Abstract
Objective To translate into Brazilian Portuguese and to cross-culturally adapt the Banff Questionnaire for Patellar Instability.
Methods The translation and cross-cultural adaptation followed the linguistic validation process proposed by international guidelines, which consists of six steps: translation, synthesis, back-translation, review by an expert committee, pretest, and final report presentation to the authors of the original questionnaire. Literate patients with recurrent patellar instability, older than 12 years of age, who signed the informed consent form or had it signed by a legal guardian were included in the study. Patients with neurological or systemic comorbidities were excluded from the study.
Results A total of 62 patients (18 males and 44 females) were included in the study. Discrepancies observed during the processes of translation and harmonization of the back-translations were modified with no need for reformulation. No pretest version replacements were required.
Conclusion The Banff Questionnaire for Patellar Instability has been successfully translated and cross-culturally adapted into Brazilian Portuguese, so it can be used to assess patients with patellar instability who speak this language.
Keywords: patellar dislocation, quality of life, surveys and questionnaires, transcultural adaptation, translation
Introduction
Patellar instability is an important knee condition not only because of its incidence – in the United States, annual estimates are 29/100 thousand people in the general population, 1 reaching 77/100 thousand people in some risk groups – 2 but also for recurring in most patients, 1 in rates ranging from 17% to 70% in selected groups. 3 4 In addition, it essentially affects the youngest, most active members of society, with a peak incidence between the ages of 15 to 19 years, 3 resulting in an economic impact regardless of the proposed treatment method. 5
Although common during sports activities, 4 atraumatic mechanisms are reported in individuals with predisposing conditions. 6 Patellar instability is sometimes accompanied by limitations regarding recreational or sports activities, and reduced quality of life. 7 8 Since patellar instability is a multifactorial condition, 1 2 3 4 5 6 7 8 9 it can be managed with several therapeutic options according to the patient's anatomical features and individual presentation. 10
The assessment of the therapeutic outcomes using clinical and radiographic criteria alone may underestimate the impact of the disease on the daily life of the patient. The health status should take into consideration the influence of the clinical condition in different daily life, work, recreation, sports and social scenarios. 11 12 The assessment instruments to address the therapeutic effectiveness and impact on the quality of life have been designed to broaden our understanding regarding health care outcomes. 13
Questionnaires such as the Kujala 14 and International Knee Documentation Committee Subjective Knee Evaluation Form (IDKC) 15 are already established in the literature as tools for this kind of clinical application. While the IKDC assesses a wide variety of knee conditions, the Kujala questionnaire is more specific to patellofemoral joint disorders, since it specifically documents patellofemoral pain. Even so, the daily subjective limitations experienced by these patients might not be fully understood, hindering the evaluation of the clinical interventions. 16 17
