Abstract
Despite high risk for HIV, South African adolescent girls and young women (AGYW) experience numerous challenges with adherence to PrEP. To better understand AGYW’s motivations for PrEP and factors that impact PrEP adherence, we conducted serial in-depth interviews with 22 South African AGYW during a 12 month prospective study. Interviews explored motivations and initial experiences of PrEP use, patterns of adherence, social support, and reasons for stopping or persisting with PrEP. We also assessed drug levels as a biomarker of adherence; dried blood spots were collected at months 1, 2, 3, 6, and 12 to assess intracellular tenofovir diphosphate levels. An end-user journey analytical approach revealed themes related to behavioral and emotional aspects of use, including multilevel factors leading to divergent PrEP adherence trajectories. Our findings highlight how internal versus external motivations drive PrEP use, as well as how positive identity formation and challenges are handled, which are essential to understand AGYW in their PrEP journeys.
Keywords: HIV Prevention, Oral Pre-exposure Prophylaxis, End-user journey, South Africa, Adolescent girls and young women
Introduction
In sub-Saharan Africa, adolescent girls and young women (AGYW) aged 15–24 accounted for 25% of new HIV infections in 2017, despite representing only 10% of the region’s population (1). Furthermore, South Africa has the highest number of HIV-infected persons globally, and the highest HIV incidence in the country is among AGYW (2, 3). In 2018, new infections among AGYW were more than double those among young men (4). In a recent study on hormonal contraceptive methods, there was an HIV incidence of approximately 4% among the young women who participated (5).
PrEP is highly efficacious when taken correctly (6). The South African Health Products Regulatory Authority (SAHPRA) approved the use of daily Truvada© for oral pre-exposure prophylaxis (PrEP) in 2015 (5), and the WHO broadened its recommendations by endorsing PrEP for all population groups at substantial risk of HIV infection prioritizing AGYW for PrEP delivery (6). Evidence suggests that young women face many challenges with daily pill taking, and this has resulted in sub-optimal adherence in clinical studies (7). The VOICE trial was unable to demonstrate PrEP efficacy due to low PrEP adherence, especially among younger women, who were at greatest risk for HIV infection (8). The HPTN 082 study assessed PrEP uptake and effect of drug level feedback on adherence to PrEP among AGYW in South Africa and Zimbabwe, and observed a significant drop in adherence after the first three months of PrEP use based on longitudinal measurement of intracellular tenofovir diphosphate (TFV-DP) levels, demonstrating the challenge of keeping AGYW engaged with daily oral PrEP (9).
Qualitative research has highlighted both external factors and internal drivers impacting adherence to PrEP in reproductive-age women, including rumors around product efficacy, HIV stigma, low social support, concerns about male partners’ reactions and underestimation of one’s risk behavior (10, 11). Nevertheless, a greater understanding of AGYW’s circumstances that motivate PrEP uptake, effective use and persistence is needed. One of the biggest challenges with PrEP implementation among African AGYW is a lack of understanding patterns of use, including temporary and permanent discontinuation (12). So far, evidence suggests that peer influence, and a desire to maintain sexual relationships have immediate rewards and are prioritized over HIV prevention, which has less immediate benefits (13). Family support, especially from mothers, impacts both health behavior and health-related decision-making of adolescents (14–17).
In the 3P (Perception, Partners, and Pills) study, an open label PrEP demonstration study among AGYW in Cape Town, South Africa, PrEP uptake and persistence over one year were high, although high adherence dropped significantly after the first 3 months (18). The 3P study included longitudinal in-depth interviews, which investigated how motivation, risk perception, social and environmental influences, and other life factors informed AGYW’s decisions to try PrEP. Longitudinal interviews also explored their 12-month ‘journey’ with PrEP, including experiences of adherence and persistence or discontinuation. Drawing upon key findings from interview data, this manuscript aims to contribute towards a greater understanding of the circumstances that impact AGYW PrEP uptake and patterns of use.
Methods
Research setting and study participants
The 3P study was conducted among 200 HIV-negative, sexually active AGYW aged 16–25 who were willing to take PrEP, recruited from a peri-urban Cape Town township with an HIV prevalence rate of 23% (19). In this township, 91% of the population identifies as Black African, there is a 31% unemployment rate, and 72 % of the population resides in informal dwellings (e.g. shacks) (20). Many participants heard about PrEP from friends/other community resources, and a 90-second PrEP demand creation video and two informational brochures were used to recruit AGYW (https://goo.gl/HDZ34D) (21). Women who met inclusion criteria and agreed to study participation were dispensed PrEP with their first dose observed, and followed for 12 months. Study visits were conducted at months one, two, three, six, and 12 with collection of dried blood spots (DBS) to assess intracellular tenofovir diphosphate (TFV-DP) levels as a marker of PrEP adherence (18), and participants received retrospective drug-level feedback and adherence counseling at their next study visit (months 2, 3, 4) during the first three months of the study. Half the participants were randomized to receive a small incentive ($13) conditioned on high adherence in the prior month, defined as TFV-DP ≥ 700 fmol/punch (18).
Longitudinal Qualitative Data Collection
Twenty-two participants were purposively selected at enrollment to participate in the qualitative component of 3P, encompassing serial in-depth-interviews (IDIs) at their month one (M1), three (M3), and twelve (M12) visits. Participants were selected to represent a range of ages and both study arms (incentive arm and standard of care). M1 IDIs focused on initial interest and motivation to use PrEP, initial experiences of PrEP use, disclosure, and social support/opposition. M3 IDIs further explored early patterns of adherence (both self-reported and drug-level feedback) and the impact of PrEP on relationships and social experiences. M12 IDIs elicited participants’ reflections on their overall PrEP journey, reasons for stopping or persisting with PrEP and experience in the 3P study. All interviews were conducted in the preferred language of the participant (English or isiXhosa) by a trained female social scientist. Interviews were audio-recorded, transcribed and translated by interviewers, undergoing quality checks at the study site and by the US-based data center (RTI/WGHI). Participants completed demographic and behavioral survey questions at baseline. The study protocol was reviewed and approved by the University of Cape Town Human Research Ethics Committee (HREC).
