4) |
25 |
46.9 (21.0 to 91.1) |
1.4 (0.6 to 2.7) |
25 |
63.8 (12.1 to 132.4) |
1.7 (0.3 to 3.6) |
25 |
197.2 (47.0 to 377.6) |
2.2 (0.5 to 4.2) |
24 |
| Diet high in sugar‐sweetened beverages |
7.2 (5.6 to 9.0) |
2.3 (1.9 to 2.8) |
24 |
62.5 (44.0 to 79.6) |
1.8 (1.3 to 2.3) |
24 |
80.8 (54.2 to 104.8) |
2.2 (1.5 to 2.8) |
23 |
193.1 (127.4 to 248.5) |
2.1 (1.4 to 2.7) |
25 |
| Diet low in fiber |
11.4 (4.6 to 19.0) |
3.7 (1.5 to 6.2) |
20 |
166.6 (74.4 to 269.9) |
4.9 (2.2 to 7.7) |
19 |
96.9 (37.4 to 171.7) |
2.6 (1.0 to 4.6) |
22 |
348.9 (147.6 to 568.3) |
3.8 (1.6 to 6.2) |
21 |
| Diet low in seafood omega‐3 fatty acids |
12.5 (4.1 to 17.7) |
4.1 (1.3 to 5.5) |
19 |
136.3 (52.0 to 184.5) |
4.0 (1.6 to 5.3) |
22 |
132.7 (69.4 to 172.5) |
3.6 (1.9 to 4.5) |
18 |
337.3 (165.6 to 435.7) |
3.7 (1.8 to 4.7) |
23 |
| Diet low in polyunsaturated fatty acids |
14.8 (2.1 to 29.9) |
4.8 (0.7 to 9.6) |
17 |
166.7 (19.5 to 340.4) |
4.9 (0.6 to 7.7) |
17 |
130.3 (16.7 to 268.8) |
3.6 (0.4 to 7.3) |
20 |
346.2 (44.2 to 707.3) |
3.8 (0.5 to 7.7) |
22 |
| Diet high in trans fatty acids |
16.7 (2.7 to 26.1) |
5.4 (0.8 to 8.3) |
15 |
269.4 (31.6 to 371.7) |
8.0 (1.0 to 10.7) |
11 |
218.5 (28.3 to 308.9) |
6.0 (0.8 to 8.4) |
12 |
645.0 (75.9 to 882.3) |
7.1 (0.8 to 9.5) |
11 |
| Diet high in sodium |
21.9 2.3 59.3 |
7.1 (0.8 to 19.6) |
12 |
215.7 (24.6 to 564.6) |
6.4 (0.7 to 16.6) |
14 |
431.5 (138.9 to 855.3) |
11.8 (3.9 to 23.3) |
9 |
777.2 (185.3 to 1773.1) |
8.5 (2.1 to 19.4) |
10 |
| Diet high in red meat |
7.5 (0.7 to 15.2) |
2.4 (0.2 to 4.6) |
23 |
69.8 (9.2 to 133.3) |
2.1 (0.3 to 3.9) |
23 |
180.2 (29.7 to 337.6) |
4.9 (0.8 to 9.1) |
15 |
351.2 (55.9 to 642.7) |
3.8 (0.6 to 7.1) |
20 |
| Low physical activity |
10.8 (3.7 to 25.3) |
3.5 (1.2 to 8.0) |
22 |
154.5 (57.1 to 331.7) |
4.6 (1.7 to 9.5) |
20 |
205.8 (74.8 to 417.3) |
5.6 (2.1 to 11.4) |
13 |
486.8 (175.7 to 1003.3) |
5.3 (1.9 to 11.0) |
15 |
| Metabolic risks |
242.1 (201.4 to 285.5) |
78.6 (72.2 to 85.0) |
2806.8 (2475.5, to3126.9) |
82.9 (76.9 to 88.7) |
2999.1 (2627.5 to 3339.7) |
81.9 (74.8 to 88.3) |
7526.9 (6657.2 to 8311.7) |
82.4 (75.7 to 88.5) |
||||
| High systolic blood pressure |
161.3 (126.5 to 198.8) |
52.4 (44.3 to 60.3) |
1 |
1856.1 (1533.8 to 2194.9) |
54.8 (46.7 to 63.2) |
1 |
1964.3 (1553.3 to 2381.2) |
53.6 (42.9 to 63.7) |
1 |
4861.6 (3927.2 to 5853.4) |
53.2 (43.4 to 62.8) |
1 |
| High LDL cholesterol |
114.8 (85.3 to 148.8) |
37.3 (29.1 to 46.1) |
2 |
1374.2 (1064.8 to 1717.1) |
40.6 (32.3 to 49.5) |
2 |
1549.5 (1141.7 to 1988.3) |
42.3 (31.6 to 53.6) |
2 |
3784.3 (2826.6 to 4824.7) |
41.4 (31.5 to 52.1) |
2 |
| High fasting plasma glucose |
68.8 (40.5 to 109.7) |
22.4 (13.3 to 35.2) |
4 |
923.2 (545.5 to 1439.0) |
27.3 (16.6 to 42.3) |
3 |
810.1 (460.6 to 1292.0) |
22.1 (12.7 to 34.5) |
3 |
2353.4 (1361.2 to 3701.9) |
25.8 (15.0 to 40.3) |
3 |
| High body‐mass index |
40.8 (21.1 to 66.0) |
13.2 (7.3 to 20.8) |
6 |
609.6 (381.9 to 866.3) |
18.0 (11.4 to 25.5) |
5 |
648.1 (373.1 to 989.5) |
17.7 (10.2 to 26.7) |
5 |
1662.3 (1005.2 to 2462.3) |
18.2 (11.0 to 26.6) |
5 |
| Impaired kidney function |
30.9 (20.7 to 43.0) |
10.1 (7.0 to 13.3) |
9 |
433.2 (290.1 to 582.4) |
12.8 (8.7 to 17.2) |
9 |
486.7 (328.1 to 658.2) |
13.3 (9.0 to 17.7) |
8 |
1220.8 (825.0 to 1631.3) |
13.4 (9.1 to 17.7) |
8 |
| All risk factors |
284.6 (243.5 to 330.1) |
92.5 (90.0 to 94.7) |
3187.4 (2890.3 to 3480.1) |
94.2 (91.9 to 96.2) |
3416.8 (3070.0 to 3713.7) |
93.3 (90.4 to 95.8) |
8542.4 (7811.7 to 9142.3) |
93.5 (90.8 to 95.9) |
||||
| DALYs | ||||||||||||
| Environmental/occupational risks |
3300.5 (2726.0 to 3891.1) |
44.8 (41.2 to 48.9) |
30721.3 (26771.0 to 34744.1) |
38.7 (35.4 to 41.9) |
20772.7 (17712.1 to 23952.4) |
30.4 (27.2 to 33.8) |
59385.1 (52184.3 to 66601.1) |
32.6 (29.6 to 35.7) |
||||
| Air pollution |
2813.5 (2315.5 to 3335.0) |
38.2 (34.8 to 42.4) |
25012.2 (21855.3 to 28481.5) |
31.5 (28.8 to 34.4) |
15157.3 (12859.2 to 17550.5) |
22.2 (19.6 to 24.7) |
45354.4 (39644.7 to 51231.6) |
24.9 (22.4 to 27.5) |
||||
| Particulate matter pollution |
2813.5 (2315.5 to 3335.0) |
38.2 (34.8 to 42.4) |
25012.2 (21855.3 to 28481.5) |
31.5 (28.8 to 34.4) |
15157.3 (12859.2 to 17550.5) |
22.2 (19.6 to 24.7) |
45354.4 (39644.7 to 51231.6) |
24.9 (22.4 to 27.5) |
||||
| Ambient particulate matter pollution |
601.6 (342.4 to 947.2) |
8.2 (4.7 to 12.6) |
11 |
16464.4 (13034.7 to 19837.8) |
20.7 (16.8 to 24.3) |
6 |
12794.4 (10582.3 to 14939.8) |
18.7 (15.9 to 21.3) |
6 |
32174.3 (26024.8 to 37713.8) |
