Abstract
Background/Objectives:
Pediatric healthcare encounters declined during the COVID-19 pandemic, and pediatric residency programs have adapted trainee schedules to meet the needs of this changing clinical environment. We sought to evaluate the impact of the pandemic on pediatric interns’ clinical exposure.
Methods:
In this retrospective cohort study, we quantified patient exposure among pediatric interns from a single large pediatric residency program at a freestanding children’s hospital. Patient encounters and shifts per pediatric intern in the inpatient and emergency department (ED) settings were evaluated during the COVID-19 pandemic, March-June 2020, as compared to these three months in 2019. Patient encounters by diagnosis were also evaluated.
Results:
The median number of patient encounters per intern per two-week block declined on the pediatric hospital medicine (PHM) service (37.5 vs 27.0, p<0.001) and intensive care step-down unit (29.0 vs. 18.8, p=0.004) during the pandemic. No significant difference in ED encounters was observed (63.0 vs. 40.5, p=0.06). The median number of shifts worked per intern per two-week block also decreased on the PHM service (10.5 vs. 9.5, p<0.001). Across all settings, there were more encounters for screening for infectious disease and fewer encounters for respiratory illnesses.
Conclusions:
Pediatric interns at the onset of the COVID-19 pandemic were exposed to fewer patients and had reduced clinical schedules. Careful consideration is needed to track and supplement missed clinical experiences during the pandemic.
Keywords: graduate medical education, emergency pediatrics, general pediatrics, COVID-19 pandemic
Introduction
In the setting of social distancing measures during the coronavirus 2019 (COVID-19) pandemic, pediatric hospitals have reported lower pediatric patient volumes across hospital settings.1–5 In response to these changes and in an effort to minimize resident exposure, residency programs have altered resident schedules.6,7 We sought to evaluate the impact of the COVID-19 pandemic on pediatric interns’ exposure to different types and care settings of pediatric diseases, at the onset of the pandemic and amidst the initial surge. We hypothesized that pediatric interns evaluated fewer patients and that these patients had a different spectrum of disease during the COVID-19 pandemic.
Methods
Study Design and Setting
We performed a retrospective cohort study at a freestanding children’s hospital of patients cared for by pediatric interns from a single large pediatric residency program. The study hospital’s institutional review board approved the study protocol. At the study hospital, interns rotate through the pediatric hospital medicine service (PHM), an intensive care unit (ICU) step-down service, and the emergency department (ED).8 These rotations were selected, as they represent common settings through which pediatric residents across the country typically rotate during the intern year. At the onset of the pandemic, in response to perceived reductions in patient volumes and in an effort to minimize infectious risks, our residency program reduced intern clinical schedules. Shift length was not adjusted during the study period. Patient encounters from other affiliating hospitals where interns also rotate were excluded from analysis given storage in different data warehouses that were not available for data extraction.
Patient Population
We queried the enterprise data warehouse at the study institution and identified patients and the pediatric interns who cared for them during the initial peak of the COVID-19 pandemic (March through June 2020) at the study location as compared to March through June 2019. We included patient encounters in the hospital’s ED and inpatient setting including the PHM and ICU step-down services. We included patient encounters where an intern either wrote a note in the ED or wrote a note or placed an order in the inpatient setting. Patients on whom interns wrote orders during daily rounds were counted towards patient exposures with the rationale that interns had the opportunity to learn about these patients. For the inpatient setting, a patient encounter may span multiple days so documentation of a note or order on any day was counted as a single patient encounter exposure.
Study Outcomes
We evaluated the number of patient encounters per pediatric intern per two-week block and per shift and the number of shifts per intern per two-week block. Shifts worked were determined using the residency program’s online scheduling platform. International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM), codes were collected for all patient encounters. We converted these ICD-10-CM codes into a smaller group of clinically meaningful categories using the Clinical Classifications Software Refined (CCSR) database, developed by the Agency for Healthcare Research and Quality.9 We then evaluated the number of patient encounters with a given CCSR code seen per pediatric intern per two-week block in the inpatient and ED settings.