Data Analysis
Demographic data was analyzed descriptively using SAS v9.4. Transcripts were coded in Dedoose (version 8.2.18, Los Angeles, CA). The codebook was iteratively developed around an ‘end-user journey’ analytical approach (adapted from1), to understand AGYW’s perceptions of their needs and decision-making processes from initial PrEP awareness, uptake and initiation, through adherence and persistence, and we built chronological time into our analytical approach (Figure 1). The longitudinal nature of the 3P data allowed for an analysis of the developing journey and points of engagement or disengagement for each participant. An end-user journey approach, central to the human-centered design framework, highlights the shifting need-states of the user and evolving barriers and facilitators over the course of adopting a new technological innovation such as PrEP. The human-centered design framework can be particularly effective in helping to recognize and represent the unique contexts and circumstances that shape user behaviors (22). Additional codes were added in the early stages of coding to capture emerging themes. During the coding process inter-coder reliability among the 3 coders (SOR, MH, and NL) was high (>= 80%). A case analysis approach (23) was utilized through which each participant’s PrEP journey, including her DBS results, was reviewed, summarized and memoed. Themes across case analyses and steps of the PrEP journey were highlighted in an analytical matrix, to draw out patterns of use as well as barriers and facilitators; our approach was aligned with the framework analysis method (24). Cases were analyzed by adherence groupings with participants divided based on their adherence patterns from DBS data (Figure 2). Persistence is defined here by staying engaged with PrEP use, meaning medium to high adherence throughout the study, based on DBS results. All findings were discussed by the analytical team (SOR, LM, MH, AVS) to reach consensus.
Figure 1.
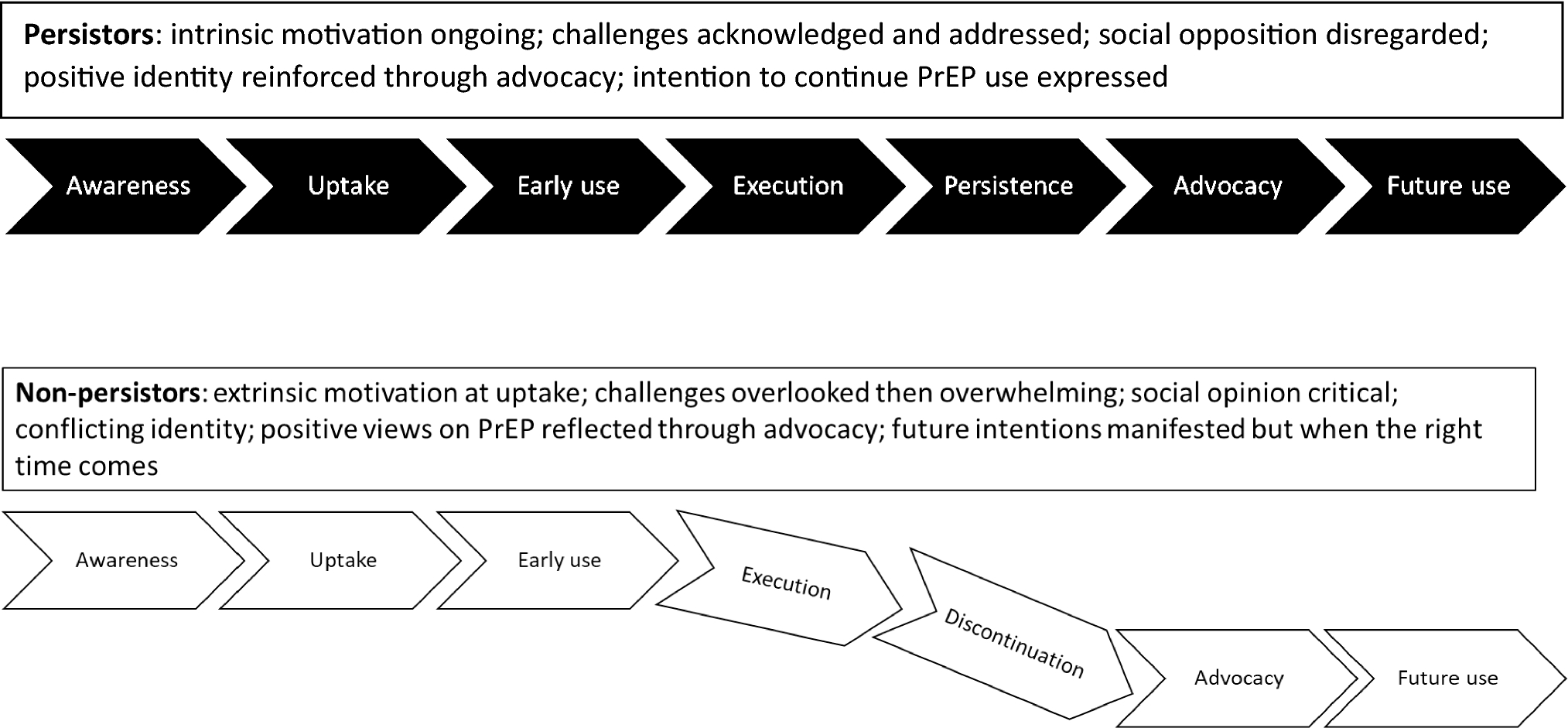
A schematic of the end-user PrEP journey. Each term in these arrows represents a journey code from the larger codebook used for qualitative analysis. Adapted from USAID Project Imbali Journey Map (http://www.engagehcd.com/dpv-ring)
Figure 2.
