Abstract
Objective
The worldwide increase in the incidence of syphilis necessitates alertness to the occurrence of neurosyphilis. Early recognition of neurosyphilis allows for timely treatment, leading to a better treatment outcome. This retrospective study aims to describe the clinical presentation of neurosyphilis in a recent series of neurosyphilis patients.
Method
All patients were included with a new, laboratory confirmed, diagnosis of neurosyphilis in the period 2004-2018. The clinical data were analysed.
Results
34 neurosyphilis patients (1 woman and 33 men) were identified. Age varied from 31-84 years (median age: 44 years). A history of syphilis infection was known for 11 (32%) patients; 12 (35%) patients were HIV seropositive. The distribution of the clinical syndromes was as follows: 16 patients with early neurosyphilis (acute meningitis, meningovasculitis and/or uveitis), 9 patients with late neurosyphilis (General Paralysis of the Insane and/or Tabes Dorsalis), 2 patients with symptoms of both early and late neurosyphilis, 6 patients with asymptomatic neurosyphilis and in 1 patient insufficient data were available to determine a clinical syndrome. Early neurosyphilis was seen in all age categories, late neurosyphilis only occurred in patients > 40 years.
Conclusions
Neurosyphilis occurs in adults in all age groups, in men more frequent than in women, often in HIV-infected patients, and can present with a wide range of clinical syndromes. Usually no previous infection with syphilis is known.
Keywords: neurosyphilis, neuropsychiatry, treponema pallidum, syphilis, HIV co-infection
Introduction
A worldwide increase in the incidence of syphilitic infections is reported since the turn of the 21st century (Fenton et al. 2008). In 2008, the World Health Organization estimated 10.6 million cases among adults worldwide. In the European Union and European Economic Areas, 28,701 syphilis cases (6.0 per 100,000 population) were reported in 2015, mostly in patients older than 25 years of age (ECDC 2017). Between 2010 and 2015, many countries observed a sharp increase of over 50% in the rates of reported syphilis infections, mainly in man having sex with men (MSM) (ECDC 2017), probably related to changing sexual and social norms and to interactions with increasingly prevalent Human Immunodeficiency Virus (HIV) infection (Fenton et al. 2008). Syphilis seems to occur more frequently in the context of substance abuse, migration and underinvestment in public-health services (Fenton et al. 2008).
The causative bacterium of syphilitic infection, the neurotropic Treponema pallidum subspecies pallidum, probably enters the central nervous system (CNS) shortly after infection in up to one-quarter of patients with early syphilis (Marra 2004). In 16-48% of cases with early (primary or secondary) syphilis, abnormalities in the cerebrospinal fluid (CSF) have been detected (Berger and Dean 2014). In a minority of the cases, those unable to spontaneously eradicate the infection from the CSF, asymptomatic or symptomatic neurosyphilis will develop within months or decades (Berger and Dean 2014). In the pre antibiotic era, the Oslo study on the natural history of untreated syphilis demonstrated that 9.4% of the men and 5.0% of the women ultimately developed neurosyphilis (Clark and Danbolt 1955). Since then, early treatment of syphilitic infection with penicillin, antibiotic treatment for intercurrent infections, variation in the incidence of different strains of syphilis, and HIV co-infection, may have changed the course of the disease. However, recent data on the natural history of syphilis are unavailable as yet.
The clinical manifestations of neurosyphilis are traditionally divided into ‘early’ and ‘late’ neurosyphilis. Early neurosyphilis, presenting as meningitis or meningovascular disease, typically manifests within months to several years after the initial infection. Within a year of initial infection involvement of the meninges may result in meningitis with headache, meningismus and cranial nerve palsies, in particular VI, VI, VI and I. Meningovascular disease typically occurs after 6-7 years. About 10% of patients with neurosyphilis and almost 3% of all syphilis patients present with a stroke. In one study, up to 74% of this category of patients were under the age of 50 (Abkur et al. 2015).
Late neurosyphilis primarily affects the CNS parenchyma and occurs 15-30 years after initial infection and results most commonly in the clinical syndromes of General Paralysis of the Insane (GPI) (also termed General Paralysis or Dementia Paralytica) and Tabes Dorsalis (TD) (also known as syphilitic myelopathy) (Berger and Dean 2014). GPI presents with progressive neuropsychiatric symptoms. TD, which affects the dorsal roots, posterior column of the spinal cord, and optic nerves, presents as sensory ataxia with incontinence, pain, and optic atrophy (Marra 2004). Pupillary abnormalities, including Argyll-Robertson pupils (pupils that are small, asymmetric, irregular, and poorly responsive to direct light with maintained appropriate constriction on accommodation) were once a hallmark symptom of TD.
