Abstract
Background
Fibromuscular dysplasia (FMD) is a nonatherosclerotic arterial disease that has a variable presentation including pulsatile tinnitus (PT). The frequency and characteristics of PT in FMD are not well understood. The objective of this study was to evaluate the frequency of PT in FMD and compare characteristics between patients with and without PT.
Methods and Results
Data were queried from the US Registry for FMD from 2009 to 2020. The primary outcomes were frequency of PT among the FMD population and prevalence of baseline characteristics, signs/symptoms, and vascular bed involvement in patients with and without PT. Of 2613 patients with FMD who were included in the analysis, 972 (37.2%) reported PT. Univariable analysis and multivariable logistic regression were performed to explore factors associated with PT. Compared with those without PT, patients with PT were more likely to have involvement of the extracranial carotid artery (90.0% versus 78.6%; odds ratio, 1.49; P=0.005) and to have higher prevalence of other neurovascular signs/symptoms including headache (82.5% versus 62.7%; odds ratio, 1.82; P<0.001), dizziness (44.9% versus 22.9%; odds ratio, 2.01; P<0.001), and cervical bruit (37.5% versus 15.8%; odds ratio, 2.73; P<0.001) compared with those without PT.
Conclusions
PT is common among patients with FMD. Patients with FMD who present with PT have higher rates of neurovascular signs/symptoms, cervical bruit, and involvement of the extracranial carotid arteries. The coexistence of the 2 conditions should be recognized, and providers who evaluate patients with PT should be aware of FMD as a potential cause.
Keywords: cerebrovascular dissection, fibromuscular dysplasia, pulsatile tinnitus, vasculopathy
Subject Categories: Vascular Disease, Peripheral Vascular Disease
Fibromuscular dysplasia (FMD) is a noninflammatory, nonatherosclerotic arterial disease that can affect most arteries and result in stenoses, aneurysm, dissection, or arterial tortuosity. 1 , 2 , 3 Clinical manifestations are variable and include several neurologic manifestations. 4 , 5 , 6 , 7 Tinnitus is the conscious perception of auditory sensation in the absence of corresponding external stimuli and has been described in 10% to 15% of the general population. 8 Pulsatile tinnitus (PT) is a swooshing/whooshing sound that is synchronous with the heartbeat. While PT has been described in patients with FMD, 4 , 5 reports have been limited. The aims of this study were to report the frequency of PT in patients enrolled in the US Registry for FMD and to compare differences in characteristics between patients with and without PT within the US Registry.
Methods
The data that support the findings of this study are available from the corresponding author upon reasonable request. Data were queried from the US Registry for FMD, the design of which has been previously published. 4 Enrollment in the Registry began in January 2009. Each participating center obtained approval from its respective institutional review board. Subjects provided informed consent for enrollment in the US Registry for FMD. Eligibility for enrollment was determined on the basis of identification of the characteristic appearance of FMD from vascular imaging in at least 1 vascular bed. Data for baseline demographic characteristics, past medical history, presenting signs/symptoms, physical exam, and vascular bed involvement for patients enrolled in the Registry as of December 23, 2020, who were aged ≥18 years at the time of enrollment were included. Statistical analysis was performed using Student t tests and Wilcoxon rank‐sum tests on continuous variables, and χ2 and Fisher's exact tests on categorical variables to evaluate the differences between patients with and without PT. All P values reported were 2‐sided, with a significance level of 0.05 throughout. Statistically significant variables from the univariable analysis were further examined with multivariable logistic regression. Variables included in the final model were those consistently statistically significant (P<0.05). In addition, because of potential clinical relevance, vertebral artery involvement was kept throughout model selections despite its statistical nonsignificance.
