Abstract
Objective:
To compare the treatment effects between skeletal anchored facemask (SAFM) and tooth-borne facemask (TBFM) on different maturation stages and vertical skeletal patterns.
Materials and Methods:
In this retrospective study, 28 patients who were treated with TBFM treatment and 19 patients who were treated with SAFM were reviewed. Cephalograms at the beginning and end of facemask application were obtained and assessed. Each treatment group was divided according to skeletal maturity and facial angle type. Nonparametric Mann-Whitney U-test was used for comparisons of maturity stage and vertical skeletal type between the treatment groups.
Results:
SAFM produced a significant increase in the anterior-posterior position of orbitale (SNOr) and A point (N. per. to A). The high mandibular plane angle group of SAFM revealed greater anterior movement than that of TBFM without opening of the mandibular plane. In the SAFM group, the angulation of the maxillary incisors was retroclined at CVM3 compared to CVM4. In the younger group (CVM3), SAFM showed greater changes in the variables of orbitale (2.909°) and maxillary length (5.818 mm), compared to TBFM.
Conclusions:
Compared with the TBFM group, the findings suggest significant advantages for the SAFM group for relative skeletal maturity and vertical skeletal pattern.
Keywords: Tooth-borne facemask, Skeletal anchored facemask
INTRODUCTION
Class III malocclusion during the developing stage is one of the most challenging orthodontic problems. Once patients start orthodontic treatment, including orthopedic intervention, the total treatment time could be extended enough to terminate the remaining skeletal growth. Otherwise, patients might experience relapse and require additional treatment. If a positive overjet can not be obtained or maintained, an alternative treatment option could be surgical intervention.
Protraction of the maxilla with a facemask is a common treatment option for Class III malocclusion with maxillary undergrowth, especially at earlier ages. It augments growth at sutural sites of the maxillary complex by adding separating force to natural growth.1 However, the timing of such treatment is a main concern when using the facemask. Although such interventions are recommended during primary dentition or early mixed dentition stages,1,2 there are opposing opinions regarding the outcomes of using a facemask across age groups.2,3
The advantages of the tooth-borne anchorage facemask (TBFM) are forward movement and counterclockwise rotation of the maxillae, downward and backward rotation of the mandible, increased mandibular plane angle and lower facial height, proclination of the maxillary incisors, and lingual tipping of the mandibular incisors.4–6 However, TBFMs are not without disadvantages, including loss of anchorage by mesial migration of maxillary molars, including other dentoalveolar effects, and the inability to apply the correct orientation of orthopedic forces to the maxilla.
To overcome the disadvantages of a tooth-borne appliance, several innovative designs for absolute anchorage facemasks have been devised. Kokich et al.7 applied extraoral protraction force to deliberately ankylosed deciduous canines. Singer et al.8 used osseointegrated implants in the zygomatic buttress to obtain direct attachment to the maxilla. Hong et al.9 used an onplant on the palatal bone as anchorage for facemask. Currently, miniplates are commonly used for rigid fixation of the bony segments in maxillary surgery, and these have been shown to offer a reliable means of rigid anchorage for applying orthodontic and orthopedic forces. Additionally, the use of mini-implants can avoid dental side effects, in terms of the mesial migration effects of the conventional facemask.10,11 There are two different locations in which anchoring miniplates may be used for the facemask: the lateral nasal wall of the maxilla and the bony surface of the zygomatic buttress. Although the zygomatic buttress can be used for children in the early mixed dentition stage, the lateral nasal wall is more beneficial because of its anatomical location, which is anterior to the center of the nasomaxillary complex.
Several studies11–14 describing outcomes for the skeletal anchored facemask (SAFM) have been published. However, these studies have compared such outcomes among different types of SAFMs. In this study, we compare the treatment outcomes between SAFM and TBFM for maturation stage and vertical skeletal pattern.
