Abstract
When COVID-19 disrupted autism spectrum disorder (ASD) research globally many clinical trials of behavioral interventions pivoted to telehealth. Telehealth has the potential to increase geographic reach and improve racial/ethnic diversity in research. This matters because most ASD intervention studies have primarily included White, upper-middle income families from North America and Europe. Participant homogeneity limits our ability to identify what types of intervention works in which context for which populations. Importantly, telehealth needs to ‘fit’ the local context, and in particular, include strategies that factor in the ‘digital divide’. This Short Report details contextual considerations and pre-implementation pragmatic adaptations in two ASD clinical trials that include Early Start Denver Model (ESDM)-informed caregiver coaching in the United States and South Africa. By comparing and contrasting how implementation context informed the telehealth pivot in these two clinical trials in different hemispheres we highlight equity considerations for adaption. The pandemic is an opportunity to understand how remote intervention can ‘fit’ diverse contexts, while providing valid scientific results. It is however important that adaptations be documented and feasibility of the adapted approach be tracked. COVID-19 related telehealth adaptations of behavioral interventions could facilitate the development of new strategies with wider global impact.
Keywords: Telehealth, Caregiver coaching, Autism spectrum disorder, Adaptation, Digital divide
Introduction
The COVID-19 pandemic caused many autism spectrum disorder (ASD) clinical trials to pivot to telehealth (Amaral & de Vries, 2020). For trials evaluating caregiver coaching, telehealth has a number of advantages over in-person delivery, including cost-effectiveness, greater access to underserved populations, and improved understanding of family routines (Knutsen et al., 2016). Telehealth has the potential to increase geographic reach and diversity of participants. Globally, numerous gaps exist in who benefits from intervention research. The vast majority of intervention research has been lab-based and conducted with Caucasian, upper/middle income families in the United States (US) and Europe (Stahmer, Dababnah, & Rieth, 2019). Representation in trials across the full range of heterogeneity is essential for understanding which treatments are broadly effective.
In order to increase representation in clinical trials, interventions may need to be adapted to address comorbidities in addition to workforce capacity (Divan et al., 2019). The Exploration, Preparation, Implementation, Sustainment (EPIS) implementation science framework, provides a structure to guide how researchers adapted pre-COVID-19 study designs and understanding the degree to which new telehealth platforms fit the implementation context (Aarons, Hurlburt, & Horwitz, 2011). EPIS emphasizes the importance of contextual barriers and facilitators, and innovation factors that relate to the intervention. Clearly documenting each aspect of adaptation is needed. Stirman and colleagues developed a Framework for Reporting Adaptations and Modifications (FRAME), which characterizes different forms of intervention modifications (Wiltsey Stirman, Baumann, & Miller, 2019). Without understanding the adaptations that have occurred, evaluation of strategies that result in differences in implementation success may be impeded.
In this Short Report we detail contextual considerations and pre-implementation telehealth adaptations due to COVID-19 using constructs from the EPIS framework and FRAME in two clinical trials that are evaluating Early Start Denver Model (ESDM)-informed caregiver coaching in the US and South Africa. ESDM is an evidence-based naturalistic developmental behavioral intervention, which promotes child social engagement by embedding social learning opportunities in preferred routines, thereby heightening the reward value of engagement, and increasing child social attention (Dawson et al., 2010; Schreibman et al., 2015). New social learning experiences impact child brain development, in addition to their social partners, by rewarding their partner’s efforts, and thereby motivating them to interact more with their child. By comparing how different contexts in the US versus South Africa informed researchers’ pivot to telehealth, we highlight equity considerations for adaption.
