Abstract
Objective
Anecdotal reports indicate an increase in mental health presentations and acuity to EDs during the COVID‐19 pandemic and associated stay at home restrictions. Paediatric and adolescent data to confirm this are unavailable in the Australian setting.
Methods
Retrospective electronic medical record review of all ED patients with mental health discharge codes at a large tertiary children's hospital in Australia during the period of stay at home restrictions from 1 April to 30 September 2020 compared with the same dates in 2019.
Results
We found a 40% decrease in ED presentations (18 935–11 235) with a concurrent 47% increase in mental health presentations (809–1190) to ED during the study periods between 2019 and 2020. This resulted in an increase of 100 mental health admissions from ED. Diagnoses with greatest percentage increases were eating disorders, social issues and suicidality. We found suicidality presentation numbers were highest in June to September 2020 compared with 2019. Patients with a diagnosis of suicidality had a higher rate of re‐presentation in 2020 (1.83 presentations per patient) compared to 2019 (1.38 presentations per patient).
Conclusions
Despite an overall decrease in ED presentations, the absolute increase in mental health presentations for children and adolescents during the stay at home restriction period was pronounced. It is unclear how sustained this change and the impact on mental health resource use will be post‐pandemic.
Keywords: self‐harm, children, adolescents, COVID‐19, suicidality
We explored the impact of prolonged COVID‐19 restrictions in Melbourne, Australia on mental health and specifically suicidality presentations to the paediatric ED. We found a 47% increase in all mental health presentations and a 59% increase in suicidality presentations during the stay at home restriction period in 2020, compared with the same dates in 2019.

Key findings.
In line with other reports, total paediatric ED visits decreased by 40% during the stay at home restrictions period of the COVID‐19 pandemic.
During the same period, absolute numbers for ED presentations for mental health increased by 47% and for suicidality by 59% compared with pre‐pandemic data.
There was also an absolute increase of 109% in eating disorder diagnoses and an increase of 88% in diagnoses of social issues.
Introduction
Children and adolescents with mental health (MH) issues make up a significant number of paediatric ED (PED) presentations. In 2018, 6.7% of all ED presentations to the Royal Children's Hospital (RCH), Melbourne, aged 7 up to 18 years of age were assigned a MH diagnosis. 1 Overall, self‐harm and suicidal ideation (including drug overdose and suicide attempt) made up 55% of all MH presentations. 1
The World Health Organization characterised COVID‐19 as a pandemic on 11 March 2020 2 and by late March 2020 there were over 900 active COVID‐19 cases in Australia, 3 prompting national stay at home restrictions from 25 March until 11 May 2020. 4 An increase in community cases of COVID‐19 in Melbourne in late June prompted re‐introduction of stay at home restrictions for specific postcodes from 30 June 4 and then for the entirety of metropolitan Melbourne from 8 July. 5 Because of ongoing increases in daily COVID‐19 case numbers across Victoria, stage 4 restrictions were introduced on 2 August for metropolitan Melbourne and Mitchell Shire and stage 3 restrictions remained in regional Victoria. 6 These were in place until a gradual easing of restrictions between late September and 26 October 2020. 7
In the early stages of the pandemic, MH presentations to metropolitan Melbourne PEDs increased by 35%, despite an overall reduction in PED presentations. 8 In the adult population, there was a decrease in ED attendance to metropolitan EDs in Victoria, New South Wales and Western Australia, 9 , 10 , 11 with a concurrent decrease in MH presentations in both Victoria 9 and Western Australia, 11 and an increase in MH presentations in New South Wales. 10
Internationally, several centres found a similar decrease in total PED presentations 12 , 13 and most report a concurrent decrease in MH presentations. 14 , 15 , 16 , 17 , 18 , 19 , 20 Two studies from the USA, however, found a steady increase in the proportion of MH presentations from April to October 21 and significantly higher rates of suicidal ideation and attempts in 2020 compared with 2019. 22 Anecdotally, MH presentations to RCH ED, particularly those associated with suicidality, have continued to increase beyond the early stages of the pandemic, but this has not yet been examined. This retrospective review aims to explore the effects of prolonged stay at home restrictions in metropolitan Melbourne on ED MH presentations and particularly those with a diagnosis of suicidality.
