Abstract
Background
Critical limb ischemia (CLI) represents the most severe form of peripheral artery disease and is associated with significant mortality and morbidity. Contemporary data comparing the sex differences in trends, revascularization strategies, and in‐hospital outcomes among patients with CLI are scarce.
Methods and Results
Using the National Inpatient Sample database years 2002 to 2015, we identified hospitalizations for CLI. Temporal trends for hospitalizations for CLI were evaluated. The differences in demographics, revascularization, and in‐hospital outcomes between both sexes were compared. Among 2 400 778 CLI hospitalizations, 43.6% were women. Women were older and had a higher prevalence of obesity, hypertension, heart failure, and prior stroke. Women were also less likely to receive any revascularization (34.7% versus 35.4%, P<0.001), but the trends of revascularization have been increasing among both sexes. Revascularization was associated with lower in‐hospital mortality among women (adjusted odds ratio [OR], 0.76; 95% CI, 0.71–0.81) and men (adjusted OR, 0.69; 95% CI, 0.65–0.73). On multivariable analysis adjusting for patient‐ and hospital‐related characteristics as well as revascularization, women had a higher incidence of in‐hospital mortality, postoperative hemorrhage, need for blood transfusion, postoperative infection, ischemic stroke, and discharge to facilities compared with men.
Conclusions
In this nationwide contemporary analysis of CLI hospitalizations, women were older and less likely to undergo revascularization. Women had a higher incidence of in‐hospital mortality and bleeding complications compared with men. Sex‐specific studies and interventions are needed to minimize these gaps among this high‐risk population.
Keywords: critical limb ischemia, mortality, revascularization, sex, women
Subject Categories: Peripheral Vascular Disease, Vascular Disease
Nonstandard Abbreviations and Acronyms
- AKI
acute kidney injury
- CLI
critical limb ischemia
- NIS
National Inpatient Sample
Clinical Perspective
What Is New?
In this nationwide analysis of critical limb ischemia hospitalizations, women were older and less likely to undergo revascularization.
Women with critical limb ischemia had a higher incidence of adjusted in‐hospital mortality, bleeding complications, and discharge to facilities compared with men.
Endovascular revascularization was associated with lower adjusted in‐hospital mortality among both women and men compared with surgical revascularization.
What Are the Clinical Implications?
Sex‐specific studies and interventions are needed to minimize these gaps among patients with critical limb ischemia.
Lower extremity peripheral artery disease (PAD) affects millions of patients worldwide and carries significant morbidity and mortality. 1 Studies suggest that the prevalence of PAD is comparable among women and men, 1 yet women are less frequently diagnosed and treated. 1 , 2 Importantly, women have been underrepresented in clinical registries and trials of PAD. 3 , 4 , 5 , 6 This has led to a Call to Action by the American Heart Association recommending further sex‐specific studies related to PAD. 3
Critical limb ischemia (CLI) represents the most severe form of PAD and is associated with considerable morbidity including limb loss, impaired quality of life, and mortality if not adequately managed. 7 Studies suggest that women are more likely to present with advanced and multivessel PAD. 8 , 9 Few studies have explored the sex‐specific differences in presentation, revascularization, and outcomes among patients with PAD. 6 , 8 , 10 , 11 , 12 However, studies examining the sex‐specific differences among patients with CLI have focused mainly on outcomes after surgical intervention. 13 , 14 With the advancements in endovascular techniques, the use of percutaneous revascularization has increased exponentially for appropriate patients with CLI. 15 To better address these knowledge gaps, we aimed to investigate the trends and revascularization strategies, and to compare in‐hospital outcomes among women and men with CLI using a large nationally representative database.
Methods
Data that support the findings of this study are available from the corresponding author upon reasonable request.
Data Source
Data for this investigation were obtained from the National Inpatient Sample (NIS) database for January 2002 through September 2015. The NIS is part of the Healthcare Cost and Utilization Project, sponsored by the Agency for Healthcare Research and Quality. 16 The NIS is the largest inpatient‐care database in the United States. The NIS contains discharge data from a ≈20% stratified sample of US hospitals through 2012. Since 2012, the NIS represents a sample of 20% discharges from all hospitals. 16 The NIS provides a weight variable for establishing an estimate of national statistics. Because the NIS is a public database containing deidentified information, this study was exempt from institutional review board approval.
Study Population
Hospitalizations for adults aged ≥18 years with primary International Classification of Diseases, Ninth Revision, Clinical Modification (ICD‐9‐CM) diagnostic codes for CLI were identified (Table S1). 17 , 18 Using ICD‐9‐CM procedure codes, we identified hospitalizations receiving endovascular revascularization (peripheral balloon angioplasty, atherectomy, or stent placement), surgical revascularization, and combined endovascular/surgical revascularization (ie, hybrid revascularization) (Table S1). 17 , 18 Cases with missing data on sex indicator or any of the study outcomes were excluded.
Patient and Hospital Characteristics
Baseline characteristics included patient demographics, relevant comorbidities (eg, hypertension, hyperlipidemia, diabetes, coronary artery disease, cardiomyopathy, heart failure, valvular heart disease, obesity, smoking history, chronic kidney disease, prior myocardial infarction, previous percutaneous coronary intervention, previous coronary artery bypass grafting, and prior stroke) were identified using corresponding ICD‐9‐CM codes. A list of ICD‐9‐CM codes used to identify the comorbidities and therapies is summarized in Table S1. Hospital‐related characteristics included bed size (small, medium, and large), location (urban versus rural), hospital region (Northeast, Midwest, South, and West), and teaching status.