MATERIALS AND METHODS
Samples were collected from a private orthodontic clinic in Chunan, South Korea. Twenty-eight patients (seven boys and 21 girls; mean age, 10.09 years; range, 9.0–13.9 years) with TBFM and 19 patients (eight boys and 11 girls; mean age, 11.21 years; range, 9.1–13.0 years) with SAFM were chosen with the following inclusion criteria: overjet greater than −2 mm, no craniofacial deformity, cervical vertebra maturation stage of 3 or 4, and no previous orthodontic treatment or surgery. This study was approved by the institutional review board at Chunan, South Korea.
Subgrouping was accomplished by vertical dimension according to reference values (FMA 26, L.F.H. 47) and by maturation stage (CVM3 and CVM4).15 According to the vertical dimensions, subjects were divided into four groups, as follows: FMH (TBFM with high vertical type), FML (TBFM with low vertical type), SAH (SAFM with high vertical type), and SAL (SAFM with low vertical type). Likewise, subjects were divided into four groups by skeletal maturity: FM3 (TBFM at CVM3 stage), FM4 (TBFM at CVM4 stage), SA3 (SAFM at CVM3 stage), and SA4 (SAFM at CVM4 stage).
In the SAFM group, a minimum of three to four screws was placed to resist the maxillary protraction force. The end of the miniplates is located on the keratinized attached gingiva to prevent possible gingival irritation. Maxillary protraction is started 2–3 weeks after placing the miniplates on both sides. An elastic force of 400–500 g per side is applied. The direction of force is approximately 30° downward to the occlusal plane. Patients are instructed to wear the facemask at all times, except during meals and sports activities.
In the TBFM group, patients were treated with conventional facemasks and had a hyrax palatal expander, which was banded on the maxillary first premolars and first molars with two hooks soldered to each first premolar band. Patients were advised to activate the appliance one or two times per day until the required expansion was achieved (average time, 4–6 weeks), with slight overcorrection of the crossbite. After this process, the expander was stabilized. Patients in this group were instructed to wear the facemask for 12–14 hours a day.
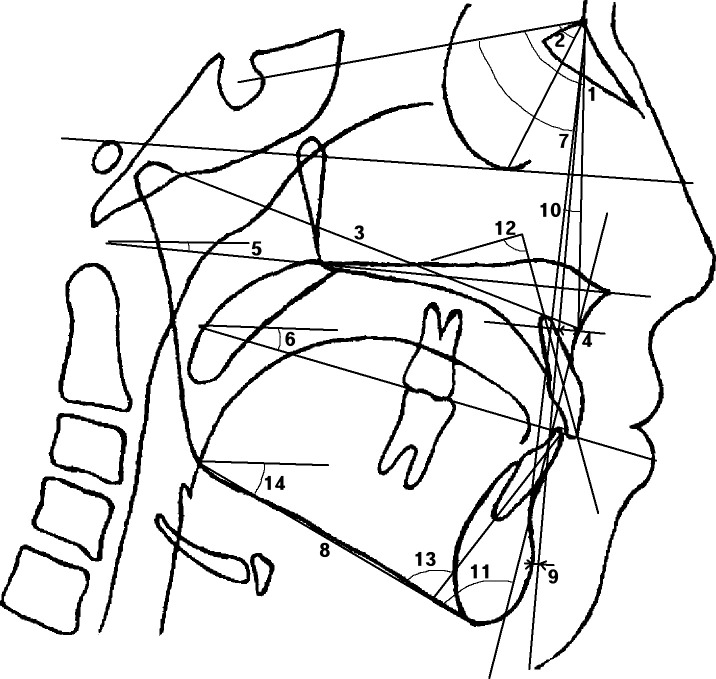
Lateral cephalometric films were obtained at the start of facemask treatment (T1) and at the end of facemask treatment (T2). Cephalometric linear and angular measurements are shown in Figure 1.
Figure 1.
Cephalometric measurements. 1. SNA; 2. SNOr; 3. Mx. length; 4. N. per. to A; 5. Palatal P 6. U. occ. P. to FH; 7. SNB; 8. Mn. length; 9. N. per. to Pog; 10. ANB; 11. A-B to Mn. Pi 12. U1 to SN; 13. IMPA; and 14. FMA.
