Abstract
Objective
To assess the patterns in psychiatric admissions, referrals, and suicidal behavior before and during the COVID‐19 pandemic.
Methods
This study utilized health records from hospitals and Emergency Medical Services (EMS) covering 46% of the Danish population (n = 2,693,924). In a time‐trend study, we compared the number of psychiatric in‐patients, referrals to mental health services and suicidal behavior in years prior to the COVID‐19 pandemic to levels during the first lockdown (March 11 – May 17, 2020), inter‐lockdown period (May 18 – December 15, 2020), and second lockdown (December 16, 2020 – February 28, 2021).
Results
During the pandemic, the rate of psychiatric in‐patients declined compared to pre‐pandemic levels (RR = 0.95, 95% CI = 0.94 – 0.96, p < 0.01), with the largest decrease of 19% observed three weeks into the first lockdown. Referrals to mental health services were not significantly different (RR = 1.01, 95% CI = 0.92 – 1.10, p = 0.91) during the pandemic; neither was suicidal behavior among hospital contacts (RR = 1.04, 95% CI = 0.94 – 1.14, p = 0.48) nor EMS contacts (RR = 1.08, 95% CI = 1.00 – 1.18, p = 0.06). Similar trends were observed across nearly all age groups, sexes, and types of mental disorders examined. In the age group <18, an increase in the rate of psychiatric in‐patients (RR = 1.11, 95% CI = 1.07 – 1.15, p < 0.01) was observed during the pandemic; however, this did not exceed the pre‐pandemic, upwards trend in psychiatric hospitalizations in the age group <18 (p = 0.78).
Conclusion
The COVID‐19 pandemic has been associated with a decrease in psychiatric hospitalizations, while no significant change was observed in referrals to mental health services and suicidal behavior. Psychiatric hospitalizations among children and adolescents increased during the pandemic; however, this appears to be a continuation of a pre‐pandemic trend.
Keywords: COVID‐19, hospitalizations, psychiatry, referral and consultation, suicide
Significant Outcomes
The number of in‐patients at psychiatric clinics decreased throughout the COVID‐19 pandemic, especially during societal lockdowns.
Suicidal behavior and referrals to mental health services in the general population did not change significantly during the pandemic.
In the age group <18, a pre‐pandemic increase in admissions to psychiatric clinics continued during the pandemic.
Limitations
Registration of suicidal behavior might be of varying completeness, and the data do not enable distinction between completed suicides and attempted suicides.
Data do not include primary care providers and private clinics.
A longer pre‐exposure period would be desirable.
1. INTRODUCTION
The COVID‐19 pandemic caused by the SARS‐CoV‐2 virus has, as of August 2021, resulted in more than 200 million verified cases of SARS‐CoV‐2 infections and over 4.2‐million deaths associated with COVID‐19 have been registered globally. 1 The pandemic has put significant strain on health care systems and several reports have expressed concerns about decreased availability and potential inadequacy of mental health treatment as a result. 2 , 3 , 4 A deficit in psychiatric care during the pandemic is of special concern because of a deterioration in well‐being in the general population, as well as potential neuropsychiatric sequelae from COVID‐19, 5 , 6 , 7 both of which could be risk factors for increased psychiatric admission and suicide rates. 8
However, evidence regarding the consequences of the pandemic and associated lockdowns on psychiatric care and suicidal behavior remains scarce. 6 A systematic review from January 2021 identified only one published study reporting on admission rates to psychiatric clinics during the COVID‐19 pandemic. 9 The study found a decrease in psychiatric admissions, yet only investigated a 40‐day period during the initial pandemic in Italy. 10 Likewise, two British studies not included in the systematic review found a decrease in both referrals and admissions to mental health trusts; however, these studies were only based on data from single sites. 11 , 12 On the contrary, recent data from the United States show an increase in mental health conditions observed in emergency rooms (ERs) during COVID‐19. 13 Regarding suicidal behavior, a systematic review has suggested that suicide rates increased during previous pandemics 14 ; however, only limited long‐term data are available on suicidal behavior during the COVID‐19 pandemic. 15 , 16 Current evidence from Australia, 17 Massachusetts, 18 and Norway 19 suggests no changes in suicide rates during the pandemic while studies from the United Kingdom, 20 France, 21 and Peru 22 find a decrease in self‐harm, suicide attempts and suicides, respectively. On the contrary, recent data from Japan 23 show an increase in suicides the last months of the pandemic following an initial decline and data from the United States show an increase in suicide attempts registered in ERs. 13 A recent study on preliminary data from multiple countries found no evidence of increases in suicidal behavior in the early months of the COVID‐19 pandemic, 24 but no published studies have—to the best of our knowledge—probed trends in suicidal behavior extending beyond October 2020; thus, effects of recent pandemic waves and lockdowns have not been examined. Despite the fact that a mental disorder diagnosis represents a significant risk factor for death by suicide, 25 no identified studies have probed suicide patterns during the COVID‐19 pandemic among patients with pre‐existing mental disorders or assessed population‐level effects of COVID‐19 on patterns in referral and admission rates to mental health services.
