Abstract
Background
Data are limited about young adults' characteristics and outcomes undergoing coronary artery bypass grafting (CABG).
Methods and Results
We used the National Inpatient Sample database to identify adults aged 18 to 45 years who underwent CABG between 2004 and 2018. The data were weighted to generate national estimates of the entire US hospitalized population. We identified 110 463 CABG cases, equivalent to 62.2 per 1 000 000 person‐years; 27.1% were women, and 70.2% were White adults. Overall, annual CABG volume per 1 000 000 significantly decreased from 87.3 in 2004 to 45.7 in 2018. The prevalence of obesity, diabetes mellitus, hypertension, drug abuse, and chronic medical conditions increased over time. Overall, inpatient mortality was 1.76%; ST‐segment–elevation myocardial infarction, non–ST‐segment–elevation myocardial infarction, heart failure, peripheral vascular disease, renal failure, and valvular surgery were associated with higher inpatient mortality. Women had higher inpatient mortality than men (2.29% versus 1.57%), and Black patients had higher deaths than White patients (2.86% versus 1.58%). Inpatient mortality remained stable overall, according to sex, race, or clinical indication of CABG. However, the mean length of stay (8.4 days in 2004 to 9.5 days in 2018) and inflation‐adjusted cost of care ($40 522.8 in 2004 to $52 434.2 in 2018) significantly increased during the study period.
Conclusions
Despite the increased burden of cardiometabolic risk factors, the inpatient mortality in young adults undergoing CABG remained stable during the last 15 years. However, CABG volumes have decreased, but length of stay and inflation‐adjusted costs have increased over time.
Keywords: coronary artery bypass grafting, cost of care, mortality, young adults
Subject Categories: Quality and Outcomes, Mortality/Survival, Cardiovascular Surgery, Revascularization, Cardiovascular Disease
Nonstandard Abbreviations and Acronyms
- NIS
National Inpatient Sample
Clinical Perspective
What Is New?
Between 2004 and 2018, young adults hospitalized for coronary artery bypass grafting have noted a substantial increase in cardiometabolic comorbidities.
Coronary artery bypass grafting surgery volume has decreased, inpatient mortality has remained stable, but the length of stay and inflation‐adjusted care costs have increased over time.
What Are the Clinical Implications?
Strenuous efforts are needed to attenuate the comorbidity burden in young adults.
Public health strategies should focus on providing cost‐effective management in young adults requiring coronary artery bypass grafting.
Coronary artery disease (CAD) is the leading cause of mortality, morbidity, and economic loss worldwide. 1 Premature CAD (aged ≤45 years) may lead to loss of lifetime productivity, increase lifetime healthcare usage, and poor prognosis. 2 , 3 Consequently, recent evidence suggests that an overall improvement in cardiac mortality has stalled in young adults (aged ≤45 years) in the United States since 2011. 4
Surgical revascularization is a durable therapeutic strategy that lowers the rates of adverse cardiovascular events, improves the quality of life, and reduces the need for repeat revascularization. 5 , 6 , 7 However, most coronary artery bypass graft (CABG) surgery data have primarily focused on elderly patients, and a limited number of studies have explored outcomes in younger adults. 8 , 9 Furthermore, prior studies of CABG in young patients have been mostly single‐center analyses, without providing a perspective on the clinical risk profile, mortality, and healthcare resource usage at the national scale. 8 , 9 , 10 Therefore, analyzing the most recent CABG trends becomes relevant to public health interventions to assess clinical and economic burden in young adults undergoing surgical revascularization. Consequently, we analyzed data from the large US administrative claims‐based database and examined trends in clinical characteristics, CABG volume, mortality, health care resource utilization, and expenditure in young adults.
Methods
Data Sharing Statement
The National Inpatient Sample (NIS) data sets used in this project are publicly available and are easily replicable from the methods described in the article.
Setting
We used the NIS, an all‐payer database that approximates a 20% stratified sample of discharges from US community hospitals participating in the Healthcare Cost Utilization Project—sponsored by the Agency for Healthcare and Research and Quality. 11 The database contains the clinical and resource utilization information abstracted from discharges from 47 US states covering >97% of the US population. The annual sample encompasses ≈8 million hospital discharges across different geographic regions and hospital types. This study was exempt from the institutional review board approval, given the NIS database's de‐identified nature and public availability.
Study Design
We conducted an observational analysis using data from January 2004 to December 2018 to identify all hospitalizations in young patients 3 , 12 requiring CABG using an International Classification of Diseases, Ninth Revision, Clinical Modification (ICD‐9‐CM) procedure code of 36.1x and International Classification of Diseases, Tenth Revision, Clinical Modification (ICD‐10‐CM) procedure codes: "0210083" to "02134ZF". 13 , 14 Since premature CAD refers to the onset of disease in adults aged ≤45 years, 2 , 3 we defined young adults as those aged 18 to 45 years. 3 , 12 Several relevant clinical and socioeconomic features were described, including demographics, comorbidities, clinical presentation (ST‐segment–elevation myocardial infarction [STEMI], non–ST‐segment–elevation myocardial infarction [NSTEMI], and non‐myocardial infarction [unstable angina and stable ischemic heart disease]), insurance status, household income, and discharge disposition. Tables S1 and S2 list the diagnosis codes used in this analysis.
We classified discharge disposition as (1) home; (2) short‐term care facility (short‐term rehabilitation or inpatient rehabilitation); (3) long‐term care facility (skilled nursing and intermediate care facility); and (4) against medical advice.
Outcomes
The outcomes of interest were trends in clinical characteristics, inpatient mortality, length of stay (LOS), and inflation‐adjusted care costs for hospitalization in young adults undergoing CABG.