Methods
Design and setting
We conducted a retrospective review of all ED patients with MH discharge codes between April to September 2019 and 2020 at the RCH in Melbourne, Australia. The dates selected were a 6‐month period in 2020 where stay at home restrictions were in place for the majority of the time in metropolitan Melbourne. The same period in 2019 was selected for comparison. In order to assess if any changes in 2019 were consistent with prior years in terms of MH presentations, we also investigated the overall MH data from the same time period in 2018.
RCH is a large tertiary children's hospital with an annual census of 85 347 children (2018) and is a designated MH facility under Victorian Mental Health Act regulation, 23 servicing the population of children and adolescents in greater Melbourne. The MH service consists of the ED, a 16‐bed adolescent inpatient unit and accessible outpatient services. 24 The study was approved by the Human Research and Ethics Committee at RCH (QA 69652 RCHM‐2020).
Study procedure
A list of 66 MH related ICD 10 diagnostic codes were used to identify MH presentations to ED from 1 April to 30 September 2019 and the same time period in 2020. This list included all psychiatric diagnoses available to the treating clinician and other diagnoses not specifically psychiatric but often associated with a MH presentation (ingested foreign body, forearm laceration and hallucination). We confirmed eligibility by chart review and, for identified patients, extracted relevant demographic, timing, diagnostic and disposition data.
Inclusion criteria
All MH presentations aged 7–18 years presenting to ED during the study dates who had a MH diagnosis assigned by the ED treating clinician (junior and senior medical staff and nurse practitioners).
Exclusion criteria
Children under 7 years of age and over 18 years of age.
Presentations with a diagnosis of ingested foreign body, forearm laceration or hallucination where there was no MH issue.
Definitions
Stay at home restrictions or ‘lockdowns’ – a Public Health Order requiring people to stay at home except for essential needs. 5 Stage 3 restrictions included these stay at home orders and additionally banned visitors to houses, limited gatherings outside the house and introduced compulsory face coverings outside the house. 5 Stage 4 restrictions included all stage 3 restrictions and additionally limited time outside the house to 1 h a day for exercise, introduced a curfew from 20.00 to 5.00 hours and limited travel to no more than 5 km from the home. 6
Analysis
Data were entered into an Excel database (Microsoft, Seattle, WA, USA) and analysed using Stata 14 (StataCorp, College Station, TX, USA). From total ED presentations aged 7–18 years of age during the study dates in 2018, 2019 and 2020, we identified all MH related presentations and determined ED treating clinician diagnoses. We then assessed demographic, process and diagnostic data for all MH presentations and those with a diagnosis of suicidality during the study dates in 2019 compared with 2020, using frequencies and percentages with 95% confidence intervals (CIs). Patients in the suicidality cohort included diagnoses of suicidal ideation, suicidal thoughts, suicidal risk, suicide attempt, self‐harm citing suicidality and deliberate drug overdose citing suicidality. We also determined month‐by‐month comparison of all ED presentations, MH presentations and diagnoses of suicidality during the study dates in 2019 compared with 2020.
Results
During the study dates in 2018, there were 18 972 presentations of 7–18 year olds to ED, of which 882 (4.6%) were related to a MH diagnosis. Of the presentations with a MH diagnosis, 435 (49.3%) had a diagnosis of suicidality. During the same period in 2019, there were 18 935 presentations of 7–18 year olds to ED and 809 (4.3%) were related to a MH diagnosis (Fig. 1). Of the presentations with a MH diagnosis, 419 (51.8%) had a diagnosis of suicidality (Fig. 1). In 2020 during the same time period, there were 13 546 presentations of 7–18 year olds to ED; 2311 presented solely for COVID‐19 testing and were redirected to the respiratory infection clinic, and 11 235 were seen in ED. Of these, 1190 (10.6%) were related to a MH diagnosis (Fig. 1) and 667 (56.1%) had a diagnosis of suicidality (Fig. 1).
Figure 1.
