Abstract
Objective:
To evaluate the combined effects of material type, surface treatment, and thermocycling on the bond strength of orthodontic brackets to materials used for the fabrication of provisional crowns.
Materials and Methods:
Four materials were included in this study (ProTemp, Trim Plus, Trim II, and Superpont C+B). Sixty cylindrical specimens (1 × 3 cm) were prepared from each material and equally divided into three groups. The first group was ground with silica carbide paper, the second was polished with pumice, and the last group was sandblasted with 50-µm aluminum oxide particles. Stainless-steel maxillary central incisor brackets (Victory Series, 3M) were bonded to the provisional material specimens with Transbond XT light-cured composite resin, and half of the specimens from each group were thermocycled 500 times in 5°C and 55°C water baths. Then the brackets were debonded with shear testing, and the results were statistically analyzed by three-way analysis of variance and Tukey's multiple-comparison tests at α = 0.05. Adhesive Remnant Index (ARI) was also identified.
Results:
Before and after thermocycling, ProTemp materials showed the highest shear bond strength with orthodontic brackets (10.3 and 13.1 MPa, respectively). The statistical analysis indicated an interaction among the three independent variables (P < .05) and statistically significant differences in bond strength among provisional materials (P < .001), surface treatments (P < .001), and thermocycling (P < .05). According to the ARI, most groups demonstrated adhesive failure.
Conclusions:
The provisional material type, surface treatment, and artificial aging have a significant effect on bond strength. Sandblasting treatment exerts a beneficial effect on shear bond strength.
Keywords: Provisional materials, Orthodontic brackets, Adhesives, Shear bond strength, Thermocycling
INTRODUCTION
The adult dentition is usually characterized by previous and ongoing restorative procedures, and in many cases, orthodontic procedures must be modified and performed in conjunction with other dental interventions. As a result, orthodontists frequently bond brackets onto provisional crowns for adjunctive or comprehensive orthodontic treatment.
Many factors influence material selection in the fabrication of provisional restorations, including physical, mechanical, and handling properties as well as biocompatibility.1 However, as in the case of natural teeth, the bonded brackets should have sufficient bond strength to withstand orthodontic forces. A weak bond of the brackets to provisional materials will lead to a high failure rate, with adverse consequences on the cost and efficiency of orthodontic therapy as well as on patient comfort. Many factors influence the strength of the bond between the bracket and provisional materials, including the type of provisional material,2–5 the adhesive material,6,7 the time of storage following bonding,8 and thermocycling.9
Various studies2–5 have addressed the combinations of different types of provisional restorations, different adhesives, and different methods of treating provisional surfaces prior to bracket bonding. However, the combined effect of thermocycling with different types of provisional materials and surface treatments has not yet been tested. Therefore, the aim of this study was to evaluate the effects of the three aforementioned independent parameters on the bond strength of orthodontic brackets to provisional materials.
MATERIALS AND METHODS
Specimen Preparation
Four different commonly used provisional material types were used in this study (Table 1). Sixty cylindrical specimens (diameter, 1 cm; height, 2 cm) were prepared from each material (n = 240). For the chemically cured provisional material resin, the specimens were constructed in a machined metal mold with internal concavity dimensions of 1 cm (diameter) and 2 cm (height) (Figure 1a). The materials were mixed according to the manufacturer's instructions; the molds were filled and allowed to set at room temperature. To standardize the heat-activated provisional material resin, a wax pattern was obtained (diameter, 1 cm; height, 2 cm) from the machined metal mold. The wax pattern was then invested in dental stone within a conventional denture flask. After the stone had set, the wax was boiled out, and the provisional resin material was mixed, packed, and heat-processed according to the manufacturer's instructions.
