Abstract
Aims
The coronavirus disease‐2019 (COVID‐19) pandemic has changed the landscape of medical care delivery worldwide. We aimed to assess the influence of COVID‐19 pandemic on hospital admissions and in‐hospital mortality rate in patients with acute heart failure (AHF) in a retrospective, multicentre study.
Methods and results
From 1 January 2019 to 31 December 2020, a total of 101 433 patients were hospitalized in 24 Cardiology Departments in Poland. The number of patients admitted due to AHF decreased by 23.4% from 9853 in 2019 to 7546 in 2020 (P < 0.001). We noted a significant reduction of self‐referrals in the times of COVID‐19 pandemic accounting 27.8% (P < 0.001), with increased number of AHF patients brought by an ambulance by 15.9% (P < 0.001). The length of hospital stay was overall similar (7.7 ± 2.8 vs. 8.2 ± 3.7 days; P = not significant). The in‐hospital all‐cause mortality in AHF patients was 444 (5.2%) in 2019 vs. 406 (6.5%) in 2020 (P < 0.001). A total number of AHF patients with concomitant COVID‐19 was 239 (3.2% of AHF patients hospitalized in 2020). The rate of in‐hospital deaths in AHF patients with COVID‐19 was extremely high accounting 31.4%, reaching up to 44.1% in the peak of the pandemic in November 2020.
Conclusions
Our study indicates that the COVID‐19 pandemic led to (i) reduced hospital admissions for AHF; (ii) decreased number of self‐referred AHF patients and increased number of AHF patients brought by an ambulance; and (iii) increased in‐hospital mortality for AHF with very high mortality rate for concomitant AHF and COVID‐19.
Keywords: Heart failure, COVID‐19, In‐hospital mortality, Hospitalization
Introduction
The coronavirus disease‐2019 (COVID‐19) pandemic has dramatically changed the health care landscape worldwide. The heavy burden of reallocation of resources to fight the pandemic brought the shortcomings in treatment of other medical conditions. Acute heart failure (AHF) is a life‐threatening emergency requiring urgent in‐hospital diagnostics and treatment. It is usually a consequence of decompensation of a chronic heart failure (HF). 1 The main underlying causes of AHF include acute coronary syndrome, myocarditis, valvular disease, arrhythmia, uncontrolled hypertension, generalized infection (including COVID‐19), and non‐adherence to therapy. Patients presenting with more severe symptoms [in higher class of New York Heart Association (NYHA) classification] have worse prognosis. 2 The prevalence of HF is 1–2% of adult population, while according to the ESC‐HF pilot study, the 12 months of hospitalization rates are 32–44%. 3 Since the beginning of the COVID‐19 pandemic, the rate of hospital admissions due to various cardiovascular causes declined significantly. 4 , 5 , 6 , 7 Data from many countries report reduced number of admitted AHF patients presenting with more severe symptoms as compared with previous years. 8 , 9 , 10 , 11 , 12 , 13 , 14 Co‐occurrence of severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) infection and HF together with older age and lung disease create so‐called ‘deadly quartet’ associated with very poor prognosis. 15
We aimed to assess the influence of COVID‐19 pandemic on hospital admissions and in‐hospital mortality rate in patients with AHF in a retrospective, multicentre study in Poland.
Methods
We performed a retrospective analysis of hospital records of consecutive patients hospitalized in 24 Cardiology Departments (Supporting Information, Table S1 ) in Poland in 2019 and 2020. Out of total number of hospitalizations, we extracted patients admitted due to AHF (International Statistical Classification of Diseases and Related Health Problems codes for HF I50.x) from 1 January 2019 to 31 December 2020 (pre‐COVID‐19 vs. COVID‐19 eras). The AHF was defined accordingly to 2016 European Society of Cardiology guidelines for the diagnosis and treatment of AHF and chronic HF as rapid onset or worsening of symptoms and/or signs of HF. 1 We confronted the number of AHF hospitalizations, modes of admission, baseline characteristics, and in‐hospital mortality rate in patients hospitalized due to AHF during the pandemic in 2020 vs. 2019. We also retrieved data on concomitant presence of SARS‐CoV‐2 infection and evaluated its influence on in‐hospital mortality. The study was conducted in accordance with the Declaration of Helsinki and was approved by the local ethics committee (study approval reference number KB 353/2021).