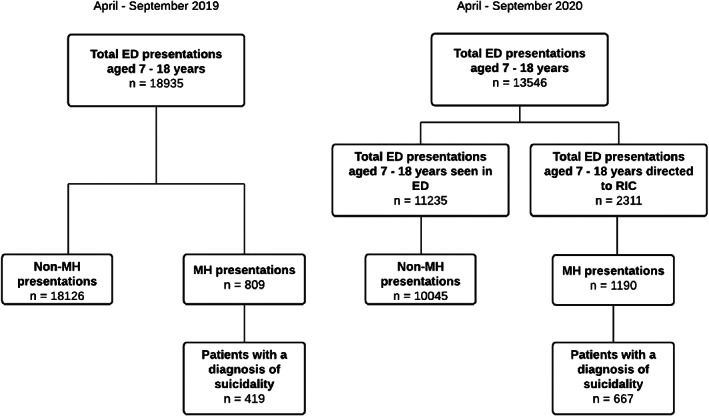
Flowchart identifying patients with a mental health (MH) diagnosis and specifically a diagnosis of suicidality.
This represents an absolute decrease in total ED presentations of 40.7% (95% CI 40–41.4), with a concurrent 47.1% (95% CI 43.6–50.6) increase in MH presentations (Table 2). This was associated with an additional 100 admissions (184–284) (Table 1). Of the MH presentations, there was an absolute increase in eating disorder, social issues and suicidality diagnoses, compared with 2019 (Table 2).
TABLE 1.
ED mental health presentations aged 7–18 years April–September 2019 and 2020
| Demographics | Total mental health presentations | Comparison of 2019 and 2020 | ||||
|---|---|---|---|---|---|---|
| 2019 (n = 809) | 2020 (n = 1190) | |||||
| n | % total | n | % total | Variable compared | OR (95% CI) | |
| Sex | ||||||
| Female | 561 | 69.3 | 903 | 75.9 | F:M | 1.37 (1.12–1.68) |
| Male | 240 | 29.7 | 282 | 23.7 | ||
| Other | 8 | 1.0 | 5 | 0.4 | ||
| Age, years | ||||||
| 7–12 | 145 | 17.9 | 164 | 13.8 | 7–12:13–18 | 1.37 (1.07–1.74) |
| 13–18 | 664 | 82.1 | 1026 | 86.2 | ||
| ATS† category | ||||||
| 1 | 20 | 2.5 | 22 | 1.8 | ATS† Cat1–2:Cat3–5 | 0.81 (0.61–1.08) |
| 2 | 64 | 7.9 | 127 | 10.7 | ||
| 3 | 542 | 67.0 | 813 | 68.3 | ||
| 4 | 173 | 21.4 | 220 | 18.5 | ||
| 5 | 10 | 1.2 | 8 | 0.7 | ||
| LOS, h | ||||||
| <4 | 310 | 38.3 | 533 | 44.8 | >12 h:<12 h | 1.15 (0.82–1.61) |
| >4–6 | 266 | 32.9 | 335 | 28.2 | <4 h:>4 h | 1.31 (1.09–1.57) |
| >6–8 | 110 | 13.6 | 133 | 11.2 | ||
| >8–10 | 40 | 4.9 | 57 | 4.8 | ||
| >10–12 | 25 | 3.1 | 35 | 2.9 | ||
| >12 | 58 | 7.2 | 97 | 8.2 | ||
| Arrival method | ||||||
| Other (private car) | 435 | 53.8 | 602 | 50.6 | Road amb:other method | 1.18 (0.99–1.42) |
| Road ambulance | 355 | 43.9 | 572 | 48.1 | ||
| Police vehicle | 13 | 1.6 | 14 | 1.2 | ||
| Disposition | ||||||
| Discharged | 604 | 74.7 | 867 | 72.9 | Admitted:discharged | 1.12 (0.91–1.38) |
| Admitted | 184 | 22.7 | 284 | 23.9 | ||
| Left AMA | 6 | 0.7 | 5 | 0.4 | ||
| ED SSU | 13 | 1.6 | 32 | 2.7 | ||
| Left without treatment | 2 | 0.2 | 2 | 0.2 | ||
Australasian triage scale. Cat 1–2 = severe behavioural disturbance with immediate threat of harm to self or others; Cat 3–5 = nil behavioural disturbance to moderate behavioural disturbance with risk of harm to self or others. 25
AMA, against medical advice; LOS, length of stay; SSU, short stay unit.
TABLE 2.
