Abstract
Coronavirus disease 2019 (COVID‐19), caused by severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) infection, has become a pandemic worldwide. Although COVID‐19 mainly affects the respiratory system, gastrointestinal (GI) manifestations have been frequently reported in such cases, even as initial symptoms. There have been several studies on different GI manifestations in patients with mild and severe disease or in remission. In this review article we summarized different GI manifestations of COVID‐19 at various disease stages and the possible mechanisms based on published literatures, as well as the significance of GI manifestations in systemic inflammatory injury.
Keywords: COVID‐19, gastrointestinal manifestation, mechanism, SARS‐CoV‐2, systemic inflammatory injury
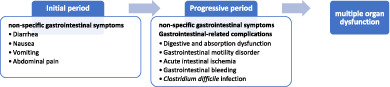
In this review article, we summarized different gastrointestinal (GI) manifestations of coronavirus disease 2019 (COVID‐19) at different disease stages and the possible mechanisms. GI symptoms may occur at 3‐10 days after the development of respiratory symptoms or fever, or sometimes present initially before the appearance of, or even without respiratory discomfort. During the disease progression, in addition to non‐specific GI symptoms, GI‐related complications, including digestive and absorption dysfunction, GI motility disorder, acute intestinal ischemia, GI bleeding and Clostridium difficile infection may appear as well. As the gut is always regarded as the motor of multiorgan dysfunction, GI dysfunction prompts a systemic inflammatory response and is closely related to poor patient prognosis in COVID‐19.
1. INTRODUCTION
Coronavirus disease 2019 (COVID‐19) is a life‐threatening condition caused by severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) infection, which was first discovered in Wuhan, Hubei Province in December 2019, and has quickly become a pandemic worldwide. COVID‐19 mainly affects the respiratory system, presenting as symptoms including fever, cough and dyspnea, 1 which are the principal clinical manifestations used to recognize COVID‐19 at the beginning of the pandemic. However, as the number of confirmed cases has surged, extrapulmonary manifestations, specifically gastrointestinal (GI) symptoms, have been frequently described. Some patients present with GI symptoms even without typical respiratory symptoms. Therefore, GI symptoms should not be neglected in the identification of COVID‐19. Moreover, there have been several studies on different GI manifestations of patients with mild or severe COVID‐19 and those in remission, 2 , 3 , 4 from which we may conclude that GI symptoms may have distinct features at different stages of the disease. Therefore, overall understanding of GI symptoms in COVID‐19 may help identify potentially infected patients effectively and predict disease progression. In this article we summarized GI manifestations and possible mechanisms at different COVID‐19 stages by reviewing the recently published literatures, trying to explain the significance of GI manifestations in the systemic inflammatory response.
2. EPIDEMIOLOGY OF GI SYMPTOMS IN COVID‐19
It has been proposed that SARS‐CoV‐2 may be transmitted to human beings by bats through other animals as the intermediate hosts. According to the recent reports that inspect the trend of confirmed cases in China, most new‐onset patients used to have a history of exposure to the seafood market, and SARS‐CoV‐2 can be detected in their fecal samples. Additionally, cases of familial clustering of COVID‐19 characterized by having only GI symptoms have been reported, 5 indicating that the virus may also be found in the GI tract, resulted in a possible fecal–oral transmission. A possibility that the GI tract is the first site to be invaded by SARS‐CoV‐2 cannot be excluded. Moreover, animal experiment has shown that both intranasal or intragastric inoculation with SARS‐CoV‐2 can lead to infection. 6 Humans are generally susceptible to SARS‐CoV‐2, especially elderly individuals or those with chronic comorbidities, and are inclined to progress to the severe or critical type of disease. 3 At present, there is no evidence that whether patients with underlying GI disease have an increased incidence of COVID‐19. 7
The incubation period of the disease in patients with GI symptoms is roughly the same as that of the general population, and the infection period may be longer because SARS‐CoV‐2 can still be detected from the fecal sample even after GI symptoms disappear.
Until August 2021, the number of cumulative confirmed cases of COVID‐19 has exceeded 200 million worldwide. Due to various sample sizes, primary end‐points and definition of symptoms, together with potential bias in retrospective studies, the proportion of patients with GI manifestations differs in published studies. A meta‐analysis involving 78 studies showed that up to 20% of COVID‐19 cases presented with GI symptoms, mainly including diarrhea, anorexia, nausea and vomiting. 8 We arrived at roughly similar results by summarizing the recent literatures (Table 1), showing that the incidence of GI symptoms in Chinese patients with COVID‐19 was approximately 11.2%‐40.1%, which is slightly lower than that in United States (22.4%‐74.0%) and European countries (12.5%‐72.6%). One study reported that the incidence of diarrhea in 305 patients in Wuhan was 49.5%, whereas 29.4% and 15.9% patients, respectively, reported nausea and vomiting. 9 Moreover, about 16% patients manifest only GI symptoms. 10 In an American study of 164 cases approximately half reported one or more GI symptoms, which were more common among adolescents and hospitalized patients than non‐hospitalized adult individuals. 11 In this study, diarrhea was the most frequent (38%) GI symptom, and patients with three or more GI symptoms accounted for 10%, while these manifestations were the only clinical performance in four patients. Given the rapidly evolving nature of the COVID‐19 pandemic, the variants of SARS‐CoV‐2 are continuously changing and its GI characteristics are also dynamic, which partly explains the differences among studies. 12
TABLE 1.
Characteristics of included studies about COVID‐19 with gastrointestinal symptoms