Description of Clinical Trials Pre-COVID:
A study in the Duke Centre for Autism and Brain Development at Duke University in North Carolina was designed to examine the impact of combination medication and ESDM-informed caregiver-coaching for improving social skills of children ages 3–10 years with co-occurring ASD and attention-deficit/hyperactivity disorder (ADHD). Prior to COVID-19, caregiver coaching was conducted in the laboratory. The structure of each session followed ESDM caregiver-coaching, including a check-in with the caregiver; warm-up activity and reflection; review of session topic; coaching on session topic and reflection; and closing, which addresses generalization and implementation difficulties (Figure 1a illustrates pre-COVID in-person session structure). A portion of the first coaching session was devoted to developing a small set of goals with the caregiver. While all sessions were delivered by an ESDM-certified caregiver coach and fidelity scales were used, pre-COVID-19 adaptations to improve ‘fit’ with target population and study were made. These included shortening the number of weekly sessions from 12 to 8, 1-hour sessions, including a session on managing challenging behaviors associated with ADHD, and adapting strategies for older and more developmentally advanced participants (for example, a greater focus on pragmatic language, social skills, and creative play) (See Table 1).
Figure 1.
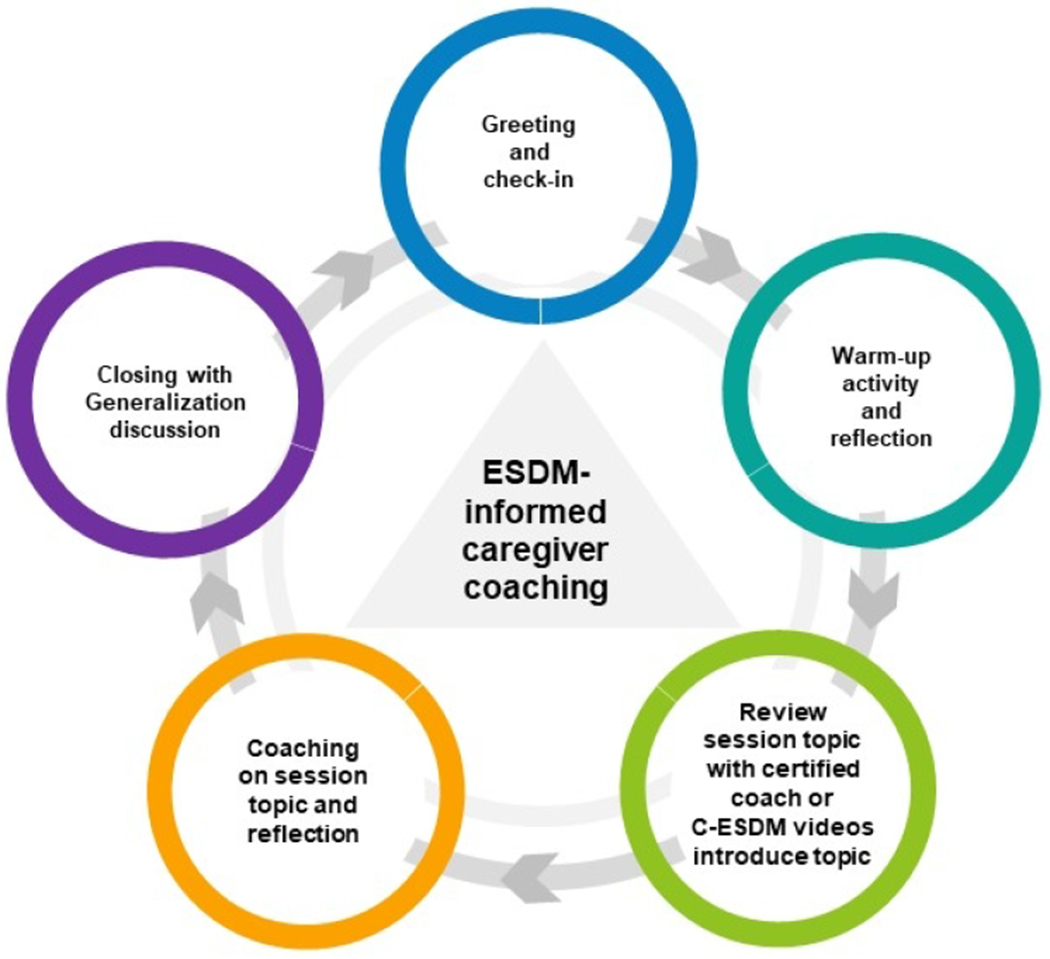
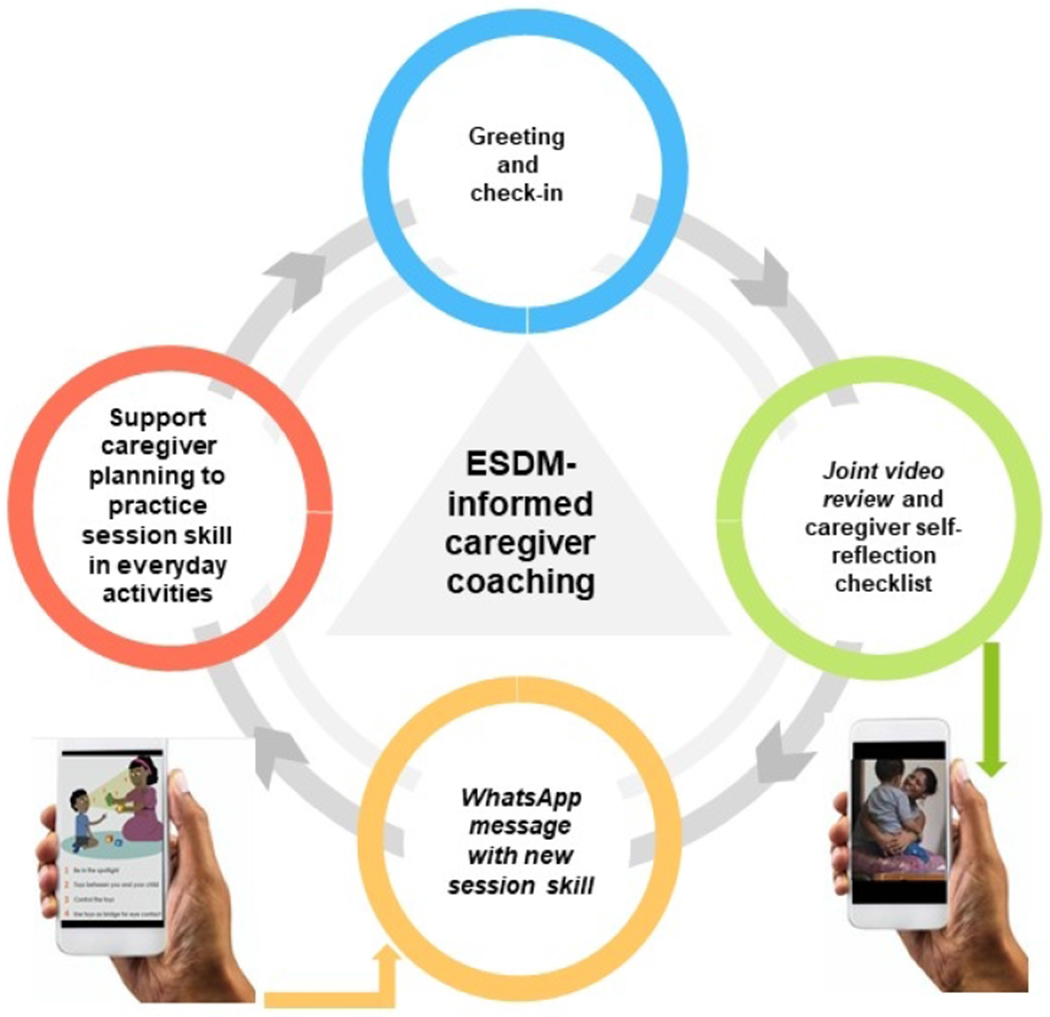
a: In-person session structure at both sites and synchronous telehealth session structure at Duke
b: Asynchronous telehealth session structure at the University of Cape Town Note: Features unique to this model marked in italics
Table 1:
Pre-COVID and Post-COVID Adaptations
| Duke University |
| Pre-COVID Adaptations |
| Approach adapted for children ages 3-10 years with co-occurring ASD and ADHD |
| Adaptations by ESDM certified trainers and ESDM co-developer |
| Coaching sessions reduced from 12 to 8, 1-hour in-person sessions |
| Two goals developed by caregiver in first coaching session (No Curriculum Checklist) |
| Post-COVID Adaptations |
| Telehealth adaptations by ESDM trainers and ESDM co-developer |