Outcome Measures
The temporal trends in hospitalizations and revascularization modalities in women versus men presenting with CLI were reported. The main study outcome was in‐hospital mortality. Other secondary outcomes included amputation‐free survival (defined as freedom from death or major amputation during the hospitalization), major amputation, minor amputation, postoperative infection, postoperative hemorrhage, acute stroke, and acute kidney injury (AKI). Procedures and inpatient outcomes were abstracted and reported using ICD‐9‐CM Clinical Classifications Software codes and Elixhauser comorbidities as reported by the Healthcare Cost and Utilization Project (Table S1).
Statistical Analysis
Discharge (trend) weights were used to compute national estimates. As per Healthcare Cost and Utilization Project regulations, all analyses were conducted using the complex sample feature of SPSS software (IBM, Armonk, NY), which accounts for discharge weights, hospital clustering, and stratification across the NIS database. 19 Categorical variables were compared using the χ2 test and reported as numbers and percentages. Continuous variables were compared using the Student t test or Mann‐Whitney U test depending on the distribution curve and were reported as mean±standard deviation or median and interquartile range depending on the distribution curve. Trend analyses were performed using linear regression analysis or curvilinear regression analysis depending on the shape of the curve. 20
Multivariable regression analysis was conducted to adjust for in‐hospital outcomes for CLI in women versus men. The model included the following 25 variables: age, race, diabetes, hypertension, obesity, history of heart failure, chronic lung disease, pulmonary circulation disorders, chronic liver disease, chronic kidney disease, chronic anemia, coagulopathy, hypothyroidism, history of smoking, coronary artery disease, prior myocardial infarction, history of implantable cardiac defibrillator, history of cardiac pacemaker, prior stroke, prior percutaneous coronary intervention, prior previous coronary artery bypass grafting, hospital bed size, hospital region, hospital teaching status, and the revascularization modality. In hospitalizations with missing covariates, multivariable regression analyses were performed on complete cases. All variables were forced into the multivariable model using the enter method. A secondary propensity‐score matching analysis was conducted to compare the in‐hospital outcomes between women and men. The matching was performed using the MatchIt R package (R software; R Foundation for Statistical Computing, Vienna, Austria). Each case was matched to a control that was closest in terms of the calculated propensity score, using the nearest neighbor technique, with a caliper width of 0.2. The propensity score was calculated from the same patient‐ and hospital‐related variables used in the regression models. Subgroup analyses according to age (ie, <50 versus ≥50 years) and hospital location (ie, urban versus rural) were also performed to compare in‐hospital mortality and postoperative hemorrhage.
To compare the outcomes of endovascular versus surgical revascularization, a propensity‐score matching model was used to reduce the risk of selection bias. The matching was performed using MatchIt R package. Each case was matched to a control that was closest in terms of calculated propensity score, using the nearest neighbor technique, with a caliper width of 0.2. The propensity score was calculated from the same patient‐ and hospital‐related variables in the regression models, except for revascularization modality (Table S2). Associations were considered significant if the P value was ≤0.05. We used the SPSS version 24.0 software and R software for all statistical analyses.
Results
Study Cohort
Between January 2002 and September 2015, there were 2 401 110 hospitalizations with a primary diagnosis of CLI. After excluding cases with missing data on sex indicator (n=15) or missing study outcomes (n=317), the final analysis included 2 400 778 hospitalizations; 1 047 406 (43.6%) were women. Women with CLI were older and less likely White or Hispanic. Women had a higher prevalence of obesity, hypertension, heart failure, and prior stroke. Women had a lower prevalence of smoking, diabetes, coronary artery disease, prior myocardial infarction, prior percutaneous coronary intervention, and prior coronary artery bypass grafting. Table 1 summarizes the baseline patient‐ and hospital‐related characteristics.