Data Analyses
Categorical descriptive statistics were used to summarize patient and encounter characteristics. Continuous variables were summarized by median and interquartile range. Wilcoxon rank sum tests (for continuous data) and 2-sample Poisson tests (for incidence data, such as encounters per intern-block) were performed to compare differences in primary outcomes between 2019 and 2020.
Results
Median (interquartile range) patient encounters per intern per two-week block declined by 28.0% on the PHM service (37.5 (36.0-43.0) vs 27.0 (22.0-36.0), p < 0.001) and by 35.5% on the ICU step-down service (29.0 (21.5-35.0) vs. 18.75 (14.0-22.0), p = 0.004) during the pandemic as compared to the year prior (Figure 1A). Median patient encounters per intern per two-week block were not significantly different before versus during the pandemic in the ED (63.0 (57.0-71.0) vs. 40.5 (32.0-57.0), p = 0.06; Figure 1A). The median number of patient encounters per intern per shift declined in the ED (6.7 (6.3-7.1) vs. 4.5 (3.2-5.7), p = 0.04) and in the ICU step-down service (2.7 (2.0-3.5) vs. 1.8 (1.6-2.2), p = 0.03), while encounters per shift were not significantly different for interns on the PHM service during the pandemic (3.5 (3.3-4.2) vs. 3.3 (2.7-3.9), p = 0.13; Figure 1B). Importantly, the number of shifts worked per intern per two-week block was significantly less during the pandemic on the PHM service, while there was no significant difference observed in the ED and the ICU step-down service (Figure 1C).
Figure 1:
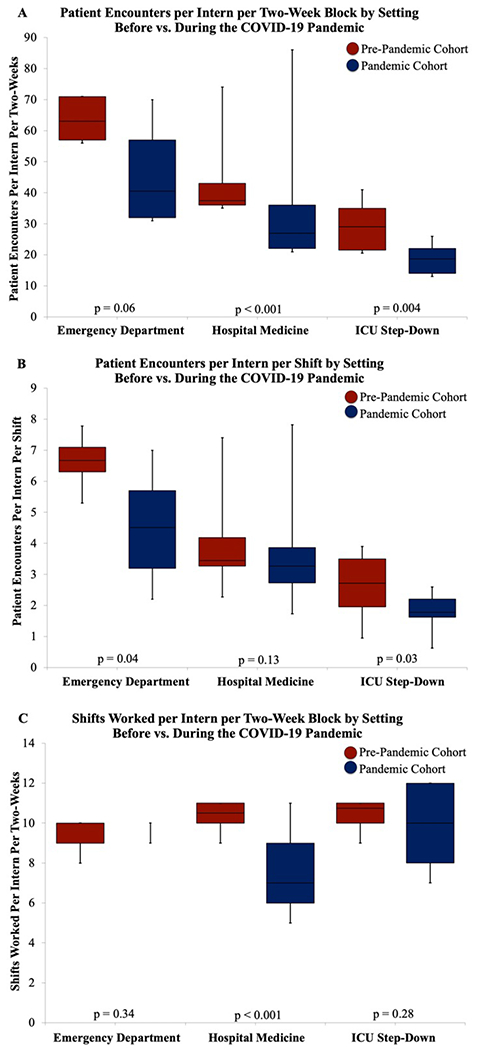
Box and whisker plot of (A) patient encounters per intern per two-week block, (B) patient encounters per intern per shift, and (C) shifts worked per intern per two-week block in the emergency department (ED), pediatric hospital medicine (PHM), and intensive care unit (ICU) step-down settings before vs. during the COVID-19 pandemic.