Hiemstra et al. 18 developed the Banff Questionnaire for Patellar Instability 7 18 to assesses the quality of life of these patients in terms of symptoms and functional, social, and economic activities. The present study aimed to translate and cross-culturally adapt the Banff Questionnaire into Brazilian Portuguese.
Methodology
The present study was initiated after approval by the Ethics in Research Committee under number CAAE 70103717.3.0000.5505. Data was collected from the Knee Group outpatient clinic of our institution. Literate patients with recurrent patellar instability, older than 12 years of age, who signed the informed consent form or had it signed by a legal guardian were included in the present study. Patients with neurological or systemic comorbidities were excluded from the study.
Sample size was calculated based on the number of variables analyzed, as recommended in the literature, and set at a minimum of 62 patients, that is, twice the number of questions contained in the Banff instrument. 19
In total, 62 patients with recurrent patellar instability participated in the present study. The diagnosis was established by a history of at least two episodes of patellar dislocation observed by the patient or third parties, along with the findings of the clinical examination and imaging tests, as described by Brattstroem. 20
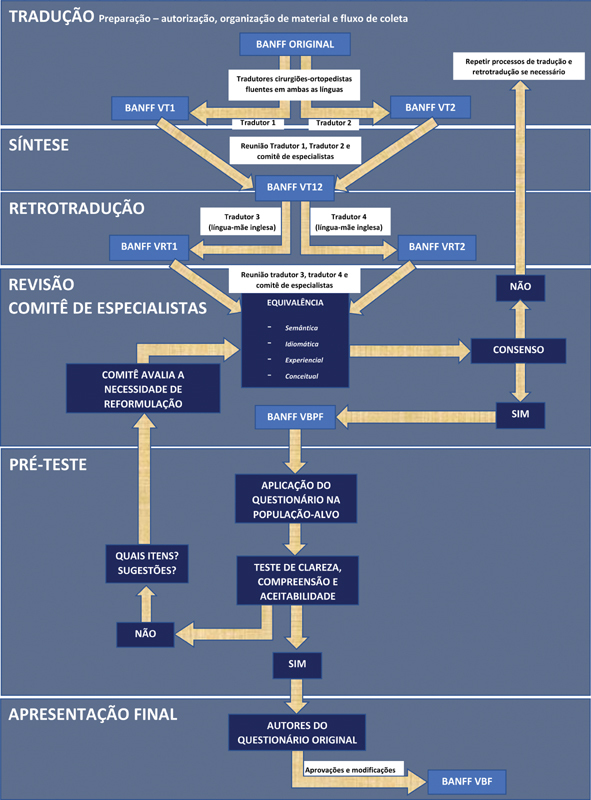
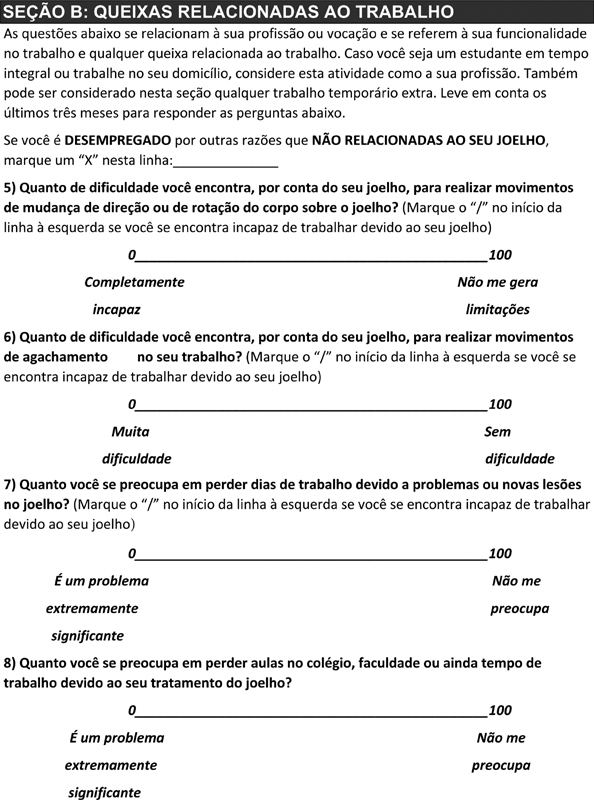
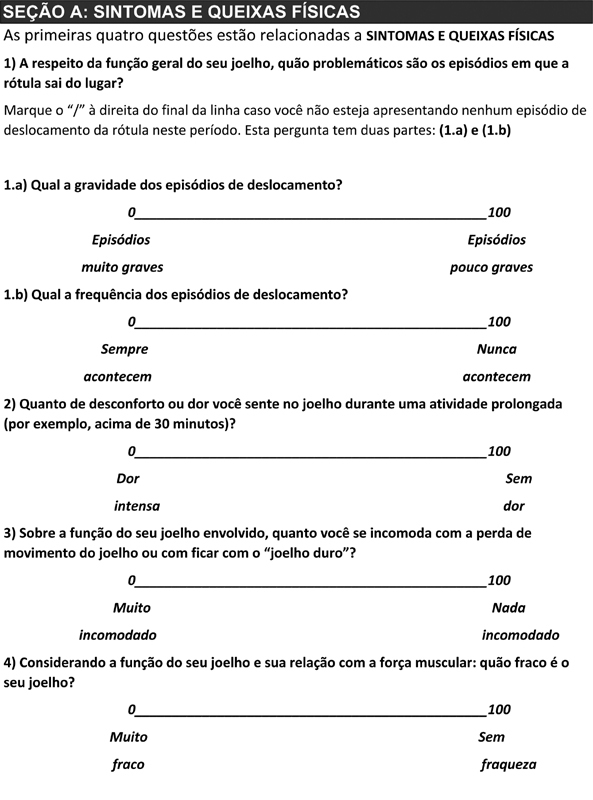
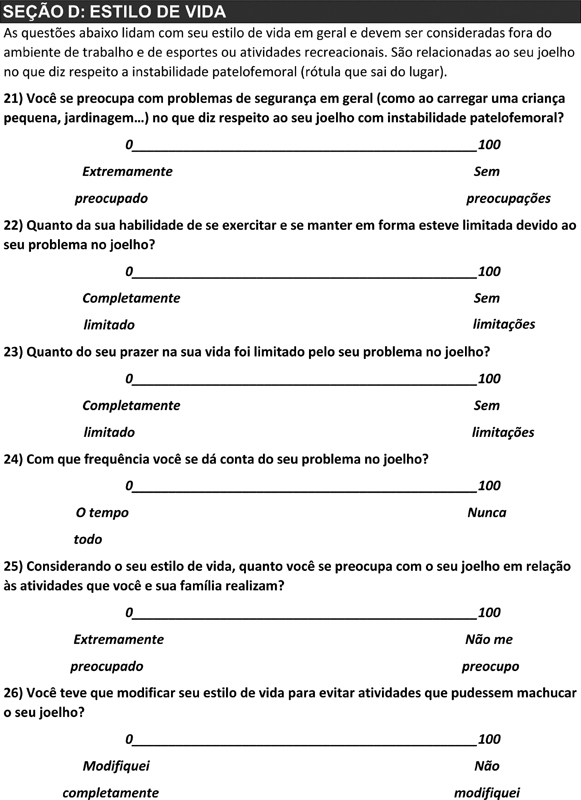
The translation and cross-cultural adaptation of the Banff Questionnaire for Patellar Instability into Brazilian Portuguese followed the internationally accepted linguistic validation process described by Guillemin et al. 21 and modified by Beaton et al. 22 23 Linguistic validation aims to generate a translation that is both equivalent to the original text and comprehensible by the target population. The method used in the present study is described below ( Figure 1 ).
Fig. 1.
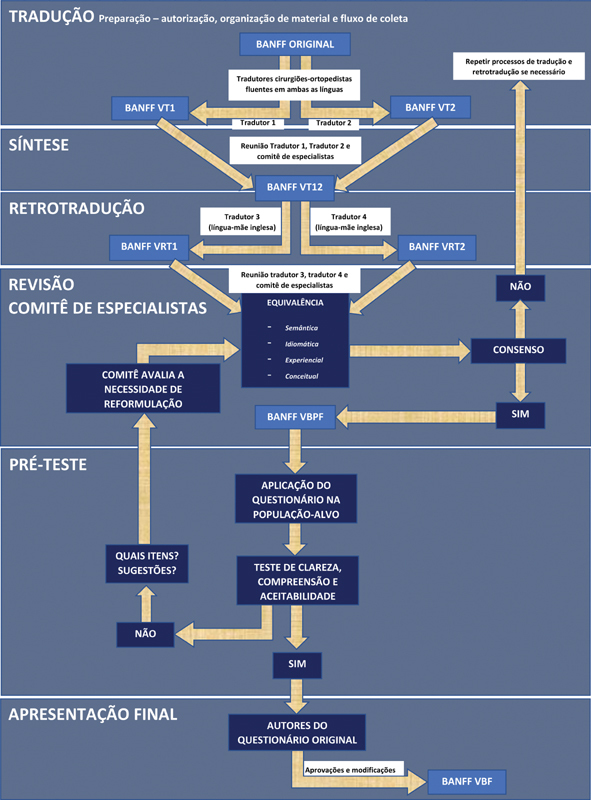
Flowchart of the linguistic validation of the Brazilian Portuguese version of the banff questuionnaire. Abbreviations: VT1, translated version 1; VT2, translated version 2; VT12, translated version 12; VRT1, back-translated version 1; VRT2, back-translated version 2; VBPF, Brazilian Portuguese prefinal version; VBF, Brazilian Portuguese final version.
Translation: the translation started after obtaining the authorization to use the questionnaire by the authors of the original article, the review of the questionnaire items and organization of the material and the data collection flow, that is, the “Preparation” process. The 32 questions, instructions, answer options and other items from the original questionnaire in English were independently translated into Portuguese by 2 Brazilian orthopedic surgeons fluent in both languages, resulting in 2 translated texts (Banff VT1 and Banff VT2).