In accordance with most previous studies, we hypothesized that the number of referrals to mental health services and in‐patients at psychiatric clinics decreased during the COVID‐19 pandemic, whereas suicidal behavior was unchanged. We utilized population‐based electronic health records from hospitals and Emergency Medical Services (EMSs) in two regions of Denmark covering 46% of the population to provide data on suicidal behavior during the COVID‐19 pandemic at one‐year follow‐up and unique, population‐based data on psychiatric admission patterns and referrals not previously reported in the literature.
1.1. Aims of the study
To provide and compare data on the number of in‐patients at psychiatric clinics, referrals to mental health services, as well as suicidal behavior (self‐harm, suicide attempts, and suicide) in years prior to and during the COVID‐19 pandemic. For secondary analyses, the data were further stratified according to pre‐existing mental disorders, age groups, and sex. Data on suicidal behavior were additionally stratified for method of self‐harm.
2. MATERIAL AND METHODS
2.1. Study design
We performed a population‐based, time‐trend cohort study using data from hospitals and EMS from The Capital Region of Denmark and Region Zealand, two administrative regions of Denmark. Hospital data were extracted as de‐identified population‐level data from electronic health records (EHR). Both regions utilize the same EHR system (EPIC, version 2019, Verona, Wisconsin, USA), which contains data from all hospital contacts in the regions. A total of 2,813,784 unique patients were registered in the EPIC EHR system as of March 1, 2021. The EPIC EHR system was implemented at all hospitals in the two regions from 2016 to 2017. Diagnoses in the EHRs—including codes for suicide and self‐harm—are defined and coded according to the ICD‐10 system by the responsible clinicians. Data from the EMS were extracted from the Prehospital Medical Record used since 2016 by the ambulance personnel when transporting a patient. 26
2.2. Setting
The Danish health care system is almost exclusively public funded with free access to care. National policies on COVID‐19 testing, restrictions and vaccinations have been nearly uniform across the country. The first case of COVID‐19 was confirmed in Denmark on February 27, 2020. The pandemic in Denmark has consisted of a first lockdown from March 11, 2020, a gradual reopening from May 18, 2020 and a second lockdown from December 16, 2020 that was still ongoing at the end of the study period. The first administration of COVID‐19 vaccines in Denmark began on December 27, 2020 and is currently ongoing.
2.3. Time period
Data on in‐patients at psychiatric clinics were gathered from January 1, 2018 to February 28, 2021. Hospital‐registered data on suicidal behavior (defined as suicides, suicide attempts, and self‐harm) were gathered from January 1, 2019 to February 28, 2021. Data on referrals were gathered from January 1, 2018 to February 28, 2021. EMS data on suicidal behavior were recorded from January 1, 2016 to February 28, 2021. Diagnostic data on mental disorders in the EPIC EHR system time‐stamped up to 20 years prior to hospitalization or suicidal behavior were included.
2.4. Outcome
Primary outcomes:
The number of hospitalized patients at psychiatric, in‐patient clinics prior to the pandemic (January 1, 2018 – March 10, 2020) as compared to numbers during the first lockdown (March 11, 2020 – May 17, 2020), the inter‐lockdown period (May 18, 2020 – December 15, 2020), and the second lockdown (December 16, 2020 – February 28, 2021).
The number of suicidal behavior events registered in hospital EHRs (ie, suicides, suicide attempts or self‐harm) (ICD‐10 codes: X60‐84) prior to the pandemic (Jan 1, 2019 – March 10, 2020) as compared to numbers during the first lockdown, the inter‐lockdown period, and the second lockdown.
Secondary outcomes:
The number of suicidal behavior events registered in the EMS records prior to the pandemic (January 1, 2016 – March 10, 2020) as compared to numbers during the first lockdown, the inter‐lockdown period, and the second lockdown.
The number of referrals to mental health services prior to the pandemic (January 1, 2018 – March 10, 2020) as compared to numbers during the first lockdown, the inter‐lockdown period, and the second lockdown.
The above outcomes stratified when possible by (1) sex, (2) age group, (3) psychiatric diagnosis and (4) method of self‐harm (see Table S1).
2.5. Data Collection
Anonymized, retrospective aggregate‐level data on the number of in‐patients at psychiatric clinics (per year and week) and diagnostic events of suicide, self‐harm, and suicide attempt (per year and week) stratified by sex, age, psychiatric diagnosis, and method of self‐harm were extracted from the EHR (see Methods S1 for additional information). A detailed search strategy is described in Table S1. Referrals to mental health services (per week) were extracted from EHRs and provided by The Capital Region of Denmark and therefore only covered this region. For data from EMS, entries mentioning “suicide” or “suicide attempt” were extracted by an algorithm alongside data on the patient's sex, date of birth, and time of ambulance call. This approach has previously been validated. 27 It was not possible to differentiate between suicides and suicide attempts in the available dataset.