| Telehealth coaching adapted for synchronous delivery (asynchronous available if limited broadband) |
| Session structure and content maintained with synchronous telehealth delivery |
| No additional training needed to facilitate synchronous telehealth coaching |
| University of Cape Town |
| Pre-COVID Adaptations |
| Adaptations of training approach and supervision structure for non-specialist delivery |
| Adaptations by ESDM certified trainer and ESDM certified therapists |
| C-ESDM videos used to convey session topics in 12, 1-hour in-person coaching sessions |
| Text-based visual aids (‘refrigerator lists’) with core intervention content displayed during coaching |
| Post-COVID Adaptations |
| Telehealth adaptations by ESDM trainer, certified therapists, with consultation from C-ESDM developer |
| Telehealth coaching adapted for asynchronous delivery |
| Session structure adaptations: Pre-recorded caregiver-child video, WhatsApp message with session skill |
| Two goals developed by caregiver in first coaching session (No Curriculum Checklist) |
| Session content adaptations: Self-reflection checklist, session-specific visual and text-based WhatsApp messages, and non-specialist session scripts |
| Additional training of non-specialists on new materials and technological requirements |
In a study in the Centre for Autism Research (CARA) at the University of Cape Town (UCT) in South Africa, a caregiver coaching version of the Community-ESDM (C-ESDM), an open access, web-based tool, was adapted pre-COVID-19 for non-specialist delivery with children with ASD who were 2-6 years old. Task shifting or task sharing coaching to a non-specialist workforce is responsive to low resource environments and a key implementation strategy. Prior to COVID-19, all caregiver coaching sessions were conducted at partner school sites. While the structure of the 12, 1-hour coaching sessions followed the same ESDM-coaching approach utilized at Duke University (Figure 1a illustrates pre-COVID in-person session structure), pre-COVID-19 adaptations were made to improve contextual ‘fit’. These included: adapting the training approach and supervision structure for non-specialists; using C-ESDM videos to convey session topics; and displaying simple text-based visual aids (‘refrigerator lists’) containing core intervention content in each session (See Table 1). Fidelity of intervention implementation was assessed using ESDM fidelity scales. Both US and South African studies are on-going.