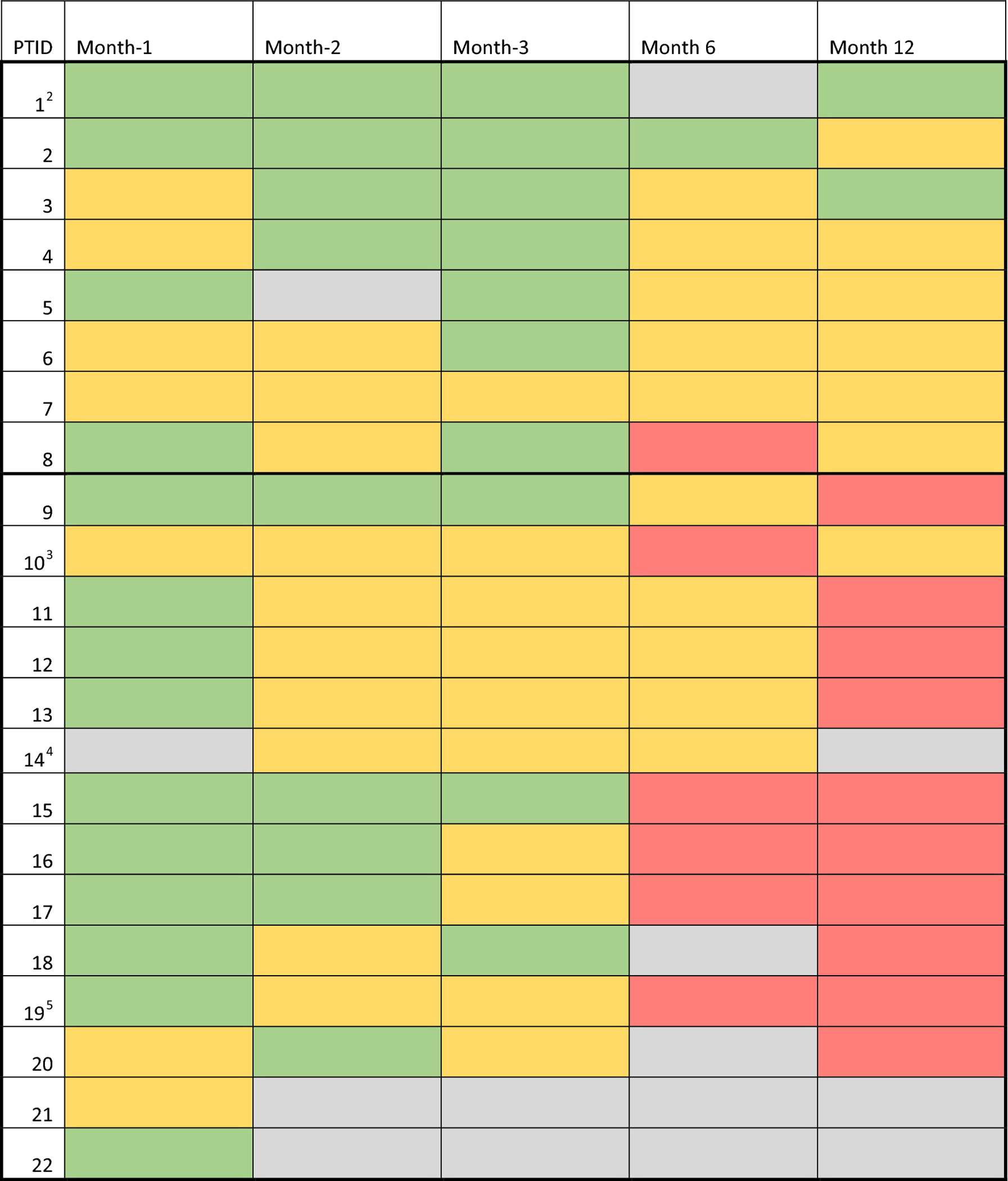
Adherence heat map of the 3P qualitative participants over the 12 months 3P study (n = 22). First box (1–8) represents persistors, second box (9–22) represents non-persistors. Intracelllular TFV-DP levels from DBS as a biomarker of PrEP adherence in the past month were collected at months 1, 2, 3, 6 and 12 (top row) for each participant. Adherence levels are depicted in Green (high adherence: ≥ 500 fmol/punch at M1 and ≥ 700 fmol/punch at any later time point), Yellow (medium adherence: 16.6–499 fmol/punch at M1 and 16.6–699 fmol/punch at any later time point) and Red (low adherence: < 16.6fmol/punch at any time point, which indicates no evidence of product use in the past month, 11). Missed visits or those who refused DBS, are depicted in grey (Color figure online)
Results
Study population
Eighteen of 22 3P qualitative participants completed ≥3 interviews (Table I). Two participants moved away (one after M1, one after M3) and one lost interest in PrEP and stopped attending study visits after M2. Participants were on average 20 years old, approximately half had vaginal sex in the past 30 days, and more than three quarters reported food scarcity in the past 30 days, highlighting one of the many stressors affecting their daily lives.
Table I.
3P qualitative participant characteristics at baseline (N=22)
| Characteristic 1 | N | % |
|---|---|---|
| Total Participants | 22 | 100 |
| Completed at least three interviews2 | 18 | 81 |
| Completed two interviews | 2 | 9 |
| Completed one interview | 2 | 9 |
| Median age, range | 20.5 (16–25) | |
| Completed secondary school | 9 | 41 |
| Food scarcity in past 30 days3 | 17 | 77 |
| Sexual and risk behaviors | ||
| Had a primary sex partner in past 3 months4 | 21 | 96 |
| Does not know primary partner’s HIV status | 8 | 37 |
| Knows that or is unsure if primary partner has sex with others | 20 | 91 |
| Experienced any IPV in the past year | 3 | 14 |
| Had vaginal sex in past 30 days | 12 | 55 |
| PrEP disclosure | ||
| Told anyone about plan to take PrEP | 20 | 91 |
| Person told (n=20): | ||
| friends | 15 | 75 |
| mother or father | 14 | 70 |
| sex partner | 12 | 60 |
| other family member | 12 | 60 |
| sister or brother | 11 | 55 |
| neighbors | 1 | 5 |
| other, unspecified | 4 | 20 |
| nurse or doctor outside the study | 0 | 0 |
| PrEP Persistence classification | ||
| Persistors | 8 | 37 |
| Non-Persistors | 14 | 64 |
The majority of questions were asked upon study enrollment. Exceptions are noted.
One participant received an additional interview (4 total) due to her unique circumstances.
Question asked at study recruitment: “In the past 30 days, how frequently did you worry that your household would not have enough food?”
Question asked at study screening.
Participants’ TFV-DP drug levels over the course of 12 months (Figure 2), reflected varying degrees of persistence with oral PrEP. Participants 1–8 were classified as persistors. Those who used PrEP for less than 12 months (participants 9–22) were classified as non-persistors; six non-persistors used PrEP for 6 months or more, six only during M1-M3, and the remaining two during M1 only (Figure 2).
From uptake to advocacy and future use: behavioral and emotional aspects of the end-user journey
We explored behaviors and attitudes towards PrEP among persistors and non-persistors to distinguish their PrEP journeys (Figure 1). Table II outlines key themes along the PrEP journey, contrasting persistors and non-persistors, and provides illustrative quotes to support these findings.
Table II.
PrEP journey codes & illustrative quotes
| Stage of Journey* | Persistors (PTIDs 1–8) : Key themes & quotes | Non-Persistors (PTIDs 9–22): Key themes & quotes |
|---|---|---|
| Uptake: PrEP awareness & her decision to use it |
Proactive in PrEP uptake: heard about PrEP in community/ from outside source and demonstrated active interest.