17.7 (14.7 to 20.3) |
7 |
| Household air pollution from solid fuels |
2211.9 (1672.1 to 2843.7) |
30.0 (24.1 to 36.3) |
3 |
8547.7 (5725.1 to 11894.2) |
10.8 (7.4 to 14.6) |
10 |
2362.9 (1208.0 to 4010.8) |
3.5 (1.8 to 5.9) |
21 |
13180.1 (9051.4 to 18251.8) |
7.2 (5.0 to 9.9) |
12 |
| Suboptimal temperature |
388.1 (218.2 to 523.4) |
5.3 (3.0 to 6.9) |
3990.4 1918.9 5495.2 |
5.0 (2.4 to 6.7) |
4781.8 (3304.4 to 6505.7) |
7.0 (4.8 to 9.4) |
11147.2 (7627.1 to 14343.2) |
6.1 (4.2 to 7.8) |
||||
| High temperature |
47.8 (−96.5 to 105.8) |
0.6 (−1.2 to 1.5) |
26 |
705.5 (−915.8 to 1714.1) |
0.9 (−1.2 to 2.2) |
26 |
157.2 (−86.5 to 330.0) |
0.2 (−0.1 to 0.5) |
26 |
974.0 (−1054.9 to 2209.6) |
0.5 (−0.6 to 1.2) |
26 |
| Low temperature |
341.9 (228.7 to 468.1) |
4.6 (3.2 to 6.1) |
18 |
3312.3 2105.0 4492.3 |
4.2 (2.6 to 5.6) |
21 |
4635.8 (3120.5 to 6410.8) |
6.8 (4.6 to 9.1) |
11 |
10217.6 (7285.5 to 13306.5) |
5.6 (4.1 to 7.2) |
15 |
| Other environmental risks |
425.4 (261.0 to 619.3) |
5.8 (3.6 to 8.1) |
4701.7 2940.5 6647.4 |
5.9 (3.8 to 8.1) |
2757.5 (1509.1 to4281.4) |
4.0 (2.3 to 6.1) |
8368.7 (4896.4 to 12449.2) |
4.6 (2.7 to 6.7) |
||||
| Lead exposure |
425.4 (261.0 to 619.3) |
5.8 (3.6 to 8.1) |
16 |
4701.7 (2940.5 to6647.4) |
5.9 (3.8 to 8.1) |
16 |
2757.5 (1509.1 to 4281.4) |
4.0 (2.3 to 6.1) |
17 |
8368.7 (4896.4 to 12449.2) |
4.6 (2.7 to 6.7) |
18 |
| Behavioral risks |
4784.8 (3921.8 to 5724.2) |
64.9 (57.7 to 71.1) |
54996.6 (48292.3 to 61648.7) |
69.2 (62.8 to 74.3) |
47858.7 (42009.4 to 53511.3) |
70.1 (64.0 to 75.5) |
125894.2 (112086.3 to 139552.4) |
69.2 (63.1 to 74.4) |
||||
| Tobacco |
1403.2 (1172.6 to 1668.1) |
19.0 (17.7 to 20.5) |
20564.6 (18373.1 to 22653.2) |
25.9 (24.5 to 27.2) |
21426.4 (19287.7 to 23852.1) |
31.4 (29.9 to 33.0) |
50725.1 (46709.8 to 54647.3) |
27.9 (26.6 to 29.1) |
||||
| Smoking |
1148.2 (964.4 to 1374.8) |
15.6 (14.5 to 16.8) |
7 |
16962.1 (15179.7 to 18813.4) |
21.4 (20.1 to 22.6) |
5 |
18621.4 (16634.7 to 20751.6) |
27.3 (25.7 to 28.8) |
3 |
43452.8 (40296.9 to 46783.9) |
23.9 (22.8 to 25.0) |
3 |
| Secondhand smoke |
307.9 (231.0 to 392.7) |
4.2 (3.3 to 5.1) |
21 |
4491.7 (3573.1 to 5449.7) |
5.7 (4.6 to 6.8) |
17 |
3854.6 (3089.9 to 4686.1) |
5.6 (4.6 to 6.7) |
14 |
9566.1 (7720.3 to 11527.1) |
5.3 (4.3 to 6.3) |
16 |
| Alcohol use |
−136.9 (−243.4 to −32.4) |
−1.9 (−3.2 to −0.5) |
27 |
−698.2 (−1622.1 to 298.1) |
−0.9 (−2.1 to 0.4) |
27 |
−634.9 (−2086.6 to 792.4 |
−0.9 (−3.0 to 1.1) |
27 |
−2002.9 (−5192.2 to 1210.8) |
−1.1 (−2.9 to 0.7) |
27 |
| Dietary risks |
4213.4 (3296.8 to 5165.6) |
57.2 (48.1 to 65.1) |
46290.8 (38413.0 to 53808.3) |
58.3 (49.0 to 65.5) |
38471.5 (31383.3 to 45528.6) |
56.3 (46.9 to 64.5) |
103864.0 (86829.0 to 120418.9) |
57.1 (47.9 to 64.8) |
||||
| Diet low in fruits |
518.4 (208.4 to 792.6) |
7.0 (2.9 to 10.2) |
12 |
5923.0 (2616.3 to8617.0) |
7.5 (3.3 to 10.7) |
13 |
2717.2 (915.5 to 4311.2) |
4.0 (1.4 to 6.2) |
18 |
10233.4 (4241.4 to 15123.4) |
5.6 (2.3 to 8.2) |
14 |
| Diet low in vegetables |
720.9 (443.5 to 1002.4) |
9.8 (6.2 to 13.3) |
9 |
5119.0 (2810.4 to 7417.4) |
6.4 (3.6 to 9.1) |
15 |
1533.5 (789.5 to 2187.0) |
2.2 (1.2 to 3.3) |
24 |
8383.0 (4666.2 to 11970.2) |
4.6 (2.5 to 6.5) |
17 |
| Diet low in legumes |
975.6 (231.5 to 1654.5) |
13.2 (3.2 to 21.3) |
8 |
11339.7 (2493.7 to 18438.0) |
14.3 (3.2 to 22.9) |
8 |
8260.5 (1689.8 to 13358.6) |
12.1 (2.5 to 19.5) |
10 |
24309.0 (5263.1 to 39575.3) |
13.4 (3.0 to 21.4) |
8 |
| Diet low in whole grains |
1350.1 (513.8 to 1827.9) |
18.4 (6.9 to 24.0) |
5 |
13949.2 (5491.1 to 18410.2) |
17.6 (6.9 to 22.9) |
7 |
12342.6 (4516.7 to 16125.6) |
18.1 (6.6 to 23.4) |
7 |
32206.5 (12173.3 to 41835.0) |
17.7 (6.6 to 23.0) |
6 |
| Diet low in nuts and seeds |
431.7 (226.7 to 615.4) |
5.9 (3.0 to 8.0) |
15 |
6949.0 (3937.4 to 9314.8) |
8.7 (5.0 to 11.6) |
12 |
3753.1 (1692.1 to 5540.0) |
5.5 (2.5 to 7.9) |
15 |
12279.0 (6364.3 to 16919.1) |
6.7 (3.5 to 9.2) |
13 |
| Diet high in processed meat |
105.6 (16.3 to 300.2) |
1.4 (0.2 to 3.9) |
25 |
1226.6 (525.7 to 2397.6) |
1.5 (0.7 to 3.0) |
25 |
1336.9 (223.1 to 2883.4) |
2.0 (0.3 to 4.2) |
25 |
4141.9 (998.6 to 8024.1) |
2.3 (0.6 to 4.4) |
24 |
| Diet high in sugar‐sweetened beverages |
168.0 (127.3 to 216.6) |
2.3 (1.8 to 2.7) |
24 |
1503.0 (993.6 to 1975.7) |
1.9 (1.2 to 2.4) |
24 |
1555.2 (969.0 to 2053.0) |
2.3 (1.5 to 2.9) |
23 |
3973.2 (2470.2 to 5218.8) |
2.2 (1.4 to 2.8) |
25 |
| Diet low in fiber |
316.0 (128.3 to 529.4) |
4.3 (1.7 to 7.2) |
20 |
