Abstract
Background
Online platforms are used to manage aspects of our lives including health outside clinical settings. Little is known about the effectiveness of using online platforms to manage hypertension. We assessed effects of tweeting/retweeting cardiovascular health content by individuals with poorly controlled hypertension on systolic blood pressure (SBP) and patient activation.
Methods and Results
We conducted this 2‐arm randomized controlled trial. Eligibility included diagnosis of hypertension; SBP >140 mm Hg; and an existing Twitter account or willingness to create one to follow study Twitter account. Intervention arm was asked to tweet/retweet health content 2×/week using a specific hashtag for study duration (6 months). The main measures include primary outcome change in SBP; secondary outcome point change in Patient Activation Measure (PAM). We remotely recruited and enrolled 611 participants, mean age 52 (SD, 11.7). Mean baseline SBP for the intervention group was 155.8 and for control was 155.6. At 6 months, mean SBP for intervention group was 137.6 and for control was 135.7. Mean change in SBP from baseline to 6 months for the intervention group was −18.5 and for control was −19.8 (P=0.48). Mean PAM at baseline for the intervention group was 70.3 for control was 72.7. At 6 months, mean PAM scores were 71.1 (intervention) and 75.6 (control). Mean change in PAM score for the intervention group was 0.0 and for control was 3.3 (P=0.12).
Conclusions
Recruiting and engaging patients and collecting outcome measures remotely are feasible using Twitter. Encouraging patients with poorly controlled hypertension to tweet or retweet health content on Twitter did not improve SBP or PAM score at 6 months.
Registration
URL: https://www.clinicaltrials.gov. Unique identifier: NCT02622256.
Keywords: blood pressure, digital health, hypertension, online post, social media, Twitter
Subject Categories: Hypertension, High Blood Pressure, Quality and Outcomes, Coronary Artery Disease
Nonstandard Abbreviations and Acronyms
- EMR
electronic medical record
- PAM
Patient Activation Measure
- SBP
systolic blood pressure
Clinical Perspective
What Is New?
This randomized controlled trial for patients with a diagnosis of hypertension was conducted online via Twitter, prompting intervention participants to tweet health content twice per week.
We demonstrate the feasibility of collecting key clinical outcomes (systolic blood pressures and patient activation measures) via remote methods.
What Are the Clinical Implications?
For patients with a diagnosis of hypertension, Twitter can be a challenging space to influence behavior change to affect clinical outcomes; we did not observe improvement in systolic blood pressure or patient activation measures at 6 months.
Participants are willing to consent remotely to give researchers access to their Twitter handles as well as their medical records.
Future studies could leverage online interventions to foster behavior change by employing robust strategies for increasing online engagement.
Nearly half of all adults in the Unites States have hypertension, and many of these indviduals have poorly controlled blood pressure (BP). Hypertension control is determined by patient activities outside of the clinical encounter such as diet, exercise, and medication adherence. 1 Several approaches (eg, self‐care courses, home telemonitoring) have been evaluated for aiding patients but are often resource intensive and of variable effectiveness. 2 Strategies with targeted text messaging to enhace engagement and self‐management for cardiovascular conditions like diabetes and heart failure, however, have shown promising results for improving clinical and process outcomes. 3 , 4 , 5
Online social media platforms might provide some of the elements of successful targeted approaches to the management of cardiovascular disease. 6 Twitter, for example, enables individuals to receive or generate targeted messaging on an existing messaging platform without associated texting fees or a time‐ and resource‐intensive messaging infrastructure. With more than 300 million active users worldwide each month, 7 the reach of Twitter is considerable. Online social networks can enable better engagement and patient‐to‐patient support for information, advice, skills teaching, active participation, self‐esteem, motivation, and access to groups with similar challenges. 8 , 9
We sought to evaluate if encouraging hypertensive patients to regularly tweet about heart health could improve their systolic blood pressure (SBP) and patient activation to better manage their health.
Methods
Study Design
Deidentified data are available on request. This was a randomized controlled trial, unblinded, with a parallel‐group design. The Penn Heart Study was approved by the University of Pennsylvania Institutional Review Board. The trial was registered with http://www.clinicaltrials.gov (unique identifier: NCT02622256).
Recruitment and Enrollment
Individuals receiving care in primary care clinics at a large urban academic medical center from June 2016 to October 2017 were assessed for eligibility. Eligibility criteria were (1) age ≥21 years, (2) existing diagnosis of hypertension (International Classification of Diseases, Ninth Revision [ICD‐9] diagnostic codes 401, 401.0, 401.1, 401.9, 405, 405.0, 405.1, 405.9), (3) SBP >140 recorded in the electronic medical record (EMR) at a primary care clinic visit in the study time frame, (4) not pregnant, (5) having a Twitter account or willingness to create one for the purposes of the study, and (6) willingness to follow the study (ie, Penn Heart Study) Twitter feed. Lists of potential participants meeting the first 3 criteria were sent to us weekly via data pulls from the Penn Data Store, Penn Medicine’s repository for clinical data. Those patients were then contacted by email and those meeting the other 2 criteria were eligible to enroll. Interested participants provided electronic consent and were randomly assigned 1:1 to either the control or intervention group.