Synthesis: both versions were compared by an expert committee, resulting in “Banff Version T12” (Banff VT12).
Back translation: the Banff VT12” was back translated by two native English speakers who were also fluent in Portuguese, and blinded as to the original questionnaire and with no knowledge of the subject. The aim of this stage was to find conceptual translation errors and gross inconsistencies from the previous steps and to generate two “back-translated versions” (Banff VRT1 and Banff VRT2).
Expert committee review: a new meeting including the third and fourth translators and the same expert committee was held to search for inconsistencies and check correspondences between the back-translated texts (Banff VRT1 and Banff VRT2), the initial translation (Banff VT12), and the original questionnaire. The harmonization of discrepancies, seeking semantic, idiomatic, experiential, and conceptual equivalence between the texts, resulted in a “Banff Brazilian Prefinal Version” (in Portuguese, “Banff Versão Brasileira Pré-Final”, VBPF). This text consolidated all information produced so far in an easily understandable instrument used at the pretest with the sample from the study.
Pretest: this step was carried out at the Knee Group's outpatient clinic at Hospital São Paulo, Orthopedics and Traumatology Department, Escola Paulista de Medicina, Universidade Federal de São Paulo (UNIFESP), using the “Banff VBPF” and a probing technique: 21 after the application of the questionnaire, each patient was individually surveyed for clarity, understanding and acceptability of each item from the instrument. Doubts or suggestions would require an item reformulation to be discussed with the committee; otherwise, we would proceed to the last step.
Presentation of the final version to the authors of the original questionnaire: reports prepared during all steps of the process were submitted along with discrepancies and the committee consensus on each Banff VBPF item. The main author of the original questionnaire approved this version with no suggestions or changes. The Banff VBPF was then renamed “Banff Brazilian Final Version” (in Portuguese, “Banff Versão Brasileira Final”, VBF).
Results
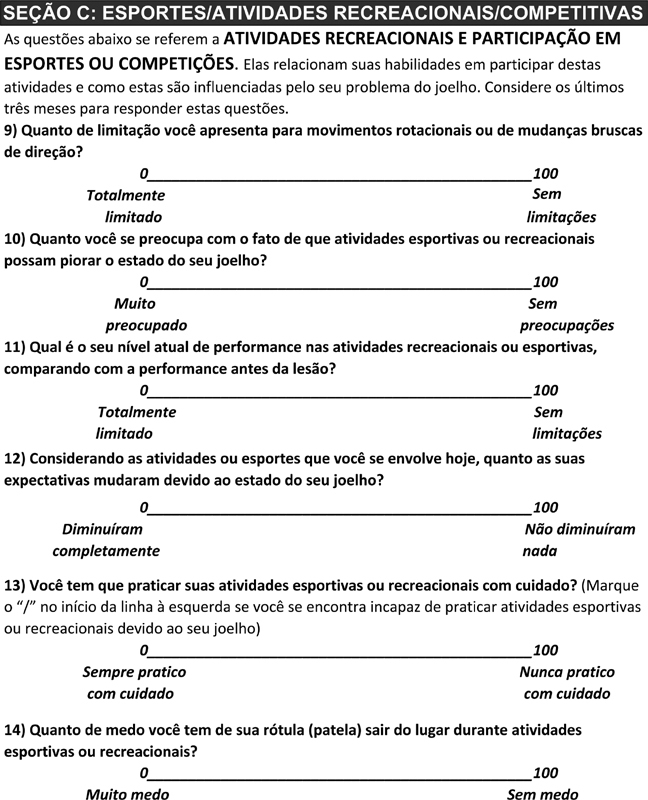
The pretest occurred from June 2018 to August 2019 at the aforementioned Knee Group's outpatient clinic. The study included a total of 62 patients with a mean age of 29.2 years (standard deviation: 11.6 years), ranging from 12 to 57 years old. Most patients (44 subjects; 70.69%) were female, whereas 18 (29%) were male. The Banff scores are summarized in Table 1 .
Table 1. Pretest Banff Score.
| Banff Score | Mean | Standard deviation | Minimum | Maximum | 95% confidence interval |
|---|---|---|---|---|---|
| General | 30.33 | 15.7 | 4.68 | 86.5 | 26.71–33.96 |
| Male gender | 33.09 | 19.04 | 24.65–41.54 | ||
| Female gender | 29.19 | 14.21 | 25.27–33.11 |
During the reconciliation of VT1 and VT2, the expert committee found a total of 22 discrepant items in 32 questions, 19 discrepant items in 32 answers, and 18 discrepant items in 21 information, title or instruction sentences from the original questionnaire. Emphasizing the need to maintain the equivalence, as proposed by Guillemin et al., 21 each item was individually analyzed by the committee in an attempt to reach a consensus at the synthesis stage and maintain the features from the original version.
The VT12 questionnaire was back translated, resulting in the two English texts shown in Figure 1 , called VRT1 and VRT2. During the harmonization, the semantic, idiomatic, experiential, and conceptual cross-cultural equivalences 22 of each item regarding its original version were analyzed; no reformulation by the committee was required when the concordance index among its 5 members was higher than 80%. 24
Only one analysis was required by the expert committee. The back-translated versions resulted in 26 discrepant items in 32 questions, 29 discrepant items in 32 answers, and 20 discrepant items in 21 information, title, or instruction sentences. All discrepancies were resolved, resulting in the VBPF. The committee pointed out the need for some adaptations in the VBPF to maintain both the equivalence to the original version and the instrument comprehension by the Brazilian population with no change in the analyzed measures. A summary of this process is exemplified in Table 2 .
