Abstract
Tumours of the ampulla of Vater are relatively uncommon lesions of the digestive system. They are typically diagnosed at an earlier stage than other types of tumours in this region, due to their tendency to invoke symptoms by obstructing the bile duct or pancreatic duct. Consequently, many are potentially curable by excision. Surgical ampullectomy (SA) (or transduodenal ampullectomy) for an ampullary tumour was first described in 1899, but was soon surpassed by pancreatoduodenectomy (PD), which offered a more extensive resection resulting in a lower risk of recurrence. Ongoing innovation in endoscopic techniques over recent decades has led to the popularization of endoscopic papillectomy (EP), particularly for adenomas and even early cancers. The vast majority of resectable ampullary tumours are now treated using either PD or EP. However, SA continues to play a role in specific circumstances. Many authors have suggested specific indications for SA based on their own data, practices, or interpretations of the literature. However, certain issues have attracted controversy, such as its use for early ampullary cancers. Consequently, there has been a lack of clarity regarding indications for SA, and no evidence-based consensus guidelines have been produced. All studies reporting SA have employed observational designs, and have been heterogeneous in their methodologies. Accordingly, characteristics of patients and their tumours have differed substantially across treatment groups. Therefore, meaningful comparisons of clinical outcomes between SA, PD and EP have been elusive. Nevertheless, it appears that suitably selected cases of ampullary tumours subjected to SA may benefit from favourable peri-operative and long-term outcomes with very low mortality and significantly long survival, hence its role in this setting warrants further clarification, while it can also be useful in the management of specific benign entities. Whilst the commissioning of a randomised controlled trial seems unlikely, well-designed observational studies incorporating adjustments for confounding variables may become the best available comparative evidence for SA, potentially informing the eventual development of consensus guidelines. In this comprehensive review, we explore the role of SA in the modern management of ampullary lesions.
Keywords: Ampulla of Vater, Ampullary tumours, Surgical ampullectomy, Transduodenal ampullectomy, Endoscopic papillectomy, Pancreatoduodenectomy
Core Tip: The role of surgical or transduodenal ampullectomy in the management of ampullary lesions has not been well-defined and the available evidence has been entirely observational. However, it appears that suitably selected cases of ampullary tumours may benefit from favourable peri-operative and long-term outcomes with very low mortality and significantly long survival, hence the role of surgical ampullectomy in this setting warrants further clarification, while it can also be useful in the management of specific benign entities. In this comprehensive review, we explore the role of surgical ampullectomy in the modern management of ampullary lesions.
INTRODUCTION
Ampullary adenocarcinoma (AAC) is the most common cancer of the ampulla of Vater, but represents only 7% of peri-ampullary cancers, and fewer than 1% of all cancers of the digestive system[1,2]. Its prognosis is relatively favourable compared to other cancers near the ampulla: 5-year survival is 41.5%-53% following surgical resection[1,3,4]. AACs are widely believed to develop within adenomas following an adenoma-carcinoma sequence[5]. Histological examinations have detected AACs within 40.9% of surgically resected lesions which were pre-operatively considered to be adenomas[6]. Therefore, ampullary adenomas are typically considered to be pre-cancerous rather than benign lesions, and some authors have suggested that all ampullary lesions should be regarded as potentially malignant[6].
Ampullary tumours may cause symptoms by obstructing the flow of bile or pancreatic juice, even when relatively small, and many asymptomatic tumours are easily detected during endoscopic investigations for unrelated issues[6].Consequently, ampullary tumours are often detected at an earlier stage than other tumours in this region[6,7]. Accordingly, many patients will be potentially curable by surgical excision. Surgical ampullectomy (SA) (or transduodenal ampullectomy) for ampullary cancer was first described by Halsted in 1899[8]. Recurrences were common, therefore SA was largely abandoned in favour of the more extensive pancreatoduodenectomy (PD), first described in 1898 by Codivilla and subsequently refined throughout the first half of the 20th century[9]. A study at the John Hopkins Hospital, Maryland, United States, found that PD was performed for 96.7% of ampullary tumours resected between 1970 and 2007[6]. The major criticism of PD has been its historically high morbidity and mortality, often associated with pancreatic fistulae. However, it has become evident in recent years that specialist high-volume tertiary centres can achieve comparatively better clinical outcomes and a mortality less than 5%[2].
Recent innovation in endoscopic techniques has led to increasing interest in endoscopic papillectomy (EP), which is considerably less invasive than SA and PD. It is worth noting that the endoscopic procedure is often referred to as an ampullectomy. However, only excision of the duodenal mucosa and submucosa at the papilla is involved; it is therefore more accurately referred to as a papillectomy[10]. Accordingly, whilst EP and SA are both local excision techniques, EP is less extensive than SA, which involves excision of the entire ampulla together with small parts of the duodenal wall, bile duct, pancreatic duct, and occasionally pancreatic parenchyma. A recent study of EP for non-invasive ampullary tumours demonstrated eventual endoscopic tumour clearance in 91.1% of patients, including repeat procedures for recurrences, which occurred in 32.7%[11]. Adverse events occurred in 18.9%, most commonly haemorrhage (11.3%); other complications included papillary stenosis, acute pancreatitis, and duodenal perforation. The mortality of EP has been reported as 0.3% or lower[10]. Many authors have advocated EP as the preferred treatment for small non-invasive ampullary tumours, including adenomas containing high-grade dysplasia (HGD) or carcinoma in-situ (Cis), although historically objections against EP were expressed from authors of studies which reported procedure-related deaths[10-16]. EP has also been suggested as a suitable treatment for carefully selected early ampullary cancers, although this has been controversial and some authors have advocated PD for all ampullary cancers in patients who are adequately fit due to the risk of lymphatic involvement[6,10,17,18].
Despite the dominance of EP and PD, SA is still performed in certain circumstances. Determining which patients will benefit from SA requires an understanding of specific factors which may make EP or PD unfeasible or unacceptable. We aim to review the role of SA in the modern management of resectable ampullary tumours.
PRE-OPERATIVE EVALUATION
The purpose of pre-operative evaluation of ampullary tumours is to determine their malignant potential, assess resectability, and establish stage in the case of possible cancers. There has been particular emphasis on the role of endoscopic biopsies and endoscopic ultrasound (EUS)[12]. However, supporting information from other investigations has usually been required, including endoscopy, computed tomography (CT), magnetic resonance imaging (MRI), endoscopic retrograde cholangiopancreatography (ERCP), and intraductal ultrasonography (IDUS)[10].
It has been well demonstrated that pre-operative endoscopic biopsies cannot reliably exclude the presence of small foci of cancer, as small superficial tissue samples are not representative of the whole tumour[19,20]. The reported sensitivity of endoscopic biopsies for detecting cancer, relative to post-operative histology of excised tumours, ranges from 42%-89%, and specificity from 79%-100%[12,18,20-22]. Positive predictive value ranges from 50%-100%, and negative predictive value from 73%-94%[12,20,22]. Diagnostic accuracy has been reported from 45%-100%[12,14,21-28]. The type of endoscope used has been found to affect the diagnostic accuracy of biopsies: those obtained using side-viewing duodenoscopes have outperformed samples taken using forward-viewing endoscopes (85.7% vs 45%, P = 0.004)[29]. Perhaps the most clinically significant performance metric for endoscopic biopsy is the false negative rate, ranging from 10%-60%[7,18,22-24,27,30].
