Abstract
Background
We sought to examine bilateral total knee arthroplasty (BTKA) vs unilateral TKA (UTKA) utilization and in-hospital complications comparing African Americans (AAs) and Whites.
Methods
In this retrospective analysis of patients ≥50 years who underwent elective primary TKA, National Inpatient Sample - Healthcare Cost and Utilization Project database (2007–2016) was used. We computed differences in temporal trends in utilization and major in-hospital complication rates of BTKA vs UTKA comparing AAs and Whites. We performed multivariable logistic regression models to assess racial differences in trends adjusting for individual-, hospital- and community-level variables. Discharge weights were used to enable nationwide estimates. We used multiple imputation procedures to impute values for 12% missing race information.
Results
An estimated 276,194 BTKA and 5,528,429 UTKA were performed in the US. The proportion of BTKA amongst all TKAs declined, and AAs were significantly less likely to undergo BTKA compared to Whites throughout the study period (trend P = 0.01). In-hospital complication rates for UTKA were higher in AAs compared to Whites throughout the study period (trend P < .0001). However, for BTKA, the in-hospital complication rates varied between Whites and AAs throughout the study period (trend P = 0.09).
Conclusion
In this nationwide sample of patients from 2007–2016 who underwent total knee arthroplasty, the utilization of BKTA was higher in Whites compared to AAs. On the other hand, while AAs have consistently higher in-hospital complication rates in UTKA over the time period, this pattern was not consistent for BTKA.
Keywords: racial disparities, bilateral total knee arthroplasty, unilateral total knee arthroplasty, knee osteoarthritis
Introduction
Knee Osteoarthritis (OA) is a leading cause of chronic pain and disability in the elderly, and about a third of the patients present with bilateral symptomatic arthritis [1, 2]. When medical/conservative management fails, end-stage knee OA can be successfully managed via elective total knee arthroplasty (TKA) [3]. TKA is one of the most common surgeries performed in the US, with 7.8 million surgeries performed between 1993–2012 [4, 5]. Additionally, its use is expected to increase, as it is estimated that by 2050, 1.5 million cases will be performed every year [5]. In patients with end-stage bilateral OA, treatment options include either a staged TKA procedure, often with a few months in between surgeries, or a simultaneous bilateral TKA (BTKA) procedure during the same anesthetic session. The choice in treatment strategy largely depends on patient and surgeon preferences, and guidelines vary per institution [6]. Even though literature regarding outcomes in simultaneous BTKA procedure has not consistently been favorable, it remains popular in select patients due to use of a single anesthetic, shorter overall surgical time, less time lost from work, lower cost, and lower overall use of narcotics [7–10].
Although arthritis-related activity, disabling work limitations, and severe pain (which are indications for TKA) disproportionately impact African American (AA) patients compared to White patients [11], there are marked racial disparities documented in utilization and outcomes in unilateral TKA (UTKA). Prior analyses have demonstrated racial disparities in UTKA where AAs had reduced utilization and higher complication rates compared to Whites [12–14].
In addition to UTKA, patients may have the option of undergoing BTKA when indicated and appropriate. The utilization of BTKA surged in the early 2000s [6], and it is still extensively performed throughout the United States. However, it is not clear whether there are racial variations in either utilization or in-hospital complication rates of BTKA as have been reported as demonstrated in UTKA.
The objective of our analysis was to examine racial variations in trends of BTKA utilization and in-hospital complication rates adjusting for important demographic and clinical confounders. We hypothesized that similar to UTKA, BTKA utilization is lower and complications are higher in AAs compared to Whites.
Methods
Data Source:
We used data from the National Inpatient Sample (NIS) database from 2007 through 2016. NIS is the largest publicly available inpatient database in the United States. It is sponsored by the Agency for Healthcare Research and Quality (AHRQ) and the Healthcare Cost and Utilization Project (HCUP). Unweighted, it contains data from more than 7 million hospital stays each year. Weighted, it provides estimates on more than 35 million hospitalizations nationally. Prior to 2012, the NIS included all discharge data from more than 1,000 hospitals each year, approximating a 20 percent stratified sample of U.S. community hospitals. NIS was redesigned in 2012, and now creates a sample of discharge records from all HCUP-participating hospitals rather than all discharge records from a sample of hospitals. NIS represents >95% of the US population. Inpatient stay records in NIS include clinical and resource use information available from discharge abstracts derived from state-mandated hospital discharge reports. No unique patient identifiers are contained in the NIS for the hospitalization records.
Analytic Sample:
We identified our analytic sample using the International Classification of Diseases 9th Revision (ICD-9) codes from 2006 through September 2015 and ICD-10 codes from October 2015 through December 2016. Our sample includes all patients who underwent elective primary TKA using the ICD-9 procedure code 81.54 for TKA and BTKA (when the procedure code was used twice in the same admission) from January 1, 2012 through September 30, 2015, and ICD-10 procedure codes 0SRC0x and 0SRD0x thereafter [15]. Study exclusion criteria included the following: age <50 (since >50 years is when a large proportion of end-stage OA patients have surgery); patients with inflammatory arthritis (rheumatoid arthritis, ankylosing spondylitis, spondyloarthropathy, systemic lupus erythematosus, psoriatic arthritis); emergency admissions; patients with pathological fracture; metastatic and bone cancer; avascular necrosis; or have more than two knee replacements on record in the admission (likely administrative dataset error). Accordingly, 9.8% of the sample size was excluded using the criteria above.
Key Study Outcomes:
We studied the trends of BTKA utilization among all TKAs over the time period 2007–2016. Next, we plotted the utilization rate of BTKAs per 100,000 population amongst AAs and Whites over time. We studied differences in temporal trends in utilization of BTKA compared to UTKA between AAs and Whites. We studied major in-hospital complications, which included postoperative myocardial infarction, prosthetic device complication, surgical wound infection, and venous thromboembolism [16]. These were identified using ICD-9/10 codes (Appendix table 1). We studied differences in temporal trends of in-hospital complication rates of UTKA and BTKA stratified by AAs and Whites. We limited our cohort to patients whose race was categorized as either Non-Hispanic White or AA since these are well studied disparity groups in UTKA.
Study Covariates:
Baseline patient characteristics of individual demographics (age, race, primary expected payer), ecological characteristics (median household income per ZIP Code) and hospital characteristics (hospital region, bed size, location/teaching status) were included. Comorbidities were determined using discharge diagnosis codes and an Elixhauser Index was calculated [17, 18]. Patients with morbid obesity (not included in Elixhauser index) were identified using ICD-9 code 27801 and ICD-10 code E660.
Statistical Analysis:
We performed descriptive statistics to compare demographic and hospital characteristics between UTKAs and BTKAs. All categorical variables are reported as weighted frequencies and percentages using sampling weights and hospital clusters. The mean and standard errors are reported for continuous variables. Community-level income is based on the median household income of the patient’s ZIP Code of residence. Bivariate comparisons between BTKAs and UTKAs were conducted based on the Rao-Scott chi-square test.