2.6. Statistical analysis
The number of in‐patient at psychiatric clinics, suicidal behavior events and referrals are reported as weekly and annual counts. Levels and trends in the number of suicidal behavior events, in‐patients and referrals are compared between time periods using negative‐binomial models with a log link. For illustration purposes, smoothed curves were estimated using a natural cubic‐spline model with 20–32 degrees of freedom. For additional information on statistical modeling, see Methods S1. Analyses were stratified according to age groups, sex, and psychiatric diagnosis where possible. Two‐sided p < 0.05 was considered significant and 95% confidence intervals are reported. P‐values adjusted for multiple testing for secondary analyses were obtained using Holm's method and adjusted p‐values are reported in the manuscript. 28 Adjustment across all strata (ie, sex, diagnosis, and age group) and across all investigated time periods (ie, the pandemic, first lockdown, inter‐lockdown, and second lockdown) was done separately for each outcome (ie, referrals, in‐patients and suicidal behavior events in hospitals and EMS). Statistical analyses were conducted in R version 4.0 29 using the MASS package 30 for estimation of negative‐binomial models.
2.7. Ethical approval
The Ethics Committee of the Capital Region of Denmark waives approval for studies on anonymized aggregate‐level data (Section 14.2 of the Committee Act. 2; http://www.nvk.dk/english). Data authority approval was obtained according to Danish standards (P‐2020–962). Data management was conducted in accordance with the General Data Protection Regulation (GDPR) of the European Union. 31 Results from ≤5 patients are displayed as “≤5” to ensure data privacy.
2.8. Role of the funding source
The sponsors had no role in the acquisition of the data, interpretation of the results or the decision to publish the findings.
3. RESULTS
3.1. Overall, annual trends in psychiatric hospitalizations, referrals and suicidal behavior
The annual number of in‐patient at psychiatric clinics declined by −0.7% from 2018 to 2019 (14,126 vs. 14,021 in‐patients) and further by −1.9% from 2019 to 2020 (14,021 vs.13,749) (Table S2). The annual number of referrals to mental health service decreased by −2.4% from 2018 to 2019 (36,082 vs. 35,212) and increased by 3.6% from 2019 to 2020 (35,212 vs. 36,465). Hospital‐recorded suicidal behavior decreased by −6.6% from 2019 to 2020 (1080 vs. 1009 events) (Table S3). EMS‐registered suicidal behavior decreased by −7.6% from 2019 to 2020 (2382 vs. 2200) following a three‐year increase by 79.4% from 2016 to 2019 (1328 vs. 2382) (Table S4). The age group <18 years of age deviated from this pattern. In this age group, in‐patients increased by 3.2% from 2018 to 2019 (744 vs. 768) and further by 7.4% from 2019 to 2020 (768 vs. 825). Hospital‐recorded suicidal behavior in the age group <18 decreased by 4.4% from 2019 to 2020 (295 vs. 282); however, it reached 124 events by 28 of February of 2021, accounting for 46.1% of total suicidal behavior events. Most patients exhibiting suicidal behavior had pre‐existing mental disorders (Table S3). In the EMS data, the age group <18 accounted for 5.2% of suicidal behavior in 2019, 5.9% in 2020 and 9.0% in 2021 (January and February only) (Table S4).
3.2. The impact of the COVID‐19 pandemic on psychiatric hospitalizations
During the first lockdown, the weekly number of in‐patients at psychiatric clinics declined by −19% from week 10 to week 13 (1918 vs. 1554 in‐patients) and remained below the level of the preceding year for all but two weeks of the pandemic (Figure 1A). Overall, the rate of in‐patients was lower by −5.1% during the pandemic as compared to pre‐pandemic levels (RR = 0.95, CI = 0.94 – 0.96, p < 0.01) (Table 1). Compared to the pre‐lockdown period, the rate of in‐patients declined by −11% (RR = 0.89, CI = 0.87 – 0.90, p < 0.01) during the first lockdown, by −3% (RR = 0.97, CI = 0.96 – 0.98, p < 0.01) in the inter‐lockdown period and by −5% (RR = 0.95, CI = 0.93 – 0.97, p < 0.01) during the second lockdown (Table 1). Similar results were observed across nearly all age groups, sexes, and types of mental disorders examined. Of note, in the age group >80, no significant change was observed (RR = 0.98, CI = 0.93 – 1.03, p = 1.00), and in the age group <18, the rate of hospitalizations was increased by 11% (RR = 1.11, CI = 1.07 – 1.15, p < 0.01) during the pandemic (Figure 2A; Table S5). However, when comparing the rate of change in hospitalizations in the age group <18 prior to the pandemic to the rate of change during the pandemic, the increase in psychiatric hospitalizations during the pandemic did not significantly exceed the pre‐pandemic, upwards trend (p = 0.78) (Figure 2A; Table S6).