Surveys
Participants in the control and intervention groups were asked to complete a survey at the initiation of the study and a survey 6 months later at the completion of the study. The initial survey included questions about: sociodemographic information, self‐reported BP measures, weight, height, prior diagnoses, medication adherence, social media use, perceived usefulness, and ease of use of technology and the 13 item Patient Activation Measure (PAM). 10 , 11 The PAM is a well‐validated and reliable tool that uses a 100‐point scale as well as levels of activation (levels 1–4) to assess a person’s ability to manage his or her own health. The PAM provides insight into a person’s skills, confidence, and attitudes, specifically those that influence the adoption of healthy behaviors like self‐management of one’s own health care. An activation level of 1 (lowest level of activation) indicates someone who is not engaged with his or her health/healthcare needs, while an activation level of 4 (highest level of activation) indicates someone who has taken control of and advocates for his or her own health. 10 , 11 , 12 The follow‐up survey at 6 months included similar questions about self‐reported BP measures, weight, height, medication adherence, and the 13‐item PAM.
Intervention
Participants in the intervention group were asked to tweet or retweet health‐related content twice per week. They were also asked to use the hashtag “#health” in their posts. “Health” was purposely left undefined and up to each individual’s interpretation. All intervention participants were reminded weekly through email to tweet or retweet. Control participants were only asked to follow the study handle (@PennHeartStudy) on Twitter and to complete the baseline and final surveys.
Characterizing Health‐Related Tweets
Heart health was defined as any tweet mentioning cardiovascular health or coming from a source that provides information on cardiovascular health in the form of recipes, news articles, or other forms of advice. Tweets could be coded to more than 1 category. For example, “Some #hearthealthy options for #SuperBowl2018! Don’t indulge too much! #HeartHealthMonth!,” could be coded as diet/nutrition, heart health, and news (eg, article from the American Heart Association).
Usage of the Twitter Platform
We collected data about the number of tweets for each participant at enrollment and at the completion of the study. Throughout the study period, the research team generated health‐related tweet content for the Penn Heart Study Twitter account to facilitate participant engagement through retweeting and to inspire creation of original content.
Compensation
Participants were compensated with an Amazon gift card for successful completion of both the baseline and final surveys worth a total of $25. Participants who provided a secondary baseline BP measurement by sending in a photograph—in addition to the measurement collected from the EMR—were entered into a raffle to win an Apple Watch.
Outcome Measures
The primary outcome measure was change in SBP from baseline to study completion. As a pragmatic trial, the study used existing data to track outcomes to the extent possible. Initial BP measurements were obtained from the EMR. For the majority of patients, final BP measurements were obtained 5 to 8 months after enrollment from a documented reading in the the EMR. For patients who did not have a documented BP reading in the health system during this 5‐ to 8‐month time period, we requested that patients either meet our team in person for a manual reading or provide a photograph from their mobile phone of the screen showing their BP reading from a home BP cuff, pharmacy machine, or doctor’s office from outside of our health system.
The secondary outcome measure was the difference across arms in pre‐post PAM scores. The PAM‐13 is a reliable and valid scale for assessing patients’ self‐reported confidence, skill, and knowledge for being able to manage their health or chronic conditions. 12 PAM is scored on a scale from 0 to 100, with 100 representing the highest activation level. 10 , 11
Power Analysis
Sample size estimates were based on the ability to detect a 5 mm Hg difference in SBP at 90% power and type I error of 0.05. We planned to enroll ≈240 in each control and intervention group, for a total of 480 participants, accounting for 35% lost to follow‐up for an online Twitter intervention (total up to 648).
Statistical Analysis
The study was designed to detect a 5‐mm Hg change in SBP and as an intent‐to‐treat analysis. We used paired t‐tests to compare the mean difference in SBP between the intervention and control groups. We also conducted a multiple linear regression analysis for change in SBP that included baseline SBP and covariates, which were imbalanced after randomization to improve efficiency of our estimates. The distribution of change in SBP was assessed, and it was not skewed so we did not apply any transformation.
For the analysis of outcome measures, we used a paired t‐test for pre‐post PAM/SBP comparison, while a 2‐sample t‐test was used to compare PAM/SBP (either values at baseline/6‐month, or pre‐post difference) in intervention versus control group. We also used multiple linear regression model to account for additional imbalances in demographic and baseline health characteristics not evenly distributed by arm. All models included a binary indicator for control/intervention group and adjusted for baseline PAM score. Missing 6‐month SBP and PAM scores were multiply imputed respectively, using linear regression adjusted for study arm, participant demographics, baseline body mass index, prior Twitter usage, self‐rate of health, and baseline SBP (or baseline PAM score).