Utilization rate of BTKAs per 100,000 population over time was examined and plotted. We assessed differences in trends in the utilization of BTKA and UTKA by using binary outcomes (bilateral = 1, unilateral = 0). We conducted logistic regression analysis for sample survey data using the PROC SURVEYLOGISTIC command in SAS to assess whether trends in BTKA and UTKA utilization differed over time. We first performed univariate logistic regression using discharge period (defined as every two years) as the independent variable. To assess race differences over time in BTKA utilization compared to UTKA, we used an interaction term of race (White vs AA) and discharge period. This was adjusted using multivariable logistic regression accounting for demographics (age, sex, insurance); comorbidities (Elixhauser index, morbid obesity); ecological-level (median household income) and hospital-level (volume, bed size, region, and teaching/rural locations) confounders. We plotted utilization trends of BTKA amongst all TKAs stratified by race.
Next, we assessed whether there is a racial trend difference in developing in-hospital complications separately for UTKAs and BTKAs. For univariate logistic regression model, we used complications (Yes/No) as the dependent variable and period*race as the interaction effects of both time period and race on the dependent variable. We performed a multivariable logistic regression model adjusting for the same covariates as described above.
The relationship between in-hospital complications and race was also assessed without interaction in a survey logistic regression model using period as a fixed effect. Unadjusted and adjusted odds ratios (aORs) of in-hospital complications were estimated.
For sensitivity analysis, we performed multiple imputation for race. Specifically, we imputed missing race data using the discriminant function imputation [19], which is suitable for addressing missingness of unordered discrete response categories like patient race. In this procedure, we assumed missing data were missing at random (MAR) and simulated group probabilities of patient race for a given observation from a fitted model consisting of a set of predictor variables. The missing race values are then replaced with the simulated probabilities for a given observation. We created 10 copies of imputed data and used PROC SURVEYLOGISTIC to run regression models for each imputed dataset. Summary estimates were derived by combining the results of analyses carried out on the imputed datasets with PROC MIANALYZE. To assess the overall significance of the race and period interaction, we reported the median p-values from the Wald chi-square tests in models of the 10 imputed datasets.
All analyses accounted for the complex survey design, stratification, and clustering of the data per NIS database recommendations. All p-values were two-sided with statistical significance evaluated at the 0.05 alpha level. All survey-specific analyses were performed in SAS Version 9.4 (SAS Institute, Inc., Cary, NC). Elixhauser comorbidity and surgical complication variables were derived using R Studio Version 1.2.1335 and R Version 3.6.0.
Results
Baseline characteristics:
From 2007 through 2016, an estimated 276,194 BTKA (unweighted observations 56,745) and 5,528,429 UTKA (unweighted observations 1,135,151) were identified. The average age was higher in the UTKA group (67.3 years) than in the BTKA group (65.0 years) (Table 1). Females had a higher proportion of TKAs performed overall (62.1% UTKA and 55.9% BTKA). More patients had private insurance in the BTKA group (48.9%) compared to UTKA (36.0%), whereas more patients had Medicaid/Medicare insurance among UTKA (60.3%) compared to BTKA (47.9%). Furthermore, BTKA patients had fewer comorbidities compared to UTKA patients (Elixhauser Index ≥ 5, 5.1% BTKA vs 5.9% UTKA). The proportion of patients with morbid obesity is similar (7.4% BTKA vs 7.3% UTKA). We observed a higher proportion of BTKA surgeries performed in hospitals where the volume per year is greater than 200 (46.7% in BTKA vs 40.1% in UTKA).
Table 1.
Weighted frequencies and percentages of demographic characteristics among unilateral TKA vs. bilateral TKA.
| Variable | Unilateral TKA N = 5,528,429 (Unweighted N = 1,135,151) |
Bilateral TKA N = 276,194 (Unweighted N = 56,745) |
Pa |
|---|---|---|---|
| Patient Characteristics | |||
| Age, mean (SE) | 67.3 (0.04) | 65.0 (0.07) | <.0001 |
| Sex: Female, n(%) | 3,429,484 (62.1) | 154,442 (55.9) | <.0001 |
| Race, n(%): | |||
| White | 4,051,648 (73.3) | 212,468 (76.9) | <.0001 |
| African American | 352,933 (6.4) | 14,441 (5.2) | |
| Other | 464,407 (8.4) | 16,443 (6.0) | |
| Missing | 659,439 (11.9) | 32,842(11.9) | |
| Insurance, n(%): | <.0001 | ||
| Medicaid/Medicare | 3,334,412 (60.3) | 132,400 (47.9) | |
| Private | 1,987,693 (36.0) | 135,046 (48.9) | |
| Other | 196,313 (3.6) | 7935 (2.9) | |
| Missing | 10,011 (0.2) | 814 (0.3) | |
| Median Household Income, n(%): | <.0001 | ||
| 0–25th percentile | 1,195,291 (22.0) | 54,786 (20.2) | |
| 26th to 50th percentile (median) | 1,457,458 (26.8) | 70,589 (26.0) | |
| 51st to 75th percentile | 1,453,058 (26.7) | 72,734(26.8) | |
| 76th to 100th percentile | 1,329,802 (24.5) | 73,386 (27.0) | |
| Morbid Obesity, n(%) | 401,892 (7.3) | 20,411 (7.4) | 0.47 |
| Elixhauser lndexd, n(%): | <.0001 | ||
| 0 | 716,559(13.0) | 41,550(15.0) | |
| 1–4 | 4,484,941 (81.1) | 220,638 (80.0) | |
| ≥5 | 326,928 (5.9) | 14,007 (5.1) | |
| Hospital Characteristics | |||
| Hospital Region, n(%): | <.0001 | ||
| Northeast | 917,803 (16.6) | 66,665 (24.1) | |
| Midwest | 1,506,373 (27.2) | 76,960 (27.9) | |
| South | 2,014,531 (36.4) | 93,533 (33.9) | |
| West | 1,089,721 (19.7) | 39,037 (14.1) | |
| Hospital Bedsize, n(%): | 0.13 | ||
| Small | 1,194,134 (21.7) | 54,440 (19.8) | |
| Medium | 1,483,188 (26.9) | 75,706 (27.5) | |
| Large | 2,834,371 (51.4) | 144,900 (53.0) | |
| Hospital Volume (cases per year), n(%): | <.0001 | ||
| <100 | 2,045,350 (37.0) | 86,630 (31.4) | |
| 100–200 | 1,267,000 (22.9) | 60,708 (22.0) | |
| >200 | 2,216,078 (40.1) | 128,856 (46.7) | |
| Hospital Location/Teaching status, n(%): | <.0001 | ||
| Rural | 626,057(11.4) | 38,329 (13.9) | |
| Urban nonteaching | 2,312,373 (42.0) | 101,667 (37.0) | |
| Urban teaching | 2,573,263 (46.7) | 135,051 (49.1) |
Note: All values were estimated using sampling weights and hospital clusters.