| Manuscript type | Study period (2020) | Patients (n) | Age, y (mean ± SD or median [IQR]) | Male sex, % or n (%) | Patients with GI symptoms, n (%) | Diarrhea, % or n (%) | Time end‐point | Hospitalization, n (%) | ICU stay, n (%) | Death, % or n (%) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| First author (publication year) | Country or region | Nausea n (%) | Vomiting n (%) | Abdominal pain n (%) | Anorexia n (%) | Duration of GI symptoms (d) Mean ± SD or median (IQR) | Follow‐up (d) | |||||||||||
|
Papa 86 (2020) |
Italy | Case‐control | 15/3‐14/4 |
34* 71 # |
71 (64‐82)*, 74 (59.5‐81) # |
22*, 43 # |
3*, 44 # |
— | — | — | — | — | — | — | Discharge | Case‐control | 15/3‐14/4 |
34* 71 # |
|
Aghemo 87 (2020) |
Italy | Retrospective | 22/2/‐30/3 | 292 | 65 ± 14.1 | 199 (68.2) | 69/245 (28.2) | 69/255 (27.1) | — | 11/274 (4.0) | — | — | — | — | Discharge, death or to ICU | Retrospective | 22/2/‐30/3 | 292 |
|
Ahmad 88 (2021) |
Pakistan | Retrospective | 16/3‐14/4 | 194 | 34 (27‐48) | 157 (80.9) | 20 (10.31) | — | 8 (4.12) | — | — | 5 (2.58) | — | — | 2020‐4‐14 | Retrospective | 16/3‐14/4 | 194 |
| An 89 (2020) | China | Retrospective | 16/1‐30/3 | 205 | 54 (22‐77) | 122 (59.5) | 79 (38.5) | 20 (9.8) | 12 (5.9) | 6 (2.9) | 4 (2.0) | 59 (28.8) | — | — | Discharge | Retrospective | 16/1‐30/3 | 205 |
| Aumpan 90 (2020) | Thailand | Retrospective | 1/1‐30/4 |
40 (30 & ; 10 † ) |
30.5 ± 9.2 | 18 (45) | 12 (30) | 15 (2/30 & 4/10 † ) | 5 (0/30 & 2/10 † ) | 5 (1/30 & , 1/10 † ) | 17.5 (5/30 & ; 2/10 † ) | — | — | Discharge | Retrospective | 1/1‐30/4 |
40 (30 & ; 10 † ) |
|
|
Bishehsari 91 (2021) |
USA | Retrospective | 12/3‐3/4 | 921 |
47.6 (16.0) € 52.4 (17.1) ‡ |
409 (44.4) | 206 (22.4) | 144 (15.6) | 127 (13.8) | 52 (5.6) | — | — | — | — | Retrospective | 12/3‐3/4 | 921 | |
|
Burke 11 (2020) |
USA | Retrospective | 19/1‐3/6 | 164 | 50 | 56 | 97 (59) | 38 | — | 13 | — | — | — | — | — | Retrospective | 19/1‐3/6 | 164 |
|
Cao 92 (2020) |
China | Retrospective | — | 63 ‡ ; 94 € | 51.9 ± 14.9 ‡ , 47.5 ± 14.0 € | 24 (38.1) ‡ ; 50 (53.2) € | 63 (40.1) | 25/63 (39.7) | 21/63 (33.3) | — | — | 47/63 (74.6) | 10.7 ± 4.5 ‡ , 9.1 ± 5.2 € | 16.0 ± 4.9 | Discharge | Retrospective | — | 63 ‡ ; 94 € |
|
Carvalho‐Schneider 93 (2021) |
France | Retrospective | 17/3‐3/6 | 150 a ; 150 b ; 130 c | 49 ± 15 | 66 (44) | 48 (33.1) a 26 (17.3) b 15 (11.5) c |
5 (3.8) c |
— | — | — | — | — | 60 | — | Retrospective | 17/3‐3/6 | 150 a ; 150 b ; 130 c |
|
Chen 94 (2020) |
USA | Case‐control | 9/3‐15/4 |
101* 239 # |
48.3 ± 14.7*; 46.3 ± 15.6 # | 41 (41)*; 55 (23) # |
75 (74)*; 126 (53) # |
51 (50)*; 72 (30) # |
30 (30)*; 62 (26) # |
14 (14)*; 29 (12) # | 26 (26)*; 46 (19) # | 54 (53)*; 63 (26) # | — |
4 (4)*; 4 (5) # |
Prevalence of GI symptoms | Case‐control | 9/3‐15/4 |
101* 239 # |
|
Chen 95 (2020) |
China | Retrospective | 25/1‐21/3 | 1077 | 59.0 (47.0‐68.0) | 550 (49.4) | 359 (33.3) | 208 (57.9) | 71 (19.8) | 38 (10.6) | — | — | — | Discharge | Retrospective | 25/1‐21/3 | 1077 | |
|
Chen 18 (2020) |
China | Retrospective | 20/1‐9/2 | 42 | 51 (42.8‐62) | 15 (35.7) | 8 (19.1) | 7 (16.7) | 4 (9.5) | 3 (7.1) | 5 (11.9) | — | — | — | Discharge | Retrospective | 20/1‐9/2 | 42 |
|
Cholankeril 96 (2020) |
USA | Retrospective | 9/3‐7/4 | 207 | 49 (34‐65) | 104 (50.2) | 70 (34.5) | 22 (10.8) | — | — | 14 (7.1) | — | 1 (0‐4) | — | At presentation | Retrospective | 9/3‐7/4 | 207 |
|
Deng 97 (2020) |
China | Retrospective | 24/1‐10/3 | 61 d | 54.8 (12.9) | 25 (41) | — | 3 (4.9) | — | — | — | — | — | 10 (7‐13) | — | Retrospective | 24/1‐10/3 | 61 d |
|
Duque 98 (2021) |
Portugal | Retrospective | Before 1/4 | 2031 | 50 ± 19.8 | 973 (47) | — | 290 (14.3) | 202 (10) | 134 (6.6) | — | — | — | — | Retrospective | Before 1/4 | 2031 | |
|
Elmunzer 99 (2020) |
North America | Retrospective | 15/4‐5/6 | 1992 | 51 (41‐68) | 1128 (56.6) | 1052 (53) | 34 | 27 | 16 | 11 | — | — | — | June 5, 2020 | Retrospective | 15/4‐5/6 | 1992 |
|
Fallouh 100 (2021) |
USA | Retrospective | 24/2‐21/5 | 382 | 62.2 ± 16.8 | 203 (53.1) | 202 (52.9) | 28.8 | 22 | 17 | 11.8 | 24.9 | — | — | — | Retrospective | 24/2‐21/5 | 382 |
| Ferm 101 (2020) | USA | Retrospective | 14/3‐1/4 | 892 | 59 (47‐72) | 534 (59.9) | 219 (24.6) | 177 (19.8) | 148 (16.6) | 91 (10.2) | 70 (7.8) | 105 (11.8) | 4 (3‐7) | — | April 1, 2020 | Retrospective | 14/3‐1/4 | 892 |
|
Graham 102 (2021) |
UK | Retrospective | 23/2‐23/4 | 478 | 70 (23) | 279 (58.4) | 161 (33.7) | 17.4 | 7.5 | 13 | 7.3 | 13.8 | — | — | — | Retrospective | 23/2‐23/4 | 478 |
|
Greco 103 (2021) |
Italy | Retrospective | Mar‐Jul | 495 | 70 ± 17 | 23 (37.1) | 62 (12.5) | — | — | — | — | — | — | — | 100 days | Retrospective | Mar‐Jul | 495 |
|
Guerra 104 (2020) |
Spain | Cross‐sectional | 24/4‐27/5 | 82 e | 46 ± 14 | 38 (46.3) | — | 35 (42.7) | — | — | 12 (14.6) | — | — | — | May 27, 2020 | Cross‐sectional | 24/4‐27/5 | 82 e |
|
Kim 105 (2021) |
Korea | Retrospective | 19/2‐30/4 | 5253 | — |
1796 (40.4) & 380 (47.0)† |
— |
375 (8.4) & 87 (10.8) † |
178(4.0) & 62 (7.7) † |
— | — | — | — | — | Retrospective | 19/2‐30/4 | 5253 | |
|
Lapostolle 17 (2020) |
France | Prospective |
24/3‐6/4 |
1487 | 44 (32‐57) | 700 (47) | — | 352 (23.7) | 288 (19.4) | 168 (11.3) | — | 305 (20.5) | — | 0.5 | 48h | Prospective |
24/3‐6/4 |
1487 |
|
Laszkowska 106 (2020) |
USA | Retrospective | 11/3‐28/4 | 2804 | 63.4 ± 18.4 | 1565 (56) | 1084 (38.7) | 657 (23.4) | 648 (23.2) | — | 334 (11.9) | — | 13.8 | — | Discharge | Retrospective | 11/3‐28/4 | 2804 |
|
Leal 107 (2021) |
Portugal | Retrospective | Mar‐Apr | 201 | 71 (26) | 113 (56.2) | 60 (29.9) | 36 (17.9) | 14 (7) | 22 (10.9) | 10 (5) | 60 (29.9) | 9 (12) | — | — | Retrospective | Mar‐Apr | 201 |
|
Luo 10 (2021) |
China | Retrospective | 10/1‐29/2 |
183 f ; 1228 g |
53.8 f ; 56.2 g |
55.7 f ; 64.5 g | — | 68 (37.1) f | 134 (73.2) f | 119 (65.0) f | 65 (35.5) f | 180 (98.3) f | — | — | — | Retrospective | 10/1‐29/2 |
183 f ; 1228 g |
|
Mario 108 (2020) |
Spain | Retrospective‐prospective | 11/3‐21/4 | 76 | 45.8 ± 11.4 | 23 (30.3) | 45 (59.2) | 31 (40.8) | 17 (22.4) | 7 (9.2) | 21 (27.6) | 12 (15.8) | — | Up to 2020/04/21 | First negative PCR | Retrospective‐prospective | 11/3‐21/4 | 76 |
|
Martin 46 (2020) |
USA | Case‐control | 4‐23/4 |
41 h 82 i |
68.7 ± 15.1 h , 67.6 ± 14.3 i | 27 (66) h , 54 (66) i | — | 11 (27) h , 27 (33) i | — | — |