4429.8 (1985.5 to 7167.9) |
5.6 (2.5 to 8.7) |
18 |
2066.6 (794.0 to 3639.4) |
3.0 (1.2 to 5.2) |
22 |
7943.0 (3373.6 to 12978.3) |
4.4 (1.8 to 7.0) |
20 |
| Diet low in seafood omega‐3 fatty acids |
328.7 (105.9 to 472.3) |
4.5 (1.4 to 6.0) |
19 |
3517.8 (1291.9 to 4779.0) |
4.4 (1.7 to 5.8) |
20 |
2674.9 (1377.4 to 3509.5) |
3.9 (2.0 to 4.9) |
19 |
7409.7 (3373.5 to 9687.0) |
4.1 (1.9 to 5.2) |
23 |
| Diet low in polyunsaturated fatty acids |
396.0 (55.5 to 801.0) |
5.4 (0.7 to 10.8) |
17 |
4391.7 (494.1 to 8939.9) |
5.5 (0.6 to 11.2) |
19 |
2668.7 (327.0 to 5462.1) |
3.9 (0.4 to 8.1) |
20 |
8012.9 (969.2 to 16249.2) |
4.4 (0.5 to 9.0) |
19 |
| Diet high in trans fatty acids |
434.8 (62.8 to 681.0) |
5.9 (0.8 to 8.9) |
14 |
7026.9 (757.7 to 9634.3) |
8.8 (1.0 to 11.8) |
11 |
4442.8 (536.2 to 6299.3) |
6.5 (0.8 to 9.0) |
12 |
14234.2 (1580.4 to 19410.2) |
7.8 (0.9 to 10.5) |
11 |
| Diet high in sodium |
502.1 (56.5 to 1380.9) |
6.8 (0.8 to 18.9) |
13 |
5506.2 (664.7 to 13883.1) |
6.9 (0.9 to 17.4) |
14 |
9534.4 (3583.9 to 17346.5) |
13.9 (5.4 to 25.3) |
8 |
17353.9 (4712.3 to 36861.5) |
9.5 (2.6 to 20.3) |
10 |
| Diet high in red meat |
210.9 (16.0 to 431.0) |
2.8 (0.2 to 5.5) |
23 |
1811.2 (227.0 to 3476.8) |
2.3 (0.3 to 4.3) |
23 |
4041.5 (763.0 to 7352.2) |
5.9 (1.1 to 10.7) |
13 |
7742.3 (1340.0 to 14077.7) |
4.3 (0.7 to 7.6) |
21 |
| Low physical activity |
216.5 (67.2 to 553.9) |
2.9 (0.9 to 7.1) |
22 |
2834.7 (993.2 to 6465.1) |
3.6 (1.2 to 7.9) |
22 |
3044.1 (1062.3 to 6572.4) |
4.5 (1.6 to 9.5) |
16 |
7586.7 (2613.5 to 16747.2) |
4.2 (1.4 to 9.1) |
22 |
| Metabolic risks |
5904.1 (4880.7 to 6982.1) |
80.1 (74.5 to 85.4) |
66864.3 (59824.9 to 74118.4) |
84.2 (79.2 to 88.9) |
57478.9 (51676.0 to 63447.9) |
84.2 (78.7 to 89.3) |
153132.1 (138737.4 to 166795.4) |
84.1 (78.9 to 89.1) |
||||
| High systolic blood pressure |
3913.3 (3136.6 to 4793.8) |
53.1 (46.1 to 60.0) |
1 |
43855.4 (37223.2 to 50863.4) |
55.2 (47.7 to 62.2) |
1 |
37876.8 31625.1 44054.7 |
55.5 (47.2 to 63.4) |
1 |
99397.3 (84594.0 to 114599.3) |
54.6 (46.8 to 61.9) |
1 |
| High LDL cholesterol |
3167.6 (2445.5 to 3988.7) |
43.0 (35.7 to 51.1) |
2 |
36744.1 (29932.5 to 44167.9) |
46.2 (38.6 to 54.3) |
2 |
32561.5 (26484.5 to 39434.1) |
47.7 (39.1 to 56.8) |
2 |
84916.4 (69572.6 to 101382.5) |
46.6 (38.5 to 55.0) |
2 |
| High fasting plasma glucose |
1440.5 (914.6 to 2200.2) |
19.6 (12.3 to 30.1) |
4 |
19480.1 (12178.0 to 29165.7) |
24.5 (15.4 to 36.9) |
3 |
14266.4 (9167.9 to 21592.5) |
20.9 (13.6 to 31.5) |
5 |
43253.3 (27821.4 to 64164.6) |
23.8 (15.3 to 35.8) |
4 |
| High body mass index |
1212.4 (647.1 to 1923.3) |
16.4 (9.2 to 25.1) |
6 |
17398.3 (11114.2 to 24277.4) |
21.9 (14.2 to 30.3) |
4 |
15459.8 (9247.1 to 22706.6) |
22.6 (13.6 to 32.9) |
4 |
41369.8 (26027.7 to 58657.9) |
22.7 (14.6 to 32.0) |
5 |
| Impaired kidney function |
690.0 (467.3 to 943.4) |
9.4 (6.7 to 12.2) |
10 |
9646.1 (6657.7 to 12773.4) |
12.1 (8.5 to 16.0) |
9 |
8606.5 (5994.3 to 11537.3) |
12.6 (8.9 to 16.4) |
9 |
22516.9 (15811.0 to 29665.1) |
12.4 (8.8 to 16.1) |
9 |
| All risk factors |
6851.9 (5826.9 to 7984.3) |
93.0 (91.1 to 94.7) |
75243.9 (68129.9 to 82384.2) |
94.7 (93.1 to 96.1) |
64607.6 (58844.1 to 70173.0) |
94.6 (92.6 to 96.3) |
172100.0 (160171.2 to 184131.0) |
94.5 (92.7 to 96.2) |
||||
DALYs indicates disability‐adjusted life years; IHD, ischemic heart disease; LDL, low‐density lipoprotein; and PAF, population‐attributable fraction. Deaths‐ and DALY‐based PAFs were ranked for 27 individual risk factors at level 4.
The number ranges in parentheses refers to 95% uncertainty intervals of corresponding numbers. *UI: uncertainty interval.
Figure 1. Age‐standardized risk‐attributable death and DALY rates, and male‐to‐female ratio in age‐standardized death and DALY rates for IHD both globally and in low‐ and middle‐income countries from 2000 to 2019.
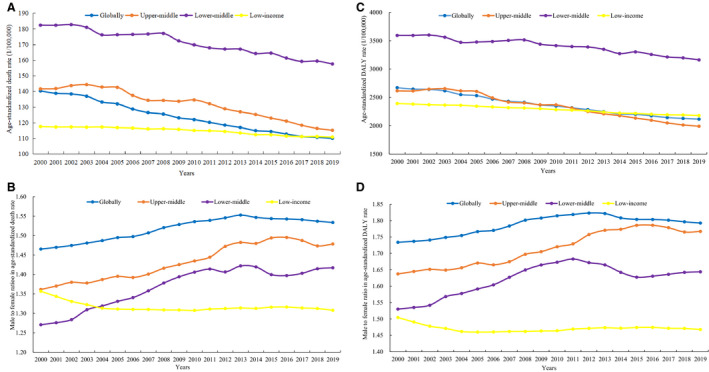
A, Age‐standardized death rate for IHD attributable to all modifiable risk factors (1/100 000) from 2000 to 2019; (B) male‐to‐female ratio in age‐standardized death rate for IHD attributable to all modifiable risk factors from 2000 to 2019; (C) age‐standardized DALY rate for IHD attributable to all modifiable risk factors (1/100 000) from 2000 to 2019; (D) male‐to‐female ratio in age‐standardized DALY rate for IHD attributable to all modifiable risk factors from 2000 to 2019. DALY indicates disability‐adjusted life year; and IHD, ischemic heart disease. Without animals/cells/observations and statistical test.