Total numbers and diagnoses of ED presentations of patients aged 7–18 years for April–September with percentage change between 2019 and 2020
| 2019 | 2020 | Percentage change (95% CIs) | |||
|---|---|---|---|---|---|
| n | % total | n | % total | ||
| All ED presentations | 18 935 | NA | 11 235 | NA | −40.7 (−40.0 to −41.4) |
| All non‐MH presentations | 18 126 | 95.7 | 10 045 | 89.4 | −44.6 (−43.9 to −45.3) |
| All ED MH presentations | 809 | 4.3 | 1190 | 10.6 | +47.1 (43.6–50.6) |
| ICD‐10 MH diagnosis†, n | 809 | 1190 | |||
| All suicidality | 419 | 51.8 | 667 | 56.1 | +59.2 (54.3–63.9) |
| Suicidality and SH with suicidality | 313 | 38.7 | 515 | 43.3 | +64.5 (59.0–69.8) |
| Deliberate drug overdose | 106 | 12.9 | 152 | 12.3 | +43.4 (33.8–53.4) |
| Other MH disorder | 121 | 15.0 | 138 | 11.6 | +14.0 (8.4–21.5) |
| Anxiety | 79 | 9.8 | 99 | 8.3 | +25.3 (16.2–36.4) |
| Destructive behaviour | 71 | 8.8 | 90 | 7.6 | +26.8 (16.9–38.6) |
| Eating disorder | 32 | 4.0 | 67 | 5.6 | +109.4 (91.1–125.0) |
| Social issue | 34 | 4.2 | 64 | 5.4 | +88.2 (72.6–96.7) |
Diagnoses with fewer than 30 presentations per year were not included because of small numbers.
CI, confidence interval; MH, mental health; NA, not applicable; SH, self‐harm.
Figure 2 shows ED attendances for all diagnoses were reduced in April 2020 compared with 2019, and remained variably reduced each month during the study dates. Both total MH presentations and presentations with a diagnosis of suicidality were increased for each month but most significantly from June to September in 2020, compared with 2019 (Fig. 2).
Figure 2.
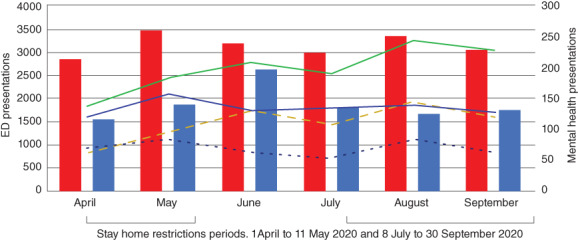
Monthly variance of total ED presentations, MH‐related presentations and suicidality diagnosis presentations from 1 April to 30 September 2019 and 2020, showing stay at home restrictions periods in 2020. Stay at home restrictions periods 1 April to 11 May 2020 (stage 3 restrictions)
4
and 8 July to 30 September (stage 3 restrictions from 8 July to 1 August, stage 4 restrictions from 2 August to 27 September).
5
,
6
( ), All ED presentations 2019; (
), All ED presentations 2019; ( ), all ED presentations 2020; (
), all ED presentations 2020; ( ), all MH presentations 2019; (
), all MH presentations 2019; ( ), all MH presentations 2020; (
), all MH presentations 2020; ( ), suicidality Dx 2019; (
), suicidality Dx 2019; ( ), suicidality Dx 2020. Dx, diagnosis; MH, mental health.
), suicidality Dx 2020. Dx, diagnosis; MH, mental health.
Patients presenting with a MH diagnosis during the study dates in 2020 were more likely to be female (odds ratio [OR] 1.37, 95% CI 1.12–1.68), aged 13–18 years of age (OR 1.37, 95% CI 1.07–1.74) and stay longer than 4 h in ED (OR 1.31, 95% CI 1.09–1.57) compared with patients with a MH diagnosis in 2019 (Table 1).
In 2019, a total of 584 patients accounted for 809 MH presentations, which is an average of 1.39 presentations per patient (range 1–12, median = 1). Most (82%, n = 479) patients presented to ED once and 18% (n = 105) presented more than once. In 2020, a total of 682 patients accounted for 1190 MH presentations, which represents an average of 1.74 presentations per patient (range 1–35, median = 1). Again, most (77.1%, n = 526) patients presented to ED once and 22.9% (n = 156) presented more than once. Patients with a diagnosis of suicidality had a higher rate of re‐representation in 2020 (1.83 presentations per patient) compared to 2019 (1.38 presentations per patient).
