Abstract
PURPOSE:
One third of the U.S. adult population is estimated to have prediabetes. Hispanics have a 50% higher type 2 diabetes (T2DM) death rate compared to non-Hispanic whites, yet low participation in lifestyle change programs, making this subgroup an important target for prevention efforts. The purpose of this study was to determine the effects of an exercise intervention implementing the Center for Disease Control and Prevention (CDC) National Diabetes Prevention Program (NDPP) plus recreational soccer (RS) in Hispanic men.
METHODS:
Overweight and obese Hispanic men, aged 30–57 years with prediabetes at screening were recruited from the community. Trained soccer coaches led 30-min facilitated discussion of the NDPP modules after each RS session, with two wkly sessions delivered over 12 wks, then once a wk until 24 wks. The 1-h RS sessions followed the Football Fitness curriculum structure. Standardized study assessments included objectively measured physical activity via fitness tracker, physical fitness via validated field tests, GPS soccer specific metrics and behavior change questionnaires. Mixed models assessed the outcomes as a function of time and cohort and incorporated an unstructured covariance structure to examine the difference between baseline, 12 and 24 wks. All analyses were conducted as intent-to-treat and generated using SAS v 9.4.
RESULTS:
Hispanic males (n=41; mean age 41.9 [6.2 SD] years) were obese at baseline (mean BMI 32.7, standard error [0.7]). After 24 wks of the NDPP+RS intervention, there were significant beneficial changes in vertical jump (2.8 [1.3] cm; p=0.048), agility and lower extremity muscular power (figure 8-run) at 12 wks (−4.7% change; p=0.001) and 24 wks (−7.2% change; p<0.0001), predicted VO2 max (12 wks: 1.9%; p=0.007; 24 wks 1.0%; p=0.036), modified push-ups increased 22% (p<0.0001) at 12 wks and 31% (p<0.0001) at 24 wks, dynamic sit-ups increased 10% (p= 0.005) at 12 wks and 15% (p<0.0001) at 24 wks.
CONCLUSION:
Among middle-aged Latino men, broad-ranging significant improvements in physical fitness were observed after 24 wks participating in lifestyle education plus RS in a single arm feasibility trial.
Keywords: soccer, football, recreational sport, exercise, fitness
Introduction
While the exact dose of physical activity (PA) for the prevention of type 2 diabetes (T2DM) is unknown, data shows that increased physical inactivity and sedentary behavior perpetuates the incidence of diabetes and other obesity-related chronic diseases.1–4 There is significant evidence to support that even moderate amounts of wkly PA decreases the risk of type 2 diabetes onset.5,6 The U.S National Diabetes Prevention Program (NDPP) implements an evidence-based model to help pre-diabetic individuals navigate the process for engaging in sustainable lifestyle changes, including diet and PA improvements and a 5–7% weight loss goal. The NDPP uses a classroom-based, peer-facilitated approach to encourage participation in regular PA, largely on the participants own time, with the goal to achieve compliance with the PA guidelines (150 mins of moderate-to-vigorous PA/wk) prioritizing walking and potentially with the help of pedometers or fitness trackers.7
In the original NDPP study, 67% of the participants were able to achieve the PA goals using a one-on-one counseling approach.7 Participants meeting the PA goals but not reaching the weight loss goals still showed a 44% reduction in T2DM incidence.8 Today, most NDPP offerings use a group-based approach (50%) and enrollment is much lower in non-Hispanic whites when stratified by race/ethnicity.9
Hispanic men are the least likely to participate in a year-long classroom-based NDPP and also have low recreational PA levels.10,11 Social support, self-efficacy, enjoyment and motivation to start and maintain PA and lifestyle changes are important drivers of program efficacy. Participation in recreational sports can be a conducive environment to promote physical activity engagement given their fun, social, and competitive nature. Recreational soccer (RS), played as small-sided games (5v5 or 7v7) on a smaller pitch, induces higher heart rates for longer periods, high anaerobic energy production with concomitant lower rates of perceived exertion, compared to jogging or walking programs12,13 This combination leads to longer retention and a more enjoyable experience.14–16 In some respects, RS can be considered a modality of high intensity interval training (HIIT) with a wide range of physiologic effects that surpasses recreational running or other fitness training.13,17–20
Recreational soccer interventions have been shown to improve cardiometabolic risk and increase cardiorespiratory fitness in untrained adults.21,22 However, these intervention approaches have not been yet tested in settings outside of Europe, South America and Asia. We conducted a pilot, single-arm, unblinded clinical trial to assess the implementation feasibility and physical fitness impacts in U.S Hispanic men, using an adapted NDPP six-month program. Our hypothesis was that enrolled Hispanic men increase participation in regular physical activity and improve their physical fitness by engaging in a recreational soccer-based adaptation to the traditional NDPP.
Methods
Participants
Study Inclusion and Exclusion Criteria
The inclusion criteria for participation in the study were: 1) Hispanic/Latino men aged 35–55 years; 2) body mass index (BMI) ≥ 25 kg/m2; 3) elevated risk for diabetes, operationalized as a score ≥ 9 in the CDC pre-diabetes risk calculator (13); 4) not engaged in regular soccer practice or other PA or lifestyle intervention program in the last year; 5) ability to read in English or Spanish and to provide inform consent. Participants were excluded if: 1) they reported a T2DM diagnosis or medication (oral or injected); 2) BMI ≥ 40; 3) resting blood pressure ≥170/100 mm Hg at screening; 4) any mobility issues or contraindications for HIIT PA program.23
Study Design
This study was designed as a pilot study to determine feasibility of recruitment and retention of Hispanic men in Atlanta, GA, USA. This single arm unblinded clinical trial recruited a total of 41 participants from April to July 2018. (ClinicalTrials.gov Identifier: NCT03595384).24 Participants were recruited from local Atlanta area Latino organizations using online (social media, websites, email listservs) and print (study recruitment fliers) advertisements methods. Sample size was determined using a 10% attrition rate and we calculated that 40 participants would provide at least 86% power to detect a mean difference in PA as the primary outcome (100 mins/wk; standard deviation (SD) 200 mins) and over 90% for detecting significant changes in weight (1.45 kg; SD 0.18) and VO2max (3.93 ml/kg/min; SD 0.5) from baseline to 24 wks using a two-sample t-test. Interested participants were provided an online survey to ascertain eligibility (Centers for Disease Control and Prevention (CDC) pre-diabetes screening, demographic questions and PA habits) and those meeting inclusion criteria were invited to an initial session at a local soccer field for informed consent and confirmatory baseline assessments including BMI, blood pressure, HbA1c and exercise pre-participation risk screening.23,25 Siemens DCA Vantage HbA1c point-of-care devices (Erlangen, Germany) were used for diabetes screening. A cut off point of 6.5% was used as a putative definition of T2DM26,27 and these individuals were referred to a local clinic for confirmatory testing and appropriate management. Both systolic and diastolic blood pressure were measured while sitting using a calibrated electronic blood pressure sphygmomanometer (Omron, Kyoto, Japan) prior to any activity and after five mins of rest. Prior to testing, subjects were asked to refrain from physical activity for 48 hs prior to test day, refrain from alcohol 24 h prior to testing, and refrain from caffeinated drinks, smoking and other stimulants one h prior to testing. Participants meeting inclusion and exclusion criteria were invited to participate in the study.
All participants were informed of risks and provided informed consent in the language of their choice. The study was carried out in accordance with the guidelines set by the Institutional Review Board at Emory University (IRB#00100342).
Outcomes
The primary outcomes was aerobic fitness determined by the Yo-Yo Intermittent Recovery Test Level 1 (Yo-Yo IR1) (test-retest CV – 4.9%28). Predicted VO2max was calculated from the Yo-Yo IR1 stage level reached.14,29,30 Secondary outcomes included strength determined by handgrip measurement (Takei Digital Grip Strength Dynamometer, Model T.K.K.5401, Tokyo, Japan)31,32, vertical jump (VERT, Fort Lauderdale, FL, USA)33, and figure 8 run test, modified push-ups, dynamic sit-ups, all using the Assessing Levels of Physical Activity (ALPHA) Battery Fit test protocols.34,35 The Yo-Yo IR1 was conducted on the soccer field using an automated timed voice recording. Two cones were set 20 m apart for each participant. Completed stage level was recorded for each participant. Handgrip strength was determined using the National Health and Examination Survey protocol.36,37 Each hand was measured three times alternatively and kg were recorded. The average of the three measurements from the dominant hand results are reported here. Vertical jump was measured twice with the VERT device attached to the waistband and the two measurements were averaged. Daily steps, sleep, sedentary time, light physical activity and weekly average moderate to vigorous PA (MVPA) were measured using Garmin wearable devices (Vivofit 3, Olathe, KS, USA).38,39 The Garmin Vivofit 3 has been shown equivalent to Yamax pedometers and have a 1-yr battery life which increases participant’s wear time.39 Garmins were given in the 3rd week of the intervention to coincide with the first physical activity NDPP core module. We also collected behavior change questionnaire data using the Brief Resilience Scale (BREQ-2) and Behavioral Regulation in Exercise questionnaire.40,41 Assessments were conducted at baseline before the first soccer session, after the 12-wk initial soccer conditioning phase, and at 24-wks after the soccer league (maintenance phase of the program). Participants were all briefed on the various measurements prior to the tests and all study staff were trained and demonstrated ability to perform measurements. STROBE-compliant flowchart of recruitment included in Supplemental materials Figure 1.