EUS has been described as a critical investigation for ampullary tumours, due to its ability to determine the extent of local invasion and identify lymph node metastases[12]. It has therefore assumed an important role in evaluating likelihood of malignancy, resectability, and pre-operative staging. Its sensitivity for detecting ampullary tumours is 97.6%[31]. EUS findings suggestive of malignancy include intraductal extension, invasion of the sphincter of Oddi, duodenum or portal vein, and lymphadenopathy[12]. In addition, fine needle aspiration of lymph nodes can be performed during EUS to obtain samples for cytological examination, further enhancing its utility in detecting cancer and staging. Its accuracy in determining N-stage has been reported as 66.7%[31]. EUS has been found to have an accuracy of 78%-87.8% in assessing the extent of local invasion, and has a tendency towards overestimation rather than underestimation[22,31,32]. Differentiation of T3 and T4 cancers from non-invasive tumours and early cancers has been described as easy, however some authors have found EUS unhelpful, particularly for discriminating non-invasive tumours from T1 cancers[19,22,33]. Its sensitivity for intraductal extension relative to post-operative histology is 80%, and specificity 93%[34]. Accuracy in determining resectability of ampullary and pancreatic cancers has been reported as 72%[35]. Rejeski et al[36] reported a set of EUS findings which detected ampullary tumours requiring surgery rather than EP with a sensitivity of 97.1%, although this was not prospectively validated on an independent data sample.
CT has been found to have a relatively low sensitivity for detecting ampullary tumours, sometimes as low as 20%[30,31]. It has a similarly poor performance in evaluating local invasion, with a T-stage accuracy of 26.1%[31]. However, its N-stage accuracy has been measured at 43.5% with no statistically significant difference from EUS or MRI, and it can detect distant metastases[12,31]. MRI has been demonstrated to be comparable to EUS: Its sensitivity for detecting ampullary tumours was 81.3%, T-staging accuracy 53.8%, and N-staging accuracy 76.9%, with no statistically significant differences from EUS[31].
Endoscopy using either a forward-viewing endoscope or side-viewing duodenoscope allows visualization of the ampullary lesion, to evaluate malignant potential and endoscopic resectability[37]. In general, tumours which are firm, immobile, friable, ulcerated, or have an indistinct margin are likely to be malignant[10,12]. A small study in 2015 found a sensitivity of 94.7% and a specificity of 89.5% for AAC diagnosed using the following endoscopic criteria: “enlarged papilla with uneven granular or nodular appearance of overlying mucosa, associated with spontaneous bleeding, ulceration, and friable or indurated surface”[29]. However, there has not been a robust evaluation of specific criteria for distinguishing ampullary adenomas from early AAC based on endoscopic appearances[10]. There has been controversy regarding whether tumour size correlates with the likelihood of cancer: whilst some authors have supported this assertion, several studies, including a recent meta-analysis, have found no correlation[6,12,37,38]. ERCP is useful for evaluating intraductal extension: it has been found to have a sensitivity of 83% and a specificity of 93% for detecting intraductal extension relative to post-operative histology, which was comparable to EUS[34].
INDICATIONS
Studies of SA have all been observational and heterogenous in their methodologies and findings, resulting in a deficient evidence base[38]. Furthermore, SA has been an uncommon treatment for a rare tumour, and has therefore attracted relatively little attention. Consequently, no evidence-based consensus guidelines have been produced regarding suitable indications for SA. Recognizing this, many authors have described specific indications or decision-making algorithms based on their own data, practices, or interpretations of the literature[6,10,12-14,17,19-24,27,28,32,39-50]. A summary of generally accepted indications, contra-indications, and controversies is presented in Table 1.
Table 1.
Indications for surgical ampullectomy
|
Lesion type
|
Generally accepted indications
|
Uncertainties
|
Generally accepted contra-indications
|
Ref.
|
| Adenoma | Lesion too large for EP, including those with HGD or Cis | Tumour size thresholds | [6,10,12,13,20-24,26,37-40,42,44,46,49,51,52] | |
| Failed EP, including recurrence or positive margins | [42,52] | |||
| FAP patients | [53-55] | |||
| AAC | T1 or T2, unfit for PD | T1 or T2, fit for PD | T3 or T4, fit for PD | [6,21-24,30,39,41,43-46,49,51,58] |
| Well-differentiated | Moderately-differentiated | Poorly-differentiated | [21,23,30,39,43,49,56,57,60] | |
| Nodal or distant metastases | [21,23,24,30,39,41,49] | |||
| Requirement for lymphadenectomy | [39,57] | |||
| Intraductal extension | [10,12,19,21,26,56] | |||
| Others | Sphincterotomy-associated biliary stricture | [70] | ||
| Neuroendocrine tumours | [66,67] |
AAC: Ampullary adenocarcinoma; FAP: Familial adenomatous polyposis; EP: Endoscopic papillectomy; HGD: High-grade dysplasia; PD: Pancreatoduodenectomy.
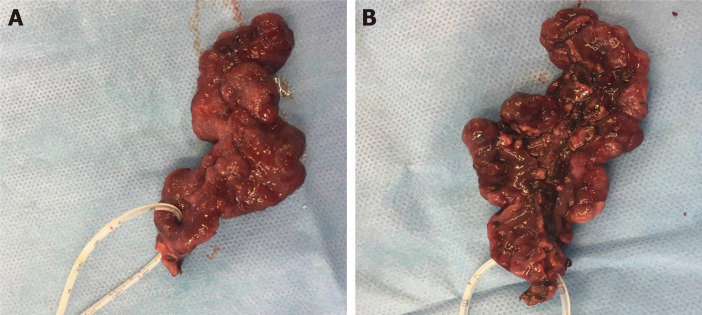
The least controversial indication has been ampullary adenoma. Historically, PD was considered preferable due to diagnostic uncertainty, however the trend over time has been towards less invasive options. For smaller adenomas, EP has become the preferred option, with SA reserved for cases which are too large for endoscopic resection[46]. Suggested minimum sizes to consider SA range from 2 to 3 cm, or what the endoscopist considers too large for EP[10,13,26,39,49]. A few authors have proposed maximum sizes for SA of 2.5-4 cm, on the justification that larger adenomas may be more likely to contain cancer[20,22,51]. However, most authors have not reported an upper size threshold; this position is supported by the significant amount of data finding no such correlation between size and malignant potential[6,12,37,38]. Accordingly, SA has been successfully performed for carefully selected large adenomas (Figure 1). Many authors have suggested SA is suitable for adenomas containing HGD, whilst EP is adequate for low-grade dysplasia[13,42,49,51,52]. Similarly, adenoma with Cis has been widely reported as an indication for SA[12,21,23,24,40,44]. SA has also been recommended for adenomas which recur after EP, and when EP has failed to achieve clear margins[42,52].
Figure 1.
A 7-cm polypoid tubulovillous adenoma extending from the ampulla of Vater down to D3, removed by means of open surgical ampullectomy-excision of adenoma en block, following cholecystectomy and catheterization of the ampulla for identification. Preoperative biopsies showed low-grade dysplasia (LGD) and this 74-year old patient with severe comorbidities was initially counselled for pancreatoduodenectomy. Meticulous preoperative endoscopic evaluation revealed its polypoid configuration, possibly emanating from a mucosal stalk, which was confirmed intraoperatively. A: The ampulla is encircled by a fine catheter. Final histology confirmed the presence of a tubulovillous adenoma with extensive LGD and focal high-grade dysplasia. All margins were clear of tumour or dysplasia. (V. Mavroeidis’ archive). B: Inferior aspect of the specimen, depicting the duodenal margin along the tumour, and the insertion point of the catheter into the ampulla. (V. Mavroeidis’ archive).
Ampullary tumours may occur in patients with familial adenomatous polyposis (FAP), an inherited syndrome characterized by hundreds or thousands of polyps in the colon and rectum, and commonly also in the duodenum[53]. The risk of ampullary cancer in FAP patients has been reported to be 124-fold that of the general population[54]. A classification of duodenal polyposis was developed by Spigelman et al[55], based on the number, size and histology of polyps, as shown in Table 2. A consensus guideline produced by the Mallorca Group in 2008 considered PD or pancreas-sparing duodenectomy necessary for older patients with Spigelman stage IV polyposis, due to the high risk of developing duodenal cancer[53]. It was suggested that local surgery may be appropriate for patients under 40 years with stage III or IV disease. The most important advantage of local surgery was considered to be the postponement of more extensive resections in younger FAP patients. The role of SA, relative to EP and PD, in FAP patients has not been well-defined.