Results
Of 2814 patients with FMD enrolled in the registry, 2613 (92.9%) had data regarding PT as a presenting symptom of FMD at the time of diagnosis (Table 1). Of these, 972 (37.2%) patients reported PT while 1641 (62.8%) did not. Patients with PT were more often women (98.9% versus 93.8%; P<0.001) and were younger at time of FMD diagnosis (53.3 versus 55.2 years; P<0.001). Patients with PT were less likely to have hypertension (56.0% versus 64.9%; P<0.001) or use antihypertensive medications, including diuretics (19.5% versus 24.9%; P=0.002), angiotensin‐converting enzyme inhibitors (16.4% versus 20.6%; P=0.011), angiotensin receptor blockers (15.5% versus 20.8%; P=0.001), beta blockers (30.6% versus 38.0%; P<0.001), and calcium channel blockers (18.4% versus 22.0%; P=0.030). A history of headaches (82.5% versus 62.7%; P<0.001) was more common among patients reporting PT, but there was no difference in headache type, including migraine (56.6 versus 54.5; P=0.38) and tension (25.7% versus 22.2%; P=0.084). Patients with PT were more likely to present with a cervical bruit (37.5% versus 15.8%; P<0.001), cervical artery dissection (19.4% versus 14.1%; P<0.001), and other neurovascular signs/symptoms including transient ischemic attack (10.8% versus 7.3%; P=0.003), dizziness (44.9% versus 22.9%; P<0.001), neck pain (41.3% versus 19.4%; P<0.001), and nonpulsatile tinnitus (28.5% versus 19.6%; P<0.001) at the time of FMD diagnosis. There was no difference in presentation with stroke among those without or with PT (7.2% versus 8.4%; P=0.31).
Table 1.
Baseline Demographic and Clinical Characteristics in Patients With FMD With and Without PT
| N (%) | All Patients | Patients With PT | Patients Without PT | P Value |
|---|---|---|---|---|
| 2613 | 972 (37.2%) | 1641 (62.8%) | ||
| Demographics | ||||
| Female, n (%) | 2500 (95.7) | 961 (98.9) | 1539 (93.8) | <0.001 |
| Age at symptom onset, mean±SD (median) | 50.7±13.6 (50.7) | 49.7±11.6 (49.6) | 51.3±14.6 (51.7) | 0.001 |
| Age at diagnosis, y, mean±SD (median) | 54.5±12.3 (53.9) | 53.3±10.5 (52.3) | 55.2±13.2 (55.2) | <0.001 |
| Past medical history, n (%) | ||||
| Headache | 1825/2606 (70.0) | 799/969 (82.5) | 1026/1637 (62.7) | <0.001 |
| Migraine type | 975/1760 (55.4) | 434/767 (56.6) | 541/993 (54.5) | 0.38 |
| Tension type | 417/1760 (23.7) | 197/767 (25.7) | 220/993 (22.2) | 0.084 |
| Daily headache | 244/1160 (21.0) | 129/536 (24.1) | 115/624 (18.4) | 0.019 |
| Hypertension | 1598/2593 (61.6) | 535/956 (56.0) | 1063/1637 (64.9) | <0.001 |
| Anxiety | 542/2086 (26.0) | 222/780 (28.5) | 320/1306 (24.5) | 0.046 |
| Depression | 458/2086 (22.0) | 182/780 (23.3) | 276/1306 (21.1) | 0.24 |
| History of smoking | 755/2570 (29.4) | 258/955 (27.0) | 497/1615 (30.8) | 0.043 |
| Presenting symptoms/signs at FMD diagnosis, n (%) | ||||
| Neck pain | 676/2466 (27.4) | 372/900 (41.3) | 304/1566 (19.4) | <0.001 |
| Dizziness | 764/2476 (30.9) | 403/897 (44.9) | 361/1579 (22.9) | <0.001 |
| Nonpulsatile tinnitus | 577/2528 (22.8) | 261/915 (28.5) | 316/1613 (19.6) | <0.001 |
| Stroke | 205/2579 (7.9) | 69/952 (7.2) | 136/1627 (8.4) | 0.31 |