Twitter Data
We collected data about the frequency of tweets for each study participant at the initiation and completion of the study. We also identified the content of tweets for study participants using the Twitter Application Programming Interface, which enables collecting data from the timelines (prior 3200 tweets) of individuals based on their Twitter handle. To characterize what participants in the intervention group were tweeting about during the study time frame, we used the machine learning process of Latent Dirichlet Allocation to categorize tweets by topics. Each topic was then hand coded for themes. A codebook was developed by the research team for this purpose. Research personnel (J.M. and J.S.L.) coded a 10% sample of tweets, with a third reviewer for adjudication. J.M. then coded the remainder of the tweets, for a total of 1646 tweets coded.
We used summary statistics to describe differences in the overall counts and content of tweets during the study time period across the control and intervention groups. For the intervention group, we reported the counts and characterization of tweets with #health or @pennheartstudy that this group was nudged to generate.
Results
From June 2016 to October 2017, we emailed about 14 500 potential participants with a link for a screening survey to assess eligbility. There were 3518 individuals who accessed the screening survey for eligibility; 628 (18%) met the inclusion criteria and were randomized; 17 intervention participants withdrew from the study, leaving 611 (97%) in our final enrolled sample (Figure).
Figure 1. Consolidated Standards of Reporting Trials diagram.
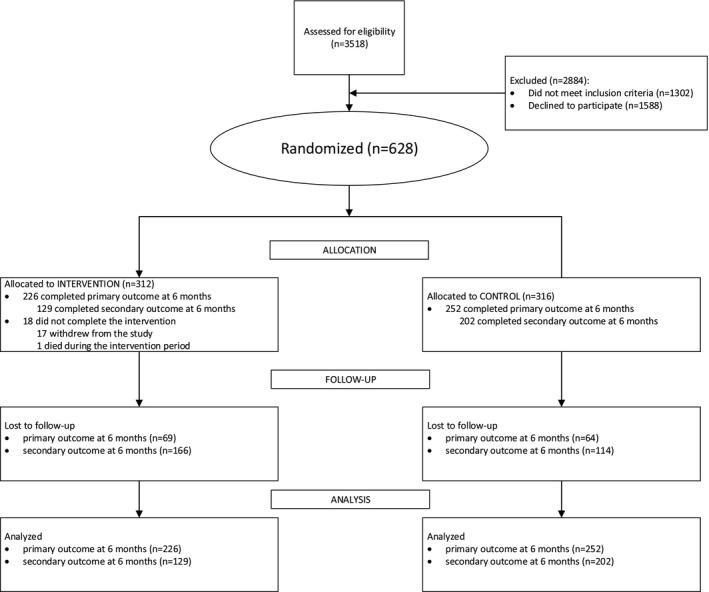
This figure illustrates the study Consolidated Standards of Reporting Trials diagram regarding participant inclusion, exclusion, and outcomes. *The 17 participants who withdrew from the study were in the intervention arm, White (n=16; 94%), and majority men (n=10; 59%).
Participant Demographics
We conducted a 2‐sample t‐test for continuous variables and a chi‐square test for categorical variables. The control and intervention groups had similar demographics (race: White, 60.1% versus 53.9%; Black, 34.2% versus 41.0% [P=0.2318], annual household income: under 50 000, 35.5% versus 37.2%; ≥100 000, 38.3% versus 28.2% [P=0.0201]), although there were more men in the control (47.5%) versus intervention (39.3%) (P=0.0424). Mean ages for both groups was 52.0 (P=0.9801; Table 1).
Table 1.
Patient Demographics and Baseline Clinical Data
| Variable |
Total (n=611) |
Control (n=316) |
Intervention (n=295) |
P Value |
|---|---|---|---|---|
| Sex | 0.0424 | |||
| Male | 266 (43.5) | 150 (47.5) | 116 (39.3) | |
| Female | 345 (56.5) | 166 (52.5) | 179 (39.3) | |
| Other | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
| Race or Ethnicity | 0.2318 | |||
| Asian | 7 (1.1) | 5 (1.6) | 2 (0.7) | |
| Black | 229 (37.5) | 108 (34.2) | 121 (41.0) | |
| Latino/Spanish | 9 (1.5) | 6 (1.9) | 3 (1.0) | |
| Other* or unknown | 17 (2.8) | 7 (2.2) | 10 (3.4) | |
| White | 349 (57.1) | 190 (60.1) | 159 (53.9) | |
| Education | 0.7835 | |||
| College graduate | 328 (53.7) | 172 (54.4) | 156 (52.9) | |
| High school or lower | 71 (11.6) | 34 (10.8) | 37 (12.5) | |
| Some college | 212 (34.7) | 110 (34.8) | 102 (34.6) | |
| Employment status | 0.297 | |||
| Homemaker | 32 (5.2) | 15 (4.7) | 17 (5.8) | |
| Student | 3 (0.5) | 3 (0.9) | 0 (0.0) | |
| Employed | 387 (63.3) | 206 (65.2) | 181 (61.4) | |
| Out of work | 80 (13.1) | 36 (11.4) | 44 (14.9) | |