FIGURE 1.
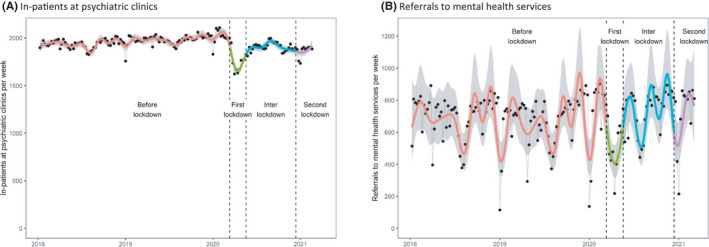
Trends in the number of in‐patients at psychiatric clinics and referrals to mental health services during COVID‐19. Black dots represent weekly numbers. Smoother curves are added using natural cubic splines. Grey areas represent 95% confidence intervals. (A) In‐patients at psychiatric clinics (B) Referrals to mental health services
TABLE 1.
Rate ratio for the number of psychiatric in‐patients, referrals to mental health services and suicidal behavior during the pandemic vs. pre‐pandemic a .
| Outcome | Pandemic vs. Pre‐pandemic | 1st lockdown vs. Pre‐pandemic | Inter lockdown vs. Pre‐pandemic | 2nd lockdown vs. Pre‐pandemic | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| RR | 95% CI | p‐value | RR | 95% CI | p‐value | RR | 95% CI | p‐value | RR | 95% CI | p‐value | |
| Psychiatric in‐patients | 0.95 | (0.94 – 0.96) | <0.0001 | 0.89 | (0.87 – 0.90) | <0.0001 | 0.97 | (0.96 – 0.98) | <0.0001 | 0.95 | (0.93 – 0.97) | <0.0001 |
| Referrals to mental health services | 1.01 | (0.92 – 1.10) | 0.9060 | 0.76 | (0.64 – 0.91) | 0.0021 | 1.07 | (0.97 – 1.20) | 0.1925 | 1.04 | (0.89 – 1.22) | 0.6560 |
| Suicidal behavior (hospital‐recorded) | 1.04 | (0.94 – 1.14) | 0.4768 | 1.00 | (0.84 – 1.19) | 0.9973 | 1.04 | (0.93 – 1.17) | 0.4710 | 1.05 | (0.88 – 1.25) | 0.5715 |
| Suicidal behavior (EMS‐recorded) b | 1.08 | (1.00 – 1.18) | 0.0580 | 1.03 | (0.87 – 1.22) | 0.7533 | 1.14 | (1.03 – 1.26) | 0.0146 | 1.00 | (0.85 – 1.16) | 0.9582 |
Abbreviations: CI, Confidence Interval; EMS, Emergency Medical Services; RR, Rate ratio.
The number of suicidal behavior events, in‐patients and referrals are compared between time periods using negative‐binomial models with a log link (see Methods S1). Analyses were stratified according to age groups, sex and psychiatric diagnosis where possible (see Table S3). Two‐sided p < 0.05 are considered significant and significant results are highlighted in bold.
These estimates are compared to 4 years prior to the pandemic, and during the pre‐pandemic period a gradual increase in the number of suicidal behavior events recorded at EMS where observed, which changed to a gradual decrease during the pandemic, as also depicted in Figure 3B.
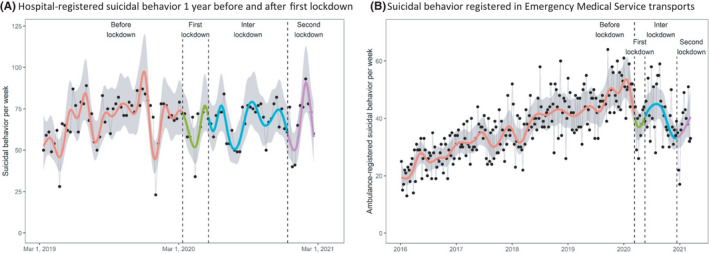
FIGURE 3.
