Abstract
Objective:
To measure and compare bracket transfer accuracy of five indirect bonding (IDB) techniques.
Materials and Methods:
Five IDB techniques were studied: double polyvinyl siloxane (double-PVS), double vacuum-form (double-VF), polyvinyl siloxane vacuum-form (PVS-VF), polyvinyl siloxane putty (PVS-putty), and single vacuum-form (single-VF). Brackets were bonded on 25 identical stone working models. IDB trays were fabricated over working models (n = 5 per technique) to transfer brackets to another 25 identical stone patient models. The mesiodistal (M-D), occlusogingival (O-G), and faciolingual (F-L) positions of each bracket were measured on the working and patient models using digital photography (M-D, O-G) and calipers (F-L). Paired t-tests were used to compare bracket positions between working and patient models, and analysis of variance was used to compare bracket transfer accuracy among the five techniques.
Results:
Between the working and patient models, double-VF had the most teeth with significant differences (n = 6) and PVS-VF the fewest (n = 1; P < .05). With one exception, all significant differences were ≤0.26 mm and most (65%) were ≤0.13 mm. When the techniques were compared, bracket transfer accuracy was similar for double-PVS, PVS-putty, and PVS-VF, whereas double-VF and single-VF showed significantly less accuracy in the O-G direction.
Conclusions:
Although overall differences in bracket position were relatively small, silicone-based trays had consistently high accuracy in transferring brackets, whereas methods that exclusively used vacuum-formed trays were less consistent.
Keywords: Indirect bonding, Bracket bonding accuracy
INTRODUCTION
A challenge in orthodontics is achieving ideal bracket position, which minimizes archwire bends and the need for bracket repositioning. In 1972, Silverman et al.1 were the first to publish an indirect bonding (IDB) technique. Brackets were positioned on dental casts and custom trays were fabricated to transfer the brackets to the patients' teeth. IDB has subsequently increased in popularity due to unimpaired visibility during bracket positioning, improved patient comfort, and reduced chair time.1–5
Most studies investigating the accuracy of IDB have made comparisons to direct bonding. Although bracket positioning is often similar, Aguirre et al.6 found that IDB was more accurate in the angulation of maxillary and mandibular canine brackets and for vertical bracket placement on maxillary canines, whereas direct bonding was more accurate with mandibular second premolars. Koo et al.7 found that, on average, IDB was more accurate with regard to bracket height, with no significant difference between IDB and direct bonding for angulation and mesiodistal position. Similarly, Hodge et al.8 found no statistically significant differences in the overall accuracy of bracket placement between direct bonding and IDB, although they did note a larger range in positioning for direct bonding.
Most of the IDB trays described in the literature use vacuum-formed thermoplastics, silicone impression materials, or a combination of both. Despite the various tray techniques available, only one study has compared bracket transfer accuracy between different IDB techniques.9 This study, which compared three IDB techniques, found that bracket transfer accuracy was significantly better for trays made of addition silicone than for single vacuum-formed trays.9 The purpose of the current study was to measure and compare bracket transfer accuracy of five IDB techniques.2,10–13
MATERIALS AND METHODS
Fabrication of Working and Patient Stone Models
A maxillary typodont (Model 3134, Viade Products Inc, Camarillo, Calif) served as the master model. For measurement purposes, each tooth had two reference notches: one on the facial and another on the lingual (Figure 1). Silicone molds of the master model were fabricated (Excel Orthodontics Inc, Tigard, Ore). From the molds, 50 identical orthodontic stone models (White ISO Type 3, Whip Mix, Louisville, Ky) were fabricated; 25 served as “working models” to which the brackets were bonded and 25 as the “patient models” to which the brackets were transferred.