The mean number of patient encounters per pediatric intern with a given diagnosis is compared before versus during the pandemic in Figure 2A–C. In the inpatient and ED settings, there was an increase in mean encounters per intern per two-week block for the CCSR code, “exposure, encounters, screening or contact with infectious disease”. On the PHM service, the average intern saw 80% fewer patients with “acute bronchitis” during the pandemic (Figure 2B), and reductions in encounters for respiratory illnesses were observed across all three settings. In the ED, there was also a 55% decrease in mean encounters per intern for abdominal pain (Figure 2A).
Figure 2:
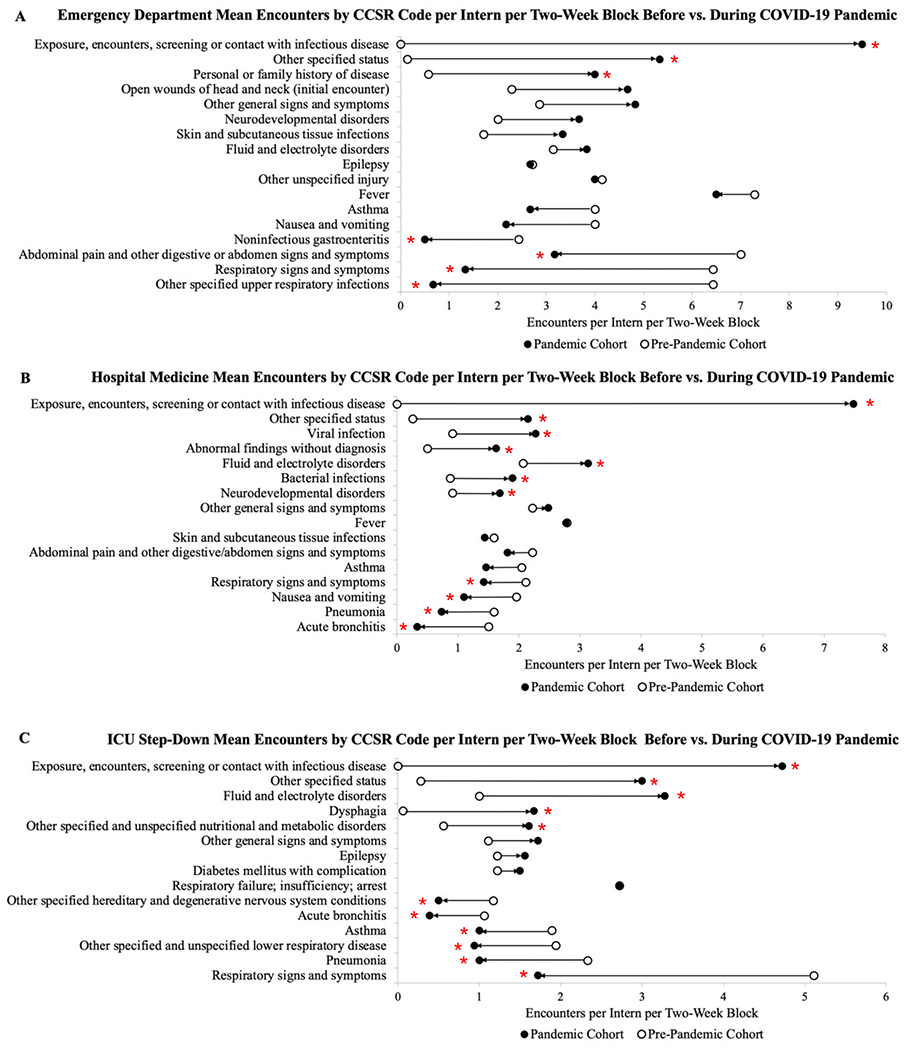
Encounters associated with common CCSR codes before vs. during the COVID-19 pandemic for the (A) emergency department (ED), (B) pediatric hospital medicine (PHM), and (C) intensive care unit (ICU) step-down settings. Values reported as mean encounters by CCSR code per intern per two-week block. Common CCSR codes were identified by the top 10 CCSR codes by setting for both the pre-pandemic and pandemic cohorts. *Indicates statistically significant difference between the pre-pandemic and pandemic cohorts (p < 0.05).