1 (2) h 8 (10) i |
7 (17) h 26 (32) i |
— | — | Discharge | Case‐control | 4‐23/4 |
41 h 82 i |
|
Mokarram 109 (2021) |
Italy | Retrospective | Mar‐Sept | 91 | 51 | 56 (51) | — | 29 (31.8) | 39 (42.8) | 24 (26.3) | 11 (12) | 40 (43.9) | — | — | — | Retrospective | Mar‐Sept | 91 |
|
O'Keefe 110 (2021) |
USA | Retrospective | 24/3‐26/5 | 337 (223 & ; 106 ¶ ; 8 † ) | 45.7 (44.1‐47.2) | 108 (32) | — |
62 (28) & 48 (45) ¶ 2 (25) † |
32 (15) & |
— |
27 (12) & 25 (24) ¶ 1 (13) † |
— |
6 (5‐8) j |
30 | — | Retrospective | 24/3‐26/5 | 337 (223 & ; 106 ¶ ; 8 † ) |
|
Park 111 (2020) |
Korea | Prospective | 4‐24/4 | 46 & | 26 (18‐57) | 21 (45.6) | 16 (34.7) | 7 (15.2) | 1 (2.1) | 0 | 5 (10.8) | 5 (10.8) | — | 52 (39‐61) | 2020/4/24 | Prospective | 4‐24/4 | 46 & |
|
Ramachandran 112 (2020) |
USA | Case‐control | 18‐31/3 |
31 ‡ 119 € |
57.6 ± 17.2 ‡ , 63.3 ± 14.6 € |
19 (62.3) ‡ 64 (53.8) € |
— | 15 (48.4) ‡ | — | — | — | — | — | — | Discharge | Case‐control | 18‐31/3 |
31 ‡ 119 € |
|
Remes‐Troche 113 (2020) |
Mexico | Retrospective | 1/4‐5/5 | 112 | 43.72 ± 15 | 81 (72.3) | 23 (20.5) | 20 (17.8) | — | 8 (7.1) | 11 (9.8) | — | — | — | May 5, 2020 | Retrospective | 1/4‐5/5 | 112 |
|
Renelus 114 (2020) |
USA | Retrospective | 10/3‐13/4 | 734 | 66.1 ± 15.6 | 379 (51.6) | 231 (31.5) | 149 (20.3) | 109 (14.9) | 62 (8.5) | 68 (9.3) | — | — | 30/4 2020 | Retrospective | 10/3‐13/4 | 734 | |
|
Saeed 115 (2020) |
Norway | Retrospective | 17/3‐1/4 | 76 (9*) | 48 (31‐81) | — | 76 (100) | 1 (11.1)* | 8 (88.9)* | 5 (55.6)* | 76 (100) | — | — | 14.1 | — | Retrospective | 17/3‐1/4 | 76 (9*) |
|
Schettino 116 (2020) |
Italy | Prospective cohort | 23/3‐5/4 | 190 | 64.6 ± 15.4 | 127 (66.8) | 138 (72.6) | 72 (37.9) | 32 (20) | 19 (10) | 6 (3.1) | 97 (51) | — | — | Discharge or death | Prospective cohort | 23/3‐5/4 | 190 |
|
Shang 13 (2020) |
China | Retrospective | 20/1‐29/2 | 157 j | 59 (43‐67) | 75 (47.8) | — | 157 (100) | 42 (26.8) | 32 (10.4) | 8 (5.1) | — | 4.5±1.6 | — | Discharge | Retrospective | 20/1‐29/2 | 157 j |
|
Sierpinski 117 (2020) |
Poland | Cross‐sectional | 17‐18/4 | 1942 | 50 | 773 (39.8) | 53.60 | 470 (24.2) | — | — | — | 912 (47) | — | — | — | Cross‐sectional | 17‐18/4 | 1942 |
| Sulaiman 118 (2020) | Iraq | Retrospective | 2/3‐1/5 | 140 | 45.0 ± 16.8 | 100 (71.4) |
78 (55.7) 33 (23.6) f |
41 (29.3) | — | 31 (22.1) | 42 (30) | 40 (28.6) | — | — | Discharge | Retrospective | 2/3‐1/5 | 140 |
|
Sun 119 (2021) |
China | Retrospective | 20/2‐31/3 | 932 (880 & , ¶ ; 52 † ) | 58 (48‐67) | 375 (40.2) | — | 73 (8.3) & , ¶ , 7 (13.5) † | 31 (3.5) & , ¶ ; 1 (1.9) † | — | 178 (20.2) & , ¶ ; 25 (48.1) † | 5 (4‐12) | 90 | — | Retrospective | 20/2‐31/3 | 932 (880 & , ¶ ; 52 † ) | |
| Taziki Balajelini 120 (2021) | Iran | Retrospective | Feb‐Jul | 599 | 38.3 ± 13.6 | 286 (47.8) | 251 (41.9) | 151 (25.2) | 123 (20.5) | 77 (12.9) | 159 (26.5) | — | — | — | — | Retrospective | Feb‐Jul | 599 |
|
Tsibouris 121 (2020) |
Greece | Retrospective | 6/4‐6/5 | 61 | 70 (55‐83) | 34 (55.7) | — | 11/61 | 4/61 | 2/61 | — | — | — | May 6, 2020 | Retrospective | 6/4‐6/5 | 61 | |
|
Xiao 122 (2020) |
China | Descriptive |
10/1‐17/2 |
90 | 61.0 (48.3‐69.0) | 51 (57) | — | 90 (100) | 22 (24) | 15 (17) | 6 (7) | 22 (24) | 5 (2.0‐9.3) | — | Discharge | Descriptive |
10/1‐17/2 |
90 |
|
Xu 123 (2020) |
China | Retrospective | 26/1‐20/3 | 48 | 41 (18‐90) | 25 (52.1) | 12 (25) | 3 | 1 | — | — | 3 | — | — | — | Retrospective | 26/1‐20/3 | 48 |
|
Yang 124 (2020) |
China | Retrospective | 2‐13/2 | 50 (23 ‡ ; 27 g ) |
44.6 ± 2.8 ‡ 42.5 ± 3.3 g |
13 (56.5) ‡ 15 (55.6) g |
23 (100) ‡ | — | — | — | — | — | 12.13 ± 2.44 ‡ | — | Discharge | Retrospective | 2‐13/2 | 50 (23 ‡ ; 27 g ) |
| Yoshida 125 (2020) | USA | Retrospective | 27/2‐5/7 | 776 | 60.5 (16.1) | 365 (47.3) | 269 (36.6) | 187 (25.4) | 154 (21) | 65 (8.8) | — | — | — | — | Retrospective | 27/2‐5/7 | 776 | |
|
Zhang 126 (2020) |
China | Retrospective | — | 505 | 51.2±17.2 | 228 (45.1) | 164 (32.5) | 62/164 | 27/164 | 13/164 | 17/164 | 93/164 | — | — | — | Retrospective | — | 505 |
|
Zhang 69 (2020) |
China | Retrospective | 20/1‐29/2 | 409 (307 m ; 102 n ) | 65 (range 28‐87) |
162 (52.8) m 72(70.6) n |
— | 61 (19.9) m , 30 (29.4) n | 38 (12.4) m , 12 (11.8) n | 33 (12.4) m , deceased: 9 (8.8) n | 23 (7.5) m , 5 (4.9) | — | 4.2 ± 1.5 m , 4.9 ± 1.5 n | — | Discharge or death | Retrospective | 20/1‐29/2 | 409 (307 m ; 102 n ) |
|
Zhang 3 (2020) |
China | Retrospective | 17/1‐12/2 | 788 (52 & ; 658 ¶ ; 61 † ; 17**) |
37.5 (19.3‐45.8) & 45.0 (35.0‐55.0) ¶ 55.0 (44.0‐62.0) † , 70.0 (55.0‐73.0)** |
26 (50.0) & 329 (50.0) ¶ 39(63.9) † 13(76.5)** |
7(13.5) & , 63(9.6) ¶ , 12(19.7) † , 6(35.3)** | — | — | — | — | — | — | — | Discharge | Retrospective | 17/1‐12/2 | 788 (52 & ; 658 ¶ ; 61 † ; 17**) |
|
Zheng 127 (2020) |
China | Retrospective | 5/1‐9/3 | 1320 (192 ‡ ; 1128 € ) |
50 (38‐56) ‡ 51 (41‐58) € |
90(46.9) ‡ 489(43.4) € |
192 (100) ‡ 0 € |
107 (55.7) ‡ | — | — | 11 (5.7) ‡ | 62 (32.3) ‡ | — | — | Discharge | Retrospective | 5/1‐9/3 | 1320 (192 ‡ ; 1128 € ) |
| Zhu 128 (2020) | China | Retrospective | Before Feb 4, | 90 d | 52 (37.8‐59) | 32 (32.7) | — | 8 (8.2) d | — | — | — | — | — | 14 | 2 weeks | Retrospective | Before Feb 4, | 90 d |
COVID‐19 cases group.
Control group without COVID‐19.
Mild COVID‐19.
Moderate COVID‐19.
Severe COVID‐19.
Critical COVID‐19.
COVID‐19 with GI symptoms.
COVID‐19 without GI symptoms.
Initial onset of COVID‐19.
30 days after initial onset of COVID‐19.
60 days after initial onset of COVID‐19.
COVID‐19 patients in recovery stage.
COVID‐19 with inflammatory bowel disease.
COVID‐19 patients with GI symptom only.
COVID‐19 patients with respiratory symptom.
COVID‐19 patients with GIB.
COVID‐19 patients without GIB.
COVID‐19 patients with diarrhea.
COVID‐19 patients with nausea.
COVID‐19 patients with abdominal pain.
Survived COVID‐19 patients.
Deteriorated COVID‐19 patients.
Abbreviations: —, not available; GI, gastrointestinal; GIB, gastrointestinal bleeding; ICU, intensive care unit.
3. GI MANIFESTATIONS AND POTENTIAL MECHANISMS IN COVID‐19 AT DIFFERENT STAGES
GI symptoms can occur at any stage of COVID‐19, not only as the initial symptoms, but may emerge during the entire course of the disease as well. However, GI performance may differ during different disease stages.