Table 2.
Spigelman’s classification of duodenal polyposis
|
Characteristics
|
|
Points
|
| Number of polyps | 1 to 4 | 1 |
| 5 to 20 | 2 | |
| > 20 | 3 | |
| Size of polyps | 1 to 4 mm | 1 |
| 5 to 10 mm | 2 | |
| > 10 mm | 3 | |
| Histological type | Tubular polyp, hyperplasia, inflammation | 1 |
| Tubulovillous | 2 | |
| Villous | 3 | |
| Dysplasia | Mild | 1 |
| Moderate | 2 | |
| Severe | 3 |
A total of 0 points = stage 0; 1 to 4 points = stage I; 5 to 6 points = stage II; 7 to 8 points = stage III; and 9 to 12 points = stage IV[55].
Intraductal extension of tumours has been found to be suggestive of malignancy, and therefore has been regarded as a contra-indication by those who oppose SA for early cancers in fit patients[12,26]. However, up to 1 cm of intraductal extension has been considered permissible when undertaking EP for tumours measuring less than 2 cm which are not thought to be malignant[10]. Among proponents of SA for early cancers in fit patients, there has been some disagreement regarding the extent to which intraductal extension is permissible before conversion to PD. Lai et al[21] reported that SA was indicated for up to 1 cm of extension into the bile duct or pancreatic duct. However, Aiura et al[19,56] precluded from consideration any cases with tumour extension into the pancreatic duct, while considering any degree of ingress into the bile duct, as this could be addressed by resection of the extrahepatic bile duct.
The role of SA as a treatment for AAC has been extensively debated. Particular attention has been paid to predictors of lymph node metastasis, as this may be the major factor responsible for recurrence following SA, and is also associated with poor prognosis[2,4,32,56]. It has been widely recognized that PD is the most effective treatment for ampullary cancer[6]. Proponents of SA have argued that it may be adequately effective for certain early cancers, whilst avoiding unnecessary morbidity associated with PD[41]. Although there has been unanimous agreement that the absence of lymph node and distant metastases (N0 M0) is an absolute prerequisite for SA, there has been variability in criteria for size, T-stage, intraductal extension, and grade[21,23,24,30,39,41,49]. Several authors have recommended a maximum tumour size of 2 or 3 cm, as size has been found to correlate to risk of lymph node metastases; however, the majority has not specified a maximum size limit[6,21,24,30,41,45,49]. The use of SA as an alternative to PD for T1 Lesions has been widely supported[21-24,30,39,41,43,45,46,49]. Lymphadenectomy has been considered essential by some authors when SA was performed for T1 lesions[39,57]. Some authors have objected to SA for T1 cancers in patients who are adequately fit for PD, as the risk of lymph node metastasis from T1 tumours is 22%-30%[6,39,44,51,58]. The majority of studies have not supported the use of SA for T2 cancers in fit patients, although some have suggested it is appropriate provided the tumour measures less than 2 or 3 cm[41,45]. SA has not been advised for T3 or T4 cancers in fit patients. The interpretation of recommendations regarding T-stage is further complicated by differences in definitions proposed by various editions of the Union for International Cancer Control TNM classification, and some authors have not specified which edition their recommendations have been based on. Further changes to T-stage definitions for ampullary cancer have been proposed, as the correlation of the 8th edition definitions with prognosis has been questioned by some authors[59].
The histological grade has been found to predict the risk of lymph node metastases. A study by Amini et al[57] found lymph node metastases in 10% of well-differentiated, 12% of moderately-differentiated, and 27% of poorly-differentiated ampullary cancers (P = 0.007). Well-differentiated lesions have therefore been considered the most suitable cancerous candidates for SA[21,23,30,39,43,49,56]. Some authors have also supported its use for moderately-differentiated tumours[21,39,43,49]. However, Aiura et al[56] regarded SA as inappropriate for moderately- and poorly-differentiated lesions as their study reported lymph node metastases in 62.1% of cancers of these grades. Beger et al[39] also considered SA unsuitable for poorly-differentiated cancers. Furthermore, over recent years, the clinical relevance of the histological heterogeneity of AAC has become better understood, with accumulating evidence regarding differences in responses to treatment between the intestinal, pancreatobiliary and mixed types[60].
There has been general agreement that SA may be particularly appealing for early ampullary cancers in patients who are unfit for PD and in whom EP is not feasible, although there has been some controversy regarding the appropriateness of SA in elderly, frail patients[3,7,13,17,28,32,50,52,61-63]. Some studies have suggested SA may have value as a palliative treatment; however, it has not been made apparent how SA would be advantageous compared to common palliative options such as stenting and bypass procedures[12,50,62,64,65].
Although SA has most commonly been used for adenomas and AACs, treatment of other lesions has been described. Milanetto et al[66] considered SA appropriate for well-differentiated ampullary neuroendocrine tumours (NETs) less than 2 cm in size, and for larger well-differentiated NETs in patients unfit for PD; however, some authors have expressed concern regarding its potential to underestimate the stage and under-treat NETs[67]. SA for a patient with an intraductal papillary neoplasm of the bile duct, considered unsuitable for EP due to intraductal extension of more than 10 mm, has also been reported[68]. SA has also been employed for the treatment of inflammatory and fibrotic stenoses of the ampulla[69]. Endoscopic biliary sphincterotomy has been proposed as an effective first-line treatment for post-sphincterotomy stenosis, as the lesion is limited to the intra-duodenal portion of the orifice and the sphincterotomy can be extended[70]. In cases of sphincterotomy-associated biliary stricture, in which the stenosis extends along the bile duct, either endoscopic balloon dilatation or SA has been considered necessary[70].
SURGICAL TECHNIQUE
The technique of SA has been extensively described, including reports of minimal access approaches[20,30,39,46,62,68,71-73]. Pre-operative endoscopic stenting of the bile duct may be employed to relieve jaundice, and is helpful in locating the bile duct during surgery. The abdomen is accessed, either by laparotomy using a right subcostal or upper midline incision, or by minimal access methods. The abdomen is then explored for evidence of metastases. If the bile duct was not stented pre-operatively and a cholecystectomy is to be performed, a stent may be inserted via the cystic duct through the ampulla to assist in its identification (Figure 1). The hepatic flexure of the colon is mobilized, followed by the second part of the duodenum using the Kocher manoeuvre. The position of the ampulla is determined by palpation of the tumour or stent. A 4-5 cm longitudinal duodenotomy is then performed opposite the ampulla. Stay sutures are placed in the duodenal wall using 2-0 silk to maintain adequate exposure. The bile duct and pancreatic duct can be cannulated via the ampulla to assist with their identification, if a stent was not already in place. Once the ampullary tumour has been identified, some authors have recommended placing a 2-0 silk suture through it to facilitate retraction. Submucosal injection of adrenaline solution has been reported, to elevate the lesion and reduce bleeding[73].
