Abstract
Objective:
To assess short-term alterations in the volume of pharyngeal airway space and maxillary sinuses associated with rapid maxillary expansion (RME) and facemask (FM) use in growing Class III maxillary-deficient patients.
Materials and Methods:
Twenty-two patients (14 girls, eight boys) treated with the RME/FM and having pretreatment and posttreatment cone beam–computed tomographic scans were identified from the archives of the Marmara University, Department of Orthodontics. According to the protraction force that was used, they were divided into two groups: a group with 400 g protraction force (12 subjects) and a group with 800 g protraction force (10 subjects). Mean age for the study group was 10 years. All patients were diagnosed with normal/low vertical growth pattern, maxillary deficiency, and normal mandible. No control group was available for this study. For each patient, a hyrax expansion screw with acrylic cap splint was constructed and RME was performed for 10 days. On the seventh day, protraction with a FM started.
Results:
The results showed a statistically significant increase in the volume of maxillary sinuses after treatment, which was related to the growth. On the other hand, the increase in the volume of pharyngeal airway was not statistically significant.
Conclusions:
RME/FM treatment did not affect at all the volume of maxillary sinuses and actually inhibited the normal expected increase of the volume of the pharynx when compared with a control group comprising normal individuals.
Keywords: 3D, Pharyngeal airway space, Maxillary sinuses, Facemask, Rapid palatal expansion
INTRODUCTION
Numerous studies demonstrate that rapid maxillary expansion/facemask (RME/FM) use in growing patients causes remarkable dental, skeletal, and soft tissue changes.1 As a result of these changes in hard and soft tissues, it has been suggested that RME/FM treatment in growing Class III patients may alter the volume of the pharyngeal airway (PA) and maxillary sinuses. The effect of maxillary protraction associated with the use of RME/FM on the dimensions of human PA is a very controversial issue. Few studies have been published, and all of them are based on two-dimensional (2D) evaluations of pharyngeal airway space by the use of conventional cephalograms. The purpose of this study was to evaluate the PA and maxillary sinus volume changes in Class III growing patients undergoing RME/FM treatment using cone beam–computed tomography (CBCT) and to contribute to the literature on an issue that has not been evaluated before in three dimensions (3D).
MATERIALS AND METHODS
The records of 22 patients (eight males and 14 females) treated with RME/FM and with pretreatment and posttreatment CBCTs were selected from the archive of Marmara University, Department of Orthodontics, İstanbul, Turkey. The mean ages of the male and female patients were 10.3 and 9.9 years, respectively. Mean age for the study group was 10 years. The skeletal maturation age was assessed using the vertebral maturation method.2 All of the patients were in the active growth period. The study was approved by the ethical committee of the Medical Faculty of Marmara University (İstanbul, Turkey).
Inclusion criteria were as follows: patients with Class III skeletal relationship due to maxillary retrognathism; age between 8 and 11 years; no previous orthodontic/orthopedic treatment; no systemic diseases, craniofacial anomalies, or temporomandibular joint disorders; no tonsillectomy/adenoidectomy; and no carious, gingival/periodontal lesions.
The patients were divided in two groups according to the amount of protraction force applied. In the first group of five males and seven females approximately 400 g of elastic force was applied for each side. In the second group of three males and seven females approximately 800 g of elastic force was used for each side.
The expansion device used was an acrylic cap splint Hyrax (GH Wire Company, Hanover, Germany). The expansion screw was activated twice a day for a period of 10 days. Patients were treated with maxillary protraction for an average period of 10 months. Maxillary protraction was performed using a FM on the seventh day of RME. The FM treatment was terminated and the Hyrax appliance was removed when an overjet of 5 mm and full Class II molar and canine relationship were achieved. All patients received a Class III bionator for retention. Upon completion of the desired permanent dentition, fixed orthodontic appliances were bonded.