Statistical analysis
The Kolmogorov-Smirnov test was used to check for normality of the variables. The independent t-test was used to assess differences between TBFM and SAFM group. To assess differences between the subgroups the data were compared using the Mann-Whitney U-test, which is a nonparametric test as a result of its low power, small sample number, and nonnormality.
Ten patients were randomly selected, and their cephalograms were assessed and reassessed 5 weeks later by the same investigator. The intraobserver differences between the two measurements were analyzed by computing the intraclass correlation coefficients, which were found to be 0.95 for the angular measurements and 0.97 for the linear measurements. Statistical analysis was carried out with SPSS PC1 (version 14.0, SPSS, Chicago, Ill) at a significance level of .05.
RESULTS
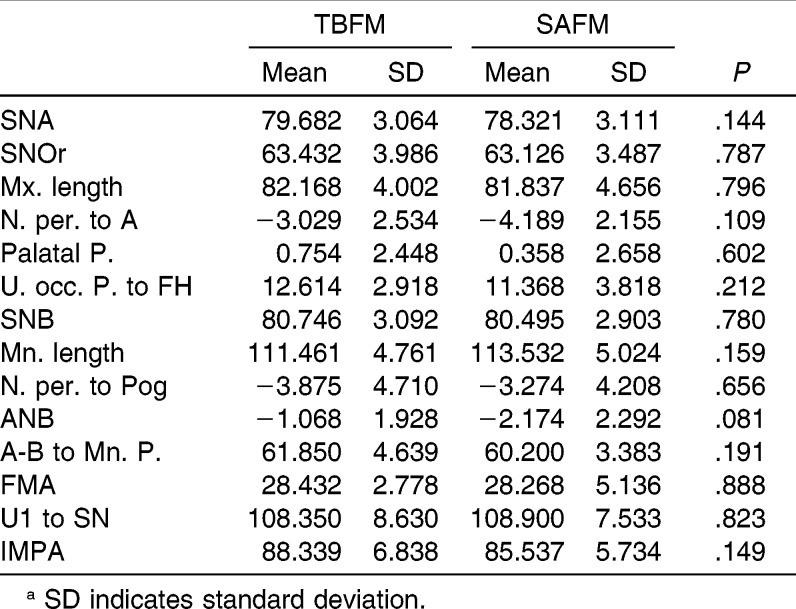
Since both TBFM and SAFM groups were normally distributed, an independent t-test was performed to evaluate the difference between the groups. Table 1 summarizes the comparison of TBFM and SAFM at baseline (Table 1). There were no significant differences in any of the cephalometric measurements between the groups at T1.
Table 1.
Comparison Between Tooth-Borne Facemask (TBFM) and Skeletal Anchored Facemask (SAFM) at Baseline. No Significant Difference Was Observed Between Two Groups (t-Test)a
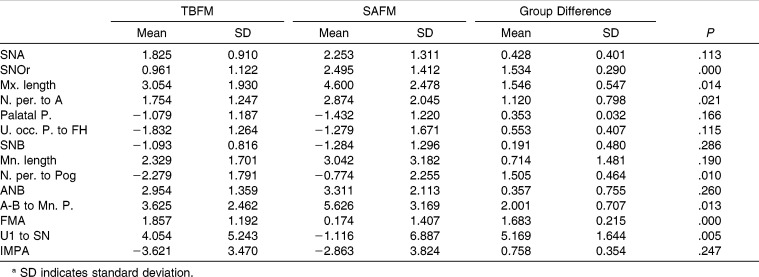
In the after-treatment comparison, Table 2 showed that orbitale point (SNOr) of SAFM group has been displaced more forward (2.495 degrees) compared to TBFM (.0961 degrees). Variables related to A point (Mx. length and N. per. to A) increased significantly in the SAFM group. It was found that FMA, U1 to SN, and maxillary length between the two groups were significantly different.
Table 2.
