In a recent article published in this Journal (Lührs et al., 2021), Dr. Oscar Lührs and the gynecologic oncology team led by Prof. Jan Persson in Lund, Sweden, rightly drew the attention on the need of better identifying discontinuous disease located between the uterus, corpus and cervix, and the regional lymph nodes generally referred to as pelvic nodes.
On this matter, it is important to remind the pivotal work of Erich Burghardt and his followers in Graz, Austria (Burghardt et al., 1988, Girardi et al., 1989, Girardi et al., 1993, Winter et al., 2002) who used the technique of giant pathological sections of the paracervix in radical hysterectomy specimens. They were able, well before the sentinel node era, to detect to the involvement of paracervical lymph nodes, which they described as “discontinuous parametrial involvement”. In 2000, Benedetti-Panici et al., using the same technique, came up with consistent findings (Benedetti-Panici et al., 2000). Evidence was given in these studies that the lateral part of the paracervix, an area left in place at the time of “modified” radical hysterectomy and “parietal” pelvic lymphadenectomy – with an arbitrary caudal limit as defined by the obturator nerve -, can contain metastatic nodes which are potential sites of recurrence even in patients with negative parietal pelvic nodes.
These findings, combined with the magnification provided by the laparoscopic vision, inspired in the late ‘90s a new concept, called “paracervical lymphadenectomy” (Querleu et al., 1998, Querleu et al., 2002). The rationale of this technique was to consider the lateral part of the paracervix as a lymph-node bearing area which can be cleared while preserving the nerves (autonomic) and vessels (Meigs’ “web”) which cross or are components of this structure. The objective was to complement the “modified” paracervical resection, limited to the medial part of the paracervix, by an oncologically relevant procedure aiming at removing microscopic cancer disease while sparing the patient the long-term adverse functional effects of the “classical” radical hysterectomy, as defined at that time by clamping the entirety of the paracervix at the internal iliac vessels.
The concept was later incorporated in the definition of some sub-types of the Querleu-Morrow classification of radical hysterectomy (Querleu and Morrow, 2008). The possibility of adding a paracervical lymphadenectomy to a type B operation was opened, thus defining two subtypes: B1, original type B, and B2, with paracervical lymphadenectomy.
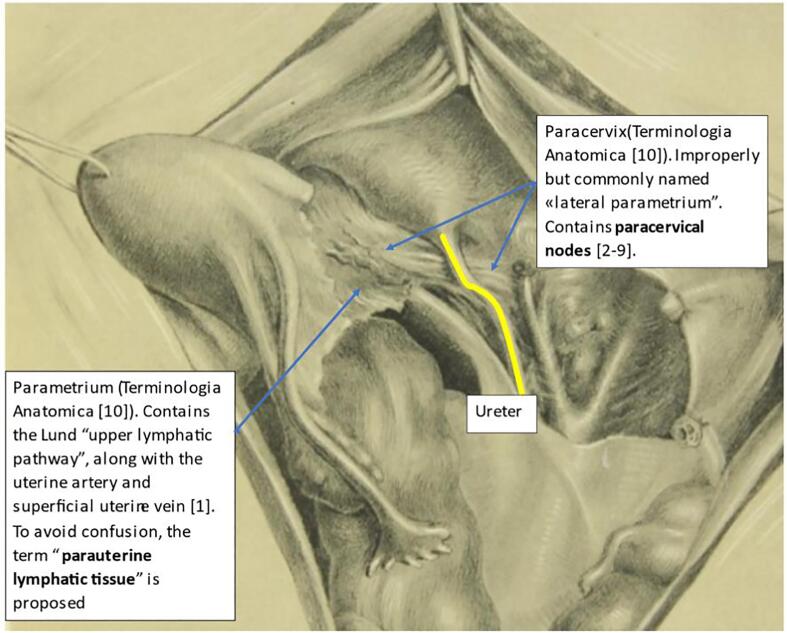
The Lund’s work adds a novel complement to this concept. Intracervical injection of indocyanine green leads to the intraoperative identification of lymph nodes so far neglected. The authors suggest to selectively remove and ultrastage what they have called the “upper lymphatic pathway” of the uterus, that is located in the broad ligament, cephalic to the ureter. The anatomical description of the area to which the Lund group refers is summarized in Fig. 1. As a matter of fact, the upper pathway is routinely removed when the uterine artery is ligated at its origin, along with the inconstant superficial uterine vein, and when the whole content of the supra-ureteral part of the broad ligament is removed. We would consequently suggest to replace the term “resection of the upper paracervical lymphovascular tissue” by a more descriptive “resection of the parauterine lymphatic tissue”.
Fig. 1.
Indeed, some confusion may arise from the use in their title of the adjective paracervical. As a matter of fact, the anatomical area lateral to the uterine corpus they are referring to is not the paracervix. In addition, in their text and Table 2, the nodes removed during the procedure are named parametrial, while the structure is named paracervical.
Terminologia Anatomica (Ercoli et al., 2005) names “parametrium” the structure joining the corpus uteri to the pelvic sidewall while the tissue joining the uterine cervix and upper vagina to the pelvic side wall is named “paracervix” (Fig. 1). The current problem is that generations of surgeons have named the Terminologia Anatomica paracervix “lateral parametrium”, or even more improperly cardinal, or Mackenrodt, ligament. For this reason, even though the nodes referred to in the paper are rightly named “parametrial”, it is suggested to use the adjective “parauterine” to avoid confusion. Of note, Terminologia Anatomica also avoids using the adjectives “upper” and “lower”, which are dependent on the position of the patient and the surgeon.