| Retired | 109 (17.8) | 56 (17.7) | 53 (18.0) | |
| Annual household income | 0.0201 | |||
| ≥$100 000 | 188 (33.3) | 111 (38.3) | 77 (28.2) | |
| $50 000–$99999 | 171 (30.3) | 76 (26.2) | 95 (34.7) | |
| <$50000 | 205 (36.3) | 103 (35.5) | 102 (37.2) | |
| Missing | 47 (7.7) | 26 (8.2) | 21 (7.1) | |
| US residence | 0.3335 | |||
| No | 1 (0.2) | 1 (0.3) | 0 (0.0) | |
| Yes | 610 (99.8) | 315 (99.7) | 295 (100) | |
| State of residence | 0.0167 | |||
| Pennsylvania | 495 (81.1) | 247 (78.4) | 248 (84.1) | |
| New Jersey | 97 (15.9) | 53 (16.8) | 44 (14.9) | |
| Other | 18 (3.0) | 15 (4.8) | 3 (1.0) | |
| Missing | 1 (0.2) | 1 (0.3) | 0 (0.0) | |
| Self‐rating of health | 0.0452 | |||
| Fair | 223 (36.5) | 113 (35.8) | 110 (37.3) | |
| Good | 293 (48.0) | 160 (50.6) | 133 (45.1) | |
| Poor | 44 (7.2) | 17 (5.4) | 27 (9.2) | |
| Very good | 43 (7.0) | 25 (7.9) | 18 (6.1) | |
| Very poor | 8 (1.3) | 1 (0.3) | 7 (2.4) | |
| Prior Twitter Use | 0.3954 | |||
| No | 199 (32.6) | 98 (31.0) | 101 (34.2) | |
| Yes | 412 (67.4) | 218 (69.0) | 194 (65.8) | |
| Age, y, mean (SD) | 52.0 (11.7) | 52.0 (12.2) | 52.0 (11.2) | 0.9801 |
| BMI, mean (SD) | 34.3 (9.3) | 33.6 (8.5) | 35.0 (10.0) | 0.0624 |
Other indicates self‐reported races or ethnicities not included in Asian, Black, Latino/Spanish, White.
Primary Outcome Measure
At baseline the mean SBP was 155.6 mm Hg (SD, 12.5) for control and 155.8 mm Hg (SD, 11.8) for intervention (P=0.85). At 6 months the SBP was 135.7 mm Hg (SD, 16.9) for control and 137.6 mm Hg (SD, 18.3) for intervention (P=0.23). The change in SBP for control compared with intervention was −19.8 (SD, 19.3) and −18.5 (SD, 20.4) respectively (P=0.48). No statistically significant results were found for subgroup analyses presented in the methods, including those using imputed data (Table 2). Imputed data show a mean change in 6‐month SBP of −19.6 (SD, 22.0) for control and −18.4 (SD, 23.1) for intervention (P=0.52; Table 2). Controlling for demographics, clinical data, and prior Twitter use, in the logistic regression model there were no statistically significant differences in the 6 month outcomes of SBP (estimate 1.23 [−2.081 to 4.55 CI]; P value 0.46; Table 3).
Table 2.
Unadjusted Comparison of Systolic Blood Pressure (mm Hg) and the Patient Activation Measure (Paired t‐test)
| Measures | Control | Intervention | Total | P value |
|---|---|---|---|---|
| Systolic blood pressure at baseline, mean (SD) | 155.6 (12.5) | 155.8 (11.8) | 155.7 (12.1) | 0.8526 |
| Systolic blood pressure at 6 months, mean (SD) | 135.7 (16.9) | 137.6 (18.3) | 136.6 (17.6) | 0.2259 |
| Change in systolic blood pressure at 6 months, mean (SD) | −19.8 (19.3) | −18.5 (20.4) | −19.2 (19.8) | 0.4836 |
| Imputed systolic blood pressure at 6 months, mean (SD) | 135.9 (19.9) | 137.3 (21.5) | 136.6 (20.6) | 0.4172 |
| Change in imputed systolic blood pressure at 6 months SBP change, mean (SD) | −19.6 (22.0) | −18.4 (23.1) | −19.0 (22.5) | 0.5184 |
| Patient activation measure at baseline, mean (SD) | 72.7 (16.9) | 70.3 (19.0) | 71.6 (18.0) | 0.1063 |
| Patient activation measure at 6 months, mean (SD) | 75.6 (16.3) | 71.1 (17.2) | 73.8 (16.8) | 0.0185 |
| Change in patient activation measure at 6 months, mean (SD) | 3.3 (17.4) | 0.0 (20.7) | 2.0 (18.8) | 0.1244 |
| Imputed patient activation measure at 6 months, mean (SD) | 76.4 (23.6) | 70.5 (23.0) | 73.6 (24.2) | 0.0017 |
| Change in imputed patient activation measure at 6 months, mean (SD) | 3.7 (24.5) | 0.2 (25.4) | 2.0 (25.7) | 0.0739 |
Table 3.