The statistical analysis was carried out using the Statistica 13.0 package (TIBCO Software Inc, California, USA). Continuous variables were presented as means with standard deviations. The Shapiro–Wilk test demonstrated non‐normal distribution of the investigated data. Therefore, for comparison of continuous variables between 2019 and 2020, non‐parametric Wilcoxon signed rank test was used. Categorical variables were expressed as the number and the percentage. Categorical variables were compared using the χ 2 test. Results were considered significant at P < 0.05.
Results
From 1 January 2019 to 31 December 2020, a total of 101 433 of patients were hospitalized in 24 Cardiology Departments in Poland (Supporting Information, Table S1 ). The total number of hospitalizations in 2019 was 59 175, while in 2020 it was 42 258, accounting a decrease of 28.6% (P < 0.001) [Figure 1(A) ].
Figure 1.
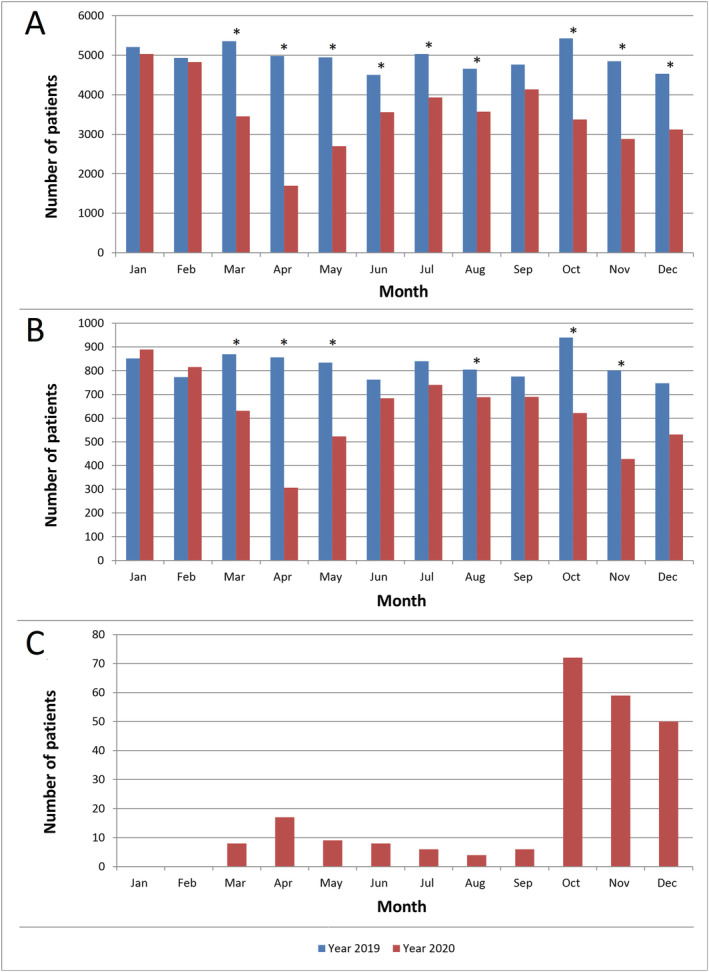
Number of hospitalizations: total (n = 101 433) (A), due to acute heart failure (n = 17 399) (B), and due to acute heart failure with concomitant COVID‐19 (n = 239) (C). *P < 0.05.
The number of patients admitted due to AHF decreased by 23.4% from 9853 in 2019 to 7546 in 2020 (P < 0.001). The reduction of hospitalizations rate due to AHF was the most visibly pronounced at the beginning of the pandemic in Poland during the first public lockdown from March to May 2020 and during its peak from October to November 2020 [Figure 1(B) ].
Interestingly, the total number of self‐referred patients was reduced by 27.8% (P < 0.001) with significantly lower rates achieved during the first public lockdown in April 2020 and in the peak of the pandemic in the fourth quarter of 2020 as compared with the time‐matched period in 2019. In the same timeframe, the number of patients brought by an ambulance was significantly higher in 2020 vs. 2019 with an increase of 15.9% (P < 0.001) (Table 1 ).