3.1. GI symptoms at disease onset
Time length from the onset of the disease to the appearance of GI symptoms in COVID‐19 varies among studies. In some patients GI symptoms appear initially prior to or even without respiratory symptoms or fever, although in most patients GI manifestations occur within 3‐10 days of illness. 13 Most patients present with diarrhea, nausea, and vomiting, either alone or simultaneously. Diarrhea and loss of appetite are the two most common symptoms and may be related to the severity of the disease. 14 , 15 , 16 The proportion of patients with COVID‐19 having diarrhea has been reported to be 3.7%‐12.4%. 17 , 18 Most patients had mild symptoms that last for 1‐7 days, such as watery yellow stool without mucus, pus or blood, often in the absence of obvious dehydration. Stool routine test is usually normal. 19 , 20 , 21 Clinicians should be alerted when diarrhea occurs so as to diagnose COVID‐19 at an early stage and to control possible fecal–oral transmission. Diarrhea may also serve as an indicator of poor prognosis in these patients due to their increased risks of secondary infection and multisystem involvement. 14 , 15 , 22 , 23 In addition, almost half these patients have taste disorder as a coexisting or sole clinical manifestation. 24 , 25 The possible mechanism may be that angiotensin converting enzyme 2 (ACE2), one of the receptors for SARS‐CoV‐2, distributes in not only pulmonary alveolar cells but also GI epithelial cells, including oral mucosa. 26 , 27 The spike protein on the surface of SARS‐CoV‐2 may directly damage GI epithelial cells by binding to ACE2, causing loss of the normal function of ACE2, leading to disturbed intestinal amino acid metabolism and gut dysbiosis, and eventually induces intestinal inflammation and immune disorders. 23 , 28
Although abdominal pain in COVID‐19 is relatively rare, it must always be carefully differentiated from acute abdominal diseases, especially when it is not accompanied by any other manifestation except for GI symptoms. Several COVID‐19 cases have been reported to experience abdominal pain of different degree at disease onset, either diffuse or limited, with or without diarrhea and vomiting. 29 , 30 , 31 Some of the patients present with abdominal tenderness and tension, although there are no signs of peritonitis or appendicitis on their abdominal computed tomography (CT) scan. A real‐time reverse transcriptase‐polymerase chain reaction (RT‐PCR) for SARS‐CoV‐2 nucleic acid detection may sometimes be negative, and does not always conform to the patient's clinical manifestations. Therefore, there is a need for repeated SARS‐CoV‐2 nucleic acid detections or to make diagnosis until respiratory symptoms and/or characteristic chest CT scan features appear. 18 , 32
Viral infections usually lead to a prodrome of non‐specific GI symptoms, which makes the diagnosis of GI involvement in COVID‐19 challenging at the early stage. However, given its acute and severe onset, the prodromal symptoms are usually mild. 33 In such cases, an epidemiological investigation needs to be considered. For those who are suspected to have COVID‐19, SARS‐CoV‐2 testing and radiological examination are urgently needed. A SARS‐CoV‐2 fecal test may help differentiate the prodrome and GI involvement as well. In terms of their duration and severity, prodromal symptoms tend to be transient and self‐limiting, while in most COVID‐19 cases GI symptoms persist for about 10 days and may be aggravated with respiratory deterioration. Moreover, other factors such as the patient's prior or current medication and history of GI comorbidities should not be neglected. Microbial agents may affect the gut immune response and gut microbiota and in turn the clearance of the virus from the gut. 34 Therefore, the American Gastroenterological Association Institute has suggested that for patients with COVID‐19 who are under medication, treatment‐related adverse GI effects should be considered and evaluated. 35
3.2. GI symptoms at disease progression
The appearance and aggravation of GI symptoms can be used to indicate disease progression. GI symptoms are more commonly seen in severe and critically ill patients compared with those with mild disease, and is related to an increased risk of adverse outcomes (odds ratio [OR] 1.9, P = 0.047). 3 , 19 In addition to non‐specific GI symptoms, COVID‐19 mainly leads to a variety of GI‐related complications during disease progression, including dysfuction of digestion and absorption, GI motility disorder, acute intestinal ischemia, GI bleeding, Clostridium difficile (C. difficile) infection and pancreatic injury.
Dysfunction of digestion and absorption, which mainly manifests as intolerance of enteral nutrition and worsening of diarrhea, results in the lack of nutrients and malnutrition, thus a deterioration of the overall condition. Nutrition plays a vital role in the recovery process of these patients. Monitoring of stool weight can be used to assess the nutritional status of patients with severe disease, which can also be regarded as an indicator for their tolerance to enteral nutrition. 36
Half of the critically ill patients are reported to have severe GI motility disorder. 37 Gastric retention is common, as enteral nutrition is usually given to these patients through a nasogastric tube. Some patients have typical manifestations of intestinal obstruction that may develop into intestinal necrosis and require emergency surgery. Local or extensive ischemia may be related to factors such as small intestinal vascular thrombosis, enteric nerve dysfunction caused by viral infection, and systemic metabolic and acid‐base imbalance. 38
Many studies have reported that patients with COVID‐19 may have acute abdominal pain and bloody stool that might conform to the diagnosis of ischemic bowel disease. One report 39 confirmed the presence of non‐occlusive mesenteric ischemia on abdominal CT scan in these patients. This can further be confirmed histopathologically when the necrotic bowel has to be surgically removed. 40 , 41 COVID‐19‐related hypercoagulability status has been confirmed to be associated with a poor prognosis. 42 , 43 Based on this hypercoagulable tendency coupled with the induction of systemic inflammatory response and cytokine storm, disease progression is often difficult to control and almost always related to death.
GI bleeding can also be observed in patients with COVID‐19, with a prevalence of approximately 3.04%. 44 , 45 The common reasons include peptic ulcer, esophagitis and rectal ulcer. 46 Possible mechanisms include GI mucosal damage caused by viral invasion, long‐term hypoxemia, and multiorgan failure with coagulation disorders. In addition, use of glucocorticoids, oral nonsteroidal anti‐inflammatory drugs or anticoagulants, which are usually used to treat comorbidities, can cause GI bleeding as well. 47
Destruction of the intestinal mucosal barrier by SARS‐CoV‐2 increases the risk of co‐infection with other pathogens. There are few reports of positive bacterial culture in fecal sample of patients with COVID‐19, but most hospitals use antibiotics empirically to lower a possibility of gut‐derived bacteremia. However, due to the widespread use of antibiotics, the incidence of C. difficile infection has been gradually increasing. Data from the Detroit Medical Center in the United States 22 shows that from March to April 2020 the incidence of C. difficile infection is 3.6/10 000 patient‐days, which is higher than that during January and February (3.32/10 000 patient‐days). C. difficile infection can appear at the same time as respiratory symptoms present or within 1 week after COVID‐19 is diagnosed. Patients with C. difficile infection are more severely ill and have a higher mortality rate compared with those without C. difficile infection. Similarly, COVID‐19 patients can infect with cytomegalovirus, which is thought to be related to the function of T lymphocytes and elevated interleukin (IL)‐6 levels. 48 , 49
Pancreatic involvement has been reported in some patients with COVID‐19, including pancreatic enzyme changes, acute pancreatitis and subsequent metabolic disorders. 50 , 51 , 52 One systematic review 53 revealed that 11.7% of patients presented with hyperlipasemia, ranging from an upper limit of around 50‐60 U/L to a lipase level of over 300 U/L. Unlike the obvious pancreatic impairment in acute pancreatitis, hyperlipasemia in patients with COVID‐19 may be occult with unclear etiology. However, hyperlipasemia may be used to recognize disease progression at the early stage and serum lipase levels may be a marker of disease severity. High serum lipase levels usually predict pancreatic damage and are significantly associated with an increased need for intensive care unit (ICU) admission. 54 , 55 The potential mechanisms may include a high ACE2 expression in the pancreas, which suggests that SARS‐CoV‐2 can also attack the pancreas, leading to direct pancreatic injury and inflammatory response. 53 , 56 Additionally, secondary damage from systematic cytokine storm and drug‐related pancreatic injury may be involved as well. 57 , 58
Other GI complications in COVID‐19, such as bowel obstruction or perforation, have been rarely reported. Possible causes may be direct bowel damage by SARS‐CoV‐2 infection, and local ischemia or necrosis due to the inflammatory response and hypercoagulable state. 59 , 60