Table 1.
Baseline Patient‐ and Hospital‐Related Characteristics Among Women Versus Men With Critical Limb Ischemia
| Women, n=1 047 406, n (%) | Men, n=1 353 704, n (%) | P value | |
|---|---|---|---|
| Age, y, mean±SD | 72.1±13.6 | 68.4±12.7 | <0.001 |
| Race/ethnicity | |||
| White | 568 880 (64.3) | 787 021 (68.3) | <0.001 |
| Black | 192 047 (21.7) | 193 687 (16.8) | |
| Hispanic | 84 499 (9.6) | 120 872 (10.5) | |
| Asian/Pacific Islander | 12 763 (1.4) | 15 296 (1.3) | |
| Other races* | 6034 (0.7) | 7460 (0.6) | |
| Smoking | 131 176 (12.5) | 236 664 (17.5) | <0.001 |
| Obesity | 113 734 (11.0) | 113 360 (8.4) | <0.001 |
| Hypertension | 745 948 (71.9) | 934 893 (69.7) | <0.001 |
| Hypothyroidism | 152 436 (14.7) | 83 464 (6.2) | <0.001 |
| Chronic kidney disease | 288 973 (27.80) | 428 639 (31.90) | <0.001 |
| Chronic liver disease | 14 806 (1.4) | 33 803 (2.5) | <0.001 |
| Diabetes | 505 219 (48.7) | 716 988 (53.4) | <0.001 |
| Anemia | 300 542 (29.0) | 351 124 (26.2) | <0.001 |
| Heart failure | 209 416 (20.2) | 258 830 (19.3) | <0.001 |
| Chronic pulmonary disease | 240 267 (23.20) | 311 715 (23.20) | 0.57 |
| Valvular disease | 63 038 (6.1) | 67 849 (5.1) | <0.001 |
| Coronary artery disease | 394 495 (37.7) | 621 865 (45.9) | <0.001 |
| Prior myocardial infarction | 82 195 (7.8) | 137 245 (10.1) | <0.001 |
| Prior coronary artery bypass surgery | 92 077 (8.8) | 203 383 (15.0) | <0.001 |
| Prior implantable cardioverter defibrillator | 9691 (0.9) | 33 573 (2.5) | <0.001 |
| Prior cardiac pacemaker | 36 750 (3.5) | 51 878 (3.8) | <0.001 |
| Prior percutaneous coronary intervention | 54 461 (5.2) | 88 076 (6.5) | <0.001 |
| Prior stroke | 53 207 (5.1) | 65 248 (4.8) | <0.001 |
| Coagulopathy | 35 319 (3.4) | 53 133 (4.0) | <0.001 |
| Pulmonary circulation disease | 28 643 (2.80) | 27 175 (2.00) | <0.001 |
| Hospital‐related characteristics | |||
| Hospital bed size | |||
| Small sized | 121 579 (11.6) | 153 550 (11.4) | <0.001 |
| Medium sized | 268 472 (25.7) | 339 944 (25.2) | |
| Large sized | 654 481 (62.7) | 856 433 (63.4) | |
| Hospital region | |||
| Northeast | 218 917 (20.9) | 284 809 (21.0) | <0.001 |
| Midwest or North Central | 243 442 (23.2) | 313 211 (23.1) | |
| South | 417 892 (39.9) | 529 978 (39.2) | |
| West | 167 157 (16.0) | 225 372 (16.7) | |
| Hospital teaching status | |||
| Rural | 107 021 (10.2) | 131 045 (9.7) | <0.001 |
| Urban nonteaching | 425 875 (40.8) | 544 454 (40.3) | |
| Urban teaching | 511 636 (49.0) | 674 428 (50.0) | |
Term used by Healthcare Cost and Utilization Project (HCUP) database.
Women were less likely to receive any revascularization during the index admission (34.7% versus 35.4%, P<0.001). Compared with nonrevascularized patients, women undergoing any revascularization had a lower incidence of in‐hospital mortality (2.6% versus 4.2%; adjusted odds ratio [OR], 0.76; 95% CI, 0.71–0.81; P<0.001) as well as men (2.2% versus 3.8%; adjusted OR, 0.69; 95% CI, 0.65–0.73; P<0.001). Women were more likely to receive endovascular revascularization (15.9% versus 14.7%, P<0.001) and less likely to receive surgical revascularization (12.5% versus 13.7%, P<0.001) compared with men.
Trends in Hospitalizations for CLI Hospitalizations and Revascularization Strategies
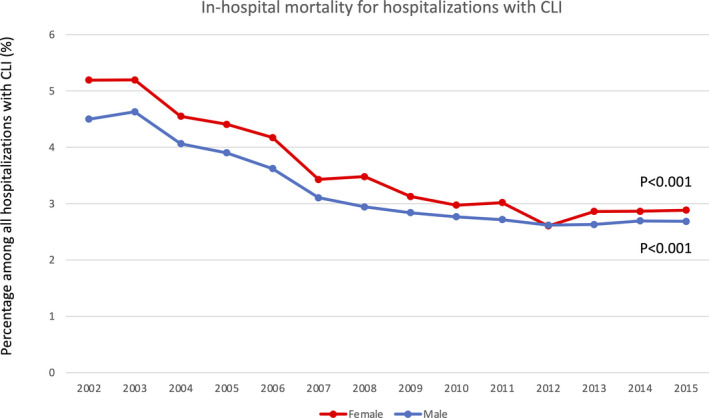
During the study period, the rates of CLI hospitalizations did not change among women (82 706 in 2002 versus 75 193 in 2015, P trend=0.10) but increased among men (95 456 in 2002 versus 111 573 in 2015, P trend<0.001) (Figure 1). There was a decrease in the rates of in‐hospital mortality among women (5.2% in 2002 versus 2.9% in 2015, P trend<0.001) and men (4.5% in 2002 versus 2.7% in 2015, P trend<0.001) (Figure 2).
Figure 1. Summary for the findings of the study.
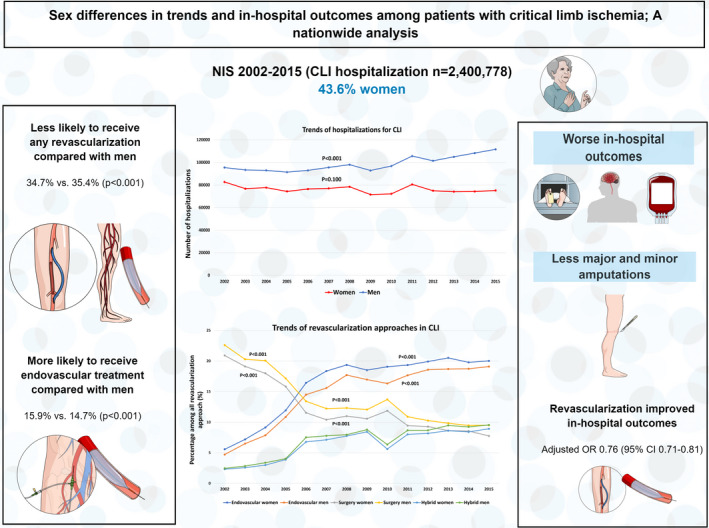
Temporal trend in hospitalizations and revascularization modalities for critical limb ischemia (CLI) among women and men. NIS, National Inpatient Sample; OR, odds ratio.
Figure 2. Temporal trends of in‐hospital mortality for hospitalization with critical limb ischemia (CLI) among women and men.