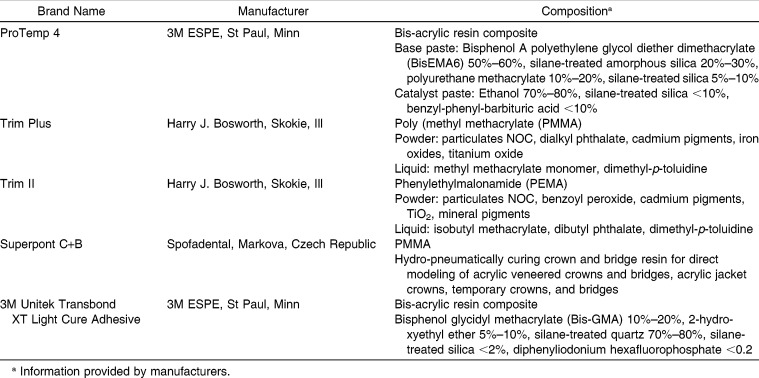
Table 1.
Brand Names, Manufacturers, and Chemical Compositions of the Materials and the Adhesive Media Included in the Present Study
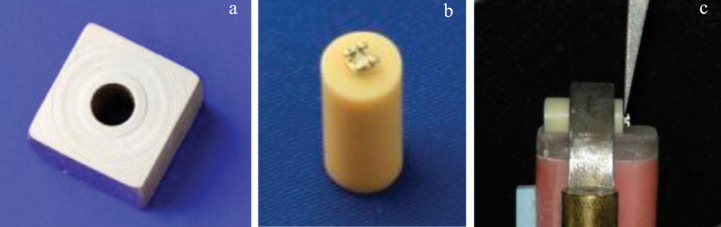
Figure 1.
(a) The metallic mold used for the production of the specimens. (b) The cylindrical specimens with the bonded bracket. (c) Mounted specimen ready to be tested in shear loading.
The 60 specimens of each material were divided equally into three groups (n = 20) (Table 2). Each group was subjected to three different surface treatments, as follows.
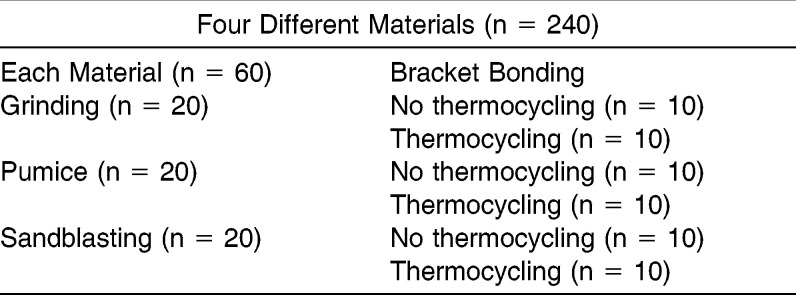
Table 2.
Grouping and Number of Specimens for Each Material Tested
Surface grinding
The specimen surfaces were ground with silica carbide paper up to a 600-grit size in a grinding/polishing machine (Polo250/3; Jean Wirtz, Düsseldorf, Germany).
Treatment with pumice
The specimen surfaces were ground as described above and were additionally polished with a pumice polishing paste (Buehler Micropolish II, Lake Bluff, Ill), first with a 1-µm and then with a 0.05-µm particle size, until a shiny, mirror-like surface was achieved.
Treatment with sandblasting
The specimen surfaces were ground and polished as described above and were additionally sandblasted with 50-µm alumina grains for 10 seconds from a distance of 10 mm by the application of 0.55 MPa of propulsion pressure (Microetcher ER, Danville Engineering Inc, Danville, Calif).
Bracket Bonding Procedure
Stainless-steel maxillary central incisor brackets (Victory Series, 3M Unitek, Monrovia, Calif) were bonded to the provisional material specimens with a light-cured composite resin (Transbond XT; 3M Unitek) by the same clinician. The surface of the provisional material was etched with 37% phosphoric acid for 30 seconds, then rinsed with water spray for 20 seconds and dried with oil-free compressed air for 20 seconds. During the bonding, a constant 5-N force was applied to the top surface of the bracket to obtain a uniform adhesive layer thickness. Any excess adhesive was removed and the adhesive was light-cured by means of an Ortholux XT Visible light-curing unit (3M Unitek) for 10 seconds on the mesial and distal sides (5 seconds on each side), according to the manufacturer's instructions. Following preparation, samples were stored in distilled water at 37°C ± 2°C for 24 hours.