Table 2. Cross-cultural adaptation of selected Banff Patella Instability Instrument (BPII) items.
| Question | Original Text (BPII) | Translation (VT12) | Changes for VBPF | Comment |
|---|---|---|---|---|
| 1a | “…severity of the 'giving way' episodes?” | “…episódios em que a rótula (patela) sai do lugar? (Gravidade)” | “…episódios em que a rótula sai do lugar? Qual a gravidade dos episódios de deslocamento?" | Expression with no idiomatic equivalent in Portuguese. To keep it understandable to the Brazilian population and preserve its conceptual equivalence, the term “dislocation” was avoided, using “kneecap out of place” (“rótula sai do lugar”) and “displacement” (“deslocamento”) |
| 3 | “…stiffness” | “joelho duro” | “joelho duro” | Although the committee believed that the most appropriate semantic equivalence would be “rigidez” (Portuguese for “stiffness”), the expression “joelho duro” (“hard knee”) had the same conceptual equivalence but greater understanding. So, it was kept in the VBPF |
| 9 | “…sudden twisting and pivoting movements or changes in direction” | “…movimentos de giro/rotação repentinos ou movimentos de mudanças de direção repentinos" | “…movimentos rotacionais ou de mudanças bruscas de direção” | Attempt to simplify the terms from translation VT12, maintaining its conceptual equivalence |
| 14 | “…knee 'giving way'" | “…joelho 'sair do lugar'" | “…rótula (patela) sair do lugar” | Expression with no idiomatic equivalence in Portuguese. “Joelho” (“knee”) from translation VT12 was replaced by “rótula (patela)” (“patella”) because, according to the committee, the translated term suggested the idea of the entire knee dislocating, instead of the patella alone |
| 28 | “…to psychologically 'come to grips'?” | “…superar psicologicamente” | “…superar psicologicamente” | Expression with no idiomatic equivalence in Portuguese, translated into an expression of similar conceptual equivalence, which was kept in the VBPF |
Abbreviations, BPII, Banff Patella Instability Instrument; VT12, translated version 12; VBPF, Brazilian prefinal version.
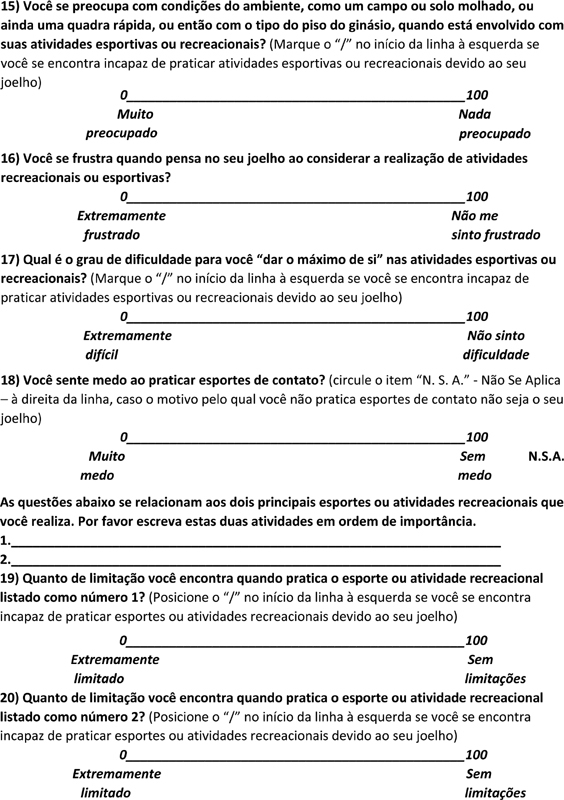
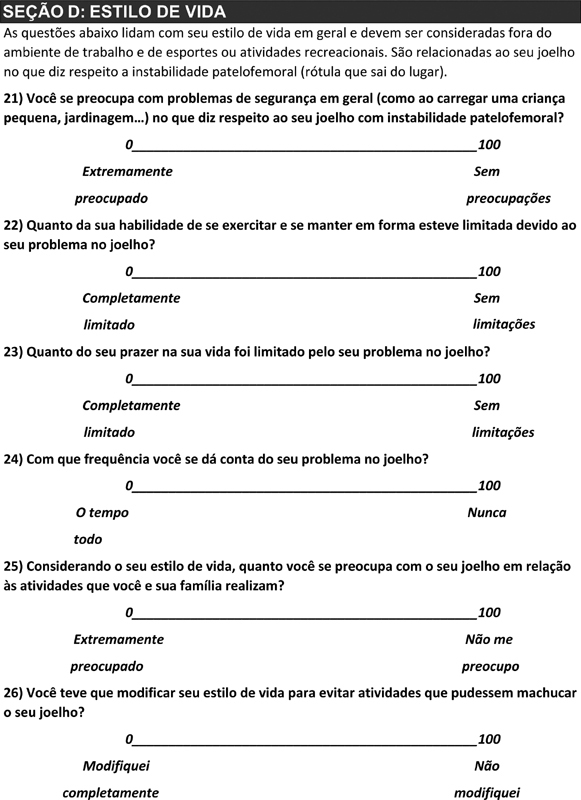
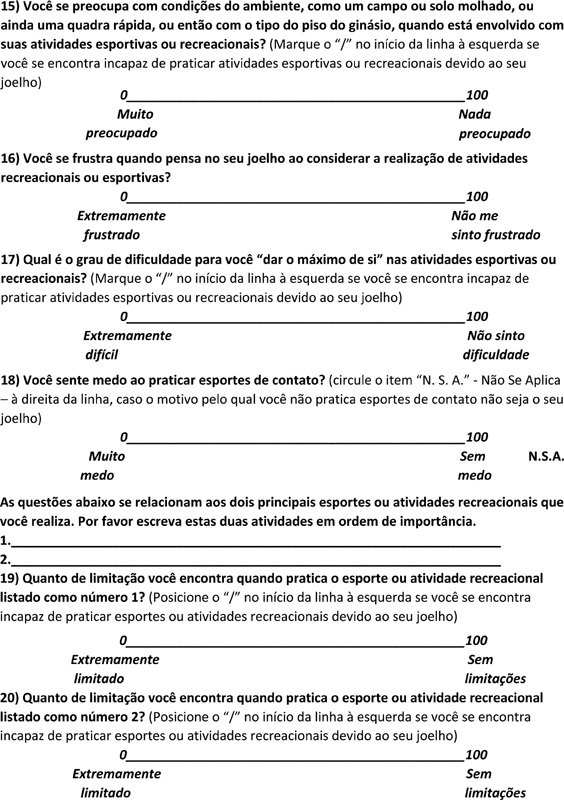
There was no record of questions, answers or other items which were not understood by the evaluated patients regarding the linguistic validation during the pretest. Therefore, the VBPF was submitted, with no need for reformulation, to the author of the original questionnaire together with a report of the adaptations made throughout the process. The author of the original questionnaire approved this version with no suggested modifications; as such, the VBF became the Banff Questionnaire for Patellar Instability – Brazilian Version, available in Annex 1 .