There has been an increase in total revascularization regardless of strategy among women (28.8% in 2002 versus 36.7% in 2015, P trend<0.001) and men (29.8% in 2002 versus 38.1% in 2015, P trend<0.001). Among women, both endovascular revascularization (5.6% in 2002 versus 20.0% in 2015, P trend<0.001) and hybrid revascularization (2.3% in 2002 versus 8.9% in 2015, P trend<0.001) increased, but surgical revascularization decreased (20.9% in 2002 versus 7.7% in 2015, P trend<0.001). A similar pattern was observed among men with an observed increase in both endovascular revascularization (4.7% in 2002 versus 19.1% in 2015, P trend<0.001) and hybrid revascularization (2.5% in 2002 versus 9.5% in 2015, P trend<0.001), but a reduction in surgical revascularization (22.6% in 2002 versus 9.5% in 2015, P trend<0.001) (Figure 1).
In‐Hospital Outcomes
In the unadjusted analysis, women had a higher incidence of in‐hospital mortality, postoperative hemorrhage, need for blood transfusion, postoperative infection, ischemic stroke, and discharge to facilities compared with men. Women were less likely to undergo major or minor amputations and had a lower incidence of AKI but a higher incidence of amputation‐free survival (Table 2). These findings remained consistent in the multivariable logistic regression model adjusting for the patient‐ and hospital‐related characteristics as well as the revascularization strategy. The secondary analysis using the propensity‐score matching model also demonstrated similar findings (Table S3). Women had higher rates of in‐hospital mortality across the various racial and ethnic groups (Table S4).
Table 2.
In‐Hospital Outcomes Among Women Versus Men With Critical Limb Ischemia
| Outcome | Incidences, % | Unadjusted odds ratio | 95% CI | Adjusted odds ratio* | 95% CI | P value | |
|---|---|---|---|---|---|---|---|
| Women | Men | ||||||
| Mortality | 3.7 | 3.2 | 1.13 | 1.10–1.17 | 1.07 | 1.03–1.11 | <0.001 |
| Amputation‐free survival | 81.9 | 81.2 | 1.05 | 1.03–1.06 | 1.10 | 1.10–1.12 | <0.001 |
| Major amputation | 15.3 | 16.3 | 0.92 | 0.91–0.94 | 0.88 | 0.86–0.89 | <0.001 |
| Minor amputation | 9.8 | 14.7 | 0.63 | 0.62–0.65 | 0.66 | 0.65–0.67 | <0.001 |
| Postoperative infection | 2.2 | 2.0 | 1.10 | 1.06–1.15 | 1.20 | 1.14–1.25 | <0.001 |
| Postoperative hemorrhage | 8.0 | 7.0 | 1.16 | 1.13–1.18 | 1.19 | 1.16–1.22 | <0.001 |
| Blood transfusion | 18.1 | 15.6 | 1.19 | 1.17–1.21 | 1.17 | 1.15–1.19 | <0.001 |
| Acute myocardial infarction | 2.9 | 3.1 | 0.95 | 0.92–0.99 | 1.02 | 0.98–1.06 | 0.24 |
| Ischemic stroke | 0.9 | 0.7 | 1.27 | 1.19–1.35 | 1.20 | 1.12–1.29 | <0.001 |
| Acute kidney injury | 11.2 | 12.5 | 0.88 | 0.87–0.90 | 0.86 | 0.84–0.88 | <0.001 |
| Facility discharge | 40.2 | 35.2 | 1.24 | 1.22–1.25 | 1.04 | 1.03–1.06 | <0.001 |
Multivariate logistic regression model adjusting for patient‐ and hospital‐related characteristics and revascularization strategy.
On subgroup analysis according to age, women aged ≥50 years had higher adjusted in‐hospital mortality compared with men (adjusted OR, 1.08; 95% CI, 1.04–1.12), but there was no difference in the adjusted in‐hospital mortality rates between women and men aged <50 years (adjusted OR, 1.07; 95% CI, 0.87–1.32). In addition, women had higher adjusted postoperative hemorrhage in the subgroup of those aged ≥50 years (adjusted OR, 1.19; 95% CI, 1.16–1.22) and <50 years (adjusted OR, 1.23; 95% CI, 1.10–1.37) compared with men (Figure S1). Women aged ≥50 years had higher adjusted in‐hospital mortality rates (adjusted OR, 2.55; 95% CI, 2.12–3.06) and postoperative hemorrhage (adjusted OR, 1.15; 95% CI 1.03–1.28) compared with women aged <50 years.
Among admissions in urban areas, adjusted in‐hospital mortality (adjusted OR, 1.08; 95% CI, 1.04–1.12) and postoperative hemorrhage (adjusted OR, 1.19; 95% CI, 1.16–1.22) was higher in women versus men. However, there was no significant difference in in‐hospital mortality between women versus men in rural areas (adjusted OR, 0.97; 95% CI, 0.84–1.10) (Figure S1).
Outcomes of Endovascular Versus Surgical Revascularization
Among women with CLI who underwent either endovascular or surgical intervention (n=297 658), 128 604 who had endovascular revascularization were matched with 127 353 who had surgical revascularization. The absolute standardized differences for the patient‐ and hospital‐related characteristics were <10% in both groups (Figure S2A). Compared with surgical revascularization, endovascular revascularization was associated with a lower incidence of in‐hospital mortality, minor amputation, postoperative hemorrhage, need for blood transfusion, postoperative infection, and discharge to facilities, but a higher incidence of major amputation and AKI (Table 3). In addition, endovascular revascularization was associated with a shorter length of stay (5 days [interquartile range, 2–10 days] versus 7 days [interquartile range, 4–13 days], P<0.001).