Country Specific
The PAF (%) of DALYs from overall modifiable risk factors varied from 87.4 (84.1–90.4) in Ethiopia (in LICs) to 97.4 (96.4–98.2) in Iraq (in UMCs) (Table S5). A >13‐fold difference in age‐standardized rates (per 100 000) of attributable deaths and DALYs persisted among the 137 LMICs in 2019, with the lowest rates (44.3; 32.9–57.3 and 786.7; 579.7–1025.2) found in Peru (in UMCs) and the highest (660.4; 588.5–734.1 and 10506.1; 9231.9–11896.1) found in Uzbekistan (in LMCs). The second‐ and third‐leading age‐standardized risk‐attributable rates (per 100 000) occurred in Azerbaijan (in UMCs; 423.2; 370.7–476.8) and Tajikistan (in LICs; 410.2; 349.0–479.8) for mortality, and in Solomon Islands (in LMCs; 10199.5; 8153.9–12273.7) and Nauru (in UMCs; 7946.1; 6402.3–9674.6) for DALYs (Tables S6 and S7).
Age and Sex Specific
In 2019, the proportions of IHD deaths and DALYs attributable to overall risk factors were higher in men than in women among LMICs (Table S8). The largest risk‐attributable proportion of deaths and DALYs was in the 50‐ to 69‐year‐old age group; this was true for LICs, LMCs, and UMCs (Tables S9 and S10). Age‐standardized risk‐attributable death and DALY rates for IHD were much higher among men than women, with the male‐to‐female ratio ranging from 1.31 and 1.47 in LICs to 1.48 and 1.77 in UMCs (Figure 1D; Tables S11 and S12).
Clusters of Risk Factors
Income‐Classified Region
The proportion of IHD deaths and DALYs attributable to risk factors at level 1 varied with income. A cluster of metabolic risk factors was the leading cause of risk‐attributable IHD burden among LMICs, with the proportion in LMCs and UMCs being higher than that in LICs. Environmental risks had a greater impact on IHD deaths and DALYs in LICs (41.7%; 38.1%–45.9% of deaths; 44.8%; 41.2%–48.9% of DALYs) than in LMCs (35.2%; 32.0%–38.2% of deaths and 38.7%; 35.4%–41.9% of DALYs), or UMCs (27.8%; 24.7%–31.0% of deaths and 30.4%; 27.2%–33.8% of DALYs). Conversely, behavioral risk factors accounted for increasingly large proportions of IHD DALYs as income levels increased (Table 1).
PAFs of IHD burden for risk clusters at level 2 showed homogeneity among LMICs, with dietary risks representing the leading behavior risk cluster. The highest proportions of IHD deaths and DALYs attributable to air pollution were observed in LICs (34.6%; 31.2%–39.0% and 38.2%; 34.8%–42.4%, respectively), which were far above the 20.2% (17.9%–22.4%) of deaths and 24.9% (22.4%–27.5%) of DALYs attributable to air pollution at the global level. Among the LMICs, UMCs experienced the largest proportions of deaths and DALYs attributable to tobacco (24.2%; 22.8%–25.8% of deaths and 31.4%; 29.9%–33.0% of DALYs) and low physical activity (5.6%; 2.1%–11.4% of deaths and 4.5%; 1.6%–9.5% of DALYs) (Table 1).
Age and Sex Specific
Age‐ and sex‐specific PAFs of deaths and DALYs showed homogeneity among LMICs. Clusters of environmental, behavioral, and metabolic risk factors accounted for higher proportions of deaths and DALYs in populations aged 25 to 59 years than in those aged ≥70 years, and PAFs for behavioral and metabolic risk factors were substantially greater than environmental risk PAFs across all age groups. In LMICs, the highest PAFs for behavioral risk factors occurred in people aged 35 to 39 years and decreased with age, and this PAF was higher in men than in women in >30‐year‐old age groups. For metabolic risk factors, higher PAFs in men were seen in those aged <44 years. This pattern was reversed after age 45 years in LICs, with a similar turn being observed in the 45‐ to 49‐year‐old age group in LMCs, and in those aged 50 to 54 years in UMCs. Conversely, women aged <49 years had higher PAFs for environmental risk factors in LICs, while in LMCs and UMCs men aged >65 years and >60 years had higher PAFs, respectively (Tables S13–S18).
Individual Risk Factors
Income‐Classified Region
The individual risk factors with the top 3 PAFs (%) for deaths in LICs were high systolic blood pressure (52.4; 44.3–60.3), high LDL cholesterol (37.3; 29.1–46.1), and household air pollution from solid fuels (27.2; 21.8–33.6). In LMCs, the PAFs (%) ranged from −0.9 (−2.0 to 0.2) for alcohol use to 54.8 (46.7–63.2) for high systolic blood pressure. The behavioral risk factor with DALY PAF >20% was smoking in LMCs (21.4%; 20.1–22.6) and UMCs (27.3%; 25.7–28.8). In the dietary risk category, diet low in whole grains accounted for the largest proportion of IHD burden in LMICs, with diet high in processed meat accounting for the lowest (Table 1).
Country Specific
Although the impact of each risk factor varied by country, high systolic blood pressure and high LDL cholesterol remained the 2 leading causes of DALYs among the 137 countries, with the former being the leading risk factor in 116 countries (28 LICs, 37 LMCs, and 51 UMCs), while high LDL cholesterol was the leading cause in the remaining 21 countries (3 LICs, 10 LMCs, and 8 UMCs) (Figure 2A through 2C). There were substantial variations in the impact of a given IHD risk factor on DALYs at the national level. For example, IHD‐caused DALYs attributable to household air pollution from solid fuels were highest in Somalia (in LICs; 46.1%) and were lowest in Jordan (0.0%) (Figures 2A through 2C; Tables S19–S21).
Figure 2. Country‐level proportion of IHD DALYs attributable to 27 individual risk factors in low‐ and middle‐income countries in 2019.
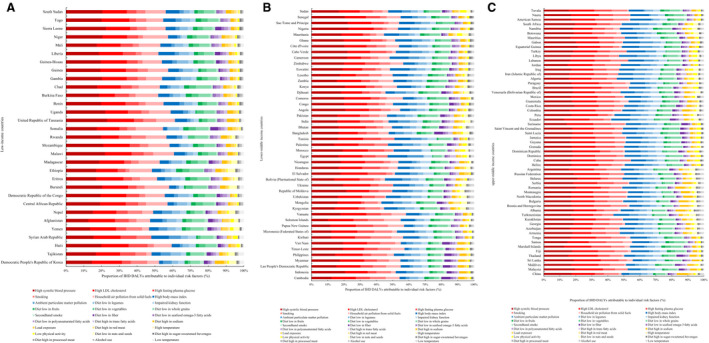
A, Country‐level proportion of IHD DALYs attributable to individual risk factors in low‐income countries; (B) national‐level proportion of IHD DALYs attributable to individual risk factors in lower‐middle income countries; (C) national‐level proportion of IHD DALYs attributable to individual risk factors in upper‐middle‐income countries. DALYs indicates disability‐adjusted life years; and IHD, ischemic heart disease. Without animals/cells/observations and statistical test.
Sex Specific
The PAF rankings of deaths and DALYs for most individual risk factors were similar in both sexes in LMICs. However, PAFs were substantially higher among men for smoking in LMICs, whereas the PAF for household air pollution ranked higher in women than in men in LICs and LMCs (Tables S22–S23).
Temporal Trends in IHD PAF and Attributable Burden From 2000 to 2019
Temporal Trends in PAF Ranks
Death‐based and DALY‐based PAF rankings for individual risk factors at level 4 varied across LMICs during the 2000 to 2019 period. In LICs, household air pollution remained the third risk factor for IHD death and DALYs. Of the 10 leading risks for death and DALYs, metabolic risks rose in rank, whereas environmental and behavioral risks fell from 2000 to 2019 in LMCs. In UMCs, a diet high in sodium was the 10th‐leading risk for death in 2000, and it climbed to the ninth position in 2019. DALYs attributable to high body mass index increased in rank from sixth in 2000 to fifth in 2019 (Table 1).