GPS exercise performance data during soccer sessions
A soccer-specific global positioning system (GPS) was used for the first two cohorts of participants. Data were collected using a 10 Hz GPS/GNSS Playertek system (Catapult Sports, Melbourne, Australia) which includes a 400 Hz sampling rate and 3 axes accelerometer. Each participant was assigned a specific numbered GPS Playertek Device which they consistently used for every session they attended. This process was documented on the session attendance log. After each session, the exercise statistics collected on all used GPS Playertek devices were uploaded to the online Playertek database using Catapult software. Here, the data from each device was matched with the participant’s profile, and then organized by cohort. Metrics calculated in the PlayerTek team software included session duration, total distance covered, sprint distance (5 m/s), estimated energy expenditure, distance covered per min, player load, power score, work ratio, power plays and top speed.42 Participants who attended the sessions regularly, used the GPS Playertek devices at higher frequencies, compared to those with lower rates of attendance.
Program Delivery Personnel
Three bilingual coaches (Fédération Internationale de Football Association (FIFA) or US Soccer certificate) were recruited and trained on intervention procedures. They all completed the “Football is Medicine” training course (6 hs theory, 2 hs practice) and received a copy of the Coaches “Football Fitness Manual” with drills exercises developed by Krustrup et al.43 They also received training on safety precautions according to the American College of Sports Medicine Exercise Pre-participation Guidelines and obtained a certification in cardio-pulmonary resuscitation.23 Furthermore, they were also trained by a certified NDPP lifestyle coach on how to deliver and facilitate the NDPP curriculum.44
Intervention
After the baseline assessments, participants were asked to attend a group soccer practice twice a week for a 12-wk period designed to replicate the concept of “pre-season conditioning.” Three groups of 10–14 participants were assembled, assigned a coach and session scheduling was tailored to the group’s preference based on field availability and location convenience for participants. Sessions were held on the evenings (typically Friday and Sunday) allowing at least 48 hs rest for recovery and to maximize physiologic adaptations. Each RS conditioning session included an evidence-based 10-min dynamic warm-up (FIFA 11+),45 20 mins of soccer-specific drills with and without the ball and 20-min recreational short-sided soccer games 5v5 up to 7v7 format depending on session attendance. During this 12-wk period, participants completed the NDPP core curriculum modules (one/wk). At the end of the soccer session and while hydrating and cooling down, participants sat in a group to discuss the NDPP modules with facilitation by their coach, during the last 30 mins of each 80-min study session. Sessions were held in parallel for the three cohorts in a full-size soccer artificial turf soccer field. Participants were encouraged to bring family and/or friends as spectators for additional social support. Although family/friends were not allowed to actively participate in the RS or NDPP programming, significant others often walked/jogged around the field and children actively used an adjacent playground (no evaluation data collected on this).
Upon successfully completing the “pre-season soccer conditioning” phase and the 12-wk assessment, participants transitioned to the “soccer maintenance” phase of the intervention for an additional 12 wks. During this phase, RS sessions were offered only once/wk and consisted of a 10-min dynamic warm-up and a 40-min recreational soccer game (two 18-min halves and a 4-min half time break). Participants were divided into six teams and a league-style scheduled was created to encourage healthy competition but with modifications to reduce risk of injuries (no slide tackles, no standing goalie). Teams were reshuffled every four wks to encourage group cohesion. Individuals were awarded points mostly (70%) based on attendance and weight loss or maintenance (negative points if no attendance or if participant gained more than 1 kg from previous wk), while the outcome of the game (3 points for win; 1 point for tie) was valued at 30%. A facilitated discussion of the NDPP maintenance modules was held for 30 mins after each session in this maintenance phase. At the end of the 24-wk study period, a closing ceremony was held and all participants attending at least 50% of all soccer sessions given a certificate of program graduation while those with the best attendance and sportsmanship recognized with plaques.
A closed and encrypted chat (WhatsApp platform) was created for each cohort and full group to facilitate peer-support, communication and session attendance (i.e schedule changes). Coaches provided attendance encouragement wkly and participants also used it to post encouraging messages and provide support (i.e. picture examples of their dietary choices, activity levels outside of soccer sessions, etc.). Coaches recorded session attendance, wkly weights and rates of perceived exertion (10-point modified Borg scale)46 and reported any injuries or adverse events.
Data Analysis
All analyses were conducted as intent-to-treat. Mixed models with unstructured heterogeneous covariance structures, were used to analyze outcomes at each time point. The maximum likelihood estimation procedure was used to handle missing data. For each outcome measure, the model assessed the outcome as a function of time (baseline, 12 and 24-wks) and adjusted for assigned cohort. All dependent variables were modeled using fixed effects. Least square means adjusted for cohort effect were reported for each outcome. Hypotheses were two sided and tested at a 0.05 significance level. Analyses were conducted using SAS 9.4 (SAS Institute, Cary, North Carolina, USA).
Results
Baseline demographics are shown in Table 1. The mean age of 41 participants was 41.9 (SD=6.2) years old. Most of the participants were married (83%) and were employed (93%) and 43.6% had a college or technical school degree. A little more than half (51%) had a family history of diabetes (14.6% had a sibling and 43.9% a parent with diabetes).
Table 1.
Demographics
| Characteristics | N (%) |
|---|---|
| Age, years, mean (SD), range | 41.9 (6.2), 32–57 |
| Male | 41 (100) |
| Family history of diabetes | 21 (51) |
| Have a sibling with diabetes | 6 (15) |
| Have a parent with diabetes | 18 (44) |
| Country of origin | |
| Mexico | 16 (39) |
| Venezuela | 4 (10) |
| Ecuador | 3 (7) |
| Guatemala | 4 (10) |
| Colombia | 7 (17) |
| Other | 7 (17) |
| Marital status | |
| Single, divorced or widowed | 7 (12) |
| Married or domestic partner | 36 (88) |
| Education | |
| Some high school or less | 7 (17) |
| High school | 10 (24) |
| College degree | 18 (44) |
| Tech school | 4 (10) |
| Employment | |
| Employed | 37 (90) |
| Unemployed | 3 (10) |
| Smoking | |
| Current smoker | 2 (5) |
| Former smoker | 3 (7) |
| Never smoke | 11 (27) |
| Missing | 25 (61) |
Objectively-measured Physical Activity
Garmin Vivofit 3 fitness trackers were given in the third week of the intervention. Baseline means and standard error (SE) and ranges for daily steps, daily mins of light PA, weekly average minutes of MVPA, daily hours of sleep and sedentary time were 12,645 (769) 7,482–23,868 steps, 107 (7) 57–189 mins, 73 (17) 0–258 mins, 7.1 (0.2) 6.3–8.5 hs, 15.2 (0.2) 13.8–16.4, respectively. There was then a significant decline in daily steps from baseline to 3 (−12%; p=0.014) and 24 wks −23%; p=0.005) (Figure 1). Daily light PA also declined slightly from baseline to 12 wks (−11%; p=0.06) and again at 24 wks (−26%; p< 0.0001). There were no significant changes in wkly MVPA duration or of sedentary time and sleep.
Figure 1.