Thermocycling
The three groups of each material were divided equally into two subgroups (Table 2), one of which was subjected to a thermocycling procedure applying 500 cycles of alternating 5°C and 55°C water baths. The specimens were incubated for 30 seconds in cold or hot water, with a 5-second interval between successive immersions, employing a thermocycling machine (THE-1100, SD Mechatronik, Feldkirchen-Westerham, Germany).
Bracket Debonding Procedure
The specimens were shear loaded (Figure 1c) glycidyl methacrylate at the bracket-specimen interface at a crosshead speed of 1 mm/min to fracture mounted on a universal testing machine (Instron 8500R, High Wycombe, Bucks, UK). Then the surface of each specimen was examined under a light microscope at 25× magnification to assess the remaining Adhesive Remnant Index (ARI).
Statistical Analysis
The bond strength data were analyzed by three-way analysis of variance (ANOVA), with material, surface treatment, and thermocycling as discriminating variables, and with a Tukey's multiple-comparison test at α = 0.05.
RESULTS
The results of shear bond testing and the outcome of statistical analysis are schematically illustrated in Figure 2. There was an interaction among the three independent variables of material type, surface treatment, and thermocycling (P < .05). An ANOVA showed statistically significant differences in bond strength among the provisional materials (P < .001), surface treatments (P < .001), and thermocycling (P < .05).
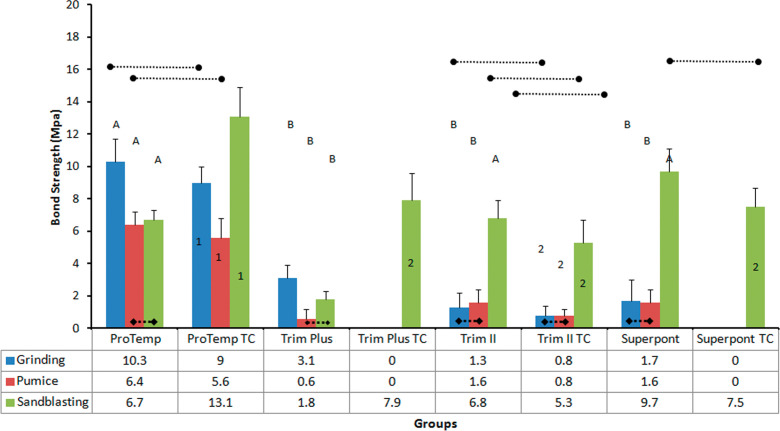
Figure 2.
Mean bond strengths (table with data) and standard deviations of all groups tested. Dotted lines with rectangular ends show groups without statistically significant differences among the surface treatments. Dotted lines ending with circles represent groups without statistically significant differences before and after thermocycling. The same capital letter illustrates groups without differences among materials with the same surface treatment and before thermocycling, and numbers indicate groups without significant differences among materials with the same surface treatment and after thermocycling (P > .05).
In the nonthermocycling condition, ProTemp showed significantly higher bond strength (P < .05) than did the other provisional materials, regardless of the surface treatment, apart from Trim II and Superpont C+B in the sandblasting group. No significant differences were found among Trim Plus, Trim II, and Superpont C+B in the ground and pumiced groups. In the thermocycling category, Trim Plus and Superpont showed zero values in the ground and pumiced groups, but no differences were observed among the three materials in the sandblasting group (P > .05). Again, ProTemp showed significantly higher values after thermocycling.