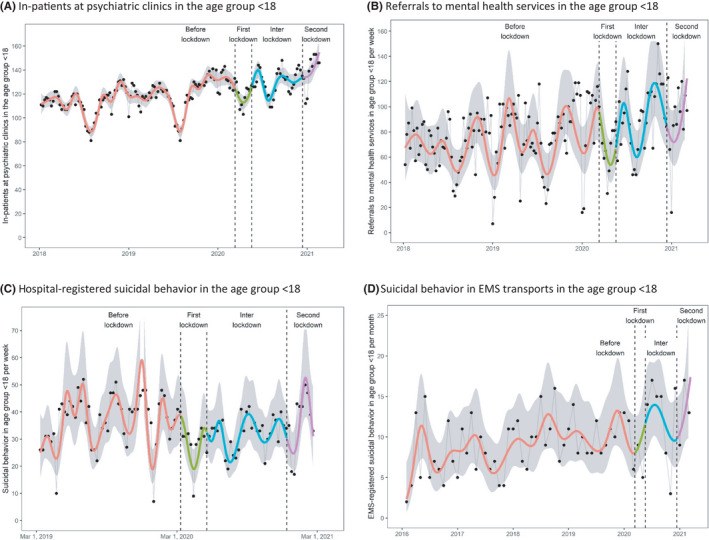
Trends in psychiatric hospitalizations, referrals and suicidal behavior in the age group <18 during COVID‐19. Black dots represent weekly numbers (monthly counts in D). Smoother curves are added using natural cubic splines. Grey areas represent 95% confidence intervals. (A) In‐patients at psychiatric clinics in the age group <18. (B) Referrals to mental health services in the age group <18. (C) Hospital‐registered suicidal behavior in the age group <18. (D) Suicidal behavior in EMS transports in the age group <18
3.3. The impact of COVID‐19 on referrals to mental health services
The weekly number of referrals to mental health services declined by 45% from week 10 (772) to week 13 (425) but normalized in the following weeks and were, overall, not significantly different to pre‐pandemic levels (RR = 1.01, CI = 0.92 – 1.10, p = 0.91) (Figure 1B; Table 1). Compared to the pre‐lockdown period, the rate of referrals was lower by −24% (RR = 0.76, CI = 0.64 – 0.91, p < 0.01) during the first lockdown, but not different in the inter‐lockdown period (RR = 1.07, CI = 0.97 – 1.20, p = 0.19) or the second lockdown (RR = 1.04, CI = 0.89 – 1.22, p = 0.66) (Table S5). The rate of referrals in the age group <18 during the pandemic was not significantly changed after adjustment for multiple testing (p = 0.07). Furthermore, the rate of change in the age group <18 during the pandemic was also not significantly different from the pre‐pandemic trend (Ratio = 1.37, CI = 0.97 – 1.93, p = 0.28) (Figure 2B, Table S6).
3.4. Hospital‐registered suicidal behavior during COVID‐19
The hospital‐registered rate of suicidal behavior events during the pandemic did not change significantly compared to the pre‐pandemic period (RR = 1.04, CI = 0.94 – 1.14, p = 0.48) (Figure 3A, Table 1); nor did it change during the first lockdown (RR = 1.00, CI = 0.84 – 1.19, p = 1.00), the inter‐lockdown period (RR = 1.04, CI = 0.93 – 1.17. p = 0.47) or second lockdown (RR = 1.05, CI = 0.88 – 1.25, p = 0.57). This pattern was observed for nearly all age groups and people with pre‐existing mental disorders (Table S5). An exception was the age group 18–29, where the rate of events increased by 41% during the first lockdown (RR = 1.41, CI = 1.14 – 1.74, p = 0.05); however, there was no significant difference between the pre‐pandemic and overall pandemic rate (p = 0.58), after adjusting for multiple testing (Table S5). Moreover, the trend in hospital‐recorded suicidal behavior during the pandemic as a whole showed a relative decline compared with the pre‐pandemic trend in both the general population (Ratio = 0.68, CI = 0.51 – 0.91, p = 0.01) and in the age group 18–29 (Ratio = 0.49, CI = 0.33 – 0.73, p = 0.02), among men (Ratio = 0.60, CI = 0.44 – 0.81, p = 0.03) and among patients with pre‐existing mental disorders (Ratio = 0.59, CI = 0.43 – 0.80, p = 0.02) after adjusting for multiple testing of secondary outcomes.
FIGURE 2.
Trends in suicidal behavior during COVID‐19. Black dots represent weekly numbers. Smoother curves are added using natural cubic splines. Grey areas represent 95% confidence intervals. (A) Hospital‐registered suicidal behavior 1 year before and after first lockdown. (B) Suicidal behavior registered in Emergency Medical Service transports
3.5. Patients transported in ambulances because of suicidal behavior during COVID‐19
The rate of total suicidal behavior events registered in EMS transports was not significantly different to pre‐pandemic levels (RR = 1.08, CI = 1.00 – 1.18, p = 0.06) (Figure 3B, Table S5). A gradual, pre‐pandemic increase in the number of suicidal behavior events changed to a significantly different, gradual decrease during the pandemic (Ratio = 0.74, CI = 0.62 – 0.87, p < 0.01) (Figure 3B, Table S6). Despite this, suicidal behavior events during the first (RR = 1.03, CI = 0.87 – 1.22, p = 0.75) and second lockdown (RR =1.00, CI =0.85 – 1.16, p = 0.96) were not different to pre‐pandemic levels, whereas an increase by 14% was observed in the inter‐lockdown period (RR = 1.14, CI = 1.03 – 1.26, p = 0.01); however, because of the gradual increase in EMS‐recorded suicidal behavior within the pre‐pandemic period these estimates do not exceed the levels observed the year prior to the pandemic (Figure 3B). In the age group <18, the weekly number of EMS‐registered events was low (range = 0–8) and thus, monthly counts were used and showed no significant difference in suicidal behavior after adjustment for multiple testing (p = 0.06) (Figure 2D; Table S5).