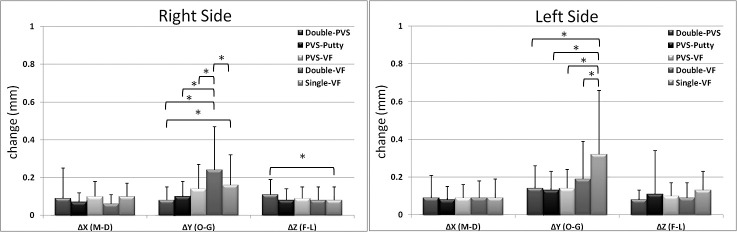
Figure 1.
Maxillary typodont with reference notches on facial and lingual surfaces.
Indirect Bonding Techniques
The working models were coated twice with separating agent (Al-Cote, Dentsply International, York, Penn) and dried for 8 hours. Adhesive precoated brackets (APC II Victory Series, 3M Unitek, Monrovia, Calif) were placed and light-cured in ideal positions14 on incisors, canines, premolars, and first molars. Following measurements, reference notches were blocked out with light-curing resin to prevent tray material locking. Five trays per technique were then fabricated over their corresponding working models (Table 1): double polyvinyl siloxane (double-PVS), double vacuum-form (double-VF), polyvinyl siloxane vacuum-form (PVS-VF), polyvinyl siloxane putty (PVS-putty), and single vacuum-form (single-VF). All trays were fabricated following the guidelines provided by publications describing each technique. In general, all trays extended from the facial over to the occlusal and at least half of the lingual surfaces.2,10–13
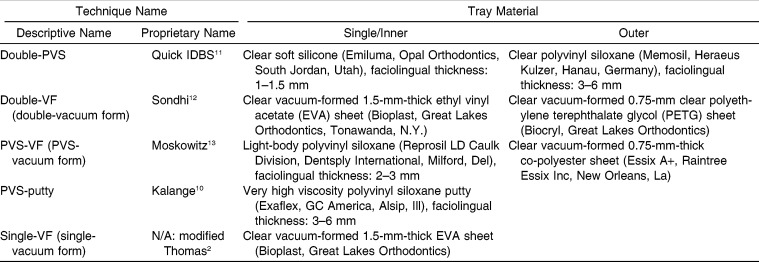
Table 1.
Tray Descriptions for Indirect Bonding Techniques Studied
Working model-tray assemblies were soaked in water for 1 hour to dissolve the separating agent. After removal, trays with brackets were cleaned using a detergent solution in an ultrasonic cleaner as described by Sondhi.12 A two-part (A-B) chemically cured bonding adhesive (Sondhi Rapid-Set Indirect Bonding Adhesive, 3M Unitek, St Paul, Minn) was used during IDB. Part A was applied to the patient model teeth and part B to the custom composite pads on brackets. Each tray was seated uniformly and held in place, with firm pressure applied parallel to the occlusal plane, by the investigator's right hand. For double-VF and single-VF, the anterior of the trays often did not adapt well to the facial surfaces of anterior teeth; therefore, pressure was applied with the investigator's left hand to the tray's anterior surface to ensure bonding. After 2.5 minutes, the bonding adhesive was set and the trays were carefully removed from the lingual to the buccal.
Photographic Measurements: Mesiodistal and Occlusogingival
Bonded teeth on both working and patient models were photographed individually using a Nikon D70 camera with a 105-mm Micro lens set on manual with an F-stop of 40 at 1∶500 of a second (Nikon, Tokyo, Japan) and ring flash (Macro Speedlight SB-29, Nikon) set at M1/4 illumination. To standardize images, the camera and models were placed on a custom jig that also held a millimeter ruler for calibration purposes (Figure 2). The models were placed on the jig using removable positioners (one for each tooth) that were fabricated to place the tooth's facial surface centered on and parallel to the camera lens.
Figure 2.

A jig with fixed positioning blocks was used to establish repeatable locations of the camera, ruler, and models.