P-values are calculated based on the Rao-Scott chi-square test for all categorical variables and 2-sample independent t-test for continuous variables. Significance levels: * = p<0.05, ** = p<0.01, *** = p<0.001.
Clinical comorbidities were identified based on coding algorithms developed by Quan and colleagues (enhanced Elixhauser version), using either ICD-9-CM or ICD-10 codes, as appropriate. The Elixhauser co-morbidity index score is calculated based on the cumulative number of comorbidity conditions.
Over the study period, there were estimated 352,933 (8.0%) and 14,441 (6.4%) African American patients who underwent UTKA and BTKA respectively in our study cohort limited to AA and White patients only (Table 2). Among UTKAs and BTKAs, female patients account for a higher percentage in AA patients (73.2% in UTKAs; 71.0% BTKAs) compared to White patients (60.7% in UTKAs; 54.6% BTKAs). Those with private insurance account for a higher percentage in BTKAs for both AAs (47.1% in BTKAs vs. 36.5% in UTKAs) and white patients (49.0% in BTKAs vs. 47.1% in UTKAs) compared to UTKAs.
Table 2.
Baseline characteristics and outcomes by TKA type and race group.
| Variable | Unilaterala | Bilateralb | ||||
|---|---|---|---|---|---|---|
| AA N = 352,933 |
White N = 4,051,648 |
Pc | AA N = 14,441 |
White N = 212,468 |
Pc | |
| Patient characteristics | ||||||
| Age, mean (SD) | 64.5 (0.1) | 67.7 (0.03) | *** | 63.1(0.2) | 65.1(0.1) | *** |
| Sex: Female, n(%) | 258,392 (73.2) | 2,460,479 (60.7) | *** | 10,252 (71.0) | 115,904 (54.6) | *** |
| Insurance, n(%): | *** | *** | ||||
| Medicaid/Medicare | 203,455 (57.6) | 2,466,140(60.9) | 6816 (47.2) | 102,350 (48.2) | ||
| Private | 128,893 (36.5) | 1,448,700 (35.8) | 6806 (47.1) | 104,024 (49.0) | ||
| Other | 19,909 (5.6) | 129,701 (3.2) | 795 (5.5) | 5440 (2.6) | ||
| Missing | 675 (0.2) | 7106 (0.2) | 24 (0.2) | 653 (0.3) | ||
| Median Household Income (by patient’s zipcode), n(%): | *** | *** | ||||
| 0–25th percentile | 157,040 (45.4) | 784,160 (19.7) | 6212 (43.9) | 38,572 (18.5) | ||
| 26th to 50th percentile (median) | 78,446 (22.7) | 1,077,478 (27.0) | 3102(21.9) | 54,262 (26.0) | ||
| 51st to 75th percentile | 63,387 (18.3) | 1,088,899 (27.3) | 2680 (18.9) | 56,655 (27.1) | ||
| 76th to 100th percentile | 47,393 (13.7) | 1,035,870 (26.0) | 2153 (15.2) | 59,562 (28.5) | ||
| Morbid Obesity, n(%) | 43,566 (12.3) | 285,211 (7.0) | *** | 1917 (13.3) | 14,901 (7.0) | *** |
| Elixhauser lndexd, n(%): | *** | *** | ||||
| 0 | 25,683 (7.3) | 539,763 (13.3) | 1047 (7.2) | 33,448 (15.7) | ||
| 1–4 | 300,256 (85.1) | 3,271,112 (80.7) | 12,335 (85.4) | 168,489 (79.3) | ||
| ≥5 | 26,994 (7.6) | 240,773 (5.9) | 1060 (7.3) | 10,531 (5.0) | ||
| Hospital characteristics | ||||||
| Hospital Region, n(%): | *** | *** | ||||
| Northeast | 58,354 (16.5) | 773,576(19.1) | 3582 (24.8) | 57,780 (27.2) | ||
| Midwest | 63,098 (17.9) | 983,137 (24.3) | 1888 (13.1) | 53,093 (25.0) | ||
| South | 197,266 (55.9) | 1,523,134(37.6) | 8078 (55.9) | 73,723 (34.7) | ||
| West | 34,215 (9.7) | 771,801 (19.0) | 894 (6.2) | 27,873 (13.1) | ||
| Hospital Bedsize, n(%): | *** | ** | ||||
| Small | 65,375 (18.6) | 898,459 (22.2) | 2444 (16.9) | 43,096 (20.4) | ||
| Medium | 99,951 (28.5) | 1,089,113(27.0) | 4763 (33.0) | 59,827 (28.3) | ||
| Large | 185,914(52.9) | 2,052,658 (50.8) | 7212 (50.0) | 108,479 (51.3) | ||
| Hospital Volume (cases per year), n(%): | *** | *** | ||||
| <100 | 144,175 (40.9) | 1,513,543 (37.4) | 5257 (36.4) | 67,465 (31.8) | ||
| 100–200 | 80,239 (22.7) | 936,164 (23.1) | 3530 (24.4) | 46,065 (21.7) | ||
| >200 | 128,519 (36.4) | 1,601,941 (39.5) | 5655 (39.2) | 98,938 (46.6) | ||
| Hospital Location/Teaching status, n(%) | *** | *** | ||||
| Rural | 19,757 (5.6) | 461,980 (11.4) | 1115 (7.7) | 27,879 (13.2) | ||
| Urban nonteaching | 118,487 (33.7) | 1,736,575 (43.0) | 4732 (32.8) | 80,179 (37.9) | ||
| Urban teaching | 212,995 (60.6) | 1,841,675 (45.6) | 8572 (59.4) | 103,345 (48.9) | ||
Note: AA = African American; WH = White. All values were estimated using sampling weights and hospital clusters.
Unilateral unweighted frequencies: N = 72,565 for AA; N = 830,071 for WH
Bilateral unweighted frequencies: N = 2967 for AA; N = 43,574 for WH
P-values are calculated based on the Rao-Scott chi-square test is a design-adjusted version of the Pearson chi-square test. Significance levels:
p<0.05,
p<0.01,
p<0.001.
Clinical comorbidities were identified based on coding algorithms developed by Quan and colleagues (enhanced Elixhauser version), using either ICD-9-CM or ICD-10 codes, as appropriate. The Elixhauser co-morbidity index score is calculated based on the cumulative number of comorbidity conditions.
Overall Utilization Trends:
Over the 10-year study period, the proportion of BTKA amongst all TKAs declined from 5.53% in 2007–08 to 4.03% in 2015–16 (Figure 1a). Compared to UTKA, BTKA utilization significantly declined (P trend difference = 0.003) even after adjusting for individual-, ecological- and hospital-level variables described above.