“I saw it [PrEP] on the TV. I think it was on World AIDS Day, ja, on the news… some people get infected at the early ages, so I didn’t want to be one of them. So I thought maybe PrEP pill could help me on that.” (PTID 8, age 22) |
Likely to be influenced by peers to join the study.
“I was told by my friend that there is something like PrEP which protects people from getting HIV so I came and joined the study.” (PTID 19, age 19) |
| Early use: the initial month of use, including appraisal and adjustment to taking PrEP |
Reported initial side effects more often than non-persistors; demonstrated will to overcome challenges.
“What was hard for me in the beginning was swallowing the pill. I wasn’t used to it so in the beginning I would put it at the back of my mouth and chase it with water or dissolve it in a spoon so it could be easier. I am used to it now though.” (PTID 5, age 20) |
Most described PrEP as easy in the initial month of use, few reports of side effects/other challenges.
“I thought it was going to be a big challenge but it was not…if you put yourself into it and tell yourself ‘okay fine this is what I wanted so let me just do it’, then it is easy.” (PTID 16, age 22) “I feel happy. I feel like I’m in control of my own safety. So, if I don’t take my pills, then I can get HIV, but if I do, then I don’t. So, ja, it’s up to me.” (PTID 9, age 17) |
| Execution: use of PrEP over the first few months. Self-evaluation of how well she takes her pills as prescribed. |
Developed tactics and strategies to support her PrEP use.
“When I won’t be home- I will know this beforehand- I will know that I need to pack my pills as well. I don’t forget them, when I don’t take them it’s not because I have forgotten, but I have a reason for missing it.” (PTID 8, age 22) |
Adherence dropped, issues with PrEP-related stigma, motivation dwindles, given present-bias.
“So even if I’d think of taking the pill, it’d be like eish, I’m not sick, I don’t see the whole point of taking the pill because I am not sick, and I don’t feel anything, and it’s not like I’m going to be looking for HIV. I won’t be getting it any time soon, so it can wait, I’m going to take it another day. Relax.” (PTID 10, age 19) |
| Persistence: how well she adheres to/persists with PrEP on a longer-term basis (beyond 3 months) |
Persistent: Adherence clubs and strong commitment to self-protection cited as facilitators to long term persistence.
“Meeting other people in the (adherence) club is a motivation, you realize that you are not alone. The discussions are also motivational because you are all on the same page.” (PTID 2, age 24) “My goal was to stay negative, […] and in order for me to stay negative I had to keep on taking PrEP.” (PTID 3, age 25) |
Non-Persistent:
Facing challenges with maintaining commitment to PrEP use, feeling overwhelmed by pill 3-monthly supply, not able to re-engage with PrEP regimen. “I was lazy to take my pill when I was getting my three months’ supply because they were too much, so you would look at them and be lazy.” (PTID 15, age 24) |
| Discontinuation: stopping PrEP, disengaging with journey |
N/A |
Discontinuation due to challenges with pill taking, social opposition or traumatic/unexpected event. Sense of disappointment/failure around inability to continue PrEP use.
“I am not happy that I will no longer continue with the pills because of my mom. She believes in God, she doesn’t believe that I have sex and do other things. She doesn’t want me to take the pills…so I couldn’t take them well. I decided to stop using them.” (PTID 17, age 17) “I feel like I failed the study and I failed myself. It’s just that; that feeling.” (PTID 16, age 22) |
| Advice/Advocacy: advice that she would give/has given to others about PrEP |
Majority encouraged other AGYW, acted as PrEP advocates.
“So, young people believe that studies are not right, but I told my cousin about PrEP. She didn’t want to listen because she hates studies. So, I sat her down and explained about it. In PrEP you can tell the study staff if it’s not suitable for you and ask them to refer you to another study. So, she realized that PrEP is helpful.” (PTID 5, age 20) |
Despite discontinuation, several still recommended PrEP for self-protection.
“I would tell the person [asking about the study] that this is good because it prevents you from getting HIV and as I said it gives you responsibility about your life and what is happening in your life.” (PTID 9, age 17) |
| Future Use: restarting PrEP if she stopped/ continue PrEP after study end |
Expressed desire to continue with PrEP.
“I want to remain safe… I could even use it for the rest of my life.” (PTID 8, age 22) |
Most stated that they would try taking PrEP again if the circumstances that caused them to stop were to change.
“I want to be in control of my body, I want to remain protected even if I get raped.” (PTID 17, age 17) |
Key themes are listed in italics.
code and code description from the codebook.
Persistors appeared proactive with PrEP uptake and often demonstrated intrinsic motivation, which can be described as an internal drive to take PrEP and seeking it through one’s own initiative. Motivation may have been increased by support from others, but for these participants, PrEP use was not dependent on the approval of family, friends, or sexual partners. Side effects (headache, nausea, dizziness) among persistors were salient and often reported during the first month of PrEP use. However, they demonstrated a will to continue PrEP despite initial challenges and most found ways to deal with side effects, such as adjusting the time they took PrEP or seeking help from clinic staff to alleviate side effects. Facilitators to PrEP persistence included attending the study’s PrEP adherence clubs and a strong sense of commitment to reducing their risk of HIV acquisition. Persistors often became PrEP advocates, encouraging other young women in the community to take PrEP and join the 3P study. They typically felt empowered as a PrEP user. Compared to non-persistors, persistors reflected upon the circumstances in their lives and communities that created risk for HIV and responded with a strong commitment to PrEP use despite challenges or social opposition they faced.
PrEP uptake among non-persistors appeared more socially motivated and peer-influenced; many joined 3P because friends told them about it, and a number joined together with friends. Non-persistors indicated being often extrinsically motivated, meaning they were more dependent upon encouragement and validation from others. They appeared focused on personal behaviors that create risk for HIV, and some described stigmatizing views of sexual activity among young women. Non-persistors commonly described PrEP as easy to use initially, but later struggled with remembering to take pills and several said that they felt overwhelmed by the three months’ supply given at quarterly visits. Non-persistors were more likely to report that their PrEP use was derailed by social opposition or unexpected events. The behaviors and emotions of non-persistors were more reactive than proactive; they demonstrated less self-reflection and resiliency in their commitment to PrEP compared to persistors. Their adherence was more likely to be impacted by external challenges or conflicts, and discontinuation was largely viewed as unintentional. Many described factors out of their control that caused them to stop PrEP, such as social opposition or an unexpected change in circumstance like travel or disruption of daily routine. Non-persistors appeared more conflicted about their identities as PrEP users, which were often linked to their inability to persist and a sense of failure. Nevertheless, they expressed interest in taking PrEP in the future if their current challenging circumstances for PrEP use were to change, and several advocated PrEP to other friends, suggesting positive views about PrEP despite having discontinued it.