Treatment Changes Between Tooth-Borne Facemask (TBFM) and Skeletal Anchored Facemask (SAFM). SAFM Shows Significant Changes in the Variables of Maxillary Position. Group Difference Shows the Difference Between TBFM and SAFM Groups. Less Change on Mandibular Plane and Minus Change on Maxillary Incisors Are Statistically Significant (t-Test)a
In the high angle group, the vertical dimension of FMH (FMA, 1.718) compared to that of SAH (FMA, −0.108) showed a negative change. In the after-treatment comparison of dental measurements, the inclination of the maxillary incisors was not significantly different between FMH and SAH. In both high and low vertical skeletal groups, forward movements of orbitale were greater for the SAFM group than for the TBFM group (Table 3).
Table 3.
Treatment Changes Between Tooth-Borne Facemask and Skeletal Anchored Facemask (SAFM) on Different Facial Angle. Anterior Movement of Orbitale Was Prominent in the SAFM on Both Facial Angles. Minus Change in Maxillary Incisors of SAFM Was Observed in the High Facial Angle Comparison (Mann-Whitney U-Test)a
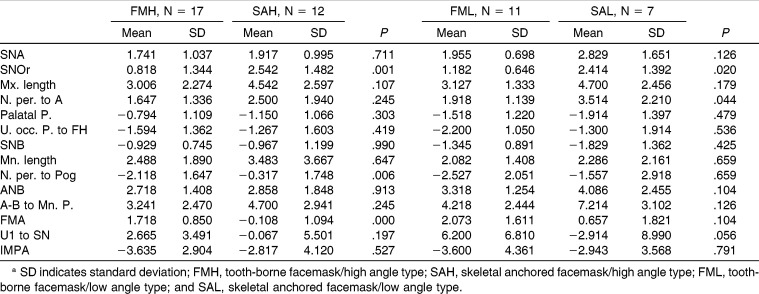
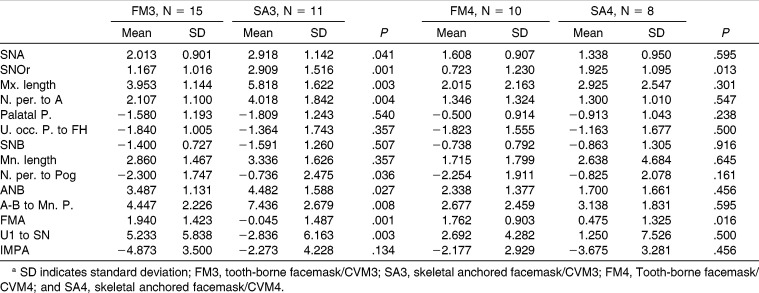
According to the skeletal maturation, SNA, SNOr, and Mx. length in the SA3 (SAFM group at CVM3 stage) were greater than in FM3 (TBFM group at CVM3 stage), indicating a greater anterior movement of maxillary basal bone in the SAFM group, especially during early ages (Table 4). At the CVM4 stage, only SNOr of SA4 was significantly different from FM4, and the change was smaller than at the SA3 stage.
Table 4.