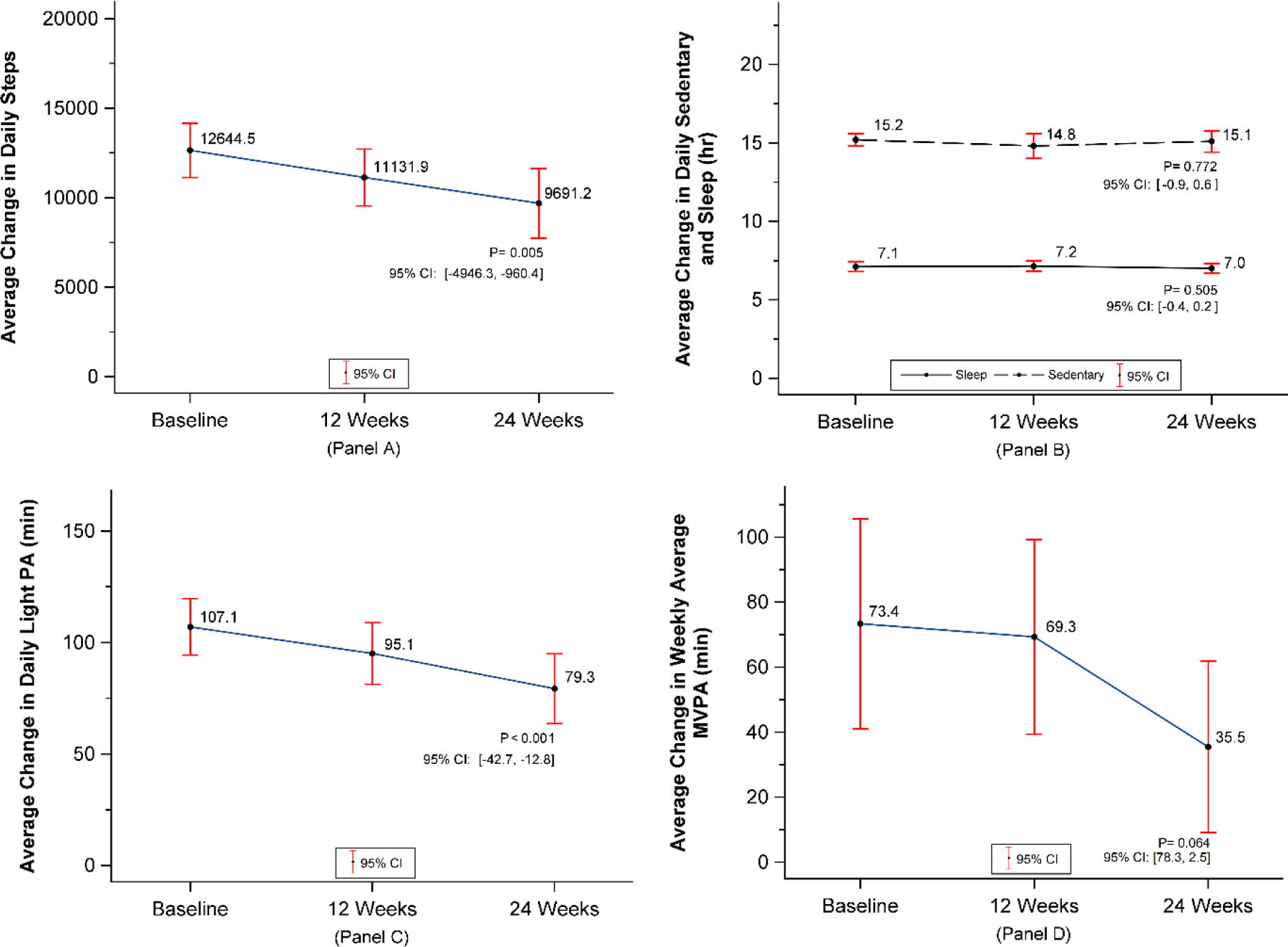
Objectively measured physical activity measurements at baseline, 12 and 24 wk time points. Panel A – Average change in daily steps measured by Garmin Vivofit 3; Panel B – Average change in daily sedentary and sleep time in hs; Panel C – Average change in daily light physical activity in mins; Panel D – Average change in wkly average moderate to vigorous physical activity in mins.
Physical Fitness
Baseline estimated VO2max via Yo-Yo IR1was 38.9 ml/kg/min (0.2 SE; Range 32.0–41.4) and significantly increased over time (12 wks: 1.9%; p=0.007; 24 wks 1.0%; p=0.036) (Figure 2).30 For agility, the figure-8 run test was used. At baseline, the mean time in s was 7.2 (SE 0.1) and the range was 5.3–9.2 s. There was a significant decrease at 12 wks (−4.7% change; p=0.001) and a further decrease at 24 wks (−7.2% change; p<0.0001).
Figure 2.
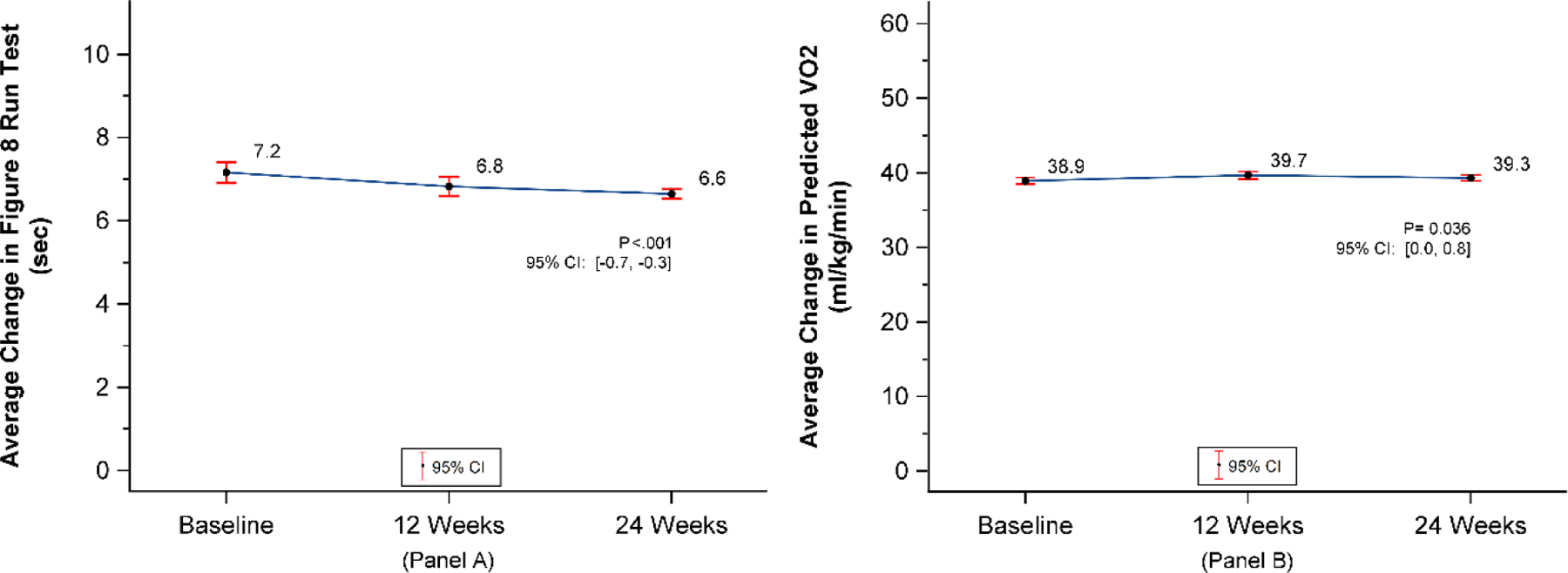
Aerobic fitness measurements at baseline, 12 and 24 wk time points. Panel A – Average change in agility figure 8 run test in s; Panel B – Average change in predicted VO2 max (ml/kg/min).
Muscle strength was measured in a variety of ways. Handgrip was on average 49.2 kg (SE 1.2) range – 28.5–67.0 kg using the dominant hand. There was an increase of 5% (p=0.02) at 12 wks and 7% (p=0.002) at 24 wks. From the ALPHA Battery tests, dynamic sit-ups were 13 reps (SE 0.4) range- 5–15 at baseline and increased 10% (p= 0.005) at 12 wks and 15% (p<0.0001) at 24 wks, modified push-ups averaged 13 reps (SE 0.4) range 7–20 reps and increased 22% (p<0.0001) at 12 wks and 31% (p<0.0001) at 24 wks. (Figure 3) Vertical jump was used to measure leg strength and was 43 cm (SE 1.2) range 25.6–61.5 cm at baseline and increased 13% (p=0.03) at 12 wks and 6% (p=0.05) at 24 wks. (Figure 3)
Figure 3.