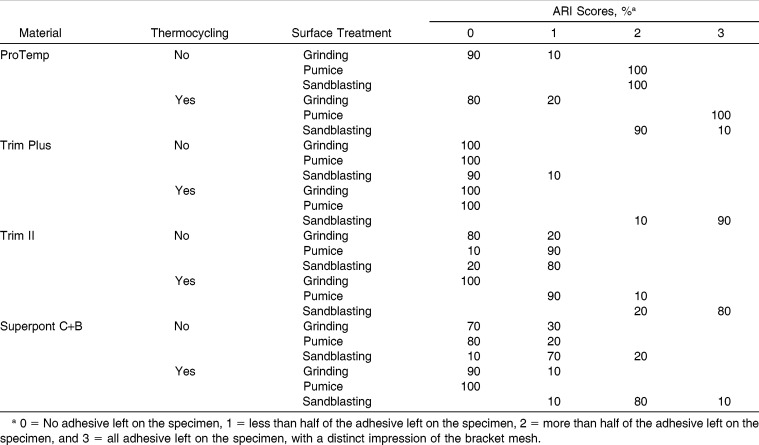
Surface treatments influenced the shear bond strength of the four types of provisional materials. In the nonthermocycling group (Figure 2) for ProTemp and Trim Plus, the ground groups exhibited statistically significant differences (P < .05) relative to the pumiced and sandblasting groups, whereas for Trim II and Superpont, the sandblasted surface treatment demonstrated significant differences (P < .05) in shear bond strength relative to the ground and pumiced groups. In contrast, with thermocycling (Figure 2), the sandblasted groups demonstrated significantly higher mean shear bond strengths than did the other surface treatment groups, regardless of material type. One interesting result was the total debonding of orthodontic brackets after thermocycling for Trim Plus and Superpont in the ground and pumiced groups. The obtained ARI scores are presented in Table 3.
Table 3.
Distribution of Adhesive Remnant Index (ARI) Scores for All Groups Tested
DISCUSSION
The results of this study showed that the independent variables tested showed significant interactions; that is, they had a synergistic effect on bond strength (P < .05). The tested materials were chosen because each belongs to a different category of contemporary materials used for the production of provisional restorations (Table 1). The pumiced group is representative of the clinical practice in which the restoration surfaces are cleaned and polished before bonding. The ground group with rougher surfaces may represent a clinically worn provisional restoration that was not polished before bracket bonding although worn surfaces may have a vast range of surface roughness. The sandblasting is readily used chairside before bonding of orthodontic brackets. Storage in water for 24 hours and 500 cycles of water thermocycling are recommended by ISO 11405:200310 to identify materials that can sufficiently sustain the wet environment. In this study, a crosshead speed of 1 mm/min was selected, although previous studies have reported speeds ranging from 0.5 to 5 mm/min.11 In any case, these ranges of crosshead speeds lack relevance to clinical conditions,12,13 in which even 200 mm/min is considered to be lower than the intraoral condition.
Ideally, the bond strength of brackets to provisional material should be sufficiently strong to prevent bracket debonding during the treatment; however, the bracket should still be able to be easily removed without harm to the tooth surface. It is widely reported in relevant literature14,15 that the minimum adequate bond strength should be between 6 and 8 MPa. However, this “threshold strength” approach has been criticized in that it overlooks the intraoral degradation of adhesive resin12,13 caused by fatigue,16 temperature and pH variations,17 and microbial degradation.18 Additionally, previous studies19,20 have shown that in vivo–aged bond strengths are significantly lower than the strength of artificially aged laboratory-tested bonds. In any case, the Bis-acryl (ProTemp) material exhibited a bond strength superior to that of the other provisional material types3,4 in the ground and pumiced groups, which agrees with results from previous studies.2 Therefore, the use of a Bis-acrylic composite is recommended for provisional restorations in cases in which orthodontic treatment is needed. The superior bond strength of the Bis-acrylic composite may be attributed to the presence of bifunctional acrylates, which cross-link to provide advanced mechanical strength and increased resistance to weakening in the presence of water.21,22 Conversely, this mechanism is not applicable for the other materials, which may explain their inferior bond strength.22
In addition to the combination of materials, bond strength also depends on the surface treatment applied. The surfaces that were well polished with pumice did not provide any source of mechanical bonding, and thus only chemical bonding is possible. Although the ground surfaces did provide a few valleys, the results of this study are not conclusive, since ProTemp and Trim Plus showed increased bond strength, whereas the ground and pumiced groups showed no significant differences for Trim II and Superpont. This finding may imply that the two independent variables have a synergistic effect on bond strength, as shown by the statistical analysis; thus, further research is required. Sandblasting increased the bond strength in all groups except for ProTemp, which indicates that this type of surface roughening, with small valleys and protruding peaks, provides beneficial mechanical interlocking.