JPEG images (300 × 300 dpi) were imported into Adobe Photoshop Elements 10 (Adobe Systems Inc, San Jose, Calif) and magnified 8.5 times. For each bracket, mesiodistal (M-D) (x-axis) and occlusogingival (O-G) (y-axis) measurements were made as follows (Figure 3):
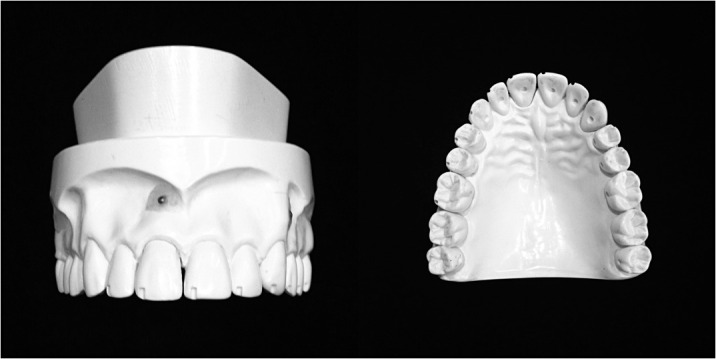
Figure 3.
Measurement points for molars and nonmolars, with constructed origin and grid. Points A and B were used for photography, and points C and D were used for caliper measurements.
A software-constructed grid was calibrated so that the distance between the gridlines equaled 1.00 mm.
The image was rotated so that the horizontal and vertical lines outlining the corner of the facial reference notch closest to the bracket paralleled the gridlines.
The origin of the grid was made coincident with the intersection of the lines outlining the corner of the reference notch.
Two points (A, B) were selected to coincide with the intersection of the inside of the mesial and distal tie wings with the occlusal edge of the scribe line base, except for the molars, where the inner occlusal corners of the tie wings were used.
For each point, x- and y-coordinate values were recorded to the nearest 0.01 mm.
Point coordinates were recorded three times consecutively on the same image and then averaged.
Caliper Measurements: Faciolingual
Digital calipers (ECCO-100795, US Dental Depot Inc, Ft Lauderdale, Fla) were used to measure faciolingual (F-L) (z-axis) bracket positions as follows:
Two points (C, D) were selected at the gingival and occlusal ends of the bracket scribe line, except for molars, where the points were locatetd at the intersection of the gingival and occlusal scribe lines with the bracket base (Figure 3).
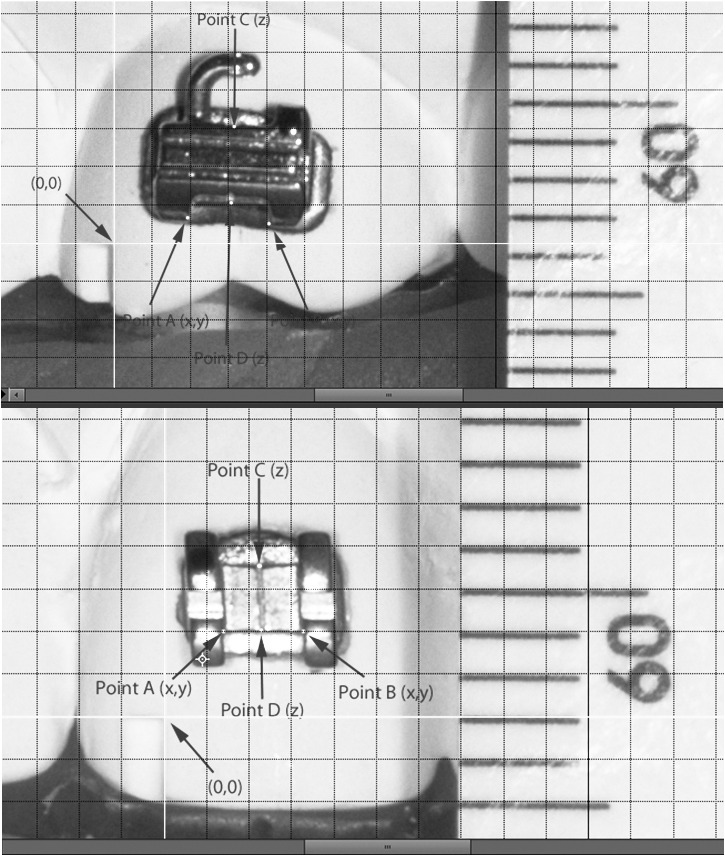
The nonmobile tip of a digital caliper was placed at the depth of the lingual reference notch, and the mobile tip was aligned with each of the points (Figure 4).
