Abstract
Objective:
To determine the treatment effects of the Xbow appliance on the upper airway dimensions and volume using cone-beam computed tomography (CBCT); to evaluate the cephalometric changes in the skeletal and dental structures of the skeletal Class II patients.
Materials and Methods:
The sample consisted of 25 Class II patients (11 male, 14 female) with a mean age of 11.1 ± 1.1 years. CBCT images were obtained at the beginning of the treatment (T0) and after the debonding of the Xbow (T1).
Results:
Changes in superior, middle, and inferior parts of the oropharynx in the retroglossal region and changes in the oropharyngeal airway volume were statistically significant (P < .05, P < .01). The differences favoring the Xbow for the changes in the direction of Class II correction included SNA, SNB, ANB, maxillary depth angles, and point A-NPg and Co-B distances. Data of the dental parameters showed palatal tipping and extrusion of the maxillary incisors, labial tipping of the mandibular incisors, and mesial movement and extrusion of the mandibular molars.
Conclusions:
Treatment with the Xbow appliance in Class II patients resulted in favorable increase in the oropharyngeal airway dimensions and volume. Further studies with larger study samples and with control groups are needed.
Keywords: Crossbow, Xbow, CBCT, Upper airway, Class II division 1 malocclusion
INTRODUCTION
Class II malocclusion is a common orthodontic problem that can be treated by different approaches and appliances according to the existing anteroposterior discrepancy and the age and cooperation of the patient.1,2 When the malocclusion is caused by mandibular retrusion, functional appliances are used for the stimulation of the mandibular growth and control of the direction of maxillary and mandibular alveolar development.3 Among the available Class II correctors, fixed options have been gaining popularity. To date, many authors4–12 have evaluated the effects of different types of fixed functional appliances and reported that Class II malocclusion was corrected by a combination of skeletal and dental modifications.
Recently, the Crossbow (Xbow) appliance has been introduced for the treatment of patients with Class II malocclusions.13 In clinical practice, the treatment stages for Xbow13 application are: (1) maxillary expansion in cases of relative maxillary construction; (2) segmental leveling of upper incisors, if required; (3) activation of Forsus4 fatigue resistant device springs; (4) overcorrection until the half-cusp Class III relation of upper premolar and molars; and (5) removal of the springs and a retention phase to allow some musculoskeletal and dental relapse.
Various researchers have emphasized the relationship between pharyngeal, dentofacial, and craniofacial structures14–16 and compared the airway dimensions of patients with different malocclusions and those with normal respiratory functions.17–20 There are a few studies21–25 reporting the effects of Class II functional appliances on the upper airway with conventional radiographic methods. The introduction of cone-beam computed tomography (CBCT) has enabled three-dimensional examination of the airway, with the further benefit of low radiation dose.26
The aims of this prospective study were to evaluate the changes on the upper airway dimension and volume in patients with Class II maloclussion treated with the Xbow appliance and to determine the cephalometric changes in the skeletal and dental structures with the use of CBCT.
MATERIALS AND METHODS
The sample consisted of 25 subjects (14 female, 11 male) referred to the Department of Orthodontics. The average age at the beginning of the treatment was 11.1 ± 1.1 years (range 9.1–12.5 years). A summary of the treatment sample characteristics is given in Table 1. All patients and parents were informed about the orthodontic treatment and signed an informed consent. The institutional ethical review board approved the protocol used (registration LUT 12/10). Because of ethical reasons, a control group of untreated individuals with the same age could not be used.
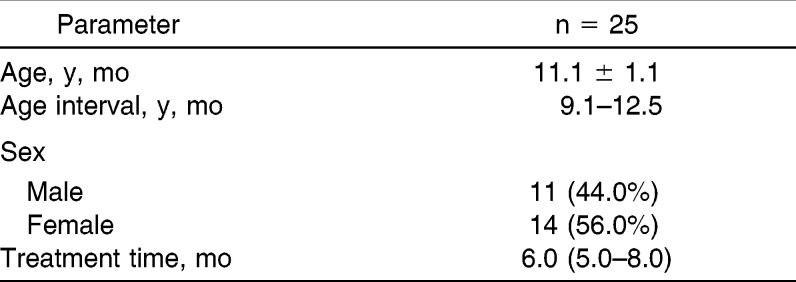
Table 1.
Summary Statistics for the Cases
The inclusion criteria included (1) skeletal Class II malocclusion with mandibular retrusion, (2) late mixed or permanent dentition period, (3) prepeak or peak pubertal growth stage, and (4) overjet of 5 mm or more. Exclusion criteria included (1) congenital craniofacial deformities and (2) history of obstructive sleep apnea and snoring. Intraoral and extraoral photographs, dental models, and CBCT images were all obtained from the subjects at the beginning of the treatment (T0) and after debonding of the Xbow (T1).
The treatment protocol begins with maxillary expansion for constricted arches or in cases of relative maxillary construction. After maxillary expansion, the lower arch and locks were positioned and Forsus springs were inserted bilaterally. The springs were activated every 6 weeks until the maxillary first premolars and molars were in an overcorrected half-cusp Class III relationship. Then, the springs were removed, and the Xbow framework was left in place for 1 to 2 months to monitor the physiologic adaptation.