Table 1.
Modes of hospital admissions
| Month | Number of sites | Self‐referred | P | Brought by an ambulance | P | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 2019 | 2020 | 2019 | 2020 | ||||||||
| N | % | N | % | N | % | N | % | ||||
| 1 | 22 | 392 | 55.4 | 459 | 60.5 | ns | 265 | 37.5 | 254 | 33.5 | ns |
| 2 | 22 | 375 | 57.7 | 425 | 60.8 | ns | 223 | 34.3 | 246 | 35.2 | ns |
| 3 | 22 | 408 | 56.0 | 299 | 55.7 | ns | 288 | 39.5 | 213 | 39.7 | ns |
| 4 | 22 | 430 | 59.1 | 116 | 45.7 | <0.001 | 249 | 34.2 | 124 | 48.8 | <0.001 |
| 5 | 22 | 417 | 60.4 | 255 | 58.5 | ns | 230 | 33.3 | 162 | 37.2 | ns |
| 6 | 22 | 360 | 57.1 | 303 | 53.1 | ns | 230 | 36.5 | 212 | 37.1 | ns |
| 7 | 22 | 409 | 59.1 | 357 | 56.7 | ns | 231 | 33.4 | 214 | 34.0 | ns |
| 8 | 22 | 393 | 57.2 | 330 | 57.6 | ns | 253 | 36.8 | 211 | 36.8 | ns |
| 9 | 22 | 378 | 58.9 | 352 | 59.9 | ns | 219 | 34.1 | 207 | 35.2 | ns |
| 10 | 22 | 509 | 65.4 | 260 | 51.1 | <0.001 | 222 | 28.5 | 222 | 43.6 | <0.001 |
| 11 | 22 | 418 | 61.0 | 152 | 45.1 | <0.001 | 234 | 34.2 | 159 | 47.2 | <0.001 |
| 12 | 22 | 378 | 59.6 | 208 | 49.4 | 0.001 | 229 | 36.1 | 191 | 45.4 | 0.003 |
| Year | 22 | 4867 | 59.0 | 3516 | 55.8 | <0.001 | 2873 | 34.8 | 2415 | 38.2 | <0.001 |
ns, not significant.
The length of hospital stay ranged from 7 to 9 days and was significantly longer only in the very peak of pandemic in November 2020 vs. November 2019 (8.9 ± 4.0 vs. 7.3 ± 2.8 days; P = 0.026) (Table 2 ). Patients hospitalized due to AHF during the pandemic vs. 2019 were of similar age (Supporting Information, Table S1 ).
Table 2.
The length of hospitalization due to acute heart failure
| Month | Number of sites | 2019 | 2020 | P | ||
|---|---|---|---|---|---|---|
| Mean hospitalization length (days) | SD | Mean hospitalization length (days) | SD | |||
| 1 | 23 | 7.57 | 2.53 | 7.49 | 2.05 | ns |
| 2 | 23 | 7.77 | 2.75 | 7.95 | 2.83 | ns |
| 3 | 23 | 7.26 | 2.77 | 7.79 | 3.32 | ns |
| 4 | 23 | 8.50 | 3.39 | 8.87 | 3.72 | ns |
| 5 | 23 | 7.65 | 2.31 | 8.42 | 4.33 | ns |
| 6 | 23 | 8.15 | 4.15 | 8.74 | 3.76 | ns |
| 7 | 23 | 7.88 | 2.85 | 7.29 | 3.32 | ns |
| 8 | 23 | 7.41 | 2.45 | 8.36 | 4.33 | ns |
| 9 | 23 | 7.42 | 2.44 | 7.65 | 3.79 | ns |
| 10 | 23 | 7.54 | 2.35 | 7.97 | 4.18 | ns |
| 11 | 23 | 7.30 | 1.95 | 8.91 | 4.02 | 0.026 |
| 12 | 23 | 8.02 | 3.07 | 8.84 | 4.37 | ns |
| Year | 24 | 7.70 | 2.77 | 8.18 | 3.68 | ns |
ns, not significant; SD, standard deviation.