| Amaurosis fugax | 88/2527 (3.5) | 41/925 (4.4) | 47/1602 (2.9) | 0.048 |
| TIA | 218/2531 (8.6) | 100/924 (10.8) | 118/1607 (7.3) | 0.003 |
| Horner syndrome | 82/2498 (3.3) | 43/909 (4.7) | 39/1589 (2.5) | 0.002 |
| Cervical bruit | 566/2383 (23.8) | 327/871 (37.5) | 239/1512 (15.8) | <0.001 |
| Carotid or vertebral artery dissection | 407/2536 (16.0) | 183/943 (19.4) | 224/1593 (14.1) | <0.001 |
| Aneurysms | 437/2529 (17.3) | 133/942 (14.1) | 304/1587 (19.2) | 0.001 |
| Carotid or vertebral artery aneurysm | 230/2537 (9.1) | 83/940 (8.8) | 147/1597 (9.2) | 0.75 |
| Physical exam findings at FMD diagnosis, n (%) | ||||
| Neurological examination | ||||
| Nonreactive pupils | 73/2253 (3.2) | 38/880 (4.3) | 35/1373 (2.5) | 0.021 |
| Lid droop | 93/2243 (4.1) | 50/877 (5.7) | 43/1366 (3.1) | 0.003 |
| Cranial nerves deficit | 68/2203 (3.1) | 32/844 (3.8) | 36/1359 (2.6) | 0.13 |
| Focal neuro deficit | 106/2213 (4.8) | 39/841 (4.6) | 67/1372 (4.9) | 0.79 |
| Medications, n (%) | ||||
| Diuretics | 569/2489 (22.9) | 180/925 (19.5) | 389/1564 (24.9) | 0.002 |
| ACE inhibitors | 471/2478 (19.0) | 150/916 (16.4) | 321/1562 (20.6) | 0.011 |
| ARBs | 465/2468 (18.8) | 142/918 (15.5) | 323/1550 (20.8) | 0.001 |
| Beta blockers (including alpha/beta blockers) | 881/2500 (35.2) | 284/929 (30.6) | 597/1571 (38.0) | <0.001 |
| Calcium channel blockers | 512/2475 (20.7) | 169/919 (18.4) | 343/1556 (22.0) | 0.030 |
ACE indicates angiotensin‐converting enzyme; ARB, angiotensin receptor blocker; FMD, fibromuscular dysplasia; PT, pulsatile tinnitus; and TIA, transient ischemic attack.
Anatomically, extracranial carotid artery involvement was more common among patients with PT than those without (90.0% versus 78.6%; P<0.001), while there was no difference in involvement in vertebral (42.9% versus 41.5%; P=0.55) or intracranial (16.2% versus 17.3%; P=0.57) arteries (Table 2). Renal artery (57.5% versus 71.1%; P<0.001) and mesenteric artery (13.9% versus 20.3%; P=0.001) involvement was less common in patients with PT. However, multivessel involvement of FMD, defined as >1 vascular bed involved, was more common (62.7% versus 58.3%; P=0.029) in patients with PT.
Table 2.
Arterial Bed Involvement and Vascular Manifestations in Patients With FMD With and Without PT
| N (%) | All FMD patients | Patients With PT | Patients Without PT | P Value |
|---|---|---|---|---|
| 2613 | 972 (37.2%) | 1641 (62.8%) | ||
| Vascular bed involvement, n (%) | ||||
| Renal | 1371/2074 (66.1) | 437/760 (57.5) | 934/1314 (71.1) | <0.001 |
| Extracranial carotid and/or vertebral | 2003/2366 (84.7) | 857/939 (91.3) | 1146/1427 (80.3) | <0.001 |
| Extracranial carotid | 1937/2330 (83.1) | 833/926 (90.0) | 1104/1404 (78.6) | <0.001 |
| Vertebral | 786/1870 (42.0) | 324/756 (42.9) | 462/1114 (41.5) | 0.55 |
| Intracranial | 280/1664 (16.8) | 115/709 (16.2) | 165/955 (17.3) | 0.57 |
| Mesenteric | 268/1514 (17.7) | 84/606 (13.9) | 184/908 (20.3) | 0.001 |
| FMD vascular beds involved in a patient, n (%) | ||||
| 1 | 1048 (40.1) | 363 (37.3) | 685 (41.7) | 0.029 |
| ≥2 | 1565 (59.9) | 609 (62.7) | 956 (58.3) | |
FMD indicates fibromuscular dysplasia; and PT, pulsatile tinnitus.