Statistical Analysis
The national estimates of the entire US hospitalized population were calculated using the Agency for Healthcare and Research and Quality sampling and weighting method. 15 We divided the study population into 3 groups of 5‐year intervals (2004–2008, 2009–2013, and 2014–2018). We described continuous variables as mean and SE and categorical variables as numbers and percentages. We used the Rao‐Scott Chi‐square test for between‐group comparisons for categorical variables. We performed weighted logistic regression to estimate odds ratios (ORs) and 95% CIs to determine inpatient mortality predictors. We constructed a multivariable logistic regression model using variables identified as significant predictors (P≤0.05) of mortality in the univariate models (Table S3).
Hospital total charges were converted to cost estimates using hospital‐specific cost‐to‐charge ratios provided by Healthcare Cost Utilization Project. Total costs were inflated to 2019 US dollars using the Consumer Price Index inflation calculator published by the US Bureau of Labor Statistics. 16 We performed a multivariate linear regression model to examine the correlation of clinical complications and components of hospital resource usage with the inflation‐adjusted cost of care.
We estimated CABG per 1 000 000 young US adults; the denominator for the young population was extracted from the Census Bureau estimates of US resident populations for each study year. 17 We estimated inpatient mortality as the proportion of deaths in young adults undergoing CABG over a total number of young CABG admissions. We adjusted mortality for the following variables: age, sex, Charlson comorbidity index, valve surgery, insurance status, hospital location/teaching status, hospital region, and hospital bed size.
Trends in CABG per 1 000 000, LOS, and cost of care, were examined using weighted linear regression, and binary logistic regression was used for inpatient mortality, with year as the sole predictor. Accordingly, P values for trends were determined based on these models. 18
We further stratified inpatient mortality analyses by sex, race, and clinical indication for CABG. Additionally, we performed sensitivity analyses for young adults comparing clinical and economic outcomes among adults who underwent isolated CABG versus CABG plus concomitant valve surgery. We used Stata 16.0 (StataCorp, College Station, TX) 19 for all analyses, which were survey‐specific, using Stata's "svy" functions. 19 Statistical significance was set at ≤5%.
Results
Between 2004 and 2018, a total of 110 463 weighted cases of CABG were identified in young adults, equivalent to 62.2 (95% CI, 62.1–62.3) per 1 000 000 person‐years. The mean (SE) age of the population was 40.9 (0.03) years, 27.1% were women, and 70.2% were White adults (Table 1). Most procedures were performed in hospitals in the South region (48.5%; Figure 1A), large bed‐sized hospitals (72.5%), and urban teaching hospitals (65.3%). The volume of CABG procedures was lowest in rural hospitals (3.8%). Medicare or Medicaid beneficiaries had lower proportions of procedures (29.2%) than those with private insurance (53.6%). A minority of patients had prior percutaneous coronary intervention (14.8%), prior CABG (1.4%), prior myocardial infarction (17.1%), and prior stroke (2.7%). A total of 5.1% participants underwent concurrent percutaneous coronary intervention and 7.5% concomitant valve surgery. Approximately a third of the patients (31.9%) lived in ZIP codes with the lowest quartile of income.
Table 1.
Baseline Characteristics and Trends in Young Adults Undergoing CABG in the United States, 2004 to 2018
| Variable, n (%) |
2004–2008 (n=46 273) |
2009–2013 (n=34 820) |
2014–2018 (n=29 370) |
|---|---|---|---|
| Age, mean (SE), y | 41.09 (0.04) | 40.85 (0.05) | 40.80 (0.06) |
| Women | 11 871 (25.66) | 9270 (27.92) | 8315 (28.32) |
| Race | |||
| White adults | 23 461 (73.07) | 21 707 (70.08) | 18 630 (67.12) |
| Black adults | 3352 (10.44) | 3880 (12.53) | 3475 (12.52) |
| Hispanic adults | 2738 (8.53) | 2934 (9.47) | 2380 (10.62) |
| Others † | 2558 (7.97) | 2456 (7.93) | 2715 (9.78) |
| Comorbidities | |||
| Chronic pulmonary disease* | 7462 (16.13) | 5530 (15.88) | 4615 (15.71) |
| Atrial fibrillation | 2577 (5.57) | 2343 (6.73) | 2110 (8.85) |
| Diabetes mellitus | 14 972 (32.36) | 13 855 (39.79) | 13 080 (44.54) |
| Hypertension | 27 682 (59.82) | 24 277 (69.72) | 19 335 (65.83) |
| Obesity | 8680 (18.76) | 10 109 (29.03) | 11 440 (38.95) |
| Heart failure | 275 (0.59) | 371 (1.07) | 380 (1.29) |
| Peripheral vascular disease | 2466 (5.33) | 2277 (6.54) | 2195 (7.47) |
| Renal failure | 2930 (6.33) | 3513 (10.09) | 3705 (12.61) |
| Liver disease | 508 (1.1) | 449 (1.29) | 680 (2.32) |
| Neurological disorders | 1115 (2.41) | 1040 (2.99) | 1200 (4.09) |