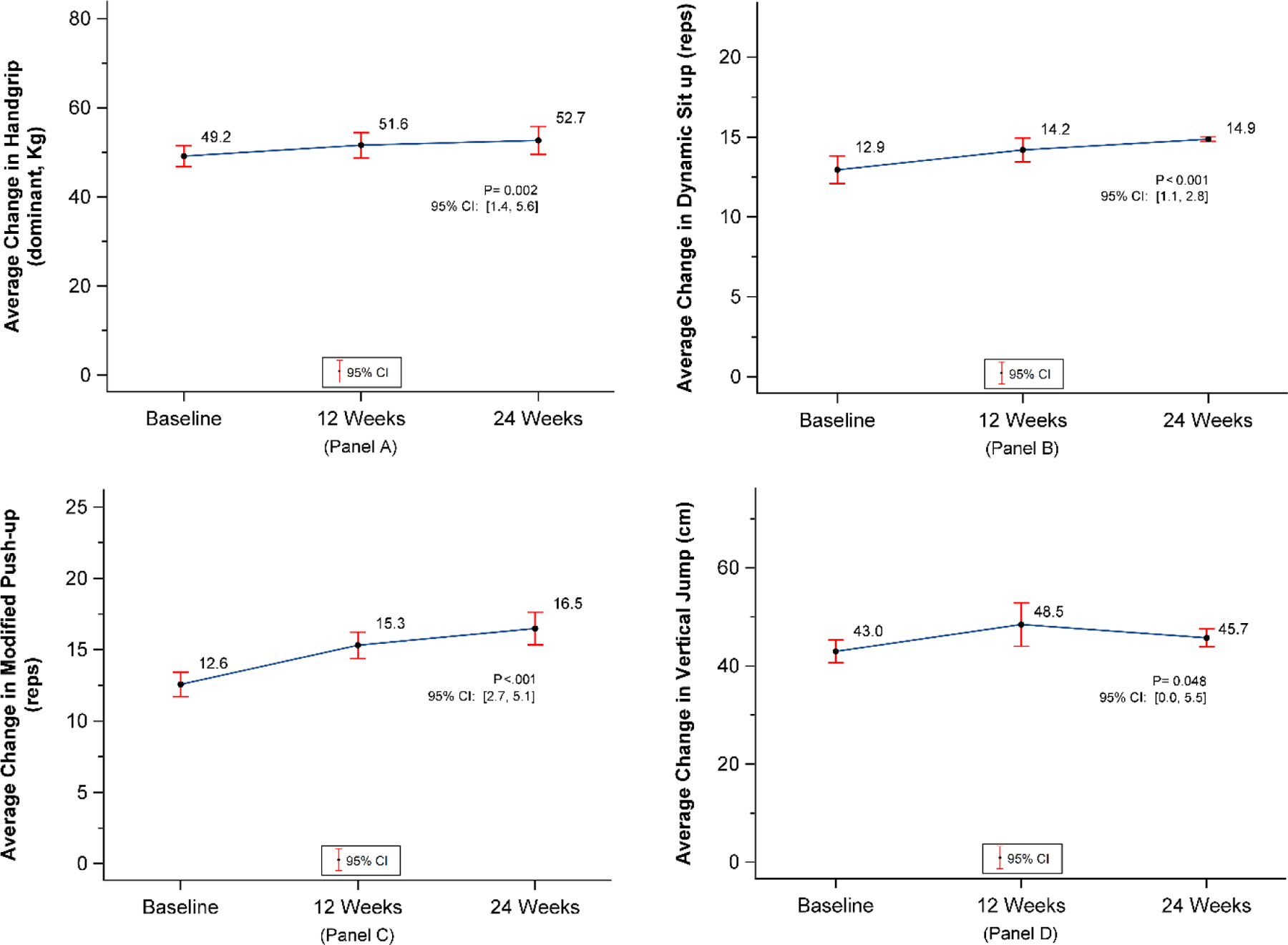
Muscle strength measurements at baseline, 12 and 24 wk time points. Panel A – Average change in handgrip strength in the dominant hand measured in kilograms; Panel B – Average change in dynamic sit ups in repetitions; Panel C – Average change in modified push-ups in repetitions; Panel D – Average change in vertical jump in centimeters.
GPS Soccer-session data
Most metrics displayed a statistically significant change over the six-month intervention. There was no increase in session exercise duration at the end of the 24 wks, but a slight increase at the 12-wk mark. (Figure 4) There was also no change in top speed over the 24 wks. (Figure 5)
Figure 4.
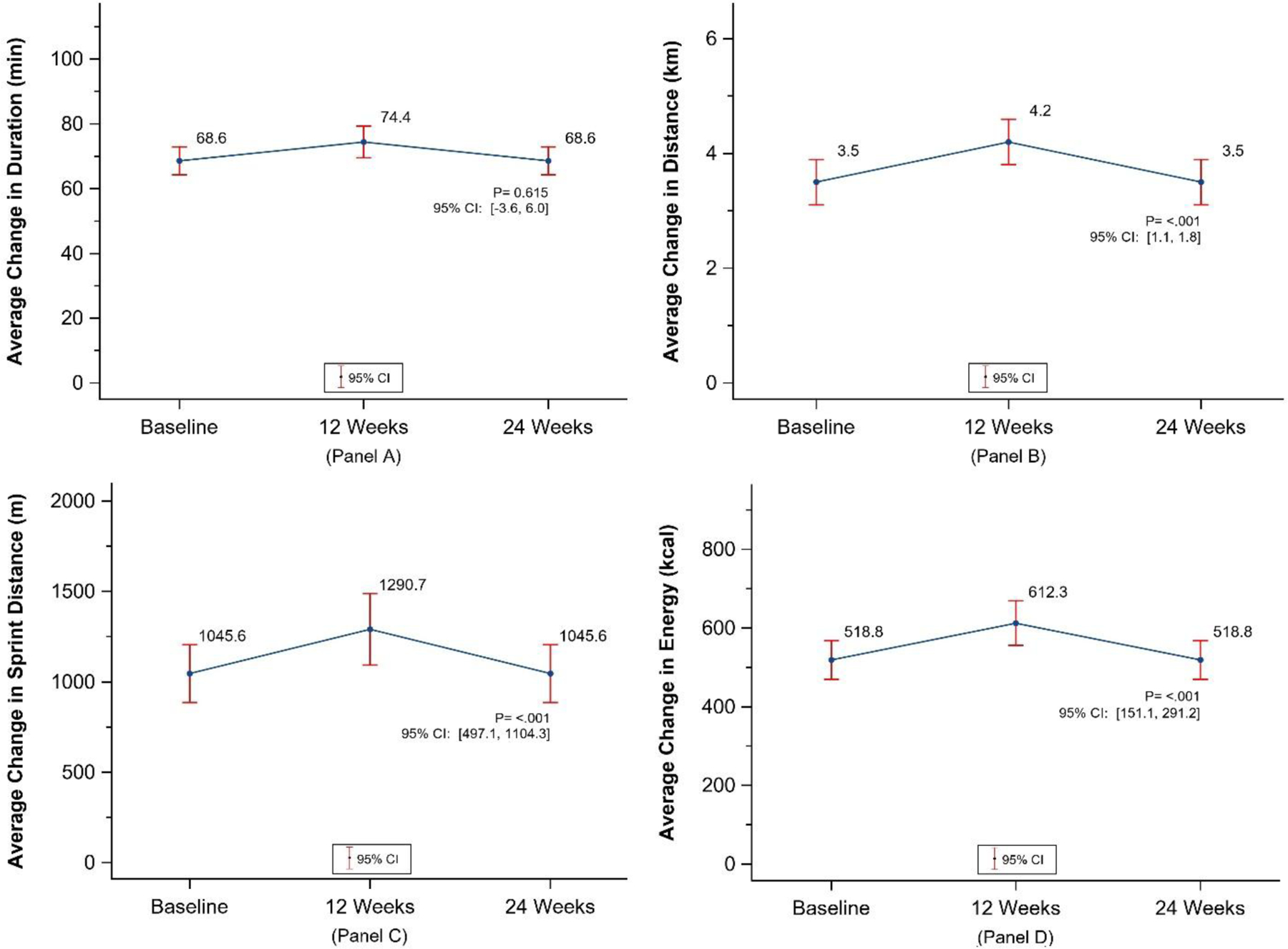
Soccer specific GPS metrics at baseline, 12 and 24 wk time points. Panel A – Average change in session duration in mins; Panel B – Average change in total distance during a session in kilometers; Panel C – Average change in sprint distance in meters; Panel D – Average change in energy expenditure in kilocalories during a session.
Figure 5.
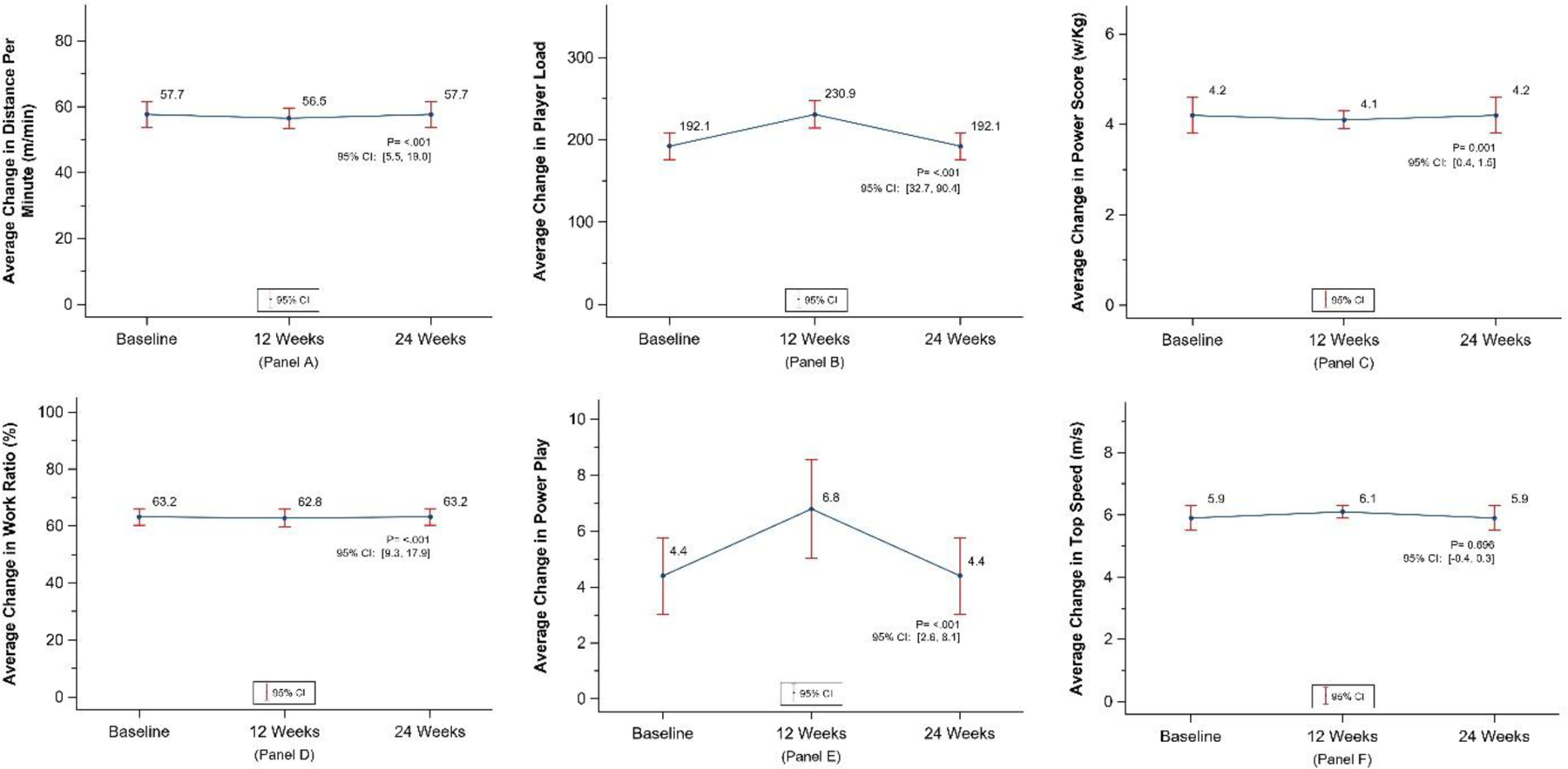
Soccer specific GPS metrics at baseline, 12 and 24 wk time points. Panel A – Average change in total distance per min; Panel B – Average change in player load; Panel C – Average change in power score in watts per kilogram; Panel D – Average change in work ratio as a percentage; Panel E – Average change in power play (count); Panel F – Average change in top speed in meters per second.