A total number of AHF patients with concomitant COVID‐19 was 239 (3.2% of AHF patients hospitalized in 2020), and the vast majority of them were hospitalized during the peak of the pandemic in Poland from October to December 2020 [Figure 1(C) ].
The in‐hospital all‐cause mortality in AHF patients was 406 (6.5%) in 2020 vs. 444 (5.2%) in 2019 (P < 0.001) (Table 3 ). The in‐hospital mortality rates were highest at the beginning of the pandemic in Poland during the public lockdown in March 2020 and during its peak in November 2020 as compared with 2019 (Figure 2 ).
Table 3.
The in‐hospital mortality for acute heart failure
| Month | Number of sites | In‐hospital mortality for AHF without COVID‐19 | In‐hospital mortality for AHF with COVID‐19 | P a | P b | ||||
|---|---|---|---|---|---|---|---|---|---|
| 2019 | 2020 | 2020 | |||||||
| N | % | N | % | N | % | ||||
| 1 | 23 | 54 | 7.3 | 45 | 5.7 | 0 | — | ns | — |
| 2 | 23 | 40 | 5.9 | 47 | 6.6 | 0 | — | ns | — |
| 3 | 23 | 44 | 5.8 | 40 | 7.3 | 0 | 0.0 | ns | ns |
| 4 | 23 | 35 | 4.6 | 26 | 10.4 | 6 | 35.3 | <0.001 | 0.002 |
| 5 | 23 | 28 | 3.9 | 25 | 5.6 | 3 | 33.3 | ns | 0.007 |
| 6 | 23 | 31 | 4.8 | 34 | 5.8 | 1 | 12.5 | ns | ns |
| 7 | 23 | 35 | 4.8 | 28 | 4.4 | 1 | 16.7 | ns | ns |
| 8 | 23 | 37 | 5.2 | 23 | 3.9 | 1 | 25.0 | ns | ns |
| 9 | 23 | 37 | 5.6 | 33 | 5.6 | 2 | 33.3 | ns | 0.044 |
| 10 | 23 | 26 | 3.2 | 39 | 8.5 | 19 | 26.4 | <0.001 | <0.001 |
| 11 | 23 | 40 | 5.6 | 39 | 13.4 | 26 | 44.1 | <0.001 | <0.001 |
| 12 | 23 | 37 | 5.6 | 27 | 7.1 | 16 | 32.0 | ns | <0.001 |
| Year | 23 | 444 | 5.2 | 406 | 6.5 | 75 | 31.4 | <0.001 | <0.001 |
AHF, acute heart failure; COVID‐19, coronavirus disease‐2019; ns, not significant.
For the comparison of 2019 and 2020 without coexisting COVID‐19.
For the comparison of 2020 without coexisting COVID‐19 and with coexisting COVID‐19.
Figure 2.
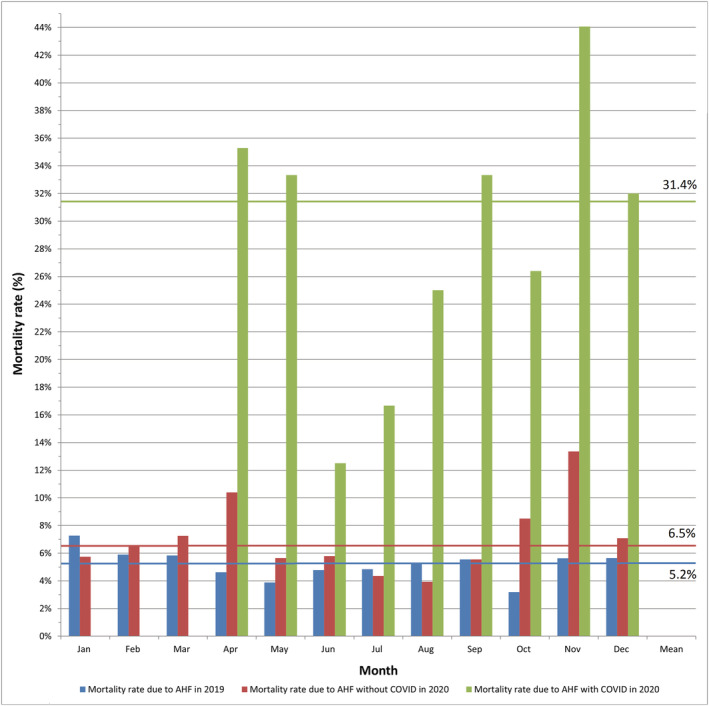
In‐hospital mortality due to acute heart failure in patients with and without COVID‐19. *P < 0.05. AHF, acute heart failure; COVID‐19, coronavirus disease‐2019.