CBCTs were taken at two periods. The pretreatment CBCT was taken 1 week before the bonding of the Hyrax appliance (T0), and the posttreatment scans were obtained 1 week after the removal of the Hyrax appliance (T1). CBCT (3M, St Paul, Minn) scans were made at 20 kV and 1–4 mA using the following protocol: 21.1-cm field of view, 0.0936 Voxel size, 58 microsieverts of maximum radiation, and 40-second maximum and 7.8-second minimum scanning times. All of the scans were acquired with the patient sitting upright with the Frankfort horizontal plane parallel to the floor, in centric occlusion. The patient's head position was adjusted with the help of two laser beams, one parallel to the floor, coinciding with the Frankfort horizontal plane, and one vertical beam passing through the patient's facial midline. The patients were asked not to swallow or move their heads or tongues during exposure.
The data obtained from the images were transferred to a computer, where volumetric changes of the PA and maxillary sinuses and several skeletal changes were measured using MIMICS 14.0 software launched by Materialise (Materialise Europe, World Headquarters, Leuven, Belgium). All measurements were done by the same operator. In order to determine the method error, 10 randomly selected CBCTs were retraced on the same computer by the same operator. Before landmark identification, the 3D volumetric images were oriented with the MIMICS 14.0 program. The midsagittal plane was adjusted on the skeletal midline, and the axial plane was adjusted to show the Frankfort horizontal plane. From each CBCT a 2D cephalogram was extracted. On those cephalograms SN-CVT angle (CVT: the line connecting the most posterosuperior point on the odontoid process of the axis with the most posteroinferior point on the body of the fourth cervical vertebra) was measured, and no statistically significant change was found.
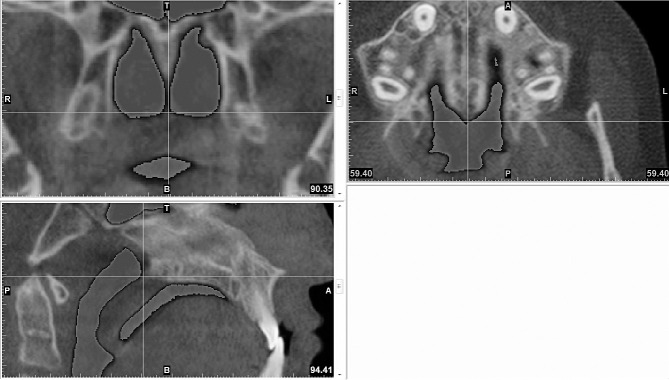
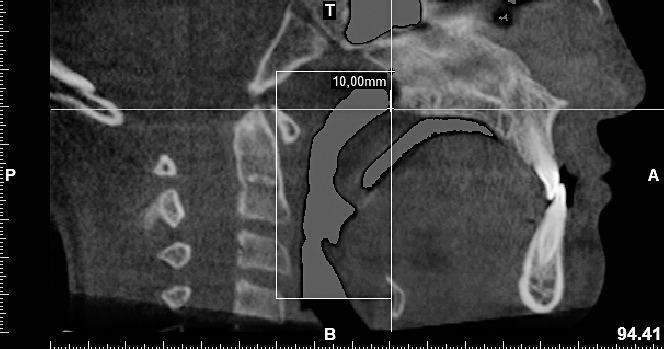
The PA volume was calculated according to the following borders. The anterior border was defined by a vertical plane passing through PNS. The superior border was a parallel line to the Frankfort horizontal plane passing 10 mm superior to the PNS. The posterior border was the posterior pharyngeal wall. The inferior border was a horizontal plane (parallel to Frankfort horizontal) passing from the most anterior and inferior point of the third vertebra (Figures 1 and 2). The 3D image of the PA was divided into upper and lower parts by a plane drawn from PNS to the most anterior and inferior point of the first vertebrae. All landmarks were identified in the axial, coronal, and sagittal views (Figure 3). When polyps were observed during assessment of the volume of maxillary sinuses volume, these polyps were included in the mask of the isolated sinuses since they were occupying space that should be normally occupied by air (Figure 4).
Figure 1.
Boarders of measured PA.