Several variations of excision and reconstruction have been described. The duodenal tissue may be dissected circumferentially, leaving the bile duct and pancreatic duct initially intact; the ducts are marked with sutures before transecting them. The ducts are then approximated to the duodenal wall using interrupted 4-0 or 5-0 absorbable sutures, and to each other at their closest margins to form a common wall. Alternatively, Mathiel et al[71] recommended a “suturing as you go” method, to prevent duct retraction. Dissection begins at the 11 o’clock position, proceeding towards the bile duct. When the bile duct is entered, a 4-0 or 5-0 absorbable suture is placed to approximate the bile duct to the wall of the duodenum. As the bile duct is gradually opened, further sutures are placed. Dissection proceeds clockwise, until the pancreatic duct is encountered at the 2 o’clock position. The pancreatic duct is progressively sutured in a similar manner. After the mass is completely excised, the common wall of the bile and pancreatic ducts is formed using 5-0 absorbable sutures. There has not been a comparative evaluation of excision and reconstruction techniques.
Histological examination of the excised lesion by intra-operative frozen section to confirm clear margins has been strongly advocated for, particularly when cancer is suspected[7,62,63]. SA with frozen section has been conceptualized as a “macro biopsy”, having both diagnostic and therapeutic functions[50,58]. Schoenberg et al[18] described performing frozen section allowing a 1 cm margin of macroscopically normal tissue around the lesion. The operation can be converted to PD if clear margins cannot be obtained, or if the histological characteristics are worse than anticipated. Frozen section has generally been found to be accurate relative to post-operative histology of the resected specimen: reported accuracy ranges from 75%-100%[14,20,21,23,25-27,30,43,63]. The lowest reported diagnostic sensitivity has been 57%, in a cohort of 7 patients[63]. Other measurements of sensitivity range from 85.6% to 97%[18,21,24]. The combination of pre-operative endoscopic biopsies and intra-operative frozen section has been found to improve diagnostic accuracy to 100%[30,62].
Having confirmed complete excision has been achieved, the patency of the bile and pancreatic ducts is then assessed. Visualization of the expulsion of bile and pancreatic juice has been suggested to adequately confirm duct patency[71]. However, probing of the ducts using biliary dilators has also been reported, to ensure the diameter of the ducts is sufficient to tolerate an expected contraction of 50% due to scarring; 6-8 mm for the bile duct, and 4-5 mm for the pancreatic duct has been considered adequate[30,62]. Some surgeons have advocated temporary stenting to maintain patency during healing, for example by inserting a 14-gauge silicone catheter into each duct and securing it in place with an absorbable suture[46,73]. The duodenum can then be closed transversely to avoid stricturing, using an absorbable suture in either a single or double layer, or a stapling device. In minimal access cases, a single-layer 3-0 continuous barbed absorbable suture may be preferable[73]. A drain may be placed near the duodenotomy at the discretion of the surgeon.
Some authors have incorporated additional components within SA procedures. Excision of supraduodenal lymph nodes and nodes anterior and posterior to the pancreatic head has been described during SA for T1 AACs, on the justification that such lesions are often associated with local lymph node metastases[39,49,57]. SA combined with excision of the extrahepatic bile duct has also been reported, to deal with intraductal extension along the bile duct, provided none occurred along the pancreatic duct[19,56].
CLINICAL OUTCOMES
No randomized controlled trial (RCT) has been conducted to compare SA to EP or PD for any indication[38]. The evidence has been entirely observational; most studies have been retrospective single-centre case series or cohort studies. Comparing clinical outcomes of SA to those of EP or PD is therefore problematic, because characteristics of patients assigned to each treatment have differed substantially[58]. Similarly, there has been a lack of comparative evaluations of minimal access vs open surgical techniques for SA. A summary of clinical outcomes of SA is presented in Table 3.
Table 3.
Clinical outcomes of surgical ampullectomy
|
Indication
|
Outcome
|
|
Estimate
|
Ref.
|
| Adenoma or AAC | Complete excision (R0) | 96.4% | [38] | |
| Adenoma or AAC | Recurrence | 9.4% | [38] | |
| Adenoma or AAC | Complications | 28.3% | [38] | |
| Adenoma or AAC | Mortality1 | 0.9% | [6,12,14,20,22,24,25,28,30,32,39,41,43,45,47-52,58,62,64,67,72,74,76-79] | |
| AAC | Survival at 5 yr | T1 | 40% | [50] |
| T1 + T2 | 64.3% | [41] | ||
| T2 | 16% | [50] | ||
| T3 | 0% | [50] | ||
| T3 + T4 | 18.2% | [41] |
Pooled mortality of cited studies (5 deaths in 532 surgical ampullectomies across 30 studies).
AAC: Ampullary adenocarcinoma.
A recent systematic review and meta-analysis by Heise et al[38] reported a pooled complete excision (R0) rate for SA of 96.4%, from 10 studies including adenomas and AACs. However, some small studies which were not included have reported less favourable results. Lindell et al[74] reported an R0 rate of 50% in a series of 10 SAs for AACs in patients unfit for PD. Similarly, Kobayashi et al[17] achieved R0 in only 50% of 6 SAs performed for adenomas and T1 cancers in unfit patients. In a series of 17 cases described by Zhong et al[50], R0 was achieved in 52.9%; this series included patients with T2 and T3 cancers, and 76% were of moderate or poor histological grade.
Local recurrence has been considered the major weakness of SA compared to PD[12]. The main recurrence pattern after R0 excision appears to be lymph node metastasis[75]. The meta-analysis by Heise et al[38] calculated a pooled recurrence rate of 9.4% over 12 studies of SA. Recurrence rates reported by individual studies within the meta-analysis ranged from 0-31.8%[24,26,49]. However, some studies not included within the analysis have observed significantly higher rates, up to 80% for AACs[41,62,74]. Recurrence rates as high as 100% have been reported in patients with FAP[16]. The wide range of recurrence rates may be explained by methodological heterogeneity between studies: there have been considerable differences in indications, patient characteristics, and follow-up duration[7]. Lifelong surveillance endoscopy has been considered necessary owing to the risk of tumour recurrence following SA[23,25,47,62].
There has been considerable interest in complications following SA, as comparatively low surgical morbidity has been the primary justification for its use in preference to PD. The pooled complication rate in the meta-analysis by Heise et al[38] was 28.3% among 13 studies; individual studies reported rates ranging from 7.7%-68%. Acute pancreatitis has been described in 10%-50% of patients following SA[12,76]. Post-operative haemorrhage has occurred in 3.8%-25% of cases, sometimes necessitating emergency re-operation[3,52]. Reported wound infection rates range from 5%-20.7%[25,30]. Other less frequent complications have included biliary or pancreatic fistulae, duodenotomy leakage, cholangitis, delayed gastric emptying, biliary strictures, adhesional intestinal obstruction, and other general post-operative complications[12,13,25,30,51,52,58,62,63,76]. Surgical mortality risk associated with SA has proven to be very favourable: across 30 studies reporting mortality statistics, only 5 deaths have occurred in 532 patients (0.9%)[6,12,14,20,22,24,25,28,30,32,39,41,43,45,47-52,58,62,64,67,72,74,76-79].
Long-term survival in patients undergoing SA for cancers has been inconsistently reported, as follow-up durations have varied within studies and among different studies. Reported overall 5-year survival rates range from 10%-77.3%[24,30,41,43,50,74]. A more useful insight may be gained by considering studies which have reported subset analyses by cancer stage. Feng et al[41], in a cohort of 25 patients, reported 5-year survival rates of 64.3% for T1/T2, and 18.2% for T3/T4 cancers. Zhong et al[50] observed 40% survival at 5 years for T1 disease, 16% for T2, and 0% for T3, in a study of 17 patients. The interpretation of long-term survival metrics is further complicated by the tendency for SA to be used in co-morbid patients.
FUTURE RESEARCH
The likelihood of an RCT being conducted to evaluate SA seems low, as it has been an uncommon treatment for a rare tumour and therefore attracts relatively little attention from researchers and funders. Furthermore, the available evidence strongly suggests that randomization would be unethical. However, the ESAP study is a planned international multicentre retrospective cohort study which aims to compare EP, SA and PD for ampullary neoplasms[80]. Its methodology includes propensity score matching to account for differences in baseline characteristics of the cohorts. The ESAP study may have the potential to become the best available evidence for SA in lieu of an RCT. Its findings could stimulate the development of consensus guidelines to clarify the role of SA in the management of ampullary tumours.