| Deficiency anemias | 5690 (12.3) | 6174 (17.73) | 4620 (15.73) |
| Hypothyroidism | 1889 (4.08) | 2213 (6.36) | 1760 (5.99) |
| Valvular disease | 139 (0.3) | 176 (0.51) | 235 (0.8) |
| Smoking | 21 934 (47.4) | 18 295 (52.54) | 17 155 (58.41) |
| Alcohol abuse | 1892 (4.09) | 1440 (4.13) | 1250 (4.26) |
| Drug abuse | 2309 (4.99) | 2094 (6.01) | 1900 (7.68) |
| Previous myocardial infarction | 6607 (14.28) | 6025 (17.3) | 4765 (20) |
| Previous CABG | 464 (1) | 404 (1.16) | 685 (2.33) |
| Previous PCI | 5885 (12.72) | 5779 (16.6) | 4685 (15.95) |
| Prior stroke | 445 (0.96) | 1208 (3.47) | 1325 (4.51) |
| Concomitant PCI | 2387 (5.16) | 1931 (5.54) | 1335 (4.55) |
| Concomitant valve surgery | 3109 (6.72) | 2885 (8.28) | 2345 (7.98) |
| Hospital location | |||
| Rural | 1716 (3.71) | 1544 (4.50) | 980 (3.34) |
| Urban non‐teaching | 16 646 (35.97) | 12 109 (35.27) | 5175 (17.62) |
| Urban teaching | 27 910.43 (60.32) | 20 679 (60.23) | 23 215 (79.04) |
| Bed size of the hospital | |||
| Small | 2396 (5.18) | 1925 (5.61) | 2785 (9.48) |
| Medium | 9355 (20.22) | 5975 (17.4) | 5175 (17.62) |
| Large | 34 522 (74.6) | 26 431 (76.99) | 18 795 (63.99) |
| Region* | |||
| Northeast | 6465 (13.97) | 4936 (14.18) | 3730 (12.7) |
| Midwest | 11 269 (24.35) | 8256 (23.71) | 6905 (23.51) |
| South | 22 587 (48.81) | 16 654 (47.83) | 14 370 (48.93) |
| West | 5952 (12.86) | 4974 (14.29) | 4365 (14.86) |
| Median income | |||
| 0–25th | 13 439 (29.82) | 11 108 (32.85) | 9870 (34.11) |
| 26–50th | 12 622 (28.01) | 9463 (27.99) | 8130 (28.1) |
| 50–75th | 10 693 (23.73) | 7912 (23.4) | 6510 (22.5) |
| 75–100th | 8310 (18.44) | 5326 (15.75) | 4425 (15.29) |
| Insurance status | |||
| Medicare or Medicaid | 11 291 (24.46) | 10 350 (29.81) | 10 500 (35.83) |
| Private insurance | 26 881 (58.24) | 17 296 (49.82) | 14 940 (50.98) |
| Self‐pay, no charge, or other | 7982 (17.29) | 7072 (20.37) | 3865 (13.19) |
| Clinical presentation | |||
| STEMI | 31 098 (67.2) | 21 877 (62.83) | 16 625 (56.61) |
| NSTEMI | 8036 (17.37) | 8885 (25.52) | 9715 (33.08) |
| Non‐myocardial infarction | 7139 (15.43) | 4058 (11.65) | 3030 (10.32) |
Non‐myocardial infarction: unstable angina and stable ischemic heart disease. CABG indicates coronary artery bypass graft; NSTEMI, non–ST‐segment–elevation myocardial infarction; PCI, percutaneous coronary intervention; and STEMI, ST‐segment–elevation myocardial infarction.
P>0.05.
Other includes Asian/Pacific Islander, and Native American.
Figure 1. Trends of characteristics and outcomes in hospitalized young adults (≤45 years) undergoing CABG in the United States, 2004 to 2018.

A, Regional distribution of hospitals performing inpatient CABG; (B) Trends of CABG volumes per 1 000 000 US young adults; (C) Trends of mean length of stay in days; (D) Trends of inflation‐adjusted cost of care in US $. CABG indicates coronary artery bypass grafting.
Overall CABG per 1 000 000 in young adults significantly decreased from 87.3 (95% CI, 87.2–87.4) in 2004 to 45.7 (95% CI, 45.6–45.8) in 2018 (P‐trend <0.01; Figure 1B).
Trends in Demographics and Comorbidities
The proportion of women, Black and Hispanic adults undergoing CABG increased, while the number of White patients receiving CABG decreased (P<0.001; Table 1). The proportion of patients who lived in ZIP codes with the lowest quartile of income increased significantly during the study duration (29.8–34.1%; P<0.001). There was also a significant increase in the proportion of Medicare/Medicaid beneficiaries from 24.5% to 35.8% over time. Hypertension (64.5%) and smoking (51.9%) were the leading risk factors; the prevalence of diabetes mellitus, hypertension, obesity, peripheral vascular disease, smoking, drug abuse, chronic renal failure, hypothyroidism, and neurological disorders significantly increased over the study duration. Between 2004 and 2018, the primary clinical presentation shifted from STEMI to NSTEMI (P<0.001), consistent with similar national trends in older adults. 20
Inpatient Mortality and Clinical Outcomes
Overall, inpatient mortality in young adults undergoing CABG was 1.76%; mortality was significantly higher in patients admitted with STEMI than those with NSTEMI (3.37% versus 1.58%). Women had higher mortality (2.3% versus 1.6%) than men, and Black patients had higher mortality than White patients (2.8% versus 1.6%). Inpatient mortality remained stable over time; this trend was consistent for sex and race (Table S4), as well as for clinical indication (Figure 2). Multivariate logistic regression showed that STEMI, NSTEMI, heart failure, peripheral vascular disease, renal failure, and valvular surgery were associated with a higher likelihood of inpatient mortality (Figure S1).
Figure 2. Trends of inpatient mortality in hospitalized young adults (≤45 years) undergoing coronary artery bypass grafting in the United States, 2004 to 2018.