The clinical diagnosis of neurosyphilis is challenging, since neurosyphilis can affect every part of the CNS and may mimic a wide variety of neurological and mental disorders. Moreover, at present no uniform clinical diagnostic criteria have been established. Therefore, CSF analysis is considered crucial for a diagnosis of neurosyphilis. However, a perfect “gold standard” diagnostic test is not available. Treponemal tests, for example the Treponemal pallidum hemagglutination (TPHA) and Treponemal pallidum particle agglutination (TPPA) tests, are used to screen for syphilitic infection. Since these tests may remain reactive for years, even after successful treatment, non-treponemal tests as the Veneral Disease Research Laboratory (VDRL) en the Rapid Plasma Reagin (RPR) test are often used to confirm active syphilitic infection (Peeling 2006). As treponemal antibodies can passively pass an intact blood-brain barrier, higher IgG levels in serum results into higher CSF levels. This leakage of antibodies through the serum-CSF barrier can be distinguished from additional intrathecal production of antibodies by the IgG-serum/CSF index, using the Reiber or TPPA index (Reiber 1994a, Reiber 1994b; Luger et al. 2000).
The present study aims to investigate the clinical characteristics of patients in whom cerebrospinal fluid tested positive for neurosyphilis in the period 2004-2018 in a country with a relatively low syphilis incidence.
Material and methods
In this retrospective case series, all patients with a clinical diagnosis of neurosyphilis, confirmed with a CSF VDRL or PRP ≥ 4, a CSF TPHA ≥ 500, and/or a TPHA CSF-serum index ≥ 70 during the period 2004 to 2018 were examined.
The study protocol was reviewed and approved by the Medical Ethics Committee of the University Medical Centre Groningen, the Netherlands (Number: 2009/333).
CSF serological tests to confirm neurosyphilis were performed by the department of medical microbiology of Certe. Certe is a reference laboratory for syphilis serology, covering a catchment population of 1.1 million inhabitants and nine hospitals in the northeast part of the Netherlands, including the University Medical Centre Groningen. In results and tables of this paper titres, such as 1:250, will be represented as dilutions only, e.g. 250, and the term VDRL will be used instead of VDRL/RPR. In the Certe laboratory the CSF VDRL was completely replaced by the RPR test in 2014 after a lengthy comparison of both methods showed essentially similar results. The TPPA serum-CSF index was calculated as follows: (TPPA cerebrospinal fluid/1000)*(albumin serum/albumin cerebrospinal fluid) (Luger et al. 2000). A TPPA CSF-serum index of ≥ 70 was considered to demonstrate laboratory evidence for a diagnosis of neurosyphilis (Luger et al. 2000). Patients with a history of prior neurosyphilis were excluded.
The medical record of each patient was extensively reviewed for demographic, clinical and laboratory data. Duration of syphilitic disease was pragmatically determined as the interval between positive syphilis serology in the serum and the CSF. Date of onset of neurosyphilis was determined as start of the first neurosyphilitic symptoms as documented in the records. Disease duration of neurosyphilis prior to diagnosis was determined as the interval between the date of reported onset of complaints compatible with neurosyphilis and that of serological confirmation of neurosyphilis. Patients with neurosyphilis were classified according to the criteria as described by Flood et al. (Flood et al. 1998; see: Appendix 1). Asymptomatic neurosyphilis was defined as laboratory confirmed neurosyphilis without neurological signs or symptoms.
For normally distributed data mean and standard deviation were calculated. Non-normally distributed data were described with median, minimum and maxim values.
The non-parametric Wilcoxon rank-sum test was used to test for differences in age distribution in relation to HIV status using an alpha of 0.05 as significant.
To illustrate the clinical presentation of neurosyphilis, a case description is presented.
Results
Patient characteristics
A total of 34 patients (33 men and 1 woman) were identified with neurosyphilis confirmed with CSF serology.
Median age was 44.1 (range 31.3 - 84.0) years. For 30 patients the referring medical speciality was known. Most patients were referred to the neurologist by internist (n=8; 27 %), general practitioner (n=7; 23%), psychiatrist (n=5; 17%) or ophthalmologist (n=4; 13%). In more than half of the male patients (n=19; 58%), the medical record mentioned that they had sex with men.