Figure 1 (a).
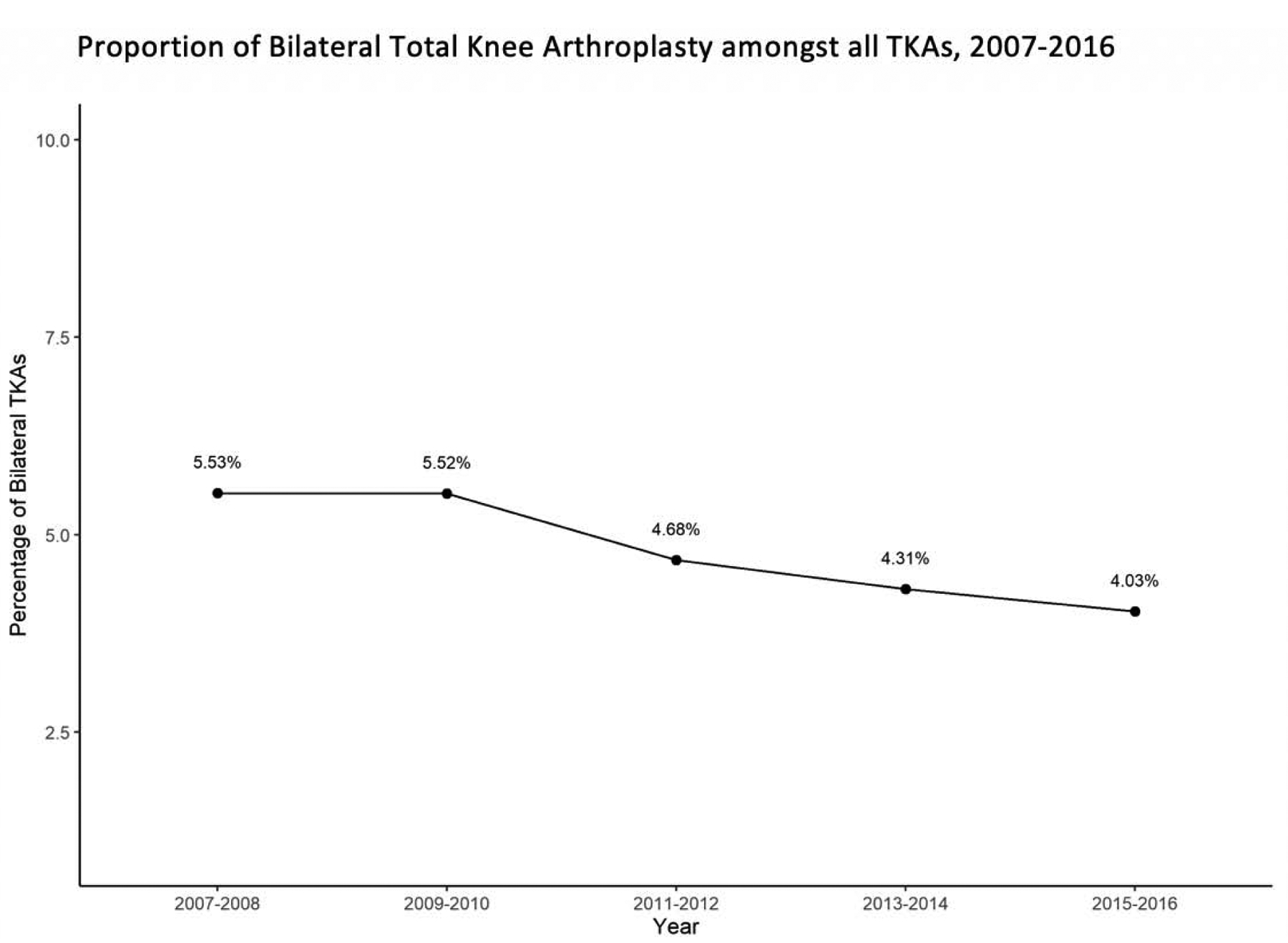
Proportional Utilization of Bilateral Total Knee Arthroplasty (TKA) amongst all TKAs over time.
Racial Variations in Utilization Rates:
Over the study period, 4,051,648 (95.0%) whites and 352,933 (96.0%) AAs underwent UTKA. Similarly, 212,468 (5.0%) whites and 14,441 (3.9%) AAs underwent BTKAs (Table 1). Amongst all TKAs throughout the study period, African Americans continued to have lower BTKA utilization rates compared to Whites (23.4 per 100,000 population in AAs vs 48.8 per 100,000 in Whites in 2007–08, whereas 27.0 per 100,000 in AAs vs 47.6 per 100,000 in Whites in 2015–16) (Figure 1b). The difference in trends between Whites and AAs for BTKA compared to UTKA was significant even after covariate adjustment (P trend difference =0.01).
Figure 1 (b).
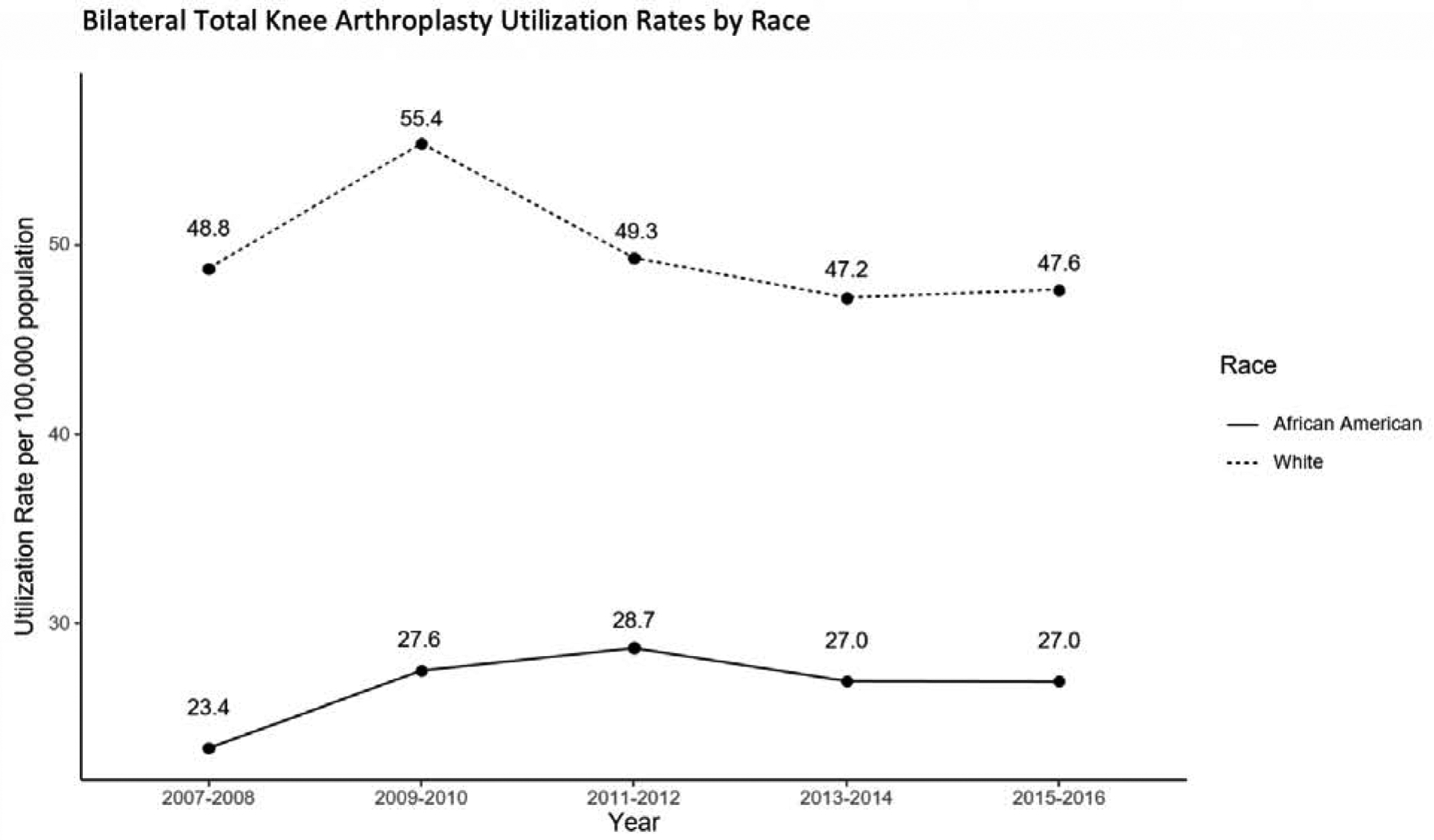
Utilization rate of Bilateral Total Knee Arthroplasty (TKA) per 100,000 population by race.