Multivariable regression analysis demonstrated findings similar to the univariate analysis (Figure). There was an association between PT and FMD involving the extracranial carotid artery (odds ratio [OR], 1.49; P=0.005) but not the vertebral artery (OR, 0.94; P=0.56). Patients with PT were more likely to be women (OR, 3.00; P=0.002), younger at age of diagnosis (OR, 1.12 for each 10‐year decrease in age; P=0.011), have a history of headaches (OR, 1.82; P<0.001), present with neck pain (OR, 1.64; P<0.001) and dizziness (OR, 2.01; P<0.001), and have a cervical bruit (OR, 2.73; P<0.001).
Figure 1. Multivariable analysis of clinical characteristics associated with pulsatile tinnitus among patients with FMD in the US Registry.
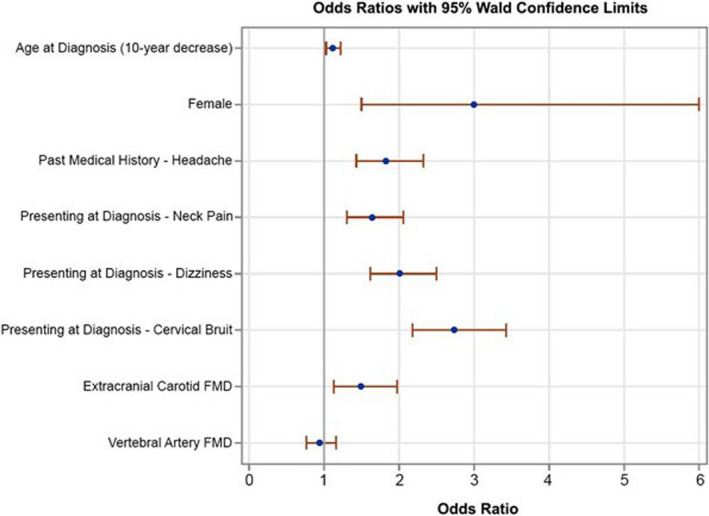
FMD indicates fibromuscular dysplasia.
Discussion
In this analysis of 2613 patients with FMD, we found that 37.2% reported PT as a presenting symptom at FMD diagnosis. There were many clinically relevant differences between patients with and without PT. Patients with PT were more likely women. A possible explanation of this finding is the known difference in FMD distribution by sex; women have a higher rate of carotid involvement with FMD. 9 PT was associated with younger age at time of FMD diagnosis and several neurovascular symptoms/signs including cervical bruit. Indeed, patients with PT were more likely to have FMD involving the extracranial carotid but not of the vertebral artery. Additionally, a history of headache was more common among patients reporting PT. Importantly, we could not identify differences in headache subtypes, likely because of missing data.
The association between FMD and PT has been previously described. 4 , 5 The European/International FMD Registry reported PT as a presenting symptom of FMD in 16.9% of patients. We report a >2‐fold higher rate of PT. The difference likely speaks to the heterogeneity of the FMD population and the differences between the 2 registries, notably the higher prevalence of cerebrovascular FMD among patients in the US Registry. The current study expands upon our understanding of the association between FMD and PT by providing more granular information regarding baseline characteristics, presenting signs/symptoms, and vascular bed involvement. Importantly, it also provides a comparison with patients with FMD who do not have PT.