Thermocycling had a detrimental effect on poly (methyl methacrylate) PMMA materials (Trim Plus and Superpont) in the ground and pumiced groups, whereas ProTemp and Trim II remained unaffected. This finding may imply that PMMA materials are more prone to water softening during artificial aging.23 Another detrimental mechanism that may be implicated in this degradation is the generation of thermal stresses. Although the coefficient of thermal expansion (CTE) of ProTemp and Transbond XT has not been previously determined, it was anticipated, based on their chemical compositions (Table 1), that ProTemp and Transbond XT would have CTE values of approximately 48 and 23 (×10−6/°C at 0°C–60°C), respectively,24 whereas for PMMA, the CTE should be 70 × 10−6/°C.25 Based on these data, the deformation of PMMA-based materials can be calculated to be approximately 200% of the deformation of the adhesive (Transbond XT) within the thermocycling temperature range (5°C–55°C), whereas for the ProTemp, this value decreased by approximately half (106%), which indicates that the PMMA adhesive interfaces underwent higher thermal stresses during thermocycling. Therefore, the use of a different adhesive with a higher CTE than that of Transbond XT may solve this problem. The bond strengths of Trim II and Superpont in the sandblasted groups remained unaffected by thermocycling, which implies that sandblasting has a beneficial effect on preserving initial bond strength values. In contrast, ProTemp and Trim Plus demonstrated increased bond strength in the sandblasted groups after thermocycling, which was unexpected. This finding may be attributed to the increased mobility of radicals, which would be expected to lead to additional polymerization during heating in the thermocycling procedure. However, this explanation requires further experimental testing.
A significant clinical demand is the maintenance of a sound, unblemished enamel surface at the end of orthodontic treatment, after bracket removal; therefore, the type of debonding (cohesive adhesive) is important. In the case of bracket debonding at the bracket-adhesive interface, the enamel surface remains relatively intact, although extensive chair time is needed for successful removal of residual adhesive. The latter concern is eliminated when the brackets fail at the adhesive-tooth interface, but the enamel surface can still deteriorate when brackets fail in this way. Although ARI was initially introduced to describe this clinical situation,26 it was extensively used later in the dental literature to characterize the fracture mode. This method has initial limitations, since it is impossible to characterize reliably the fracture mode of a system with two interfaces (enamel-adhesive and adhesive-bracket) with a simple and questionable classification of four different classes (0 to 3). It is difficult to accept that 0.1% is classified in class 1 along with 50%, and at the same time, 0.1% is different from class 0. In addition, a score of 3 has been used to describe adhesive fracture between the bracket and adhesive resin (all adhesive left on the specimen surface with a distinct impression of the bracket mesh4), and in other cases, this score has been used to describe the cohesive fracture of the adhesive resin (all adhesive remaining on tooth surface and resin imprint visible on the bracket base27). Another missing class includes situations in which part of the resin has the imprint of bracket mesh and the rest of the fracture is at the adhesive-tooth interface. Recently, an alternative scoring method9 has been developed that includes six classes, but the aforementioned limitations remain. Nevertheless, it is logical to assume that for the materials tested in this study, the situation after clinical debonding is better described by the groups that underwent thermocycling. Therefore, ProTemp in polished and sandblasted surfaces will need more time to be cleaned than in the ground group. The same is true for the rest of the materials in the sandblasted group, as the fracture site moves from the provisional material-adhesive interface (scores 0 and 1) to the adhesive-bracket interface (score 2 and 3), which implies that the mechanically inferior site of the system is located within the resin or at the adhesive resin-bracket interface rather than at the provisional material-adhesive interface.
Clinically, the fabrication of a provisional crown from Bis-acrylic composite would be a better choice, since it may minimize the incidence of bracket dislodgement during orthodontic treatment. Furthermore, a Bis-acryl composite material is widely preferred because of its superior handling characteristics, including ease of manipulation, ease of repair with a composite resin, low polymerization shrinkage, reduced porosity, and color stability.28 If other provisional material types that are non–resin-based are used, or when a highly polished provisional crown is received from a dental laboratory, the clinician is advised to sandblast the bracket bonding site before referring patients to their orthodontists.
CONCLUSIONS
The shear bond strength of orthodontic brackets to provisional materials depends on the material type, surface treatment, and artificial aging and their synergistic effect.