All CBCT images were taken with Iluma Cone Beam CT scanner (3M IMTEC, Ardmore, Okla) in natural head and maximum intercuspal position at 3.8 mA, 120 kV, and 19 × 24 field-of-view setting. Because of the lack of reproducibility of the tongue position, the patients were asked not to swallow during the scanning time. The images were viewed with the Quick Ceph Studio program (Quick Ceph System, San Diego, Calif), and lateral cephalometric and panoramic radiographs were obtained. All of the cephalometric radiographs were traced digitally with the Quick Ceph Studio program. Nine angular and 17 linear skeletal and dental variables were measured (Figure 1). For the upper airway analysis, seven linear measurements were measured cephalometrically (Figure 2).
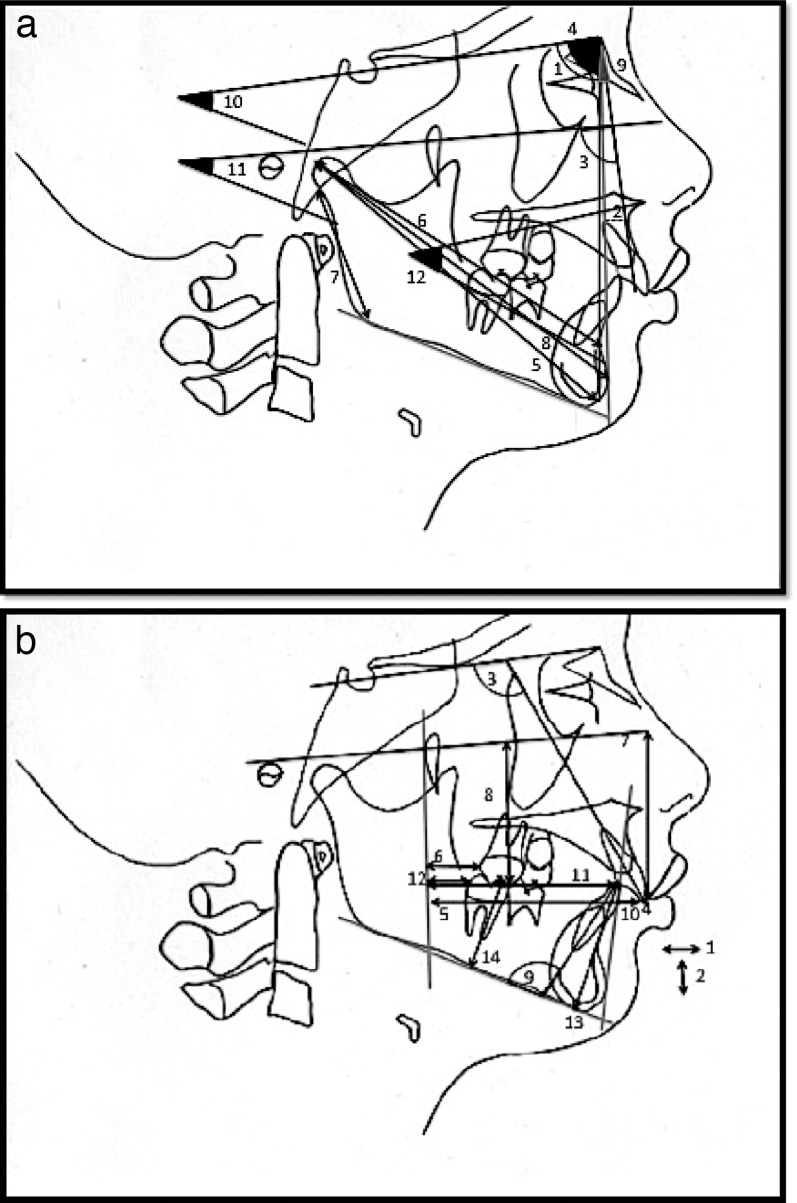
Figure 1.
(a) Skeletal cephalometric measurements. 1. SNA: angle between the maxilla and the cranial base; 2. A-NPg: the distance between point A and NPg; 3. maxillary depth: angle between NA and Frankfort horizontal; 4. SNB: angle between the mandible and the cranial base; 5. Co-Gn: mandibular length between points Co and Gn; 6. Co-B: mandibular length between points Co and B; 7. Ar-Go: mandibular ramus height; 8. Co-Pg: mandibular length between points Co and Pg; 9. ANB: angle between the maxilla and mandible; 10. GoGnSN: angle between mandibular plane and SN; 11. FMA: angle between mandibular plane and Frankfort horizontal; and 12. ANS-Xi-Pm: lower facial height. (b) Dental cephalometric measurements. 1. overjet: horizontal overlap between upper and lower incisors; 2. overbite: vertical overlap between upper and lower incisors; 3. U1-SN: upper incisor inclination related to cranial base; 4. U1-APg: upper incisor inclination related to APg line; 5. U1-PTV: the distance between the tip of the upper incisor and PTV; 6. U6-PTV: the distance between the most distal point of the distal contour of the upper molar and PTV; 7. U1-FH: the distance between the tip of the upper incisor and the Frankfort horizontal; 8. U6-FH: the distance between the tip of the mesiobuccal cusp of the upper molar and the Frankfort horizontal; 9. IMPA: lower incisor inclination related to mandibular plane; 10. L1-APg: lower incisor inclination related to APg line; 11. L1-PTV: the distance between the tip of the lower incisor and PTV; 12. L6-PTV: the distance between the most distal point of the distal contour of the lower molar and PTV; 13. L1-GoMe: the distance between the tip of the lower incisor and mandibular plane; and 14. L6-GoMe: the distance between the tip of the mesiobuccal cusp of the lower molar and the mandibular plane.