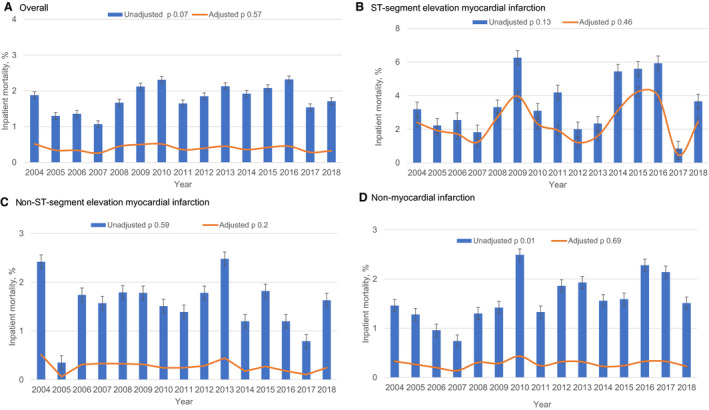
A, Overall inpatient mortality; (B) Inpatient mortality after ST‐segment–elevation myocardial infarction; (C) Inpatient mortality after non–ST‐segment–elevation myocardial infarction; (D) Non‐myocardial infarction. P values refer to P‐trends. For adjusted inpatient mortality, estimates were adjusted for age, sex, concomitant valvular surgery, Charlson comorbidity index, insurance status, hospital location/teaching status, hospital region, and hospital bed size.
During the study period, clinical complications (cardiogenic shock, acute kidney injury, stroke) and resource utilization (vasopressors, invasive ventilation) increased significantly (Table S5).
Length of Stay and Inflation‐Adjusted Cost of Care
Overall mean LOS was 8.7 (0.05) days; the mean inflation‐adjusted cost was $45 842.3 (345.7) (Table 2). The mean LOS increased from 8.4 in 2004 to 9.5 in 2018 (P‐trend <0.01; Figure 1C). The inflation‐adjusted cost of care also increased from $40 523 in 2004 to $52 434 in 2018 (P‐trend <0.01; Figure 1D). Clinical complications (acute kidney injury, cardiogenic shock, stroke, cardiac tamponade) and hospital resource usage (invasive mechanical ventilation, permanent pacemaker implantation, dialysis, tracheostomy) were significantly correlated with the LOS and inflation‐adjusted cost of care (Tables S6 and S7, respectively). The discharge disposition to home decreased (from 94.5% to 91.4%) and to long‐term care facility increased (from 3.2% to 5.6%) (P<0.001).
Table 2.
Trends in Discharge Disposition and Economic Outcome in Young Adults Undergoing CABG, 2004 to 2018
| Variable | 2004–2008 | 2009–2013 | 2014–2018 |
|---|---|---|---|
| Length of stay, mean (SE), d | 8.35 (0.08) | 8.79 (0.09) | 9.20 (0.09) |
| Inflation‐adjusted cost, US $, mean (SE) | 42 036.6 (524.9) | 46 570.8 (574.6) | 50 758.2 (636.3) |
| Discharge disposition of surviving patients, n (%) | |||
| Home | 43 737 (94.54) | 32 326 (92.89) | 26 810 (91.36) |
| Short‐term care facility | 255 (0.55) | 263 (0.76) | 230 (0.78) |
| Long‐term care facility | 1493 (3.23) | 1450 (4.17) | 1665 (5.67) |
| Against medical advice | 95 (0.2) | 54 (0.15) | 75 (0.26) |
Sensitivity Analyses
Overall, larger number of patients underwent isolated CABG (n=102 124) compared with CABG plus concomitant valve surgery (n=8339). Patients undergoing isolated CABG were slightly older, predominantly White, and had a higher proportion of smoking, diabetes mellitus, hypertension, and obesity. Whereas patients undergoing CABG plus concomitant valve surgery had higher proportions of women, Black patients, and other comorbidities (atrial fibrillation, heart failure, peripheral vascular disease, anemias, neurological disorders) (Table S8). Inpatient mortality was significantly higher in patients undergoing CABG plus concomitant valve surgery than those receiving isolated CABG (10% versus 1.1%, P<0.05). Similarly, use of resources (vasopressors, invasive ventilation, Intra‐aortic balloon pump, dialysis, tracheostomy, gastrostomy) and complications (cardiogenic shock, acute kidney injury, stroke, permanent pacemaker implantation, and cardiac tamponade) were higher with CABG plus concomitant valve surgery versus isolated CABG (Table S9). The mean LOS (13.5 versus 8.3, P<0.05) and inflation‐adjusted cost of care ($80 283 versus $43 027, P<0.05) were significantly higher with CABG plus concomitant valve surgery than isolated CABG.
Discussion
We document the following key trends in young adults undergoing CABG over the last 15 years in the United States. While the comorbidity profile has become increasingly complex, the inpatient mortality remained stable overall and according to demographic characteristics and clinical indications. CABG use has significantly decreased, whereas the LOS and inflation‐adjusted care costs have increased, mainly because of extended LOS, higher usage of hospital resources, and medical complications. Inpatient mortality, LOS, inflation‐adjusted care cost, and complications were significantly higher in adults undergoing CABG plus concomitant valve surgery than those receiving isolated CABG. Finally, a higher proportion of individuals were discharged to long‐term care facilities instead of home, further influencing the CABG's total cost burden.