The rate of in‐hospital deaths in concomitant AHF and COVID‐19 patients was extremely high accounting 31.4%, reaching up to 44.1% in the very peak of the pandemic in November 2020 (Table 3 ).
In majority of the Cardiology Departments included in the analysis, the total number of beds available during the pandemic was decreased as compared with 2019 (Table 4 ). Additional beds available for COVID‐19 patients were created with the highest number reaching 264 in November 2020.
Table 4.
Number of beds available
| Month | Number of sites | Total number of beds | Number of beds dedicated to COVID‐19 patients | |
|---|---|---|---|---|
| 2019 | 2020 | 2020 | ||
| 1 | 24 | 887 | 876 | 0 |
| 2 | 24 | 887 | 876 | 0 |
| 3 | 24 | 882 | 849 | 66 |
| 4 | 24 | 882 | 851 | 90 |
| 5 | 24 | 882 | 849 | 104 |
| 6 | 24 | 882 | 870 | 74 |
| 7 | 24 | 882 | 880 | 55 |
| 8 | 24 | 882 | 880 | 26 |
| 9 | 24 | 882 | 855 | 59 |
| 10 | 24 | 882 | 887 | 164 |
| 11 | 24 | 882 | 846 | 264 |
| 12 | 24 | 882 | 830 | 254 |
| Average monthly | 24 | 883 | 862 | 96 |
COVID‐19, coronavirus disease‐2019.
Discussion
The COVID‐19 pandemic has undoubtedly put a heavy burden on health care systems all around the globe. All efforts currently focus on delivering the highest standard of care for COVID‐19 patients. To the best of our knowledge, this is the largest multicentre study published so far including more than 100 000 patients hospitalized in 24 Cardiology Departments in Poland. Comparing pre‐COVID‐19 vs. COVID‐19 eras, we found reduced total number of hospitalizations, as well as hospitalizations due to AHF with significantly increased in‐hospital mortality in AHF patients with and without concomitant SARS‐CoV‐2 infection. The reduction of hospital admissions is consistent with data coming from mostly single‐centre reports from the UK, 8 Italy, 9 Germany, 10 the USA, 11 Canada, 12 and Australia. 13 These findings, together with our results, represent a global trend of reduced AHF hospitalizations during the COVID‐19 pandemic. It is speculated that the reasons for this phenomenon could include avoidance or delaying to seek the medical care in fear of exposure to SARS‐CoV‐2; reduced HF decompensation rates due to, for example, self‐isolation and social distancing related to reduced energy expenditure or lower risk of getting other respiratory tract infections; and improved medication and dietary adherence. 13 , 14
Our report on modes of hospital admissions gives some novel insight into better understanding of the observed reduction in AHF hospital admissions. Studies published so far did not distinguish whether the patients were self‐referred or brought by emergency teams. In our analysis, we found less self‐referred patients and more patients brought by an ambulance during the pandemic vs. 2019, which was even more pronounced during the peak of the pandemic. The reluctance to seek for medical care reflects the fear of getting COVID‐19 infection during hospitalization. Some studies suggested that delayed seeking for medical attention until symptoms are critical was responsible for higher percentage of patients with NYHA III or IV symptoms during COVID‐19 vs. non‐COVID‐19 era. 8 , 13 However, it did not directly translate into longer hospital stay. We observed longer hospital stay only in the peak of the pandemic in November 2020.