Contextual Considerations:
Adaptations were guided by the Preparation phase of EPIS, which aims to identify possible implementation barriers and facilitators in the inner and outer contexts, and construct a plan to utilize facilitators and mitigate barriers during implementation. While COVID-19 is a global pandemic, its impact varies depending on context. In EPIS, the outer context refers to factors that are external to the institution or organization. The most significant outer contextual consideration for telehealth is technology. Most telehealth interventions utilize synchronous coaching whereby the coach provides instruction via live video conferencing, which requires high speed internet. Globally, deep ‘digital divides’ exist (Kumm, Viljoen and de Vries, in revision). The Federal Communications Commission (FCC) reports that more than 21 million Americans lack adequate broadband access, with those living in rural communities and on tribal lands being particularly at risk (Federal Communications Commission, 2017). In North Carolina, 80 of 100 counties are rural, and while 99.5% of geographic area in urban counties is covered by broadband, only 82% of rural counties have this access. Durham, where Duke is located, is urban and most study participants live within surrounding suburban or urban counties, such that the percentage of participants with broadband access is high. In sub-Saharan Africa, the ‘digital divide’ is stark. Fewer than 25% of households own a computer, and even fewer connect to the internet using broadband (Pew Research Center, October 2018). However, many connect to the internet using smartphones with pre-paid mobile data. South Africa has the highest smartphone penetration across Africa, and this access is increasing (82% in 2018 and 91% in 2019). Thus, telehealth that utilizes smartphone technology may be feasible (Independent Communications Authority of South Africa, 2020; Kumm, Viljoen and de Vries, in revision).