Table 3.
Propensity‐Matched Outcomes of Endovascular Versus Surgical Revascularization Among Women With Critical Limb Ischemia
| Outcome | Incidences, % | Odds ratio | 95% CI | P value | |
|---|---|---|---|---|---|
| Endovascular | Surgical | ||||
| Mortality | 2.3 | 2.7 | 0.84 | 0.75–0.95 | 0.004 |
| Major amputation | 6.5 | 5.6 | 1.17 | 1.09–1.26 | <0.001 |
| Minor amputation | 11.7 | 12.5 | 0.93 | 0.88–0.98 | 0.01 |
| Postoperative infection | 1.2 | 3.2 | 0.37 | 0.33–0.43 | <0.001 |
| Postoperative hemorrhage | 10.1 | 16.1 | 0.58 | 0.55–0.62 | <0.001 |
| Blood transfusion | 14.0 | 29.4 | 0.39 | 0.37–0.41 | <0.001 |
| Acute kidney injury | 10.1 | 8.0 | 1.29 | 1.21–1.37 | <0.001 |
| Discharge to facility | 29.6 | 39.7 | 0.64 | 0.61–0.67 | <0.001 |
Similarly, propensity analysis matched 162 857 male patients with CLI undergoing endovascular revascularization and 161 498 undergoing surgical revascularization. There were minimal differences (ie, <10%) in the absolute standardized differences after matching (Figure 2B). Endovascular revascularization was associated with a lower incidence of in‐hospital mortality, postoperative hemorrhage, need for blood transfusion, postoperative infection, length of stay, and discharge to facilities, but a higher incidence of major amputation and AKI (Table 4).
Table 4.
Propensity‐Matched Outcomes of Endovascular Versus Surgical Revascularization Among Men With Critical Limb Ischemia
| Outcome | Incidences, % | Odds ratio | 95% CI | P value | |
|---|---|---|---|---|---|
| Endovascular | Surgical | ||||
| Mortality | 1.9 | 2.3 | 0.83 | 0.75–0.92 | 0.001 |
| Major amputation | 7.6 | 5.9 | 1.32 | 1.23–1.40 | <0.001 |
| Minor amputation | 18.2 | 17.8 | 1.02 | 0.98–1.07 | 0.28 |
| Postoperative infection | 1.2 | 2.7 | 0.43 | 0.38–0.48 | <0.001 |
| Postoperative hemorrhage | 7.5 | 12.9 | 0.55 | 0.52–0.58 | <0.001 |
| Blood transfusion | 11.1 | 22.4 | 0.43 | 0.41–0.46 | <0.001 |
| Acute kidney injury | 11.5 | 8.9 | 1.34 | 1.27–1.41 | <0.001 |
| Discharge to facility | 27.3 | 32.7 | 0.77 | 0.74–0.80 | <0.001 |
Discussion
In this nationally representative observational analysis of ≈2.4 million hospitalizations with CLI, we found that women with CLI were older and had a higher prevalence of certain cardiovascular risk factors such as obesity and hypertension compared with men. The rates of hospitalizations for CLI did not change among women but increased in men. Women with CLI were less likely to undergo any revascularization compared with men. Furthermore, women with CLI had a higher incidence of adjusted in‐hospital mortality, bleeding complications, and discharge to facilities compared with men. Endovascular revascularization was associated with lower adjusted in‐hospital mortality among women and men, compared with surgical revascularization. These findings suggest that although the rates of CLI might be higher among men, the prevalence of cardiovascular risk factors and revascularization‐related complications are likely higher among women, and women with CLI are less likely to receive any revascularization.
Prior studies exploring the sex differences among patients with PAD showed that women are older and have a higher prevalence of hypertension and obesity 10 , 11 ; however, these studies included only a small proportion of patients with CLI. Our findings extend this knowledge to a large cohort and confirm the trends seen in earlier studies. A prior analysis has shown that the rates of CLI hospitalizations remained constant from 2003 to 2011 in the United States. 17 In this study, we showed that the rates of CLI hospitalizations did not change among women but have modestly increased among men. This could be attributed to the hesitancy for hospital admittance in patients with CLI who are women or less serious presentation among women, requiring hospitalization less often. Similar to prior CLI studies that had a predominant male representation, 21 , 22 we found that the rates of revascularization were overall low (<35%), but lower among women compared with men. This is concerning given that revascularization has been associated with lower mortality, as demonstrated in our analysis, and improved quality of life in this high‐risk population. 7 , 21 This further highlights the sex‐related gaps in evidence‐based therapies that has been previously demonstrated in other cardiovascular diseases. 23 , 24 A previous analysis of the reduction of atherothrombosis for continued health (REACH) registry has shown that risk factor control is suboptimal among women compared with men with PAD. 25 Reassuringly, we found that the rates of in‐hospital mortality are decreasing among women and men. This might be related to the rise in the rates of revascularization procedures, as well as the improvements in secondary preventative strategies including smoking cessation, statin therapy, and cardiac rehabilitation. 15 , 21 , 26