A history of syphilis was documented for 11 (32%) patients. In 10 (29 %) a history of psychiatric disease was present including substance abuse (n=6), depression (n=4) and /or psychosis (n=2). No patient had a history of dementia. For twelve (35 %) patients a positive HIV serology was documented. The median interval between the diagnoses of HIV infection and neurosyphilis was 2,5 years. The median age of neurosyphilis patients with a documented HIV-infection was significantly lower as compared to those without a documented HIV infection (41.1 years versus 45.1 years; p=0.03).
Presenting symptoms and signs
Information on presenting symptoms was available in 32 (94%) of the patients (table 1).
Table 1.
Presenting symptoms in patients with laboratory confirmed neurosyphilis (n=34)
| Symptoms | n (%) |
|---|---|
| Memory or cognitive complaints | 8 (25%) |
| Visual complaints | 6 (18%) |
| Psychiatric complaints | 6 (19%) |
| Hemiparesis | 5 (16%) |
| Gait disturbances | 5 (16%) |
| Dizziness | 4 (13%) |
| Non-specific symptoms* | 10 (31%) |
| None | 3 (9%) |
*fatigue, dysphagia, headache, myalgia.
Several patients presented with more than one symptom. Most common symptoms were memory or cognitive complaints (n=8; 25%) and visual complaints (n=6; 19%). Three (9%) patients were asymptomatic. Table 2 shows the clinical findings on neurological examination at presentation.
Table 2.
Neurological signs in patients with laboratory confirmed neurosyphilis (n=34)
| Neurological signs | n (%) | missing |
|---|---|---|
| Cognitive dysfunction | 12 (39%) | 3 |
| Cranial nerve abnormalities | 6 (20%) | 4 |
| Abnormal reflexes | 5 (17%) | 5 |
| Motor abnormalities | 5 (17%) | 4 |
| Sensory abnormalities | 5 (17%) | 5 |
| Gait disturbances | 4 (14%) | 6 |
| Pupillary abnormalities | 3 (10%) | 5 |
| Epilepsy not otherwise explained | 1 (3%) | 5 |
Cognitive dysfunction or psychiatric signs at the time of neurosyphilis diagnosis were present in 12 (39%) and 8 (24%) patients, respectively. Delirium was the most common psychiatric disorder at presentation (n=4). Three patients had pupillary abnormalities.
Classification of symptoms
As depicted in table 3, clinical manifestations were categorized in 33 patients.
Table 3.
Age, HIV status and interval between positive syphilis serology in serum and CSF per classification in patients with laboratory confirmed neurosyphilis (n=34)
| N | Median age in years (range) | Number of known HIV+ patients | Interval between positive syphilis serology in the serum and the CSF in days (range) | ||
|---|---|---|---|---|---|
| Early neurosyphilis | 16 | 41 (31-84) | 97 (4-1642) | ||
| Acute syphilitic meningitis | 5 | 3 | |||
| Meningovascular syphilis | 5 | 1 | |||
| Uveitis | 5 | 3 | |||
| Acute syphilitic meningitis and uveitis | 1 | 1 | |||
| Late neurosyphilis | 9 | 61 (43-70) | 214 (28-601) | ||
| General Paralysis of the Insane | 6 | 1 | |||
| Tabes Dorsalis | 2 | 0 | |||
| General Paralysis of the Insane and Tabes Dorsalis | 1 | 0 | |||
| Combined early and late neurosyphilis | 2 | 44 (43-46) | Not available | ||
| General Paralysis of the Insane and acute syphilitic meningitis | 2 | 0 | |||
| Asymptomatic | 6 | 43 (34-45) | 2 | Not applicable | |
| Unclassifiable due to incomplete data | 1 | 1 |
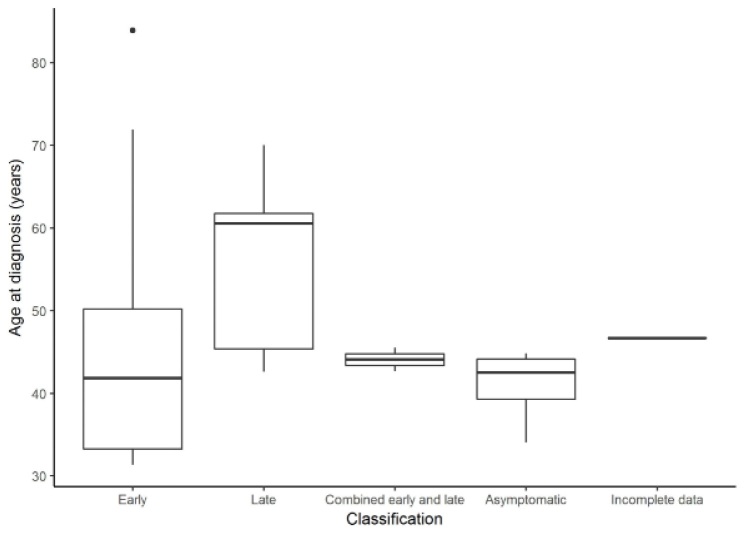
Due to incomplete data classification was not possible for 1 patient. Age at diagnosis per clinical syndrome is presented in figure 1.