In EPIS, the inner context refers to the factors within the institution or organization, such as leadership, infrastructure and resources, policies and staffing, in addition to characteristics of participants who receive the intervention. Both studies are conducted at reputable, globally recognized Universities with strong leadership, institutional review/human research ethics boards, and supportive infrastructure. Both organizations provided rapid guidance on policies concerning human subjects research, which indicated that studies should be transitioned to telehealth for the safety of staff and participants. Both studies are funded, and funding remained in place to facilitate adaptations to allow recommencing data collection. Organizational barriers included initial hesitancy to use telehealth because this approach was novel, evolving guidelines on acceptable telehealth-platforms, and large amounts of rapidly changing information on policies and procedures. Participant characteristics that facilitated telehealth transition at both sites included motivated caregivers who had received some in-person coaching prior to COVID-19 and were familiar with the study teams. While most participants had access to technology, barriers across sites included varied internet access and participant confidence in their technological skills. In the South African study in particular, lack of space, materials and resources, and busy home environments were potential barriers (Guler, de Vries, Seris, Shabalala, & Franz, 2018). In EPIS, innovation factors relate to the intervention which needs to fit with both the outer and inner context. In both studies, intervention developers are research team members, and flexible in shaping the intervention for implementation in the pandemic. This allowed flexibility to tailor the intervention, while maintaining core principles.
Post-COVID Telehealth Pragmatic Adaptations:
In both studies, pre-implementation telehealth adaptations were conducted, informed by the implementation context and documented using constructs from FRAME. Adaptation decisions were made collaboratively by the principal investigator and intervention team members. Community stakeholders were not involved in the telehealth adaptation. The immediate goal was to pivot to deliver a feasible intervention in the setting of COVID-19. At Duke, adaptations involved contextual modifications, including changes to the way in which treatment is delivered, including the coaching format and delivery setting. ESDM has been delivered through telehealth in the home environment, with research supporting synchronous coaching where session content and structure are maintained (see Figure 1a) (Vismara et al., 2016). Therefore, coaching in the child’s natural environment, the home, aligned with intervention principles. In the Duke study, the proportion of participants with broadband access has been high. Given that telehealth can increase geographic reach, including rural, low-resource communities, the study adopted an approach that could be tailored to family resources. To accommodate those without high-speed internet, a modified version was created that involved contextual modifications to the format with asynchronous delivery consisting of: a) obtaining a 6-minute video of the caregiver-child dyad engaged in free play, shared with the coach via a secure server in advance of the session; (b) during the session, the caregiver and coach reviewing the video, and the caregiver completing a self-reflection checklist; c) staff sharing with the family via email the session materials; and d) the session itself being delivered via phone. The material remained the same across approaches, although the modalities differed (live coaching vs. phone call). Overall, the study retained its fidelity and core elements. The coaches needed no additional training to transition to synchronous telehealth sessions.
In South Africa, post-COVID-19 adaptations involved contextual and content modifications, including changes to the way coaching was delivered and session materials. Knowledge of available technology informed contextual changes to both the coaching format and delivery setting. Coaching was changed to an asynchronous format, with similar adaptations to the session structure described in the paragraph above, however session materials were shared with the family via WhatsApp, a low-cost messaging software widely used in South Africa (Figure 1b illustrates asynchronous telehealth session structure). In line with institutional policies, no sensitive participant information was sent over WhatsApp in message format.