Linear Regression Model, Using Imputed Data (Dependent Variable: 6‐Month Systolic Blood Pressure)
| Parameter | Estimate | 95% CI | P Value | |
|---|---|---|---|---|
| Lower CI | Upper CI | |||
| Intervention (systolic blood pressure, 6 months) | 1.232133 | −2.0811 | 4.5454 | 0.4647 |
| Control (systolic blood pressure, 6 months) | 0 | 0 | 0 | |
| Systolic blood pressure, baseline | 0.216799 | 0.0759 | 0.3577 | 0.0027 |
| Prior Twitter use | −0.290123 | −3.8548 | 3.2746 | 0.8727 |
| Age, y | 0.027516 | −0.1635 | 0.2186 | 0.7763 |
| Sex, female | −3.335682 | −6.6668 | −0.0046 | 0.0497 |
| Race | ||||
| White | 3.100162 | −4.3841 | 10.5844 | 0.4156 |
| Black | 1.647906 | −6.1538 | 9.4496 | 0.6774 |
| Education | ||||
| Some college | 1.555525 | −4.0542 | 7.1653 | 0.5858 |
| College graduate | −3.310729 | −9.2682 | 2.6467 | 0.2747 |
| High school or lower | 0 | 0 | 0 | |
| Employment | ||||
| Employed | 3.879312 | −1.1799 | 8.9385 | 0.1325 |
| Out of work | −0.438809 | −6.6126 | 5.735 | 0.889 |
| Homemaker | 2.487147 | −5.8429 | 10.8172 | 0.5578 |
| Student | 5.990098 | −19.2372 | 31.2174 | 0.64 |
| Retired | 0 | 0 | 0 | |
| Income | ||||
| Unknown | 0.074826 | −6.3253 | 6.475 | 0.9817 |
| ≥$100 000 | 0.685239 | −4.8065 | 6.177 | 0.8057 |
| $50 000–$99 999 | −0.155039 | −4.7828 | 4.4727 | 0.9475 |
| <$50 000 | 0 | 0 | 0 | |
| Self‐reported health, self‐rated health, 1 question (SF1) | ||||
| Good | 1.522865 | −2.237 | 5.2827 | 0.4262 |
| Poor | 2.958378 | −3.1329 | 9.0496 | 0.341 |
| Very good | −0.180965 | −7.2881 | 6.9261 | 0.9601 |
| Very poor | 15.131475 | −1.5053 | 31.7682 | 0.0742 |
| Fair | 0 | 0 | 0 | |
| Body mass index | 0.093006 | −0.0796 | 0.2656 | 0.2907 |
Secondary Outcome Measure
The secondary outcome measure was the PAM‐13, which was on a scale from 0 to 100, with 100 representing the highest activation level for health management. 10 , 11 At baseline the mean PAM score was 72.7 (SD, 16.9) for the control group and for the intervention was 70.3 (SD, 19.0) (P=0.11). At 6 months the control PAM was 76.4 (SD, 23.6) and the intervention PAM was 70.5 (SD, 23; P=0.002). The mean change in PAM for control compared with intervention was 3.7 (SD, 24.5) and 0.2 (SD, 25.4), respectively (P=0.12). No statistically significant results were found for subgroup analyses, including those using imputed data (Table 2). Imputed data show a mean change in 6‐month PAM of 3.7 (SD, 24.5) for control and 0.2 (SD, 25.4) for intervention (P=0.07; Table 2). Controlling for demographics, clinical data, and prior Twitter use, in the logistic regression model there were no statistically significant differences in the 6‐month PAM scores (Table 4).
Table 4.
Linear Regression Model, Using Imputed Data (Dependent Variable: 6‐month Patient Activation Measure Score)
| Parameter | Estimate | 95% CI | P Value | |
|---|---|---|---|---|
| Lower CI | Upper CI | |||
| Intervention (Patient Activation Measure score) | −5.078008 | −8.5995 | −1.55654 | 0.0052 |
| Control (Patient Activation Measure) | 0 | 0 | 0 | |
| Patient Activation Measure, baseline | 0.327371 | 0.2168 | 0.43794 | <0.0001 |
| Prior Twitter use | 0.079464 | −3.6582 | 3.81717 | 0.9664 |
| Age | −0.214689 | −0.4264 | −0.00293 | 0.047 |
| Sex, female | 3.555223 | −0.6404 | 7.75087 | 0.0952 |
| Race | ||||
| White | 3.880341 | −7.0513 | 14.81203 | 0.4767 |
| Black | 1.870976 | −9.1713 | 12.9133 | 0.7332 |
| Education | ||||
| Some college | 1.830316 | −3.77 | 7.43064 | 0.5189 |
| College graduate | −1.333709 | −7.3367 | 4.66931 | 0.6603 |
| High school or lower | 0 | 0 | 0 | |
| Employment | ||||
| Employed | −3.080747 | −8.4087 | 2.24716 | 0.254 |
| Out of work | −5.483832 | −12.6144 | 1.64674 | 0.1297 |
| Homemaker | −8.649631 | −17.5633 | 0.26404 | 0.057 |
| Student | −16.737641 | −46.0606 | 12.58533 | 0.2574 |
| Retired | 0 | 0 | 0 | |
| Income | ||||
| Unknown | −0.658108 | −6.5662 | 5.25 | 0.8267 |
| ≥$100 000 | −1.83095 | −6.8688 | 3.20691 | 0.4733 |
| $50 000–$99 999 | −1.282237 | −6.4559 | 3.89147 | 0.6225 |
| <$50 000 | 0 | 0 | 0 | |
| Self‐reported health, self‐rated health, 1 question (SF1) | ||||
| Good | 2.994807 | −1.6391 | 7.62876 | 0.2007 |
| Poor | −1.276883 | −8.5703 | 6.01653 | 0.7285 |
| Very good | 7.198015 | −0.2161 | 14.6121 | 0.0569 |