Compared with patients with severe disease, critically ill patients with COVID‐19 are at an increased risk of serious complications. 61 GI dysfunction is closely related to poor prognosis. 62 , 63 The potential mechanism mainly involves direct viral invasion through ACE2 and the aggravation of systemic inflammation. The involvement of the digestive system is most likely due to ACE2 in the GI tract. One study 64 has revealed that plasma ACE2 activity is elevated in patients after COVID‐19 infection and is associated with its severe form. During disease progression, GI damage caused by lung injury and systematic inflammation play a dominant role. The gut–lung axis may impair pulmonary and GI functions through microbial metabolites and an abnormal immune response. Levels of lung‐derived abnormal cytokines and T cells are elevated after a viral infection, which promotes interaction with receptors in the GI tract and activates intense responses in the gut, leading to intestinal immune damage and disturbance of intestinal flora. 65 In return, bacterial imbalance and inflammatory molecules from the gut can act on the pulmonary alveolar cells through the bloodstream, further aggravating the inflammation. 66 , 67 Several studies have found that levels of inflammatory indicators generally arise at 1‐2 weeks after the disease onset and gradually increase along with disease progression. 68 , 69 Patients with diarrhea have much higher peripheral levels of IL‐6, IL‐10 and tumor necrosis factor (TNF)‐α than those without diarrhea. 69
3.3. GI symptoms at treatment intervention and remission
The main therapeutic interventions for COVID‐19 are symptomatic support, and antiviral and anti‐inflammatory therapies. Non‐specific GI symptoms such as diarrhea and abdominal pain in patients with mild disease are often self‐limiting. 5 , 19 In the remission stage, symptoms and levels of inflammatory indicators may gradually improve within a few days, but the detection of viral nucleic acid by real‐time RT‐PCR may remain positive until up to 1 month after the disappearance of symptoms. The fecal nucleic acid detection of SARS‐CoV‐2 may convert to negative results later than that of a nasopharyngeal swab, perhaps owing to the aggregation and colonization of the virus in the GI tract. 30 , 70 Early administration of enteric nutrition, use of glucocorticoids and human γ‐globulin can be considered for severe and critically ill patients. 71 , 72 Recent evidence suggests that glucocorticoids can reduce IL‐6 levels by activating ACE2 and counteract the systemic inflammatory response to reduce lung injury in patients with severe COVID‐19. 73 , 74 However, whether use of glucocorticoids can improve GI function needs further investigation. Other treatments such as interferon, lopinavir and ritonavir, antibacterial drugs and intestinal microecological modulators have been widely used in clinical practice, without evidence from rigorous large‐scale clinical trials. 75 Specific antibodies are not produced after recovery from COVID‐19. Four weeks after their discharge, 15.4% of the patients were negative for SARS‐CoV‐2 immunoglobulin G (IgG) and IgM antibodies, while one case has been reinfected in the convalescent phase. 76
4. IMPACTS OF COVID‐19 ON PATIENTS WITH DIGESTIVE COMORBIDITIES
Of COVID‐19 cases with pre‐existing chronic GI disorders, cancer and inflammatory bowel disease (IBD) are the most commonly studied. Several studies have indicated that compared with those without GI malignancies, patients with GI malignancies are more susceptible to COVID‐19 and were more likely to manifest in a severe form, which may result from higher expressions of ACE2 and TMPRSS2. 77 , 78 Although patients with IBD seem to have no increased risk of contracting COVID‐19, medications for IBD may affect the disease course. Roy et al have reported that ulcerative colitis and the use of 5‐aminosalicylates are related to an increased mortality in COVID‐19.79 Anti‐TNF therapy may attenuate serological responses to a SARS‐CoV‐2 vaccination. 80
Endoscopic assessment is generally performed for the diagnosis and treatment in patients with GI symptoms. Unfortunately, during the COVID‐19 pandemic the performance of endoscopic procedures has been restricted and delayed because of the excess burden on respiratory function and an increased risk of viral transmission during the procedures. 81 To resolve this dilemma, the need for endoscopic procedure should be fully evaluated and a risk stratification of GI disease and COVID‐19 should be performed. 82 , 83 For example, it is inevitable that patients with acute or recurrent persistent GI bleeding shall undergo endoscopy. Thus, intra‐ or post‐procedure risk management should be further implemented as the statement of the European Society of Gastrointestinal Endoscopy and the European Society of Gastroenterology and Endoscopy Nurses and Associates. 82 Moreover, some invasive procedures can be considered as a safe alterative for disease screening to minimize the unnecessary exposure to SARS‐CoV‐2 caused by fecal and radiological tests or capsule endoscopy in both patients and healthcare staff. 84 , 85
5. SUMMARY
GI manifestations can be used as an auxiliary index to assess disease severity and predict patient outcome in COVID‐19, in combination with other vital signs and supplementary examinations. There are, however, limitations about the relationship between GI manifestations and COVID‐19. There are no strict standards to detect these manifestations and it is sometimes difficult to distinguish GI manifestations at different stages of the disease because of specific individual conditions and an overlapping nature of the symptoms. Different GI symptoms are valuable in offering some clues to assess the severity of COVID‐19. The combination of GI manifestations with pulmonary or systematic conditions is extremely essential for the assessment of COVID‐19 severity. Besides, as the lack of strong specificity, many potential factors are required to be summarized as well, including GI comorbidities, medications, mental status, and functional GI diseases. The long‐term impact of COVID‐19 on the GI tract needs to be evaluated during the follow‐up period. Further studies are needed to thoroughly identify the role of GI manifestations in the pathogenesis or progression of COVID‐19 and to treat patients with COVID‐19 in this worldwide pandemic.
CONFLICT OF INTEREST
The authors have no conflict of interest.
ACKNOWLEDGMENTS
This study was supported by the National Natural Science Foundation of China (81570505 and 81970495), Health Research & Special Projects Grant of China (201002020 and 201502005), Natural Science Foundation of Beijing, China (7202161), and CAMS Innovation Fund for Medical Sciences (2016‐I2M‐3‐001 and 2019‐I2M‐2‐007).
Zhang MM, Chen LN, Qian JM. Gastrointestinal manifestations and possible mechanisms of COVID‐19 in different periods. J Dig Dis. 2021;22(12):683-694. doi: 10.1111/1751-2980.13065
Funding information CAMS Innovation Fund for Medical Sciences, Grant/Award Numbers: 2016‐I2M‐3‐001, 2019‐I2M‐2‐007; Health Research & Special Projects Grant of China, Grant/Award Numbers: 201002020, 201502005; National Natural Science Foundation of China, Grant/Award Numbers: 81570505, 81970495; Natural Science Foundation of Beijing, China, Grant/Award Number: 7202161
REFERENCES
- 1. Johnson KD, Harris C, Cain JK, Hummer C, Goyal H, Perisetti A. Pulmonary and extra‐pulmonary clinical manifestations of COVID‐19. Front Med (Lausanne). 2020;7:526. 10.3389/fmed.2020.00526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Luo S, Deng Z, Zhang X, Pan Z, Xu H. Clinical characteristics and outcomes of 2019 novel coronavirus disease patients presenting with initial gastrointestinal symptoms in Wuhan, China: a retrospective cohort study. J Gastroenterol Hepatol. 2021;36(3):694‐699. [DOI] [PubMed] [Google Scholar]
- 3. Zhang SY, Lian JS, Hu JH, et al. Clinical characteristics of different subtypes and risk factors for the severity of illness in patients with COVID‐19 in Zhejiang, China. Infect Dis Poverty. 2020;9(1):85. 10.1186/s40249-020-00710-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Zhang JJ, Dong X, Cao YY, et al. Clinical characteristics of 140 patients infected with SARS‐CoV‐2 in Wuhan, China. Allergy. 2020;75(7):1730‐1741. [DOI] [PubMed] [Google Scholar]
- 5. Chen L, Jiang L, Gong JY. Two cases of family clustered novel coronavirus pneumonia with abdominal pain as the first symptom. J Shanxi Med Univ. 2020;51(5):470‐472. [in Chinese]. [Google Scholar]
- 6. Jiao L, Li H, Xu J, et al. The gastrointestinal tract is an alternative route for SARS‐CoV‐2 infection in a nonhuman primate model. Gastroenterology. 2020;160(5):1647‐1661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Mao R, Qiu Y, He JS, et al. Manifestations and prognosis of gastrointestinal and liver involvement in patients with COVID‐19: a systematic review and meta‐analysis. Lancet Gastroenterol Hepatol. 2020;5(7):667‐678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Tariq R, Saha S, Furqan F, Hassett L, Pardi D, Khanna S. Prevalence and mortality of COVID‐19 patients with gastrointestinal symptoms: a systematic review and meta‐analysis. Mayo Clin Proc. 2020;95(8):1632‐1648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Fang D, Ma JD, Guan JL, et al. Manifestations of digestive system of hospitalized patients with coronavirus disease 2019 in Wuhan, China: a single‐center descriptive study. Chin J Dig. 2020;40(3):151‐156. [in Chinese]. [Google Scholar]