Discussion
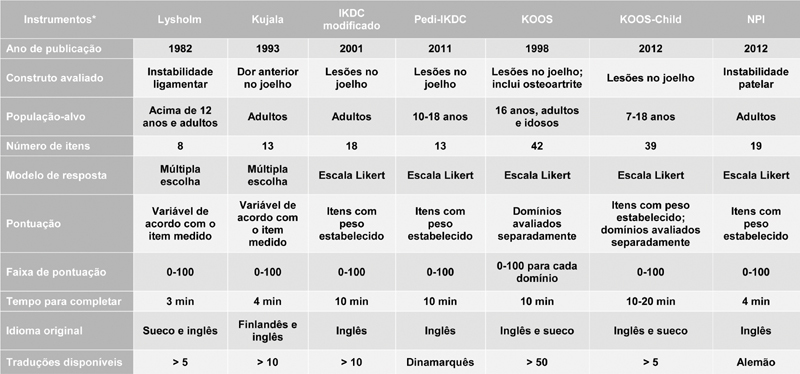
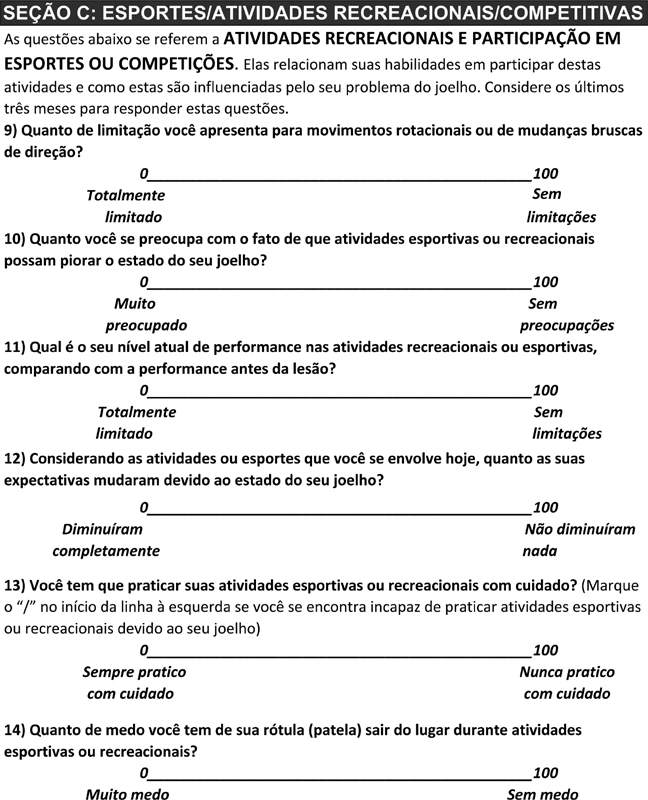
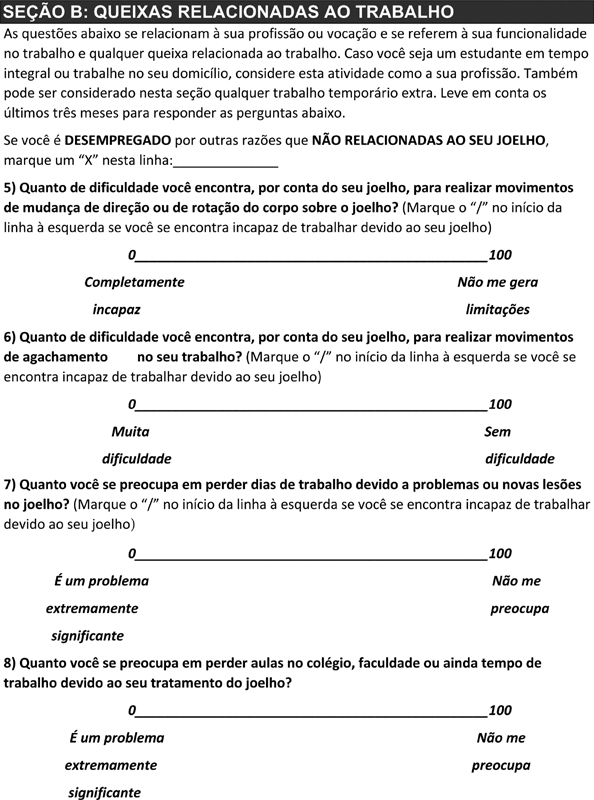
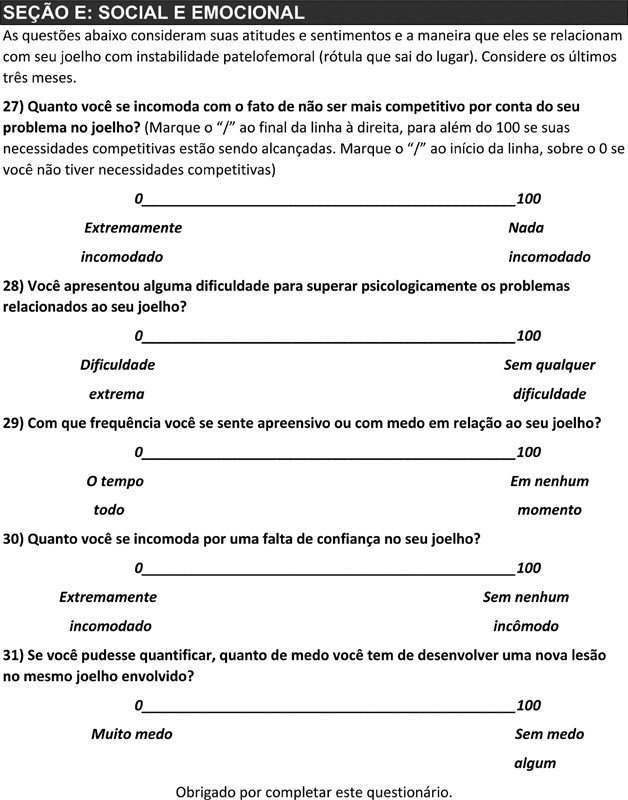
There is an increased concern in the literature not only to improve patient satisfaction but to develop outcome measures for a specific population or clinical condition. 25 Since patellar instability is a multifactorial condition, 1 2 3 4 5 6 7 8 9 10 26 27 28 it requires appropriate tools to compare different treatment strategies. Figure 2 summarizes the instruments for the assessment of patellar instability as reported by Hiemstra et al. 25
Fig. 2.