| Very poor | −6.03759 | −22.0403 | 9.96515 | 0.4545 |
| Fair | 0 | 0 | 0 | |
| Body mass index | −0.047398 | −0.2365 | 0.14173 | 0.6205 |
Twitter Use and Tweeting Behavior
Participants’ use of Twitter before the study was similar in the control and intervention groups. A total of 218 (69%) control participants were prior Twitter users compared with 194 (66%) in the intervention group, while 98 (31%) control participants and 101 (34%) intervention participants were not Twitter users before their enrollment in the study (P=0.39; Table 4). We identified the number of followers at baseline as a measure of Twitter use, with 12 as the median number of followers. A sensitivity analysis showed no difference in SBP between the control and intervention arms at 6 months when controlling for the number of followers at baseline (low defined as n=12) or below the median for the sample versus high (above the median [n=12] for the sample) (P=0.118; Table 4). Intervention participants had a total of 30 675 tweets (average,157.3) during the 6‐month study period, while control participants had a total of 12 841 tweets (average, 60.9) during the same period. The intervention group posted 1646 tweets about health using the study‐assigned hashtag (#health) and/or demarcation (@PennHeartStudy). These tweets included themes such as news (731; 44%), diet/nutrition (565; 34%), and heart health (357; 22%; Table 5).
Table 5.
Tweet Content and Frequency of Themes
| Tweet Themes |
No. of Tweets* n (1646) |
Example Tweets and Retweets |
|---|---|---|
| Diet/Nutrition | 565 (34%) |
1. RT @[ ]: Add some green to your diet with some delicious #avocados! 2. My grandmom would put a ham bone in water and make soup. #health curious about this. |
| Exercise | 227 (14%) |
1. RT @[ ]: Grab a friend or family member and help each other meet your fitness goals! #exercise #HealthyLiving 2. #health getting in shape hurts,but it’s worth it |
| Heart health | 357 (22%) |
1.RT @[ ]: Some #hearthealthy options for #SuperBowl2018! Don’t indulge too much! #HeartHealthMonth 2. @[ ]I’m keeping a positive mind for a healthier heart |
| Hypertension | 97 (6%) |
1.RT @[ ]: Interesting article! It’s important to monitor your #BloodPressure and to take care of your #teeth! #HealthyLiving #hy 2. Take a walk everyday to help with your blood pressure #health! |
| Diabetes | 123 (7%) |
1.RT @[ ]: Keep active in any way that you can & check for symptoms of prediabetes! #diabetes #exercise 2. @[ ] After stopping the predisone, I’ve lost 5 lbs in a week! #diabetes |
| Stroke | 48 (3%) |
1.RT @[ ]: You can prevent a #stroke! Learn how and know your #Risk! 2. RT @[ ]: Alexa can now help you perform CPR and help you recognize signs for #heartattack and #stroke! https://t.co/Rmjn9tSshe |
| News | 731 (44%) |
1.RT @[ ]: Some news from the NIH helping us all to eat #healthy food portions; a great way to stay #hearthealthy! 2. 5 Activities Can Cause Neck and Shoulder Pain – Penn Medicine https://t.co/hKcTbWQ3c2? #health #p[ ] |
| Risk factors | 21 (1%) |
1. RT @[ ]: Protect your liver! Learn more about how to detect risks for certain liver issues! #Knowledgeispower https://t.co/z3tBnv 2. RT @[ ]: A good excuse to eat chocolate today! Nutrients in cocoa beans can improve heart disease risk factors! #heartdisease #c |
| Motivation | 33 (2%) |
1.RT @[ ]: Optimism is good for your health!! #PositiveVibes #positivity 2. RT @[ ]: Actions speak louder than words is a good motto to live by. Act in accordance with what you say. #FridayFeeling https |
| PHI* | 35 (2%) |
1. @[ ] My bp is 127/74. Hooray 2. @[ ] I received my transplanted heart on [ ]. So I will be celebrating my 7th year out in a couple of days. Yeh! |
| Mental health | 76 (5%) |
1. RT @[ ]: #mentalhealth is also very important to keep track of! There's never any shame in seeking assistance for mental health 2.I’ve been experiencing a lot of this lately. Important info on how #stress affects #health and what to do about it |
| Politics | 6 (.4%) |
1.RT @LPNational: How #Obamacare Is Fueling America’s #Opioid Epidemic \n #health #drugwar #ACA #healthcare #OpioidEpid 2.TAKE ACTION! Tell Congress to Shift Farm Bill Subsidies to Healthy Foods! #FarmBill #Health |
PHI indicates protected health information.