Treatment Changes Between Tooth-Borne Facemask and Skeletal Anchored Facemask (SAFM) on Different Growth Stage. Most of the Skeletal Changes Were Prominent in the SAFM at the Early Maturation Stage. Minus Change in Maxillary Incisors of SAFM Was Observed in the Younger Age Comparison (Mann-Whitney U-Test)a
DISCUSSION
The facemask is a very practical tool that moves the maxillae in downward and forward directions. This movement produces two favorable effects: anterior displacement of the maxillae and backward rotation of mandible. However, the TBFM has the disadvantages of anterior rotation of the maxilla, labioversion of the maxillary incisors, loss of anchorage by mesial migration, and extrusion of maxillary molars, including other dentoalveolar effects. It also has the inability to apply the correct orientation of orthopedic force to the maxilla.4,16
The TBFM causes downward movement of the posterior maxilla and maxillary molar teeth, which in turn rotates the mandible downward and backward. This change is likely to be accompanied by subsequent horizontal mandibular growth, which would cause relapse of anterior crossbite.17–19 Another concerning aspect of this mandibular rotation is that it would worsen the opening tendency of the vertical facial type. Although the rotation pattern is beneficial for low-angle, deep-bite Class III patients, many studies20,21 have demonstrated that facemasks were contraindicated in Class III patients with high angle facial type or openbite. In order to eliminate this counterclockwise rotation effect, various locations have been used for force application7,22,23: the canine region, premolar, and deciduous molar region. Nonetheless, those trials showed that the counterclockwise rotation of the maxilla was inevitable after facemask use. Other investigators have pointed out that intraoral devices have a limited option of choosing a specific point of force application. These authors22 have proposed modified designs to apply the force from a level higher than the palatal plane, which provided promising results in preventing the counterclockwise rotation of occlusal and palatal planes. However, as a result of the bulky extraoral portions of these appliances, these devices have not been widely employed. The closure of the mandibular plane after applying SAFM has been reported in some studies.12,13 Two studies on skeletal facemask did not report the same findings. One study24 included patients with cleft palate, and the other study11 had a small sample size.
In this study, we evaluated the effect of SAFM on vertical skeletal pattern. In the high angle group, the vertical dimension (FMA) of SAFM group showed closure of the mandibular plane with a high level of significance compared to that of the TBFM group. SAFMs do not aggravate high angle patients and prevent the opening tendency of the mandibular plane. Similar patterns were observed between the younger group (CVM3) and the older group (CVM4).
Miniplates for the SAFM can be placed at either the apertura piriformis or the zygomatic buttress area. Apertura piriformis can be a proper location for placement of skeletal anchorage because it is located along the line of action, passing the center of resistance in the maxillae with easy access. This method clearly showed the closure of the mandibular plane.13 However, this anchor location cannot be used in younger patients during early mixed dentition because of the possibility that interruption of canine eruption might occur. On the other hand, SAFM applied on the zygomatic buttress did not result in active closure of the mandibular plane.10,11 This result might be due to the specific location of the skeletal anchorage. Compared to the apertura piriformis, the zygomatic buttress is located in the posterior region, which could result in a clockwise rotation of the maxilla. While evidence12 showed a closed mandibular plane in patients who have had anchors placed on the zygomatic buttress, it is hard to compare the direction of force of this intraoral method with that of extraoral traction methods.
After applying TBFM, clinicians sometimes encounter a delicate situation that might require an extraction as a result of the proclination of the maxillary incisors and crowding of the molar region in patients who have maxillary deficiency. Since the TBFM drags total maxillary dentition forward, protrusion of maxillary teeth is inevitable. In contrast to the TBFM, the lingual version of the maxillary incisors was observed in studies of SAFM.10–13 One study22 suggested that this change is the result of the clockwise rotation of the maxillary dental arch. In this study, retroclination of maxillary incisors has been observed, especially at a younger age (CVM3).
One of the fascinating results associated with the SAFM is that both upper and lower parts of the maxillae are moved forward, which changes the total facial impression.10 One previous study11 reported anterior displacement of the orbitale after SAFM use. In this study, we also observed significant changes in orbitale for patients who underwent SAFM use.
There is some controversy with regard to the timing of facemask use. Some studies6,15 reported that early application of the facemask was associated with a more favorable outcome. However, other studies did not report this result.3,4 Kim et al.15 evaluated treatment result on the protraction facemask therapy across different age groups: younger (4–10 years) and older (10–15 years). This study found that all skeletal changes were greater in the younger group than in the older group. On the contrary, there was a study4 on facemask use in Korean subjects who had been divided into three different age groups. This study concluded that the treatment effect was not significantly different across the age groups. In this study, we compared the treatment effect of both appliances at different developmental stages. Although both types of facemask are associated with greater changes for younger patients, SAFM still showed greater effects than TBFM before peak growth stage (CVM3). A new maxillary traction method using a modified rapid maxillary expander with mini-implants was recently introduced. This also provided skeletal effects similar to that associated with the miniplates, with lower surgical invasiveness.24
The critical time for Class III patients is not the mixed dentition period but the peak growth period, with greater mandibular growth during this latter time. Therefore, protraction of the maxilla should be continued until the deceleration stage of growth. Furthermore, early initiation of the facemask might encounter obstacles like transition to permanent dentition and dental issues stemming from intraoral portions of the facemask. Facemask with skeletal anchors and Class III elastics16 has been successful in the late mixed or permanent dentition phases. These could be applied as long as necessary and are compatible with braces for tooth alignment, even during the transitional period of mixed dentition.
