Substantial research has provided evidence that long-term exposure to air pollution, especially fine particulate matter (particles ⩽2.5 μm in aerodynamic diameter [PM2.5]), contributes to cardiovascular disease (CVD) (1, 2). Key to this evidence is the growing number of cohort studies that have found long-term exposures to PM2.5 air pollution to be associated with increased risk of mortality, including CVD, nonmalignant respiratory disease, and lung cancer mortality (3, 4).
PM2.5–mortality relationships have been observed mostly in broad, population-based cohorts. A few specific, susceptible subpopulations that may be especially vulnerable to air pollution exposures have been identified. For example, relatively large PM2.5–mortality associations have been observed in cohorts of patients who received a cardiac transplant (5) and survivors of myocardial infarction (MI) (6). Also, relatively large associations between PM2.5 air pollution and CVD mortality risk have recently been observed in a cohort of U.S. patients with cancer and cancer survivors (7).
Another identifiable subpopulation that may be especially vulnerable to CVD risk from exposure to air pollution consists of adults with chronic obstructive pulmonary disease (COPD). There is substantial CVD comorbidity in adults with COPD, and those with COPD are at greater risk of CVD and death (8, 9). A recent cohort study of patients with COPD and CVD or risk factors for CVD found that even acute exacerbations of COPD resulted in considerable elevated risk of subsequent CVD events (10).
In this issue of the Journal, Alexeeff and colleagues (pp. 159–167) present novel and important estimates of associations between long-term exposures to PM2.5 air pollution and risk of CVD events in a potentially vulnerable cohort—adults with COPD (11). The study area consisted of a 35-county region of northern California. Time-varying 1-year average PM2.5 air pollution exposure estimates were based on high-quality and well-documented ensemble modeling using ground, satellite, and other data with spatial resolution of 1 km × 1 km across the study area. The cohort was constructed from members of the Kaiser Permanente Northern California health plan for the years 2007–2016, allowing for excellent validation of COPD status and CVD event outcomes. In addition, the researchers had access to key covariates that allowed for model adjustments for age, sex, race/ethnicity, smoking, body mass index, baseline comorbidities, and medications as well as neighborhood education and Medicaid insurance status. After adjustment for these covariates, PM2.5 exposures were observed to be significantly associated with elevated risk of CVD mortality but not MI or stroke.
Somewhat surprisingly, the associations between PM2.5 exposures and risk of CVD mortality were not exceptionally large in the full cohort of adults with COPD compared with associations observed in broader, population-based cohorts or compared with cohorts of other potentially vulnerable populations. Figure 1 illustrates and compares PM2.5–mortality estimated hazard ratios (HRs) and 95% confidence intervals per 10 μg/m3 increase in long-term PM2.5. Estimates for all/natural-cause mortality, CVD/circulatory mortality, ischemic heart disease mortality, and stroke/cerebrovascular mortality are presented. To allow for easy direct comparisons, the actual numeric values of the HRs for CVD mortality are also presented in Figure 1. The blue diamonds are estimates from a systematic review and meta-analysis (4) and are meta estimates representative of broad-based cohorts from the general population—although there is substantial heterogeneity in estimates across cohorts. The green circles are estimates from other selected potentially vulnerable cohorts, including the cardiac transplant cohort (5), the MI survivor cohort (6), and the patients with cancer/cancer survivor cohort (7). The orange squares are estimates from the analysis by Alexeeff and colleagues of the full cohort of adults with COPD (11). The orange triangles are estimates from the analysis by Alexeeff and colleagues of the low-exposure subcohort of adults with COPD who had PM2.5 exposure below 12 μg/m3 for their entire follow up (11).
Figure 1.