Measurements were recorded to the nearest 0.01 mm.
Figure 4.
Digital caliper measuring F-L bracket position, with nonmobile end of caliper placed at the depth of the lingual reference notch and mobile end on points C and D (see Figure 3).
Measurements were repeated three times consecutively and averaged.
Statistical Analysis
To determine the method error, five arbitrarily selected model images (one per technique) were re-measured at least 2 weeks after initial measurements, followed by the use of Dahlberg's formula.15–18
To assess the accuracy of each technique, bracket coordinate value differences for each tooth between working and patient model pairs (n = 5) were analyzed using paired t-tests. For technique comparisons, analyses were conducted for all teeth grouped, anterior teeth, posterior teeth, and left and right sides of the arch using analysis of variance followed by Tukey post hoc comparisons. Significance was set to P < .05.
RESULTS
Method Error
The method error was 0.07 mm for photographic measurements and 0.01 mm for caliper measurements.
Debonded Brackets
Four of the 300 brackets that were transferred debonded during tray removal: two with double-VF (teeth #14, #15) and two with single-VF (teeth #11, #12).
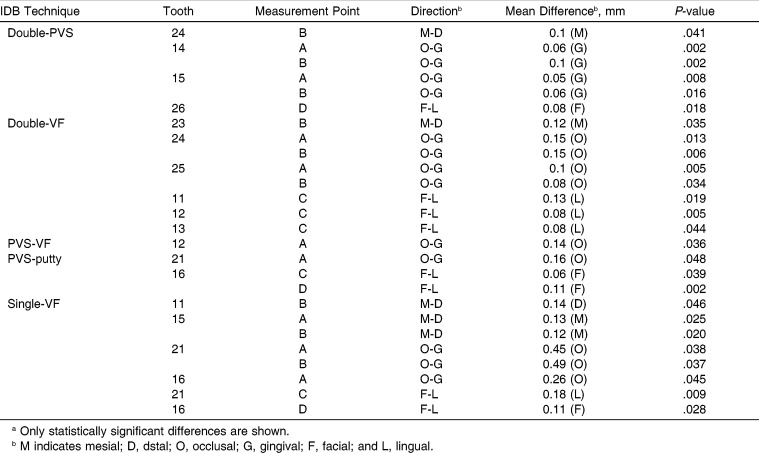
Comparisons between Working and Patient Models
All techniques had at least one tooth with significant differences in bracket position (Table 2). Double-VF had the most teeth (n = 6) with significant differences, whereas PVS-VF had the fewest (n = 1). The greatest number of significant differences occurred in the O-G dimension (n = 13), followed by F-L (n = 8) and M-D (n = 5). With the exception of tooth #21 for single-VF, all significant differences were ≤0.26 mm and most (65%) were ≤0.13 mm. Of the 17 teeth with significant differences, 10 were significantly different in one direction only.
Table 2.