Temporal Trends in Attributable Age‐Standardized Rates
Income‐Classified Region
From 2000 to 2019, age‐standardized rates for both death and DALYs attributable to modifiable risk factors decreased globally and regionally. There was a 13.6% decrease in the attributable age‐standardized IHD death rate in LMCs, and an 18.7% decrease in UMCs (Figure 1A; Table S3). Similarly, the reduction of the age‐standardized risk‐attributable DALY rate was more prominent in MICs (Figure 1C; Table S4).
Country Specific
Relative changes in age‐standardized risk‐attributable death and DALY rates were spatially heterogeneous. Age‐standardized rates attributable to risk factors declined across most LMICs, with considerable exceptions in certain countries, such as the Dominican Republic (in UMCs), Timor‐Leste (in LMCs), and Tajikistan (in LICs) (Figure 3A and 3B; Tables S6 and S7).
Figure 3. Relative change in risk‐attributable age‐standardized death and DALY rates for IHD in 137 low‐ and middle‐income countries from 2000 to 2019.
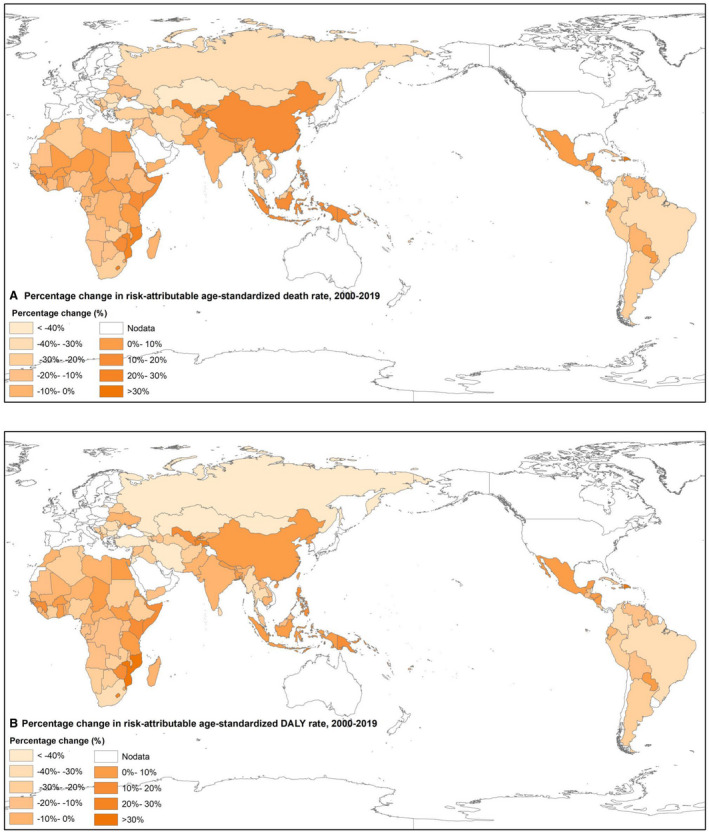
A, Percentage change in attributable age‐standardized death rates; (B) percentage change in attributable age‐standardized DALY rates. DALY indicates disability‐adjusted life year; and IHD, ischemic heart disease. Without animals/cells/observations and statistical test.
Sex Specific
The male‐to‐female ratio of age‐standardized risk‐attributable death and DALY rates for IHD showed an upward trend globally and regionally from 2000 to 2019 (Figure 1B and 1D).
Temporal Trends in Attributable Absolute Deaths and DALYs
Income‐Classified Region
We noticed an increasing trend in deaths and DALYs attributable to IHD risk factors over the periods from 2000 to 2010, 2010 to 2019, and 2000 to 2019, in LMICs as well as globally. From 2000 to 2019, IHD deaths attributable to all risk factors increased by 59.20% in LICs, 64.59% in LMCs, 50.98% in UMCs, and 38.95% worldwide. Compared with 2000 to 2010, a slower annual average increase in attributable deaths and DALYs was observed in UMCs from 2010 to 2019, while LICs and LMCs experienced the opposite trend (Table 2).
Table 2.
Relative Change in Deaths and DALYs for IHD Attributable to all Modifiable Risk Factors Globally and in Low‐ and Middle‐Income Countries From 2000 to 2019
| Regions | Death | DALYs | ||||
|---|---|---|---|---|---|---|
|
% of change (% of annual average change) |
% of change (% of annual average change) |
|||||
| 2000–2019 | 2000–2010 | 2010–2019 | 2000–2019 | 2000–2010 | 2010–2019 | |
| Low‐income | ||||||
| Male | 53.02 (1.23) | 21.15 (1.36) | 26.30 (1.44) | 51.86 (1.23) | 20.36 (1.35) | 26.17 (1.44) |
| Female | 66.98 (1.25) | 30.98 (1.41) | 27.49 (1.45) | 56.90 (1.24) | 24.92 (1.38) | 25.60 (1.43) |
| Both | 59.20 (1.24) | 25.50 (1.38) | 26.85 (1.44) | 53.93 (1.23) | 22.24 (1.36) | 25.93 (1.44) |
| Middle‐income | ||||||
| Lower‐middle | ||||||
| Male | 65.04 (1.25) | 32.41 (1.42) | 24.64 (1.43) | 57.63 (1.24) | 31.13 (1.41) | 20.21 (1.40) |
| Female | 64.00 (1.24) | 25.39 (1.38) | 30.79 (1.46) | 58.33 (1.24) | 24.38 (1.38) | 27.29 (1.44) |
| Both | 64.59 (1.25) | 29.41 (1.40) | 27.18 (1.44) | 57.89 (1.24) | 28.57 (1.40) | 22.81 (1.42) |
| Upper‐middle | ||||||
| Male | 50.47 (1.23) | 30.41 (1.41) | 15.38 (1.35) | 30.37 (1.20) | 19.87 (1.35) | 8.76 (1.27) |
| Female | 51.57 (1.23) | 28.93 (1.40) | 17.56 (1.37) | 29.55 (1.20) | 17.00 (1.33) | 10.73 (1.30) |
| Both | 50.98 (1.23) | 29.72 (1.40) | 16.39 (1.36) | 30.05 (1.20) | 18.73 (1.34) | 9.53 (1.28) |
| Globally | ||||||
| Male | 41.18 (1.22) | 19.28 (1.34) | 18.36 (1.38) | 32.26 (1.20) | 16.39 (1.32) | 13.63 (1.34) |
| Female | 36.34 (1.21) | 13.62 (1.30) | 20.00 (1.39) | 29.69 (1.20) | 11.08 (1.27) | 16.75 (1.37) |
| Both | 38.95 (1.21) | 16.67 (1.32) | 19.09 (1.39) | 31.25 (1.20) | 14.31 (1.30) | 14.82 (1.35) |
DALY indicates disability‐adjusted life years; and IHD, ischemic heart disease.
Country Specific
From 2000 to 2019, most countries experienced an increase in the number of risk‐attributable IHD deaths and DALYs, which was contrary to the decreasing age‐standardized risk‐attributable rates (Tables S24 and S25).
Age and Sex Specific
In LICs and LMCs, the increase in deaths and DALYs attributable to IHD risk factors occurred for all age groups, whereas in UMCs, a decline in deaths and DALYs was observed in the 15‐ to 49‐year‐old age group (Tables S24 and S25). A marked discrepancy in attributable IHD deaths and DALYs was found between the sexes. A greater increase occurred in men in LMCs over the 2000 to 2019 period, while in LICs and UMCs the attributable IHD burden in women experienced opposite increasing trends (Table 2).
Discussion
We conducted a comprehensive and representative analysis of income‐classified region‐, country‐, age‐, and sex‐specific IHD burden attributable to potentially modifiable risk clusters and individual risk factors among LMICs, with special attention paid to the current levels and temporal trends from 2000 to 2019. Our findings highlight the need to reduce the impact of preventable IHD burden in LMICs.