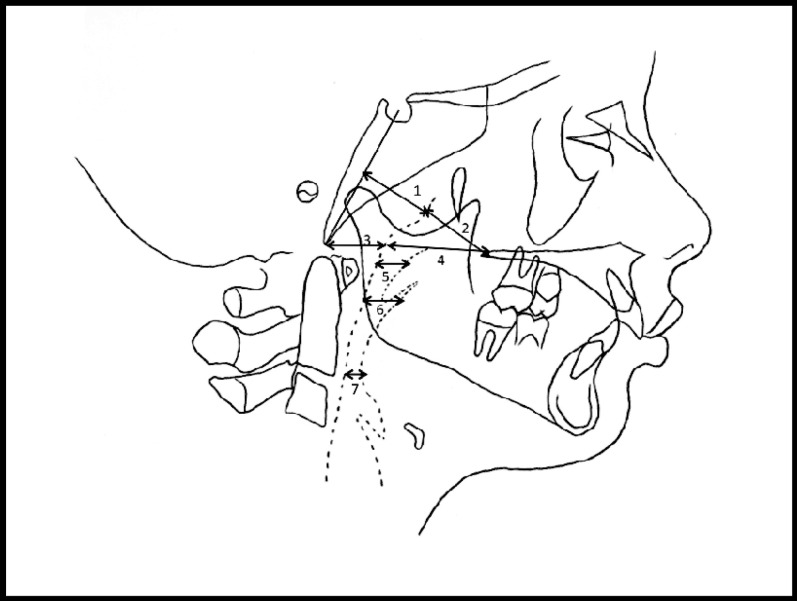
Figure 2.
Cephalometric measurements of the upper airway. 1. AD2-H; 2. PNS-AD2; 3. AD1-Ba; 4. PNS-AD1; 5. SPS (superior pharyngeal space); 6. MPS (middle pharyngeal space); and 7. IPS (inferior pharyngeal space).
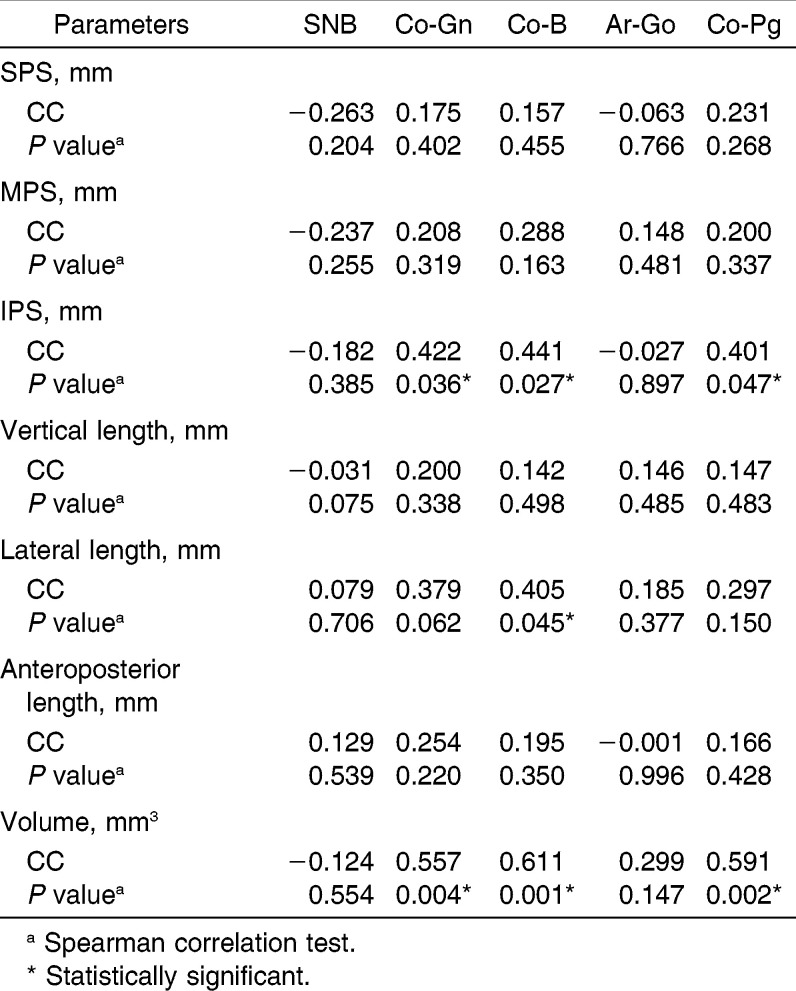
The ITK-SNAP 2.2.0 program (www.itksnap.org) was used to render the oropharynx. The defined region was the part of the pharynx that is between the palatal plane (ANS-PNS) extending to the posterior wall of the pharynx and the plane parallel to the palatal plane that passes from the most anteroinferior point of the second cervical vertebrae.27,28
After the segmentation process, the threshold value was set to between −587 and −1000 HU (Hounsfield unit) to obtain only the desired region's image, and the program measured the final oropharyngeal volume. In addition to this volumetric measurement, the vertical length of the oropharynx and the anteroposterior and lateral dimensions of the retroglossal area were measured on the midsagittal and axial slices, respectively (Figures 3 and 4).