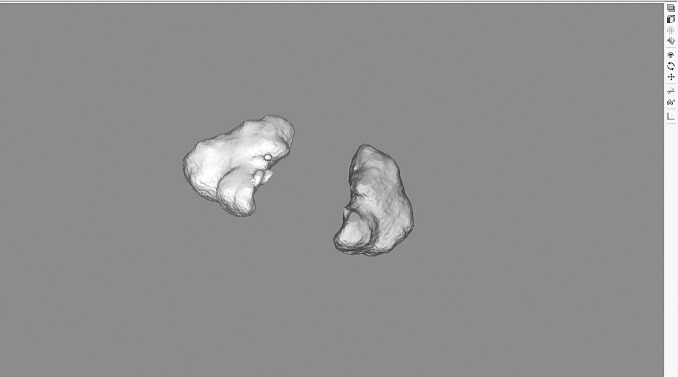
Figure 2.
3D reconstruction of PA.
Figure 3.
Identification of PNS point in axial, coronal, and sagittal views.
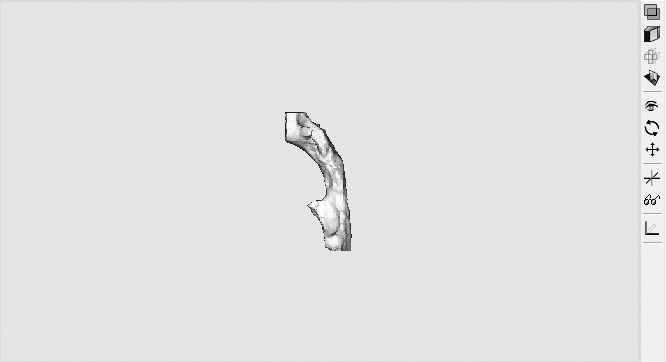
Figure 4.
Isolation of right maxillary sinus.
For the assessment of before and after treatment skeletal changes, 3D images were superimposed on the cranial base. Then, on the pretreatment 3D image, two planes were created: a sagittal plane (RP1) and a coronal plane (RP2). RP1 was created by the identification of the two Porion points and right Orbitale point, and RP2 was created vertical to RP1 passing from right and left Porion points. Then ANS, PNS, and A and B points were identified on both 3D models', coronal, axial and sagittal slices. Vertical distances of ANS and PNS points from RP1 and of A and B points from RP2 were calculated automatically by the program. Classical cephalometric images were extracted from CBCTs, and measurements of GoMe-SN, PP-SN, and OP-SN angles were performed.
Statistical Analysis
The SPSS for Windows 15.0 program was used for statistical assessment. Conformity of the parameters to the normal distribution was assessed by the Kolmogorov-Smirnov test. The Kruskal-Wallis test was used for intergroup comparisons of parameters without normal distribution, and the Mann-Whitney U-test was used for the determination of the group causing the difference. A Student's t-test was used for the intergroup comparisons of parameters with normal distribution, and the Mann-Whitney U-test was used for the intergroup comparisons of parameters without normal distribution. The paired-samples t-test was used for the in-group comparisons of parameters with normal distribution. Spearman's rho correlation analysis was used for investigation of relationships between parameters not showing conformity to the normal distribution. Significance was evaluated at a level of P < .05.