Provisional surfaces that are subjected to grinding or pumice treatment cannot withstand clinically acceptable orthodontic forces, except for Bis-acrylic composite resin.
Sandblasting has a beneficial effect on bond strength.
ACKNOWLEDGMENTS
This study was funded by a research grant (RGP-VPP-206) from the Research Group Program, Deanship of Scientific Research, King Saud University, Riyadh, Saudi Arabia.
REFERENCES
- 1.Burns DR, Beck DA, Nelson SK. A review of selected dental literature on contemporary provisional fixed prosthodontic treatment: report of the Committee on Research in Fixed Prosthodontics of the Academy of Fixed Prosthodontics. J Prosthet Dent. 2003;90:474–497. doi: 10.1016/s0022-3913(03)00259-2. [DOI] [PubMed] [Google Scholar]
- 2.Chay SH, Wong SL, Mohamed N, et al. Effects of surface treatment and aging on the bond strength of orthodontic brackets to provisional materials. Am J Orthod Dentofacial Orthop. 2007;132:e7–e11. doi: 10.1016/j.ajodo.2004.01.024. [DOI] [PubMed] [Google Scholar]
- 3.Rambhia S, Heshmati R, Dhuru V, et al. Shear bond strength of orthodontic brackets bonded to provisional crown materials utilizing two different adhesives. Angle Orthod. 2009;79:784–789. doi: 10.2319/060908-298.1. [DOI] [PubMed] [Google Scholar]
- 4.Maryanchik I, Brendlinger EJ, Fallis DW, et al. Shear bond strength of orthodontic brackets bonded to various esthetic pontic materials. Am J Orthod Dentofacial Orthop. 2010;137:684–689. doi: 10.1016/j.ajodo.2008.06.031. [DOI] [PubMed] [Google Scholar]
- 5.Blakey R, Mah J. Effects of surface conditioning on the shear bond strength of orthodontic brackets bonded to temporary polycarbonate crowns. Am J Orthod Dentofacial Orthop. 2010;138:72–78. doi: 10.1016/j.ajodo.2008.08.030. [DOI] [PubMed] [Google Scholar]
- 6.Minick GT, Oesterle LJ, Newman SM, et al. Bracket bond strengths of new adhesive systems. Am J Orthod Dentofacial Orthop. 2009;135:771–776. doi: 10.1016/j.ajodo.2007.06.021. [DOI] [PubMed] [Google Scholar]
- 7.Mackay F. The effect of adhesive type and thickness on bond strength of orthodontic brackets. Br J Orthod. 1992;19:35–39. doi: 10.1179/bjo.19.1.35. [DOI] [PubMed] [Google Scholar]
- 8.Yamamoto A, Yoshida T, Tsubota K, et al. Orthodontic bracket bonding: enamel bond strength vs time. Am J Orthod Dentofacial Orthop. 2006;130:e431–e436. doi: 10.1016/j.ajodo.2006.03.024. [DOI] [PubMed] [Google Scholar]
- 9.Bishara SE, Ostby AW, Laffoon JF, et al. Shear bond strength comparison of two adhesive systems following thermocycling. A new self-etch primer and a resin-modified glass ionomer. Angle Orthod. 2007;77:337–341. doi: 10.2319/0003-3219(2007)077[0337:SBSCOT]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 10.ISO TR 11405. Guidance on Testing on Adhesion on Tooth Structure. Geneva, Switzerland: International Organization for Standardization; 2003. [Google Scholar]
- 11.Stanford SK, Wozniak WT, Fan PL. The need for standardization of test protocols. Semin Orthod. 1997;3:206–209. doi: 10.1016/s1073-8746(97)80071-0. [DOI] [PubMed] [Google Scholar]
- 12.Eliades T, Brantley WA. The inappropriateness of conventional orthodontic bond strength assessment protocols. Eur J Orthod. 2000;22:13–23. doi: 10.1093/ejo/22.1.13. [DOI] [PubMed] [Google Scholar]