Mean Differences in Bracket Position between Working and Patient Modelsa
Comparison of Bracket Transfer Accuracy among the 5 IDB Techniques
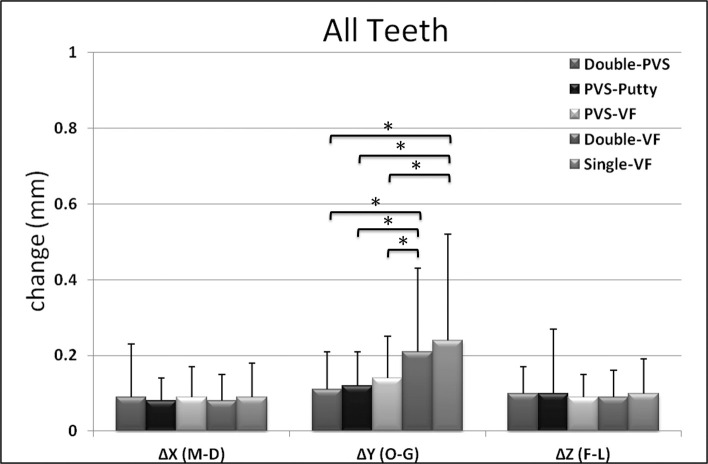
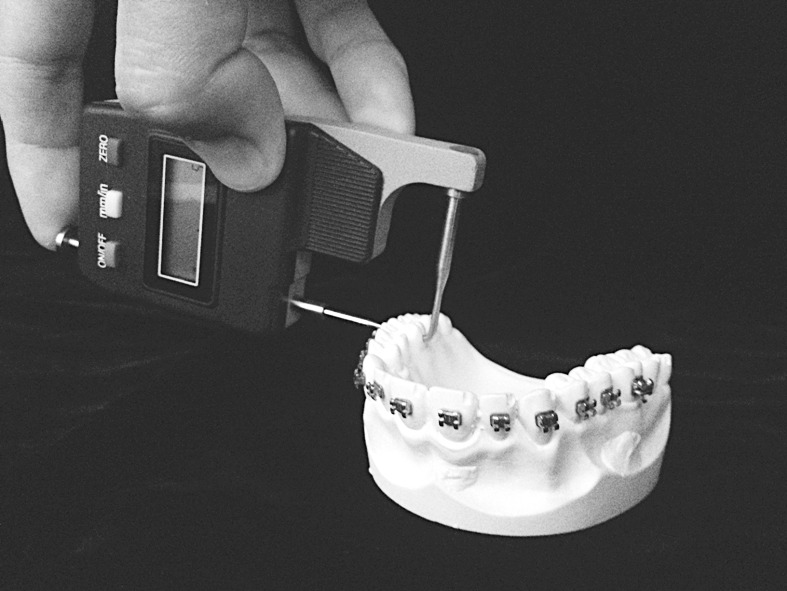
When the techniques were compared for all teeth grouped together, no transfer accuracy differences were found for double-PVS, PVS-putty, and PVS-VF, whereas double-VF and single-VF were significantly less accurate in the O-G direction (Figure 5).
Figure 5.
Comparison of mean differences in bracket position among the five techniques for all teeth grouped. * P < .05.
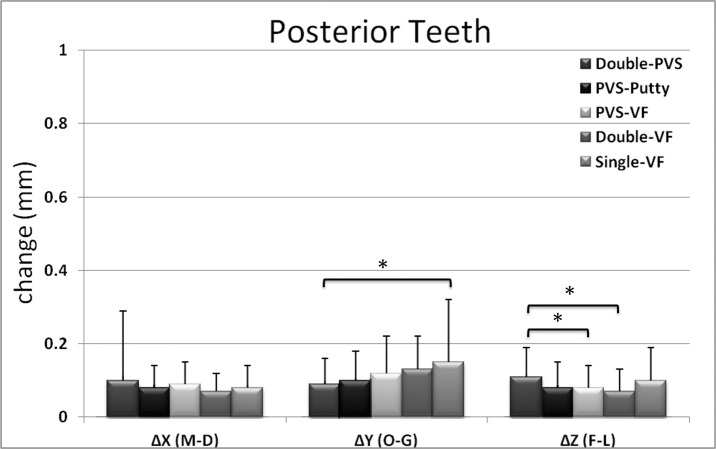
When the techniques were compared for anterior teeth only, double-VF and single-VF were, again, less accurate than the other three techniques in the O-G direction (Figure 6). With posterior teeth, only single-VF showed less O-G accuracy versus double-PVS, while double-PVS was less accurate versus PVS-VF and double-VF in the F-L direction (Figure 7). The right side of the arch showed a greater number of significant differences versus the left (Figure 8).
Figure 6.
Comparison of mean differences in bracket position among the five techniques for anterior teeth. * P < .05.
Figure 7.
Comparison of mean differences in bracket position among the five techniques for posterior teeth. * P < .05.