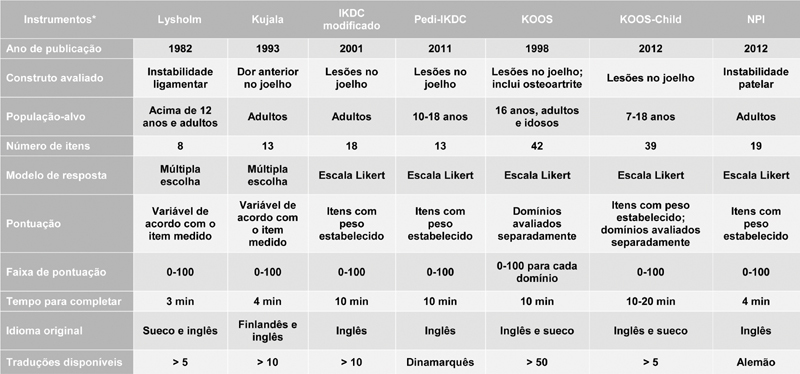
Instruments evaluating patellofemoral disorders, except for the Banff questionnaire. Abbreviations: IKDC, International Knee Documentation Committee; KOOS, Knee Injury and Osteoarthritis Outcome Score; NPI, Norwich Patellar Instability.
These data reveal that some questionnaires used for many years to assess patellofemoral joint disorders focus on characterizing other knee conditions, often emphasizing items not necessarily observed in this type of injury. In total, 60 of the 100 points of the Lysholm score, for instance, which was translated and validated for the Portuguese language, 29 measure pain and instability, making it unsuitable for an estimate of anterior pain. 14 Although widely used in patients with a previous history of patellar dislocation, the Kujala questionnaire, “Scoring of Patellofemoral Disorders”, also translated and culturally adapted into Portuguese, 30 has only 1 in 13 questions directed specifically at patellar instability.
The Banff Patella Instability Instrument (BPII) was first published in Canada, in 2013, by Hiemstra et al., 18 in an attempt to fill the void 31 of the lack of a specific questionnaire to assess patellar instability in the templates of “Patient-Reported Outcome Measures”. The 32 questions belonging to 5 different domains were listed by a modified Ebel method, performed by an international group of experts, to identify which specific outcome measures were most relevant for patellar instability. 7
Since the weight attributed to each answer is similar among different items, the final score consists of the average value of all answers from all five domains, and a higher final score reflects a better quality of life. 25 As such, the Banff questionnaire can assess the quality of life of patients with patellar instability in a more comprehensive way. 7
Even though the Norwich Patella Instability Score 32 was introduced because of a similar demand and context to the BPII to analyze outcome measures in patients with patellar instability, it focuses on characterizing physical symptoms generated by the clinical presentation. The weight attributed to its 19 items obeys a complex algorithm: the maximum score for items referring to activities that most commonly generate instability symptoms is lower, whereas activities that do not generate these same symptoms for most patients, except those with more severe instabilities, receive more points. Thus, a high final score indicates greater degrees of instability, and, therefore, worse function.
Only a fraction of the patellar instability questionnaires available in the literature was validated at any of the nine possible spheres as recommended by the Consensus-based Standards for the Selection of Health Status Measurement Instruments (COSMIN). 33 34 The BPII was analyzed per several psychometric properties, including content validity, internal consistency and reliability, 18 and construct and criterion validity. 7
In 2016, the BPII underwent a factor analysis and item reduction, 34 resulting in the BPII 2.0, with 23 items divided into the same 5 domains as its first version. This reduction was partly due to the fact that many patients did not answer all the questions; in addition, it constitutes an attempt to adapt these questions to the pediatric population. The author of the original questionnaire reported, via e-mail, that the BPII 2.0 is associated with a smaller number of unanswered questions.
Several psychometric properties of the BPII 2.0 were tested and added to its validation process, including a multicenter study of the validation of the BPII 2.0 to the Pedi-IKDC, 35 with moderate correlation, and a cross-cultural validation for the German language targeting the German, Austrian and Swiss populations. 36 In addition, the BPII 2.0 is being validated into Dutch, Spanish, Finnish and French. 25
Even after establishing a consensus, the committee had doubts in some questions from the final Portuguese translation regarding the acceptability of certain grammatical constructions (such as, “quanto medo”, regarding the intensity of fear) by the target population. Nevertheless, all questions were understood by all participants during the pretest, with no suggestions of changes. Another limitation of the present study was to carry out only the translation and cross-cultural adaptation of the Banff Questionnaire for Patellar Instability. Since the validation is a complex, iterative process, further studies are required to increase the representative sample of the Brazilian population, and our group is working on that.
Conclusion
The BPII has been successfully translated and cross-culturally adapted into Brazilian Portuguese, enabling its application to assess the quality of life of patients with patellar instability in Brazil.
Funding Statement
Suporte Financeiro Não houve suporte financeiro de fontes públicas, comerciais, ou sem fins lucrativos.
Conflito de Interesses Os autores declaram não haver conflito de interesses.
O dr. Galvao informa que fez um pedido de patente para o Questionário Banff para Instabilidade Patelar Versão Brasileira.
Trabalho realizado pelo Departamento de Ortopedia e Traumatologia, Escola Paulista de Medicina, Universidade Federal de São Paulo, São Paulo, SP, Brasil.
Study developed at the Orthopedics and Traumatology Department, Escola Paulista de Medicina, Universidade Federal de São Paulo, São Paulo, SP, Brazil.