RESULTS
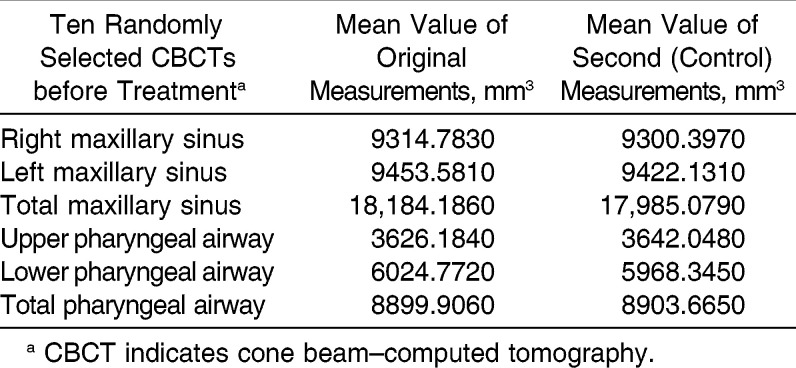
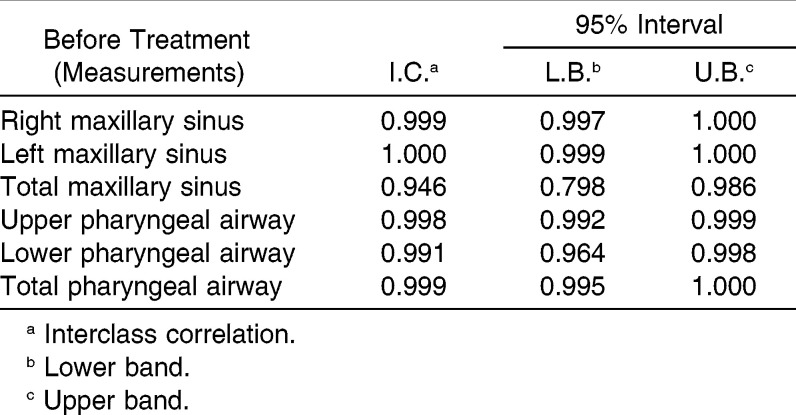
Our results demonstrated a high level of agreement between the duplicate measurements conducted by the same examiner. The interclass correlation coefficient of all the measurements showed a high rate of consonance (Tables 1 and 2).
Table 1.
Evaluation of the Reliability of the Method
Table 2.
Evaluation of the Reliability of the Method
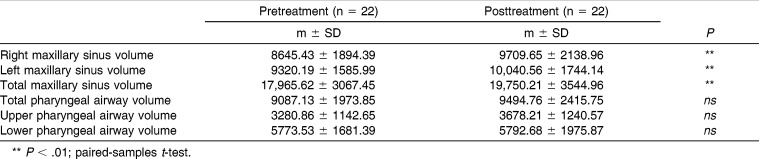
The results indicate that there is a significant increase, by a mean of 1064.22 mm3, in the right sinus volume and a significant increase, by a mean of 720.37 mm3, in the left sinus volume. Total maxillary sinus volume was also significantly increased. There was no significant difference in the amount of increase of sinus volume between the two force groups (Table 3).
Table 3.
Evaluation of the Results of the Treatment on Air Volumes of Pharyngeal Airway and Maxillary Sinuses
There was an insignificant increase (by 397.95 mm3) of the volume of upper airway, an insignificant increase of 19.15 mm3 of the volume of lower airway, and an insignificant increase of 407.63 mm3 of total PA volume (Table 3).
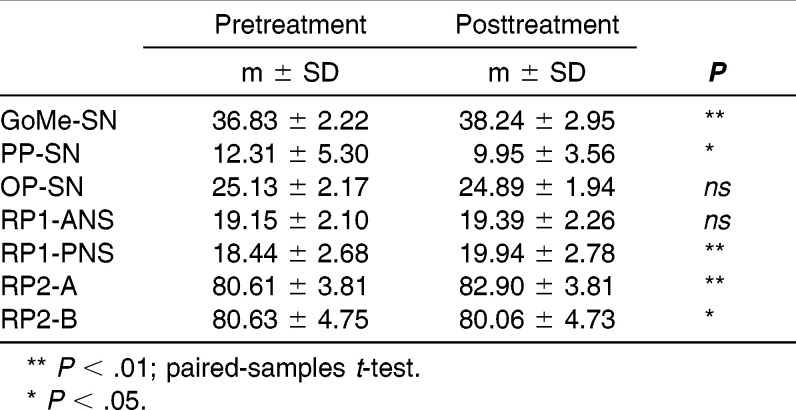
There was a significant anterior movement of A point by a mean of 2.29 mm, a posterior movement of B point by a mean of 0.57 mm, and a downward movement of PNS point by a mean of 1.5 mm. GoMe-SN angle statistically increased by a mean of 1.41°, and PP-SN decreased by a mean of 2.76° (Table 4).
Table 4.