We found temporal changes in demographic, socioeconomic, and clinical profiles in young adults hospitalized for CABG. A significant number of patients belonging to the lowest income quartile and Medicaid/Medicare insurance have increased, suggesting a higher proportion of economically underserved young adults can afford CABG, likely attributable to the Affordable Care Act and Medicaid expansion efforts. 21 In contrast, we noted a considerable rise in cardiovascular and non‐cardiovascular comorbidities in young patients. These trends are in line with a rising prevalence of cardiometabolic risk factors, smoking, and drug abuse in the young population in the United States. 22 , 23 While the prevalence of the cardiovascular disease has reduced in most age groups, 24 , 25 recent NIS analyses have shown an increase in cardiovascular comorbidities, including stroke and acute myocardial infarction in the young population. 4 , 26
Sex and racial disparities exist among patients undergoing coronary revascularization. 27 , 28 , 29 , 30 We noted that women constituted a minor proportion of CABG recipients but had higher mortality than men. These observations are consistent with prior evidence showing higher in‐hospital mortality in young women than men, 31 and that a minority of women underwent CABG compared with men. 32 , 33 A recent American Heart Association Survey reported that awareness of heart disease as the leading cause of death has declined in women by 21% between 2009 and 2019, 34 mainly in women aged 25 to 34 years and ethnic/racial minorities (Non‐Hispanic Black and Hispanic women). Similarly, young women admitted with acute myocardial infarction were more likely to have hypertension, diabetes mellitus, chronic kidney insufficiency, and prior stroke than men in a US‐based community surveillance study. 35 Furthermore, hypertension, diabetes mellitus, smoking, and obesity had a higher risk for acute myocardial infarction in women than men. 36 A recent report suggested that women aged <50 years were less likely to receive coronary revascularization or guideline‐directed medical therapies and had higher all‐cause mortality than men over a median follow‐up of 11.2 years. 37 Women are also known to have a smaller body surface area and correspondingly smaller coronary arteries, accounting for some of the excess risks they may have when undergoing CABG. 38 Finally, sex bias in identifying and managing acute myocardial infarction has been shown to influence survival rates in women. 39
Similarly, Black adults are disproportionally affected by cardiovascular risk factors than White adults. Black adults tend to develop premature CAD because of the early onset of traditional cardiovascular risk factors (eg, hypertension, diabetes mellitus, and obesity). 40 , 41 Black patients also have a greater prevalence of adverse health behaviors such as suboptimal diet, physical activity, and medication adherence. Significant socioeconomic gradients increase this racial minority's vulnerability for premature CAD. 42 In a recent study of Medicare beneficiaries, Black patients exhibited higher in‐hospital mortality than White patients, despite an overall decline in Blacks' CABG usage. 43 Our study highlights concerning healthcare inequalities rooted in structural racism in young adults. 44
We found that crude and risk‐adjusted mortality remained stable over the last 15 years. The mortality statistics reflect improved surgical techniques, adoption of quality measures, appropriate patient selection, and concurrent medical therapy. However, our findings in the young adults do not correlate with preliminary evidence suggesting a substantial decline in CABG mortality. 14 We focused on the young study population compared with all comers, which may have masked the age‐related outcome differences in prior studies. 14 Consistent with general trends, 45 we report a significant ≈47% decline in CABG volume from 2004 to 2018. These trends likely demonstrate improved dissemination of cardiovascular health‐related information, the evolution of medical therapies, or selective replacement of surgical revascularization with the transcatheter approach. 46 , 47 , 48 Many states in the United States had adopted the policy of CABG‐mortality public reporting around the year 2000. The unintended consequence of risk aversion and case selection may have played some role in the CABG decline in the study period. 49 Nevertheless, the secular decline in CABG did not decrease LOS or improve care costs. Furthermore, percutaneous coronary intervention preferential use over CABG for relatively stable patients and diverting those with complex coronary anatomy to CABG with subsequent clinical complications might have also influenced LOS and higher costs.
CABG continues to be an expensive procedure, with annual cost estimates of about $6.5 billion to Centers for Medicare and Medicaid Services. 50 , 51 The in‐hospital cost of CABG in the United States is 82.5% higher than in Canada. 52 We noted a 29% relative increase in inflation‐adjusted costs over 15 years. Moreover, most patients were discharged to long‐term care facilities, further increasing the cost burden. Historically, CABG is proven to be cost‐effective compared with percutaneous coronary intervention with a drug‐eluting stent for complex multivessel coronary artery disease, 53 however, the upfront costs of hospitalization and direct cost of care for postoperative complications remain a concern. Despite the emphasis on health care and price transparency, a significant cost variation for CABG exists in the United States. Reduction in direct costs and centralizing the pricing based on hospital characteristics and outcomes measurement‐based "value" reimbursements may address CABG's heavy economic burden. 54 Public and health strategies should focus on providing cost‐effective management in young adults requiring CABG.
Our study has several limitations. First, we used the NIS administrative database, which is subject to coding errors, mainly because of the transition from ICD‐9 to ICD‐10 coding system during the study period. Furthermore, since ICD codes are designed for billing purposes, issues related to the validity of the codes exist as they may not reflect the true clinical outcomes. Second, we could not perform analyses according to anatomic features such as culprit artery, number of bypassed arteries, detailed procedural information, and granular patient‐level characteristics because of data limitations. Third, the NIS database does not include patients' longitudinal follow‐up after discharge; thus, long‐term outcomes cannot be analyzed. Our study did not address readmissions‐related costs, which would have driven care costs per CABG episode higher than mentioned here. Despite these limitations, the NIS database remains the most comprehensive resource for estimating procedures, clinical outcomes, and resource usage trends.
In conclusion, this 15‐year contemporary analysis of CABG hospitalization in young adults documents a decline in CABG volume without worsening inpatient mortality; however, it highlights the concerns of rising costs attributable to extended LOS and healthcare resource usage.
Sources of Funding
None.
Disclosures
Dr Virani discloses the following relations—Department of Veterans Affairs, World Heart Federation, Tahir, and Jooma Family Honorarium: American College of Cardiology (Associate Editor for Innovations, acc.org). The remaining authors have no disclosures to report.
Supporting information
Tables S1–S9
Figure S1
Supplementary Material for this article is available at https://www.ahajournals.org/doi/suppl/10.1161/JAHA.121.021361
For Sources of Funding and Disclosures, see page 8.