CONCLUSION
SA may be the best available treatment option for a specific subset of patients with ampullary tumours. It can be conceptualized as an intermediate type of excision in terms of extensiveness and morbidity, between EP and PD. Therefore, it may be appropriate in situations where EP is inadequate or impossible, or where PD is unnecessary or prohibitively risky. Whilst many authors have proposed specific indications for SA, there has been significant controversy, particularly regarding the management of early ampullary cancers. The least controversial indication appears to be ampullary adenoma, with SA being reserved for cases which are too large for endoscopic excision. Its role in the treatment of AAC has been debated. The absence of lymph node and distant metastases is an absolute prerequisite for consideration of the procedure. Its use as an alternative to PD has been supported for T1 tumours and less frequently for selected T2 tumours, whilst it has largely been discouraged for T3 and T4 tumours. Equally, it may be unsuitable for poorly-differentiated AACs. There seems to have been general agreement that SA may be particularly appealing for early ampullary cancers in patients who are unfit for PD, and in whom EP is not feasible. Importantly, high rates of long-term survival have been achieved, particularly in suitable cases of T1 tumours, whereas prognosis has been unfavourable following excision of T3 and T4 tumours. Additionally, SA may have a role in carefully selected cases of NETs, as well as in cases of inflammatory and fibrotic strictures of the ampulla. When undertaken for ampullary tumours, frozen sections of the margins have been strongly advised, particularly when cancer is suspected. Importantly, while SA may be associated with considerable morbidity, the reported mortality is less than 1%.
The available evidence has been entirely observational, and an RCT seems impractical. However, further cohort studies incorporating adjustments for confounding variables may provide more meaningful data, facilitating the definition of specific criteria and potentially informing the development of consensus guidelines. Subsequently, the use of SA in the management of ampullary lesions may increase in a more standardized fashion.
Footnotes
Conflict-of-interest statement: The authors declare no conflict of interests for this article.
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Invited article; Externally peer reviewed.
Corresponding Author's Membership in Professional Societies: General Medical Council (UK), No. 7451513; Royal College of Surgeons of England, No. 9092145; International College of Surgeons, No. M21313; Faculty of Surgical Trainers of Edinburgh, Royal College of Surgeons of Edinburgh, No. 188646; and American College of Surgeons, No. 03340060.
Peer-review started: April 18, 2021
First decision: May 13, 2021
Article in press: October 14, 2021
Specialty type: Surgery
Country/Territory of origin: United Kingdom
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Barreto SGADP, Khuri S S-Editor: Gong ZM L-Editor: A P-Editor: Gong ZM
Contributor Information
Darren L Scroggie, Department of Population Health Sciences, Bristol Centre for Surgical Research, Bristol Medical School, Bristol BS8 2PS, United Kingdom.
Vasileios K Mavroeidis, Department of HPB Surgery, University Hospitals Bristol and Weston NHS Foundation Trust, Bristol Royal Infirmary, Bristol BS2 8HW, United Kingdom. blackbasildr@yahoo.gr; Department of Surgery, The Royal Marsden NHS Foundation Trust, London SW3 6JJ, United Kingdom.
References
- 1.Rostain F, Hamza S, Drouillard A, Faivre J, Bouvier AM, Lepage C. Trends in incidence and management of cancer of the ampulla of Vater. World J Gastroenterol. 2014;20:10144–10150. doi: 10.3748/wjg.v20.i29.10144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Moekotte AL, Lof S, Van Roessel S, Fontana M, Dreyer S, Shablak A, Casciani F, Mavroeidis VK, Robinson S, Khalil K, Gradinariu G, Mowbray N, Al-Sarireh B, Fusai GK, Roberts K, White S, Soonawalla Z, Jamieson NB, Salvia R, Besselink MG, Abu Hilal M. Histopathologic Predictors of Survival and Recurrence in Resected Ampullary Adenocarcinoma: International Multicenter Cohort Study. Ann Surg. 2020;272:1086–1093. doi: 10.1097/SLA.0000000000003177. [DOI] [PubMed] [Google Scholar]
- 3.Chareton B, Coiffic J, Landen S, Bardaxoglou E, Campion JP, Launois B. Diagnosis and therapy for ampullary tumors: 63 cases. World J Surg. 1996;20:707–712. doi: 10.1007/s002689900108. [DOI] [PubMed] [Google Scholar]
- 4.Moekotte AL, van Roessel S, Malleo G, Rajak R, Ecker BL, Fontana M, Han HS, Rabie M, Roberts KJ, Khalil K, White SA, Robinson S, Halimi A, Zarantonello L, Fusai GK, Gradinariu G, Alseidi A, Bonds M, Dreyer S, Jamieson NB, Mowbray N, Al-Sarireh B, Mavroeidis VK, Soonawalla Z, Napoli N, Boggi U, Kent TS, Fisher WE, Tang CN, Bolm L, House MG, Dillhoff ME, Behrman SW, Nakamura M, Ball CG, Berger AC, Christein JD, Zureikat AH, Salem RR, Vollmer CM, Salvia R, Besselink MG, Abu Hilal M International Study Group on Ampullary Cancer (ISGACA) Collaborators, Aljarrah R, Barrows C, Cagigas MN, Lai ECH, Wellner U, Aversa J, Dickson PV, Ohtsuka T, Dixon E, Zheng R, Kowalski S, Freedman-Weiss M. Development and external validation of a prediction model for survival in patients with resected ampullary adenocarcinoma. Eur J Surg Oncol. 2020;46:1717–1726. doi: 10.1016/j.ejso.2020.04.011. [DOI] [PubMed] [Google Scholar]
- 5.Stolte M, Pscherer C. Adenoma-carcinoma sequence in the papilla of Vater. Scand J Gastroenterol. 1996;31:376–382. doi: 10.3109/00365529609006414. [DOI] [PubMed] [Google Scholar]
- 6.Winter JM, Cameron JL, Olino K, Herman JM, de Jong MC, Hruban RH, Wolfgang CL, Eckhauser F, Edil BH, Choti MA, Schulick RD, Pawlik TM. Clinicopathologic analysis of ampullary neoplasms in 450 patients: implications for surgical strategy and long-term prognosis. J Gastrointest Surg. 2010;14:379–387. doi: 10.1007/s11605-009-1080-7. [DOI] [PubMed] [Google Scholar]
- 7.de Castro SM, van Heek NT, Kuhlmann KF, Busch OR, Offerhaus GJ, van Gulik TM, Obertop H, Gouma DJ. Surgical management of neoplasms of the ampulla of Vater: local resection or pancreatoduodenectomy and prognostic factors for survival. Surgery. 2004;136:994–1002. doi: 10.1016/j.surg.2004.03.010. [DOI] [PubMed] [Google Scholar]