Mental Health outcomes
The Brief Resilience Scale was measured at baseline (mean 3.7 [SE 0.1]), at 12 wks (4.0[0.1]) and 24 wks (3.9 [0.1]). There was a significant increase in resilience in the first 12 wks (p=0.02; 95% CI 0.04, 0.51), but a non-significant change at 24 wks. The BREQ-2 did not show significant change over time; however, we were able to determine that most of the participants fell in either the introjected, identified, or intrinsic regulation which shows an increasing self-determination towards exercise. (Figure 6)
Figure 6.
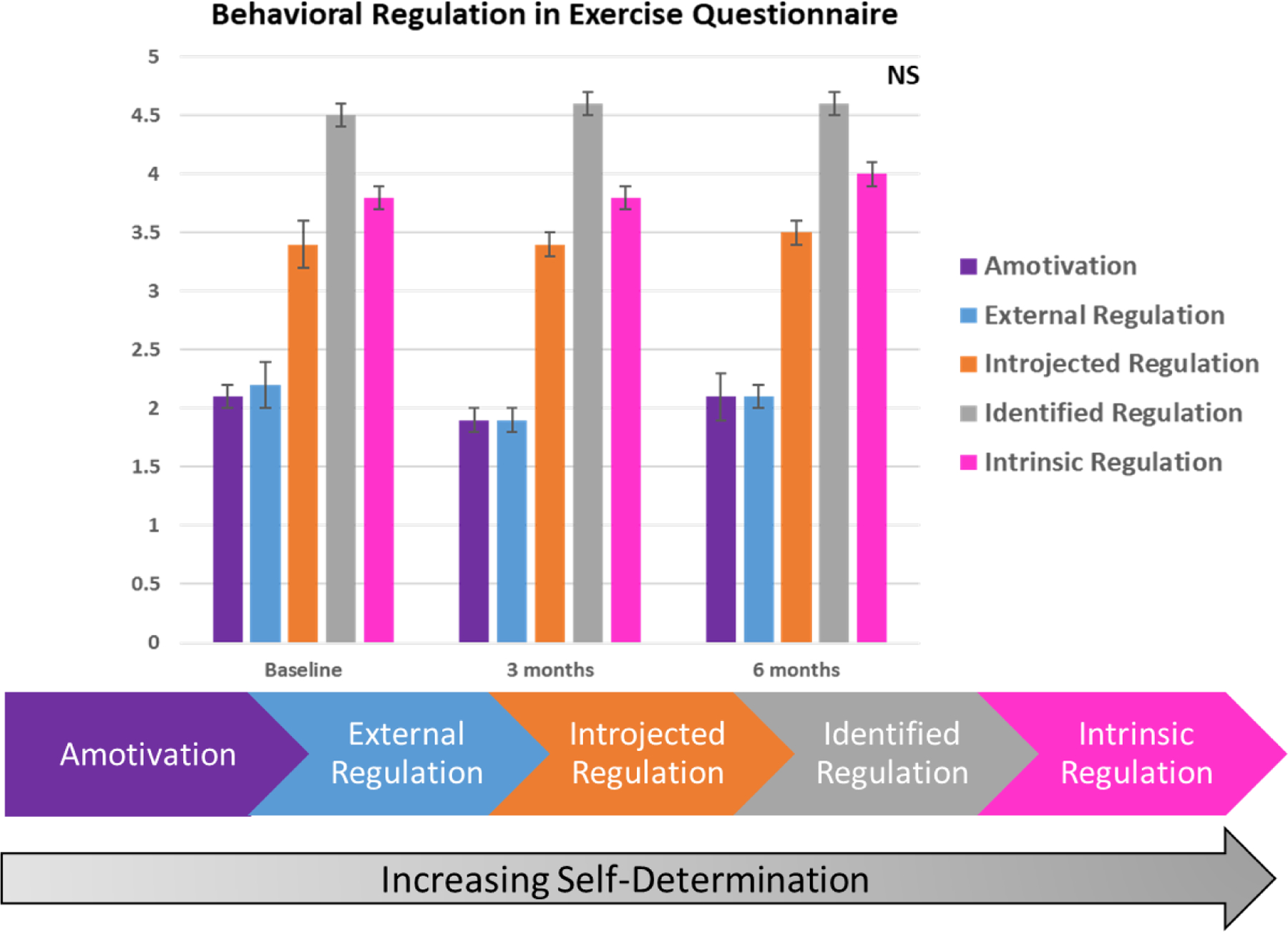
Results from the Behavior Regulation in Exercise Questionnaire at all time points showing the progression from amotivation to intrinsic regulation among Hispanic Men.
Finally, the average session perceived exertion decreased from 7 to 6 between baseline and 12 wks and to 4.7 after 24 wks. There were 16 mild injuries most being muscle strains and occurring within the first few wks of the program that resolved in 1–2 wks and no other adverse events reported. Reasons for missing sessions were reported as time management difficulties and travel for work/holidays.
Discussion
The main findings of this single arm, unblinded, clinical trial were that the program was well received and improved overall physical fitness and activity indicators in middle-aged Hispanic men living in Atlanta. This pilot feasibility study proved that the recruitment and retention is possible in understudied Hispanic men and this unique intervention approach may have potential for wider implementation as part of T2DM prevention programs.