References
- 1. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396:1204–1222. doi: 10.1016/S0140-6736(20)30925-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Michos ED, Choi AD. Coronary artery disease in young adults: a hard lesson but a good teacher. J Am Coll Cardiol. 2019;74:1879–1882. doi: 10.1016/j.jacc.2019.08.1023 [DOI] [PubMed] [Google Scholar]
- 3. Collet J‐P, Zeitouni M, Procopi N, Hulot J‐S, Silvain J, Kerneis M, Thomas D, Lattuca B, Barthelemy O, Lavie‐Badie Y, et al. Long‐term evolution of premature coronary artery disease. J Am Coll Cardiol. 2019;74:1868–1878. doi: 10.1016/j.jacc.2019.08.1002 [DOI] [PubMed] [Google Scholar]
- 4. Gupta A, Wang Y, Spertus JA, Geda M, Lorenze N, Nkonde‐Price C, D'Onofrio G, Lichtman JH, Krumholz HM. Trends in acute myocardial infarction in young patients and differences by sex and race, 2001 to 2010. J Am Coll Cardiol. 2014;64:337–345. doi: 10.1016/j.jacc.2014.04.054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Head SJ, Milojevic M, Taggart DP, Puskas JD. Current practice of state‐of‐the‐art surgical coronary revascularization. Circulation. 2017;136:1331–1345. doi: 10.1161/CIRCULATIONAHA.116.022572 [DOI] [PubMed] [Google Scholar]
- 6. Head SJ, Milojevic M, Daemen J, Ahn J‐M, Boersma E, Christiansen EH, Domanski MJ, Farkouh ME, Flather M, Fuster V, et al. Mortality after coronary artery bypass grafting versus percutaneous coronary intervention with stenting for coronary artery disease: a pooled analysis of individual patient data. Lancet. 2018;391:939–948. doi: 10.1016/S0140-6736(18)30423-9 [DOI] [PubMed] [Google Scholar]
- 7. Mark DB, Knight JD, Velazquez EJ, Wasilewski J, Howlett JG, Smith PK, Spertus JA, Rajda M, Yadav R, Hamman BL, et al. Quality‐of‐life outcomes with coronary artery bypass graft surgery in ischemic left ventricular dysfunction. Ann Intern Med. 2014;161:392. doi: 10.7326/M13-1380 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Dalén M, Ivert T, Holzmann MJ, Sartipy U. Coronary artery bypass grafting in patients 50 years or younger: a Swedish nationwide cohort study. Circulation. 2015;131:1748–1754. doi: 10.1161/CIRCULATIONAHA.114.014335 [DOI] [PubMed] [Google Scholar]
- 9. Biancari F, Gudbjartsson T, Heikkinen J, Anttila V, Mäkikallio T, Jeppsson A, Thimour‐Bergström L, Mignosa C, Rubino AS, Kuttila K, et al. Comparison of 30‐day and 5‐year outcomes of percutaneous coronary intervention versus coronary artery bypass grafting in patients aged≤50 years (the Coronary aRtery diseAse in younG adultS Study). Am J Cardiol. 2014;114:198–205. doi: 10.1016/j.amjcard.2014.04.025 [DOI] [PubMed] [Google Scholar]
- 10. Zimmerman FH, Cameron A, Fisher LD, Ng G. Myocardial infarction in young adults: angiographic characterization, risk factors and prognosis (Coronary Artery Surgery Study Registry). J Am Coll Cardiol. 1995;26:654–661. doi: 10.1016/0735-1097(95)00254-2 [DOI] [PubMed] [Google Scholar]
- 11. Databases HCUP; Healthcare Cost and Utilization Project (HCUP) . Overview of the National (Nationwide) Inpatient Sample (NIS). Available at: www.hcup‐us.ahrq.gov/nisoverview.jsp. Accessed December 25, 2020.
- 12. Heterogeneous trends in burden of heart disease mortality by subtypes in the United States, 1999–2018: observational analysis of vital statistics. BMJ. 2020;370:m2688. doi: 10.1161/CIR.0000000000000757 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Becker ER, Granzotti AM. Trends in in‐hospital coronary artery bypass surgery mortality by gender and race/ethnicity –1998‐2015: why do the differences remain? J Natl Med Assoc. 2019;111:527–539. doi: 10.1016/j.jnma.2019.04.009 [DOI] [PubMed] [Google Scholar]
- 14. Alkhouli M, Alqahtani F, Kalra A, Gafoor S, Alhajji M, Alreshidan M, Holmes DR, Lerman A. Trends in characteristics and outcomes of hospital inpatients undergoing coronary revascularization in the United States, 2003–2016. JAMA Netw Open. 2020;3:e1921326. doi: 10.1001/jamanetworkopen.2019.21326 [DOI] [PubMed] [Google Scholar]
- 15. Mosca L, Ferris A, Fabunmi R, Robertson RM. Tracking women's awareness of heart disease: an American Heart Association national study. Circulation. 2004;109:573–579. doi: 10.1161/01.CIR.0000115222.69428.C9 [DOI] [PubMed] [Google Scholar]
- 16. United States Department of Labor. Bureau of Labor Statistics . Consumer Price Index (CPI) Databases:CPI Inflation Calculator. 2021. Available at: https://www.bls.gov/data/inflation_calculator.htm. Accessed January 15, 2021.
- 17. National Center for Health Statistics, CDC . About underlying cause of death 1999–2018. Available at: https://wonder.cdc.gov/wonder/help/ucd.html at 02/10/2020. Accessed 7/1/2020.
- 18. Goel K, Gupta T, Gulati R, Bell MR, Kolte D, Khera S, Bhatt DL, Rihal CS, Holmes DR Jr. Temporal trends and outcomes of percutaneous coronary interventions in nonagenarians: a national perspective. JACC Cardiovasc Interv. 2018;11:1872–1882. doi: 10.1016/j.jcin.2018.06.026 [DOI] [PubMed] [Google Scholar]
- 19. STATA . Stata Corporation. 2020. [computer program]. [Google Scholar]
- 20. Culler SD, Kugelmass AD, Brown PP, Reynolds MR, Simon AW. Trends in coronary revascularization procedures among Medicare beneficiaries between 2008 and 2012. Circulation. 2015;131:362–370; discussion 370. doi: 10.1161/CIRCULATIONAHA.114.012485 [DOI] [PubMed] [Google Scholar]
- 21. Medicaid expansion and state trends in supplemental security income program participation. Health Aff (Millwood). 2017;36:1485–1488. doi: 10.1377/hlthaff.2016.1632 [DOI] [PubMed] [Google Scholar]
- 22. Behavioral Risk Factor Surveillance System: Center for Disease Control and Prevention. 2020.