Discussion
During the COVID-19 pandemic, pediatric interns at a large pediatric residency program were exposed to fewer patients and worked fewer shifts in the inpatient and ED settings. Our findings are supported by several recent studies demonstrating reduced pediatric patient volumes across settings nationwide.4,5,10–15 We observed declines in encounters for respiratory illnesses in support of other recent studies documenting similar trends.10,11 While there have been few published studies documenting the impact of COVID-19 on resident patient exposure, one study of an emergency medicine residency in Taiwan demonstrated that ED residents saw less than half the typical patient volume.16 Although our study reflects a single residency program’s experience, early on in the pandemic, declines in pediatric patient census have been documented nationwide. Similarly, residency programs in other specialties have reported on reduced clinical schedules.7,17 Therefore, it is likely that pediatric interns across the country saw significantly fewer pediatric patients and worked reduced shifts on pediatric clinical services during the early COVID-19 pandemic.
These changes have heightened concerns among residency program leadership and trainees about whether reduced patient exposure may impact clinical competency.7,18 In a study of radiology residents assessing the impact of exposure on performance, residents who interpreted more radiographic films had improved performance as measured by accuracy of their diagnostic reads.19 In two other studies evaluating family medicine and internal medicine residents, residents who saw more patients scored higher on in-training exams.20,21 Given this association between exposure and competency, it is therefore important for residency programs to consider tracking resident-level patient exposures during the pandemic. It is also important to recognize that concerns about competency may impact intern confidence in medical decision-making, particularly as they gain additional autonomy at the end of intern year. Acknowledging these concerns and addressing gaps in the clinical experience may alleviate this anxiety and provide interns with the tools to feel more confident and comfortable in their decision-making.
Throughout the pandemic, residency programs in specialties across the country have developed innovative strategies to augment resident clinic experience. Radiology and surgical programs have developed simulations to mimic regular work days for residents.6,24 Our program developed a virtual work from home option for residents with heightened individual or family health risks.25 While these strategies do not replace in-person clinical interactions, virtual learning and patient care play fundamental roles in advancing resident training while also minimizing infectious risks.
Our study has several important limitations. Our findings represent a single residency program’s experience during a 3-month period at the onset of the pandemic and amidst a surge of cases within the community and therefore may not be generalizable to all institutions. However, given documentation of widespread reductions in pediatric patient volumes during the pandemic, pediatric residency programs across the country likely experienced similar trends. We were also unable to assess intern patient exposure during rotations outside the main study hospital which provided important additional training opportunities that were not quantified in this study. Next steps include evaluating intern’s clinical exposure through the 2020-2021 academic year as the pandemic has progressed and also assessing national trends outside of our single institution.
In a large pediatric residency program, the onset of the COVID-19 pandemic was associated with reductions in overall clinical exposure to patients and the breadth of pediatric disease. We identified a disproportionate decrease in patient exposures for respiratory and abdominal symptoms, common complaints that are key complaints for pediatrics residents to gain experience diagnosing and managing. If the COVID-19 pandemic or future pandemics continue to negatively impact pediatric patient volumes, it will be important for residency programs to track intern patient exposures and assess whether reduced volumes impact competency and attainment of professional milestones during training. In addition, identifying reductions in patient exposures by specific setting or disease processes, as we have done in this study, would allow programs to develop targeted interventions through simulation or virtual teaching curricula to supplement the clinical experience.
Acknowledgements
We would like to acknowledge Madeline VanUmmersen and Jessica Angerman for their assistance in extracting data on pediatric intern schedules.
Funding Source:
Dr. Kenneth Michelson received funding through award 1K08HS026503 from the Agency for Healthcare Research and Quality (AHRQ). The funder/sponsor did not participate in the work.