It is possible that some limitations affected this study. First, the sample size for each group was small. Since the SAFM has been introduced into orthodontic fields recently, it is hard to obtain an adequate number of patients to fulfill the statistical requirements for parametric analysis, which results in a lower power. Second, the wearing time was different for each device, which was almost twice as long for the SAFM as for the TBFM. To more accurately compare the outcomes between the facemasks, differences in appliance wearing protocols would have to be justified in future studies.
CONCLUSIONS
SAFMs produced significant increases in all measured anterior-posterior dimensions.
Analysis of changes between the two groups on high vertical skeletal pattern showed that the orbitale in the SAFM group revealed greater anterior movement and that mandibular plane angle was decreased.
Between similar skeletal maturity groups, SAFM in CVM3 resulted in greater anterior-posterior changes, compared to TBFM, on the variables of orbitale (2.909°) and maxillary length (5.818 mm).
These data showed statistically significant advantages of the SAFM group in younger maturity and high vertical skeletal pattern compared with the TBFM group.
REFERENCES
- 1.Proffit WR. Contemporary Orthodontics. St. Louis, MO: Mosby; 1993. [Google Scholar]
- 2.McNamara JA., Jr An orthopedic approach to the treatment of Class III malocclusion in young patients. J Clin Orthod. 1987;21:598–608. [PubMed] [Google Scholar]
- 3.Yüksel S, Uçem TT, Keykubat A. Early and late facemask therapy. Eur J Orthod. 2001;23:559–568. doi: 10.1093/ejo/23.5.559. [DOI] [PubMed] [Google Scholar]
- 4.Baik HS. Clinical results of the maxillary protraction in Korean children. Am J Orthod Dentofacial Orthop. 1995;108:583–592. doi: 10.1016/s0889-5406(95)70003-x. [DOI] [PubMed] [Google Scholar]
- 5.Kapust AJ, Sinclair PM, Turley PK. Cephalometric effects of face mask/expansion therapy in Class III children: a comparison of three age groups. Am J Orthod Dentofacial Orthop. 1998;113:204–212. doi: 10.1016/s0889-5406(98)70141-6. [DOI] [PubMed] [Google Scholar]
- 6.Cha KS. Skeletal changes of maxillary protraction in patients exhibiting skeletal Class III malocclusion: a comparison of three skeletal maturation groups. Angle Orthod. 2003;73:26–35. doi: 10.1043/0003-3219(2003)073<0026:SCOMPI>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 7.Kokich VG, Shapiro PA, Oswald R, Koskinen-Moffett L, Clarren SK. Ankylosed teeth as abutments for maxillary protraction: a case report. Am J Orthod. 1985;88:303–307. doi: 10.1016/0002-9416(85)90129-0. [DOI] [PubMed] [Google Scholar]
- 8.Singer SL, Henry PJ, Rosenberg I. Osseointegrated implants as an adjunct to facemask therapy: a case report. Angle Orthod. 2000;70:253–262. doi: 10.1043/0003-3219(2000)070<0253:OIAAAT>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 9.Hong H, Ngan P, Han G, Qi LG, Stephen HY. Use of onplants as stable anchorage for facemask treatment. Angle Orthod. 2005;75:453–460. doi: 10.1043/0003-3219(2005)75[453:UOOASA]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 10.Cha BK, Lee NK, Choi DS. Maxillary protraction treatment of skeletal Class III children using miniplate anchorage. Korean J Orthod. 2007;37:73–84. [Google Scholar]
