Abstract
Opportunistic infections are widely described in patients with novel coronavirus disease 2019 (COVID-19); however, very few studies have addressed those affecting the oral cavity. Given the lack of information on the clinical presentations and the available treatment options, the present study aimed to show a case in which a combination of antimicrobial photodynamic therapy (aPDT) and photobiomodulation therapy (PBMT) was used for the management of two concomitant COVID-19-associated opportunistic oral infections (oral pseudomembranous candidiasis and recurrent herpes labialis). Within 7 days and without any systemic drug administration, all the lesions resolved completely, and the patient no longer reported oral pain or discomfort. According to the current case report and taking into consideration the significant gaps in the knowledge and understanding of COVID-19, this combination of phototherapy modalities seems to be a promising tool for managing viral and fungal opportunistic oral infections.
Keywords: COVID-19, SARS-CoV-2, Antimicrobial photodynamic therapy, Photobiomodulation therapy, Herpes Labialis, Candidiasis
1. Introduction
The high incidence rates of severe infection and mortality of the Novel Coronavirus disease 2019 (COVID-19) are probably related to inefficient immunity to the virus, viral replication in the respiratory tract, and coinfections [1]. There is not enough information on COVID-19-associated opportunistic infections to date; however, the most common in critical patients are those affecting the respiratory tract, bloodstream, and urinary tract [2]. Moreover, fungal infections are the most frequently reported, followed by viral, bacterial, protozoa, and helminth ones [3].
Orofacial lesions have already been described in COVID-19 patients [4]. Some hypothesize that these lesions would arise from indirect mechanisms of viral infection, i.e., from either the compromised general medical status or therapeutic drugs administered [5]. Within the group of COVID-19-associated opportunistic oral infections, despite limited studies, the most reported so far include candidiasis and herpes simplex infection [6].
In light of these facts, this article reports a clinical case in which a combination of antimicrobial photodynamic therapy (aPDT) and photobiomodulation therapy (PBMT) was used for the management of COVID-19-associated opportunistic oral infections.
2. Case report
A Brazilian 88-year‐old female, with no history of chronic diseases, sought medical help owing to a flu-like syndrome suggestive of COVID-19. The RT-PCR test confirmed the clinical suspicion and azithromycin and prednisone were prescribed.
About 10 days later, she developed pneumonia, dyspnea, and a painful, burning sensation throughout her mouth. Levofloxacin, dexamethasone, acetylsalicylic acid, and acetylcysteine were prescribed, as well as ipratropium bromide inhalation. After a mild improvement in the clinical medical status, the patient attended a private dental office complaining of oral pain arising from the upper denture.
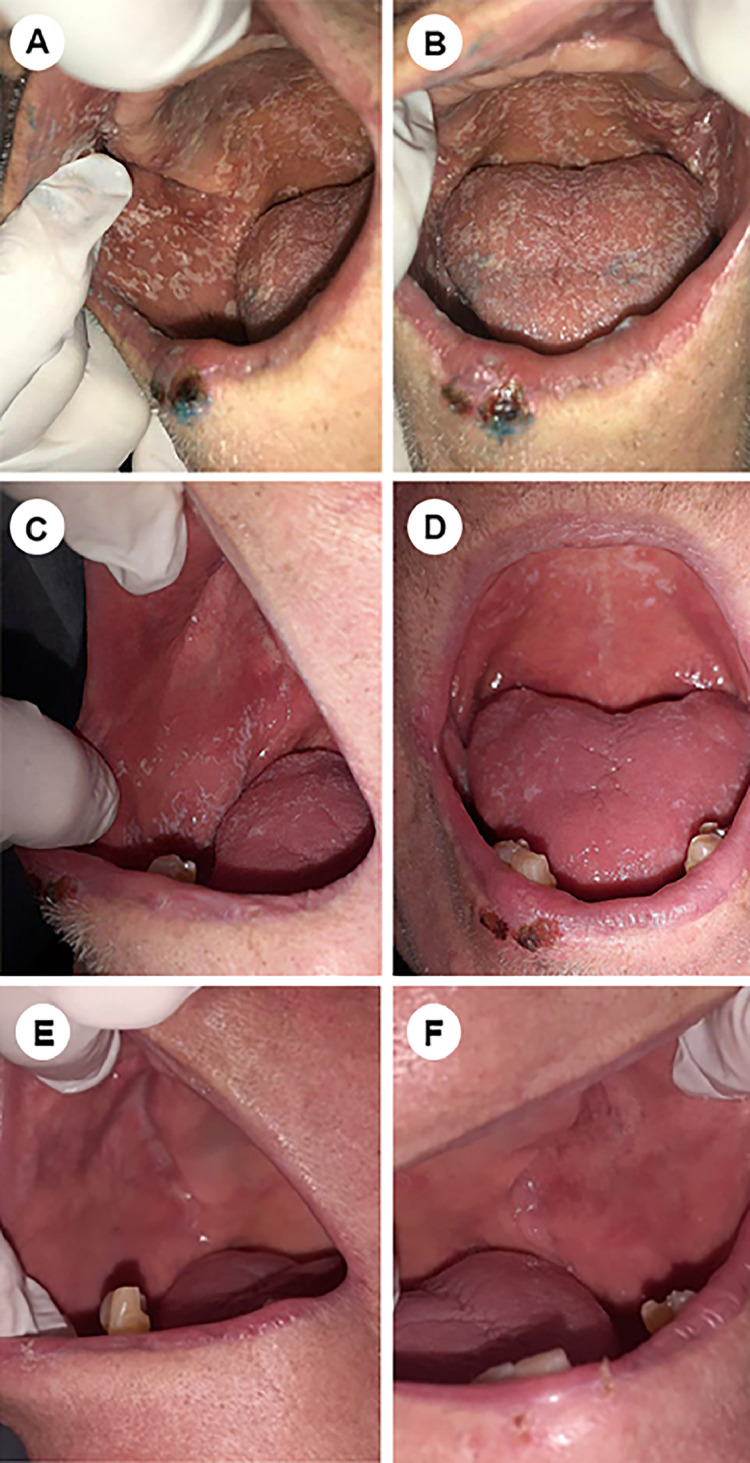
It was noted two bleeding ulcers on the lower lip and extensive, creamy white, plaque-like lesions throughout the oral cavity, which could be removed by gentle scraping, leaving the underlying mucosal surface erythematous. According to the clinical signs, symptoms, and the past medical history, diagnoses of oral pseudomembranous candidiasis and recurrent herpes labialis were given.