Abbreviations:
- CCSR
Clinical Classifications Software Refined
- ED
emergency department
- ICD-10-CM
International Classification of Diseases, Tenth Revision, Clinical Modification
- ICU
intensive care unit
- PHM
pediatric hospital medicine
Footnotes
Financial Disclosure: The authors have no financial relationships relevant to this article to disclose.
Conflicts of Interest: The authors have no conflicts of interest relevant to this article to disclose.
References
- 1.Zachariah P, Johnson CL, Halabi KC, et al. Epidemiology, Clinical Features, and Disease Severity in Patients With Coronavirus Disease 2019 (COVID-19) in a Children’s Hospital in New York City, New York. JAMA Pediatr. 2020;174(10):e202430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dong Y, Mo X, Hu Y, et al. Epidemiology of COVID-19 Among Children in China. Pediatrics. 2020;145(6):e20200702. [DOI] [PubMed] [Google Scholar]
- 3.Tagarro A, Epalza C, Santos M, et al. Screening and Severity of Coronavirus Disease 2019 (COVID-19) in Children in Madrid, Spain [published online ahead of print, 2020 Apr 8]. JAMA Pediatr. 2020;e201346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Isba R, Edge R, Jenner R, Broughton E, Francis N, Butler J. Where have all the children gone? Decreases in paediatric emergency department attendances at the start of the COVID-19 pandemic of 2020. Arch Dis Child. 2020;105(7):704. [DOI] [PubMed] [Google Scholar]
- 5.Wilder JL, Parsons CR, Growdon AS, Toomey SL, Mansbach JM. Pediatric Hospitalizations During the COVID-19 Pandemic [published online ahead of print, 2020 Nov 3]. Pediatrics. 2020;e2020005983. [DOI] [PubMed] [Google Scholar]
- 6.Johnson J, Chung MT, Carron MA, Chan EY, Lin HS, Hotaling J. Novel Changes in Resident Education during a Pandemic: Strategies and Approaches to Maximize Residency Education and Safety. Int Arch Otorhinolaryngol. 2020;24(3):e267–e271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fero KE, Weinberger JM, Lerman S, Bergman J. Perceived Impact of Urologic Surgery Training Program Modifications due to COVID-19 in the United States. Urology. 2020;143:62–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Miller KA, Hillier D, Russ C, Luercio M, Winn AS. Applying Self-Determination Theory to Redesign an Inpatient Care Team. Acad Pediatr. 2019;19(3):351–353. doi: 10.1016/j.acap.2018.09.010 [DOI] [PubMed] [Google Scholar]
- 9.Healthcare Cost and Utilization Project (HCUP). Clinical Classifications Software Refined (CCSR) for ICD-10-CM Diagnoses.” Agency for Healthcare Research and Quality, https://www.hcup-us.ahrq.gov/toolssoftware/ccsr/ccs_refined.jsp. Accessed November 15, 2020. [Google Scholar]
- 10.Kenyon CC, Hill DA, Henrickson SE, Bryant-Stephens TC, Zorc JJ. Initial effects of the COVID-19 pandemic on pediatric asthma emergency department utilization. J Allergy Clin Immunol Pract. 2020;8(8):2774–2776.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hatoun J, Correa ET, Donahue SMA, Vernacchio L. Social Distancing for COVID-19 and Diagnoses of Other Infectious Diseases in Children. Pediatrics. 2020. September 2 [accessed 2020 Sep 10]:e2020006460. [DOI] [PubMed] [Google Scholar]
- 12.Bram JT, Johnson MA, Magee LC, et al. Where Have All the Fractures Gone? The Epidemiology of Pediatric Fractures During the COVID-19 Pandemic. J Pediatr Orthop. 2020;40(8):373–379. [DOI] [PubMed] [Google Scholar]