The cause of PT in patients with FMD remains unclear. PT can be caused by vascular disorders including stenosis or tortuosity of the carotid artery, intraluminal webs resulting in turbulent flow, and other vascular abnormalities including aneurysms, dissections, or arteriovenous fistulas, all potentially present in patients with FMD. 10 , 11 , 12 Another potential contributor to PT in patients with FMD is the presence of an S‐curve, or extreme arterial tortuosity, of the internal carotid artery, resulting in turbulent blood flow and PT. A review of 116 patients with FMD found 32% of patients had an S‐curve present in the internal carotid artery. 13 We are unable to comment on the prevalence of S‐curve presence in this study, as these data are not collected by the US Registry. Notably, carotid involvement in FMD is typically in the mid or distal artery, close to the ear, which may be a contributing factor. From the non‐FMD literature, other factors associated with PT include nonvascular disorders such as intracranial tumors, intracranial hypertension, and sarcoidosis. However, in many cases of PT, there is no clear cause. In a single‐center review of 84 patients with PT, 68% of patients were found to have an underlying etiology, usually vascular in nature; however, an underlying etiology could not be identified in the remaining 32% of patients. 10 Among patients with PT in this study, 22.9% were found to have a carotid or vertebral dissection, 8.8% had a carotid or vertebral aneurysm, and 37.5% had a cervical bruit, a manifestation of turbulence. Still, approximately one‐third of the patients did not have any associated vascular findings, consistent with prior studies. Another potential contributor to PT is antihypertensive medications 14 ; however, in this study, antihypertensive medications were used less in patients with FMD presenting with PT compared with those without PT. Indeed, additional research to better understand both FMD and its relationship to PT is needed.
This study has limitations. We could not offer a comparison with patients with PT who do not have FMD. As this study uses the US Registry for FMD, the data reported are observational and descriptive. Data for the US Registry are obtained via standardized data collection form to maintain uniformity between Registry sites, and thus open‐ended questions are not used. The data collection form does not capture information about the frequency of PT as a self‐reported symptom by patient within the Registry. Unfortunately, information on tortuosity of cerebrovascular arteries, a potential contributor to PT, was not available. Finally, there are limited longitudinal data within the Registry, such as effect of medical therapy for PT and rates of resolution of PT. Still, this represents the largest data set on FMD and PT.
Conclusions
PT is common among patients with FMD. These patients have higher rates of neurovascular symptoms and extracranial carotid artery involvement compared with those without PT. Additional studies are required to better understand the mechanisms of PT in FMD and to delineate optimal treatment strategies. These data also support investigation of the prevalence of FMD among people who present with PT and awareness of FMD as a cause of PT among providers who evaluate patients with this symptom.
Sources of Funding
The United States Registry for Fibromuscular Dysplasia is funded by the Fibromuscular Dysplasia Society of America.
Disclosures
Drs Gornik and Olin are members of the Medical Advisory Board of the Fibromuscular Dysplasia Society of America, a nonprofit organization. Dr Froehlich is a consultant for Boehringer Ingelheim, Janssen Biotech, Johnson & Johnson Health Care Systems Inc., and Pfizer. Dr Gray is a consultant for Surmodics, Inc. and an independent contractor for data and safety monitoring for Terumo BCT, Inc. Dr Weinberg is a consultant for Magneto Thrombectomy Solutions, Penumbra Inc., ‐ National PI. The remaining authors have no disclosures to report.
Acknowledgments
The authors thank Ms. Pamela Mace, Executive Director of the FMD Society of America, for her leadership and ongoing support of the US Registry for FMD. We thank Eva Kline‐Rogers of the University of Michigan Research Clinical Outcomes Research and Reporting Program for her work leading the Registry coordinating center. We thank all of our patients who continue to participate and support the US Registry for FMD.
For Sources of Funding and Disclosures, see page 5.