Population estimates obtained from the Intercensal Race-Specific Estimates of Resident Population by Sex and Age for the United States: April 1, 2000 to July 1, 2010; Annual Estimates of the Resident Population by Sex, Age, Race, and Hispanic Origin for the United States: April 1, 2010 to July 1, 2019. Source: the U.S. Census Bureau, Population Division.
Racial Variations in Major In-hospital Complication Rates:
Over the 10-year period, in-hospital complication rates were 1.09% in UTKA (60,252) and 1.03% in BTKA (2,834). For UTKA, our results show significantly lower in-hospital complication rates in Whites compared to AAs throughout the study period (1.35% in Whites vs 1.50% in AAs, 2007–08, 1.00% in Whites vs 1.35% in AAs in 2015–16, P trend difference <.0001). After adjusting for covariates, AAs were associated with higher odds of in-hospital UTKA complications compared to Whites (aOR: 1.10, 95% CI: 1.02–1.19, P = 0.01) (Figure 1c). However, for BTKA, the in-hospital complication rates varied between Whites and AA throughout the study period (1.21% in Whites vs 1.27% in AAs, 2007–08; 1.03% in Whites vs. 1.08% in AAs, 2011–12; 0.86% in Whites and 0.92% in AAs, 2015–16, P trend difference 0.09) (Figure 1d). After adjusting for covariates, in-hospital complications for BTKA were not significantly different among AAs and Whites throughout the study period (aOR: 0.84, 95% CI: 0.56–1.24, p > 0.05).
Figure 1 (c).
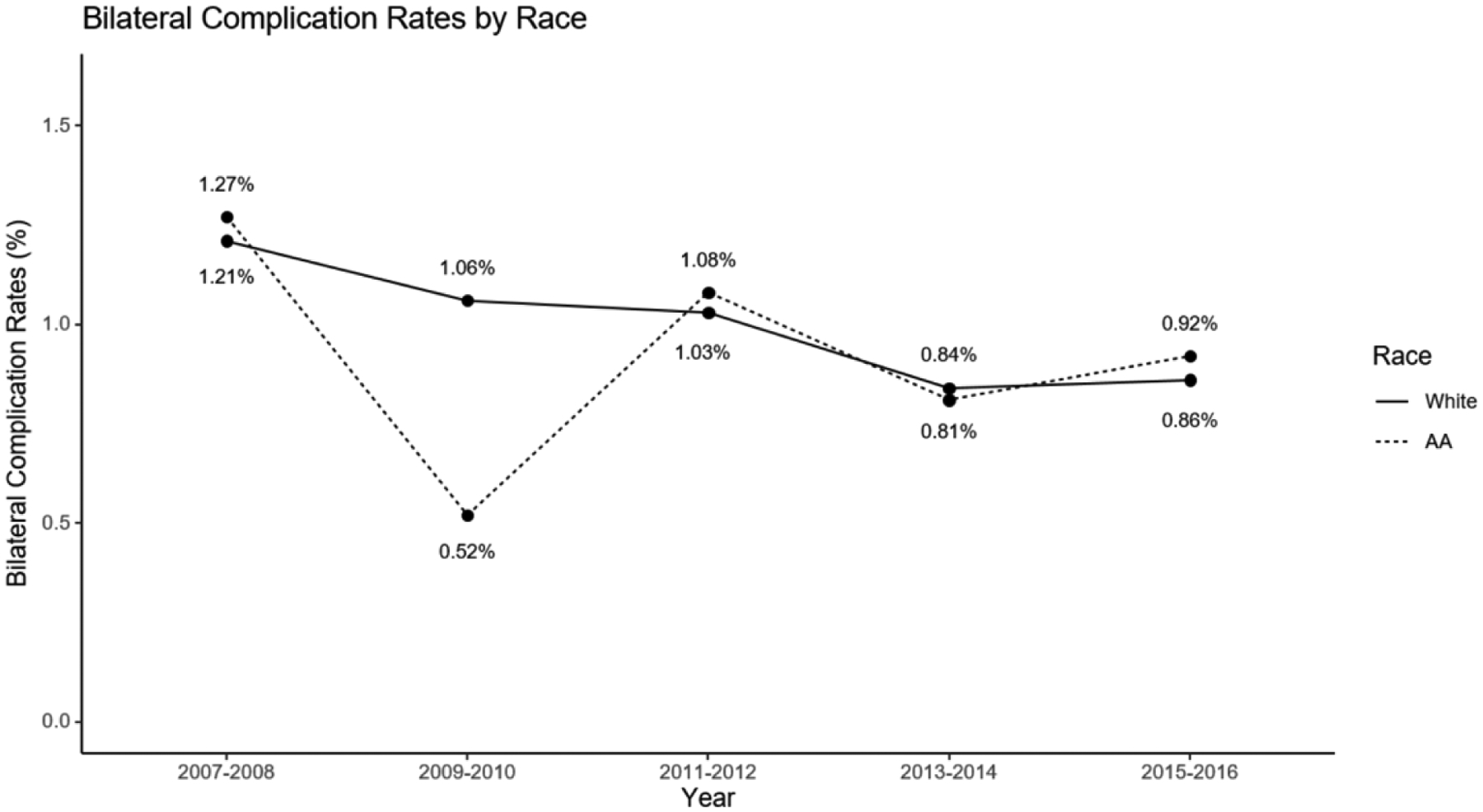
Bilateral total knee arthroplasty in-hospital complications in Whites and African Americans.