- 13.Chaiyachati BH, Agawu A, Zorc JJ, Balamuth F. Trends in Pediatric Emergency Department Utilization after Institution of Coronavirus Disease-19 Mandatory Social Distancing [published online ahead of print, 2020 Jul 20]. J Pediatr. 2020;226:274–277.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.McDonnell T, Nicholson E, Conlon C, et al. Assessing the Impact of COVID-19 Public Health Stages on Paediatric Emergency Attendance. Int J Environ Res Public Health. 2020;17(18):6719. Published 2020 September 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ferrero F, Ossorio MF, Torres FA, Debaisi G. Impact of the COVID-19 pandemic in the paediatric emergency department attendances in Argentina [published online ahead of print, 2020 Jun 18]. Arch Dis Child. 2020;archdischild-2020-319833. [DOI] [PubMed] [Google Scholar]
- 16.Lo HY, Lin SC, Chaou CH, Chang YC, Ng CJ, Chen SY. What is the impact of the COVID-19 pandemic on emergency medicine residency training: an observational study. BMC Med Educ 2020;20(1):348. Published 2020 October 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chick RC, Clifton GT, Peace KM, et al. Using Technology to Maintain the Education of Residents During the COVID-19 Pandemic. J Surg Educ. 2020;77(4):729–732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Oshiro KT, Turner ME, Torres AJ, Crystal MA, Vincent JA, Barry OM. Non-Elective Pediatric Cardiac Catheterization During COVID-19 Pandemic: A New York Center Experience. J Invasive Cardiol. 2020;32(7):E178–E181. [DOI] [PubMed] [Google Scholar]
- 19.Agarwal V, Bump GM, Heller MT, et al. Resident Case Volume Correlates with Clinical Performance: Finding the Sweet Spot. Acad Radiol. 2019;26(1):136–140. [DOI] [PubMed] [Google Scholar]
- 20.Iglar K, Murdoch S, Meaney C, Krueger P. Does clinical exposure matter? Pilot assessment of patient visits in an urban family medicine residency program. Can Fam Physician. 2018;64(1):e42–e48. [PMC free article] [PubMed] [Google Scholar]
- 21.Mizuno A, Tsugawa Y, Shimizu T, Nishizaki Y, Okubo T, Tanoue Y, Konishi R, Shiojiri T, Tokuda Y. The impact of the hospital volume on the performance of residents on the general medicine in-training examination: A multicenter study in Japan. Internal Medicine. 2016. [accessed 2020 Sep 30];55(12):1553–1558. https://pubmed.ncbi.nlm.nih.gov/27301504/. doi: 10.2169/internalmedicine.55.6293 [DOI] [PubMed] [Google Scholar]
- 22.Kwan C, Pusic M, Pecaric M, Weerdenburg K, Tessaro M, Boutis K. The Variable Journey in Learning to Interpret Pediatric Point-of-care Ultrasound Images: A Multicenter Prospective Cohort Study. AEM Educ Train. 2019;4(2):111–122. Published 2019 July 30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lee MS, Pusic M, Carrière B, Dixon A, Stimec J, Boutis K. Building Emergency Medicine Trainee Competency in Pediatric Musculoskeletal Radiograph Interpretation: A Multicenter Prospective Cohort Study. AEM Educ Train. 2019;3(3):269–279. Published 2019 March 12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Recht MP, Fefferman NR, Bittman ME, et al. Preserving Radiology Resident Education During the COVID-19 Pandemic: The Simulated Daily Readout. Acad Radiol. 2020;27(8):1154–1161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Luercio M, Ward VL, Sectish TC, Mateo CM, Michelson CD. One Size Does Not Fit All: Implementation of an Equitable and Inclusive Strategic Response to Address Needs of Pediatric Resident Physicians during the COVID-19 Crisis [published online ahead of print, 2020 Oct 14]. J Pediatr. 2020;S0022-3476(20)31290-7. [DOI] [PMC free article] [PubMed] [Google Scholar]