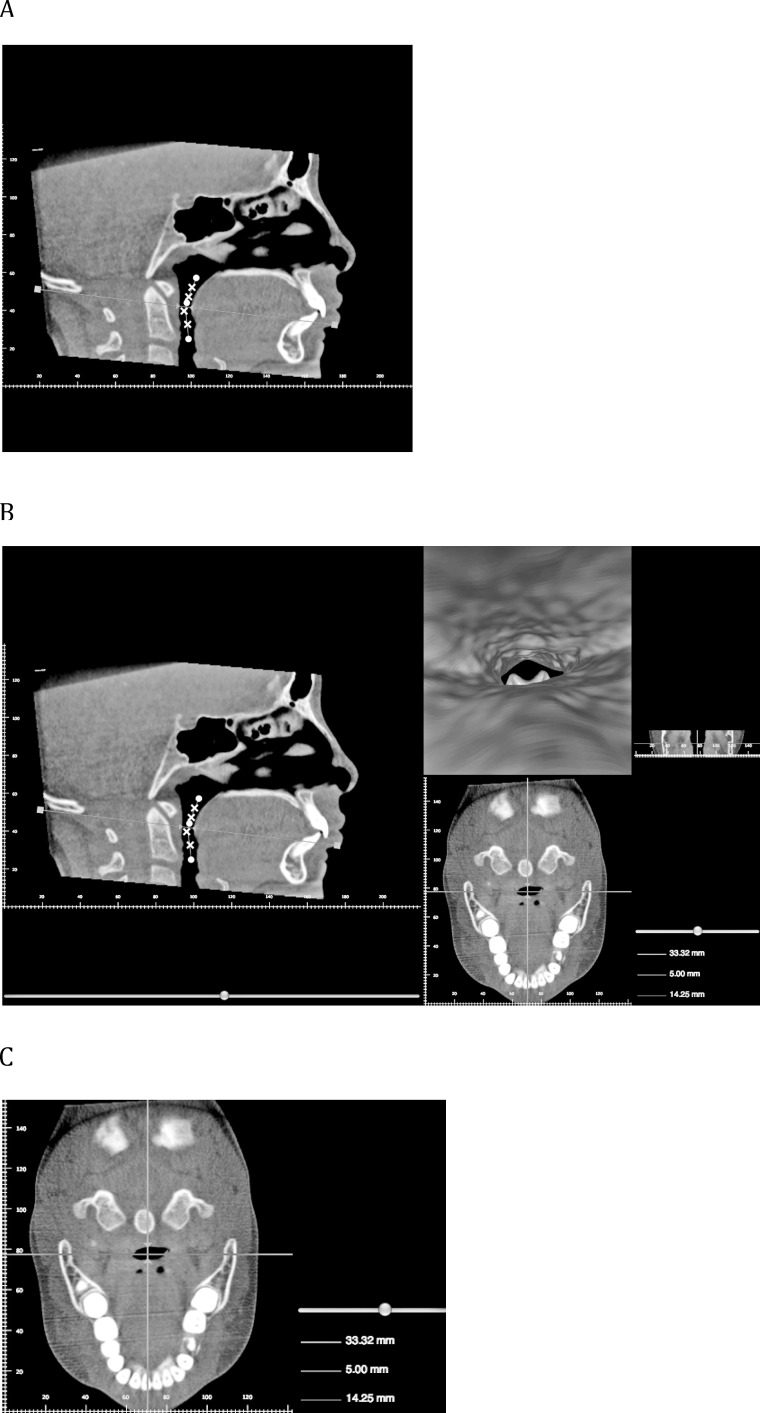
Figure 3.
(A) Oropharyngeal length. (B) Sagittal view: retroglossal region. (C) Axial view: anteroposterior and lateral dimensions of the retroglossal region.
Figure 4.
Segmentation process and final oropharyngeal airway volume.
SPSS (SPSS Inc, Chicago, IL, USA) software (for Windows 11.5) was used for all statistical analysis. To test whether the distribution of continuous variables came close to normal was investigated by the Shapiro-Wilk test. Descriptive statistics were displayed as mean ± standard deviation or median for continuous variables and as number of cases and percentages for nominal variables. The reproducibility of pretreatment and posttreatment measurements was evaluated by calculation of the intraclass correlation coefficient and 95% confidence intervals. The significance of the difference of mean values after treatment was investigated by dependent t-test. The changes in median values were determined by Wilcoxon signed rank test. To check the correlations between mandibular cephalometric variables and upper airway measurements, the Spearman correlation was performed. The statistical significance was set at .05.