At the first appointment, an aPDT session was suggested (Fig. 1 A,B), as well as the use of nystatin mouthwash for 7 days. Despite the difficulty in mouth opening and debilitating general condition, for aPDT, 0.01% methylene blue spray solution was applied onto the most painful oral regions for 5 min, and 660-nm laser irradiation was performed on contact mode (Therapy XT, DMC, São Carlos, SP, Brazil), through 43 irradiation points (40 over the oral cavity and 3 over the labial ulcers) and with 100 mW, 1 J, and 10 s per point. After 24 h, the patient reported pain relief and the same protocol was then repeated.
Fig. 1.
Clinical appearance: oral pseudomembranous candidiasis and recurrent herpes labialis lesions. A, B. At diagnosis; C,D. 72 h after the first laser session; E,F. 7 days after the first laser session, showing the lesions completely resolved.
On the third day and considering the pain alleviation achieved, another aPDT session was performed, but with higher energy irradiation: 5 J and 50 s per point on the oral mucosa. In addition, given the clinical improvement seen in the labial lesions, already with a crust aspect and without bleeding, a PBMT session was performed as follows: 660-nm, 100 mW, 1 J, and 10 s per point. At this moment, the patient no longer experienced oral pain and very few intraoral lesions could be noted (Fig. 1C,D).
On the seventh day, all the lesions resolved completely (Fig. 1E,F). The patient reported total pain remission and no difficulty in eating, drinking, and speaking.
3. Discussion
The combination of phototherapies resulted in an important clinical improvement of the patient's oral condition within a few days. To the best of the authors’ knowledge, this is the first report case on the benefits of this phototherapeutic approach to two concomitant COVID-19-associated opportunistic oral infections (i.e., fungal and viral infections).
Immunosuppressive therapy is considered an important risk factor for opportunistic infections in COVID-19 patients. Corticosteroids are immunosuppressive drugs commonly prescribed for these patients [3], as seen in the current case report. Besides that, the patient also received long-term antibiotics, which probably altered her oral microbiota.
Given the effectiveness of aPDT in inhibiting bacterial, fungal, and viral infections, as well as the potential of PBMT for pain relief and inflammation control [5], the authors hypothesized that combining both phototherapies would be interesting. Moreover, taking into account that drug-drug interaction may be a challenge in opportunistic infections in COVID-19 patients [3], no systemic medication was needed for the resolution of the local coinfections. Other advantages comprised ease of application, low cost, and safety [4].
Despite the positive clinical result achieved within a short period, the current study has clear limitations as every case report. Given that the first outbreak of COVID-19 has occurred very recently and well-controlled clinical investigations are still virtually impossible [5], case reports might provide clinicians early information and novel insights into the treatment and pathophysiology of emerging diseases and conditions such as COVID-19 [4]. Therefore, further studies are actually required to better elucidate the role of these phototherapies in COVID-19-associated opportunistic oral infections.
References
- 1.Ezeokoli O.T., Pohl C.H. Opportunistic pathogenic fungal co-infections are prevalent in critically ill COVID-19 patients: are they risk factors for disease severity? South African Med. J. 2020;110:1081. doi: 10.7196/SAMJ.2020.v110i11.15248. [DOI] [PubMed] [Google Scholar]
- 2.Zhang H., Zhang Y., Wu J., Li Y., Zhou X., Li X., Chen H., Guo M., Chen S., Sun F., Mao R., Qiu C., Zhu Z., Ai J., Zhang W. Risks and features of secondary infections in severe and critical ill COVID-19 patients. Emerg. Microbes Infect. 2020;9:1958–1964. doi: 10.1080/22221751.2020.1812437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Abdoli A., Falahi S., Kenarkoohi A. COVID-19-associated opportunistic infections: a snapshot on the current reports. Clin. Exp. Med. 2021 doi: 10.1007/s10238-021-00751-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Teixeira I.S., Leal F.S., Tateno R.Y., Palma L.F., Campos L. Photobiomodulation therapy and antimicrobial photodynamic therapy for orofacial lesions in patients with COVID-19: a case series. Photodiagnosis Photodyn. Ther. 2021;34 doi: 10.1016/j.pdpdt.2021.102281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ramires M.C.C.H., Mattia M.B., Tateno R.Y., Palma L.F., Campos L. A combination of phototherapy modalities for extensive lip lesions in a patient with SARS-CoV-2 infection. Photodiagnosis Photodyn. Ther. 2021;33 doi: 10.1016/j.pdpdt.2021.102196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Aragoneses J., Suárez A., Algar J., Rodríguez C., López-Valverde N., Aragoneses J.M. Oral manifestations of COVID-19: updated systematic review with meta-analysis. Front. Med. 2021;8 doi: 10.3389/fmed.2021.726753. [DOI] [PMC free article] [PubMed] [Google Scholar]