As reported by the Statistics Poland, the global death rates in Poland increased by 16.5% from 409 709 in 2019 to 477 355 in 2020. 16 Interestingly, there were 41 422 deaths due to COVID‐19 accounting for 61.2% of the difference in death rates in 2019 vs. 2020. According to our observations, the COVID‐19 pandemic has brought an increase of in‐hospital mortality for both SARS‐CoV‐2 positive and negative AHF patients as compared with 2019. The two‐centre analysis by Cannatà et al. compared 578 patients hospitalized for HF between January and June 2020 with 794 patients from a corresponding period of 2019. 17 The study reported a significantly higher mortality rate among HF patients in 2020 compared with 2019, with only nine reported COVID‐19 cases. Similarly, Frankfurter et al. noticed a trend towards higher mortality in the COVID‐19 era vs. time‐matched 2019 cohort. 12 A single‐centre study by Colivicchi et al. analysed AHF patients admitted to an emergency department during the first Italian lockdown, excluding those with any evidence of SARS‐CoV‐2 infection. 9 They reported 17.2% all‐cause in‐hospital mortality in February–April 2020 vs. 6.3% in the corresponding period of 2019. Yet, a Danish nationwide cohort study conducted by Andersson et al. concluded that on the population‐based level, mortality in HF patients has not been impacted by the national lockdown. 18 Interestingly, in some studies from the USA and Australia, the in‐hospital mortality rates did not differ in COVID‐19 vs. non‐COVID‐19 eras, despite reporting decreased hospital admissions with patients presenting in higher NYHA class. 11 , 13
It was postulated by Calcaterra et al. that concomitant COVID‐19 infection and HF together with older age and lung disease create the deadly quartet. 15 This combination was responsible for a very high mortality rate in Northern Italy accounting 31% in the city of Bergamo. In the Cardio‐COVID‐Italy multicentre, retrospective, observational study including 692 COVID‐19 patients, the in‐hospital mortality rate was two times higher in patients with both COVID‐19 and HF as compared with patients with no HF history, which were 41.1% vs. 20.9%, respectively. 19 This is consistent with an extremely high mortality of 31.4% among patients with coexisting COVID‐19 and AHF observed in our study. However, the recently published nationwide Danish cohort study did not find single cardiovascular morbidity to influence prognosis in men, with only modestly increased risk of severe COVID‐19 infection in women with HF. 20
Limitations
Several limitations of our study should be acknowledged. Firstly, it is a retrospective study. Secondly, analysed data were derived from hospital electronic databases not providing detailed characteristics of patients or additional test results; thus, they were not available for the assessment. Thirdly, any clinical information including cause, percentage of new onset AHF, clinical trajectory, or severity of the disease is also missing. Fourthly, although we found that concomitant COVID‐19 worsen the prognosis in AHF patients, we did not document COVID‐19 to be a direct cause of AHF.
Conclusions
Our study indicates that the COVID‐19 pandemic led to (i) reduced hospital admissions for AHF during the pandemic; (ii) decreased number of self‐referred AHF patients and increased number of AHF patients brought by an ambulance during the pandemic; and (iii) increased in‐hospital mortality for AHF with very high mortality rate for concomitant AHF and COVID‐19.
Conflict of interest
None declared.
Funding
The study received no external funding.
Supporting information
Table S1. Data collected from all sites.
Kubica, J. , Ostrowska, M. , Stolarek, W. , Kasprzak, M. , Grzelakowska, K. , Kryś, J. , Kubica, A. , Adamski, P. , Podhajski, P. , Navarese, E. P. , Anielska‐Michalak, E. , Brycht, O. , Curzytek, A. , Dudek, A. , Gromadziński, L. , Grzelakowski, P. , Kamiński, L. , Kleinrok, A. , Kostkiewicz, M. , Koziński, M. , Król, P. , Kulawik, T. , Minczew, G. , Mindykowski, M. , Pawlak, A. , Prokopczuk, J. , Skonieczny, G. , Sobkowicz, B. , Sowiński, S. , Stankala, S. , Szymański, P. , Wester, A. , Wilczewski, P. , Bartuś, S. , Budaj, A. , Gąsior, M. , Gruchała, M. , Drożdż, J. , Jaguszewski, M. , Jankowski, P. , Legutko, J. , Lesiak, M. , Leszek, P. , Mitkowski, P. , Nessler, J. , Tomaszuk‐Kazberuk, A. , Tycińska, A. , Zdrojewski, T. , and Kaźmierczak, J. (2022) Impact of COVID‐19 pandemic on acute heart failure admissions and mortality: a multicentre study (COV‐HF‐SIRIO 6 study). ESC Heart Failure, 9: 721–728. 10.1002/ehf2.13680.