Tweets could contain more than 1 theme.
Discussion
We sought to evaluate how encouraging active use of a social media platform to post about health‐related topics would impact health outcomes of patients with a chronic health condition. The primary finding of this study is that we did not observe a change in BP readings of participants with poorly controlled hypertension who engaged in the study. Our study results of declines in BP for both groups may reflect the observer effect phenomenon. The BP reduction in both arms could be the result of observation or may be regression to the mean. We also did not observe that nudging individuals to post on social media had a significant impact on their reported patient activation.
This study evaluates social media for both its efferent and afferent pathways—how it can be used for generating information and influencing behaviors. There is considerable evidence that letting people know what other people do is one of the most effective ways of increasing that behavior. 13 This social norming of behaviors is facilitated through online “sharing”—enabling others to model behavior against broader groups whose actions would have been invisible and therefore uninfluential without these new media channels. For individuals with chronic illnesses, automated self‐management support (eg, mobile health) and online communities have been shown to improve clinical outcomes, patient satisfaction, and reduce healthcare costs and usage. 3 , 14
There may have been several factors contributing to the stability of SBP and PAM measures across control and intervention groups. The study population was older than the average Twitter user, and they may not have engaged as readily. The mean age of our participants was 52, but the highest percentage of Twitter users is in the 18‐to‐29 age group. 15 Compared with Facebook and Instagram, Twitter is used less frequently for research; however, Twitter has considerable benefits because the content is generally public and more observable for tracking an intervention and mediators of an intervention. 15 An additional challenge is that an estimated 40% of Twitter is made up of observers or users who infrequently tweet and primarily use the platform to consume information. 16
Although the study did not demonstrate differences in the a priori determined clinical outcome, we were able to successfully execute the study design using several notable remote approaches that could have relevance for future studies using social media platforms. We were able to remotely recruit over 600 participants and obtain their consent to collect both social media and health record data. Study participants generated ≈1646 tweets over 6 months that were shared with our research team and could be used to understand knowledge, beliefs, and attitudes about health‐related information in the study population. We were also able to nudge many of the participants to proactively tweet about health‐related topics. Although separate from the focus of this study, understanding how patients share, interact, and respond to online information can inform how to design future studies that are conducted in social media environments.
Limitations
The study design was intended to be pragmatic and model real‐world use of social media, but this approach may have had an impact on compliance with the intended intervention. We did not provide any additional nudges throughout, and although a weekly reminder was useful, participants may have needed feedback on how their tweets were being received. Tweeting into a vacuum with little engagement may have had an impact on sustainability. Our intervention required sustained use of Twitter over 6 months, yet Twitter use and engagement can be episodic. In addition, because of limitations in accessing the full outpatient health records of participants, we were not able to assess when participants were initially diagnosed with hypertension and the effect that medication adherence could have had on our participants’ management of their hypertension throughout the study. We observed that only 48% (142/295) of our intervention participants tweeted or retweeted during the 6‐month study period as encouraged, and so the actual impact of regular tweeting about health may not have been fully actualized. Creating de novo content requires a certain amount of inertia, and prior work shows that individuals more often engage on social media as passive consumers. Ninety percent of social media users are lurkers (passive consumers), 9% occasionally contribute content, and only 1% account for most of the content according to the 90‐9‐1 principle. 17 Another reason we may have observed no change in BP or PAM may be that retweeting is a passive form of knowledge dissemination on Twitter, and the chosen hashtag was specifically generic.
Conclusions
This study was conducted to evaluate if regularly tweeting about health could improve BP and patient activation over 6 months. Although we did not demonstrate differences in the primary or secondary outcome, we were able to demonstrate that patients were willing to share access to all of their Twitter data and EMR with researchers and post online about health. There may be other forms of online engagement (eg, Twitter chats) that would have allowed for more connectivity of our research team with study participants and study participants with others who have shared interests online. Our findings can inform future work focused on better understanding the ways in which people with hypertension use Twitter to share information about health and for future interventions looking to influence behavior change and improve health outcomes using emerging digital platforms.
Sources of Funding
This work was supported by the NIH/NHLBI (Twitter and Cardiovascular Health R01: HL122457‐01A1).
Disclosures
Dr Merchant reports research funding (NIH R01 122457). Dr Asch has received research funding from NIH; owns stock in Berkshire Hathaway; is a partner in and part owner of VAL Health; and has received compensation and/or travel support for speaking, writing, or consulting from the following organizations: AFYA, MTS Health Partnership, Children’s Hospital of Philadelphia, University of Virginia, Salzburg Global Seminars, GSK, JFK Health System, Cosmetic Boot Camp, Meeting Designs, Capital Consulting, Healthcare Financial Management Association, Joslin Diabetes Center, National Academy of Medicine, the Commonwealth Fund, Massachusetts Medical Society, Endocrine Society, Osteoarthritis Research Society International, Baystate Medical Center, Weill‐Cornell Medical College, Association of American Medical Colleges, TED MED, National Alliance of Health Care Purchaser Coalitions, Deloitte, Harvard University, American Association for Physician Leadership, Brandeis University, University of Rochester, Partner’s Health Care System, John Dolan Lectureship, Johns Hopkins University, and MITRE. The remaining authors have no disclosures to report.