4. DISCUSSION
This population‐based study using data from hospital and Emergency Medical Service electronic health records covering almost half of the Danish population shows that, overall, the number of in‐patient at psychiatric clinics decreased after nation‐wide restrictions were imposed and remained at a slightly reduced level throughout the pandemic. This was most significant during full lockdowns; however, no compensatory increase in admissions was found during the gradual reopening of society. Suicidal behavior did not increase during the first year of the COVID‐19 pandemic; rather, the trend in suicidal behavior showed a relative decline during the pandemic as compared to the pre‐pandemic trend. Referrals to mental health services were not significantly different during the pandemic, except for a substantial, initial decline during the first lockdown.
Our data on psychiatric hospitalizations support findings in previous studies from Italy 10 and the United Kingdom, 11 , 12 where a decrease in referrals and admissions was observed during the first lockdown. Suicidal behavior—an important proxy for mental health—seems not to have been significantly changed in the general study population after the first year of the COVID‐19 pandemic. This finding agrees with previous studies from Australia, 17 Massachusetts, 18 Norway, 19 the United Kingdom, 20 France, 21 and Peru 22 finding no change in suicides or self‐harm during the COVID‐19 pandemic. Two studies from United States 13 and Japan 23 including data up until October 2020 show an increase in suicide attempts and suicides, respectively, which is not replicated in our Danish study population with an extended follow‐up period including data up until February 2021. Of note, data from the United States show racial disparities in suicidal behavior during the pandemic—an inequality that the present study does not include adequate data to investigate. 32
Concerns have been raised about the effects of the pandemic on mental health among children and adolescents. An increase in suicidal behavior among children and adolescent was partially observed in Japanese data, 23 while Australian and British data did not find similar trends. 17 , 20 In the present study, we did not observe increases in suicidal behavior or referrals to mental health services in the age group <18 after adjusting for multiple testing, in agreement with the Australian and British studies. However, we detected an increase in the number of in‐patients at psychiatric clinics in the age group <18 during the pandemic, which was primarily explained by an increase in hospitalizations among women. This increase did not differ significantly from the pre‐pandemic, upwards trends for psychiatric admissions for this age group and can thus not be attributed to the pandemic per se.
Strengths of this study include the up‐to‐date nature of the data, which extends the time period of suicidal behavior investigations during COVID‐19 by four months. Furthermore, this study provides the first long‐term, multi‐site investigation of psychiatric admissions and referrals during the pandemic. Data covered almost half of the Danish population in a freely accessible healthcare system, providing large scale data from a naturalistic setting. The weekly number of patients admitted to in‐patient psychiatric clinics ranged from 1524 to 1973 unique patients, corresponding well to the official number of in‐patient beds (1545) at psychiatric wards of the two regions. The latest, official figure for the number of suicide attempts recorded in the Danish registers for the investigated regions shows a total of 1366 attempts in 2018, 33 which is comparable to—albeit slightly higher than—the 2019 and 2020 numbers from the hospital EHRs.
Limitations include the fact that diagnostic coding in the EPIC EHR system might be of varying completeness, particularly in the initial years after the introduction of the EPIC system, and that it was not possible to differentiate between suicide attempts, self‐harm, and actual suicides; nor obtain data on the number of patients receiving the diagnosis of intentional self‐harm (ICD‐10: Y87), which was not listed in the EHR. Thus, the number of suicidal behavior events are underreported; however, consistently so throughout the period. Deaths by suicide are registered in the Danish Cause of Death Register, 34 which could not be included in this study. However, our conclusion agrees with preliminary data from the Danish Health Authorities, showing no increases in completed suicides, with 552 completed suicides in 2020 compared to 600 and 582 in 2019 and 2018, respectively. 35 Furthermore, a selection bias might arise from the fact that contacts in primary care and private clinics are not recorded in the EHR system. Misclassification bias might arise from imprecise diagnosis of suicide attempts by clinicians, but as the above‐mentioned, overall trend is identified in data from both EMS records and hospital EHRs, we consider this bias limited. An increased pre‐exposure period might be desirable and the results from short time periods, such as the lockdown periods, should be interpreted with caution. The generalizability of the findings could be strengthened by future studies in other countries. Finally, the findings are observational in nature and a direct causal relationship between the pandemic/lockdowns and changes in the psychiatric outcomes cannot be established with absolute certainty. Thus, our data do not elucidate the underlying mechanism causing these associations. Changes in help‐seeking behavior during the pandemic might result in psychiatric admissions and referrals not to be increased; however, we could not include population prevalence of psychiatric symptoms not leading to hospital contacts or referrals.