References
- 1. Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JGF, Coats AJS, Falk V, González‐Juanatey JR, Harjola VP, Jankowska EA, Jessup M, Linde C, Nihoyannopoulos P, Parissis JT, Pieske B, Riley JP, Rosano GMC, Ruilope LM, Ruschitzka F, Rutten FH, van der Meer P, ESC Scientific Document Group . 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J 2016; 37: 2129–2200. [DOI] [PubMed] [Google Scholar]
- 2. Chen J, Normand SLT, Wang Y, Krumholz HM. National and regional trends in heart failure hospitalization and mortality rates for Medicare beneficiaries, 1998–2008. JAMA 2011; 306:1669–1678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Maggioni AP, Dahlström U, Filippatos G, Chioncel O, Leiro MC, Drozdz J, Fruhwald F, Gullestad L, Logeart D, Fabbri G, Urso R, Metra M, Parissis J, Persson H, Ponikowski P, Rauchhaus M, Voors AA, Nielsen OW, Zannad F, Tavazzi L. EURObservational Research Programme: regional differences and 1‐year follow‐up results of the Heart Failure Pilot Survey (ESC‐HF Pilot). Eur J Heart Fail 2013; 15: 808–817. [DOI] [PubMed] [Google Scholar]
- 4. Metzler B, Siostrzonek P, Binder RK, Bauer A, Reinstadler SJ. Decline of acute coronary syndrome admissions in Austria since the outbreak of COVID‐19: the pandemic response causes cardiac collateral damage. Eur Heart J 2020; 41: 1852–1853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. De Filippo O, D'Ascenzo F, Angelini F, Bocchino PP, Conrotto F, Saglietto A, Secco GG, Campo G, Gallone G, Verardi R, Gaido L, Iannaccone M, Galvani M, Ugo F, Barbero U, Infantino V, Olivotti L, Mennuni M, Gili S, Infusino F, Vercellino M, Zucchetti O, Casella G, Giammaria M, Boccuzzi G, Tolomeo P, Doronzo B, Senatore G, Grosso Marra W, Rognoni A, Trabattoni D, Franchin L, Borin A, Bruno F, Galluzzo A, Gambino A, Nicolino A, Truffa Giachet A, Sardella G, Fedele F, Monticone S, Montefusco A, Omedè P, Pennone M, Patti G, Mancone M, De Ferrari GM. Reduced rate of hospital admissions for ACS during Covid‐19 outbreak in northern Italy. N Engl J Med 2020; 383: 88–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Bhatt AS, Moscone A, McElrath EE, Varshney AS, Claggett BL, Bhatt DL, Januzzi JL, Butler J, Adler DS, Solomon SD, Vaduganathan M. Declines in hospitalizations for acute cardiovascular conditions during the COVID‐19 pandemic: a multicenter tertiary care experience. J Am Coll Cardiol 2020; 76: 280–288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Hawranek M, Grygier M, Bujak K, Bartuś S, Gierlotka M, Wojakowski W, Legutko J, Lesiak M, Pączek P, Kleinrok A, Milewski K, Kubica J, Tajstra M, Dudek D, Witkowski A, Gąsior M. Characteristics of patients from the polish registry of acute coronary syndromes during the COVID‐19 pandemic: the first report. Kardiol Pol 2021; 79: 192–195. [DOI] [PubMed] [Google Scholar]
- 8. Bromage DI, Cannatà A, Rind IA, Gregorio C, Piper S, Shah AM, McDonagh TA. The impact of COVID‐19 on heart failure hospitalization and management: report from a heart failure unit in London during the peak of the pandemic. Eur J Heart Fail 2020; 22: 978–984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Colivicchi F, Di Fusco SA, Magnanti M, Cipriani M, Imperoli G. The impact of the coronavirus Disease‐2019 pandemic and italian lockdown measures on clinical presentation and Management of Acute Heart Failure. J Card Fail 2020; 26: 464–465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Bollmann A, Hohenstein S, Meier‐Hellmann A, Kuhlen