Acknowledgments
We would like to thank research assistants Jonathan Muruako, Joon‐Sub Lee, and Justine Marks for their assistance with coding of tweet themes.
For Sources of Funding and Disclosures, see page 10.
References
- 1. Asch DA, Muller RW, Volpp KG. Automated hovering in health care–watching over the 5000 hours. N Engl J Med. 2012;367:1–3. doi: 10.1056/NEJMp1203869 [DOI] [PubMed] [Google Scholar]
- 2. Schechter CB, Cohen HW, Shmukler C, Walker EA. Intervention costs and cost‐effectiveness of a successful telephonic intervention to promote diabetes control. Diabetes Care. 2012;35:2156–2160. doi: 10.2337/dc12-0048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Nundy S, Razi RR, Dick JJ, Smith B, Mayo A, O'Connor A, Meltzer DO. A text messaging intervention to improve heart failure self‐management after hospital discharge in a largely African‐American population: before‐after study. J Med Internet Res. 2013;15:e53. doi: 10.2196/jmir.2317 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Quinn CC, Shardell MD, Terrin ML, Barr EA, Ballew SH, Gruber‐Baldini AL. Cluster‐randomized trial of a mobile phone personalized behavioral intervention for blood glucose control. Diabetes Care. 2011;34:1934–1942. doi: 10.2337/dc11-0366 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Krishna S, Boren SA, Balas EA. Healthcare via cell phones: a systematic review. Telemed J E Health. 2009;15:231–240. doi: 10.1089/tmj.2008.0099 [DOI] [PubMed] [Google Scholar]
- 6. Sinnenberg L, DiSilvestro CL, Mancheno C, Dailey K, Tufts C, Buttenheim AM, Barg F, Ungar L, Schwartz H, Brown D, et al. Twitter as a potential data source for cardiovascular disease research. JAMA Cardiol. 2016;1:1032–1036. doi: 10.1001/jamacardio.2016.3029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Twitter . Number of monthly active twitter users worldwide from 1st quarter 2010 to 1st quarter 2019 (in millions). Statista Web site. https://www.statista.com/statistics/282087/number‐of‐monthly‐active‐twitter‐users/. Accessed August 6, 2021
- 8. O'Connor A, Jackson L, Goldsmith L, Skirton H. Can I get a retweet please? Health research recruitment and the Twittersphere. J Adv Nurs. 2014;70:599–609. doi: 10.1111/jan.12222 [DOI] [PubMed] [Google Scholar]
- 9. Sinnenberg L, Buttenheim AM, Padrez K, Mancheno C, Ungar L, Merchant RM. Twitter as a tool for health research: a systematic review. Am J Public Health. 2017;107:e1–e8. doi: 10.2105/AJPH.2016.303512 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Patient activation measure (PAM) . Insignia Health Web site. https://www.insigniahealth.com/products/pam‐survey. Accessed August 6, 2021.
- 11. Davis FD. Perceived usefulness, perceived ease of use, and user acceptance of information technology. MIS Quarterly. 1989;13:319–340. doi: 10.2307/249008 [DOI] [Google Scholar]
- 12. Hibbard JH, Mahoney ER, Stockard J, Tusler M. Development and testing of a short form of the patient activation measure. Health Serv Res. 2005;40:1918–1930. doi: 10.1111/j.1475-6773.2005.00438.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Cialdini RB. Harvard Business Review. Harnessing the science of persuasion. Harvard Business Review online. https://hbr.org/2001/10/harnessing‐the‐science‐of‐persuasion. Published October 2001. Accessed August 6, 2021.
- 14. Nundy S, Mishra A, Hogan P, Lee SM, Solomon MC, Peek ME. How do mobile phone diabetes programs drive behavior change? Evidence from a mixed methods observational cohort study. Diabetes Educ. 2014;40:806–819. doi: 10.1177/0145721714551992 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Smith A, Pew AM. Research Center . Social media use in 2018. Pew Research Internet and Technology newsletter. 2018: Published online March 1. http://www.pewinternet.org/2018/03/01/social‐media‐use‐in‐2018/.
- 16. Pickering B, Huffington Post . 10 Types of Twitter Users. HuffPost online. http://www.huffingtonpost.com/ben‐pickering/types‐of‐twitter‐users_b_4208702.html. Published online November 3, 2013; updated December 6, 2017. Accessed January 1, 2020.
- 17. van Mierlo T. The 1% rule in four digital health social networks: an observational study. J Med Internet Res. 2014;16:e33. doi: 10.2196/jmir.2966 [DOI] [PMC free article] [PubMed] [Google Scholar]