Evidence on sex‐specific differences in the outcomes of patients with PAD have been controversial and mostly noncontemporary. 27 , 28 , 29 A sex‐specific analysis of the examining use of ticagrelor in peripheral artery disease (EUCLID) trial found that women had a lower risk of all‐cause mortality, but similar risk of limb adverse events at a mean of 30 months. 10 Among studies focusing on patients with PAD who underwent endovascular revascularization, women were found to have higher rates of bleeding and vascular complications. 8 However, the rate of in‐hospital mortality was similar in one study, 8 and long‐term mortality was higher among women in another study. 11 Studies evaluating sex‐specific differences among patients with CLI have been limited. 14 , 30 One study comparing the outcomes after surgical interventions showed that women had lower patency rates after bypass surgery. 14 Another single‐center study of 219 patients (44% women) demonstrated that women had higher rates of the composite of mortality, myocardial infarction, or stroke, and lower rates of postprocedural patency for infrainguinal endovascular interventions. 30 In our study, which focused on patients with CLI, we found that women had higher rates of in‐hospital mortality, bleeding complications, but a lower rate of amputations and AKI. Several factors could contribute to these findings, such as the smaller blood vessel diameter along with the higher prevalence of more complex and multilevel disease among women. 6 , 30 Importantly, we found that the higher rates of mortality and bleeding complications among women were mainly observed in those aged ≥50 years (ie, likely postmenopausal), supporting the hypothesis of the protective role for estrogen against potential limb ischemia in women. 31
Randomized trial data comparing endovascular therapy versus surgical interventions are scarce. 32 The bypass versus angioplasty in severe ischaemia of the leg (BASIL) trial demonstrated that an endovascular approach was comparable to surgery for CLI. 32 However, endovascular techniques have evolved since the BASIL trial. Furthermore, sex‐specific differences in the outcomes of both strategies have not been assessed in the BASIL trial. 32 In the propensity‐matched analysis, we showed that endovascular revascularization was associated with lower in‐hospital mortality in both women and men. These findings should only be considered as hypothesis generating given the potential for selection bias. The ongoing best endovascular versus best surgical therapy for patients with critical limb ischemia (BEST‐CLI) trial is comparing the outcomes of endovascular and surgical revascularization approaches among patients with CLI eligible for both modalities. 33 Hopefully, the BEST‐CLI trial will recruit a representative sample of women to evaluate sex differences in outcomes with both revascularization strategies.
The strengths of this analysis are driven from the large sample size with national representation, in a more contemporary population than previous studies. However, the findings of this analysis should be interpreted in the context of certain limitations. First, this is an observational nonrandomized study. Although we adjusted for potential confounders and conducted several statistical models, the risk of unmeasured confounding could not be excluded. Second, the NIS lacks data on outcomes beyond the index hospitalization. Specifically, for those with CLI that was untreated, there is no information on their long‐term outcomes, and those untreated were more likely to be women. Third, the NIS is an administrative database that relies on ICD‐9‐CM codes, and thus is subject to miscoding and undercoding. Fourth, we did not have access to important clinical data, because imaging, extent of the disease, and medical therapies administrated during the hospitalization were not available. Fifth, data on menopausal state and estrogen replacement therapy were not available in this data set, so a subgroup analysis for age <50 versus ≥50 years was performed, which is the mean age of menopause in the United States for the past 2 decades. 34 Sixth, this analysis was not designed to directly compare the outcomes of different revascularization strategies (ie, endovascular or surgical) between women and men. Finally, the clinical reasoning for choosing one revascularization technique versus the other could not be determined. We attempted to mitigate this by performing a propensity‐matched model.
Conclusions
In this nationwide contemporary analysis of CLI hospitalizations, we demonstrated that women with CLI were older and had a higher prevalence of certain cardiovascular risk factors such as obesity and hypertension compared with men. The rates of hospitalizations for CLI did not change among women but increased in men. Women with CLI were less likely to undergo any revascularization compared with men, but the trends of revascularization have been increasing among both sexes, particularly endovascular revascularization. Women with CLI had a higher incidence of adjusted in‐hospital mortality, bleeding complications, and discharge to facilities compared with men. Endovascular revascularization was associated with lower adjusted in‐hospital mortality among both women and men, compared with surgical revascularization, although the interpretation of this finding is limited by the observational nature of the study.
Sources of Funding
Open Access funding was provided by the Qatar National Library.
Disclosures
Dr Elgendy has disclosures unrelated to this article's content including receiving research grants from Caladrius Biosciences, Inc. The remaining authors have no disclosures to report.
Supporting information
Tables S1–S4
Figures S1–S2
For Sources of Funding and Disclosures, see page 9.