The endurance levels of participants significantly improved from a baseline estimated VO2max of 38.9 ml/kg/min by 1.9% percent at 12 wks and then slightly decreased to a 1.0% improvement at 24 wks.28–30 Although this is a small change, it does highlight the gradual fitness improvements made by all participants. The decrease in average VO2max between 12 and 24 wks could be explained by the tapering of aerobic exercise from two soccer sessions per wk to one in order to match the structure of the DPP program. According to a systematic review of recreational soccer interventions, untrained men require on average 2.3 soccer sessions per wk to improve aerobic fitness levels.47 In contrast, our study did not meet that threshold, yet small improvements were still observed in aerobic fitness at the end of the program. This is important because even slight increases in aerobic fitness can lead to a reduction in clustered metabolic risk for at-risk individuals.48
Overall, the soccer NDPP study reported smaller percent increases in VO2max compared to other recreational soccer interventions.13 This result could be explained by the overall design of the soccer NDPP program, which provided a more comprehensive approach to diabetes prevention using both physical activity and classroom-based learning, instead of focusing solely on physical fitness, as other similar programs have done.47 Additionally, the length of individual soccer sessions was shorter for the soccer NDPP program (50 mins) compared to other recreational soccer interventions (60 mins).49 Furthermore, developing an exercise program for prediabetic, and sedentary individuals may have resulted in a low baseline level of aerobic fitness shown to be a common fitness characteristic of people with prediabetes.5 Finally, almost all recreational soccer research programs conducted with populations outside of the United states, specifically in Northern Europe and in Brazil.13,18,47,50 Therefore, the cultural differences between these regions of the world may lead to differing levels of aerobic fitness related to physical activity and sedentary lifestyle, including within different ethnic groups which comprise the U.S Latino/Hispanic community.51,52
Physical activity was objectively measured by use of a fitness tracker (Garmin vivofit 3). We saw a decrease in overall steps and MVPA after 12 wks. This may be due to many reasons. We did not introduce the fitness tracker until wk 3 to coincide with the first physical activity education session. This population was likely highly active to begin with due to many having a manual labor occupation. The interpretation of these first few wks is difficult and could be a mix of reactivity to the device and the program already beginning. Despite the decreasing trend, the overall activity levels (9,000 steps) were much higher than the average for Hispanic men and higher than in other NDPP programs that were measured objectively, which is infrequent.53 This decrease also implies that for these men more than one soccer session per week would be critical to attain PA goals. In addition, there was not an increase in sedentary time or change in sleep time, these remained stable.54,55
Various measures of muscle strength were measured and improved over the 24-wk intervention. Indirect measures of strength through exercise tests are uncommon in the recreational soccer literature. Our study opted for these field tests to decrease participant burden and provide a more pragmatic approach. However, other recreational soccer studies study muscle adaptation at the physiological level and muscle force through isometric measures. In a study of middle-aged untrained men, Krustrup et al. (2010) found increases in quadriceps muscle mass and hamstring strength after 12 wks of soccer versus running alone.56 Similarly, in a study of postmenopausal women, hamstring strength measured via isokinetic dynamometer improved after four months of soccer training in postmenopausal women compared to running training.57 Another study in men with prostate cancer saw a 1.7 cm improvement in jump height58 after a 32-wk intervention compared to standard care. Our study of younger healthier men saw a mean change of 5.5 cm at 12 wks and 2.8 at 24 wks. The NDPP does not focus on muscle strength, but more aerobic activities that meet the physical activity guidelines of 150 mins per wk. Further, it has been suggested to forgo the physical activity goal altogether to obtain better retention.9 Muscle strengthening exercises has been shown to improve diabetes prevention due to increased glucose disposal.59,60 Fløtum et.al. also conducted a single arm recreational soccer program in the Faroe Islands, a country of ~50,000 inhabitants.61 They saw a retention rate of 42% after 18 wks compared to our 65% retention rate at 24 wks. Despite slightly different measurement techniques, saw similar improvements to our study in agility and aerobic performance.61
Interestingly, most GPS-derived metrics related to soccer performance increased significantly with the intervention from baseline to follow-up. This indicates that the format and intensity of the intervention was adequate to induce locomotor, physiologic and neuromuscular changes necessary to not only improved physical fitness markers but also aerobic and anaerobic work capacity during soccer play.62,63 The use of GPS devices to monitor RS sessions in our study adds to the literature64 and to the experience from previous RS trials that used heart rate monitoring and reported improvements in fitness-related metrics such as resting and recovery heart rate.22,47,61 Furthermore, despite the relatively high intensity levels during the RS sessions in our intervention and the low baseline fitness levels of our participants, we saw a very limited number of mild musculoskeletal injuries and perceived session intensity actually declined over time. These findings are similar to those reported in previous RS trials and attributed to adequate implementation and delivery of an intervention plan guided by evidence-based resources.17,65
By the end of the 24-wk program, the participants reported a 59% increase in levels of resilience, or the process of adapting successfully in the face of adversity, trauma, or significant sources of stress. Additionally, group participants reported a slight increase in intrinsic motivation throughout the intervention, based on the BREQ-2 research instrument. Although these findings were not statistically significant, the positive increase in scores post vs. pre-program alludes to an overall shift from external, non-self-determined motivation to exercise (approval, status, appearance), to internal, self-determined motivation (strength, personal rewards).
This preliminary finding highlights the potential mental health benefits of the soccer NDPP program. The design of the program, which harnessed the power of group physical activity and social support, may have played a role in instilling resilience and increasing motivation in participants to overcome their sources of stress together. Overall, the link between recreational soccer and improved mental health has not been thoroughly studied, especially among older adult men. Eime et al. reported that women who participate in sports clubs and organized recreational activity compared to individual physical activity such as going to the gym or walking, receive more mental health benefits including higher life satisfaction.66 They and others67,68 have hypothesized that the social supportive structure of group physical activity promotes social connectedness, social support, and peer bonding, which in turn increases levels of overall physical activity and can improve mental health. Anecdotally, these aspects were observed throughout the soccer NDPP program. Program satisfaction surveys completed by participants at the end of the intervention emphasized the importance of the relationships they built with their fellow team members and coaches, and they expressed a strong interest to continue playing soccer with one another. During the course of the program, participants’ families often attended the NDPP sessions to provide social support and sometimes train alongside their father or husband. Future research should objectively explore how social and group physical activity seen in recreational soccer can improve the overall mental health of its players, with a specific focus on adult men. Future research should objectively explore how social and group physical activity seen in recreational soccer can improve the overall mental health of its players, with a specific focus on adult men.
Furthermore, only a handful of researchers have explored the relationship between physical activity and mental health in Latino populations.52,69,70 Currently, none have focused specifically on the impact of group recreational sports such as soccer with this racial group. Our study highlights the potential to fill that gap. Given the global enthusiasm for soccer, it makes sense to thoroughly identify the potential mental health benefits of soccer-based recreational sports programs.
There are some limitations to this study. The main limitation is the lack of control group. This study was designed as a feasibility trial to determine the likelihood of recruiting and retaining this hard to reach Hispanic population. Using a culturally tailored approach to reach this population enhanced this novel U.S. study. Furthermore, our longitudinal approach with objective exercise measurements (GPS and PA wearable) at multiple time points to measure change over time within each individual is also a strength. Secondly, while our target population was Hispanic men due to their increased risk of T2DM, this limits the generalizability of the effects of recreational soccer in other race and ethnicity groups. However, this is a high risk population that is understudied. Finally, our sample size for this pilot study was small, further studies should include larger randomized controlled trials to compare physical fitness and activity outcomes.