Figure 1 (d).
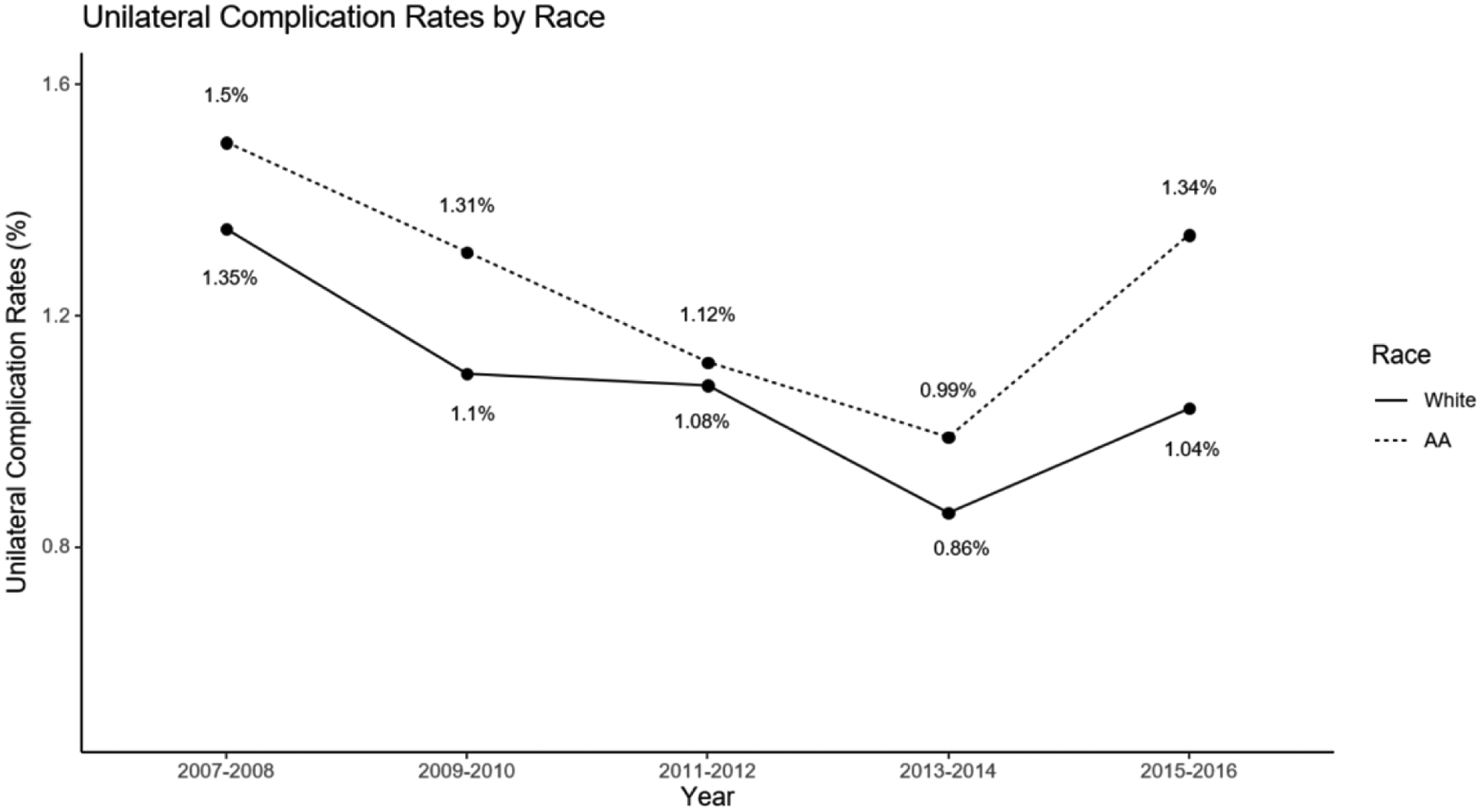
Unilateral total knee arthroplasty in-hospital complications in Whites and African Americans.
Imputation Results:
Given that we had 12.1% missing data on race, we performed imputation analysis as described in the methods above. After imputation, we had 4,621,370 (92.2%) Whites and 391,155 (7.8%) AAs in UTKA, and 240,798 (93.6%) Whites and 16,393 (6.4%) AAs in BTKA.
The imputed data and complete case data generated consistent significant results (p-value < 0.05) in the multivariable regression models described above for utilization and complications between AAs and Whites except for BTKA complications. For the BTKA complications model where we detected insignificant results in racial trend differences (P trend difference = 0.09), after imputation, the difference in AA vs Whites was statistically significant (P trend difference < 0.001). As the sample size increased after imputation, the power of the analysis to detect significance in BTKA complication trends between AA and Whites also increased. However, a statement on which group had a higher complication rate throughout the study period cannot be made due to diverging patterns over time (Figure 1c).
We also assessed how well the multiple imputation was performed by conducting imputation diagnostics using the total variance and relative efficiency measures. We observed a low total variance (all close to 0) and high relative efficiencies of at least 0.97, both of which suggested that we achieved high precision of the parameter estimates using 10 imputation repetitions.
Discussion
In this study of a nationwide sample of patients collected for the NIS between the years of 2007 and 2016, we found that even though utilization of BTKA compared to UTKA has decreased over time, BTKA is still widely performed. During the study period, African Americans consistently had lower utilization rates relative to Whites, and this was significant even after adjusting for important confounders like comorbidities. We also found that in-hospital complication rates for UTKA were consistently higher in AAs compared to Whites. However, for BTKA complications, the pattern varied between time periods.
A number of studies in the literature have documented decreased utilization of TKA in AAs relative to Whites [20] [21] [22]. However, this trend in utilization rates has not been investigated for BTKA specifically. Zhang et al. used nationally representative data to demonstrate decreased TKA utilization in AAs compared to Whites [20]. Additionally their study elucidated a 32% AAs vs White TKA utilization disparity that persisted over time. Other studies, which analyzed a variety of different cohorts, have also demonstrated disparities in the utilization of TKA [21] [22]. Jones et al. analyzed TKA utilization in the VA population (2000–2001) and showed that AAs were significantly less likely than Whites to undergo TKA [21]. Singh et al. demonstrated that this trend was also seen using Medicare data over time, as utilization of primary TKA was 36% lower for AAs compared to Whites in 1991 and 40% lower in 2008 [22].