Overall Modifiable Risk Factors
According to the present study, the IHD PAFs (whether for deaths or for DALYs) in relation to all modifiable risk factors combined were consistently high, which were over 90% in LMICs in 2019. With the quantification of the high exposure to IHD risk factors over the life course, cost‐effective public health interventions are expected to be identified in all income settings. Increasing trends of attributable IHD deaths and DALYs in all income‐classified regions from 2000 to 2019 were also observed, which was probably a function of growing and aging populations. 1
The age‐standardized risk‐attributable IHD death and DALY rates have considerably improved in LMICs, which may be related to effective primary healthcare reform, 21 updated medical technology, 22 incremental investment in IHD prevention, 23 and national authorities’ efforts to facilitate environments prioritizing healthcare services. 22 However, the risk‐attributable IHD burden differed across the most affected and the least affected countries, and the gap was found to be growingly wider. From 2010 to 2019, we observed for the first time diverging temporal trends of IHD burden between UMCs and LICs. Some countries with considerably increased IHD burden, such as the Dominican Republic, Timor‐Leste, and Tajikistan, need to reinforce public care interventions for IHD through the reduction of modifiable risk factors.
We found that in LMICs, higher proportions of death and DALYs occurred among populations aged 25 to 59 years, and the high‐risk individuals were younger than those reported in India. 24 The inconsistency in burden estimates may be attributed to the different methods used in the 2 studies. Our findings provided an opportunity to deliver IHD interventions earlier in young adults, with the aim to keep a proper trajectory through the life course.
Risk Factors and Risk Clusters
Our findings showed homogeneity in metabolic risk patterns across regions categorized by income, where the metabolic risk cluster was consistently the predominant risk factor for IHD in LMICs. Furthermore, high blood pressure and high LDL cholesterol were the 2 leading contributors among the 137 countries. The high exposure to metabolic risks may act as a key driver of increasing absolute attributable IHD burden. 1 However, we found that exposure to clusters of environmental and behavioral risk factors was associated with economic development. IHD burden attributable to the cluster of environmental risk factors increased significantly with decreased income levels. Compared with MICs, LICs experienced a larger IHD burden attributable to environmental risk factors, including ambient and household air pollution. The association between environmental risks and IHD mortality can be explained by biological mechanisms. Long‐term exposure to particulate matter is strongly associated with endothelial dysfunction, 25 systematic inflammation, 26 and increased blood pressure, 26 all of which contribute to the morbidity and mortality of IHD. A previous GBD study 13 showed that in high‐income countries, the contribution of air pollution to cardiovascular disease burden consistently decreased. If this trend continues, the discrepancy between high‐income countries and LICs will increase further. For LICs, implementing available interventions to improve environmental management, especially reducing exposure to air pollution from burning coal and other solid fuels, should be the main priority to reduce risk‐attributable IHD burden. 5 , 27
Conversely, the cluster of behavioral risk factors, such as tobacco and low physical activity, denoted an increasing trend with economic development. The joint effects of the 2 risk clusters increased from 2000 to 2019, with high fasting plasma glucose found to be the main contributor in LMCs, and diets high in sodium and high body mass index the main contributors in UMCs. These indicate that managing an increasing IHD burden attributable to behavioral and metabolic risks is anticipated to be an uphill battle for MICs, especially for UMCs. 28 , 29 , 30
Consistent with previous studies, our study revealed that the prevalence of each modifiable risk factor varied across countries classified by economic level, such as high alcohol drinking in Russia, 29 common drug use in South Africa, 31 and high sodium consumption and tobacco use in China, 2 , 32 combined with the widespread rising prevalence of physical inactivity 10 , 33 and suboptimal dietary habits including diets low in nuts, whole grains, fruits, and vegetables. 34 These disparities of the epidemiology of risk factors can be partly explained by inconsistent professional knowledge of prevention and control for IHD, and the varying accessibility and affordability of health care across countries with varying income levels. 3
With respect to the causal relationship between economic status and premature deaths from cardiovascular disease, the PURE (Prospective Urban Rural Epidemiology) study, 5 enrolling 155 722 participants from 21 LICs, MICs, and high‐income countries, suggested that education level was considered the most important socioeconomic factor to avert attributable cardiovascular disease burden. Better access to education in high‐income countries led to healthier behaviors, increased availability of high‐quality health care, and reduced mortality, compared with LMICs. Therefore, increased investments in education in lower‐income countries should be the highest priority to reduce the growing disparities in IHD burden. 35 , 36 , 37 , 38 In addition, extremely low rates of awareness, treatment, and control for hypertension and high LDL cholesterol among LMICs, 39 worldwide population growth and aging, and other socioeconomic, demographic, and cultural factors, had large effects on the geographic discrepancies observed in modifiable risk factors’ epidemiologic transitions across general populations.
Marked differences in risk‐attributable IHD burden were observed between the sexes. Our results suggested that men had notably higher IHD burdens for overall and behavioral risk factors, and experienced a more rapid increase from 2000 to 2019, which can be closely related to more unhealthy lifestyles among men compared with women. 7 For example, the PAF for smoking was notably higher among men in LICs and MICs. To control the risk‐attributable IHD burden, preventive interventions to reduce behavioral risks that targeted men were more effective than interventions targeting women, particularly in LMCs.
As a previous study 40 proposed, a 25% reduction in cardiovascular disease premature deaths by 2025, as advocated for by the United Nations, will be reached only if all modifiable risk factor interventions can be achieved in LMICs. Since the varying prevalence of leading risk factors for IHD has a direct or indirect impact on risks of morbidity and mortality, 5 efficient responses of international and national health systems and cost‐effective interventions should be strengthened among low‐to‐middle‐income countries with restricted access to health care. Furthermore, as the emerging field of mobile health, known as “mHealth,” provides a potential opportunity to deliver public health services to IHD patients, 41 individual‐targeted interventions based on mobile phone technology may be implemented considering that mHealth can effectively monitor and identify risk factors on time. The differences observed in this study call for income‐classified region‐ and country‐specific initiatives to implement interventions that will reduce preventable IHD burden.
Strengths and Limitations
To the best of our knowledge, this is the first timely and comprehensive assessment of IHD deaths and DALYs attributable to potentially modifiable risk factors in 137 LMICs from 2000 to 2019, based on regionally and nationally representative data from the most updated 2019 GBD study. Our income‐classified region‐, country‐, sex‐, and age‐specific findings uncover some valuable insights for informing governments of tailored strategies and programs that can prioritize the primary prevention of IHD. For instance, for certain countries with the highest IHD burden attributable to high blood pressure, it is of utmost importance to promote the nationwide practice of favorable lifestyles and the availability and affordability of guideline‐recommended antihypertensive therapies for patients in the prevention and treatment of IHD 3 . Of note, better guidance in implementing public health interventions suitable to differing economic levels needs to be emphasized to ensure that medical and healthcare services are equally available to manage the risk‐attributable burden. In this way, mitigation of preventable IHD burden should be positioned as a priority agenda by international and national healthcare policy makers in LMICs.
The GBD study has some limitations, which have been described elsewhere. 1 , 15 , 16 , 17 Some of the most important limitations may have affected this study. First, the correlation between attributed prevalence and deaths for IHD brings uncertainties to the calculation of years lived with disability and years of life lost, which leads to decreased precision of attributed DALYs. Second, even though our analysis of IHD burden was conducted using regionally and nationally representative data, we failed to examine subnational discrepancies with available data, which underscores the need to undertake more specific assessments at the state, province, county, urban, or rural level in future studies. Third, with improvements in early diagnostic techniques over the past 2 decades, inconsistencies in diagnostic criteria for IHD over time may cause measurement errors in the data acquisition process. Fourth, even though the TMREL estimates were discussed and approved by international risk factor epidemiologists, evidence of TMREL selection was uncertain for some risk factors, particularly in LICs with limited risk exposure data. For example, the TMREL for LDL cholesterol was set at 0.7 to 1.3 mmol/L, where the risk for IHD associated with cholesterol can be minimized in the general population; however, the discrepancy between the TMREL and the healthy level expected to be targeted after treatment may not have been fully considered. Fifth, country‐level data on many modifiable risk factors were insufficient in some LMICs. National estimation for the IHD prevalence were highly dependent on predictors in the model with unified and standard methodologies of the GBD 2019 study. Results at the country level would be more reliable if the input data limitation was addressed.