Figure 1.
Average age (years) at diagnosis per classification (n=34)
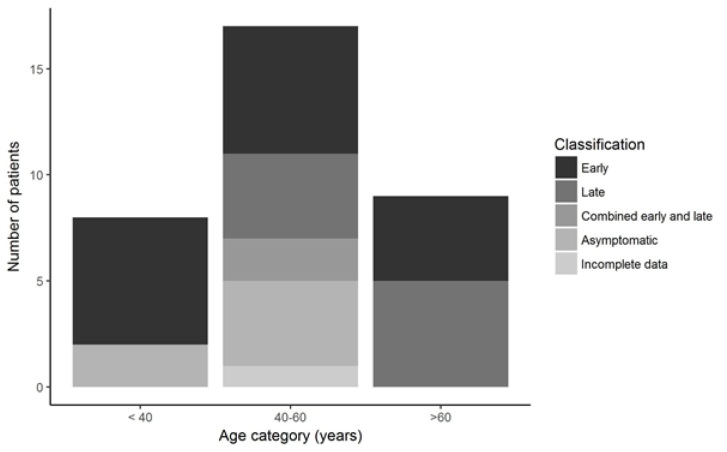
GPI was the most frequent syndrome (n=9, 27%), followed by acute syphilitic meningitis (n=6; 18%). Early neurosyphilis was noticed in all age categories. Late neurosyphilis was not present in patients below 40 years of age (see figure 2).
Figure 2.
Classification of neurosyphilis per age category (n=34)
Duration of syphilitic disease
The interval between positive syphilis serology in the serum and the CSF was less than one year in 24 patients. Of those, 10 presented with early neurosyphilis, seven with late neurosyphilis, four were asymptomatic and two patients presented with combined early and late neurosyphilis. In 10 patients, the interval between positive syphilis serology in the serum and the CSF was more than one year, in that six presented with early neurosyphilis, two with late neurosyphilis whereas two were asymptomatic.
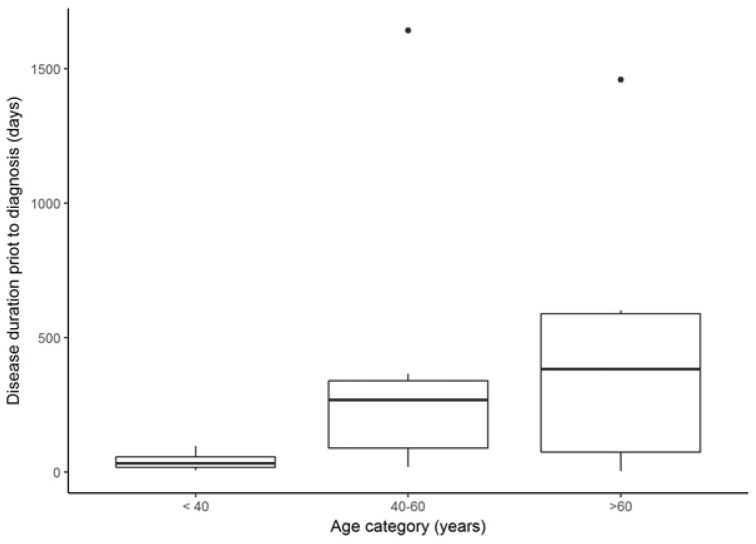
Median interval between positive syphilis serology in the serum and the CSF was 138 days (ranging from 4 days to 4.5 years). Date of first symptoms of neurosyphilis was reported for 17 (61%) out of 28 patients with symptomatic neurosyphilis. As presented in figure 3, disease duration of neurosyphilis prior to diagnosis differed between age categories (43 days for patients aged < 40 year, 269 days for those aged from 40-60 year and 383 days for those > 60 years).
Figure 3.
Disease duration of neurosyphilis prior to diagnosis per age category in days (n=34)
All patients had a TPPA CSF-serum index of ≥ 70. Additional laboratory results are presented in table 4.
Table 4.