R, Hindricks G. Emergency hospital admissions and interventional treatments for heart failure and cardiac arrhythmias in Germany during the Covid‐19 outbreak: insights from the german‐wide helios hospital network. Eur Heart J Qual Care Clin Outcomes 2020; 6: 221–222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Cox ZL, Lai P, Lindenfeld J. Decreases in acute heart failure hospitalizations during COVID‐19. Eur J Heart Fail 2020; 22: 1045–1046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Frankfurter C, Buchan TA, Kobulnik J, Lee DS, Luk A, McDonald M, Ross HJ, Alba AC. Reduced rate of hospital presentations for heart failure during the COVID‐19 pandemic in Toronto, Canada. Can J Cardiol 2020; 36: 1680–1684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Toner L, Koshy AN, Ko J, Driscoll A, Farouque O. Clinical characteristics and trends in heart failure hospitalizations: an australian experience during the COVID‐19 lockdown. JACC Heart Fail 2020; 8: 872–875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Barghash MH, Pinney SP. Heart failure in the COVID‐19 pandemic: where has all New York's congestion Gone? J Card Fail 2020; 26: 477–478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Calcaterra G, Bassareo PP, Barillà F, Sergi D, Chiocchi M, Romeo F, Mehta JL. The deadly quartet (Covid‐19, old age, lung disease, and heart Failure) explains why coronavirus‐related mortality in northern Italy was so high. Curr Cardiol Rev 2021; 17: 74–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Poland, Statisctics. Mortality and deaths by caused in 2020. https://stat.gov.pl/en/topics/population/mortality‐and‐deaths‐by‐causes‐/mortality‐and‐deaths‐by‐causes‐in‐2020,1,1.html. 13 September 2021.
- 17. Cannatà A, Bromage DI, Rind IA, Gregorio C, Bannister C, Albarjas M, Piper S, Shah AM, McDonagh TA. Temporal trends in decompensated heart failure and outcomes during COVID‐19: a multisite report from heart failure referral centres in London. Eur J Heart Fail 2020; 22: 2219–2224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Andersson C, Gerds T, Fosbøl E, Phelps M, Andersen J, Lamberts M, Holt A, Butt JH, Madelaire C, Gislason G, Torp‐Pedersen C, Køber L, Schou M. Incidence of new‐onset and worsening heart failure before and after the COVID‐19 epidemic lockdown in Denmark: a Nationwide cohort study. Circ Heart Fail 2020; 13: e007274. [DOI] [PubMed] [Google Scholar]
- 19. Tomasoni D, Inciardi RM, Lombardi CM, Tedino C, Agostoni P, Ameri P, Barbieri L, Bellasi A, Camporotondo R, Canale C, Carubelli V, Carugo S, Catagnano F, Dalla Vecchia LA, Danzi GB, Di Pasquale M, Gaudenzi M, Giovinazzo S, Gnecchi M, Iorio A, La Rovere MT, Leonardi S, Maccagni G, Mapelli M, Margonato D, Merlo M, Monzo L, Mortara A, Nuzzi V, Piepoli M, Porto I, Pozzi A, Sarullo F, Sinagra G, Volterrani M, Zaccone G, Guazzi M, Senni M, Metra M. Impact of heart failure on the clinical course and outcomes of patients hospitalized for COVID‐19. results of the cardio‐COVID‐Italy multicentre study. Eur J Heart Fail 2020; 22: 2238–2247. [DOI] [PubMed] [Google Scholar]
- 20. Phelps M, Christensen DM, Gerds T, Fosbøl E, Torp‐Pedersen C, Schou M, Køber L, Kragholm K, Andersson C, Biering‐Sørensen T, Christensen HC, Andersen MP, Gislason G. Cardiovascular comorbidities as predictors for severe COVID‐19 infection or death. Eur Heart J Qual Care Clin Outcomes 2021; 7: 172–180. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Data collected from all sites.