We also investigated the emotional dimension of the PrEP journey in addition to attitudes and behaviors, as emotional states were central to the AGYW’s overall PrEP experience. The following domains were especially rich: a) motivations to initiate and persist with PrEP, and whether the drive was mostly intrinsic vs. extrinsic, b) perception of risk and vulnerability to HIV (note: HIV risk refers to personal behavior that increases susceptibility to HIV infection; vulnerability refers to one’s felt susceptibility to HIV infection, which is not necessarily correlated with behavior (25)); and c) forming an identity as a PrEP user (Figure 1). For many participants, motivation, risk perception, and identity formation were connected thoughout the course of their PrEP journey, and two main trajectories emerged. One trajectory, often demonstrated by persistors, was that of intrinsic motivation to take PrEP and positive identity formation (in harmony with core beliefs and values) where HIV risk is related to the high prevalence in the community. The second trajectory, more likely represented by non-persistors, is one of extrinsic motivation to take PrEP, HIV risk is linked to more personal (and stigmatized) behaviors, and conflictual feelings around their identity as a PrEP user.
The case studies of participants, ‘Fezeka’ (persistor) and ‘Zola’ (non-persistor), from the two persistence groups were purposively selected as they characterized key aspects of identified different trajectories, alongside the end-user journey. For confidentiality purposes, all names given are pseudonyms.
Case 1: intrinsic motivation and positive identity formation
Fezeka (PTID 1, age 24) was motivated to join the study because she felt at risk for HIV due to her partner’s infidelity and his refusal to use condoms. She described her partner as someone who does not care about HIV. Although she said she loved him, she also said their relationship was not good; she portrayed him as dishonest, having other girlfriends, and as a heavy drinker. Discussing her need for PrEP, Fezeka explained, “I hated that we weren’t using condoms. I tried talking to him for us to start using condoms, but he said I was cheating. I kept my mouth shut after that and just came to the [research] centre, so that even if there is no condom use, I know I am okay on my side.” Fezeka’s decision to use PrEP was one of taking her sexual health into her own hands. She has a young daughter, and this motivated her to stay healthy: “I wish I could die when my child has grown up, so then I wish to continue with PrEP as the person I am.” Her mother, cousin, aunt and uncle are living with HIV, and she wanted her life to be different; Fezeka’s drive to protect herself was increased by exposure to multiple family members living with HIV.
Fezeka reported challenges with taking PrEP which she overcame. Specifically, she initially had a hard time swallowing the large pill, did not like the taste it left in her mouth, and sometimes felt nauseous. She needed to overcome broader anxiety issues about taking pills, as at a younger age she had attempted suicide by overdosing with diabetes medication. Before she started PrEP, she had avoided taking pills of any kind. She learned that breaking the PrEP tablets in half made them easier to swallow, which helped her take PrEP every day from the outset. Fezeka shared her perception that taking PrEP improved her overall health, “I no longer suffer from headaches and I do not fall sick often as compared to before joining PrEP.” In the first six months of the study she forgot her pill a few times, but said she became very committed in the last six months and was never forgetting to take the pill. At one point, her partner tried to convince her to stop taking PrEP so they could conceive, but she refused this would require her to stop PrEP (South African policy at the time stipulated that PrEP should not be allowed during pregnancy). Being in the study increased feelings of safety and taught her about self-care, as she learned “to love me before I love anybody else.” Fezeka felt confident in her decision to take PrEP and was not concerned with other’s misconceptions around PrEP: “I know who I am, I know about the study even though people were saying that I will have HIV; though I am taking a pill, I was able to stand against that and tell them that is not going to happen.”
Fezeka expressed a desire to continue PrEP use for another ten years and was concerned the study was ending: “while I was taking my PrEP I did not have any worries; no matter what happens I knew I was safe.” Reflecting on her journey, she said that she didn’t receive much support from anyone in her life around PrEP use; she saw it as a self-motivated experience.
Case 2: Changing motivation and conflicting identity
Zola (PTID 19, age 19) learned about PrEP for the first time from a friend and decided to join the 3P study along with two other friends. Her motivation to use PrEP stemmed from a recent incident of rape during a break-in; she described condom use with her partner as “off and on”, but was most concerned about getting HIV from rape and wanted to feel protected. Zola told her siblings and cousins soon after she began using PrEP and they were all supportive and often reminded her to take the pill. She also disclosed her PrEP use to her partner, who supported her by giving her pill reminders and even expressed interest in taking PrEP himself. In the initial month of use, Zola felt there was nothing difficult about taking PrEP and said, “I take it every day because I know I will be protected.” Her drug level for M1 reflected high adherence (green, Figure 2).
After M1, Zola developed a rash on her face. The clinic gave her a cream but it did not help and she decided to take short break from PrEP. Then she travelled to another part of the country over the December holidays and forgot to take her pills with her. Zola described her sense of unease around being completely without PrEP: “I didn’t feel good because I knew it would be a while before I come back and I was worried that I wouldn’t have any in my body. I was also concerned about how it would be like when I take them again.” Upon her return, she went to the clinic and received PrEP refills, but her initial motivation and dedication waned. Zola struggled to take the pill daily and said that she experienced nausea and had difficulty swallowing the pill. She said she was “forgetting most of the time” and lost social support, as her family members stopped reminding her and she was no longer friends with the girls she joined 3P with. Her sister told her that she was “messing up her life” by stopping PrEP, and she felt that her partner lost interest in her when she stopped taking her pills. This perceived shift in their relationship created doubts about her partner’s sexual behavior: “I used to know my partner but not anymore, so now I am not sure what he is doing when I am not around.” Zola had low adherence at M6 and by M12 she was no longer on PrEP; she stopped completely when she could not find her pills and she didn’t return to the clinic for a resupply. She reported that she would prefer a form of HIV prevention that stays in the body for longer (e.g. injectable), but also maintained she would be interested in using PrEP again because of its protection, as she said “I will continue forever, I won’t stop.” These statements reveal conflict between her experience with PrEP and her aspirations of use. Despite her early discontinuation, Zola recommended PrEP to two of her friends and said that she would tell others about the benefits and challenges of PrEP use.