- 8.Halsted WS. Contributions to the Surgery of the Bile Passages, Especially of the Common Bile-Duct. Boston Med Surg J . 1899;141:645–654. [Google Scholar]
- 9.Are C, Dhir M, Ravipati L. History of pancreaticoduodenectomy: early misconceptions, initial milestones and the pioneers. HPB (Oxford) 2011;13:377–384. doi: 10.1111/j.1477-2574.2011.00305.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kandler J, Neuhaus H. How to Approach a Patient With Ampullary Lesion. Gastroenterology. 2018;155:1670–1676. doi: 10.1053/j.gastro.2018.11.010. [DOI] [PubMed] [Google Scholar]
- 11.Lee R, Huelsen A, Gupta S, Hourigan LF. Endoscopic ampullectomy for non-invasive ampullary lesions: a single-center 10-year retrospective cohort study. Surg Endosc. 2021;35:684–692. doi: 10.1007/s00464-020-07433-7. [DOI] [PubMed] [Google Scholar]
- 12.Ceppa EP, Burbridge RA, Rialon KL, Omotosho PA, Emick D, Jowell PS, Branch MS, Pappas TN. Endoscopic versus surgical ampullectomy: an algorithm to treat disease of the ampulla of Vater. Ann Surg. 2013;257:315–322. doi: 10.1097/SLA.0b013e318269d010. [DOI] [PubMed] [Google Scholar]
- 13.Mansukhani VM, Desai GS, Mouli S, Shirodkar K, Shah RC, Palepu J. Transduodenal ampullectomy for ampullary tumors. Indian J Gastroenterol. 2017;36:62–65. doi: 10.1007/s12664-016-0726-0. [DOI] [PubMed] [Google Scholar]
- 14.Mathur A, Paul H, Ross S, Luberice K, Hernandez J, Vice M, Rosemurgy AS. Transduodenal ampullectomy for ampullary adenomas: a safe and effective procedure with long-term salutary outcomes. Am Surg. 2014;80:185–190. [PubMed] [Google Scholar]
- 15.Ödemiş B, Durak MB, Cengiz M. Endoscopic Ampullectomy of Benign Ampullary Lesions: Outcomes From a Single Center Study. Surg Laparosc Endosc Percutan Tech. 2020;30:270–275. doi: 10.1097/SLE.0000000000000775. [DOI] [PubMed] [Google Scholar]
- 16.Soravia C, Berk T, Haber G, Cohen Z, Gallinger S. Management of advanced duodenal polyposis in familial adenomatous polyposis. J Gastrointest Surg. 1997;1:474–478. doi: 10.1016/s1091-255x(97)80136-9. [DOI] [PubMed] [Google Scholar]
- 17.Kobayashi A, Konishi M, Nakagohri T, Takahashi S, Kinoshita T. Therapeutic approach to tumors of the ampulla of Vater. Am J Surg. 2006;192:161–164. doi: 10.1016/j.amjsurg.2006.05.002. [DOI] [PubMed] [Google Scholar]
- 18.Schoenberg MH, Treitschke F, Harada N, Beger HG. Benign tumour of the ampulla of Vater: surgical treatment and prognosis. Eur J Surg. 1998;164:765–770. doi: 10.1080/110241598750005408. [DOI] [PubMed] [Google Scholar]
- 19.Aiura K, Shinoda M, Nishiyama R. Surgical technique for complete resection of the extrahepatic portion of the common bile duct and the ampulla of Vater for tumors of the ampulla of Vater. J Hepatobiliary Pancreat Sci. 2011;18:276–281. doi: 10.1007/s00534-010-0308-y. [DOI] [PubMed] [Google Scholar]
- 20.Clary BM, Tyler DS, Dematos P, Gottfried M, Pappas TN. Local ampullary resection with careful intraoperative frozen section evaluation for presumed benign ampullary neoplasms. Surgery. 2000;127:628–633. doi: 10.1067/msy.2000.106532. [DOI] [PubMed] [Google Scholar]
- 21.Lai JH, Shyr YM, Wang SE. Ampullectomy versus pancreaticoduodenectomy for ampullary tumors. J Chin Med Assoc. 2015;78:339–344. doi: 10.1016/j.jcma.2015.02.002. [DOI] [PubMed] [Google Scholar]
- 22.Rattner DW, Fernandez-del Castillo C, Brugge WR, Warshaw AL. Defining the criteria for local resection of ampullary neoplasms. Arch Surg. 1996;131:366–371. doi: 10.1001/archsurg.1996.01430160024003. [DOI] [PubMed] [Google Scholar]
- 23.Liu F, Cheng JL, Cui J, Xu ZZ, Fu Z, Liu J, Tian H. Surgical method choice and coincidence rate of pathological diagnoses in transduodenal ampullectomy: A retrospective case series study and review of the literature. World J Clin Cases. 2019;7:717–726. doi: 10.12998/wjcc.v7.i6.717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gao Y, Zhu Y, Huang X, Wang H, Yuan Z. Transduodenal ampullectomy provides a less invasive technique to cure early ampullary cancer. BMC Surg. 2016;16:36. doi: 10.1186/s12893-016-0156-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Grobmyer SR, Stasik CN, Draganov P, Hemming AW, Dixon LR, Vogel SB, Hochwald SN. Contemporary results with ampullectomy for 29 "benign" neoplasms of the ampulla. J Am Coll Surg. 2008;206:466–471. doi: 10.1016/j.jamcollsurg.2007.09.005. [DOI] [PubMed] [Google Scholar]
- 26.Kim AL, Choi YI. Safety of duodenal ampullectomy for benign periampullary tumors. Ann Hepatobiliary Pancreat Surg. 2017;21:146–150. doi: 10.14701/ahbps.2017.21.3.146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Roggin KK, Yeh JJ, Ferrone CR, Riedel E, Gerdes H, Klimstra DS, Jaques DP, Brennan MF. Limitations of ampullectomy in the treatment of nonfamilial ampullary neoplasms. Ann Surg Oncol. 2005;12:971–980. doi: 10.1245/ASO.2005.03.009. [DOI] [PubMed] [Google Scholar]
- 28.Toh SK, Davies N, Dolan P, Worthley C, Townsend N, Williams JA. Good outcome from surgery for ampullary tumour. Aust N Z J Surg. 1999;69:195–198. doi: 10.1046/j.1440-1622.1999.01521.x. [DOI] [PubMed] [Google Scholar]
- 29.Lee HS, Jang JS, Lee S, Yeon MH, Kim KB, Park JG, Lee JY, Kim MJ, Han JH, Sung R, Park SM. Diagnostic Accuracy of the Initial Endoscopy for Ampullary Tumors. Clin Endosc. 2015;48:239–246. doi: 10.5946/ce.2015.48.3.239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Demetriades H, Zacharakis E, Kirou I, Pramateftakis MG, Sapidis N, Kanellos I, Betsis D. Local excision as a treatment for tumors of ampulla of Vater. World J Surg Oncol. 2006;4:14. doi: 10.1186/1477-7819-4-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chen CH, Yang CC, Yeh YH, Chou DA, Nien CK. Reappraisal of endosonography of ampullary tumors: correlation with transabdominal sonography, CT, and MRI. J Clin Ultrasound. 2009;37:18–25. doi: 10.1002/jcu.20523. [DOI] [PubMed] [Google Scholar]
- 32.Song J, Liu H, Li Z, Yang C, Sun Y, Wang C. Long-term prognosis of surgical treatment for early ampullary cancers and implications for local ampullectomy. BMC Surg. 2015;15:32. doi: 10.1186/s12893-015-0019-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cahen DL, Fockens P, de Wit LT, Offerhaus GJ, Obertop H, Gouma DJ. Local resection or pancreaticoduodenectomy for villous adenoma of the ampulla of Vater diagnosed before operation. Br J Surg. 1997;84:948–951. doi: 10.1002/bjs.1800840711. [DOI] [PubMed] [Google Scholar]