Interestingly, the rates of involvement of both the parauterine segment (Lührs et al., 2021 Sep 8) and of the lateral paracervix (Querleu et al., 1998) are similar, and low, in the order of 2%, even though the two structures are different. This is pure coincidence, but overall reflects the uncommon involvement of nodes located between the uterus and cervix and the pelvic sidewall in very early cervical cancers. The proportion is higher in more bulky tumors (Burghardt et al., 1988, Girardi et al., 1989). An issue is to name, or not, the paracervical or parauterine nodes “sentinel lymph nodes” when the state of the art on this matter is to name sentinel only regional (lateropelvic, common iliac, or aortic) nodes.
This discussion is not only academic, as it impacts the template of radical hysterectomy. The parauterine lymphatic and/or the lateral paracervical lymph-bearing tissue are easy to remove. The resection of these tissues admittedly identifies a small proportion of patients with microscopic in-transit cancer cells, yet without additional risk or long-term side effect. Specifically to the parauterine area, or upper lymphatic pathway, routine division of the uterine artery at its origin allows to remove some oncologically relevant tissue and should be part of every radical hysterectomy, and possibly of every hysterectomy for cancer.
The discussion also impacts the technique of pelvic lymphadenectomy, as the traditional template of parietal lymph node dissection, traditionally limited by the obliterated umbilical artery medially and the obturator nerve caudally, is not a comprehensive pelvic lymph node dissection. Finally, clinical stage I cervical cancers with positive paracervical or parauterine lymph nodes can be staged either high risk stage I, or microscopic stage IIB, or stage IIIC1 cervical cancer. A consensus on staging assignment in the presence of positive paracervical or parauterine lymph nodes is badly needed.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- Benedetti-Panici P., Maneschi F., D'Andrea G., Cutillo G., Rabitti C., Congiu M., Coronetta F., Capelli A. Early cervical carcinoma. The natural history of lymph node involvement redefined on the basis of thorough parametrectomy and giant section study. Cancer. 2000;88(10):2267–2274. [PubMed] [Google Scholar]
- Burghardt, E., Haas, J., Girardi, F., 1988. The significance of the parametrium in the operative treatment of cervical cancer. Baillière's Clin. Obstetrics Gynaecol. 2, 879–888. https://doi.org/10.1016/s0950-3552(98)80015-1. [DOI] [PubMed]
- Ercoli A., Delmas V., Fanfani F., Gadonneix P., Ceccaroni M., Fagotti A., Mancuso S., Scambia G. Terminologia Anatomica versus unofficial descriptions and nomenclature of the fasciae and ligaments of the female pelvis: a dissection-based comparative study. Am. J. Obstet. Gynecol. 2005;193(4):1565–1573. doi: 10.1016/j.ajog.2005.05.007. [DOI] [PubMed] [Google Scholar]
- Girardi F., Lichtenegger W., Tamussino K., Haas J. The importance of parametrial lymph nodes in the treatment of cervical cancer. Gynecol. Oncol. 1989;34(2):206–211. doi: 10.1016/0090-8258(89)90143-1. [DOI] [PubMed] [Google Scholar]
- Girardi F., Pickel H., Winter R. Pelvic and parametrial lymph nodes in the quality control of the surgical treatment of cervical cancer. Gynecol. Oncol. 1993;50:333. doi: 10.1006/gyno.1993.1220. [DOI] [PubMed] [Google Scholar]
- Lührs O., Ekdahl L., Geppert B., Lönnerfors C., Persson J. Resection of the upper paracervical lymphovascular tissue should be an integral part of a pelvic sentinel lymph node algorithm in early stage cervical cancer. Gynecol. Oncol. 2021 doi: 10.1016/j.ygyno.2021.08.031. S0090-8258(21)01328-7. [DOI] [PubMed] [Google Scholar]
- Querleu D., Leblanc E. In: Endoscopic surgery for gynaecologists. 2nd ed. Sutton C., Diamond M., editors. Saunders; London: 1998. Laparoscopic pelvic lymphadenectomy; pp. 407–416. [Google Scholar]
- Querleu D., Morrow C.P. Classification of radical hysterectomy. Lancet Oncol. 2008;9(3):297–303. doi: 10.1016/S1470-2045(08)70074-3. [DOI] [PubMed] [Google Scholar]
- Querleu D., Narducci F., Poulard V., Lacaze S., Occelli B., Leblanc E., et al. Modified radical vaginal hysterectomy with or without laparoscopic nerve-sparing dissection: a comparative study. Gynecologic Oncol. 2002;85:154–158. doi: 10.1006/gyno.2002.6588. [DOI] [PubMed] [Google Scholar]
- Winter R., Haas J., Reich O., Koemetter R., Tamussino K., Lahousen M., Petru E., Pickel H. Parametrial spread of cervical cancer in patients with negative pelvic lymph nodes. Gynecol. Oncol. 2002;84(2):252–257. doi: 10.1006/gyno.2001.6495. [DOI] [PubMed] [Google Scholar]