Evaluation of the Results of the Treatment on Skeletal Structures
DISCUSSION
At present, the US Nuclear Regulatory Commission (USNRC) has limited the radiation exposure of the public to 1 mSv (1000 µSv) per year. With our CBCT the maximum radiation per scan was 0.058 mSv (58 µSv). The CBCTs were taken from each patient twice in a period of 10 months, which results in 0.112 mSv of radiation, representing 11% of the allowed dosage per year, well below the USNRC safety limit (USNRC Biological Effects of Radiation 2004). However, it is clear that no amount of radiation can be regarded as a “safe,” and it is the practitioner's ethical obligation to limit unnecessary radiation exposure.
Our results showed an insignificant increase (407.63 mm3) in the volume of upper and lower airway. For ethical reasons there was no control group of Class III samples available in this study. However, the 3D growth studies of Schendel and Jacobson3 and Li et al.4 provided detailed data concerning the normal growth of PA between the ages of 8 and 12. According to Schendel and Jacobson,3 the normal expected growth of PA in a period of 10 months in growing patients between 10 and 13 years of age is 897.2 mm3, while according to Li et al.4 the expected increase in the volume of the PA due to growth procedures between the ages of 7.5 and 11 years of age is 974.704 mm3. However, the soft palate, which is attached to the maxilla, can be affected by positional changes in the maxilla and its physical contact with the tongue.5 While providing a strong indication that the amount of increase in the airway volume that we have found is less than the amount of expected growth, these studies have a significant limitation. They all were made on normal growing individuals, and it is much more likely that the group being treated had already experienced deficient maxillary growth,6,7 which would be expected to have an impact of lesser airway development (compared to what one would expect to see in untreated normal growing controls).
The only studies available in the literature examining the effect of RME/FM or FM treatment alone on the PA volume are done by evaluation of 2D cephalograms. Lee et al.,5 Sayınsu et al.,8 and Kaygısız et al.9 demonstrated improvement in the nasopharyngeal airway dimensions with maxillary protraction in skeletal Class III children. Oktay and Ulukaya10 observed significant increases in the width of the PA. These authors assumed that there were no increases in PA volume due to the growth, and they did not use a control group. The studies that did include a control group demonstrated that RME/FM treatment improved naso- and oropharyngeal airway dimensions in the short term.11–13 Mucedero et al.12 concluded that the favorable skeletal maxillary and mandibular changes produced by FM with or without RME were not associated with significant changes in the sagittal oropharyngeal and nasopharyngeal airway dimensions. The interesting finding of Mucedero et al.12 was the relatively high standard deviations of their cephalometric findings. More specifically, in one-third of their cases, the result of the FM treatment was actually a decrease in the volume of PA. Baccetti et al.13 found no significant changes for the oro- and nasopharyngeal sagittal airway dimensions induced by FM/Bite Block therapy when compared with untreated Class III subjects.
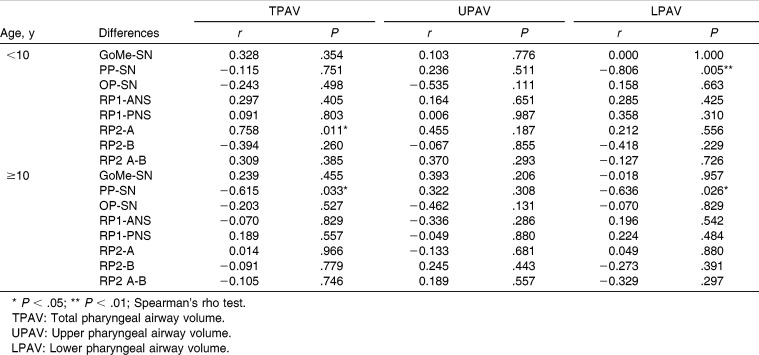
In our research extended correlation statistics were performed to examine the relationship between the changes of the airway volumes/skeletal points and different parameters, such as age, gender, daily FM use, and duration of treatment (Table 5). The most important correlation was a significant positive correlation between PP-SN angle and total and lower PA volume. That means that a decrease in the PP-SN angle is followed by a decrease in the lower airway and total PA volume. This weak correlation may support our hypothesis that the PNS's drop causes spontaneous drop of soft palate and, as a result, constriction of the volume of lower airway.
Table 5.