References
- 1. Fowkes FGR, Rudan D, Rudan I, Aboyans V, Denenberg JO, McDermott MM, Norman PE, Sampson UKA, Williams LJ, Mensah GA, et al. Comparison of global estimates of prevalence and risk factors for peripheral artery disease in 2000 and 2010: a systematic review and analysis. Lancet. 2013;382:1329–1340. doi: 10.1016/S0140-6736(13)61249-0 [DOI] [PubMed] [Google Scholar]
- 2. Sigvant B, Wiberg‐Hedman K, Bergqvist D, Rolandsson O, Andersson B, Persson E, Wahlberg E. A population‐based study of peripheral arterial disease prevalence with special focus on critical limb ischemia and sex differences. J Vasc Surg. 2007;45:1185–1191. doi: 10.1016/j.jvs.2007.02.004 [DOI] [PubMed] [Google Scholar]
- 3. Hirsch AT, Allison MA, Gomes AS, Corriere MA, Duval S, Ershow AG, Hiatt WR, Karas RH, Lovell MB, McDermott MM, et al. A call to action: women and peripheral artery disease: a scientific statement from the American Heart Association. Circulation. 2012;125:1449–1472. doi: 10.1161/CIR.0b013e31824c39ba [DOI] [PubMed] [Google Scholar]
- 4. Abtan J, Bhatt DL, Elbez Y, Sorbets E, Eagle K, Reid CM, Baumgartner I, Wu D, Hanson ME, Hannachi H, et al. Geographic variation and risk factors for systemic and limb ischemic events in patients with symptomatic peripheral artery disease: insights from the REACH Registry. Clin Cardiol. 2017;40:710–718. doi: 10.1002/clc.22721 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Mansoor H, Elgendy IY, Williams RS, Joseph VW, Hong YR, Mainous AG. A risk score assessment tool for peripheral arterial disease in women: from the National Health and Nutrition Examination Survey. Clin Cardiol. 2018;41:1084–1090. doi: 10.1002/clc.23032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Brinza EK, Armstrong EJ. Sex‐related differences in outcomes after vascular interventions. Vasc Med. 2018;23:560–569. doi: 10.1177/1358863X18790105 [DOI] [Google Scholar]
- 7. Shishehbor MH, White CJ, Gray BH, Menard MT, Lookstein R, Rosenfield K, Jaff MR. Critical limb ischemia: an expert statement. J Am Coll Cardiol. 2016;68:2002–2015. doi: 10.1016/j.jacc.2016.04.071 [DOI] [PubMed] [Google Scholar]
- 8. Jackson EA, Munir K, Schreiber T, Rubin JR, Cuff R, Gallagher KA, Henke PK, Gurm HS, Grossman PM. Impact of sex on morbidity and mortality rates after lower extremity interventions for peripheral arterial disease: observations from the Blue Cross Blue Shield of Michigan Cardiovascular Consortium. J Am Coll Cardiol. 2014;63:2525–2530. doi: 10.1016/j.jacc.2014.03.036 [DOI] [PubMed] [Google Scholar]
- 9. Hedayati N, Brunson A, Li CS, Baker AC, Pevec WC, White RH, Romano PS. Do women have worse amputation‐free survival than men following endovascular procedures for peripheral arterial disease? An evaluation of the California State‐Wide Database. Vasc Endovascular Surg. 2015;49:166–174. doi: 10.1177/1538574415608269 [DOI] [PubMed] [Google Scholar]
- 10. Haine A, Kavanagh S, Berger JS, Hess CN, Norgren L, Fowkes FGR, Katona BG, Mahaffey KW, Blomster JI, Patel MR, et al. Sex‐specific risks of major cardiovascular and limb events in patients with symptomatic peripheral artery disease. J Am Coll Cardiol. 2020;75:608–617. doi: 10.1016/j.jacc.2019 [DOI] [PubMed] [Google Scholar]
- 11. Choi KH, Park TK, Kim J, Ko Y‐G, Yu CW, Yoon C‐H, Lee J‐H, Min P‐K, Koh YS, Chae I‐H, et al. Sex differences in outcomes following endovascular treatment for symptomatic peripheral artery disease: an analysis from the K‐ VIS ELLA Registry. J Am Heart Assoc. 2019;8:e010849. doi: 10.1161/JAHA.118.010849 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Ramkumar N, Suckow BD, Brown JR, Sedrakyan A, Cronenwett JL, Goodney PP. Sex‐based assessment of patient presentation, lesion characteristics, and treatment modalities in patients undergoing peripheral vascular intervention. Circ Cardiovasc Interv. 2018;11:e005749. doi: 10.1161/CIRCINTERVENTIONS.117.005749 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Lagergren ER, Kempe K, Craven TE, Kornegay ST, Garg N, Velazquez‐Ramirez G, Hurie JB, Edwards MS, Corriere MA. Gender‐specific differences in great saphenous vein conduit. A link to lower extremity bypass outcomes disparities? Ann Vasc Surg. 2017;38:36–41. doi: 10.1016/j.avsg.2016.09.003 [DOI] [PubMed] [Google Scholar]
- 14. Duffy RP, Adams JE, Callas PW, Schanzer A, Goodney PP, Ricci MA, Cronenwett JL, Bertges DJ. The influence of gender on functional outcomes of lower extremity bypass. J Vasc Surg. 2014;60:1282–1290. doi: 10.1016/j.jvs.2014.05.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Gerhard‐Herman MD, Gornik HL, Barrett C, Barshes NR, Corriere MA, Drachman DE, Fleisher LA, Fowkes FGR, Hamburg NM, Kinlay S, et al. 2016 AHA/ACC guideline on the management of patients with lower extremity peripheral artery disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2017;135:e686–e725. doi: 10.1161/CIR.0000000000000470 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. NIS, HCUP Nationwide Inpatient Sample . Healthcare cost and utilization project (HCUP). Available at: https://www.hcup‐us.ahrq.gov/nisoverview.jsp. Accessed March 20, 2020.