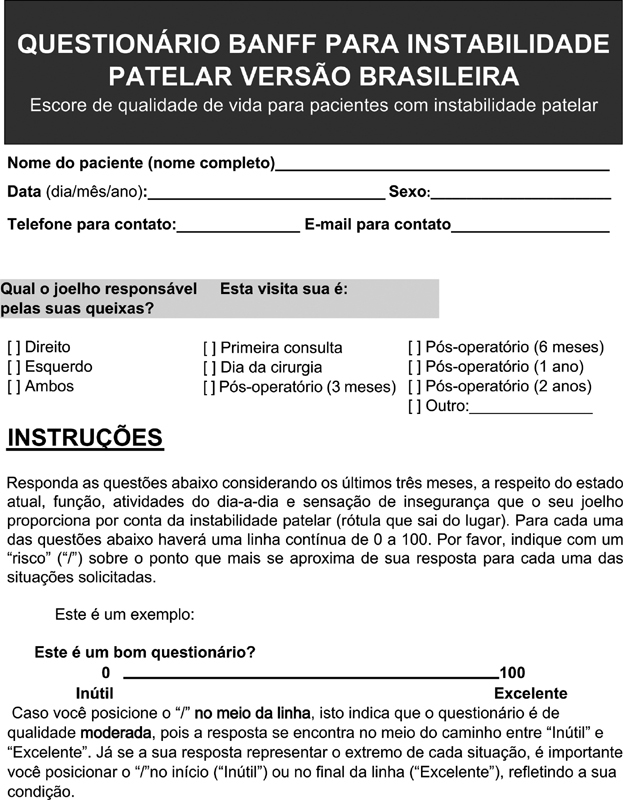
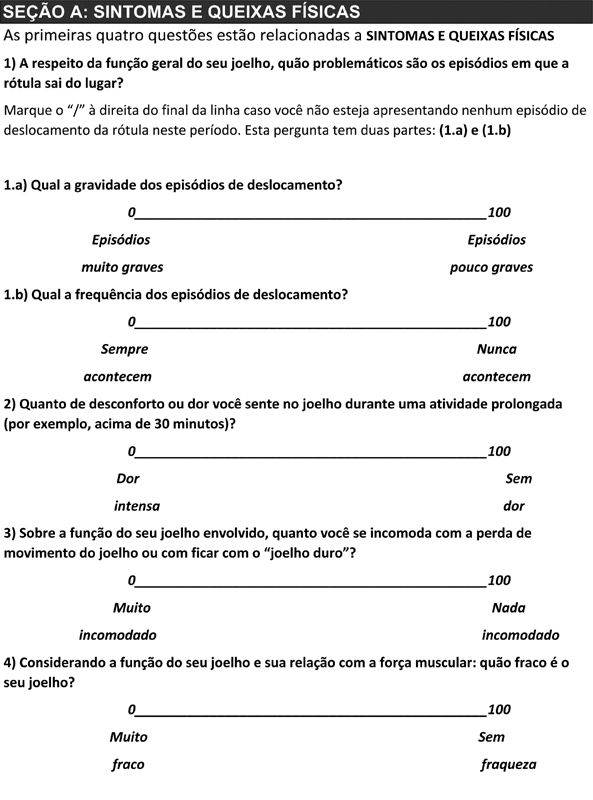
Apêndice 1.
Questionário Banff para Instabilidade Patelar Versão Brasileira.
Referências
- 1.Colvin A C, West R V. Patellar instability. J Bone Joint Surg Am. 2008;90(12):2751–2762. doi: 10.2106/JBJS.H.00211. [DOI] [PubMed] [Google Scholar]
- 2.Sanders T L, Pareek A, Hewett T E, Stuart M J, Dahm D L, Krych A J. Incidence of First-Time Lateral Patellar Dislocation: A 21-Year Population-Based Study. Sports Health. 2018;10(02):146–151. doi: 10.1177/1941738117725055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Waterman B R, Belmont P J, Jr, Owens B D. Patellar dislocation in the United States: role of sex, age, race, and athletic participation. J Knee Surg. 2012;25(01):51–57. doi: 10.1055/s-0031-1286199. [DOI] [PubMed] [Google Scholar]
- 4.Fithian D C, Paxton E W, Stone M L. Epidemiology and natural history of acute patellar dislocation. Am J Sports Med. 2004;32(05):1114–1121. doi: 10.1177/0363546503260788. [DOI] [PubMed] [Google Scholar]
- 5.Nwachukwu B U, So C, Schairer W W. Economic Decision Model for First-Time Traumatic Patellar Dislocations in Adolescents. Am J Sports Med. 2017;45(10):2267–2275. doi: 10.1177/0363546517703347. [DOI] [PubMed] [Google Scholar]
- 6.Aglietti P. Philadelphia: Churchill Livingstone; 2001. Disorders of the patellofemoral joint; pp. 913–1045. [Google Scholar]
- 7.Hiemstra L A, Kerslake S, Lafave M, Mohtadi N G. Concurrent Validation of the Banff Patella Instability Instrument to the Norwich Patellar Instability Score and the Kujala Score in Patients With Patellofemoral Instability. Orthop J Sports Med. 2016;4(05):2.325967116646085E15. doi: 10.1177/2325967116646085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hiemstra L A, Kerslake S, Lafave M. Medial Patellofemoral Ligament Reconstruction Femoral Tunnel Accuracy: Relationship to Disease-Specific Quality of Life. Orthop J Sports Med. 2017;5(02):2.325967116687749E15. doi: 10.1177/2325967116687749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Petri M, Ettinger M, Stuebig T. Current Concepts for Patellar Dislocation. Arch Trauma Res. 2015;4(03):e29301. doi: 10.5812/atr.29301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kader D, Matar H, Caplan N. Patellofemoral joint instability: a review of current concepts. J Orthop Trauma. 2016;6(01):1–8. [Google Scholar]
- 11.Berlim M T, Fleck M P.Qualidade de vida: um novo conceito para a pesquisa e prática em psiquiatria Rev Bras Psiquiatr 20032504249–252.15328553 [Google Scholar]
- 12.Duarte P S, Miyazaki M C, Ciconelli R M, Sesso R. Tradução e adaptação cultural do instrumento de avaliação de qualidade de vida para pacientes renais crônicos (KDQOL-SF) Rev Assoc Med Bras (1992) 2003;49(04):375–381. doi: 10.1590/s0104-42302003000400027. [DOI] [PubMed] [Google Scholar]
- 13.Lopes A D, Stadniky S P, Masiero D, Carrera E F, Ciconelli R M, Griffin S. Tradução e adaptação cultural do WORC: um questionário de qualidade de vida para alterações do manguito rotador. Rev Bras Fisioter São Carlos. 2006;10(03):309–315. [Google Scholar]
- 14.Kujala U M, Jaakkola L H, Koskinen S K, Taimela S, Hurme M, Nelimarkka O. Scoring of patellofemoral disorders. Arthroscopy. 1993;9(02):159–163. doi: 10.1016/s0749-8063(05)80366-4. [DOI] [PubMed] [Google Scholar]
- 15.Hefti F, Müller W, Jakob R P, Stäubli H U.Evaluation of knee ligament injuries with the IKDC form Knee Surg Sports Traumatol Arthrosc 19931(3-4):226–234. [DOI] [PubMed] [Google Scholar]
- 16.Acquadro C, Conway K, Girourdet C, Mear I.Linguistic Validation Manual for Patient Reported Outcomes(PRO) Instruments Lyon (France)MAPI Research Trust; 2004. Available from: URL:http://www.mapi-research.fr/i_02_manu.htm
- 17.Acquadro C, Janbom B, Ellis D, Marquis P. 2nd ed. Philadelphia: Lippincott-Raven; 1996. Language and translation issues; pp. 575–585. [Google Scholar]
- 18.Hiemstra L A, Kerslake S, Lafave M R, Heard S M, Buchko G M, Mohtadi N G. Initial validity and reliability of the Banff Patella Instability Instrument. Am J Sports Med. 2013;41(07):1629–1635. doi: 10.1177/0363546513487981. [DOI] [PubMed] [Google Scholar]
- 19.Hair J F, Black B, Babin B, Anderson R E, Tatham R L. 6th ed. Bill Black, Louisiana State University; 2006. Multivariate Data Analysis. [Google Scholar]