- 10. Luo S, Zhang X, Xu H. Don't overlook digestive symptoms in patients with 2019 novel coronavirus disease (COVID‐19). Clin Gastroenterol Hepatol. 2020;18(7):1636‐1637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Burke RM, Killerby ME, Newton S, et al; Case Investigation Form Working Group. Symptom profiles of a convenience sample of patients with COVID‐19 — United States, January–April 2020. MMWR Morb Mortal Wkly Rep. 2020;69(28):904‐908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Kurtz P, Bastos LSL, Dantas LF, et al. Evolving changes in mortality of 13,301 critically ill adult patients with COVID‐19 over 8 months. Intensive Care Med. 2021;47(5):538‐548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Shang H, Bai T, Chen Y, et al. Outcomes and implications of diarrhea in patients with SARS‐CoV‐2 infection. Scand J Gastroenterol. 2020;55(9):1049‐1056. [DOI] [PubMed] [Google Scholar]
- 14. Choi MH, Ahn H, Ryu HS, et al. Clinical characteristics and disease progression in early‐stage COVID‐19 patients in South Korea. J Clin Med. 2020;9(6):1959. 10.3390/jcm9061959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Wang B, Wang Z, Zhao J, et al. Epidemiological and clinical course of 483 patients with COVID‐19 in Wuhan, China: a single‐center, retrospective study from the mobile cabin hospital. Eur J Clin Microbiol Infect Dis. 2020;39(12):2309‐2315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Wang F, Qu M, Zhou X, et al. The timeline and risk factors of clinical progression of COVID‐19 in Shenzhen, China. J Transl Med. 2020;18(1):270. 10.1186/s12967-020-02423-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Lapostolle F, Schneider E, Vianu I, et al. Clinical features of 1487 COVID‐19 patients with outpatient management in the Greater Paris: the COVID‐call study. Intern Emerg Med. 2020;15(5):813‐817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Chen Y, Chen L, Deng Q, et al. The presence of SARS‐CoV‐2 RNA in the feces of COVID‐19 patients. J Med Virol. 2020;92(7):833‐840. [DOI] [PubMed] [Google Scholar]
- 19. Jin X, Lian JS, Hu JH, et al. Epidemiological, clinical and virological characteristics of 74 cases of coronavirus‐infected disease 2019 (COVID‐19) with gastrointestinal symptoms. Gut. 2020;69(6):1002‐1009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Chen J, Liu J. Analysis of clinical characteristics of elderly patients with novel coronavirus pneumonia with digestive symptoms as the initial clinical manifestations. J Clin Intern Med. 2020;37(3):240‐241. [in Chinese]. [Google Scholar]
- 21. Pan L, Mu M, Yang P, et al. Clinical characteristics of COVID‐19 patients with digestive symptoms in Hubei, China: a descriptive, cross‐sectional, multicenter study. Am J Gastroenterol. 2020;115(5):766‐773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Sandhu A, Tillotson G, Polistico J, et al. Clostridioides difficile in COVID‐19 patients, Detroit, Michigan, USA, March–April 2020. Emerg Infect Dis. 2020;26(9):2272‐2274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Zuo T, Zhang F, Lui GCY, et al. Alterations in gut microbiota of patients with COVID‐19 during time of hospitalization. Gastroenterology. 2020;159(3):944‐955.e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Aziz M, Perisetti A, Lee‐Smith WM, Gajendran M, Bansal P, Goyal H. Taste changes (dysgeusia) in COVID‐19: a systematic review and meta‐analysis. Gastroenterology. 2020;159(3):1132‐1133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Sudre CH, Keshet A, Graham MS, et al. Anosmia, ageusia, and other COVID‐19‐like symptoms in association with a positive SARS‐CoV‐2 test, across six national digital surveillance platforms: an observational study. Lancet Digit Health. 2021;3(9):e577‐e586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Zhang H, Li HB, Lyu JR, et al. Specific ACE2 expression in small intestinal enterocytes may cause gastrointestinal symptoms and injury after 2019‐nCoV infection. Int J Infect Dis. 2020;96:19‐24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Eshraghi AA, Mirsaeidi M, Davies C, Telischi FF, Chaudhari N, Mittal R. Potential mechanisms for COVID‐19 induced anosmia and dysgeusia. Front Physiol. 2020;11:1039. 10.3389/fphys.2020.01039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Hashimoto T, Perlot T, Rehman A, et al. ACE2 links amino acid malnutrition to microbial ecology and intestinal inflammation. Nature. 2012;487(7408):477‐481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Ahmed AOE, Mohamed SF, Saleh AO, Al‐Shokri SD, Ahmed K, Mohamed MFH. Acute abdomen‐like‐presentation associated with SARS‐CoV‐2 infection. IDCases. 2020;21:e00895. 10.1016/j.idcr.2020.e00895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Ahmed AOE, Badawi M, Ahmed K, Mohamed MFH. Case report: COVID‐19 masquerading as an acute surgical abdomen. Am J Trop Med Hyg. 2020;103(2):841‐843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Cabrero‐Hernandez M, Garcia‐Salido A, Leoz‐Gordillo I, et al. Severe SARS‐CoV‐2 infection in children with suspected acute abdomen: a case series from a tertiary hospital in Spain. Pediatr Infect Dis J. 2020;39(8):e195‐e198. [DOI] [PubMed] [Google Scholar]
- 32. Lv DF, Ying QM, Weng YS, et al. Dynamic change process of target genes by RT‐PCR testing of SARS‐Cov‐2 during the course of a coronavirus disease 2019 patient. Clin Chim Acta. 2020;506:172‐175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Kim ES, Chin BS, Kang CK, et al; Korea National Committee for Clinical Management of COVID‐19 . Clinical course and outcomes of patients with severe acute respiratory syndrome coronavirus 2 infection: a preliminary report of the first 28 patients from the Korean cohort study on COVID‐19. J Korean Med Sci. 2020;35(13):e142. 10.3346/jkms.2020.35.e142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Perisetti A, Gajendran M, Goyal H. Putative mechanisms of diarrhea in COVID‐19. Clin Gastroenterol Hepatol. 2020;18(13):3054‐3055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Sultan S, Altayar O, Siddique SM, et al. AGA Institute rapid review of the gastrointestinal and liver manifestations of COVID‐19, meta‐analysis of international data, and recommendations for the consultative management of patients with COVID‐19. Gastroenterology. 2020;159(1):320‐334.e27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Wierdsma NJ, Peters JHC, Weijs PJM, et al. Malabsorption and nutritional balance in the ICU: fecal weight as a biomarker: a prospective observational pilot study. Crit Care. 2011;15(6):R264. 10.1186/cc10530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Kaafarani HMA, El Moheb M, Hwabejire JO, et al. Gastrointestinal complications in critically ill patients with COVID‐19. Ann Surg. 2020;272(2):e61‐e62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Wells CI, O'Grady G, Bissett IP. Acute colonic pseudo‐obstruction: a systematic review of aetiology and mechanisms. World J Gastroenterol. 2017;23(30):5634‐5644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Bhayana R, Som A, Li MD, et al. Abdominal imaging findings in COVID‐19: preliminary observations. Radiology. 2020;297(1):E207‐E215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Chan KH, Lim SL, Damati A, et al. Coronavirus disease 2019 (COVID‐19) and ischemic colitis: an under‐recognized complication. Am J Emerg Med. 2020;38(12):2758.e1‐2758.e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Amarapurkar AD, Vichare P, Pandya N, Deshpande S. Haemorrhagic enteritis and COVID‐19: causality or coincidence. J Clin Pathol. 2020;73(10):686. 10.1136/jclinpath-2020-206743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Spiezia L, Boscolo A, Poletto F, et al. COVID‐19‐related severe hypercoagulability in patients admitted to intensive care unit for acute respiratory failure. Thromb Haemost. 2020;120(6):998‐1000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Connors JM, Levy JH. Thromboinflammation and the hypercoagulability of COVID‐19. J Thromb Haemost. 2020;18(7):1559‐1561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Trindade AJ, Izard S, Coppa K, et al; Northwell COVID‐19 Research Consortium . Gastrointestinal bleeding in hospitalized COVID‐19 patients: a propensity score matched cohort study. J Intern Med. 2020;289(6):887‐894. [DOI] [PubMed] [Google Scholar]
- 45. Gadiparthi C, Perisetti A, Sayana H, Tharian B, Inamdar S, Korman A. Gastrointestinal bleeding in patients with severe SARS‐CoV‐2. Am J Gastroenterol. 2020;115(8):1283‐1285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Martin TA, Wan DW, Hajifathalian K, et al. Gastrointestinal bleeding in patients with coronavirus disease 2019: a matched case‐control study. Am J Gastroenterol. 2020;115(10):1609‐1616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Gulen M, Satar S. Uncommon presentation of COVID‐19: gastrointestinal bleeding. Clin Res Hepatol Gastroenterol. 2020;44(4):e72‐e76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. D'Ardes D, Boccatonda A, Schiavone C, et al. A case of coinfection with SARS‐COV‐2 and cytomegalovirus in the era of COVID‐19. Eur J Case Rep Intern Med. 2020;7(5):001652. 10.12890/2020_001652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Kadambari S, Klenerman P, Pollard AJ. Why the elderly appear to be more severely affected by COVID‐19: the potential role of immunosenescence and CMV. Rev Med Virol. 2020;30(5):e2144. 10.1002/rmv.2144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Al‐Kuraishy HM, Al‐Gareeb AI, Alblihed M, Guerreiro SG, Cruz‐Martins N, Batiha GES. COVID‐19 in relation to hyperglycemia and diabetes mellitus. Front Cardiovasc Med. 2021;8:644095. 10.3389/fcvm.2021.644095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Wang K, Luo J, Tan F, et al. Acute pancreatitis as the initial manifestation in 2 cases of COVID‐19 in Wuhan, China. Open Forum Infect Dis. 2020;7(9):ofaa324. 10.1093/ofid/ofaa324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Bircakova B, Bruha R, Lambert L, Grusova G, Michalek P, Burgetova A. A bimodal pattern of the onset of COVID‐19 related acute pancreatitis supports both the cytotoxic and immune‐related pathogenesis – a systematic review. Scand J Gastroenterol. 2021;56(7):870‐873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Goyal H, Sachdeva S, Perisetti A, Mann R, Inamdar S, Tharian B. Hyperlipasemia and potential pancreatic injury patterns in COVID‐19: a marker of severity or innocent bystander? Gastroenterology. 2021;160(3):946‐948.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Barlass U, Wiliams B, Dhana K, et al. Marked elevation of lipase in COVID‐19 disease: a cohort study. Clin Transl Gastroenterol. 2020;11(7):e00215. 10.14309/ctg.0000000000000215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. McNabb‐Baltar J, Jin DX, Grover AS, et al. Lipase elevation in patients with COVID‐19. Am J Gastroenterol. 2020;115(8):1286‐1288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Yang JK, Lin SS, Ji XJ, Guo LM. Binding of SARS coronavirus to its receptor damages islets and causes acute diabetes. Acta Diabetol. 2010;47(3):193‐199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Nitsche CJ, Jamieson N, Lerch MM, Mayerle JV. Drug induced pancreatitis. Best Pract Res Clin Gastroenterol. 2010;24(2):143‐155. [DOI] [PubMed] [Google Scholar]