In this study, we show that the number of psychiatric admissions has decreased significantly throughout the COVID‐19 pandemic, especially during societal lockdowns. Even though the reason for this decrease is not established, decreased help‐seeking behavior could be one of several explanations and increased outreach efforts could potentially counter this trend. Suicidal behavior and referrals to mental health services appear not to have been significantly changed during the pandemic at one‐year follow‐up. However, long‐term consequences are still unexplored and a potential financial crisis after the pandemic could affect the general mental health in the population, including suicidal behavior.
CONFLICT OF INTEREST
The authors declare that there are no conflicts of interest.
AUTHOR CONTRIBUTIONS
TBR and MEB conceived and designed the study. TBR, SNFB, FF, and HCC collected the data. RHBC conducted the statistical analyses. TBR and MEB drafted the manuscript. All authors edited and approved the final version of the manuscript.
PEER REVIEW
The peer review history for this article is available at https://publons.com/publon/10.1111/acps.13369.
Supporting information
Supplementary Material
ACKNOWLEDGMENTS
We thank Christian Brandstrup Starup and Line Meyhoff Aastrup for assistance with data extraction from the EPIC EHR. We furthermore thank Aske Skouboe and Jacob Bille Krogh for providing additional data on referrals, invaluable input and fruitful discussions. The research was funded by an unrestricted grant from The Lundbeck Foundation (grant number R268‐2016‐3925) and the Novo Nordisk Foundation (grant number NNF21OC0067769).
Rømer TB, Christensen RHB, Blomberg SN, Folke F, Christensen HC, Benros ME. Psychiatric Admissions, Referrals, and Suicidal Behavior Before and During the COVID‐19 Pandemic in Denmark: A Time‐Trend Study. Acta Psychiatr Scand. 2021;144:553–562. 10.1111/acps.13369
DATA AVAILABILITY STATEMENT
All presented data are available to Danish researchers after approval of access from the data accessor authorities.
REFERENCES
- 1.WHO Coronavirus Disease (COVID‐19) Dashboard. Accessed August 6, 2021. https://covid19.who.int
- 2. Bojdani E, Rajagopalan A, Chen A, et al. COVID‐19 pandemic: impact on psychiatric care in the United States. Psychiatry Res. 2020;289: doi: 10.1016/j.psychres.2020.113069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Carpiniello B, Tusconi M, Zanalda E, et al. Psychiatry during the Covid‐19 pandemic: a survey on mental health departments in Italy. BMC Psychiatry. 2020;20(1):593. doi: 10.1186/s12888-020-02997-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Del Rio C, Collins LF, Malani P. Long‐term Health Consequences of COVID‐19. JAMA. 2020;324(17):1723‐1724. doi: 10.1001/jama.2020.19719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Troyer EA, Kohn JN, Hong S. Are we facing a crashing wave of neuropsychiatric sequelae of COVID‐19? Neuropsychiatric symptoms and potential immunologic mechanisms. Brain Behav Immun. 2020;87:34‐39. doi: 10.1016/j.bbi.2020.04.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Vindegaard N, Benros ME. COVID‐19 pandemic and mental health consequences: systematic review of the current evidence. Brain Behav Immun. 2020;89:531‐542. doi: 10.1016/j.bbi.2020.05.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Pierce M, Hope H, Ford T, et al. Mental health before and during the COVID‐19 pandemic: a longitudinal probability sample survey of the UK population. The Lancet Psychiatry. 2020;7(10):883‐892. doi: 10.1016/S2215-0366(20)30308-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Reger MA, Stanley IH, Joiner TE. Suicide mortality and coronavirus disease 2019‐a perfect storm? JAMA Psychiatry. 2020;77(11):1093‐1094. doi: 10.1001/jamapsychiatry.2020.1060. [DOI] [PubMed] [Google Scholar]
- 9. Neelam K, Duddu V, Anyim N, Neelam J, Lewis S. Pandemics and pre‐existing mental illness: A systematic review and meta‐analysis. Brain Behav Immun Health. 2021;10:100177. doi: 10.1016/j.bbih.2020.100177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Clerici M, Durbano F, Spinogatti F, Vita A, De Girolamo G, Micciolo R. Psychiatric hospitalization rates in Italy before and during COVID‐19: did they change? An analysis of register data. Ir J Psychol Med. 2020;37(4):283‐290. doi: 10.1017/ipm.2020.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Abbas MJ, Kronenberg G, McBride M, et al. The early impact of the COVID‐19 pandemic on acute care mental health services. Psychiatric Services. 2021;72(3):242–246. doi: 10.1176/appi.ps.202000467 [DOI] [PubMed] [Google Scholar]