Conclusions
In summary, the age‐standardized risk‐attributable rates of death and DALY for IHD showed a decreasing trend among LMICs from 2000 to 2019. However, the considerable increase in absolute number of attributable IHD deaths and DALYs indicates that the overall burden remains high. Substantial heterogeneity was observed in the epidemiologic transition of IHD burden attributable to behavioral, environmental, and metabolic risk factors across LICs, LMCs, and UMCs. Moreover, the discrepancy in risk‐attributable IHD burden between LICs and MICs has increased, with a higher burden attributable to environmental risks in LICs and higher burdens attributable to behavioral and metabolic risk factors in MICs. Our findings can serve as a useful reference to inform targeted strategies that account for economic development at both income‐classified region and country levels.
Sources of Funding
This study was supported by the National Natural Science Foundation of China (81872721) and National Key Research and Development Program of China (2017YFC1310902) to Dr Liu. The funder of the study had no role in the design and conduct of the study, in the collection, analysis, and interpretation of the data, and in the preparation, review, and approval of the manuscript.
Disclosures
None.
Supporting information
Data S1–S2
Tables S1–S25
Figure S1
Acknowledgments
We are grateful to the 2019 Global Burden of Disease Study collaborators for providing the data used in this study.
Supplementary Material for this article is available at https://www.ahajournals.org/doi/suppl/10.1161/JAHA.121.021024
For Sources of Funding and Disclosures, see page 15.
Contributor Information
Chunping Wang, Email: chpwang@wfmc.edu.cn.
Shiwei Liu, Email: shiwei_liu@aliyun.com.
References
- 1. GBD 2019 Risk Factors Collaborators . Global burden of 87 risk factors in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396:1223–1249. doi: 10.1016/S0140-6736(20)30752-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Wong MCS, Zhang DX, Wang HHX. Rapid emergence of atherosclerosis in Asia: a systematic review of coronary atherosclerotic heart disease epidemiology and implications for prevention and control strategies. Curr Opin Lipidol. 2015;26:257–269. DOI: 10.1097/MOL.0000000000000191. [DOI] [PubMed] [Google Scholar]
- 3. Zhao D, Liu J, Wang M, Zhang X, Zhou M. Epidemiology of cardiovascular disease in China: current features and implications. Nat Rev Cardiol. 2019;16:203–212. DOI: 10.1038/s41569-018-0119-4. [DOI] [PubMed] [Google Scholar]
- 4. Abegunde DO, Mathers CD, Adam T, Ortegon M, Strong K. The burden and costs of chronic diseases in low‐income and middle‐income countries. Lancet. 2007;370:1929–1938. DOI: 10.1016/S0140-6736(07)61696-1. [DOI] [PubMed] [Google Scholar]
- 5. Yusuf S, Joseph P, Rangarajan S, Islam S, Mente A, Hystad P, Brauer M, Kutty VR, Gupta R, Wielgosz A, et al. Modifiable risk factors, cardiovascular disease, and mortality in 155 722 individuals from 21 high‐income, middle‐income, and low‐income countries (PURE): a prospective cohort study. Lancet. 2020;395:795–808. DOI: 10.1016/S0140-6736(19)32008-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Lozano R, Fullman N, Abate D, Abay SM, Abbafati C, Abbasi N, Abbastabar H, Abd‐Allah F, Abdela J, Abdelalim A, et al. Measuring progress from 1990 to 2017 and projecting attainment to 2030 of the health‐related Sustainable Development Goals for 195 countries and territories: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392:2091–2138. DOI: 10.1016/S0140-6736(18)32281-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Zhang G, Yu C, Zhou M, Wang L, Zhang Y, Luo L. Burden of Ischaemic heart disease and attributable risk factors in China from 1990 to 2015: findings from the global burden of disease 2015 study. BMC Cardiovasc Disor. 1990;2018:18. DOI: 10.1186/s12872-018-0761-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Shams‐Beyranvand M, Farzadfar F, Naderimagham S, Tirani M, Maracy MR. Estimation of burden of ischemic heart diseases in Isfahan, Iran, 2014: using incompleteness and misclassification adjustment models. J Diabetes Metab Disord. 2014;2017:16. DOI: 10.1186/s40200-017-0294-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Maharani A, Sujarwoto, Praveen D, Oceandy D, Tampubolon G, Patel A. Cardiovascular disease risk factor prevalence and estimated 10‐year cardiovascular risk scores in Indonesia: the SMARThealth extend study. PLoS One. 2019;14:e0215219. DOI: 10.1371/journal.pone.0215219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Silva DAS, Malta DC, Souza MDFM, Naghavi M. Burden of ischemic heart disease mortality attributable to physical inactivity in Brazil. Revista de Saúde Pública. 2018;52:72. DOI: 10.11606/S1518-8787.2018052000413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Dale CE, Fatemifar G, Palmer TM, White J, Prieto‐Merino D, Zabaneh D, Engmann JEL, Shah T, Wong A, Warren HR, et al. Causal associations of adiposity and body fat distribution with coronary heart disease, stroke subtypes, and type 2 diabetes mellitus. Circulation. 2017;135:2373–2388. DOI: 10.1161/CIRCULATIONAHA.116.026560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Sulo G, Igland J, Nygård O, Vollset SE, Ebbing M, Cerqueira C, Egeland GM, Jørgensen T, Tell GS. Trends in the risk of early and late‐onset heart failure as an adverse outcome of acute myocardial infarction: a Cardiovascular Disease in Norway project. Eur J Prev Cardiol. 2017;24:971–980. DOI: 10.1177/2047487317698568. [DOI] [PubMed] [Google Scholar]
- 13. Roth GA, Johnson CO, Abate KH, Abd‐Allah F, Ahmed M, Alam K, Alam T, Alvis‐Guzman N, Ansari H, Ärnlöv J, et al. The burden of cardiovascular diseases among US States, 1990–2016. JAMA Cardiol. 2018;3:375. DOI: 10.1001/jamacardio.2018.0385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Knudsen AK, Allebeck P, Tollånes MC, Skogen JC, Iburg KM, McGrath JJ, Juel K, Agardh EE, Ärnlöv J, Bjørge T, et al. Life expectancy and disease burden in the Nordic countries: results from the Global Burden of Diseases, Injuries, and Risk Factors Study 2017. Lancet Public Health. 2019;4:e658–e669. DOI: 10.1016/S2468-2667(19)30224-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Vos T, Lim SS, Abbafati C, Abbas KM, Abbasi M, Abbasifard M, Abbasi‐Kangevari M, Abbastabar H, Abd‐Allah F, Abdelalim A, et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396:1204–1222. DOI: 10.1016/S0140-6736(20)30925-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Lozano R, Fullman N, Mumford JE, Knight M, Barthelemy CM, Abbafati C, Abbastabar H, Abd‐Allah F, Abdollahi M, Abedi A, et al. Measuring universal health coverage based on an index of effective coverage of health services in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396:1250–1284. DOI: 10.1016/S0140-6736(20)30750-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Wang H, Abbas KM, Abbasifard M, Abbasi‐Kangevari M, Abbastabar H, Abd‐Allah F, Abdelalim A, Abolhassani H, Abreu LG, Abrigo MRM, et al. Global age‐sex‐specific fertility, mortality, healthy life expectancy (HALE), and population estimates in 204 countries and territories, 1950–2019: a comprehensive demographic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396:1160–1203. DOI: 10.1016/S0140-6736(20)30977-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Forouzanfar MH, Afshin A, Alexander LT, Anderson HR, Bhutta ZA, Biryukov S, Brauer M, Burnett R, Cercy K, Charlson FJ, et al. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388:1659–1724. DOI: 10.1016/S0140-6736(16)31679-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Gakidou E, Afshin A, Abajobir AA, Abate KH, Abbafati C, Abbas KM, Abd‐Allah F, Abdulle AM, Abera SF, Aboyans V, et al. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390:1345–1422. DOI: 10.1016/S0140-6736(17)32366-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Institute for Health Metrics and Evaluation (IHME) . GBD results tool. http://ghdx.healthdata.org/gbd‐resultstool. (accessed Jan 20, 2020)