Laboratory data in patients with a clinical diagnosis and laboratory confirmed neurosyphilis (n=34) CSF = cerebrospinal fluid; TPHA = Treponema Pallidum Haemagglutination Test; VDRL = Venereal Disease Research Laboratory
| Median (interquartile range) | Missing | |
|---|---|---|
| Total CSF protein | 0.52 (0.38-0.98) g/l | 10 |
| Number of mononuclear cells in CSF | 21 (4-48) | 11 |
| VDRL in CSF | 2 (0-4) | 9 |
| TPHA index | 345 (163-1292) | 0 |
Treatment
Information on antibiotic treatment was available for 28 (82%) patients. All but one patient were initially treated with penicillin; one received doxyxycline. Information on dosing was available for 17 patients. Three patients were treated with less than 18 million units per day. Information on duration of penicillin treatment was available in 23 patients in that 21 received antibiotic treatment for 14 days, one for 10 days and one for six days. Additional treatment with steroids was known for three patients of whom two had uveitis and one GPI.
Case description
A 40-year-old Caucasian man, married and working full time as a circus employee, was admitted to a psychiatric hospital with acute onset of confusion. His medical history was characterized by chronic episodic alcohol abuse and sporadic epileptic seizures. Recently, the patient had been diagnosed with cerebral infarction in the left parieto-occipital region. Apart from alcohol misuse, no specific etiology of a suspected stroke could be identified. His EEG recording showed epileptiform discharges and since the patient was known to have had several epileptic seizures, alcohol withdrawal epileptic seizures were suspected. Treatment with antiepileptic drugs and secondary stroke prevention measures were initiated.
One day prior to admission to the psychiatric hospital, the patient was referred to the emergency department of a general hospital because of several tonic-clonic epileptic seizures within the past 24 hours. Against medical advice, he left the hospital after one day. However, later that day he was admitted to a psychiatric hospital with acute onset of confusion, hypermotility, altered behavior, and irritability.
At psychiatric admission, a poorly groomed, right-handed man was seen with a blood pressure of 127/74 mmHg at a pulse rate of 94 / min. The patient was without fever and systemic examination was unremarkable. Albeit that he was alert and attended to the examiner when his name was called, there was disorientation in time and place. He did not understand all the questions and did not follow commands. He showed paucity of speech, often answered monosyllabically, was unable to concentrate and was not able to recall anything from the days prior to admission. In addition, there were gaps in his long-term memory. There were no indications of delusions or hallucinations. His mood was neutral, with no indication of suicidal ideation or ideas of self-harm. The fingertip nose test and the knee heel test were performed correctly. The tendon reflexes on the arms were low and on the legs lively. His walking pattern was slow and broad-based. He was incontinent for urine and feces. Initially, the patient was cooperative, later he became irritable and refused further physical examination. On the second day of admission, the patient developed a delirium with vivid visual hallucinations.
Laboratory investigations revealed positive serological blood tests for syphilis in serum (TPPA 5000,000; VDRL 32) and CSF (TPPA 500,000; VDRL 16) without any hematological, renal, hepatic, thyroid, or metabolic dysfunctions. HIV tests were negative. Subsequently, a diagnosis of meningovascular neurosyphilis was made and, in accordance with the European Guidelines (Janier et al. 2014) treatment was started with intravenous benzylpenicillin (24 million units daily in six divided doses). Because the patient repeatedly removed his infusion, after two days penicillin was replaced with doxycycline in an oral dose of twice daily 200 mg. Six days later he refused oral medication, and treatment was therefore continued with ceftriaxone 2000 mg 1 dd intramuscularly for 11 days. The comorbid psychotic symptoms were treated according to hospital standard.
In the first month after initiation of antibiotic treatment, there was a slow improvement in the patient’s functional and cognitive status. He displayed more initiative, his gait pattern improved and the incontinence disappeared. Short-term memory and orientation capacity slowly recovered over time. After 4 months, the patient was discharged.
Discussion
This retrospective study, covering a period of 14 years, provides information on the clinical presentation and treatment of 34 patients with laboratory confirmed neurosyphilis in a geographically defined area in a country with low syphilis incidence.
Patient characteristics
Age at symptomatic presentation ranged from 31-84 years (median age: 44 years), which is in accordance with the data reported by other investigators (Zhang et al. 2013, Daey Ouwens et al. 2014, Drago et al. 2016). A lower age at presentation was reported by studies in populations with high rates of syphilis and HIV-co-infection from San Francisco (range 22-88 years; median age 39 years) (Flood et al. 1998) and South Africa (range 17 - 67 years; average 39 years) (Timmermans and Car 2004).