References
- 1. Gornik HL, Persu A, Adlam D, Aparicio LS, Azizi M, Boulanger M, Bruno RM, de Leeuw P, Fendrikova‐Mahlay N, Froehlich J, et al. First International Consensus on the diagnosis and management of fibromuscular dysplasia. Vasc Med. 2019;24:164–189. DOI: 10.1177/1358863X18821816. [DOI] [PubMed] [Google Scholar]
- 2. Khoury MH, Gornik HL. Fibromuscular dysplasia (FMD). Vasc Med. 2017;22:248–252. DOI: 10.1177/1358863X17700716. [DOI] [PubMed] [Google Scholar]
- 3. Shivapour DM, Erwin P, Kim ES. Epidemiology of fibromuscular dysplasia: a review of the literature. Vasc Med. 2016;21:376–381. DOI: 10.1177/1358863X16637913. [DOI] [PubMed] [Google Scholar]
- 4. Olin JW, Froehlich J, Gu X, Bacharach JM, Eagle K, Gray BH, Jaff MR, Kim ESH, Mace P, Matsumoto AH, et al. The United States Registry for Fibromuscular Dysplasia: results in the first 447 patients. Circulation. 2012;125:3182–3190. DOI: 10.1161/CIRCULATIONAHA.112.091223. [DOI] [PubMed] [Google Scholar]
- 5. Pappaccogli M, Di Monaco S, Warchoł‐Celińska E, Lorthioir A, Amar L, Aparicio LS, Beauloye C, Bruno RM, Chenu P, de Leeuw P, et al. The European/International Fibromuscular Dysplasia Registry and Initiative (FEIRI)‐clinical phenotypes and their predictors based on a cohort of 1000 patients. Cardiovasc Res. 2021;117:950–959. DOI: 10.1093/cvr/cvaa102. [DOI] [PubMed] [Google Scholar]
- 6. Wells BJ, Modi RD, Gu X, Bumpus SM, Swan K, Froehlich JB, Gray BH, Southerland AM, Kim ESH, Fendrikova Mahlay N, et al. Clinical associations of headaches among patients with fibromuscular dysplasia: a report from the US Registry for Fibromuscular Dysplasia. Vasc Med. 2020;25:348–350. DOI: 10.1177/1358863X20923740. [DOI] [PubMed] [Google Scholar]
- 7. Lather HD, Gornik HL, Olin JW, Gu X, Heidt ST, Kim ESH, Kadian‐Dodov D, Sharma A, Gray B, Jaff MR, et al. Prevalence of intracranial aneurysm in women with fibromuscular dysplasia: a report from the US Registry for Fibromuscular Dysplasia. JAMA Neurol. 2017;74:1081–1087. DOI: 10.1001/jamaneurol.2017.1333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Langguth B, Kreuzer PM, Kleinjung T, De Ridder D. Tinnitus: causes and clinical management. Lancet Neurol. 2013;12:920–930. DOI: 10.1016/S1474-4422(13)70160-1. [DOI] [PubMed] [Google Scholar]
- 9. Kim ESH, Olin JW, Froehlich JB, Gu X, Bacharach JM, Gray BH, Jaff MR, Katzen BT, Kline‐Rogers E, Mace PD, et al. Clinical manifestations of fibromuscular dysplasia vary by patient sex: a report of the United States Registry for Fibromuscular Dysplasia. J Am Coll Cardiol. 2013;62:2026–2028. DOI: 10.1016/j.jacc.2013.07.038. [DOI] [PubMed] [Google Scholar]
- 10. Waldvogel D, Mattle HP, Sturzenegger M, Schroth G. Pulsatile tinnitus–a review of 84 patients. J Neurol. 1998;245:137–142. DOI: 10.1007/s004150050193. [DOI] [PubMed] [Google Scholar]
- 11. Sismanis A. Pulsatile tinnitus: contemporary assessment and management. Curr Opin Otolaryngol Head Neck Surg. 2011;19:348–357. DOI: 10.1097/MOO.0b013e3283493fd8. [DOI] [PubMed] [Google Scholar]
- 12. Kadian‐Dodov D, Gornik HL, Gu X, Froehlich J, Bacharach JM, Chi Y‐W, Gray BH, Jaff MR, Kim ESH, Mace P, et al. Dissection and aneurysm in patients with fibromuscular dysplasia: findings from the U.S. Registry for FMD. J Am Coll Cardiol. 2016;68:176–185. DOI: 10.1016/j.jacc.2016.04.044. [DOI] [PubMed] [Google Scholar]
- 13. Sethi SS, Lau JF, Godbold J, Gustavson S, Olin JW. The S curve: a novel morphological finding in the internal carotid artery in patients with fibromuscular dysplasia. Vasc Med. 2014;19:356–362. DOI: 10.1177/1358863X14547122. [DOI] [PubMed] [Google Scholar]
- 14. Figueiredo RR, Azevedo AA, Penido NDO. Positive association between tinnitus and arterial hypertension. Front Neurol. 2016;7:171. DOI: 10.3389/fneur.2016.00171. [DOI] [PMC free article] [PubMed] [Google Scholar]


