Introduction
During the previous severe acute respiratory syndrome pandemic of 2002-2004, adverse skin reactions to N95 masks were reported after prolonged use. These adverse skin reactions included acne, facial itch, contact urticaria, and contact dermatitis.1, 2, 3 Similarly, prolonged face mask and respirator usage during the current COVID-19 pandemic has increased the frequency of facial dermatitis in health care workers.4,5 The offending component within the face mask textile fabric may not be obvious; however, textile fibers can serve as substrates for allergenic additives, such as dyes and antiwrinkling agents that release formaldehyde.6 Face mask allergic contact dermatitis (ACD) caused by formaldehyde releasers has been noted previously.7 Complete allergen avoidance may not be feasible for all health care workers who develop face mask ACD. Thus, a simple solution is required, such as the application of a small barrier between the skin and the face mask fabric.
Case report
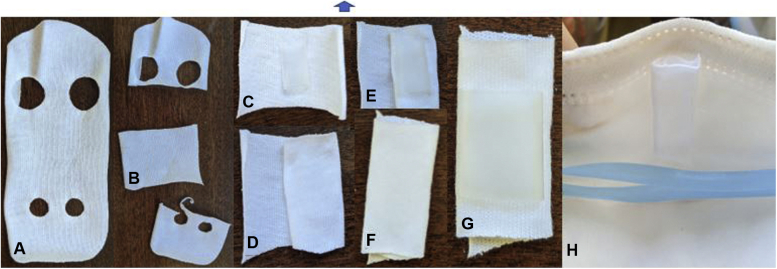
A 36-year-old physician with multiple proven contact allergens, including formaldehyde, noted redness and pain on the dorsal aspect of her nose 30 minutes after wearing a duckbill N95 respirator (Fig 1). Initially, she tolerated the duckbill N95, but after several weeks of prolonged wearing, she developed redness and pain on her nose. A self-patch with a portion of the mask yielded a positive reaction with pruritic papules on day 3 post removal (Fig 2). Our challenge was to attempt to block allergens from contacting her skin, doing so without decreasing the seal of her mask. An analogous situation exists for sleep apnea patients who may develop contact dermatitis from masks but require an adequate seal.8 The RemZzzs Nasal Pillow Cpap Mask Liner (RemZzzs) is a white, 100% cotton liner marketed for use under such masks. Our patient cut and folded a small piece of liner, taped it to the inside of her mask (Fig 3, A to H), and noted complete resolution of her pain and dramatic improvement of the erythema despite hours of N95 use. Fit testing through Workforce Health and Safety remained satisfactory. We recommend a trial of RemZzzs or potentially similar thin, soft, white, 100% cotton fabrics as barriers (eg, cut-up, old, white undershirts) for those experiencing skin inflammations under N95 respirators. Fit testing should be performed to ensure continued adequate mask seal.9
Fig 1.

Allergic contact dermatitis. Facial erythema and irritation of the nasal bridge after wearing N95 mask.
Fig 2.

Self-patch test. Cluster of pruritic papules developed on day 3 after removal of self-patch–tested mask material.
Fig 3.
Steps to create the barrier strip. A, Intact barrier strip. The solid middle piece of the cloth should be cut out (B), and tape is used to fold it like a burrito with the ends untucked (C to F). Tape is placed in the center (G). The barrier is taped into place inside the mask overlying the area of skin inflammation (H).
The patient's informed consent was obtained.
Discussion
Cases of mask-related ACD have increased during the COVID-19 pandemic. These reactions are not limited to times of pandemic; health care workers, such as surgeons, often require prolonged periods of mask usage as a part of their routine job activity. Individuals with known contact allergens such as formaldehyde and formaldehyde-releasing preservatives, for example, should practice avoidance of face masks and respirators containing these allergens. This information unfortunately is not always readily available.7 Furthermore, suitable mask alternatives devoid of contact allergens are not always available. We queried Halyard, the manufacturer of our patient's N95 mask, about the presence of formaldehyde. They responded that formaldehyde was not listed on the composition disclosures of any of the raw materials used to make the mask. Polypropylene was listed as one of the components. Possible occult sources of formaldehyde in masks have been reported from polypropylene degradation during mask production, undisclosed formaldehyde in raw materials, or as a contaminant from mask packaging.5 While irritant contact dermatitis and ACD could present with an identical clinical picture, the delayed appearance of papules (day 3 after removal of self-patch–tested mask) supports the diagnosis of ACD. Allergic reactions on patch testing tend to crescendo in intensity.10 The barrier method we described could be used to block both irritant contact dermatitis and ACD by decreasing skin contact with the mask material. Other barriers, such as silicone-based dressings or gauze, might also be effective, if common sensitizers are not present. We chose a fabric of 100% cotton (nonwrinkle-resistant, soft, and white), as it was least likely to be finished with formaldehyde and unlikely to contain textile dye or other allergens. Thus, a thin barrier insert may allow continued usage of a previously problematic face mask and/or respirator.
Conflicts of interest
None disclosed.
Footnotes
Funding sources: None.
IRB approval status: Not applicable.
Supplementary data
References
- 1.Tan K.T., Greaves M.W. N95 acne. Int J Dermatol. 2004;43(7):522–523. doi: 10.1111/j.1365-4632.2004.02338.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Foo C.C., Goon A.T., Leow Y.H., Goh C.L. Adverse skin reactions to personal protective equipment against severe acute respiratory syndrome–a descriptive study in Singapore. Contact Dermatitis. 2006;55(5):291–294. doi: 10.1111/j.1600-0536.2006.00953.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Donovan J., Kudla I., Holness L.D., Skotnicki-Grant S., Nethercott J.R. Skin reactions following use of N95 facial masks. Dermatitis. 2007;18(2):104. doi: 10.1097/01206501-200706000-00013. [DOI] [Google Scholar]
- 4.Darlenski R., Tsankov N. COVID-19 pandemic and the skin: what should dermatologists know? Clin Dermatol. 2020;38(6):785–787. doi: 10.1016/j.clindermatol.2020.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yu J., Chen J.K., Mowad C.M., et al. Occupational dermatitis to facial personal protective equipment in health care workers: a systematic review. J Am Acad Dermatol. 2021;84(2):486–494. doi: 10.1016/j.jaad.2020.09.074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Svedman C., Engfeldt M., Malinauskiene L. Textile contact dermatitis: how fabrics can induce dermatitis. Curr Treat Options Allergy. 2019;6(1):103–111. doi: 10.1007/s40521-019-0197-5. [DOI] [Google Scholar]
- 7.Donovan J., Skotnicki-Grant S. Allergic contact dermatitis from formaldehyde textile resins in surgical uniforms and nonwoven textile masks. Dermatitis. 2007;18(1):40–44. doi: 10.2310/6620.2007.05003. [DOI] [PubMed] [Google Scholar]
- 8.Egesi A., Davis M.D.P. Irritant contact dermatitis due to the use of a continuous positive airway pressure nasal mask: 2 case reports and review of the literature. Cutis. 2012;90(3):125–128. [PubMed] [Google Scholar]
- 9.Colton C.E. In: Fundamentals of Industrial Hygiene. 5th ed. Plog B.A., Quinlan P.J., editors. National Safety Council; 2001. Respiratory protection; pp. 667–725. [Google Scholar]
- 10.Brasch J., Geier J., Gefeller O. Dynamic patterns of allergic patch test reactions to 10 European standard allergens. An analysis of data recorded by the Information Network of Departments of Dermatology (IVDK) Contact Dermatitis. 1996;35(1):17–22. doi: 10.1111/j.1600-0536.1996.tb02260.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.