In conclusion, this feasibility study was able to recruit 41 Hispanic men for a 24-wk recreational soccer intervention to investigate various exercise outcomes. The participants showed improvement in most measures of physical fitness and activity over time and reported to enjoy the program overall. These results indicate a soccer-base adaptation of the NDPP may be a feasible approach to engage Latino men in lifestyle and physical activity changes. Future studies should include longer controlled trials to examine habitual changes in exercise and related health impacts.
Supplementary Material
Supplemental Figure 1 STROBE-compliant participant recruitment and enrollment flow chart for cohort studies.
Role of Funding Source:
Georgia Center for Translational Diabetes Research pilot award. The funder did not have any input on study design, data collection, analysis, or interpretation.
Abbreviations:
- PA
physical activity
- T2DM
type 2 diabetes
- NDPP
National Diabetes Prevention Program
- RS
recreational soccer
- HIIT
high intensity interval training
- BMI
body mass index
- SD
standard deviation
- Yo-Yo IR1
Yo-Yo Intermittent Recovery Test Level 1
- ALPHA
Assessing Levels of Physical Activity
- MVPA
moderate to vigorous physical activity
- BREQ-2
Brief Resilience Scale
- GPS
Global Positioning System
- FIFA
Fédération Internationale de Football Association
- Kg
kilogram
- SE
standard error
References
- 1.Hu G, Jousilahti P, Barengo NC, Qiao Q, Lakka TA, Tuomilehto J. Physical Activity, Cardiovascular Risk Factors, and Mortality Among Finnish Adults With Diabetes. Diabetes Care. 2005;28(4):799–805. doi: 10.2337/diacare.28.4.799 [DOI] [PubMed] [Google Scholar]
- 2.Lee I-M, Skerrett PJ. Physical activity and all-cause mortality: what is the dose-response relation? Med Sci Sports Exerc. 2001;33(6):S459. [DOI] [PubMed] [Google Scholar]
- 3.Snowling NJ, Hopkins WG. Effects of Different Modes of Exercise Training on Glucose Control and Risk Factors for Complications in Type 2 Diabetic Patients: A meta-analysis. Diabetes Care. 2006;29(11):2518–2527. doi: 10.2337/dc06-1317 [DOI] [PubMed] [Google Scholar]
- 4.Cowan TE, Brennan AM, Stotz PJ, Clarke J, Lamarche B, Ross R. Separate Effects of Exercise Amount and Intensity on Adipose Tissue and Skeletal Muscle Mass in Adults with Abdominal Obesity. Obes Silver Spring Md. 2018;26(11):1696–1703. doi: 10.1002/oby.22304 [DOI] [PubMed] [Google Scholar]
- 5.Rowan CP, Riddell MC, Gledhill N, Jamnik VK. Aerobic Exercise Training Modalities and Prediabetes Risk Reduction. Med Sci Sports Exerc. 2017;49(3):403–412. doi: 10.1249/MSS.0000000000001135 [DOI] [PubMed] [Google Scholar]
- 6.Yang P, Swardfager W, Fernandes D, et al. Finding the Optimal volume and intensity of Resistance Training Exercise for Type 2 Diabetes: The FORTE Study, a Randomized Trial. Diabetes Res Clin Pract. 2017;130:98–107. doi: 10.1016/j.diabres.2017.05.019 [DOI] [PubMed] [Google Scholar]
- 7.Diabetes Prevention Program Research Group. Reduction in the Incidence of Type 2 Diabetes with Lifestyle Intervention or Metformin. N Engl J Med. 2002;346(6):393–403. doi: 10.1056/NEJMoa012512 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hamman RF, Wing RR, Edelstein SL, et al. Effect of weight loss with lifestyle intervention on risk of diabetes. Diabetes Care. 2006;29:2102–2107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ritchie ND, Carroll JK, Holtrop JS, Havranek EP. Effects of physical activity goal attainment on engagement and outcomes in the National Diabetes Prevention Program. Transl Behav Med. 2018;8(6):932–937. doi: 10.1093/tbm/ibx021 [DOI] [PubMed] [Google Scholar]
- 10.Merriam PA, Tellez TL, Rosal MC, et al. Methodology of a diabetes prevention translational research project utilizing a community-academic partnership for implementation in an underserved Latino community. BMC Med Res Methodol. 2009;9:20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ruggiero L, Oros S, Choi YK. Community-based translation of the Diabetes Prevention Program’s lifestyle intervention in an underserved Latino population. Diabetes Educ. 2011;37(4):564–572. [DOI] [PubMed] [Google Scholar]
- 12.Elbe A-M, Strahler K, Krustrup P, Wikman J, Stelter R. Experiencing flow in different types of physical activity intervention programs: three randomized studies. Scand J Med Sci Sports. 2010;20 Suppl 1:111–117. doi: 10.1111/j.1600-0838.2010.01112.x [DOI] [PubMed] [Google Scholar]
- 13.Krustrup P, Nielsen JJ, Krustrup BR, et al. Recreational soccer is an effective health-promoting activity for untrained men. Br J Sports Med. 2009;43(11):825–831. doi: 10.1136/bjsm.2008.053124 [DOI] [PubMed] [Google Scholar]
- 14.Bruun DM, Bjerre E, Krustrup P, et al. Community-based recreational football: a novel approach to promote physical activity and quality of life in prostate cancer survivors. Int J Environ Res Public Health. 2014;11(6):5567–5585. doi: 10.3390/ijerph110605567 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nielsen G, Wikman JM, Jensen CJ, Schmidt JF, Gliemann L, Andersen TR. Health promotion: the impact of beliefs of health benefits, social relations and enjoyment on exercise continuation. Scand J Med Sci Sports. 2014;24 Suppl 1:66–75. doi: 10.1111/sms.12275 [DOI] [PubMed] [Google Scholar]
- 16.Ottesen L, Jeppesen RS, Krustrup BR. The development of social capital through football and running: studying an intervention program for inactive women. Scand J Med Sci Sports. 2010;20 Suppl 1:118–131. doi: 10.1111/j.1600-0838.2010.01123.x [DOI] [PubMed] [Google Scholar]
- 17.Bangsbo J, Junge A, Dvorak J, Krustrup P. Executive summary: Football for health - prevention and treatment of non-communicable diseases across the lifespan through football. Scand J Med Sci Sports. 2014;24 Suppl 1:147–150. doi: 10.1111/sms.12271 [DOI] [PubMed] [Google Scholar]
- 18.Krustrup P, Dvorak J, Junge A, Bangsbo J. Executive summary: the health and fitness benefits of regular participation in small-sided football games. Scand J Med Sci Sports. 2010;20 Suppl 1:132–135. doi: 10.1111/j.1600-0838.2010.01106.x [DOI] [PubMed] [Google Scholar]
- 19.Nybo L, Sundstrup E, Jakobsen MD, et al. High-intensity training versus traditional exercise interventions for promoting health. Med Sci Sports Exerc. 2010;42(10):1951–1958. doi: 10.1249/MSS.0b013e3181d99203 [DOI] [PubMed] [Google Scholar]
- 20.Oja P, Titze S, Kokko S, et al. Health benefits of different sport disciplines for adults: systematic review of observational and intervention studies with meta-analysis. Br J Sports Med. 2015;49(7):434–440. doi: 10.1136/bjsports-2014-093885 [DOI] [PubMed] [Google Scholar]
- 21.Bellissimo MP, Arrendono KG, Paskert M, Lobelo F. A systematic review and meta-analysis of the reduction in cardiovascular disease through group sport inteventions in adults. Mayo Clin Proc. 2018;In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Milanović Z, Pantelić S, Čović N, Sporiš G, Mohr M, Krustrup P. Broad-spectrum physical fitness benefits of recreational football: a systematic review and meta-analysis. Br J Sports Med. 2019;53(15):926–939. doi: 10.1136/bjsports-2017-097885 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Riebe D, Franklin BA, Thompson PD, et al. Updating ACSM’s Recommendations for Exercise Preparticipation Health Screening. Med Sci Sports Exerc. 2015;47(11):2473–2479. doi: 10.1249/mss.0000000000000664 [DOI] [PubMed] [Google Scholar]
- 24.Soccer-based Adaptation of the Diabetes Prevention Program - Full Text View - ClinicalTrials.gov. Accessed March 6, 2020. https://clinicaltrials.gov/ct2/show/NCT03595384
- 25.Franklin Barry A., Thompson Paul D., Al-Zaiti Salah S., et al. Exercise-Related Acute Cardiovascular Events and Potential Deleterious Adaptations Following Long-Term Exercise Training: Placing the Risks Into Perspective–An Update: A Scientific Statement From the American Heart Association. Circulation. 2020;141(13):e705–e736. doi: 10.1161/CIR.0000000000000749 [DOI] [PubMed] [Google Scholar]
- 26.Centers for Disease Control and Prevention, National Diabetes Prevention Program. CDC Prediabetes Screening Test.; 2016.
- 27.Professional Practice Committee: Standards of Medical Care in Diabetes—2018. Diabetes Care. 2018;41(Supplement 1):S3–S3. doi: 10.2337/dc18-Sppc01 [DOI] [PubMed] [Google Scholar]
- 28.Krustrup P, Mohr M, Amstrup T, et al. The yo-yo intermittent recovery test: physiological response, reliability, and validity. Med Sci Sports Exerc. 2003;35(4):697–705. doi: 10.1249/01.MSS.0000058441.94520.32 [DOI] [PubMed] [Google Scholar]
- 29.Bangsbo J, Iaia FM, Krustrup P. The Yo-Yo intermittent recovery test : a useful tool for evaluation of physical performance in intermittent sports. Sports Med Auckl NZ. 2008;38(1):37–51. doi: 10.2165/00007256-200838010-00004 [DOI] [PubMed] [Google Scholar]
- 30.Póvoas S, Krustrup P, Castagna C. Submaximal field testing validity for aerobic fitness assessment in recreational football. Scand J Med Sci Sports. 2020;30(4):680–689. doi: 10.1111/sms.13606 [DOI] [PubMed] [Google Scholar]
- 31.Tveter AT, Dagfinrud H, Moseng T, Holm I. Measuring health-related physical fitness in physiotherapy practice: reliability, validity, and feasibility of clinical field tests and a patient-reported measure. J Orthop Sports Phys Ther. 2014;44(3):206–216. doi: 10.2519/jospt.2014.5042 [DOI] [PubMed] [Google Scholar]
- 32.Gerodimos V. Reliability of handgrip strength test in basketball players. J Hum Kinet. 2012;31:25–36. doi: 10.2478/v10078-012-0003-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Manor J, Bunn J, Bohannon RW. Validity and Reliability of Jump Height Measurements Obtained From Nonathletic Populations With the VERT Device. J Geriatr Phys Ther 2001. 2020;43(1):20–23. doi: 10.1519/JPT.0000000000000205 [DOI] [PubMed] [Google Scholar]
- 34.Ruiz JR, Espana Romero V, Castro Pinero J, et al. [ALPHA-fitness test battery: health-related field-based fitness tests assessment in children and adolescents]. Nutr Hosp. 2011;26(6):1210–1214. doi: 10.1590/s0212-16112011000600003 [DOI] [PubMed] [Google Scholar]
- 35.Suni JH, Rinne MB, Ruiz JR. Retest Repeatability of Motor and Musculoskeletal Fitness Tests for Public Health Monitoring of Adult Populations. J Nov Physiother. 2014;4(1):1–6. doi: 10.4172/2165-7025.1000194 [DOI] [Google Scholar]
- 36.Centers for Disease Control and Prevention. National Health and Nutrition Examination Survey (NHANES) Anthropometry Procedures Manual.
- 37.Muscle Strength Procedures Manual 2011. :55.