- 34.Ridtitid W, Schmidt SE, Al-Haddad MA, LeBlanc J, DeWitt JM, McHenry L, Fogel EL, Watkins JL, Lehman GA, Sherman S, Coté GA. Performance characteristics of EUS for locoregional evaluation of ampullary lesions. Gastrointest Endosc. 2015;81:380–388. doi: 10.1016/j.gie.2014.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Buscail L, Pagès P, Berthélemy P, Fourtanier G, Frexinos J, Escourrou J. Role of EUS in the management of pancreatic and ampullary carcinoma: a prospective study assessing resectability and prognosis. Gastrointest Endosc. 1999;50:34–40. doi: 10.1016/s0016-5107(99)70341-x. [DOI] [PubMed] [Google Scholar]
- 36.Rejeski JJ, Kundu S, Hauser M, Conway JD, Evans JA, Pawa R, Mishra G. Characteristic endoscopic ultrasound findings of ampullary lesions that predict the need for surgical excision or endoscopic ampullectomy. Endosc Ultrasound. 2016;5:184–188. doi: 10.4103/2303-9027.183978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Klair JS, Irani S, Kozarek R. Best techniques for endoscopic ampullectomy. Curr Opin Gastroenterol. 2020;36:385–392. doi: 10.1097/MOG.0000000000000657. [DOI] [PubMed] [Google Scholar]
- 38.Heise C, Abou Ali E, Hasenclever D, Auriemma F, Gulla A, Regner S, Gaujoux S, Hollenbach M. Systematic Review with Meta-Analysis: Endoscopic and Surgical Resection for Ampullary Lesions. J Clin Med. 2020;9 doi: 10.3390/jcm9113622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Beger HG, Treitschke F, Gansauge F, Harada N, Hiki N, Mattfeldt T. Tumor of the ampulla of Vater: experience with local or radical resection in 171 consecutively treated patients. Arch Surg. 1999;134:526–532. doi: 10.1001/archsurg.134.5.526. [DOI] [PubMed] [Google Scholar]
- 40.Dubois M, Labgaa I, Dorta G, Halkic N. Endoscopic and surgical ampullectomy for non-invasive ampullary tumors: Short-term outcomes. Biosci Trends. 2017;10:507–511. doi: 10.5582/bst.2016.01193. [DOI] [PubMed] [Google Scholar]
- 41.Feng J, Zhou X, Mao W. Prognostic analysis of carcinoma of the ampulla of Vater: pancreaticoduodenectomy versus local resection. Hippokratia. 2012;16:23–28. [PMC free article] [PubMed] [Google Scholar]
- 42.Kim J, Choi SH, Choi DW, Heo JS, Jang KT. Role of transduodenal ampullectomy for tumors of the ampulla of Vater. J Korean Surg Soc. 2011;81:250–256. doi: 10.4174/jkss.2011.81.4.250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Klein P, Reingruber B, Kastl S, Dworak O, Hohenberger W. Is local excision of pT1-ampullary carcinomas justified? Eur J Surg Oncol. 1996;22:366–371. doi: 10.1016/s0748-7983(96)90286-3. [DOI] [PubMed] [Google Scholar]
- 44.Lee H, Park JY, Kwon W, Heo JS, Choi DW, Choi SH. Transduodenal Ampullectomy for the Treatment of Early-Stage Ampulla of Vater Cancer. World J Surg. 2016;40:967–973. doi: 10.1007/s00268-015-3316-x. [DOI] [PubMed] [Google Scholar]
- 45.Nikfarjam M, Muralidharan V, McLean C, Christophi C. Local resection of ampullary adenocarcinomas of the duodenum. ANZ J Surg. 2001;71:529–533. doi: 10.1046/j.1440-1622.2001.02185.x. [DOI] [PubMed] [Google Scholar]
- 46.Papalampros A, Moris D, Petrou A, Dimitrokallis N, Karavokyros I, Schizas D, Delladetsima I, Pappas TN, Felekouras E. Non-Whipple Operations in the Management of Benign, Premalignant and Early Cancerous Duodenal Lesions. Anticancer Res. 2017;37:1443–1452. doi: 10.21873/anticanres.11468. [DOI] [PubMed] [Google Scholar]
- 47.Posner S, Colletti L, Knol J, Mulholland M, Eckhauser F. Safety and long-term efficacy of transduodenal excision for tumors of the ampulla of Vater. Surgery. 2000;128:694–701. doi: 10.1067/msy.2000.108218. [DOI] [PubMed] [Google Scholar]
- 48.Sa Cunha A, Larroudé D, Laurent C, Rault A, Collet D, Masson B. [Value of surgical ampullectomy in the management of benign ampullary tumors] Ann Chir. 2005;130:32–36. doi: 10.1016/j.anchir.2004.11.006. [DOI] [PubMed] [Google Scholar]
- 49.Treitschke F, Beger HG. Local resection of benign periampullary tumors. Ann Oncol. 1999;10 Suppl 4:212–214. [PubMed] [Google Scholar]
- 50.Zhong J, Palta M, Willett CG, McCall SJ, Bulusu A, Tyler DS, White RR, Uronis HE, Pappas TN, Czito BG. The role of local excision in invasive adenocarcinoma of the ampulla of Vater. J Gastrointest Oncol. 2013;4:8–13. doi: 10.3978/j.issn.2078-6891.2012.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Lee JW, Choi SH, Chon HJ, Kim DJ, Kim G, Kwon CI, Ko KH. Robotic transduodenal ampullectomy: A novel minimally invasive approach for ampullary neoplasms. Int J Med Robot. 2019;15:e1979. doi: 10.1002/rcs.1979. [DOI] [PubMed] [Google Scholar]
- 52.Hong S, Song KB, Lee YJ, Park KM, Kim SC, Hwang DW, Lee JH, Shin SH, Kwon J, Ma CH, Hwang S, Park G, Park Y, Lee SJ, Kim YW. Transduodenal ampullectomy for ampullary tumors - single center experience of consecutive 26 patients. Ann Surg Treat Res. 2018;95:22–28. doi: 10.4174/astr.2018.95.1.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Vasen HF, Möslein G, Alonso A, Aretz S, Bernstein I, Bertario L, Blanco I, Bülow S, Burn J, Capella G, Colas C, Engel C, Frayling I, Friedl W, Hes FJ, Hodgson S, Järvinen H, Mecklin JP, Møller P, Myrhøi T, Nagengast FM, Parc Y, Phillips R, Clark SK, de Leon MP, Renkonen-Sinisalo L, Sampson JR, Stormorken A, Tejpar S, Thomas HJ, Wijnen J. Guidelines for the clinical management of familial adenomatous polyposis (FAP) Gut. 2008;57:704–713. doi: 10.1136/gut.2007.136127. [DOI] [PubMed] [Google Scholar]
- 54.Offerhaus GJ, Giardiello FM, Krush AJ, Booker SV, Tersmette AC, Kelley NC, Hamilton SR. The risk of upper gastrointestinal cancer in familial adenomatous polyposis. Gastroenterology. 1992;102:1980–1982. doi: 10.1016/0016-5085(92)90322-p. [DOI] [PubMed] [Google Scholar]
- 55.Spigelman AD, Williams CB, Talbot IC, Domizio P, Phillips RK. Upper gastrointestinal cancer in patients with familial adenomatous polyposis. Lancet. 1989;2:783–785. doi: 10.1016/s0140-6736(89)90840-4. [DOI] [PubMed] [Google Scholar]