- 20.Brattstroem H.Shape of the intercondylar groove normally and in recurrent dislocation of patella. a clinical and x-ray-anatomical investigation Acta Orthop Scand Suppl 1964686868, 1–148 [PubMed] [Google Scholar]
- 21.Guillemin F, Bombardier C, Beaton D. Cross-cultural adaptation of health-related quality of life measures: literature review and proposed guidelines. J Clin Epidemiol. 1993;46(12):1417–1432. doi: 10.1016/0895-4356(93)90142-n. [DOI] [PubMed] [Google Scholar]
- 22.Beaton D E, Bombardier C, Guillemin F, Ferraz M B. Guidelines for the process of cross-cultural adaptation of self-report measures. Spine. 2000;25(24):3186–3191. doi: 10.1097/00007632-200012150-00014. [DOI] [PubMed] [Google Scholar]
- 23.Beaton D, Bombardier C, Guillemin F, Ferraz M. Recommendations for the cross-cultural adaptation of the DASH & QuickDASH outcome measures. Institute Work Health. 2007;1(01):1–45. [Google Scholar]
- 24.Pasquali L. Princípios de elaboração de escalas psicológicas. Rev Psiquiatr Clin (Santiago) 1998;25(05):206–213. [Google Scholar]
- 25.Hiemstra L A, Page J L, Kerslake S. Patient-reported outcome measures for patellofemoral instability: a critical review. Curr Rev Musculoskelet Med. 2019;12(02):124–137. doi: 10.1007/s12178-019-09537-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Franciozi C E, Ambra L F, Albertoni L JB. Anteromedial Tibial Tubercle Osteotomy Improves Results of Medial Patellofemoral Ligament Reconstruction for Recurrent Patellar Instability in Patients With Tibial Tuberosity-Trochlear Groove Distance of 17 to 20 mm. Arthroscopy. 2019;35(02):566–574. doi: 10.1016/j.arthro.2018.10.109. [DOI] [PubMed] [Google Scholar]
- 27.Franciozi C E, Ambra L F, Albertoni L J. Increased Femoral Anteversion Influence Over Surgically Treated Recurrent Patellar Instability Patients. Arthroscopy. 2017;33(03):633–640. doi: 10.1016/j.arthro.2016.09.015. [DOI] [PubMed] [Google Scholar]
- 28.Gobbi R G, Demange M K, de Ávila L FR. Patellar tracking after isolated medial patellofemoral ligament reconstruction: dynamic evaluation using computed tomography. Knee Surg Sports Traumatol Arthrosc. 2017;25(10):3197–3205. doi: 10.1007/s00167-016-4284-x. [DOI] [PubMed] [Google Scholar]
- 29.Peccin M S, Ciconelli R, Cohen M. Questionário específico para sintomas do joelho “Lysholm Knee Scoring Scale”: tradução e validação para a língua portuguesa. Acta Ortop Bras. 2006;14(05):268–272. [Google Scholar]
- 30.Aquino V S, Falcon S FM, Neves L MT, Rodrigues R C, Sendín F A. Tradução e adaptação cultural para a língua portuguesa do questionário scoring of patellofemoral disorders: estudo preliminar. Acta Ortop Bras. 2011;19(05):273–279. [Google Scholar]
- 31.Smith T O, Davies L, O'Driscoll M L, Donell S T. An evaluation of the clinical tests and outcome measures used to assess patellar instability. Knee. 2008;15(04):255–262. doi: 10.1016/j.knee.2008.02.001. [DOI] [PubMed] [Google Scholar]
- 32.Smith T O, Donell S T, Clark A. The development, validation and internal consistency of the Norwich Patellar Instability (NPI) score. Knee Surg Sports Traumatol Arthrosc. 2014;22(02):324–335. doi: 10.1007/s00167-012-2359-x. [DOI] [PubMed] [Google Scholar]
- 33.Mokkink L B, Terwee C B, Patrick D L. The COSMIN checklist for assessing the methodological quality of studies on measurement properties of health status measurement instruments: an international Delphi study. Qual Life Res. 2010;19(04):539–549. doi: 10.1007/s11136-010-9606-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lafave M R, Hiemstra L, Kerslake S. Factor Analysis and Item Reduction of the Banff Patella Instability Instrument (BPII): Introduction of BPII 2.0. Am J Sports Med. 2016;44(08):2081–2086. doi: 10.1177/0363546516644605. [DOI] [PubMed] [Google Scholar]
- 35.Lafave M R, Hiemstra L A, Parikh S N, Peterson D, Kerslake S. Validity and Reliability of the Banff Patellofemoral Instability Instrument 2.0 in an Adolescent Population. J Pediatr Orthop. 2020;40(02):e103–e108. doi: 10.1097/BPO.0000000000001407. [DOI] [PubMed] [Google Scholar]
- 36.Becher C, Attal R, Balcarek P. Successful adaption of the Banff Patella Instability Instrument (BPII) 2.0 into German. Knee Surg Sports Traumatol Arthrosc. 2018;26(09):2679–2684. doi: 10.1007/s00167-017-4673-9. [DOI] [PubMed] [Google Scholar]