- 23. @CDCgov . Heart Disease Statistical Reports for Health Professionals | cdc.gov. 2019. Available at: https://www.cdc.gov/heartdisease/statistical_reports.htm. Accessed December 25, 2020.
- 24. Yeh RW, Sidney S, Chandra M, Sorel M, Selby JV, Go AS. Population trends in the incidence and outcomes of acute myocardial infarction. N Engl J Med. 2010;362:2155–2165. doi: 10.1056/NEJMoa0908610 [DOI] [PubMed] [Google Scholar]
- 25. Krumholz HM, Normand S‐LT, Wang Y. Trends in hospitalizations and outcomes for acute cardiovascular disease and stroke, 1999–2011. Circulation. 2014;130:966–975. doi: 10.1161/CIRCULATIONAHA.113.007787 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. George MG, Tong X, Bowman BA. Prevalence of cardiovascular risk factors and strokes in younger adults. JAMA Neurol. 2017;74:695. doi: 10.1001/jamaneurol.2017.0020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Mack MJ, Brown PP, Kugelmass AD, Battaglia SL, Tarkington LG, Simon AW, Culler SD, Becker ER. Current status and outcomes of coronary revascularization 1999 to 2002: 148,396 surgical and percutaneous procedures. Ann Thorac Surg. 2004;77:761–766; discussion 766‐768. doi: 10.1016/j.athoracsur.2003.06.019 [DOI] [PubMed] [Google Scholar]
- 28. Serruys PW, Cavalcante R, Collet C, Kappetein AP, Sabik JF III, Banning AP, Taggart DP, Sabaté M, Pomar J, Boonstra PW, et al. Outcomes after coronary stenting or bypass surgery for men and women with unprotected left main disease: the EXCEL trial. JACC Cardiovasc Interv. 2018;11:1234–1243. doi: 10.1016/j.jcin.2018.03.051 [DOI] [PubMed] [Google Scholar]
- 29. Vikulova DN, Grubisic M, Zhao Y, Lynch K, Humphries KH, Pimstone SN, Brunham LR. Premature atherosclerotic cardiovascular disease: trends in incidence, risk factors, and sex‐related differences, 2000 to 2016. J Am Heart Assoc. 2019;8:e012178. doi: 10.1161/JAHA.119.012178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Yandrapalli S, Nabors C, Goyal A, Aronow WS, Frishman WH. Modifiable risk factors in young adults with first myocardial infarction. J Am Coll Cardiol. 2019;73:573–584. doi: 10.1016/j.jacc.2018.10.084 [DOI] [PubMed] [Google Scholar]
- 31. Vaccarino V, Abramson JL, Veledar E, Weintraub WS. Sex differences in hospital mortality after coronary artery bypass surgery. Circulation. 2002;105:1176–1181. doi: 10.1161/hc1002.105133 [DOI] [PubMed] [Google Scholar]
- 32. Loop FD, Golding LR, MacMillan JP, Cosgrove DM, Lytle BW, Sheldon WC. Coronary artery surgery in women compared with men: analyses of risks and long‐term results. J Am Coll Cardiol. 1983;1:383–390. doi: 10.1016/S0735-1097(83)80064-3 [DOI] [PubMed] [Google Scholar]
- 33. Gardner TJ, Horneffer PJ, Gott VL, Watkins L Jr, Baumgartner WA, Borkon AM, Reitz BA. Coronary artery bypass grafting in women. A ten‐year perspective. Ann Surg. 1985;201:780–784. doi: 10.1097/00000658-198506000-00016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Cushman M, Shay CM, Howard VJ, Jiménez MC, Lewey J, McSweeney JC, Newby LK, Poudel R, Reynolds HR, Rexrode KM, et al. Ten‐year differences in women's awareness related to coronary heart disease: results of the 2019 American Heart Association National Survey: a special report from the American Heart Association. Circulation. 2021;143:e239–e248. doi: 10.1161/CIR.0000000000000907 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Arora S, Stouffer GA, Kucharska‐Newton AM, Qamar A, Vaduganathan M, Pandey A, Porterfield D, Blankstein R, Rosamond WD, Bhatt DL, et al. Twenty year trends and sex differences in young adults hospitalized with acute myocardial infarction. Circulation. 2019;139:1047–1056. doi: 10.1161/CIRCULATIONAHA.118.037137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Mauvais‐Jarvis F, Bairey Merz N, Barnes PJ, Brinton RD, Carrero J‐J, DeMeo DL, De Vries GJ, Epperson CN, Govindan R, Klein SL, et al. Sex and gender: modifiers of health, disease, and medicine. Lancet. 2020;396:565–582. doi: 10.1016/S0140-6736(20)31561-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. DeFilippis EM, Collins BL, Singh A, Biery DW, Fatima A, Qamar A, Berman AN, Gupta A, Cawley M, Wood MJ, et al. Women who experience a myocardial infarction at a young age have worse outcomes compared with men: the Mass General Brigham YOUNG‐MI registry. Eur Heart J. 2020;41:4127–4137. doi: 10.1093/eurheartj/ehaa662 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Blankstein R, Ward RP, Arnsdorf M, Jones B, Lou YB, Pine M. Female gender is an independent predictor of operative mortality after coronary artery bypass graft surgery: contemporary analysis of 31 Midwestern hospitals. Circulation. 2005;112:I323–327. doi: 10.1161/CIRCULATIONAHA.104.525139 [DOI] [PubMed] [Google Scholar]