- 58. Wang F, Wang H, Fan J, Zhang Y, Wang H, Zhao Q. Pancreatic injury patterns in patients with coronavirus disease 19 pneumonia. Gastroenterology. 2020;159(1):367‐370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Giuffrè M, Bozzato AM, Di Bella S, et al. Spontaneous rectal perforation in a patient with SARS‐CoV‐2 infection. J Pers Med. 2020;10(4):157. 10.3390/jpm10040157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Al Argan RJ, Alqatari SG, Al Said AH, et al. Gastrointestinal perforation secondary to COVID‐19: case reports and literature review. Medicine. 2021;100(19):e25771. 10.1097/MD.0000000000025771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. El Moheb M, Naar L, Christensen M, et al. Gastrointestinal complications in critically ill patients with and without COVID‐19. JAMA. 2020;324(18):1899‐1901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Hu B, Sun R, Wu A, et al. Severity of acute gastrointestinal injury grade is a predictor of all‐cause mortality in critically ill patients: a multicenter, prospective, observational study. Crit Care. 2017;21(1):188. 10.1186/s13054-017-1780-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Sun JK, Liu Y, Zou L, et al. Acute gastrointestinal injury in critically ill patients with COVID‐19 in Wuhan, China. World J Gastroenterol. 2020;26(39):6087‐6097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Patel SK, Juno JA, Lee WS, et al. Plasma ACE2 activity is persistently elevated following SARS‐CoV‐2 infection: implications for COVID‐19 pathogenesis and consequences. Eur Respir J. 2021;57(5):2003730. 10.1183/13993003.03730-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Wang J, Li F, Wei H, Lian ZX, Sun R, Tian Z. Respiratory influenza virus infection induces intestinal immune injury via microbiota‐mediated Th17 cell‐dependent inflammation. J Exp Med. 2014;211(12):2397‐2410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Zhang D, Li S, Wang N, Tan HY, Zhang Z, Feng Y. The cross‐talk between gut microbiota and lungs in common lung diseases. Front Microbiol. 2020;11:301. 10.3389/fmicb.2020.00301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Wang J, Gao Y, Yu W, Xia Y, Sun Y. Clinical significance of acute gastrointestinal injury grades in inflammatory response of critically ill patients. Nat Med J China. 2017;97(42):3312‐3315. [in Chinese]. [DOI] [PubMed] [Google Scholar]
- 68. Chen R, Sang L, Jiang M, et al; Medical Treatment Expert Group for COVID‐19 . Longitudinal hematologic and immunologic variations associated with the progression of COVID‐19 patients in China. J Allergy Clin Immunol. 2020;146(1):89‐100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Zhang L, Han C, Zhang S, et al. Diarrhea and altered inflammatory cytokine pattern in severe coronavirus disease 2019: impact on disease course and in‐hospital mortality. J Gastroenterol Hepatol. 2020;36(2):421‐429. [DOI] [PubMed] [Google Scholar]
- 70. Ren B, Chen H, Zhang D, et al. Three cases of COVID‐19 with viral nucleic acid negative in pharynx swab and positive in stool specimens during recovery period. Chin J Clin Infect Dis. 2020;13(1):33‐38. [in Chinese]. [Google Scholar]
- 71. Ralls MW, Demehri FR, Feng Y, Woods Ignatoski KM, Teitelbaum DH. Enteral nutrient deprivation in patients leads to a loss of intestinal epithelial barrier function. Surgery. 2015;157(4):732‐742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Singer P, Blaser AR, Berger MM, et al. ESPEN guideline on clinical nutrition in the intensive care unit. Clin Nutr. 2019;38(1):48‐79. [DOI] [PubMed] [Google Scholar]
- 73. Wu C, Chen X, Cai Y, et al. Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China. JAMA Intern Med. 2020;180(7):934‐943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Xiang Z, Liu J, Shi D, et al. Glucocorticoids improve severe or critical COVID‐19 by activating ACE2 and reducing IL‐6 levels. Int J Biol Sci. 2020;16(13):2382‐2391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Sattar Y, Connerney M, Rauf H, et al. Three cases of COVID‐19 disease with colonic manifestations. Am J Gastroenterol. 2020;115(6):948‐950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Zhao G, Su Y, Sun X, et al. A comparative study of the laboratory features of COVID‐19 and other viral pneumonias in the recovery stage. J Clin Lab Anal. 2020;34(10):e23483. 10.1002/jcla.23483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Wang H, Yang J. Colorectal cancer that highly express both ACE2 and TMPRSS2, suggesting severe symptoms to SARS‐CoV‐2 infection. Pathol Oncol Res. 2021;27:612969. 10.3389/pore.2021.612969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Shafiee S, Cegolon L, Khafaei M, et al. Gastrointestinal cancers, ACE‐2/TMPRSS2 expression and susceptibility to COVID‐19. Cancer Cell Int. 2021;21(1):431. 10.1186/s12935-021-02129-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Roy S, Sheikh SZ, Furey TS. A machine learning approach identifies 5‐ASA and ulcerative colitis as being linked with higher COVID‐19 mortality in patients with IBD. Sci Rep. 2021;11(1):16522. 10.1038/s41598-021-95919-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Kaplan GG, Ma C, Charlton C, et al. Antibody response to SARS‐CoV‐2 among individuals with IBD diminishes over time: a serosurveillance cohort study [Epub ahead of print 2 August 2021]. Gut. 10.1136/gutjnl-2021-325238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Issaka RB, Feld LD, Kao J, et al. Real‐world data on the impact of COVID‐19 on endoscopic procedural delays. Clin Transl Gastroenterol. 2021;12(6):e00365. 10.14309/ctg.0000000000000365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Gralnek IM, Hassan C, Beilenhoff U, et al. ESGE and ESGENA Position Statement on gastrointestinal endoscopy and the COVID‐19 pandemic. Endoscopy. 2020;52(6):483‐490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Chai N, Mei Z, Zhang W, et al. Endoscopy works during the pandemic of coronavirus COVID‐19: recommendations by the Chinese Society of Digestive Endoscopy. United European Gastroenterol J. 2020;8(7):798‐803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Hakimian S, Raines D, Reed G, et al. Assessment of video capsule endoscopy in the management of acute gastrointestinal bleeding during the COVID‐19 pandemic. JAMA Netw Open. 2021;4(7):e2118796. 10.1001/jamanetworkopen.2021.18796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Myint A, Roh L, Yang L, Connolly L, Esrailian E, May FP. Noninvasive colorectal cancer screening tests help close screening gaps during coronavirus disease 2019. Gastroenterology. 2019;161(2):712‐714.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Papa A, Covino M, Pizzolante F, et al. Gastrointestinal symptoms and digestive comorbidities in an Italian cohort of patients with COVID‐19. Eur Rev Med Pharmacol Sci. 2020;24(13):7506‐7511. [DOI] [PubMed] [Google Scholar]