- 21. Schmidt MI, Duncan BB, e Silva GA, Menezes AM, Monteiro CA, Barreto SM, Chor D, Menezes PR. Chronic non‐communicable diseases in Brazil: burden and current challenges. Lancet. 2011;377:1949–1961. DOI: 10.1016/S0140-6736(11)60135-9. [DOI] [PubMed] [Google Scholar]
- 22. Liu S, Li Y, Zeng X, Wang H, Yin P, Wang L, Liu Y, Liu J, Qi J, Ran S, et al. Burden of cardiovascular diseases in China, 1990–2016. JAMA Cardiol. 2019;4:342. DOI: 10.1001/jamacardio.2019.0295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Ribeiro ALP, Duncan BB, Brant LCC, Lotufo PA, Mill JG, Barreto SM. Cardiovascular health in Brazil: trends and perspectives. Circulation. 2016;133:422–433. DOI: 10.1161/CIRCULATIONAHA.114.008727. [DOI] [PubMed] [Google Scholar]
- 24. Zou Z, Cini K, Dong B, Ma Y, Ma J, Burgner DP, Patton GC. Time trends in cardiovascular disease mortality across the BRICS: an age‐period‐cohort analysis of key nations with emerging economies using the Global Burden of Disease Study 2017. Circulation. 2020;141:790–799. DOI: 10.1161/CIRCULATIONAHA.119.042864. [DOI] [PubMed] [Google Scholar]
- 25. Brook RD, Rajagopalan S, Pope CA, Brook JR, Bhatnagar A, Diez‐Roux AV, Holguin F, Hong Y, Luepker RV, Mittleman MA, et al. Particulate matter air pollution and cardiovascular disease: particulate matter air pollution and cardiovascular disease. Circulation. 2010;121:2331–2378. DOI: 10.1161/CIR.0b013e3181dbece1. [DOI] [PubMed] [Google Scholar]
- 26. Corlin L, Woodin M, Hart JE, Simon MC, Gute DM, Stowell J, Tucker KL, Durant JL, Brugge D. Longitudinal associations of long‐term exposure to ultrafine particles with blood pressure and systemic inflammation in Puerto Rican adults. Environ Health‐Glob. 2018;17:33. DOI: 10.1186/s12940-018-0379-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Ostro B, Hu J, Goldberg D, Reynolds P, Hertz A, Bernstein L, Kleeman MJ. Associations of mortality with long‐term exposures to fine and ultrafine particles, species and sources: results from the California Teachers Study Cohort. Environ Health Persp. 2015;123:549–556. DOI: 10.1289/ehp.1408565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Xie X‐X, Zhou W‐M, Lin F, Li X‐Q, Zhong W‐L, Lin S‐G, Li W‐Y, Chen T‐H, Ye Y, Hu X‐J, et al. Ischemic heart disease deaths, disability‐adjusted life years and risk factors in Fujian, China during 1990–2013: data from the Global Burden of Disease Study 2013. Int J Cardiol. 2016;214:265–269. DOI: 10.1016/j.ijcard.2016.03.236. [DOI] [PubMed] [Google Scholar]
- 29. Starodubov VI, Marczak LB, Varavikova E, Bikbov B, Ermakov SP, Gall J, Glenn SD, Griswold M, Idrisov B, Kravchenko M, et al. The burden of disease in Russia from 1980 to 2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2018;392:1138–1146. DOI: 10.1016/S0140-6736(18)31485-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Ezzati M, Obermeyer Z, Tzoulaki I, Mayosi BM, Elliott P, Leon DA. Contributions of risk factors and medical care to cardiovascular mortality trends. Nat Rev Cardiol. 2015;12:508–530. DOI: 10.1038/nrcardio.2015.82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Hamid S, Groot W, Pavlova M. Trends in cardiovascular diseases and associated risks in sub‐Saharan Africa: a review of the evidence for Ghana, Nigeria, South Africa, Sudan and Tanzania. The Aging Male. 2019;22:169–176. DOI: 10.1080/13685538.2019.1582621. [DOI] [PubMed] [Google Scholar]
- 32. Zhang J, Guo X, Lu Z, Tang J, Li Y, Xu A, Lis S. Cardiovascular diseases deaths attributable to high sodium intake in Shandong Province, China. J Am Heart Assoc. 2019;8:e010737. DOI: 10.1161/JAHA.118.010737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Lear SA, Hu W, Rangarajan S, Gasevic D, Leong D, Iqbal R, Casanova A, Swaminathan S, Anjana RM, Kumar R, et al. The effect of physical activity on mortality and cardiovascular disease in 130 000 people from 17 high‐income, middle‐income, and low‐income countries: the PURE study. Lancet. 2017;390:2643–2654. DOI: 10.1016/S0140-6736(17)31634-3. [DOI] [PubMed] [Google Scholar]
- 34. Afshin A, Sur PJ, Fay KA, Cornaby L, Ferrara G, Salama JS, Mullany EC, Abate KH, Abbafati C, Abebe Z, et al. Health effects of dietary risks in 195 countries, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2019;393:1958–1972. DOI: 10.1016/S0140-6736(19)30041-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Sulo E, Nygård O, Vollset SE, Igland J, Ebbing M, Østbye T, Jørgensen T, Sulo G, Tell GS. Time trends and educational inequalities in out‐of‐hospital coronary deaths in Norway 1995–2009: a Cardiovascular Disease in Norway (CVDNOR) Project. J Am Heart Assoc. 2017;6:e005236. DOI: 10.1161/JAHA.116.005236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Skalamera J, Hummer RA. Educational attainment and the clustering of health‐related behavior among U.S. young adults. Prev Med. 2016;84:83–89. DOI: 10.1016/j.ypmed.2015.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Lager ACJ, Torssander J. Causal effect of education on mortality in a quasi‐experiment on 1·2 million Swedes. Proc Natl Acad Sci USA. 2012;109:8461–8466. DOI: 10.1073/pnas.1105839109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Rosengren A, Smyth A, Rangarajan S, Ramasundarahettige C, Bangdiwala SI, AlHabib KF, Avezum A, Bengtsson Boström K, Chifamba J, Gulec S, et al. Socioeconomic status and risk of cardiovascular disease in 20 low‐income, middle‐income, and high‐income countries: the Prospective Urban Rural Epidemiologic (PURE) study. Lancet Glob Health. 2019;7:e748–e760. DOI: 10.1016/S2214-109X(19)30045-2. [DOI] [PubMed] [Google Scholar]
- 39. Yusuf S, Islam S, Chow CK, Rangarajan S, Dagenais G, Diaz R, Gupta R, Kelishadi R, Iqbal R, Avezum A, et al. Use of secondary prevention drugs for cardiovascular disease in the community in highincome, middle‐income, and low‐income countries (the PURE Study): a prospective epidemiological survey. Lancet. 2011;378:1231–1243. DOI: 10.1016/S0140-6736(11)61215-4. [DOI] [PubMed] [Google Scholar]
- 40. Roth GA, Nguyen G, Forouzanfar MH, Mokdad AH, Naghavi M, Murray CJL. Estimates of global and regional premature cardiovascular mortality in 2025. Circulation. 2015;132:1270–1282. DOI: 10.1161/CIRCULATIONAHA.115.016021. [DOI] [PubMed] [Google Scholar]
- 41. O’Shea CJ, McGavigan AD, Clark RA, Chew DPB, Ganesan A. Mobile health: an emerging technology with implications for global internal medicine. Intern Med J. 2017;47:616–619 DOI: 10.1111/imj.13440. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data S1–S2
Tables S1–S25
Figure S1