Impact of motivation, risk response, and identity formation on PrEP use
The case studies of Fezeka and Zola highlight key differences in motivations, responses to sense of HIV risk, and formation of one’s identity as a PrEP user. Like Fezeka, other PrEP persistors described a process of acknowledging circumstances that create risk for HIV, then reflecting on these conditions and responding in a proactive manner. High HIV prevalence in the community and among family members, mistrust of sexual partners, and fear of sexual violence enhanced feeling susceptible to HIV. Persistence contributed to an optimistic outlook about the future, positive emotions, and empowerment, as one persistor stated, “I feel like a brave woman who can stand up for herself, because I’m able to protect myself. I don’t need anyone to protect me. I can protect myself with PrEP.” (PTID 3, age 25) Bongi, another persistor, highlighted the role of intrinsic motivation: “the greatest support is to motivate myself, by staying HIV free and taking PrEP.” (PTID 2, age 24) After starting PrEP, Bongi stopped going out drinking and having one-night stands. Describing the transformative experience of taking PrEP, she asserted, “I am now a dignified person, even people have noticed that I am no longer the girl I used to be. They want to know what happened to me and where I live. I now have a job, something that people never thought would happen.” The negative rumors about PrEP in her community did not deter her; she felt proud to be a PrEP user and had a strong sense of protection: “I don’t have to worry about HIV infection. I know that PrEP is protecting me.”
Zola struggled between her lived experience of PrEP use and her aspirations to feel protected and commit to PrEP. Other non-persistors revealed tensions between different aspects of their personae and their newfound identity as PrEP users. Zintle (PTID 21, age 22) started off with strong motivation and felt inspired to be part of the movement towards a future without HIV. Although she admitted to struggling with the daily regimen, when Zintle was informed that her drug level for M1 was medium (Figure 2), she became frustrated and immediately refused taking PrEP. Like Zola, her narrative reveals a struggle between the type of PrEP user she aspired to be and her own challenges in adhering to PrEP. Two non-persistors described how cultural traditions led them to stop taking PrEP. Vuyo received a calling to become a traditional healer a few months into her PrEP journey. (PTID 16, age 22) Family members asked her to stop PrEP as they believed it would conflict with the initiation rituals that she needed to go through. Vuyo felt disappointed when discontinuing PrEP to begin the process of becoming a traditional healer, but found it important to honor this part of her identity and ancestral traditions. Thandiwe also stopped taking PrEP for cultural reasons when her elders said that PrEP would conflict with the traditions of a coming of age initiation ritual she took part in. (PTID 20, age 19) Most non-persistors described some form of identity conflict or challenge that led to their PrEP discontinuation.
Unpredictability of life and impact on PrEP
Several participants experienced traumatic events that impacted their PrEP use. Zenande adhered well for the first three months of the study, but then her mother and partner passed away. Losing two loved people who supported her PrEP use negatively affected her adherence—”I needed someone to give me that courage.” (PTID 9, age 17) She eventually moved to Johannesburg to stay with relatives and discontinued PrEP, as she felt her relatives would not be supportive. When Lindiwe initially told her boyfriend about PrEP, he revealed insecurities that her PrEP use meant she was having other partners and asked her to stop, but she refused. (PTID 10, age 19) One day, he tried to commit suicide by overdosing on her PrEP pills and she found him as he was taking them. Lindiwe felt pressured by her partner to discontinue PrEP, as they were living together and she didn’t feel that she could continue after this event. Participants described other unpredicted events that led to discontinuation such as relocation or becoming pregnant. For Sisipho, first, she unexpectedly stayed with her sick child in the hospital and had no pills with her, then she travelled to her home in a rural area and received stigmatizing remarks about being HIV-positive, which she found very discouraging. (PTID 11, age 24) These led to gaps in use and an eventual stop.
Discussion
This qualitative study followed the behavioral, attitudinal and emotional journeys of PrEP use among AGYW in Cape Town, South Africa during a twelve month PrEP implementation study. Through a longitudinal analysis of the experiences of AGYW who persisted or did not persist with PrEP over 12 months, at least two distinct trajectories of PrEP use were identified. These highlighted the importance of one’s source of motivation, including personalizing risk, the value of recognizing and persevering through early challenges with use, and the importance of aligning one’s personal identity with PrEP taking behavior. External factors such as levels of support from family, traumatic and unexpected events also shaped young women’s PrEP journey. Even though nearly two thirds of participants discontinued PrEP by six months, taking PrEP was described as an overall positive experience and many expressed interest in future PrEP use, as they viewed PrEP as an self-empowering tool for HIV prevention.
While both intristic and extrinsic motivation can be useful to change behavior, this study revealed that AGYW who expressed intrisincally driven motivations for using PrEP appeared more successful at maintaining use, particularly when faced with early challenges such as side effects. This is consistent with other evidence on behavior change among young people, indicating that intrinsic motivation leads to more sustained behavioral change (26). The PRIME theory of motivation recognizes the influence of both automatic and reflective processes and suggests that lasting motivation requires a strong internal need to enact the behaviors required to meet the desired outcome; this drive must be sufficient to overcome competing wants or needs (27). The motivation must be purposive and deliberate and the behavior being enacted should be viewed as a positive aspect of one’s identity and respected by others. It’s important to note that there are a number of reasons why one may join a research study, some are personal such as the health services provided, visits reimbursements, or the “promise of a better life”, and others are altruistic, like stopping the spread of HIV (28, 29). In the 3P study, there was the potential added motivation to earn modest cash incentives for PrEP use in the incentive group (18), social validation and peer support through adherence groups and through TFV-DP drug levels. Participants reported that receiving incentives did not significantly impact their motivation to use PrEP; TFV-DP levels revealed a non-significant higher adherence among participants who received incentives during the first three months of the study (18). The desire to take PrEP in order to be a responsible young woman was expressed by many AGYW in this study. Several non-persistors revealed greater tensions between their aspirations and experiences of use, which may have impacted their comfort in discussing early challenges like side effects with study staff therefore challenging their continued use. Recognizing the different motivations that lead young women to oral PrEP studies is key for tailoring adherence support approaches. For example, participants who are more extrinsically motivated to use PrEP may need additional support when faced with stigma or disapproval from partners, family, and others in their community.