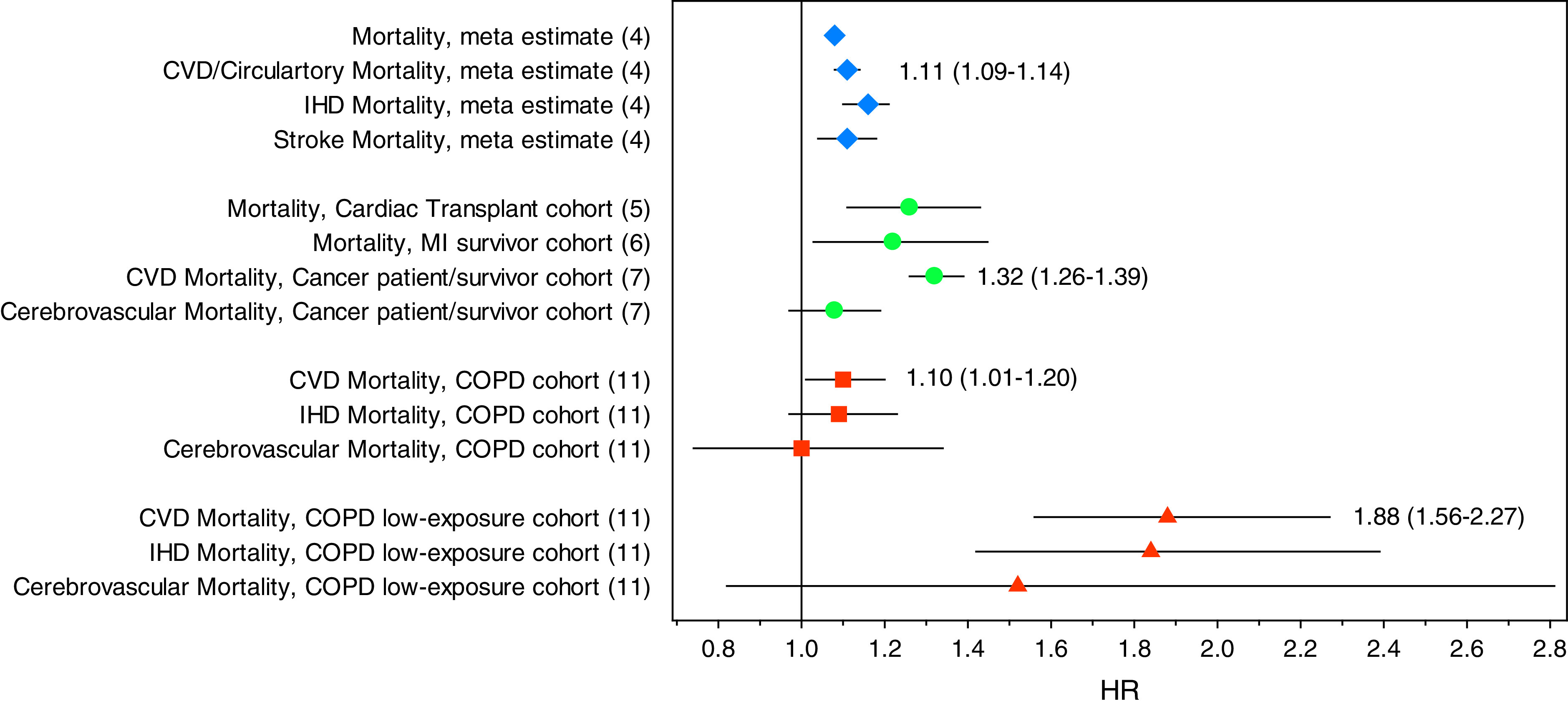
Mortality hazard ratios (95% confidence intervals) associated with a 10 μg/m3 increase in PM2.5 for all/natural-cause mortality, CVD/circulatory mortality, ischemic heart disease mortality, and stroke/cerebrovascular mortality. Blue diamonds are meta estimates from a recent systematic review (4). Green circles are estimates from selected other potentially vulnerable cohorts, including the cardiac transplant cohort (5), the MI survivor cohort (6), and the patients with cancer/cancer survivor cohort (7). Orange squares and triangles are estimates from the analysis by Alexeeff and colleagues (11) of the full chronic obstructive pulmonary disease cohort and the low-exposure subcohort, respectively. COPD = chronic obstructive pulmonary disease; CVD = cardiovascular disease; HR = hazard ratio; IHD = ischemic heart disease; MI = myocardial infarction; PM2.5 = particulate matter ⩽2.5 ?m in aerodynamic diameter.
In Figure 1, it is observed that the PM2.5–mortality HRs for the full cohort of adults with COPD are not larger than the HRs for broad-based cohorts or for the other potentially vulnerable cohorts. However, given that these adults with COPD likely have a substantially larger baseline risk for CVD, comparisons of relative risk estimates clearly do not account for potential differences in attributable risk of PM2.5 exposure among those with COPD.
Maybe the most stunning finding from this study of adults with COPD is evidence of much larger adverse PM2.5–mortality HRs per 10 μg/m3 of PM2.5 among the low-exposure (<12 μg/m3 over the full follow up) subcohort of subjects with COPD (see Figure 1). These results are somewhat troubling and perplexing. How is it plausible for these relative hazards to be so much larger in this low-exposure subcohort? Are relatively large PM2.5–mortality associations at low exposures somehow unique to persons with COPD? Or are these results because of substantive differences in the makeup and underlying baseline hazard of the low-exposure subcohort? Supplemental analysis presented with the paper (11) indicates that those in the low-exposure subcohort were relatively more likely to be white, live in more educated neighborhoods, and have fewer comorbidities. Supplemental analysis of estimated nonlinear associations with PM2.5 and cardiovascular mortality in the low-exposure subcohort indicated that the greatest increase in the HR occurred between 7 and 12 μg/m3 of PM2.5.