Figure 8.
Comparison of mean differences in bracket position among the five techniques for left and right sides of the arch. * P < .05.
DISCUSSION
This study evaluated and compared five commonly used techniques that differed in transfer tray materials. To minimize the potential effects of variables such as dental arch form, tooth shapes, and crowding, a maxillary arch was used with well-aligned teeth to allow assessment in an ideal setting. Working models served as controls for their corresponding patient models, and reference notches provided reliable points for bracket position measurement, as evidenced by method errors ≤0.07 mm.
Each technique had at least one tooth with significant differences in bracket position; however, many differences were small, suggesting the need to set thresholds of clinical significance. Armstrong et al.19 reported that changes of ≥0.25 mm for upper central and lower incisor brackets and ≥0.5 mm for remaining teeth would be clinically significant. The Model Grading System of the American Board of Orthodontics deducts points for alignment or marginal ridge discrepancies of ≥0.5 mm.20 For this study, a 0.13-mm discrepancy in any direction was deemed clinically significant, so if brackets on adjacent teeth were misplaced by 0.13 mm in opposite directions, tooth position discrepancies would be >0.25 mm. Single-VF and double-VF showed the greatest number of teeth with clinically significant differences, whereas double-PVS had none.
Two measurement points were used per dimension to determine whether the bracket position changes were rotational or purely linear. Ten teeth (at least one per technique) had significant differences in only one of two points, indicating that bracket rotations had occurred. Significant differences in the F-L measurements on tooth #21 (point C) and on tooth #16 (point D) with single-VF likely relate to the large differences that were also present in the O-G direction, causing angulation changes in the F-L line of measurement when using calipers. This is inherent to the use of calipers and may be considered a weakness of the study.
When the techniques were compared for all teeth grouped (Figure 5), bracket transfer accuracy was comparable for silicone-based techniques (double-PVS, PFS-VF, and PVS-putty). Both double-VF and single-VF were significantly less accurate than the others in the O-G direction, a result also evident for anterior but not for posterior teeth. Likewise, Dörfer et al.9 found that the greatest imprecision occurred in the vertical dimension. For posterior teeth, O-G accuracy was significantly lower for single-VF versus double-PVS (Figure 7), and although potentially clinically significant, the mean change (0.15 mm) was considerably smaller than mean O-G changes for double-VF and single-VF with anterior teeth (0.29 mm and 0.33 mm, respectively). In the F-L direction, posterior teeth showed significantly lower accuracy for double-PVS versus PVS-VF and double-VF, but the small mean change (0.11 mm) is likely not clinically significant.
The poorer O-G accuracy for anterior teeth with double-VF and single-VF can be attributed to increased elongation of the ethyl vinyl acetate (EVA) sheets over the longer anterior crowns, resulting in relatively decreased anterior tray thickness. Ryokawa et al.21 found significant decreases in material thickness and elastic modulus (decreased rigidity) for EVA following vacuum-forming. Although double-VF has an outer polyethylene terephthalate glycol (PETG) tray, it is not fused with the inner EVA tray and is trimmed occlusal to the gingival bracket wings, away from all heights of contour,12 and thus does not cover the entire O-G dimension of the brackets. The use of hand pressure against the anterior part of the tray with double-VF and single-VF in an attempt to improve the tray's adaptation undoubtedly contributed to bracket position variability with these two techniques. Similarly, the poorer bracket transfer accuracy on the right vs left side, mostly involving single-VF and double-VF in the O-G direction, could be a result of the greater sensitivity of these techniques to differences in hand pressure.