For delivery setting, instead of sessions occurring in the school, the caregiver-child video was recorded at home, a naturalistic environment. Based on knowledge of participant characteristics, content was modified to include changes in packaging of intervention materials and addition of self-reflection checklists. The in-person study used C-ESDM videos and ‘refrigerator lists’ to convey topics. Due to high data costs, streaming or downloading videos would be cost prohibitive. Therefore, the principal investigator and intervention team members, with input from a C-ESDM developer, created session-specific visual and text-based content, informed by ‘refrigerator lists’, that could be sent to caregivers via WhatsApp. During the session, the caregiver viewed materials on their phone while the non-specialist coach reviewed a script created by the research team that described the session topic. In addition, the study team added self-reflection checklists, completed by the caregiver following video review. This checklist, sent via WhatsApp, aimed to sensitize the caregiver to behaviors and helped structure the post-video reflection. The study retained its fidelity and core elements. Additional training of non-specialists was conducted by South African study team members, and consisted of 2-hour sessions over 4 days focusing on new materials, technological requirements, and 2 practice coaching sessions with a caregiver-child dyad.
Discussion
COVID-19 significantly affected clinical research globally and forced a rapid transition to telehealth (Amaral & de Vries, 2020). This transition, viewed by many as a potential silver lining of the pandemic, could have a global impact. The goal of the modifications described in this Short Report was to pivot to a feasible intervention in the setting of the pandemic that could increase reach and improve ‘fit’. Developing and testing feasible telehealth solutions will potentially improve access and representation of diverse participants in ASD clinical research. The contextually-informed telehealth pivot facilitated continuation of ASD clinical trials that included participants under-represented in research. This matters because homogeneity of research participants limits our ability to identify what types of intervention work in which context for which populations.
Even before the pandemic, health care services were becoming increasingly digitized (van Velthoven, Cordon, & Challagalla, 2019). It is, however, critical that technology fit the local context and account for the ‘digital divide’ (Kumm, Viljoen and de Vries, in revision). Adapting for equity allows those with varying levels of technology and internet to access services. If digital equity is not achieved, this will negatively impact the health and well-being of certain communities. It is important to highlight disparity in the impact of the implementation context on telehealth adaptations. While contextual adaptations sufficed in the high-resource setting, multi-level adaptations (including content, context and training) were necessary in the study conducted in the lower-resource setting.
Telehealth adaptations that ‘fit’ the local context may result in programs that are more likely to be adopted at a community level and address the research-to-practice gap. The pandemic is an opportunity to better understand how remote intervention can ‘fit’ diverse settings by accounting for technological access of end-users, while providing valid scientific results. Alongside these efforts, it is important that the feasibility of intervention adaptations be documented. Tracking adaptations could facilitate the development of new strategies with wider population-based relevance and increased global impact.
Funding acknowledgements:
This work was supported by NIH Autism Centers of Excellence Award NICHD P50HD093074, NIMH R21MH120696, and NIMH K01MH104370.
Footnotes
Conflict of Interest: Dawson is on the Scientific Advisory Boards of Janssen Research and Development, Akili Interactive, LabCorp, Inc, Roche Pharmaceutical Company, and Tris Pharma, is a consultant for Apple, Inc., Gerson Lehrman Group, Guidepoint, Inc, Axial Ventures, Teva Pharmaceutical, and is CEO of DASIO, LLC. She has received book royalties from Guilford Press, Oxford University Press, and Springer Nature Press. Howard reports personal fees from Roche.