- 17. Agarwal S, Sud K, Shishehbor MH. Nationwide trends of hospital admission and outcomes among critical limb ischemia patients: from 2003–2011. J Am Coll Cardiol. 2016;67:1901–1913. doi: 10.1016/j.jacc.2016.02.040 [DOI] [PubMed] [Google Scholar]
- 18. Kolte D, Kennedy KF, Shishehbor MH, Abbott JD, Khera S, Soukas P, Mamdani ST, Hyder ON, Drachman DE, Aronow HD. Thirty‐day readmissions after endovascular or surgical therapy for critical limb ischemia: analysis of the 2013 to 2014 Nationwide Readmissions Databases. Circulation. 2017;136:167–176. doi: 10.1161/CIRCULATIONAHA.117.027625 [DOI] [PubMed] [Google Scholar]
- 19. Khera R, Angraal S, Couch T, Welsh JW, Nallamothu BK, Girotra S, Chan PS, Krumholz HM. Adherence to methodological standards in research using the National Inpatient Sample. JAMA. 2017;318:2011–2018. doi: 10.1001/jama.2017.17653 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Elgendy IY, Ha LD, Elbadawi A, Ogunbayo GO, Olorunfemi O, Mahmoud AN, Mojadidi MK, Abuzaid A, Anderson RD, Bavry AA. Temporal trends in inpatient use of intravascular imaging among patients undergoing percutaneous coronary intervention in the United States. JACC Cardiovasc Interv. 2018;11:913–915. doi: 10.1016/j.jcin.2018.01.254 [DOI] [PubMed] [Google Scholar]
- 21. Mentias A, Qazi A, McCoy K, Wallace R, Vaughan‐Sarrazin M, Girotra S. Trends in hospitalization, management, and clinical outcomes among veterans with critical limb ischemia. Circ Cardiovasc Interv. 2020;13:e008597. doi: 10.1161/CIRCINTERVENTIONS.119.008597 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Lin JH, Brunson A, Romano PS, Mell MW, Humphries MD. Endovascular‐first treatment is associated with improved amputation‐free survival in patients with critical limb ischemia. Circ Cardiovasc Qual Outcomes. 2019;12:e005273. doi: 10.1161/CIRCOUTCOMES.118.005273 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Elgendy IY, Van Spall HGC, Mamas MA. Cardiogenic shock in the setting of acute myocardial infarction: history repeating itself? Circ Cardiovasc Interv. 2020;13:e009034. doi: 10.1161/CIRCINTERVENTIONS.120.009034 [DOI] [PubMed] [Google Scholar]
- 24. Arora S, Stouffer GA, Kucharska‐Newton AM, Qamar A, Vaduganathan M, Pandey A, Porterfield D, Blankstein R, Rosamond WD, Bhatt DL, et al. Twenty year trends and sex differences in young adults hospitalized with acute myocardial infarction. Circulation. 2019;139:1047–1056. doi: 10.1161/CIRCULATIONAHA.118.037137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Cacoub PP, Abola MT, Baumgartner I, Bhatt DL, Creager MA, Liau CS, Goto S, Röther J, Steg PG, Hirsch AT. Cardiovascular risk factor control and outcomes in peripheral artery disease patients in the Reduction of Atherothrombosis for Continued Health (REACH) Registry. Atherosclerosis. 2009;204:e86–e92. doi: 10.1016/j.atherosclerosis.2008.10.023 [DOI] [PubMed] [Google Scholar]
- 26. Kumbhani DJ, Steg PG, Cannon CP, Eagle KA, Smith SC, Goto S, Ohman EM, Elbez Y, Sritara P, Baumgartner I, et al. Statin therapy and long‐term adverse limb outcomes in patients with peripheral artery disease: insights from the REACH registry. Eur Heart J. 2014;35:2864–2872. doi: 10.1093/eurheartj/ehu080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Sigvant B, Lundin F, Wahlberg E. The risk of disease progression in peripheral arterial disease is higher than expected: a meta‐analysis of mortality and disease progression in peripheral arterial disease. Eur J Vasc Endovasc Surg. 2016;51:395–403. doi: 10.1016/j.ejvs.2015.10.022 [DOI] [PubMed] [Google Scholar]
- 28. Hussain MA, Lindsay TF, Mamdani M, Wang X, Verma S, Al‐Omran M. Sex differences in the outcomes of peripheral arterial disease: a population‐based cohort study. CMAJ Open. 2016;4:E124–E131. doi: 10.9778/cmajo.20150107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Dreyer RP, van Zitteren M, Beltrame JF, Fitridge R, Denollet J, Vriens PW, Spertus JA, Smolderen KG. Gender differences in health status and adverse outcomes among patients with peripheral arterial disease. J Am Heart Assoc. 2014;4:e000863. doi: 10.1161/JAHA.114.000863 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. McCoach CE, Armstrong EJ, Singh S, Javed U, Anderson D, Yeo KK, Westin GG, Hedayati N, Amsterdam EA, Laird JR. Gender‐related variation in the clinical presentation and outcomes of critical limb ischemia. Vasc Med. 2013;18:19–26. doi: 10.1177/1358863X13475836 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Raju R, Bland KI, Chaudry IH. Estrogen: a novel therapeutic adjunct for the treatment of trauma‐hemorrhage‐induced immunological alterations. Mol Med. 2008;14:213–221. doi: 10.2119/2008-00001.Raju [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Adam DJ, Beard JD, Cleveland T, Bell J, Bradbury AW, Forbes JF, Fowkes FG, Gillepsie I, Ruckley CV, Raab G, et al. Bypass versus angioplasty in severe ischaemia of the leg (BASIL): multicentre, randomised controlled trial. Lancet. 2005;366:1925–1934. doi: 10.2119/2008-00001 [DOI] [PubMed] [Google Scholar]
- 33. Menard MT, Farber A, Assmann SF, Choudhry NK, Conte MS, Creager MA, Dake MD, Jaff MR, Kaufman JA, Powell RJ, et al. Design and rationale of the best endovascular versus best surgical therapy for patients with critical limb ischemia (BEST‐CLI) trial. J Am Heart Assoc. 2016;5:e003219. doi: 10.1161/JAHA.116.003219 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Appiah D, Nwabuo CC, Ebong IA, Wellons MF, Winters SJ. Trends in age at natural menopause and reproductive life span among US women, 1959–2018. JAMA. 2021;325:1328–1330. doi: 10.1001/jama.2021.0278 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Tables S1–S4
Figures S1–S2