The three techniques with the highest bracket transfer accuracy used polyvinyl siloxane (addition silicone) as the material in direct contact with both brackets and tooth surfaces. This is consistent with the findings of Dörfer et al.,9 who found that the silicone transfer trays have significantly higher bracket transfer accuracy compared to a single vacuum-form tray. Additional silicone impression materials have been shown to have excellent dimensional stability, superior recovery from deformation (elastic recovery), and high rigidity.22–24 Additionally, all silicone trays were thicker faciolingually than nonsilicone trays, contributing to increased rigidity. Low rigidity in an IDB tray may result not only in inaccurate bracket position transfer, but also in an increased number of bond failures due to poor adaptation. Bhatnagar et al.25 evaluated bond failures for four IDB techniques and found the highest percentage of failures (50%) with a single-tray vacuum-formed technique that used 2-mm EVA sheets. Consistent with these results, this study showed bond failures only with methods that exclusively used vacuum-formed trays.
Based on results of this study, selection of double-PVS, PVS-VF, and PVS-putty could be based on preference or criteria such as tray cost, fabrication time, and opacity. At the time of this study, material expenses were lowest for PVS-putty and highest for double-PVS (approximately 12-fold difference).
Regarding tray fabrication time, PVS-putty was the quickest, while double-PVS required the most time (approximately 6 vs 20 minutes per tray, respectively). Because PVS-VF and PVS-putty trays are opaque, chemically cured bonding adhesive is required, whereas the translucency of double-PVS allows for the use of chemically or light-cured adhesive. In addition, the translucency of double-PVS also allows visual confirmation of tray seating during IDB.
A limitation of this study is that it used an ideal dental arch model, rather than the typical clinical scenario of crowded and/or rotated teeth. Different results might be found in arches with irregular tooth alignment, as tray dimensions would vary, and different tray materials (eg, Biocryl) may respond differently to the divergent crown angulations. Future clinical studies evaluating the accuracy of IDB may provide insights into how tray material properties affect tray seating and therefore tray-tooth registration in vivo.
CONCLUSIONS
All IDB techniques investigated had at least one tooth with statistically significant differences in bracket position, but the most clinically significant differences were found with the single-VF and double-VF techniques.
Changes in bracket position were not purely linear; some were rotational.
When the five techniques were compared, bracket transfer accuracy was comparable for the silicone-based techniques.
Double-VF and single-VF were significantly less accurate than the other techniques in the O-G direction.
REFERENCES
- 1.Silverman E, Cohen M, Gianelly AA, Dietz VS. A universal direct bonding system for both metal and plastic brackets. Am J Orthod. 1972;62:236–244. doi: 10.1016/s0002-9416(72)90264-3. [DOI] [PubMed] [Google Scholar]
- 2.Thomas RG. Indirect bonding: simplicity in action. J Clin Orthod. 1979;13:93–106. [PubMed] [Google Scholar]
- 3.Hodge TM, Dhopatkar AA, Rock WP, Spary DJ. The Burton approach to indirect bonding. J Orthod. 2001;28:267–270. doi: 10.1093/ortho/28.4.267. [DOI] [PubMed] [Google Scholar]
- 4.Kalange JT. Indirect bonding: a comprehensive review of the advantages. World J Orthod. 2004;5:301–307. [PubMed] [Google Scholar]
- 5.Guenthner TA, Larson BE. Indirect bonding: A technique for precision and efficiency. Semin Orthod. 2007;13:58–63. [Google Scholar]
- 6.Aguirre MJ, King GJ, Waldron JM. Assessment of bracket placement and bond strength when comparing direct bonding to indirect bonding techniques. Am J Orthod. 1982;82:269–276. doi: 10.1016/0002-9416(82)90461-4. [DOI] [PubMed] [Google Scholar]