RESULTS
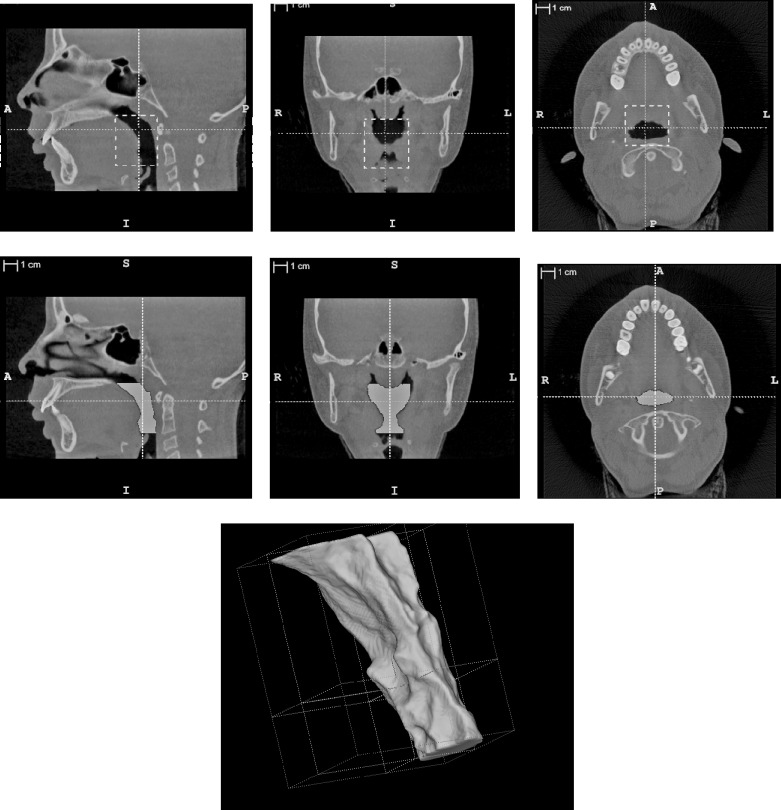
The results of the upper airway analysis and the significance of the changes are presented in Table 2. The superior pharyngeal space (SPS), middle pharyngeal space (MPS) and inferior pharyngeal space (IPS) were increased by 0.87 mm, 1.3 mm, and 1.4 mm, respectively (P < .05). The results of the measurements performed on the CBCT data indicated that all parameters increased significantly except the vertical length of oropharynx (P < .05). The anteroposterior and lateral dimensions of the retroglossal region on the axial slice were increased by 1.9 mm (P < .05) and 1.5 mm (P < .001), respectively. There was a statistically significant increase in the volume of the oropharyngeal airway after the Xbow application (1744 mm3, P < .001).
Table 2.
Cephalometric Parameters of the Upper Airway
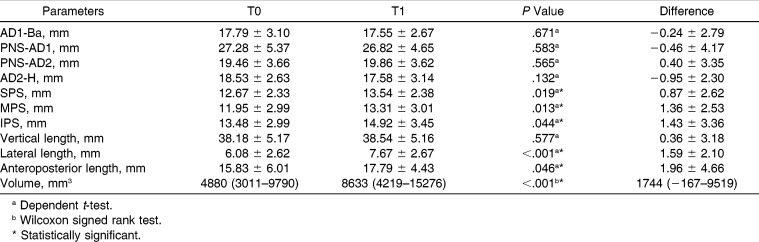
The cephalometric measurements for the dentoskeletal changes before and after application of the Xbow and the significance of these changes are shown in Table 3. The skeletal effect on maxilla was diminution of SNA and maxillary depth angles (P < .05) and point A-NPg distance (P < .001). The mandible was positioned anteriorly with a consequent decrease in ANB angle (P < .001). The increases in Co-B and Ar-Go were found to be statistically significant (P < .05). The GoGnSN, FMA, and ANS-Xi-Pm angles remained unchanged during the treatment (P > .05).
Table 3.
Cephalometric Variables of Pretreatment (T0), Posttreatment (T1), and T1-T0
The dental parameter data showed palatal tipping and extrusion of the maxillary incisors, labial tipping of the mandibular incisors, and mesial movement and extrusion of the mandibular molars. Significant distal tipping and intrusion of the maxillary molars were not observed (P > .05); however, mesial movement of the maxillary molars was inhibited.