While the literature to date supports the disparity in utilization rates demonstrated in this paper, none of the studies have specifically addressed BTKA. What we demonstrate in this paper is that the disparity in utilization is persistent when looking at BTKA trends over time. This is an important finding as it illustrates how the disparity is perpetuated for more selective procedures. While our study shows a decrease in the overall proportional use of BKTA amongst all TKA over time, these procedures are still commonly performed. After its initial surge in the early 2000s, its popularity waned as literature was published demonstrating higher complication rates in BTKA [23]. However, recent data has proposed that given advances in perioperative medical care, such as the use of tranexamic acid to decrease blood loss and transfusion requirement, the complication rates after BTKA have decreased [24]. These studies have proposed that BTKA is underutilized due to historical risk and champion its resurgence, claiming low overall complication rates and high patient satisfaction [25]. Given these developments, our paper contributes to the literature by highlighting a racial disparity in this field. The reasons for lower utilization of total knee arthroplasty in AAs have been extensively studied and are multifactorial, including access, health literacy, and trust, amongst many others. One possible reason for the disparity in BTKA utilization is a difference in access to high volume centers, which are more likely to perform bilateral procedures [20]. Additionally, as prior literature has elucidated that AAs are more likely to be hesitant about surgery than Whites, perhaps more AA patients preferred unilateral over bilateral procedures [26]. This is important as it suggests that the patient, provider, and systemic issues may create barriers to care that contribute to the racial disparities seen in UTKA are compounded for BTKA. While large database studies such as this can highlight disparate utilization and outcomes, further work at the patient level will be required to understand the barriers to health equity.
A common finding in the literature on TKA utilization is that postoperative complication rates are higher amongst AAs than Whites [20] [27]. For example, Zhang et al. found increased in-hospital complication rates in AAs relative to Whites (OR = 1.08, p = 0.01) [19]. Additionally, Nwachukwu et al. systematically reviewed six studies which reported increased complications after TKA in AAs relative to Whites, such as mortality, post-operative infection, and pulmonary embolus development [27]. Furthermore, higher postoperative complication rates, such as venous thromboembolism and cardiorespiratory complications, have been documented in BTKA relative to UTKA [28]. As BTKAs have become more commonly used over time, data has indicated that younger and healthier patients are more often selected [29]. We also demonstrate this trend in our study. Our crude in-hospital complication rates were slightly higher in UTKA compared to BTKA, which may reflect rigorous selection of the BTKA patients. Given that the rate of utilization of BTKA was lower in AAs compared to Whites, we studied the in-hospital complication rates. Our analysis demonstrates a higher proportion of in-hospital complication rates for AA compared to whites in UTKA; however, this was not consistently the case with BTKA. This important finding could be because AAs are selected more carefully for a BTKA. However, these analyses were adjusted for comorbidities, as well as individual-, hospital- and ecological-level factors which commonly affect this. While unmeasured variables can account for this, it is important to consider the possibility that many AAs who may be “appropriate” for BTKA do not undergo the BTKA procedure. This could also reflect either patient preference, physician preference or system-level factors which are important to study.
There are important limitations to consider in interpreting our results. First, the database we used covers only procedures in hospitalized patients; therefore, we have no information on same-day discharges. However, most BTKA patients are not discharged on the same day, making the observations of the study potentially more conservative. Second, we were only able to analyze in-hospital major complications. Therefore, we were unable to capture post-discharge complications. Third, although procedure codes for TKA have a sensitivity of 89% and a specificity of 98% [30], complication diagnoses may be misclassified since NIS uses billing information and discharge diagnosis. Fourth, since we rely on ICD9/10 codes for capturing comorbidities, as well as use an index like Elixhauser comorbidity, it is possible that some of the confounders are not fully captured. Lastly, we could not evaluate patient reported outcomes, labs, medication data, and other surgical factors, such as the length of surgery or surgeon volume etc., all of which may influence outcomes, and we are unable to comment on these factors. Further, we could not identify from the dataset why a procedure – UTKA vs BTKA – was chosen, which could also impact odds of major in-hospital complications.
In conclusion, in this nationwide sample of patients collected for the NIS between the years of 2007 and 2016, we found that even though utilization of BTKA compared to UTKA has decreased over time, it is widely performed. The utilization of BTKA was lower in African Americans than in Whites even after adjusting for important confounders like comorbidities. We also found that in-hospital complication rates for UTKA were consistently higher in AAs compared to Whites. However, for BTKA the pattern varied over time. Our results highlight the need for further research on the psychosocial, as well as patient- and provider-level factors that may help explain these disparities. This study does not advocate for the increased use of BTKA in AA populations. However, as the literature on BTKA continues to evolve and indications change, we propose that it is important to be vigilant about the patterns of utilization in different demographics. These results emphasize the need for more nuanced research when creating guidelines for BTKA patient selection, in order to ensure equitable access and utilization.