In the present study, the proportion of female patients was lower than that of males, whereas the reported data on the percentage of female patients varies from 9 to 25% (Flood et al. 1998, Daey Ouwens et al. 2014, Drago et al. 2016, Zhang et al. 2013, Mitsonis et al. 2008).
Male predominance has previously been observed in studies on neurosyphilis, especially in studies with a high number of HIV-infected cases (Flood et al. 1998). In the present study, HIV-seropositivity was documented for 35% of patients, which is a higher percentage as reported in other studies (Daey Ouwens et al. 2014, Drago et al. 2016).
The here reported relative absence of female patients may be related to either the high male-to-female ratio of syphilis patients in the Netherlands (ECDC 2017) or the low number of patients included.
Presenting symptoms and signs
At admission, in one third of the patients, psychiatric and / or cognitive complaints were present which is in concordance with data reported by other investigators (Mitsonis et al. 2008, Zhang et al. 2013, Lin et al. 2014). Most probably, cognitive function was not extensively assessed in all included patients, so that the current number may be an underestimation. In the pre-penicillin era, isolated neuropsychiatric symptoms often preceded the full blown clinical manifestation of GPI (Kraepelin 1913). The results of our study advocate that psychiatrists should consider neurosyphilis in the differential diagnosis of all patients with a positive syphilis serology in the blood in the presence of unexplained (progressive) changes in cognition and behaviour, especially when focal neurological signs are lacking.
In the present study, only three patients presented with TD, which is in accordance with the general observation that the incidence of TD has decreased since the beginning of the pre-antibiotic era (Wolters 1987, Carr 2003). Interestingly, speech and micturition disorders, frequently concomitant with late neurosyphilis in the past (Kraepelin 1913, Daey Ouwens et al. 2015), were not observed in the present study.
Although cognitive dysfunction as well as psychotic and depressive symptoms classically belong to GPI, these can also result from meningeal involvement (Drago et al. 2016). This may explain our finding of the coexistence of symptoms of meningitis and GPI in two patients.
Classification
Although the terms “early” and “late” suggest a correlation between duration of syphilitic disease and clinical presentation of neurosyphilis, data on the initial syphilitic infection are rarely reported. Moreover, precise definitions and consensus of the clinical characteristics that accompany these terms are lacking, in that e.g. the reported interval between initial syphilitic infection and vascular syphilis as a presenting syndrome of neurosyphilis varies from less than one year to 4 - 7 years (Carr 2003). Since detailed information about time of occurrence, duration and nature of prior syphilitic symptoms is seldom reported by patients, the interval between syphilitic infection and clinical manifest neurosyphilis is often difficult to establish. Also in this study, in the majority of patients the first known positive blood test of syphilis was performed within 90 days of CSF test of neurosyphilis, suggesting that for most patients the diagnosis of syphilis and neurosyphilis were simultaneously established. Possibly, prior syphilitic infection is not reported by patients with a low number of (unnoticed) syphilitic skin lesions. A low number of skin lesions might be related to a lower concentration of treponemas. Exposure to lower concentrations of treponemas could also attenuate the host immune response causing an impaired ability to clear those that managed to invade the CNS. Consequently, this may result in a greater likelihood to develop symptomatic neurosyphilis (Zhang et al. 2013).
Treatment
Since controlled, randomized, prospective studies for optimal dose and duration of therapy are lacking no uniform worldwide recommended treatment regimen for neurosyphilis is available as yet (Berger and Dean 2014). The European guidelines recommend daily administration of benzylpenicillin 18–24 million units intravenously, divided over 3–4 million units dosages every 4 hours for 10–14 days as first line therapy (Janier et al. 2014). Second line therapy options are ceftriaxone 1–2 g intravenously daily for 10–14 days and, if hospitalization and / or intravenously administration of antibiotics is impossible, procaine penicillin 1.2–2.4 million units intramuscular daily combined with probenecid 500 mg four times daily, both during 10–14 days.
In the present study, cognitive dysfunction and psychiatric symptoms may have hampered intravenous administration of antibiotics which probably explains intravenous treatment for less than 14 days in some patients.