References:
- Aarons GA, Hurlburt M, & Horwitz SM (2011). Advancing a conceptual model of evidence-based practice implementation in public service sectors. Adm Policy Ment Health, 38(1), 4–23. doi: 10.1007/s10488-010-0327-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amaral DG, & de Vries PJ (2020). COVID-19 and Autism Research: Perspectives from Around the Globe. Autism Res, 13(6), 844–869. doi: 10.1002/aur.2329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dawson G, Rogers S, Munson J, Smith M, Winter J, Greenson J, … Varley J (2010). Randomized, controlled trial of an intervention for toddlers with autism: the Early Start Denver Model. Pediatrics, 125(1), e17–23. doi: 10.1542/peds.2009-0958 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Divan G, Vajaratkar V, Cardozo P, Huzurbazar S, Verma M, Howarth E, … Green J (2019). The Feasibility and Effectiveness of PASS Plus, A Lay Health Worker Delivered Comprehensive Intervention for Autism Spectrum Disorders: Pilot RCT in a Rural Low and Middle Income Country Setting. Autism Res, 12(2), 328–339. doi: 10.1002/aur.1978 [DOI] [PubMed] [Google Scholar]
- Federal Communications Commission. (2017). Mapping Broadband Health in America. Retrieved from https://www.fcc.gov/health/maps
- Guler J, de Vries PJ, Seris N, Shabalala N, & Franz L (2018). The importance of context in early autism intervention: A qualitative South African study. Autism, 22(8), 1005–1017. doi: 10.1177/1362361317716604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Independent Communications Authority of South Africa. (2020). State of the ICT Sector in South Africa - 2020 Report. Retrieved from https://www.icasa.org.za/legislation-and-regulations/state-of-the-ict-sector-in-south-africa-2020-report
- Knutsen J, Wolfe A, Burke BL, Hepburn S, Lindgren S, & Coury D (2016). A Systematic Review of Telemedicine in Autism Spectrum Disorders Rev J Autism Dev Disord, 3, 330–344. doi: 10.1007/s40489-016-0086-9 [DOI] [Google Scholar]
- Kumm A, Viljoen M, & de Vries PJ (in revision). The digital divide in technologies for autism: feasibility considerations for low- and middle-income countries. J Autism Dev Disord. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pew Research Center. (October 2018). Internet connectivity seen as having positive impact on life in sub-Saharan Africa but digital divides persist Retrieved from file:///C:/Users/lf29/AppData/Local/Temp/Pew-Research-Center_Technology-use-in-Sub-Saharan-Africa_2018-10-09.pdf
- Schreibman L, Dawson G, Stahmer AC, Landa R, Rogers SJ, McGee GG, … Halladay A (2015). Naturalistic Developmental Behavioral Interventions: Empirically Validated Treatments for Autism Spectrum Disorder. J Autism Dev Disord, 45(8), 2411–2428. doi: 10.1007/s10803-015-2407-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stahmer AC, Dababnah S, & Rieth SR (2019). Considerations in implementing evidence-based early autism spectrum disorder interventions in community settings. Pediatr Med, 2. doi: 10.21037/pm.2019.05.01 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Velthoven MH, Cordon C, & Challagalla G (2019). Digitization of healthcare organizations: The digital health landscape and information theory. International Journal of Medical Informatics, 124, 49–57. doi: 10.1016/j.ijmedinf.2019.01.007 [DOI] [PubMed] [Google Scholar]
- Vismara LA, McCormick CEB, Wagner AL, Monlux K, Nadhan A, & Young GS (2016). Telehealth Parent Training in the Early Start Denver Model: Results From a Randomized Controlled Study Focus on Autism and Other Developmental Disabilities, 33(2), 67–79. doi: 10.1177/1088357616651064 [DOI] [Google Scholar]
- Wiltsey Stirman S, Baumann AA, & Miller CJ (2019). The FRAME: an expanded framework for reporting adaptations and modifications to evidence-based interventions. Implement Sci, 14(1), 58. doi: 10.1186/s13012-019-0898-y [DOI] [PMC free article] [PubMed] [Google Scholar]