Supplementary Material
Appendix Table 1:
Complication Codes Used:
| ICD9 | ICD10 | |
|---|---|---|
| Acute Myocardial Infarction | 410 | 121, 122 |
| Deep vein thrombosis | 45340, 45341, 4536, 45342, 45384, 45381, 45386, 45389, 45382, 4539, 45385, 4511, 4512, 4518, 4519 | 1801, 1802, 1803, 1809, 1822, 1823, 1828, 1829, 1824 |
| Wound complications | 99859, 9866, 99667 99830, 99831, 99832, 99833, 99851, 99883 | K6811, T814XXA |
| Device complications | 99666, 9964 | T8481XA, T84115D, T84020A, T84114A, T84218A, T8484XA, T84498A, T84199A, T84011A, T84021A, T8489XA, T8451XA, T84010A, T84091A, T84031A, T84328A, T84030A, T84099A, T84090A, T84428A, T84038A, T84061A, T84050A, T8486XA, T8452XA, T8483XA |
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Kauppila A, Kyllonen E, Mikkonen P, Ohtonen P, Laine V, Siira P, Niinimaki J, Arokoski J. Disability in end-stage knee osteoarthritis. Disabil Rehabil 31(5): 370, 2009 [DOI] [PubMed] [Google Scholar]
- 2.Metcalfe AJ, Andersson ML, Goodfellow R, Thorstensson CAJBmd. Is knee osteoarthritis a symmetrical disease? Analysis of a 12 year prospective cohort study. 13(1): 153, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Van Manen M, Nace J, Mont M. Management of primary knee osteoarthritis and indications for total knee arthroplasty for general practitioners. J Am Osteopath Assoc 112(11): 709, 2012 [PubMed] [Google Scholar]
- 4.Davidson IU, Brigati DP, Faour M, Ibrahim M, Murray TG. Same-day bilateral total knee arthroplasty candidacy criteria decrease length of stay and facility discharge. Orthopedics 41(5): 293, 2018 [DOI] [PubMed] [Google Scholar]
- 5.Inacio M, Paxton E, Graves S, Namba R, Nemes S. Projected increase in total knee arthroplasty in the United States–an alternative projection model. Osteoarthritis and cartilage 25(11): 1797, 2017 [DOI] [PubMed] [Google Scholar]
- 6.Vulcano E, Memtsoudis S, Della Valle AG. Bilateral Total Knee Arthroplasty Guidelines: Are We There Yet? J Knee Surg 26(04): 273, 2013 [DOI] [PubMed] [Google Scholar]
- 7.Memtsoudis SG, Ma Y, Della Valle AG, Mazumdar M, Gaber-Baylis LK, MacKenzie CR, Sculco TPJATJotASoA. Perioperative outcomes after unilateral and bilateral total knee arthroplasty. 111(6): 1206, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hooper GJ, Hooper NM, Rothwell AG, Hobbs T. Bilateral total joint arthroplasty: the early results from the New Zealand National Joint Registry. J Arthroplasty 24(8): 1174, 2009 [DOI] [PubMed] [Google Scholar]
- 9.Sheth DS, Cafri G, Paxton EW, Namba RS. Bilateral simultaneous vs staged total knee arthroplasty: a comparison of complications and mortality. The Journal of arthroplasty 31(9): 212, 2016 [DOI] [PubMed] [Google Scholar]
- 10.Memtsoudis SG, Ma Y, Della Valle AG, Mazumdar M, Gaber-Baylis LK, MacKenzie CR, Sculco TP. Perioperative outcomes after unilateral and bilateral total knee arthroplasty. Anesthesiology: The Journal of the American Society of Anesthesiologists 111(6): 1206, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Parmelee PA, Harralson TL, McPherron JA, DeCoster J, Schumacher HR. Pain, disability, and depression in osteoarthritis: effects of race and sex. Journal of aging and health 24(1): 168, 2012 [DOI] [PubMed] [Google Scholar]
- 12.Skinner J, Weinstein JN, Sporer SM, Wennberg JEJNEJoM. Racial, ethnic, and geographic disparities in rates of knee arthroplasty among Medicare patients. 349(14): 1350, 2003 [DOI] [PubMed] [Google Scholar]
- 13.Ibrahim SA, Stone RA, Han X, Cohen P, Fine MJ, Henderson WG, Khuri SF, Kwoh CKJA, Rheumatology ROJotACo. Racial/ethnic differences in surgical outcomes in veterans following knee or hip arthroplasty. 52(10): 3143, 2005 [DOI] [PubMed] [Google Scholar]
- 14.Ibrahim SA, Siminoff LA, Burant CJ, Kwoh CKJMc. Understanding ethnic differences in the utilization of joint replacement for osteoarthritis: the role of patient-level factors. 40(1): I, 2002 [DOI] [PubMed] [Google Scholar]
- 15.Cahue SR, Etkin CD, Stryker LS, Voss FRJAT. Procedure coding in the American Joint Replacement Registry. 2019 [DOI] [PMC free article] [PubMed]
- 16.Mehta B, Singh JA, Ho K, Parks M, Nelson C, D’Angelo D, Ibrahim SA. Race, Discharge Disposition, and Readmissions After Elective Hip Replacement: Analysis of a Large Regional Dataset. Health Equity 3(1): 628, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Quan H, Sundararajan V, Halfon P, Fong A, Burnand B, Luthi JC, Saunders LD, Beck CA, Feasby TE, Ghali WA. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Medical care 43(11): 1130, 2005 [DOI] [PubMed] [Google Scholar]
- 18.Li B, Evans D, Faris P, Dean S, Quan HJBhsr. Risk adjustment performance of Charlson and Elixhauser comorbidities in ICD-9 and ICD-10 administrative databases. 8(1): 12, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Houchens R. Missing Data Methods for the NIS and the SID. HCUP Methods Series Report# 2015–01 January 22 USAfHRa, 2015 [Google Scholar]
- 20.Zhang W, Lyman S, Boutin-Foster C, Parks ML, Pan T-J, Lan A, Ma Y. Racial and ethnic disparities in utilization rate, hospital volume, and perioperative outcomes after total knee arthroplasty. JBJS 98(15): 1243, 2016 [DOI] [PubMed] [Google Scholar]
- 21.Jones A, Kwoh CK, Kelley ME, Ibrahim SA. Racial disparity in knee arthroplasty utilization in the veterans health administration. Arthritis and rheumatism 53(6): 979, 2005 [DOI] [PubMed] [Google Scholar]
- 22.Singh JA, Lu X, Rosenthal GE, Ibrahim S, Cram P. Racial disparities in knee and hip total joint arthroplasty: an 18-year analysis of national Medicare data. Annals of the rheumatic diseases 73(12): 2107, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Restrepo C, Parvizi J, Dietrich T, Einhorn TA. Safety of simultaneous bilateral total knee arthroplasty: a meta-analysis. JBJS 89(6): 1220, 2007 [DOI] [PubMed] [Google Scholar]
- 24.Malahias M-A, Gu A, Adriani M, Addona JL, Alexiades MM, Sculco PK. Comparing the safety and outcome of simultaneous and staged bilateral total knee arthroplasty in contemporary practice: a systematic review of the literature. The Journal of Arthroplasty 34(7): 1531, 2019 [DOI] [PubMed] [Google Scholar]
- 25.Putnis SE, Klasan A, Redgment JD, Daniel MS, Parker DA, Coolican MR. One-stage sequential bilateral total knee arthroplasty: an effective treatment for advanced bilateral knee osteoarthritis providing high patient satisfaction. The Journal of Arthroplasty 35(2): 401, 2020 [DOI] [PubMed] [Google Scholar]
- 26.Ibrahim SA, Siminoff LA, Burant CJ, Kwoh CK. Variation in perceptions of treatment and self-care practices in elderly with osteoarthritis: a comparison between African American and white patients. Arthritis Care & Research: Official Journal of the American College of Rheumatology 45(4): 340, 2001 [DOI] [PubMed] [Google Scholar]
- 27.Nwachukwu BU, Kenny AD, Losina E, Chibnik LB, Katz JN. Complications for racial and ethnic minority groups after total hip and knee replacement: a review of the literature. The Journal of Bone and Joint Surgery American volume 92(2): 338, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Vulcano E, Memtsoudis S, Della Valle AG. Bilateral total knee arthroplasty guidelines: are we there yet? In. 2013 [DOI] [PubMed]
- 29.Memtsoudis SG, Ma Y, González Della Valle A, Mazumdar M, Gaber-Baylis LK, MacKenzie CR, Sculco TP. Perioperative outcomes after unilateral and bilateral total knee arthroplasty. Anesthesiology, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Daneshvar P, Forster AJ, Dervin GF. Accuracy of administrative coding in identifying hip and knee primary replacements and revisions. Journal of evaluation in clinical practice 18(3): 555, 2012 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