In a general sense, the results of this cohort study of adults with COPD are somewhat consistent with other cohort studies of air pollution. Similar PM2.5–CVD mortality associations are observed in broad, population-based cohorts as in the full cohort of adults with COPD (Figure 1). Furthermore, adverse PM2.5–mortality associations are often observed even when long-term average concentrations are below the current annual U.S. PM2.5 national ambient air quality standard for PM2.5 of 12 μg/m3 (3, 12). As Alexeeff and colleagues clearly note (11), their study contributes to the evidence that long-term exposure to PM2.5 air pollution is a risk factor for CVD and that the current long-term PM2.5 standard is not adequately protective—especially for adults with COPD.
Footnotes
Originally Published in Press as DOI: 10.1164/rccm.202103-0647ED on April 9, 2021
Author disclosures are available with the text of this article at www.atsjournals.org.
References
- 1. Brook RD, Rajagopalan S, Pope CA, III, Brook JR, Bhatnagar A, Diez-Roux AV, et al. American Heart Association Council on Epidemiology and Prevention, Council on the Kidney in Cardiovascular Disease, and Council on Nutrition, Physical Activity and Metabolism. Particulate matter air pollution and cardiovascular disease: An update to the scientific statement from the American Heart Association. Circulation . 2010;121:2331–2378. doi: 10.1161/CIR.0b013e3181dbece1. [DOI] [PubMed] [Google Scholar]
- 2. Rajagopalan S, Al-Kindi SG, Brook RD. Air pollution and cardiovascular disease: JACC State-of-the-Art review. J Am Coll Cardiol . 2018;72:2054–2070. doi: 10.1016/j.jacc.2018.07.099. [DOI] [PubMed] [Google Scholar]
- 3. Vodonos A, Awad YA, Schwartz J. The concentration-response between long-term PM2.5 exposure and mortality; A meta-regression approach. Environ Res . 2018;166:677–689. doi: 10.1016/j.envres.2018.06.021. [DOI] [PubMed] [Google Scholar]
- 4. Chen J, Hoek G. Long-term exposure to PM and all-cause and cause-specific mortality: A systematic review and meta-analysis. Environ Int . 2020;143:105974. doi: 10.1016/j.envint.2020.105974. [DOI] [PubMed] [Google Scholar]
- 5. Al-Kindi SG, Sarode A, Zullo M, Brook J, Burnett R, Oliveira GH, et al. Ambient air pollution and mortality after cardiac transplantation. J Am Coll Cardiol . 2019;74:3026–3035. doi: 10.1016/j.jacc.2019.09.066. [DOI] [PubMed] [Google Scholar]
- 6. Chen H, Burnett RT, Copes R, Kwong JC, Villeneuve PJ, Goldberg MS, et al. Ambient fine particulate matter and mortality among survivors of myocardial infarction: population-based cohort study. Environ Health Perspect . 2016;124:1421–1428. doi: 10.1289/EHP185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Coleman NC, Ezzati M, Marshall JD, Robinson AL, Burnett RT, Pope CA., III Fine particulate matter air pollution and mortality risk among US cancer patients and survivors. JNCI Cancer Spectrum. 2021;5:1–9. doi: 10.1093/jncics/pkab001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Sin DD, Man SFP. Why are patients with chronic obstructive pulmonary disease at increased risk of cardiovascular diseases? The potential role of systemic inflammation in chronic obstructive pulmonary disease. Circulation . 2003;107:1514–1519. doi: 10.1161/01.cir.0000056767.69054.b3. [DOI] [PubMed] [Google Scholar]
- 9. Müllerova H, Agusti A, Erqou S, Mapel DW. Cardiovascular comorbidity in COPD: systematic literature review. Chest . 2013;144:1163–1178. doi: 10.1378/chest.12-2847. [DOI] [PubMed] [Google Scholar]
- 10. Kunisaki KM, Dransfield MT, Anderson JA, Brook RD, Calverley PMA, Celli BR, et al. SUMMIT Investigators. Exacerbations of chronic obstructive pulmonary disease and cardiac events. Am J Respir Crit Care Med . 2018;198:51–57. doi: 10.1164/rccm.201711-2239OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Alexeeff SE, Deosaransingh K, Liao NS, Van Den Eeden SK, Schwartz J, Sidney S. Particulate matter and cardiovascular risk in adults with chronic obstructive pulmonary disease. Am J Respir Crit Care Med . 2021;204:159–167. doi: 10.1164/rccm.202007-2901OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Burnett R, Chen H, Szyszkowicz M, Fann N, Hubbell B, Pope CA, III, et al. Global estimates of mortality associated with long-term exposure to outdoor fine particulate matter. Proc Natl Acad Sci USA . 2018;115:9592–9597. doi: 10.1073/pnas.1803222115. [DOI] [PMC free article] [PubMed] [Google Scholar]