In the literature, the Jarisch-Herxheimer reaction (J-HR), a clinical syndrome composed of abrupt onset of fever, chills, myalgias, tachycardia, vasodilatation with flushing, exacerbated skin rash, and / or mild hypotension, that can occur in patients after the first adequate dose of an antimicrobial drug to treat infectious diseases, is reported in a substantial proportion of syphilis patients. In addition, HIV seropositivity (Yang et al. 2010) and several clinical manifestations of neurosyphilis, such as syphilitic optic neuritis and involvement of the auditory nerve, have been described as a potential risk factor for a dramatic course of J-HR (Zifko et al. 1994, Kojan et al. 2000, Fathilah and Choo 2003, Tucker et al. 2011). Therefore, the European guidelines recommend inpatient management in cases with cardiovascular or neurological involvement and prevention of Jarisch Herxheimer reaction by treatment with Prednisolone 20–60 mg daily for 3 days, starting antitreponemal treatment after 24 h of commencing prednisolone (Janier et al. 2014).
The present case report illustrates that meningovascular neurosyphilis is a severe condition but reversible with appropriate therapy and stresses that neurosyphilis should be included in the differential diagnosis of a young patient with a cryptogenic stroke and in any patient in an acute confusional state.
In sum, main findings of the present study concerning presentation of neurosyphilis are male predominance, regular cognitive, memory and visual complaints and a broad age range. In addition, HIV- seropositivity and prior psychiatric disease were frequently reported. Since most patients were not able to mention any previous syphilitic infection, the interval between first signs and diagnosis was generally long. The results may be biased since only those patients were included in whom CSF analysis was performed by a certificated reference laboratory. Cognitive and memory complaints were probably not systematically assessed, which may have resulted in underestimation of the presence of these symptoms.
Acknowledgements
The authors express their thanks to the treating neurologists for their kind cooperativeness.
Appendix 1: Clinico-Pathological Classification of Neurosyphilitic Symptoms Based on Flood et al. 1998
-
Early neurosyphilis
Syphilitic meningitis: acute syphilitic meningitis, defined by symptoms or findings of acute headache, and/or cranial nerve deficits, with or without meningeal signs (photophobia or meningismus)
Syphilitic meningovascular disease: defined by findings of stroke or other upper motor neuron deficits on exam with characteristic lesions on computed tomography or magnetic resonance imaging of the brain and/or changes consistent with medium-sized vessel vasculitis on angiogram; and
Uveitis, defined by symptoms of decreased vision, eye pain, or photophobia with diagnosis confirmed by slit-lamp examination
-
Late neurosyphilis
General Paralysis of the Insane: defined by a dementia syndrome or subacute psychosis not clearly explained by another process
Tabes Dorsalis: defined by posterior column deficits such as sensory ataxia, Argyll-Robertson pupil, and/or lightning pains
Financial support
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Ethical standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.
References
- Abkur TM, Ahmed GS, Alfaki NO, O’Connor M (2015). Case Report: Neurosyphilis presenting with a stroke-like syndrome. BMJ Case Rep. 2015. doi: 10.1136/bcr-2014-206988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berger JR, Dean D (2014). Neurosyphilis. In Biller J, Ferro JM (eds) Handbook of Clinical Neurology. Vol. 121, 1461-72. Elsevier, 3rd series, New York. [DOI] [PubMed] [Google Scholar]
- Carr J (2003). Neurosyphilis. Pract Neurol 3, 6, 328-341. [Google Scholar]
- Clark EG, Danbolt N (1955). The Oslo study of the natural history of untreated syphilis: An epidemiologic investigation based on a restudy of the Boeck-Bruusgaard material a review and appraisal. J Chronic Dis 2, 3, 311-344. [DOI] [PubMed] [Google Scholar]
- Daey Ouwens IM, Koedijk FD, Fiolet AT, van Veen MG, van den Wijngaard KC, Verhoeven WMA et al. (2014). Neurosyphilis in the mixed urban–rural community of the Netherlands. Acta Neuropsychiatr 26, 3, 186-192. [DOI] [PubMed] [Google Scholar]
- Daey Ouwens IM, Lens CE, Fiolet AT, Ott A, Koehler PJ, Verhoeven WMA (2015). Clinical presentation of general paralysis of the insane in a Dutch psychiatric hospital, 19241954. Eur Neurol 74, 1-2, 54-59. [DOI] [PubMed] [Google Scholar]
- Drago F, Merlo G, Ciccarese G, Agnoletti AF, Cozzani E, Rebora A, Parodi A (2016). Changes in neurosyphilis presentation: a survey on 286 patients. J Eur Acad Dermatology Venereol 30, 11, 1886-1900. [DOI] [PubMed] [Google Scholar]
- ECDC (European Centre for Disease Prevention and Control). (2017). Syphilis. In: ECDC. Annual epidemiological report for 2015. Stockholm: ECDC; 2017. Available online: https://ecdc.europa.eu/sites/portal/files/documents/AER_for_2015-syphilis.pdf.