Discussion
The present study describes changes to the absolute frequencies of paediatric and adolescent MH presentations to the ED at a tertiary children's hospital during the COVID‐19 pandemic in Australia. We found a decrease in total ED presentations of 40% during the stay at home restrictions in 2020, which was in line with other studies. 9 , 10 , 11 , 12 , 13 , 14 , 15 , 16 , 17 , 18 , 19 , 20 Despite this overall reduction, we found a notable increase of 47% in all MH diagnoses and in particular a higher than expected increase of 59% in suicidality diagnoses compared with pre‐pandemic data from 2019. The consistencies in total ED, MH and suicidality numbers between 2018 and 2019 give an indication of a consistent baseline and indicate that the changes we report in 2020 were out of the ordinary.
Although concerns that Australia would see an increase in youth suicide in 2020, 26 the local data demonstrate that the suicide frequency in Victoria did not increase from 2019 to 2020 across age groups for both males and females. 27 Internationally, suicide trends also did not rise in the early stages of the pandemic, although the picture is less clear in low‐income countries. 28
We found that patients with a MH diagnosis in 2020 were more likely to be female teenagers who stayed longer than 4 h in ED, compared with 2019. This is consistent with existing 2018 data 1 indicating that the majority of teenagers presenting to RCH ED with suicidality are female. In both 2019 and 2020, patients with a diagnosis of suicidality represented the highest total number of presentations, although re‐presentation rates were higher for patients with suicidality in 2020 compared with 2019.
Our data did not capture the full impact of this on our acute care MH resources in terms of staff time and resources, but most notably in 2020, there was almost double the number of patients whose length of stay in the department was >12 h and 100 extra patients were admitted from ED during the stay at home restriction period.
The lockdown period was a difficult time for the vulnerable children and adolescent population with MH issues in Melbourne, Australia. The large second wave of COVID‐19 infections in metropolitan Melbourne and subsequent stricter stay at home restrictions from early July to late September resulted in most children and adolescents being schooled remotely for significant periods with limited outdoor time, movement within neighbourhoods and social contact. 6 Our data showed the most pronounced increase in both MH presentations and suicidality from June to September 2020, when the impact of educational and social changes because of extended stay at home restrictions would likely have had their greatest effect. While there is no similar paediatric or adolescent data available, these findings are consistent with survey data of 760 Australian adolescents at the peak of the pandemic (June–July 2020) which found 75% of responders reported worsening of their MH and nearly half (48.3%) were experiencing distress consistent with MH illness. 29
We know that early in the pandemic, children and adolescents with MH issues were presenting more frequently to the RCH ED 9 at a time where outpatient 24 and community MH services 30 were significantly limiting face‐to‐face appointments. It is possible that continued reduction in these services during the extended stay at home restrictions in 2020, coupled with greater MH incidence in this population, 29 has contributed to the sustained increase in MH presentations to the RCH ED that we found. We do not know what impact the social and educational changes associated with stay at home restrictions have had on the increases we found in social issues and eating disorder diagnoses. It would be useful to explore whether these presentations were due to an exacerbation of existing MH illness or due to new issues and diagnoses that emerged during the stay at home restrictions period.
The increase in MH presentations we saw in 2020 may be partly explained by outliers with frequent presentations, given that the upper range of re‐presentations was almost three times higher in 2020 compared with 2019. It is possible that for these patients, ED was one of few readily accessible services available to them during the stay at home restrictions period. This has implications for both community and ED MH services planning and allocation of resources for vulnerable children and adolescents during times when stay at home restrictions are in place. Our data may be useful for modelling for expected surges in MH presentations in future lockdowns. Future research should specifically explore the reasons for presentations from the perspective of children and their families as well as MH and ED staff, and assess how long the changes in MH presentations persist. This would assist in developing models for improving MH surge capacity.
Limitations
As a retrospective study, there were limitations to the data. While most data (demographic and administrative data) was recorded with accuracy within the EMR, other data depended on the accuracy and completeness of the data recorded by the treating clinician. We relied on ICD‐10 codes assigned by the treating clinician to identify patients with MH diagnosis and extracted EMR data for demographic data rather than chart review to verify. There is potential that data could be missing but it was deemed low risk for this descriptive study. The present study was undertaken at a single large tertiary PED that could potentially limit the generalisability of the results. We excluded patients 6 years of age and younger as they likely did not present with typical MH related presentations and were unlikely to have a psychiatric diagnosis. Because of a lack of centralised data, we were unable to assess community and private MH service attendance during the study dates and explore if the increase in ED MH presentations was associated with a decrease or mirrored by an increase in MH presentations outside the ED.