- 38.Price K, Bird SR, Lythgo N, Raj IS, Wong JYL, Lynch C. Validation of the Fitbit One, Garmin Vivofit and Jawbone UP activity tracker in estimation of energy expenditure during treadmill walking and running. J Med Eng Technol. 2017;41(3):208–215. doi: 10.1080/03091902.2016.1253795 [DOI] [PubMed] [Google Scholar]
- 39.Šimůnek A, Dygrýn J, Jakubec L, Neuls F, Frömel K, Welk GJ. Validity of Garmin Vívofit 1 and Garmin Vívofit 3 for School-Based Physical Activity Monitoring. Pediatr Exerc Sci. 2019;31(1):130–136. doi: 10.1123/pes.2018-0019 [DOI] [PubMed] [Google Scholar]
- 40.Smith BW, Dalen J, Wiggins K, Tooley E, Christopher P, Bernard J. The brief resilience scale: assessing the ability to bounce back. Int J Behav Med. 2008;15(3):194–200. doi: 10.1080/10705500802222972 [DOI] [PubMed] [Google Scholar]
- 41.Markland D, Tobin V. A Modification to the Behavioural Regulation in Exercise Questionnaire to Include an Assessment of Amotivation. J Sport Exerc Psychol. 2004;26(2):191–196. doi: 10.1123/jsep.26.2.191 [DOI] [Google Scholar]
- 42.PLAYERTEK | Affordable Athlete Tracking System | Catapult Sports. Catapult. Accessed May 30, 2020. https://www.catapultsports.com/products/playertek
- 43.Krustrup P, Williams CA, Mohr M, et al. The “Football is Medicine” platform-scientific evidence, large-scale implementation of evidence-based concepts and future perspectives. Scand J Med Sci Sports. 2018;28 Suppl 1:3–7. doi: 10.1111/sms.13220 [DOI] [PubMed] [Google Scholar]
- 44.Curricula and Handouts | NDPP | Diabetes | CDC. Published October 24, 2019. Accessed March 6, 2020. https://www.cdc.gov/diabetes/prevention/resources/curriculum.html
- 45.Federation Internationale de Football Association. FIFA Diploma in Football Medicine.
- 46.Whaley MH, Woodall T, Kaminsky LA, Emmett JD. Reliability of perceived exertion during graded exercise testing in apparently healthy adults. J Cardpulm Rehabil. 1997;17(1):37–42. doi: 10.1097/00008483-199701000-00005 [DOI] [PubMed] [Google Scholar]
- 47.Milanović Z, Pantelić S, Čović N, Sporiš G, Krustrup P. Is Recreational Soccer Effective for Improving VO2max A Systematic Review and Meta-Analysis. Sports Med Auckl NZ. 2015;45(9):1339–1353. doi: 10.1007/s40279-015-0361-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Simmons RK, Griffin SJ, Steele R, Wareham NJ, Ekelund U, ProActive Research Team. Increasing overall physical activity and aerobic fitness is associated with improvements in metabolic risk: cohort analysis of the ProActive trial. Diabetologia. 2008;51(5):787–794. doi: 10.1007/s00125-008-0949-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Randers MB, Nielsen JJ, Krustrup BR, et al. Positive performance and health effects of a football training program over 12 weeks can be maintained over a 1-year period with reduced training frequency. Scand J Med Sci Sports. 2010;20 Suppl 1:80–89. doi: 10.1111/j.1600-0838.2010.01091.x [DOI] [PubMed] [Google Scholar]
- 50.de Sousa MV, Fukui R, Krustrup P, et al. Positive effects of football on fitness, lipid profile, and insulin resistance in Brazilian patients with type 2 diabetes. Scand J Med Sci Sports. 2014;24 Suppl 1:57–65. doi: 10.1111/sms.12258 [DOI] [PubMed] [Google Scholar]
- 51.Hubert HB, Snider J, Winkleby MA. Health status, health behaviors, and acculturation factors associated with overweight and obesity in Latinos from a community and agricultural labor camp survey. Prev Med. 2005;40(6):642–651. doi: 10.1016/j.ypmed.2004.09.001 [DOI] [PubMed] [Google Scholar]
- 52.Rethorst CD, Moncrieft AE, Gellman MD, et al. Isotemporal Analysis of the Association of Objectively Measured Physical Activity With Depressive Symptoms: Results From Hispanic Community Health Study/Study of Latinos (HCHS/SOL). J Phys Act Health. 2017;14(9):733–739. doi: 10.1123/jpah.2016-0648 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Sohn EK, Porch T, Hill S, Thorpe RJ. Geography, Race/Ethnicity, and Physical Activity Among Men in the United States. Am J Mens Health. 2017;11(4):1019–1027. doi: 10.1177/1557988316689498 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Lynch BM, Nguyen NH, Moore MM, et al. Maintenance of physical activity and sedentary behavior change, and physical activity and sedentary behavior change after an abridged intervention: Secondary outcomes from the ACTIVATE Trial. Cancer. 2019;125(16):2856–2860. doi: 10.1002/cncr.32142 [DOI] [PubMed] [Google Scholar]
- 55.Kozey-Keadle S, Staudenmayer J, Libertine A, et al. Changes in sedentary time and physical activity in response to an exercise training and/or lifestyle intervention. J Phys Act Health. 2014;11(7):1324–1333. [DOI] [PubMed] [Google Scholar]
- 56.Krustrup P, Christensen JF, Randers MB, et al. Muscle adaptations and performance enhancements of soccer training for untrained men. Eur J Appl Physiol. 2010;108(6):1247–1258. doi: 10.1007/s00421-009-1319-8 [DOI] [PubMed] [Google Scholar]
- 57.Krustrup P, Hansen PR, Andersen LJ, et al. Long-term musculoskeletal and cardiac health effects of recreational football and running for premenopausal women. Scand J Med Sci Sports. 2010;20 Suppl 1:58–71. doi: 10.1111/j.1600-0838.2010.01111.x [DOI] [PubMed] [Google Scholar]
- 58.Uth J, Hornstrup T, Christensen JF, et al. Efficacy of recreational football on bone health, body composition, and physical functioning in men with prostate cancer undergoing androgen deprivation therapy: 32-week follow-up of the FC prostate randomised controlled trial. Osteoporos Int. 2016;27(4):1507–1518. doi: 10.1007/s00198-015-3399-0 [DOI] [PubMed] [Google Scholar]
- 59.Yeung CHC, Au Yeung SL, Fong SSM, Schooling CM. Lean mass, grip strength and risk of type 2 diabetes: a bi-directional Mendelian randomisation study. Diabetologia. 2019;62(5):789–799. doi: 10.1007/s00125-019-4826-0 [DOI] [PubMed] [Google Scholar]
- 60.Tarp J, Støle AP, Blond K, Grøntved A. Cardiorespiratory fitness, muscular strength and risk of type 2 diabetes: a systematic review and meta-analysis. Diabetologia. 2019;62(7):1129–1142. doi: 10.1007/s00125-019-4867-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Fløtum LA, Ottesen LS, Krustrup P, Mohr M. Evaluating a Nationwide Recreational Football Intervention: Recruitment, Attendance, Adherence, Exercise Intensity, and Health Effects. BioMed Res Int. 2016;2016:7231545. doi: 10.1155/2016/7231545 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Bangsbo J. The physiology of soccer--with special reference to intense intermittent exercise. Acta Physiol Scand Suppl. 1994;619:1–155. [PubMed] [Google Scholar]
- 63.Zouhal H, Hammami A, Tijani JM, et al. Effects of Small-Sided Soccer Games on Physical Fitness, Physiological Responses, and Health Indices in Untrained Individuals and Clinical Populations: A Systematic Review. Sports Med Auckl NZ. 2020;50(5):987–1007. doi: 10.1007/s40279-019-01256-w [DOI] [PubMed] [Google Scholar]
- 64.Pantelić S, Rađa A, Erceg M, et al. Relative pitch area plays an important role in movement pattern and intensity in recreational male football. Biol Sport. 2019;36(2):119–124. doi: 10.5114/biolsport.2019.81113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Thorborg K, Krommes KK, Esteve E, Clausen MB, Bartels EM, Rathleff MS. Effect of specific exercise-based football injury prevention programmes on the overall injury rate in football: a systematic review and meta-analysis of the FIFA 11 and 11+ programmes. Br J Sports Med. 2017;51(7):562–571. doi: 10.1136/bjsports-2016-097066 [DOI] [PubMed] [Google Scholar]
- 66.Eime RM, Harvey JT, Brown WJ, Payne WR. Does sports club participation contribute to health-related quality of life? Med Sci Sports Exerc. 2010;42(5):1022–1028. doi: 10.1249/MSS.0b013e3181c3adaa [DOI] [PubMed] [Google Scholar]
- 67.Street G, James R, Cutt H. The relationship between organised physical recreation and mental health. Health Promot J Aust Off J Aust Assoc Health Promot Prof. 2007;18(3):236–239. doi: 10.1071/he07236 [DOI] [PubMed] [Google Scholar]
- 68.Giles-Corti B, Donovan RJ. The relative influence of individual, social and physical environment determinants of physical activity. Soc Sci Med 1982. 2002;54(12):1793–1812. doi: 10.1016/s0277-9536(01)00150-2 [DOI] [PubMed] [Google Scholar]
- 69.Bustamante EE, Wilbur J, Marquez DX, Fogg L, Staffileno BA, Manning A. Physical activity characteristics and depressive symptoms in older Latino adults. Ment Health Phys Act. 2013;6(2):69–77. doi: 10.1016/j.mhpa.2013.05.001 [DOI] [Google Scholar]
- 70.Marquez DX, McAuley E. Social cognitive correlates of leisure time physical activity among Latinos. J Behav Med. 2006;29(3):281–289. doi: 10.1007/s10865-006-9055-6 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Figure 1 STROBE-compliant participant recruitment and enrollment flow chart for cohort studies.