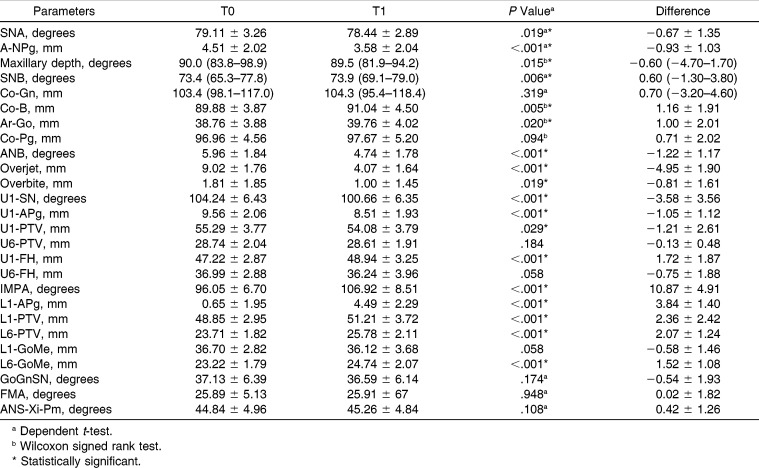
Spearman correlation coefficients between the cephalometric parameters of the oropharyngeal airway and the cephalometric variables of the mandible are presented in Table 4. Co-Gn, Co-B, and Co-Pg showed a positive correlation with IPS (P < .05). The lateral length of the retroglossal area showed a positive correlation with Co-B (P < .05). The oropharyngeal airway volume showed a positive correlation with Co-Gn, Co-B, and Co-Pg (P < .05).
Table 4.
Spearman Correlation Coefficients (CC) Between the Cephalometric Variables of the Mandible and the Parameters of the Oropharyngeal Airway
DISCUSSION
There are a few studies21–25 reporting the effects of functional appliances used in the treatment of Class II malocclusions on the upper airway; however, these studies evaluated the airway dimensions by using conventional radiographic methods. Conventional radiographic methods are two-dimensional reflections of three-dimensional structures, and overlapping of anatomic structures can be misleading. For this reason, in recent years computed tomography (CT) imaging is often used to evaluate craniofacial structures and to obtain information about the anatomy of the airway. This study was undertaken to evaluate the effects of the Xbow appliance treatment on the upper airway dimensions with the use of CBCT and to determine the skeletal and dental changes after treatment.
According to the results of this study, the Xbow application restricted the maxillary forward growth and directed it posteriorly. Higgins13 and Flores-Mir et al.29 defined the effects of the Xbow on the maxilla as the headgear effect. This effect was also noted in other nonprotrusive interarch Class II correctors.5–10 The finding of this study pertaining to the SNB angle was comparable with the values in the studies by Karacay et al.,6 Weiland and Bantleon,11 Heinig and Göz,4 and Stucki and Ingervall.30
On the other hand, Flores-Mir et al.,29 Cope et al.,7 and Covell et al.9 did not find significant changes in the position of the mandible. This contradiction might be due to differences in the pubertal development stages of the patients included.
No significant increase in the mandibular length was observed in our sample, except for Co-B and Ar-Go measurements. This finding is in agreement with the studies of the Jasper Jumper.7,9,10 On the other hand, the studies of Karacay et al.,6 Weiland and Bantleon,11 and Aras et al.12 showed significant increases in the mandibular length. This contradiction could be due to the differences between the inclusion criteria, reference points used to measure the mandibular growth, age of patients, and total duration of the treatment. Although limited for the lower jaw, skeletal changes with the use of the Xbow were observed in the maxilla and the mandible; therefore, the ANB angle decreased significantly. This finding is compatible with those of previous Xbow studies.29,31
The dentoalveolar changes obtained in this study were nearly the same as those of previous studies with fixed functional appliances.4,6,10,12,29,31 The findings that are controversial with respect to previous studies were the distal tipping and extrusion of the upper molars and intrusion of the lower incisors. In accordance with our findings, Aras et al.12 and Franchi et al.5 stated that the distal movement and intrusion of the upper molars were not statistically significant. The differences may be due to differences between the reference planes used to determine the amount of distalization and the eruption stages of the upper second molars.
Previous studies with the fixed functional appliances have reported that the GoGnSN angle was maintained stable.4,6,9–12,30 Likewise, our results showed that the angles that determine the vertical skeletal development remained almost unchanged.
In this study, we analyzed the effects of the Xbow application on the upper airway dimensions by using the cephalometric points and lines that were used in many other recent studies.17,32 The cephalometric results of this study showed a significant increase in superior, middle, and inferior parts of the oropharyngeal airway. However, the nasopharyngeal airway size and thickness of adenoids were not affected by the Xbow treatment. Previous studies reported that patients with a skeletal Class II malocclusion tended to have a smaller airway width than subjects with a normal anteroposterior skeletal relationship.18,20,28 Therefore, it can be concluded that the anterior position of the retrognathic mandible might affect the airway size positively. Ozbek et al.21 reported significant increase in the pharyngeal airway size with activator treatment in skeletal Class II cases. Hanggi et al.22 compared the effects of activator and headgear treatments on the upper airway dimensions with a control sample and found the increases in pharyngeal area, pharyngeal length, and minimum area between tongue and posterior pharyngeal wall to be statistically significant. Godt et al.23 and Yassaei et al.24 noted significant increases in oropharyngeal width and area with functional appliance treatment in Class II cases. Page25 stated that functional jaw orthopedics could be a useful treatment alternative for patients who have narrow airway sizes. The changes in airway dimension with the mandibular advancement were related to the anterior reposition of the soft palate. Also, expansion of the transverse airway width with the mandibular advancement was related to the anterior movement of hyoid bone.27,33
The anteroposterior and lateral lengths of the retroglossal area were increased by 1.9 mm and 1.5 mm, respectively. Haskell et al.33 used CBCT to evaluate the changes in upper airway size and volume after mandibular advancement with acrylic splint Herbst appliance. They reported an average increase of 2800 mm3 after treatment. In accordance with their results, we found a 1744 mm3 increase in oropharyngeal airway volume.