Conclusions
Despite an overall decrease in ED presentations, the absolute increase in MH presentations of children and adolescents during the stay at home restrictions period was notable. We found a higher than expected increase in suicidality diagnoses compared with pre‐pandemic data and this group continues to represent the highest number of presentations within the MH cohort. It is unclear how sustained this change and its associated impact on MH resource use will be post‐pandemic.
Acknowledgements
The study was unfunded but supported by a National Health and Medical Research Council Centre of Research Excellence grant for Paediatric Emergency Medicine (GNT1171228). FEB's time was part funded by an NHMRC Practitioner Fellowship, Canberra, Australia and a Royal Children's Hospital Foundation Grant, Melbourne, Australia.
Author contributions
AC and SMOD conceived the study, extracted and analysed the data and wrote the first draft of the paper. FEB assisted with the design of the study protocol, obtained ethics approval and revised the draft. All authors approved the final draft for submission.
Competing interests
FEB is a section editor for Emergency Medicine Australasia.
Anna Carison, MANP, Nurse Practitioner; Franz E Babl, MD, Emergency Physician; Sinead M O'Donnell, MD, Emergency Physician.
Data availability statement
Research data are not shared.
References
- 1. Say D, Carison A, Hill A, Hiscock H, Babl FE, O'Donnell SO. Paediatric mental health presentations to the emergency department – a retrospective study. J. Paediatr. Child Health 2020; 57: 684–95. [DOI] [PubMed] [Google Scholar]
- 2. World Health Organization . Timeline: WHO's COVID‐19 Response. 2020. [Cited 19 Mar 2021.] Available from URL: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/interactive-timeline#
- 3. Australian Government Department of Health . Coronavirus (COVID‐19) case numbers and statistics. 2020. [Cited 19 Mar 2021.] Available from URL: https://www.health.gov.au/news/health-alerts/novel-coronavirus-2019-ncov-health-alert/coronavirus-covid-19-case-numbers-and-statistics
- 4. Storen R, Corrigan N. COVID‐19: a chronology of state and territory government announcements (up until 30 June 2020). 2020. [Cited 19 Mar 2021.] Available from URL: https://parlinfo.aph.gov.au/parlInfo/download/library/prspub/7614514/upload_binary/7614514.pdf
- 5.Premier of Victoria. Statement from the Premier. 2020. [Cited 19 Mar 2021.] Available from URL: https://www.premier.vic.gov.au/statement-premier-74
- 6. State Government of Victoria . Statement on Changes to Melbourne's Restrictions. 2020. [Cited 19 Mar 2021.] Available from URL: https://www.premier.vic.gov.au/sites/default/files/2020-08/200802%20-%20Statement%20On%20Changes%20To%20Melbourne%E2%80%99s%20Restrictions.pdf
- 7. Premier of Victoria . Statement from the Premier. 2020. [Cited 19 Mar 2021.] Available from URL: https://www.premier.vic.gov.au/statement-premier-77
- 8. Cheek JA, Craig SS, West A, Lewena S, Hiscock H. Emergency department utilization by vulnerable paediatric populations during the COVID‐19 pandemic. Emerg. Med. Australas. 2020; 32: 870–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Mitchell RD, O'Reilly GM, Mitra B, Smit D, Miller J‐P, Cameron PA. Impact of COVID‐19 state of emergency restrictions on presentations to two Victorian emergency departments. Emerg. Med. Australas. 2020; 32: 1027–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Kam AW, Chaudhry SG, Gunasekaran N, White AJR, Vukasovic M, Fung AT. Fewer presentations to metropolitan emergency departments during the COVID‐19 pandemic. Med. J. Aust. 2020; 213: 370–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Dragovic M, Pascu V, Hall T, Ingram J, Waters F. Emergency department mental health presentations before and during the COVID‐19 outbreak in Western Australia. Australas. Psychiatry 2020; 28: 627–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Isba R, Edge R, Jenner R, Broughton E, Francis N, Butler J. Where have all the children gone? Decreases in paediatric emergency department attendances at the start of the COVID‐19 pandemic of 2020. Arch. Dis. Child. 2020; 105: 704. [DOI] [PubMed] [Google Scholar]