- Fathilah J, Choo MM (2003). The Jarisch-Herxheimer reaction in ocular syphilis. Med J Malaysia 58, 3, 437-439. [PubMed] [Google Scholar]
- Fenton KA, Breban R, Vardavas R, Okano JT, Martin T, Aral S et al. (2008). Infectious syphilis in high-income settings in the 21st century. Lancet Infect Dis 8, 4, 244-253. [DOI] [PubMed] [Google Scholar]
- Flood JM, Weinstock HS, Guroy ME, Bayne L, Simon RP, Bolan G (1998). Neurosyphilis during the AIDS epidemic, San Francisco, 1985-1992. J Infect Dis 177, 4, 931-940. [DOI] [PubMed] [Google Scholar]
- Janier M, Hegyi V, Dupin N, Unemo M, Tiplica GS, Potočnik M et al. (2014). European guideline on the management of syphilis. JEDV 28, 12, 1581-1593. [DOI] [PubMed] [Google Scholar]
- Kojan S, van Ness PC, Diaz-Arrastia R (2000). Nonconvulsive status epilepticus resulting from Jarisch-Herxheimer reaction in a patient with neurosyphilis. Clin Electroencephalogr 31, 3, 138-140. [DOI] [PubMed] [Google Scholar]
- Kraepelin E (1913). General Paresis. Translation by Moore JW. Nervous and Mental Disease Publishing Company, New York. [Google Scholar]
- Lin LR, Zhang HL, Huang SJ, Zeng YL, Xi Y, Guo XJ, et al. (2014). Psychiatric manifestations as primary symptom of neurosyphilis among HIV-negative patients. J Neuropsychiatry Clin Neurosci 26, 3, 233-240. [DOI] [PubMed] [Google Scholar]
- Luger AF, Schmidt BL, Kaulich M (2000). Significance of laboratory findings for the diagnosis of neurosyphilis. Int J STD AIDS 11, 4, 224-234. [DOI] [PubMed] [Google Scholar]
- Marra CM (2004). Neurosyphilis. Curr Neurol Neurosci Rep 4, 6, 435-440. [DOI] [PubMed] [Google Scholar]
- Mitsonis C, Kararizou E, Dimopoulos N, Triantafyllou N, Kapaki E, Mitropoulos P (2008). Incidence and clinical presentation of neurosyphilis: a retrospective study of 81 cases. Int J Neurosci 118, 9, 1251-1257. [DOI] [PubMed] [Google Scholar]
- Peeling RW, Holmes KK, Mabey D, Ronald A (2006). Rapid tests for STIs: the way forward. Sexually transmitted infections 82, Suppl. 5, V1-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reiber H (1994a). Flow rate of cerebrospinal fluid (CSF) a concept common to normal blood-CSF barrier function and to dysfunction in neurological diseases. J Neurol Sci 122, 2, 189-203. [DOI] [PubMed] [Google Scholar]
- Reiber H (1994b). The hyperbolic function: a mathematical solution of the protein flux/CSF flow model for blood-CSF barrier function. J Neurol Sci 126, 2, 243-245. [Google Scholar]
- Timmermans M, Carr J (2004). Neurosyphilis in the modern era. J Neurol Neurosurg Psychiatry 75, 1727-1730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tucker JD, Li JZ, Robbins GK, Davis BT, Lobo AM, Kunkel J et al. (2011). Ocular syphilis among HIV-infected patients: a systematic analysis of the literature. Sex Transm Infect 87, 1, 4-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolters EC (1987). Neurosyphilis: a changing diagnostic problem? Eur Neurol 26, 1, 23-28. [DOI] [PubMed] [Google Scholar]
- Yang CJ, Lee NY, Lin YH, Lee HC, Ko WC, Liao CH et al. (2010). Jarisch-Herxheimer reaction after penicillin therapy among patients with syphilis in the era of the HIV infection epidemic: incidence and risk factors. Clin Infect Dis 51, 8, 976-979. [DOI] [PubMed] [Google Scholar]
- Zhang HL, Lin LR, Liu GL, Zeng YL, Wu JY, Zheng WH et al. (2013). Clinical spectrum of neurosyphilis among HIV-negative patients in the modern era. Dermatology 226, 2, 148-156. [DOI] [PubMed] [Google Scholar]
- Zifko U, Lindner K, Wimberger D, Volc B, Grisold W (1994). Jarisch-Herxheimer reaction in a patient with neurosyphilis. J Neurol Neurosurg Psychiatry 57, 7, 865-867. [DOI] [PMC free article] [PubMed] [Google Scholar]