Significant correlations were observed between oropharyngeal and mandibular measurements. These positive correlations showed that changes in mandibular length may affect the oropharyngeal region.
As a result of the anterior repositioning of the mandible with the Xbow appliance, an increase in the oropharyngeal airway volume was observed. Therefore, it is thought that the application of the Xbow appliance in patients with Class II malocclusion due to mandibular retrusion may have a positive contribution to prevent developing sleep and breathing disorders. However, to determine the positive effect on the upper airway, further studies with larger study samples, other age groups, or other appliances are needed.
CONCLUSIONS
Treatment with the Xbow appliance in Class II patients resulted in favorable dental and skeletal changes in the direction of a Class II correction.
In cephalometric and three-dimensional evaluation of the upper airway, increase in the oropharyngeal airway dimensions and volume was observed. There were no changes in the nasopharyngeal region and adenoid tissues.
REFERENCES
- 1.McNamara JA., Jr Components of class II malocclusion in children 8–10 years of age. Angle Orthod. 1981;51:177–202. doi: 10.1043/0003-3219(1981)051<0177:COCIMI>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 2.Coben SE. The biology of Class II treatment. Am J Orthod. 1971;59:470–487. doi: 10.1016/0002-9416(71)90083-2. [DOI] [PubMed] [Google Scholar]
- 3.Bishara SE. Textbook of Orthodontics 1st ed. Philadelphia, Pa: Saunders Company; 2001. [Google Scholar]
- 4.Heinig N, Göz GR. Clinical application and effects of the Forsus spring. A study of new Herbst hybrid [in English, German] J Orofac Orthop. 2001;6:436–450. doi: 10.1007/s00056-001-0053-6. [DOI] [PubMed] [Google Scholar]
- 5.Franchi L, Alvetro L, Giuntini V, Masucci C, Defraia E, Baccetti T. Effectiveness of comprehensive fixed appliance treatment used with the Forsus Fatigue Resistant Device in class II patients. Angle Orthod. 2011;81:678–683. doi: 10.2319/102710-629.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Karacay S, Akin E, Olmez H, Gurton AU, Sagdic D. Forsus Nitinol Flat Spring and Jasper Jumper correctors of Class II division 1 malocclusions. Angle Orthod. 2006;76:666–672. doi: 10.1043/0003-3219(2006)076[0666:FNFSAJ]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 7.Cope JB, Buschang PH, Cope DD, Parker J, Blackwood HO. Quantitative evaluation of craniofacial changes with Jasper Jumper therapy. Angle Orthod. 1994;64:113–122. doi: 10.1043/0003-3219(1994)064<0113:QEOCCW>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 8.Mills CM, McCulloch KJ. Case report: modified use of the Jasper Jumper appliance in a skeletal Class II mixed dentition case requiring palatal expansion. Angle Orthod. 1997;4:277–282. doi: 10.1043/0003-3219(1997)067<0277:CRMUOT>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 9.Covell DA, Trammell DW, Boero RP, West R. A cephalometric study of Class II division 1 malocclusions treated with the Jasper Jumper appliance. Angle Orthod. 1999;69:311–320. doi: 10.1043/0003-3219(1999)069<0311:ACSOCI>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 10.Nalbantgil D, Arun T, Sayinsu K, Fulya I. Skeletal, dental and soft-tissue changes induced by the Jasper jumper appliance in late adolescence. Angle Orthod. 2005;75:426–436. doi: 10.1043/0003-3219(2005)75[426:SDASCI]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 11.Weiland FJ, Bantleon HP. Treatment of Class II malocclusions with the Jasper Jumper appliance—a preliminary report. Am J Orthod Dentofacial Orthop. 1995;108:341–350. doi: 10.1016/s0889-5406(95)70031-5. [DOI] [PubMed] [Google Scholar]
- 12.Aras A, Ada E, Saracoglu H, Gezer NS, Aras I. Comparison of treatments with the Forsus fatigue resistant device in relation to skeletal maturity: a cephalometric and magnetic resonance imaging study. Am J Orthod Dentofacial Orthop. 2011;140:616–625. doi: 10.1016/j.ajodo.2010.12.018. [DOI] [PubMed] [Google Scholar]
- 13.Higgins DW. Crossbow appliance (Xbow) Available at: http://www.crossboworthodontic.com Accessed October 30, 2012. [Google Scholar]
- 14.Linder-Aronson S, Leighton BC. A longitudinal study of the development of the posterior nasopharyngeal wall between 3 and 16 years of age. Eur J Orthod. 1983;5:47–58. doi: 10.1093/ejo/5.1.47. [DOI] [PubMed] [Google Scholar]