Acknowledgment of one’s risks and/or vulnerability to HIV appeared important in motivation to use PrEP. Participants who held stigmatizing views of young women’s risk behavior as well as their own, were less likely to create an empowered identity as a PrEP user and persist with PrEP for 12 months. While acknowledging that HIV risk perception can be an important motivator for PrEP adherence, internalized sexual stigma and notions of the self as a risky person can be difficult to simultaneously balance in order to view PrEP in a positive, empowering way (30). Personalizing risk may contribute to motivation, but internalized stigma can create disconnect between one’s self-perception and aspirational identity as an empowered PrEP user.
Beyond these internal factors contributing to AGYW’s PrEP journey, they were also influenced by factors operating at the household, social and community levels, as previously reported (31, 32), particularly given the high levels of stress, violence and trauma they experienced in their daily lives. In an open-label trial, Amico (33) reported that high adherence was related to a strong sense of alignment between individual and community values around PrEP, or when participants felt strongly enough about their decision to use PrEP that they did not require much social support or validation from the community. In the 3P study, a positive PrEP identity combined with ongoing intrinsic motivation was pivotal and led to PrEP persistence. In contrast, conflicts between one’s identity as a PrEP user and cultural/community values often led to discontinuation, as did stigma caused by being mistaken as HIV positive due to taking a daily medication that appears identical to the most common medication used for HIV treatment. The negative influence of stigma on PrEP use has been previously documented among African AGYW, particularly early after PrEP initiation; however, evidence also suggests that counselling and adherence clubs can aid in overcoming the consequences of perceived or experienced stigma (34).
This study has several limitations, including the small sample size of 22 of 200 AGYW in the 3P trial participating in the longititudinal IDIs. However, for qualitative studies, this sample is sufficient to reach data saturation (35). Furthermore, the longitudinal dataset generated rich insights to probe different aspects of the PrEP journey. The first two interviews, conducted at month one and three, were close in time; this data provided strong insights into the early stages of the journey. We had a gap between the month three and the month twelve interviews. Many participants discontinued PrEP by month six and it would have been beneficial to interview them closer to their time of discontinuation, especially as study visits frequency decreased to quarterly from monthly after month three. The last interview may have suffered from recall bias. Social desirability bias may have been a factor in this study. Since participants knew adherence was desired within the study—and even rewarded through financial incentives—it is possible that some may have felt disinclined to report challenges or exaggerated their commitment and adherence to PrEP, believing this was what study staff wanted to hear. At the start of each interview, participants were encouraged to share their honest experience and the importance of being non-judgmental was emphasised during interviewer training. Since we had drug level data, there was less incentive to lie about adherence and we had several reports of non-adherence, which supports the reliability of the data.
In summary, our study is among the first to explore the PrEP journey of AGYW in SSA. Our findings highlight the importance of understanding how internal factors and external circumstances intermingled and impacted women’s trajectories of use. Recognizing the different motivations that may lead young women to take oral PrEP and the range of emotional and behavioral issues affecting adherence will help programme implementors in tailoring interventions and counselling approaches to meet young women’s multifaceted needs. For example, specific support modules could address a range of factors, e.g. dealing with IPV (36), unsupportive family members (17), low motivation, and difficulties with habit formation. One size doesn’t fit all when it comes to AGYW’s needs. Our findings highlight the social and emotional dimensions of PrEP use and the importance of considering this impact on the end user experience.
Acknowledgements:
We would like to thank Dr Eve Mendel, Jacqui Dallimore, Lauren Fynn, Ntombomzi Mcanjana, the study team for the passion and care they put into this study, and the young women who participated in this study. This study was supported by the National Institutes of Health (1R01MH107251). Writing of this manuscript was supported in part by internal funds from RTI International. The content is solely the responsibility of the authors and does not necessarily represent the official views of the authors’ employers or funders.
Compliance with ethical standards:
The study protocol was reviewed and approved by the University of Cape Town Human Research Ethics Committee (HREC). All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Conflict of interest:
Dr. Connie Celum reports grants from NIH and has served as a scientific advisor to Merck and Gilead Science.
Footnotes
Informed consent:
Informed consent was obtained from all individual participants included in the study.
http://www.engagehcd.com/dpv-ring/ [note that the journey map is in the asset folder library 1]
References
- 1.UNAIDS. Miles to go: closing gaps, breaking barriers, righting injustices. Geneva: Joint UN Programme on HIV/AIDS; 2018. [Google Scholar]
- 2.UNAIDS. Global report: UNAIDS report on the global AIDS epidemic. Geneva; 2013. [Google Scholar]
- 3.UNAIDS. The Gap Report. Switzerland; 2014. [Google Scholar]
- 4.UNAIDS. South Africa: Country Overview. 2018.
- 5.Ahmed K, Baeten JM, Beksinska M, Bekker L-G, Bukusi EA, Donnell D, et al. HIV incidence among women using intramuscular depot medroxyprogesterone acetate, a copper intrauterine device, or a levonorgestrel implant for contraception: a randomised, multicentre, open-label trial. The Lancet. 2019;394(10195):303–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Donnell D, Baeten JM, Bumpus NN, Brantley J, Bangsberg DR, Haberer JE, et al. HIV protective efficacy and correlates of tenofovir blood concentrations in a clinical trial of PrEP for HIV prevention. Journal of acquired immune deficiency syndromes 2014;66(3):340–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Celum CL, Delany-Moretlwe S, Baeten JM, van der Straten A, Hosek S, Bukusi EA, et al. HIV pre-exposure prophylaxis for adolescent girls and young women in Africa: from efficacy trials to delivery. Journal of the International AIDS Society. 2019;22 (Suppl 4):e25298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hanscom B, Janes HE, Guarino PD, Huang Y, Brown ER, Chen YQ, et al. Brief Report: Preventing HIV-1 Infection in Women Using Oral Preexposure Prophylaxis: A Meta-analysis of Current Evidence. Journal of acquired immune deficiency syndromes 2016;73(5):606–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Celum C, Mgodi N, Bekker L, Hosek S, Donnell D, Anderon P, editors. Adherence 3 months after PrEP initiation among young African women in HPTN 082. Conference on Retroviruses and Opportunistic Infections (CROI); 2019. [Google Scholar]