Correlation of Pharyngeal Airway Changes with Skeletal Changes in Two Different Age Groups
We also found a significant increase in the volume of maxillary sinus as a result of RME/FM treatment of a mean of 8932.295 mm3 (Table 3). As a result of the absence of a control group, we used the data provided by 3D growth studies of Barqhouth et al.14 and Park et al.15 These 3D studies provided detailed data concerning the normal growth of maxillary sinuses between the ages of 8 and 12 years. According to the results of Barqhouth et al.,14 the maxillary sinus volume increased by a mean of 4000 mm3, which means 1000 mm3 for 1 year or 833 mm3 for a period of 10 months, while according to Park et al.,15 between the ages of 8 and 12 years there was a mean increase of 949.3 mm3 for the same time period. Despite the fact that these studies have certain limitations compared to our study, such as the patient criteria selection (our study includes only Class III maxillary-deficient low to normal angle patients), ethnicity of patients (Park et al.15 had Asian ancestry patients), and different 3D measurement technology (Barqhouth used magnetic resonance imaging and not CBCTs), they provide an indication that the increase in the volume of the maxillary sinuses of our patients occurred because of growth procedures and not because of RME/FM treatment. Again, for safer results a special control group of Class III maxillary-deficient patients is required.
There is no available literature examining the effect of RME/FM treatment on the volume of maxillary sinuses. Nevertheless, there are three available 3D studies that examine the effects of RME with Hyrax appliances on maxillary sinuses. Garrett et al.16 found that RME produces a statistically significant decrease in maxillary sinus width without using a control group, but they did not measure actual volume. Smith et al.17 agreed with our results and found no statistically significant change in the sinus volumes as a result of RME. They did not take the growth factor into consideration. Motro18 concluded that there was a significant increase in the total sinus volume after RME treatment. As a control group, he used the growth study of Barqhouth et al.14 In Motro's18 study, the mean age and the standard deviation were much higher than in this study, which may justify his results, since in nongrowing patients we cannot expect much increase in the volume of maxillary sinuses due to growth.
Limitations of this study were the small sample size and the absence of a control group. In order to accommodate for the absence of a control group we used detailed data of available 3D growth studies of normal growing samples. When the amount of radiation in a CBCT scan is reduced enough to allow us to use it on an everyday basis, a formation of an adequate Class III control group will help us reach safer results.
CONCLUSIONS
As a result of RME/FM treatment, there was a significant increase in the maxillary sinus volume, while the increases in the volumes of upper and lower PA were insignificant.
RME/FM treatment did not affect at all the volume of maxillary sinuses and actually decreased the normal expected increase of the volume of PA when compared with the results associated with control groups consisting of normal individuals.
REFERENCES
- 1.Toffol LD, Pavoni C, Baccetti T, Franchi L, Cozza P. Orthopedic treatment outcomes in Class III malocclusion. A systematic review. Angle Orthod. 2008;78:561–573. doi: 10.2319/030207-108.1. [DOI] [PubMed] [Google Scholar]
- 2.O'Reilley MT, Yanniello GJ. Mandibular growth changes and maturation of cervical vertebrae—a longitudinal cephalometric study. Angle Orthod. 1988;58:179–184. doi: 10.1043/0003-3219(1988)058<0179:MGCAMO>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 3.Schendel S, Jacobson R. Airway growth and development: a computerized 3-dimensional analysis. J Oral Maxillofac Surg. 2011;70:456–510. doi: 10.1016/j.joms.2011.10.013. [DOI] [PubMed] [Google Scholar]