- 15.McNamara JA. Influence of respiratory pattern on craniofacial growth. Angle Orthod. 1981;51:269–300. doi: 10.1043/0003-3219(1981)051<0269:IORPOC>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 16.Behlfelt K, Linder-Aronson S, McWilliam J, Neander P, Laage-Hellman J. Dentition in children with enlarged tonsils compared to control children. Eur J Orthod. 1989;11:416–429. doi: 10.1093/oxfordjournals.ejo.a036014. [DOI] [PubMed] [Google Scholar]
- 17.Zhong Z, Yang Z, Gao X, Zeng XL. A comparison study of upper airway among different skeletal craniofacial patterns in nonsnoring Chinese children. Angle Orthod. 2010;80:267–274. doi: 10.2319/030809-130.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kirjavainen M, Kirjavainen T. Upper airway dimensions in Class II malocclusion. Angle Orthod. 2007;77:1046–1053. doi: 10.2319/081406-332. [DOI] [PubMed] [Google Scholar]
- 19.Mergen DC, Jacobs RM. The size of nasopharynx associated with normal occlusion and Class II malocclusion. Angle Orthod. 1970;40:342–346. doi: 10.1043/0003-3219(1970)040<0342:TSONAW>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 20.Trenouth MJ, Timms DJ. Relationship of the functional oropharynx to craniofacial morphology. Angle Orthod. 1999;69:419–423. doi: 10.1043/0003-3219(1999)069<0419:ROTFOT>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 21.Ozbek M, Memikoglu TU, Gögen H, Lowe AA, Baspinar E. Oropharyngeal airway dimensions and functional orthopedic treatment in skeletal Class II cases. Angle Orthod. 1998;68:327–336. doi: 10.1043/0003-3219(1998)068<0327:OADAFO>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 22.Hanggi MP, Teuscher UM, Ross M, Peltomaki TA. Long-term changes in pharyngeal airway dimensions following activator-headgear and fixed appliance treatment. Eur J Orthod. 2008;30:598–605. doi: 10.1093/ejo/cjn055. [DOI] [PubMed] [Google Scholar]
- 23.Godt A, Koos B, Hagen H, Göz G. Changes in upper airway width associated with Class II treatments (headgear vs activator) and different growth patterns. Angle Orthod. 2011;81:440–446. doi: 10.2319/090710-525.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yassaei S, Bahrololoomi Z, Sorush M. Changes of tongue position and oropharynx following treatment with functional appliance. J Clin Pediatr Dent. 2007;31:287–290. doi: 10.17796/jcpd.31.4.lp479v346345460g. [DOI] [PubMed] [Google Scholar]
- 25.Page DC. The new dental-medical renaissance. Medically efficacious functional jaw orthopedics. Funct Orthod. 1999;16 [PubMed] [Google Scholar]
- 26.Kau CH, Richmond S, Palomo JM, Hans MG. Three-dimensional cone beam computerized tomography in orthodontics. J Orthod. 2005;32:282–293. doi: 10.1179/146531205225021285. [DOI] [PubMed] [Google Scholar]
- 27.Ogawa T, Enciso R, Memon A, Mah JK, Clark GT. Westwood JD. Medicine Meets Virtual Reality 13 The Magical Next Becomes the Medical Now Vol 111 2005/02/19 ed. Amsterdam, The Netherlands: IOS Press; 2005. Evaluation of 3D airway imaging of obstructive sleep apnea with cone-beam computed tomography; pp. 365–368. [PubMed] [Google Scholar]
- 28.El H, Palomo JM. Airway volume for different dentofacial skeletal patterns. Am J Orthod Dentofacial Orthop. 2011;139:e511–e521. doi: 10.1016/j.ajodo.2011.02.015. [DOI] [PubMed] [Google Scholar]
- 29.Flores-Mir C, Barnett G, Higgins DW, Heo G, Major PW. Short-term skeletal and dental effects of the Xbow appliance as measured on lateral cephalograms. Am J Orthod Dentofacial Orthop. 2009;136:822–832. doi: 10.1016/j.ajodo.2008.01.021. [DOI] [PubMed] [Google Scholar]
- 30.Stucki N, Ingervall B. The use of the Jasper Jumper for the correction of Class II malocclusion in the young permanent dentition. Eur J Orthod. 1998;20:271–281. doi: 10.1093/ejo/20.3.271. [DOI] [PubMed] [Google Scholar]
- 31.Miller RA, Flores-Mir C. Incisor inclination changes produced by two compliance-free Class II correction protocols for the treatment of mild to moderate Class II malocclusions. Angle Orthod. 2012 Oct 3 [Epub ahead of print] doi: 10.2319/062712-528.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lin YC, Lin HC, Tsai HH. Changes in the pharyngeal airway and position of the hyoid bone after treatment with a modified bionator in growing patients with retrognathia. Journal of LExperimenal & Clinical Medicine. 2011;3:93–98. [Google Scholar]
- 33.Haskell JA, McCrillis J, Haskell BS, Scheetz JP, Scarfe WC, Farman AG. Effects of mandibular advancement device (MAD) on airway dimensions assessed with cone-beam computed tomography. Semin Orthod. 2009;15:132–158. [Google Scholar]