- 56.Aiura K, Hibi T, Fujisaki H, Kitago M, Tanabe M, Kawachi S, Itano O, Shinoda M, Yagi H, Masugi Y, Sakamoto M, Kitagawa Y. Proposed indications for limited resection of early ampulla of Vater carcinoma: clinico-histopathological criteria to confirm cure. J Hepatobiliary Pancreat Sci. 2012;19:707–716. doi: 10.1007/s00534-011-0492-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Amini A, Miura JT, Jayakrishnan TT, Johnston FM, Tsai S, Christians KK, Gamblin TC, Turaga KK. Is local resection adequate for T1 stage ampullary cancer? HPB (Oxford) 2015;17:66–71. doi: 10.1111/hpb.12297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Gracient A, Delcenserie R, Chatelain D, Brazier F, Lemouel JP, Regimbeau JM. Endoscopic or surgical ampullectomy for intramucosal ampullary tumor: the patient populations are not the same. J Visc Surg. 2020;157:183–191. doi: 10.1016/j.jviscsurg.2019.11.002. [DOI] [PubMed] [Google Scholar]
- 59.Imamura T, Yamamoto Y, Sugiura T, Okamura Y, Ito T, Ashida R, Ohgi K, Uesaka K. The Prognostic Relevance of the New 8th Edition of the Union for International Cancer Control Classification of TNM Staging for Ampulla of Vater Carcinoma. Ann Surg Oncol. 2019;26:1639–1648. doi: 10.1245/s10434-019-07238-6. [DOI] [PubMed] [Google Scholar]
- 60.Moekotte AL, Malleo G, van Roessel S, Bonds M, Halimi A, Zarantonello L, Napoli N, Dreyer SB, Wellner UF, Bolm L, Mavroeidis VK, Robinson S, Khalil K, Ferraro D, Mortimer MC, Harris S, Al-Sarireh B, Fusai GK, Roberts KJ, Fontana M, White SA, Soonawalla Z, Jamieson NB, Boggi U, Alseidi A, Shablak A, Wilmink JW, Primrose JN, Salvia R, Bassi C, Besselink MG, Abu Hilal M. Gemcitabine-based adjuvant chemotherapy in subtypes of ampullary adenocarcinoma: international propensity score-matched cohort study. Br J Surg. 2020;107:1171–1182. doi: 10.1002/bjs.11555. [DOI] [PubMed] [Google Scholar]
- 61.Kunovský L, Kala Z, Procházka V, Potrusil M, Dastych M, Novotný I, Andrasina T, Pavlovský Z, Eid M, Moravcik P. Surgical Treatment of Ampullary Adenocarcinoma - Single Center Experience and a Review of Literature. Klin Onkol. 2017;31:46–52. doi: 10.14735/amko201846. [DOI] [PubMed] [Google Scholar]
- 62.Branum GD, Pappas TN, Meyers WC. The management of tumors of the ampulla of Vater by local resection. Ann Surg. 1996;224:621–627. doi: 10.1097/00000658-199611000-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Dixon E, Vollmer CM Jr, Sahajpal A, Cattral MS, Grant DR, Taylor BR, Langer B, Gallinger S, Greig PD. Transduodenal resection of peri-ampullary lesions. World J Surg. 2005;29:649–652. doi: 10.1007/s00268-005-7578-6. [DOI] [PubMed] [Google Scholar]
- 64.Nappo G, Gentile D, Galvanin J, Capretti G, Ridolfi C, Petitti T, Spaggiari P, Carrara S, Gavazzi F, Repici A, Zerbi A. Trans-duodenal ampullectomy for ampullary neoplasms: early and long-term outcomes in 36 consecutive patients. Surg Endosc. 2020;34:4358–4368. doi: 10.1007/s00464-019-07206-x. [DOI] [PubMed] [Google Scholar]
- 65.Asbun HJ, Rossi RL, Munson JL. Local resection for ampullary tumors. Is there a place for it? Arch Surg. 1993;128:515–520. doi: 10.1001/archsurg.1993.01420170045006. [DOI] [PubMed] [Google Scholar]
- 66.Milanetto AC, Pasquali C, Da Broi M, Brambilla T, Capretti G, Zerbi A. Ampullary neuroendocrine neoplasms: surgical experience of a rare and challenging entity. Langenbecks Arch Surg. 2018;403:581–589. doi: 10.1007/s00423-018-1695-9. [DOI] [PubMed] [Google Scholar]
- 67.Baptiste GG, Postlewait LM, Ethun CG, Le N, Russell MC, Kooby DA, Staley CA, Maithel SK, Cardona K. Is there an Optimal Surgical Approach to Neuroendocrine Tumors of the Ampulla? Am Surg. 2016;82:637–643. [PubMed] [Google Scholar]
- 68.de Carbonnieres A, Belle A, Gaujoux S. Transduodenal surgical ampullectomy for Intraductal Papillary Neoplasm of the bile duct () J Visc Surg. 2020;157:351–352. doi: 10.1016/j.jviscsurg.2020.06.006. [DOI] [PubMed] [Google Scholar]
- 69.Schneider L, Contin P, Fritz S, Strobel O, Büchler MW, Hackert T. Surgical ampullectomy: an underestimated operation in the era of endoscopy. HPB (Oxford) 2016;18:65–71. doi: 10.1016/j.hpb.2015.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Veldkamp MC, Rauws EA, Dijkgraaf MG, Fockens P, Bruno MJ. Iatrogenic ampullary stenosis: history, endoscopic management, and outcome in a series of 49 patients. Gastrointest Endosc. 2007;66:708–16; quiz 768, 770. doi: 10.1016/j.gie.2006.12.041. [DOI] [PubMed] [Google Scholar]
- 71.Maithel SK, Fong Y. Technical aspects of performing transduodenal ampullectomy. J Gastrointest Surg. 2008;12:1582–1585. doi: 10.1007/s11605-008-0474-2. [DOI] [PubMed] [Google Scholar]
- 72.Sauvanet A, Regimbeau JM, Jaeck D. [Technique of surgical ampullectomy] Ann Chir. 2004;129:381–386. doi: 10.1016/j.anchir.2004.06.001. [DOI] [PubMed] [Google Scholar]
- 73.Wong FCH, Lai ECH, Chung DTM, Tang CN. Robotic transduodenal excision of ampullary tumour. Hepatobiliary Surg Nutr. 2017;6:312–316. doi: 10.21037/hbsn.2016.12.04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Lindell G, Borch K, Tingstedt B, Enell EL, Ihse I. Management of cancer of the ampulla of Vater: does local resection play a role? Dig Surg. 2003;20:511–515. doi: 10.1159/000073647. [DOI] [PubMed] [Google Scholar]
- 75.Park JS, Yoon DS, Kim KS, Choi JS, Lee WJ, Chi HS, Kim BR. Factors influencing recurrence after curative resection for ampulla of Vater carcinoma. J Surg Oncol. 2007;95:286–290. doi: 10.1002/jso.20665. [DOI] [PubMed] [Google Scholar]
- 76.Miossec S, Parc R, Paye F. [Ampullectomy in benign lesion: indications and results] Ann Chir. 2004;129:73–78. doi: 10.1016/j.anchir.2003.10.025. [DOI] [PubMed] [Google Scholar]
- 77.el-Ghazzawy AG, Wade TP, Virgo KS, Johnson FE. Recent experience with cancer of the ampulla of Vater in a national hospital group. Am Surg. 1995;61:607–611. [PubMed] [Google Scholar]
- 78.Kala Z, Weber P, Hemmelová B, Marek F, Hlavsa J, Sobotka M. Ampullary tumours (ampullomas) in the elderly--an interdisciplinary problem. Indian J Med Res. 2010;131:418–421. [PubMed] [Google Scholar]
- 79.Ouaïssi M, Panis Y, Sielezneff I, Alves A, Pirrò N, Robitail S, Heyries L, Valleur P, Sastre B. Long-term outcome after ampullectomy for ampullary lesions associated with familial adenomatous polyposis. Dis Colon Rectum. 2005;48:2192–2196. doi: 10.1007/s10350-005-0187-5. [DOI] [PubMed] [Google Scholar]
- 80.Hollenbach M, Ali EA, Auriemma F, Gulla A, Heise C, Regnér S, Gaujoux S. Study Protocol of the ESAP Study: Endoscopic Papillectomy vs. Surgical Ampullectomy vs. Pancreaticoduodenectomy for Ampullary Neoplasm-A Pancreas2000/EPC Study. Front Med (Lausanne) 2020;7:152. doi: 10.3389/fmed.2020.00152. [DOI] [PMC free article] [PubMed] [Google Scholar]