- 4.Li H, Lu X, Shi J, Shi H. Measurements of normal upper airway assessed by 3-dimensional computed tomography in Chinese children and adolescents. Int J Pediatr Otorhinolaryngol. 2011;75:1240–1246. doi: 10.1016/j.ijporl.2011.06.022. [DOI] [PubMed] [Google Scholar]
- 5.Lee JW, Park KH, Kim SH, Park YG, Kim SJ. Correlation between skeletal changes by maxillary protraction and upper airway dimensions. Angle Orthod. 2011;81:426–432. doi: 10.2319/082610-499.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Guyer EC, Ellis E, McNamara JA, Jr, Behrents RG. Components of Class III malocclusion in juveniles and adolescents. Angle Orthod. 1986;56:7–30. doi: 10.1043/0003-3219(1986)056<0007:COCIMI>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 7.Battagel JM. The aetiological factors in Class III malocclusion. Eur J Orthod. 1993;15:347–370. doi: 10.1093/ejo/15.5.347. [DOI] [PubMed] [Google Scholar]
- 8.Sayinsu K, Isik F, Arun T. Sagittal airway dimension following maxillary protraction: a pilot study. Eur J Orthod. 2006;28:184–189. doi: 10.1093/ejo/cji095. [DOI] [PubMed] [Google Scholar]
- 9.Kaygısız E, Tuncer BB, Yüksel S, Tuncer C, Yildiz C. Effects of maxillary protraction and fixed appliance therapy on the pharyngeal airway. Angle Orthod. 2009;79:660–667. doi: 10.2319/072408-391.1. [DOI] [PubMed] [Google Scholar]
- 10.Oktay H, Ulukaya E. Maxillary protraction appliance effect on the size of the upper airway passage. Angle Orthod. 2008;78:209–214. doi: 10.2319/122806-535.1. [DOI] [PubMed] [Google Scholar]
- 11.Kilinç AS, Arslan SG, Kama JD, Ozer T, Dari O. Effects on the sagittal pharyngeal dimensions of protraction and rapid palatal expansion in Class III malocclusion subjects. Eur J Orthod. 2008;30:61–66. doi: 10.1093/ejo/cjm076. [DOI] [PubMed] [Google Scholar]
- 12.Mucedero M, Baccetti T, Franchi L, Cozza P. Effects of maxillary protraction with or without expansion on the sagittal pharyngeal dimensions in Class III subjects. Am J Orthod Dentofacial Orthop. 2009;135:777–781. doi: 10.1016/j.ajodo.2008.11.021. [DOI] [PubMed] [Google Scholar]
- 13.Baccetti T, Franchi L, Mucedero M, Cozza P. Treatment and post-treatment effects of facemask therapy on the sagittal pharyngeal dimensions in Class III subjects. Eur J Orthod. 2010;32:346–350. doi: 10.1093/ejo/cjp092. [DOI] [PubMed] [Google Scholar]
- 14.Barqhouth G, Prior JO, Lepori D, Duvoisin B, Schnyder P, Gudinchet F. Paranasal sinuses in children: size evaluation of maxillary, sphenoid, and frontal sinuses by magnetic resonance imaging and proposal of volume index percentile curves. Eur Radiol. 2002;12:1451–1458. doi: 10.1007/s00330-001-1218-9. [DOI] [PubMed] [Google Scholar]
- 15.Park IH, Song JS, Choi H, et al. Volumetric study in the development of paranasal sinuses by CT imaging in Asian: a pilot study. Int J Pediatr Otorhinolaryngol. 2010;74:1347–1350. doi: 10.1016/j.ijporl.2010.08.018. [DOI] [PubMed] [Google Scholar]
- 16.Garrett BJ, Caruso JM, Runqcharassaenq K, Farraqe JR, Kim JS, Taylor GD. Skeletal effects to the maxilla after rapid maxillary expansion assessed with cone-beam computed tomography. Am J Orthod Dentofacial Orthop. 2008;134:8–9. doi: 10.1016/j.ajodo.2008.06.004. [DOI] [PubMed] [Google Scholar]
- 17.Smith T, Ghoneima A, Stewart K, et al. Three-dimensional computed tomography analysis of airway volume changes after rapid maxillary expansion. Am J Orthod Dentofacial Orthop. 2012;141:618–626. doi: 10.1016/j.ajodo.2011.12.017. [DOI] [PubMed] [Google Scholar]
- 18.Motro M. Three-Dimensional Evaluation of the Maxillary Sinuses after Rapid Maxillary Expansion and Following One Year Retention Period [doctorate thesis] İstanbul, Turkey: Marmara University; 2011. [Google Scholar]