- 87. Aghemo A, Piovani D, Parigi TL, et al; Humanitas COVID‐19 Task Force . COVID‐19 digestive system involvement and clinical outcomes in a large academic hospital in Milan, Italy. Clin Gastroenterol Hepatol. 2020;18(10):2366‐2368.e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Ahmad M, Beg BM, Majeed A, et al. Epidemiological and clinical characteristics of COVID‐19: a retrospective multi‐center study in Pakistan. Front Public Health. 2021;9:644199. 10.3389/fpubh.2021.644199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. An P, Chen H, Ren H, et al. Gastrointestinal symptoms onset in COVID‐19 patients in Wuhan, China. Dig Dis Sci. 2021;66(10):3578‐3587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Aumpan N, Nunanan P, Vilaichone RK. Gastrointestinal manifestation as clinical predictor of severe COVID‐19: a retrospective experience and literature review of COVID‐19 in Association of Southeast Asian Nations (ASEAN). JGH Open. 2020;4(6):1096‐1101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Bishehsari F, Adnan D, Deshmukh A, et al. Gastrointestinal symptoms predict the outcomes from COVID‐19 infection [Epub ahead of print 12 March 2021]. J Clin Gastroenterol. 10.1097/MCG.0000000000001513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Cao C, Chen M, He L, Xie J, Chen X. Clinical features and outcomes of COVID‐19 patients with gastrointestinal symptoms. Crit Care. 2020;24(1):340. 10.1186/s13054-020-03034-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Carvalho‐Schneider C, Laurent E, Lemaignen A, et al. Follow‐up of adults with noncritical COVID‐19 two months after symptom onset. Clin Microbiol Infect. 2021;27(2):258‐263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Chen A, Agarwal A, Ravindran N, To C, Zhang T, Thuluvath PJ. Are gastrointestinal symptoms specific for coronavirus 2019 infection? A prospective case‐control study from the United States. Gastroenterology. 2020;159(3):1161‐1163.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Chen R, Yu YL, Li W, et al. Gastrointestinal symptoms associated with unfavorable prognosis of COVID‐19 patients: a retrospective study. Front Med (Lausanne). 2020;7:608259. 10.3389/fmed.2020.608259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Cholankeril G, Podboy A, Aivaliotis VI, et al. Association of digestive symptoms and hospitalization in patients with SARS‐CoV‐2 infection. Am J Gastroenterol. 2020;115(7):1129‐1132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Deng W, Guang TW, Yang M, et al. Positive results for patients with COVID‐19 discharged from hospital in Chongqing, China. BMC Infect Dis. 2020;20(1):429. 10.1186/s12879-020-05151-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Duque MP, Lucaccioni H, Costa C, et al. COVID‐19 symptoms: a case–control study, Portugal, March–April 2020. Epidemiol Infect. 2021;149:e54. 10.1017/S095026882100042X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Elmunzer BJ, Spitzer RL, Foster LD, et al.; North American Alliance for the Study of Digestive Manifestations of COVID‐19. Digestive manifestations in patients hospitalized with coronavirus disease 2019. Clin Gastroenterol Hepatol. 2021;19(7):1355‐1365.e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100. Fallouh NA, Naik KH, Udochi CO, et al. Better clinical outcomes in hospitalized COVID‐19 minority patients with accompanying gastrointestinal symptoms [Epub ahead of print 24 June 2021]. J Natl Med Assoc. 10.1016/j.jnma.2021.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101. Ferm S, Fisher C, Pakala T, et al. Analysis of gastrointestinal and hepatic manifestations of SARS‐CoV‐2 infection in 892 patients in Queens, NY. Clin Gastroenterol Hepatol. 2020;18(10):2378‐2379.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102. Graham G, Taegtmeyer M, Lewis J, Subramanian S. Gastrointestinal symptoms involvement in hospitalised COVID‐19 patients in Liverpool, UK: a descriptive cross‐sectional, single‐centre study. Clin Med (Lond). 2021;21(Suppl):23‐24. [DOI] [PubMed] [Google Scholar]
- 103. Greco S, Fabbri N, Bella A, et al. COVID‐19 inpatients with gastrointestinal onset: sex and care needs' differences in the district of Ferrara, Italy. BMC Infect Dis. 2021;21(1):739. 10.1186/s12879-021-06476-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104. Guerra I, Algaba A, Jiménez L e a. Incidence, clinical characteristics, and evolution of SARS‐CoV‐2 infection in patients with inflammatory bowel disease: a single‐center study in Madrid, Spain. Inflamm Bowel Dis. 2021;27(1):25‐33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105. Kim SY, Yoo DM, Min C, Kim JH, Choi HG. Evaluation of mortality and morbidity according to initial symptoms in COVID‐19 patients using clinical epidemiologic data from the Korea Centers for Disease Control & Prevention. Medicina (Kaunas). 2021;57(7):688. 10.3390/medicina57070688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106. Laszkowska M, Faye AS, Kim J, et al. Disease course and outcomes of COVID‐19 among hospitalized patients with gastrointestinal manifestations. Clin Gastroenterol Hepatol. 2021;19(7):1402‐1409.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107. Leal T, Costa E, Arroja B, Gonçalves R, Alves J. Gastrointestinal manifestations of COVID‐19: results from a European centre. Eur J Gastroenterol Hepatol. 2021;33(5):691‐694. [DOI] [PubMed] [Google Scholar]
- 108. Rivera‐Izquierdo M, Valero‐Ubierna MDC, Martínez‐Diz S, et al. Clinical factors, preventive behaviours and temporal outcomes associated with COVID‐19 infection in health professionals at a Spanish hospital. Int J Environ Res Public Health. 2020;17(12):4305. 10.3390/ijerph17124305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109. Mokarram P, Dalivand MM, Pizuorno A, et al. Clinical characteristics, gastrointestinal manifestations and outcomes of COVID‐19 patients in Iran; does the location matters? World J Clin Cases. 2021;9(18):4654‐4667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110. O'Keefe JB, Tong EJ, O'Keefe GD, Tong DC. Description of symptom course in a telemedicine monitoring clinic for acute symptomatic COVID‐19: a retrospective cohort study. BMJ Open. 2021;11(3):e044154. 10.1136/bmjopen-2020-044154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111. Park SK, Lee CW, Park DI, et al. Detection of SARS‐CoV‐2 in fecal samples from patients with asymptomatic and mild COVID‐19 in Korea. Clin Gastroenterol Hepatol. 2021;19(7):1387‐1394.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112. Ramachandran P, Onukogu I, Ghanta S, et al. Gastrointestinal symptoms and outcomes in hospitalized coronavirus disease 2019 patients. Dig Dis. 2020;38(5):373‐379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113. Remes‐Troche JM, Ramos‐de‐la‐Medina A, Manríquez‐Reyes M, Martínez‐Pérez‐Maldonado L, Lara EL, Solís‐González MA. Initial gastrointestinal manifestations in patients with severe acute respiratory syndrome coronavirus 2 infection in 112 patients from Veracruz in Southeastern Mexico. Gastroenterology. 2020;159(3):1179‐1181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114. Renelus BD, Khoury N, Chandrasekaran K, Bekele E, Briggs WM, Jamorabo DS. Hospitalized coronavirus disease‐2019 (COVID‐19) patients with gastrointestinal symptoms have improved survival to discharge. Dig Liver Dis. 2020;52(12):1403‐1406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115. Saeed U, Sellevoll HB, Young VS, Sandbaek G, Glomsaker T, Mala T. COVID‐19 may present with acute abdominal pain. Br J Surg. 2020;107(7):e186‐e187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116. Schettino M, Pellegrini L, Picascia D, et al. Clinical characteristics of COVID‐19 patients with gastrointestinal symptoms in northern Italy: a single‐center cohort study. Am J Gastroenterol. 2020;116(2):306‐310. [DOI] [PubMed] [Google Scholar]
- 117. Sierpiński R, Pinkas J, Jankowski M, et al. Sex differences in the frequency of gastrointestinal symptoms and olfactory or taste disorders in 1942 nonhospitalized patients with coronavirus disease 2019 (COVID‐19). Pol Arch Intern Med. 2020;130(6):501‐505. [DOI] [PubMed] [Google Scholar]
- 118. Sulaiman T, Algharawi AA, Idrees M, et al. The prevalence of gastrointestinal symptoms among patients with COVID‐19 and the effect on the severity of the disease. JGH Open. 2020;4(6):1162‐1166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119. Sun LL, Wang J, Wang YS, et al. Symptomatic features and prognosis of 932 hospitalized patients with coronavirus disease 2019 in Wuhan. J Dig Dis. 2021;22(5):271‐281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120. Taziki Balajelini MH, Rajabi A, Mohammadi M, et al. Virus load and incidence of olfactory, gustatory, respiratory, gastrointestinal disorders in COVID‐19 patients: a retrospective cohort study. Clin Otolaryngol. 2021;46(6):1331‐1338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121. Tsibouris P, Ekmektzoglou K, Agorogianni A, et al. Gastrointestinal involvement in COVID‐19 patients: a retrospective study from a Greek COVID‐19 referral hospital. Ann Gastroenterol. 2020;33(5):465‐472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122. Xiao Y, Huang S, Yan L, et al. Clinical characteristics of diarrhea in 90 cases with COVID‐19: a descriptive study. Int Emerg Nurs. 2020;52:100912. 10.1016/j.ienj.2020.100912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123. Xu J, Chu M, Zhong F, et al. Digestive symptoms of COVID‐19 and expression of ACE2 in digestive tract organs. Cell Death Discov. 2020;6:76. 10.1038/s41420-020-00307-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124. Yang TY, Li YC, Wang SC, et al. Clinical characteristics of patients with COVID‐19 presenting with gastrointestinal symptoms as initial symptoms: retrospective case series. World J Clin Cases. 2020;8(14):2950‐2958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125. Yoshida Y, Gillet SA, Brown MI, et al. Clinical characteristics and outcomes in women and men hospitalized for coronavirus disease 2019 in New Orleans. Biol Sex Differ. 2021;12(1):20. 10.1186/s13293-021-00359-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126. Zhang H, Liao YS, Gong J, Liu J, Xia X, Zhang H. Clinical characteristics of coronavirus disease (COVID‐19) patients with gastrointestinal symptoms: a report of 164 cases. Dig Liver Dis. 2020;52(10):1076‐1079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127. Zheng T, Yang C, Wang HY, et al. Clinical characteristics and outcomes of COVID‐19 patients with gastrointestinal symptoms admitted to Jianghan Fangcang Shelter Hospital in Wuhan, China. J Med Virol. 2020;92(11):2735‐2741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128. Zhu H, Fu L, Jin Y, et al. Clinical features of COVID‐19 convalescent patients with re‐positive nucleic acid detection. J Clin Lab Anal. 2020;34(7):e23392. 10.1002/jcla.23392. [DOI] [PMC free article] [PubMed] [Google Scholar]