- 39. Greenwood BN, Carnahan S, Huang L. Patient‐physician gender concordance and increased mortality among female heart attack patients. Proc Natl Acad Sci USA. 2018;115:8569–8574. doi: 10.1073/pnas.1800097115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Carnethon MR, Pu J, Howard G, Albert MA, Anderson CAM, Bertoni AG, Mujahid MS, Palaniappan L, Taylor HA Jr, Willis M, et al. Cardiovascular health in African Americans: a scientific statement from the American Heart Association. Circulation. 2017;136:e393–e423. doi: 10.1161/CIR.0000000000000534 [DOI] [PubMed] [Google Scholar]
- 41. Virani Salim S, Alonso A, Benjamin Emelia J, Bittencourt MS, Callaway CW, Carson AP, Chamberlain AM, Chang AR, Cheng S, Delling FN, American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee, et al. Heart disease and stroke statistics—2020 update: a report from the American Heart Association. Circulation. 2020;141:e139–e596. doi: 10.1161/CIR.0000000000000757 [DOI] [PubMed] [Google Scholar]
- 42. Hamad R, Penko J, Kazi DS, Coxson P, Guzman D, Wei PC, Mason A, Wang EA, Goldman L, Fiscella K, et al. Association of low socioeconomic status with premature coronary heart disease in US adults. JAMA Cardiol. 2020;5:899–908. doi: 10.1001/jamacardio.2020.1458 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Angraal S, Khera R, Wang Y, Lu Y, Jean R, Dreyer RP, Geirsson A, Desai NR, Krumholz HM. Sex and race differences in the utilization and outcomes of coronary artery bypass grafting among Medicare beneficiaries, 1999–2014. J Am Heart Assoc. 2018;7:e009014. doi: 10.1161/JAHA.118.009014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Churchwell K, Elkind MSV, Benjamin RM, Carson AP, Chang EK, Lawrence W, Mills A, Odom TM, Rodriguez CJ, Rodriguez F, et al. Call to action: structural racism as a fundamental driver of health disparities: a presidential advisory from the American Heart Association. Circulation. 2020;142:e454–e468. doi: 10.1161/CIR.0000000000000936 [DOI] [PubMed] [Google Scholar]
- 45. McNeely C, Markwell S, Vassileva C. Trends in patient characteristics and outcomes of coronary artery bypass grafting in the 2000 to 2012 Medicare population. Ann Thorac Surg. 2016;102:132–138. doi: 10.1016/j.athoracsur.2016.01.016 [DOI] [PubMed] [Google Scholar]
- 46. Boden WE, O'Rourke RA, Teo KK, Hartigan PM, Maron DJ, Kostuk WJ, Knudtson M, Dada M, Casperson P, Harris CL, et al. Optimal medical therapy with or without PCI for stable coronary disease. N Engl J Med. 2007;356:1503–1516. doi: 10.1056/NEJMoa070829 [DOI] [PubMed] [Google Scholar]
- 47. Frye RL, August P, Brooks MM, Hardison RM, Kelsey SF, MacGregor JM, Orchard TJ, Chaitman BR, Genuth SM, Goldberg SH, et al. A randomized trial of therapies for type 2 diabetes and coronary artery disease. N Engl J Med. 2009;360:2503–2515. doi: 10.1056/NEJMoa0805796 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Desai NR, Bradley SM, Parzynski CS, Nallamothu BK, Chan PS, Spertus JA, Patel MR, Ader J, Soufer A, Krumholz HM, et al. Appropriate use criteria for coronary revascularization and trends in utilization, patient selection, and appropriateness of percutaneous coronary intervention. JAMA. 2015;314:2045–2053. doi: 10.1001/jama.2015.13764 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Wasfy JH, Borden WB, Secemsky EA, Mccabe JM, Yeh RW. Public reporting in cardiovascular medicine. Circulation. 2015;131:1518–1527. doi: 10.1161/CIRCULATIONAHA.114.014118 [DOI] [PubMed] [Google Scholar]
- 50. Epstein AJ, Polsky D, Yang F, Yang L, Groeneveld PW. Coronary revascularization trends in the United States, 2001–2008. JAMA. 2011;305:1769–1776. doi: 10.1001/jama.2011.551 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. National Summary of Inpatient Charge Data by Medicare Severity Diagnosis Related Group (MS‐DRG), FY2018 | Data.CMS.gov. Created November 10, 2020. Available at: https://data.cms.gov/Medicare‐Inpatient/National‐Summary‐of‐Inpatient‐Charge‐Data‐by‐Medic/5k9u‐5g92. Accessed December 25, 2020.
- 52. Eisenberg MJ, Filion KB, Azoulay A, Brox AC, Haider S, Pilote L. Outcomes and cost of coronary artery bypass graft surgery in the United States and Canada. Arch Intern Med. 2005;165:1506. doi: 10.1001/archinte.165.13.1506 [DOI] [PubMed] [Google Scholar]
- 53. Cohen DJ, Osnabrugge RL, Magnuson EA, Wang K, Li H, Chinnakondepalli K, Pinto D, Abdallah MS, Vilain KA, Morice M‐C, et al. Cost‐effectiveness of percutaneous coronary intervention with drug‐eluting stents versus bypass surgery for patients with 3‐vessel or left main coronary artery disease. Circulation. 2014;130:1146–1157. doi: 10.1161/CIRCULATIONAHA.114.009985 [DOI] [PubMed] [Google Scholar]
- 54. Giacomino BD, Cram P, Vaughan‐Sarrazin M, Zhou Y, Girotra S. Association of hospital prices for coronary artery bypass grafting with hospital quality and reimbursement. Am J Cardiol. 2016;117:1101–1106. doi: 10.1016/j.amjcard.2016.01.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Tables S1–S9
Figure S1