- 10.Amico KR, Mansoor LE, Corneli A, Torjesen K, van der Straten A. Adherence support approaches in biomedical HIV prevention trials: experiences, insights and future directions from four multisite prevention trials. AIDS and behavior. 2013;17(6):2143–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.van der Straten A, Montgomery ET, Musara P, Etima J, Naidoo S, Laborde N, et al. Disclosure of pharmacokinetic drug results to understand nonadherence. AIDS (London, England). 2015;29(16):2161–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ndase P, Celum C, Campbell J, Bukusi E, Kiarie J, Katabira E, et al. Successful discontinuation of the placebo arm and provision of an effective HIV prevention product after a positive interim efficacy result: the partners PrEP study experience. Journal of acquired immune deficiency syndromes 2014;66(2):206–12. [DOI] [PubMed] [Google Scholar]
- 13.Gomez A, Malone S, Prasad R, Gangaramany A, Croucamp Y, Mulhausen J, et al. Understanding HIV prevention in high- risk adolescent girls and young women in two South African provinces. South African Health Review. 2019:167–72. [Google Scholar]
- 14.Albert D, Chein J, Steinberg L. Peer Influences on Adolescent Decision Making. Curr Dir Psychol Sci. 2013;22(2):114–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Okonkwo PI, Fatusi AO, Ilika AL. Perception of peers’ behaviour regarding sexual health decision making among female undergraduates in Anambra State, Nigeria. African health sciences. 2005;5(2):107–13. [PMC free article] [PubMed] [Google Scholar]
- 16.Tomé G, Matos M, Simões C, Diniz JA, Camacho I. How can peer group influence the behavior of adolescents: explanatory model. Glob J Health Sci. 2012;4(2):26–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Roberts ST, Khoza N, Rousseau-Jemwa E, Omollo V, Morton J, Bekker LG, et al. “As long as my mother supports me, then I am okay”: Family influences on oral PrEP use among adolescent girls and young women in Kenya and South Africa. Adherence Conference; June 17–19, 2019; Miami, Florida. [Google Scholar]
- 18.Celum C, Gill K, Morton J, Stein G, Myers L, Thomas K, et al. Incentives conditioned on tenofovir levels to support adherence among young South African women: a randomized trial. Journal of the International AIDS Society. 2020. (publication forthcoming). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.MASICORP. About Masiphumelele: Health- TB and HIV 2018. [Available from: https://www.masicorp.org/masicorp/about-masiphumelele/.
- 20.City of Cape Town – 2011 Census Suburb Masiphumelele [Internet]. 2011. Available from: http://resource.capetown.gov.za/documentcentre/Documents/Maps%20and%20statistics/2011_Census_CT_Suburb_Masiphumelele_Profile.pdf.
- 21.Morton JF, Myers L, Gill K, Bekker L-G, Stein G, Thomas KK, et al. Evaluation of a behavior-centered design strategy for creating demand for oral PrEP among young women in Cape Town, South Africa. Gates Open Research. 2020;4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tolley E Traditional Socio-Behavioral Research and Human-Centered Design: Similarities, Unique Contributions and Synergies. FHI; 360 December 31, 2017. [Google Scholar]
- 23.Stern E, Clarfelt A, Buikema R. The Use of Sexual History Narratives to Assess Processes of Hegemonic Masculinity among South African Men in the Context of HIV/AIDS. Men and Masculinities. 2014;18(3):340–62. [Google Scholar]
- 24.Srivastava A, Thomson SB. Framework analysis: A qualitative methodology for applied policy research. Journal of Administration and Governance. 2009;4(2):72–9. [Google Scholar]
- 25.Bradley H, Tsui A, Hindin M, Kidanu A, Gillespie D. Developing scales to measure perceived HIV risk and vulnerability among Ethiopian women testing for HIV. AIDS care. 2011;23(8):1043–52. [DOI] [PubMed] [Google Scholar]
- 26.Larson RW, Rusk N. Chapter 5 - Intrinsic Motivation and Positive Development. In: Lerner RM, Lerner JV, Benson JB, editors. Advances in Child Development and Behavior. 41: JAI; 2011. p. 89–130. [DOI] [PubMed] [Google Scholar]
- 27.West R, Michie S, Rubin GJ, Amlôt R. Applying principles of behaviour change to reduce SARS-CoV-2 transmission. Nature Human Behaviour. 2020;4(5):451–9. [DOI] [PubMed] [Google Scholar]
- 28.Stadler J, Scorgie F, van der Straten A, Saethre E. Adherence and the Lie in a HIV Prevention Clinical Trial. Med Anthropol. 2016;35(6):503–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Katz AW, Mensch BS, Woeber K, Musara P, Etima J, van der Straten A. Understanding women’s motivations to participate in MTN-003/VOICE, a phase 2b HIV prevention trial with low adherence. BMC women’s health. 2019;19(1):18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hartmann M, McConnell M, Bekker LG, Celum C, Bennie T, Zuma J, et al. Motivated Reasoning and HIV Risk? Views on Relationships, Trust, and Risk from Young Women in Cape Town, South Africa, and Implications for Oral PrEP. AIDS and behavior. 2018;22(11):3468–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.van der Straten A, Stadler J, Luecke E, Laborde N, Hartmann M, Montgomery ET. Perspectives on use of oral and vaginal antiretrovirals for HIV prevention: the VOICE-C qualitative study in Johannesburg, South Africa. Journal of the International AIDS Society. 2014;17(3 Suppl 2):19146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.van der Straten A, Stadler J, Montgomery E, Hartmann M, Magazi B, Mathebula F, et al. Women’s experiences with oral and vaginal pre-exposure prophylaxis: the VOICE-C qualitative study in Johannesburg, South Africa. PloS one. 2014;9(2):e89118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Amico KR, Wallace M, Bekker LG, Roux S, Atujuna M, Sebastian E, et al. Experiences with HPTN 067/ADAPT Study-Provided Open-Label PrEP Among Women in Cape Town: Facilitators and Barriers Within a Mutuality Framework. AIDS and behavior. 2017;21(5):1361–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Velloza J, Khoza N, Scorgie F, Chitukuta M, Mutero P, Mutiti K, et al. The influence of HIV-related stigma on PrEP disclosure and adherence among adolescent girls and young women in HPTN 082: a qualitative study. Journal of the International AIDS Society. 2020;23(3):e25463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Guest G, Bunce A, Johnson L. How Many Interviews Are Enough?: An Experiment with Data Saturation and Variability. Field Methods. 2006;18(1):59–82. [Google Scholar]
- 36.Hartmann M, Lanham M, Palanee-Phillips T, Mathebula F, Tolley EE, Peacock D, et al. Generating CHARISMA: Development of an Intervention to Help Women Build Agency and Safety in Their Relationships While Using PrEP for HIV Prevention. AIDS Educ Prev. 2019;31(5):433–51. [DOI] [PMC free article] [PubMed] [Google Scholar]