- 11.Lee NK, Yang IH, Baek SH. The short-term treatment effects of face mask therapy in Class III patients based on the anchorage device miniplates vs rapid maxillary expansion. Angle Orthod. 2012;82:846–852. doi: 10.2319/090811-584.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cevidanes L, Baccetti T, Franchi L, McNamara JA, Jr, De Clerck H. Comparison of two protocols for maxillary protraction: bone anchors versus facemask with rapid maxillary expansion. Angle Orthod. 2010;80:799–806. doi: 10.2319/111709-651.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sar C, Arman-Özçırpıcı A, Uçkan S, Yazıcı AC. Comparative evaluation of maxillary protraction with or without skeletal anchorage. Am J Orthod Dentofacial Orthop. 2011;139:636–649. doi: 10.1016/j.ajodo.2009.06.039. [DOI] [PubMed] [Google Scholar]
- 14.Baccetti T, Franchi L, McNamara JA., Jr The cervical vertebral maturation (CVM) method for the assessment of optimal treatment timing in dentofacial orthopedics. Semin Orthod. 2005;11:119–129. [Google Scholar]
- 15.Kim JH, Viana MA, Graber TM, Omerza FF, BeGole EA. The effectiveness of protraction face mask therapy: a meta-analysis. Am J Orthod Dentofacial Orthop. 1999;115:675–685. doi: 10.1016/s0889-5406(99)70294-5. [DOI] [PubMed] [Google Scholar]
- 16.McNamara JA, Jr, Brudon WL. Orthodontic and Orthopedic Treatment in the Mixed Dentition. Ann Arbor, Mich: Needham; 1993. pp. 285–293. [Google Scholar]
- 17.Lee DY, Kim ES, Lim YK, Ahn SJ. Skeletal changes of maxillary protraction without rapid maxillary expansion. Angle Orthod. 2010;80:504–510. doi: 10.2319/091609-521.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wellsa AP, Sarverb DM, Proffit WR. Long-term efficacy of reverse pull headgear therapy. Angle Orthod. 2006;76:915–922. doi: 10.2319/091605-328. [DOI] [PubMed] [Google Scholar]
- 19.Ngan PW, Hagg U, Yiu C, Wei SH. Treatment response and long-term dentofacial adaptations to maxillary expansion and protraction. Semin Orthod. 1997;3:255–264. doi: 10.1016/s1073-8746(97)80058-8. [DOI] [PubMed] [Google Scholar]
- 20.Ngan P, Yiu C, Hu A, Hägg U, Wei SH, Gunel E. Cephalometric and occlusal changes following maxillary expansion and protraction. Eur J Orthod. 1998;20:237–254. doi: 10.1093/ejo/20.3.237. [DOI] [PubMed] [Google Scholar]
- 21.Keles A, Tokmak EC, Erverdi N, Nanda R. Effect of varying the force direction on maxillary orthopedic protraction. Angle Orthod. 2002;72:387–396. doi: 10.1043/0003-3219(2002)072<0387:EOVTFD>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 22.Spolyar JL. The design, fabrication and use of full-coverage bonded rapid maxillary expansion appliance. Am J Orthod. 1984;86:136–145. doi: 10.1016/0002-9416(84)90305-1. [DOI] [PubMed] [Google Scholar]
- 23.Ahn HW, Kim HW, Yang IH, et al. Comparison of the effects of maxillary protraction using facemask and miniplate anchorage between unilateral and bilateral cleft lip and palate patients. Angle Orthod. 2012;82:935–941. doi: 10.2319/010112-1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.De Clerck H, Cevidanes L, Baccetti T. Dentofacial effects of bone-anchored maxillary protraction: a controlled study of consecutively treated Class III patients. Am J Orthod Dentofacial Orthop. 2010;138:577–581. doi: 10.1016/j.ajodo.2009.10.037. [DOI] [PMC free article] [PubMed] [Google Scholar]