- 13.Eliades T, Katsavrias E, Zinelis S, et al. Effect of loading rate on bond strength. J Orofac Orthop. 2004;65:336–342. doi: 10.1007/s00056-004-0327-x. [DOI] [PubMed] [Google Scholar]
- 14.Reynolds I. A review of direct orthodontic bonding. Br J Orthod. 1975;18:171–178. [Google Scholar]
- 15.Whitlock BO, III, Eick JD, Ackerman RJ, Jr, et al. Shear strength of ceramic brackets bonded to porcelain. Am J Orthod Dentofacial Orthop. 1994;106:358–364. doi: 10.1016/S0889-5406(94)70056-7. [DOI] [PubMed] [Google Scholar]
- 16.Moseley HC, Horrocks EN, Pearson GJ, et al. Effects of cyclic stressing on attachment bond strength using glass ionomer cement and composite resin. Br J Orthod. 1995;22:23–27. doi: 10.1179/bjo.22.1.23. [DOI] [PubMed] [Google Scholar]
- 17.Kandil SH, Kamar AA, Shaaban SA, et al. Effect of temperature and ageing on the mechanical properties of dental polymeric composite materials. Biomaterials. 1989;10:540–544. doi: 10.1016/0142-9612(89)90059-8. [DOI] [PubMed] [Google Scholar]
- 18.Matasa CG. Microbial attack of orthodontic adhesives. Am J Orthod Dentofacial Orthop. 1995;108:132–141. doi: 10.1016/s0889-5406(95)70075-7. [DOI] [PubMed] [Google Scholar]
- 19.Hajrassie MK, Khier SE. In-vivo and in-vitro comparison of bond strengths of orthodontic brackets bonded to enamel and debonded at various times. Am J Orthod Dentofacial Orthop. 2007;131:384–390. doi: 10.1016/j.ajodo.2005.06.025. [DOI] [PubMed] [Google Scholar]
- 20.Murray SD, Hobson RS. Comparison of in vivo and in vitro shear bond strength. Am J Orthod Dentofacial Orthop. 2003;123:2–9. doi: 10.1067/mod.2003.49. [DOI] [PubMed] [Google Scholar]
- 21.Haselton DR, Diaz-Arnold AM, Vargas MA. Flexural strength of provisional crown and fixed partial denture resins. J Prosthet Dent. 2002;87:225–228. doi: 10.1067/mpr.2002.121406. [DOI] [PubMed] [Google Scholar]
- 22.Diaz-Arnold AM, Dunne JT, Jones AH. Microhardness of provisional fixed prosthodontic materials. J Prosthet Dent. 1999;82:525–528. doi: 10.1016/s0022-3913(99)70050-8. [DOI] [PubMed] [Google Scholar]
- 23.Fox NA, McCabe JF, Buckley JG. A critique of bond strength testing in orthodontics. Br J Orthod. 1994;21:33–43. doi: 10.1179/bjo.21.1.33. [DOI] [PubMed] [Google Scholar]
- 24.Sideridou I, Achilias DS, Kyrikou E. Thermal expansion characteristics of light-cured dental resins and resin composites. Biomaterials. 2004;25:3087–3097. doi: 10.1016/j.biomaterials.2003.09.078. [DOI] [PubMed] [Google Scholar]
- 25.Kuntman A, Baysal B. Estimation of thermodynamic parameters for poly(ethyl methacrylate)/isopropyl alcohol system from intrinsic viscosity measurements. Polymer. 1993;34:3723–3726. [Google Scholar]
- 26.Artun J, Bergland S. Clinical trials with crystal growth conditioning as an alternative to acid-etch enamel pretreatment. Am J Orthod. 1984;85:333–340. doi: 10.1016/0002-9416(84)90190-8. [DOI] [PubMed] [Google Scholar]
- 27.Kitahara-Ceia FM, Mucha JN, Marques dos Santos PA. Assessment of enamel damage after removal of ceramic brackets. Am J Orthod Dentofacial Orthop. 2008;134:548–555. doi: 10.1016/j.ajodo.2006.08.022. [DOI] [PubMed] [Google Scholar]
- 28.Bell TA., Jr Light-cured composite veneers for provisional crowns and fixed partial dentures. J Prosthet Dent. 1989;61:266–267. doi: 10.1016/0022-3913(89)90125-x. [DOI] [PubMed] [Google Scholar]