- 7.Koo BC, Chung CH, Vanarsdall RL. Comparison of the accuracy of bracket placement between direct and indirect bonding techniques. Am J Orthod Dentofacial Orthop. 1999;116:346–351. doi: 10.1016/s0889-5406(99)70248-9. [DOI] [PubMed] [Google Scholar]
- 8.Hodge TM, Dhopatkar AA, Rock WP, Spary DJ. A randomized clinical trial comparing the accuracy of direct versus indirect bracket placement. J Orthod. 2004;31:132–137. doi: 10.1179/146531204225020427. [DOI] [PubMed] [Google Scholar]
- 9.Dorfer S, König M, Jost-Brinkmann P-G. Übertragungsgenauigkeit beim indirekten Platzieren von Brackets. Kieferorthopädie. 2006;20:91–104. [Google Scholar]
- 10.Kalange JT. Prescription-based precision full arch indirect bonding. Semin Orthod. 2007;13:19–42. [Google Scholar]
- 11.Koga M, Watanabe K, Koga T. Quick Indirect Bonding System (Quick IDBS): an indirect bonding technique using a double-silicone bracket transfer tray. Semin Orthod. 2007;13:11–18. [Google Scholar]
- 12.Sondhi A. Effective and efficient indirect bonding: the Sondhi method. Semin Orthod. 2007;13:43–57. [Google Scholar]
- 13.Moskowitz EM. Indirect bonding with a thermal cured composite. Semin Orthod. 2007;13:69–74. [Google Scholar]
- 14.McLaughlin RP, Bennett JC, Trevisi HJ. Systemized Orthodontic Treatment Mechanics 1st ed. Elsevier Limited; Philadelphia, PA: 2002. [Google Scholar]
- 15.Naraghi S, Andren A, Kjellberg H, Mohlin BO. Relapse tendency after orthodontic correction of upper front teeth retained with a bonded retainer. Angle Orthod. 2006;76:570–576. doi: 10.1043/0003-3219(2006)076[0570:RTAOCO]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 16.Caldas MP, Ambrosano GMB, Haiter Neto F. New formula to objectively evaluate skeletal maturation using lateral cephalometric radiographs. Braz Oral Res. 2007;21:330–335. doi: 10.1590/s1806-83242007000400009. [DOI] [PubMed] [Google Scholar]
- 17.Harris EF, Smith RN. Accounting for measurement error: a critical but often overlooked process. Arch Oral Biol. 2009;54S:S117. doi: 10.1016/j.archoralbio.2008.04.010. [DOI] [PubMed] [Google Scholar]
- 18.de Souza Galvao MC, Sato JR, Coelho EC. Dahlberg formula—a novel approach for its evaluation. Dental Press J Orthod. 2012;17:115–124. [Google Scholar]
- 19.Armstrong D, Shen G, Petocz P, Ali Darendeliler M. A comparison of accuracy in bracket positioning between two techniques—localizing the centre of the clinical crown and measuring the distance from the incisal edge. Eur J Orthod. 2007;29:430–436. doi: 10.1093/ejo/cjm037. [DOI] [PubMed] [Google Scholar]
- 20.American Board of Orthodontics. June 2012. The American Board of Orthodontics grading system for dental casts and panoramic radiographs. doi: 10.1016/s0889-5406(98)70179-9. Available at: http://www.americanboardortho.com Accessed December 5, 2013. [DOI] [PubMed] [Google Scholar]
- 21.Ryokawa H, Miyazaki Y, Fujishima A, Miyazaki T, Maki K. The mechanical properties of dental thermoplastic materials in a simulated intraoral environment. Orthod Waves. 2006;65:64–72. [Google Scholar]
- 22.O'Brien WJ. Dental Materials and their Selection 2nd ed. Chicago: Quintessence; 1997. [Google Scholar]
- 23.Mandikos MN. Polyvinyl siloxane impression materials: an update on clinical use. Aust Dent J. 1998;43:428–434. doi: 10.1111/j.1834-7819.1998.tb00204.x. [DOI] [PubMed] [Google Scholar]
- 24.Lu H, Nguyen B, Powers JM. Mechanical properties of 3 hydrophilic addition silicone and polyether elastomeric impression materials. J Prosthet Dent. 2004;92:151–154. doi: 10.1016/j.prosdent.2004.05.016. [DOI] [PubMed] [Google Scholar]
- 25.Bhatnagar S, Dhandapani G, Bagga DK. Evaluation of bond failures and shear bond strength in indirect bonding technique using 4 different transfer tray materials—an in vitro study. J Indian Dent Assoc. 2011;5:595–598. [Google Scholar]