- 13. Lazzerini M, Barbi E, Apicella A, Marchett F, Cardinale F. Delayed access or provision of care in Italy resulting from fear of COVID‐19. Lancet 2020; 4: E10–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Joyce LR, Richardson SK, McCombie A, Hamilton GJ, Ardagh MW. Mental health presentations to Christchurch Hospital Emergency Department during COVID‐19 lockdown. Emerg. Med. Australas. 2021; 33: 324–30. [DOI] [PubMed] [Google Scholar]
- 15. Ougrin D. Debate: emergency department health presentations of young people during the COVID‐19 lockdown. Child Adolesc. Ment. Health 2020; 25: 171–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Chaiyachati BH, Agawu A, Zorc JJ, Balamuth F. Trends in pediatric emergency department utilization after institution of coronavirus disease‐19 mandatory social distancing. J. Pediatr. 2020; 226: 274–7.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. McDonnell T, Nicholson E, Conlon C et al. Assessing the impact of COVID‐19 public health stages on paediatric emergency attendance. Int. J. Res. Public Health 2020; 17: 6719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Sheridan DC. Where have all the emergency paediatric mental health patients gone during COVID‐19? Acta Paediatr. 2020; 110: 598–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Goldman RD, Grafstein E, Barclay N, Irvine MA, Portales‐Casamar E. Paediatric patients seen in 18 emergency departments during the COVID‐19 pandemic. Emerg. Med. J. 2020; 37: 773–7. [DOI] [PubMed] [Google Scholar]
- 20. DeLaroche AM, Rodean J, Aronson PL et al. Pediatric emergency department visits at US children's hospitals during the COVID‐19 pandemic. Pediatrics 2021; 14: e2020039628. [DOI] [PubMed] [Google Scholar]
- 21. Leeb RT, Bitsko RH, Radhakrishnan L, Martinez P, Njai R, Holland KM. Mental health‐related emergency department visits among children aged <18 years during the COVID‐19 pandemic – United States, January 1–October 17, 2020. Morb. Mort. Wkly. Rep. 2020; 69: 1675–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Hill RM, Rufino K, Kurian S, Saxena J, Saxena K, Williams L. Suicide ideation and attempts in a pediatric emergency department before and during COVID‐19. Pediatrics 2021; 147: e2020029280. [DOI] [PubMed] [Google Scholar]
- 23. State Government of Victoria . Mental Health Act 2014. 2014. [Cited 19 Mar 2021.] Available from URL: https://www.legislation.vic.gov.au/in-force/acts/mental-health-act-2014/022
- 24. The Royal Children's Hospital . Department of Mental Health: Our Service Response to COVID‐19. 2020. [Cited 12 Oct 2020.] Available from URL: https://www.rch.org.au/mental-health/#our-service-response-to-covid-19
- 25. Department of Health and Ageing . Emergency Triage Education Kit. 2009. [Cited 19 Mar 2021.] Available from URL: https://acem.org.au/getmedia/c9ba86b7-c2ba-4701-9b4f-86a12ab91152/Triage-Education-Kit.aspx
- 26. Orygen Youth Health . COVID‐19 Impact Likely to Lead to Increased Rates of Suicide and Mental Illness. 2020. [Cited 12 Oct 2020.] Available from URL: https://www.orygen.org.au/About/News-And-Events/2020/COVID-19-impact-likely-to-lead-to-increased-rates
- 27. Coroner's Court of Victoria . Coroner's Court Monthly Suicide Data Report: Report 2–5 October 2020. 2020. [Cited 19 Mar 2021.] Available from URL: https://www.coronerscourt.vic.gov.au/sites/default/files/2020-10/Coroners%20Court%20Suicide%20Data%20Report%20-%20Report%202%20-%2005102020.pdf
- 28. John A, Pirkis J, Gunnell D, Appleby L, Morrissey J. Trends in suicide during the COVID‐19 pandemic. Br. Med. J. 2020; 371: m4352. [DOI] [PubMed] [Google Scholar]
- 29. Li SH, Beames JR, Newby JM, Christensen H, Werner‐Seidler A. The impact of COVID‐19 on the lives and mental health of Australian adolescents. Eur. Child Adolesc. Psychiatry 2020; 28: 1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Orygen Youth Health . Responding to the COVID‐19 Outbreak. 2020. [Cited 12 Oct 2020.] Available from URL: https://www.orygen.org.au/About/Responding-to-the-COVID-19-outbreak
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Research data are not shared.