- 12. Butler M, Delvi A, Mujic F, et al. Reduced activity in an inpatient liaison psychiatry service during the first wave of the COVID‐19 pandemic: comparison with 2019 data and characterization of the SARS‐CoV‐2 positive cohort. Front Psychiatry. 2021;12:619550. doi: 10.3389/fpsyt.2021.619550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Holland KM, Jones C, Vivolo‐Kantor AM, et al. Trends in US emergency department visits for mental health, overdose, and violence outcomes before and during the COVID‐19 pandemic. JAMA Psychiatry. 2021;78(4):372. doi: 10.1001/jamapsychiatry.2020.4402 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Zortea TC, Brenna CTA, Joyce M, et al. The impact of infectious disease‐related public health emergencies on suicide, suicidal behavior, and suicidal thoughts: A systematic review. Crisis. 2020;1‐14. doi: 10.1027/0227-5910/a000753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. John A, Pirkis J, Gunnell D, Appleby L, Morrissey J. Trends in suicide during the covid‐19 pandemic. BMJ. 2020;371:m4352 . doi: 10.1136/bmj.m4352. [DOI] [PubMed] [Google Scholar]
- 16. Kahil K, Cheaito MA, El Hayek R, et al. Suicide during COVID‐19 and other major international respiratory outbreaks: a systematic review. Asian J Psychiatr. 2021;56:102509. doi: 10.1016/j.ajp.2020.102509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Leske S, Kõlves K, Crompton D, Arensman E, de Leo D. Real‐time suicide mortality data from police reports in Queensland, Australia, during the COVID‐19 pandemic: an interrupted time‐series analysis. The Lancet Psychiatry. 2021;8(1):58‐63. doi: 10.1016/S2215-0366(20)30435-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Faust JS, Shah SB, Du C, Li S‐X, Lin Z, Krumholz HM. Suicide deaths during the COVID‐19 stay‐at‐home advisory in Massachusetts, March to May 2020. JAMA Netw Open. 2021;4(1):e2034273. doi: 10.1001/jamanetworkopen.2020.34273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Qin P, Mehlum L. National observation of death by suicide in the first 3 months under COVID‐19 pandemic. Acta Psychiatr Scand. 2021;143(1):92‐93. doi: 10.1111/acps.13246. [DOI] [PubMed] [Google Scholar]
- 20. Carr MJ, Steeg S, Webb RT, et al. Effects of the COVID‐19 pandemic on primary care‐recorded mental illness and self‐harm episodes in the UK: a population‐based cohort study. Lancet Public Heal. 2021;6(2):e124‐e135. doi: 10.1016/S2468-2667(20)30288-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Olié E, Nogue E, Christine Picot M, Courtet P. Hospitalizations for suicide attempt during the first COVID‐19 lockdown in France. Acta Psychiatrica Scandinavica. 2021;143(6):535‐536. doi: 10.1111/acps.13296 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Calderon‐Anyosa RJC, Kaufman JS. Impact of COVID‐19 lockdown policy on homicide, suicide, and motor vehicle deaths in Peru. Prev Med (Baltim). 2021;143:106331. doi: 10.1016/j.ypmed.2020.106331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Tanaka T, Okamoto S. Increase in suicide following an initial decline during the COVID‐19 pandemic in Japan. Nat Hum Behav. 2021;5(2):229‐238. doi: 10.1038/s41562-020-01042-z. [DOI] [PubMed] [Google Scholar]
- 24. Pirkis J, John A, Shin S, et al. Suicide trends in the early months of the COVID‐19 pandemic: an interrupted time‐series analysis of preliminary data from 21 countries. The Lancet Psychiatry. 2021;8(7):579‐588. doi: 10.1016/S2215-0366(21)00091-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Plana‐Ripoll O, Pedersen CB, Agerbo E, et al. A comprehensive analysis of mortality‐related health metrics associated with mental disorders: a nationwide, register‐based cohort study. Lancet. 2019;394(10211):1827‐1835. doi: 10.1016/S0140-6736(19)32316-5. [DOI] [PubMed] [Google Scholar]
- 26. Lindskou TA, Mikkelsen S, Christensen EF, et al. The Danish prehospital emergency healthcare system and research possibilities. Scand J Trauma Resusc Emerg Med. 2019;27(1):100. doi: 10.1186/s13049-019-0676-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Blomberg SNF, Rosenkrantz OCM, Lippert F, Collatz CH. Injury from electric scooters in Copenhagen: a retrospective cohort study. BMJ Open. 2019;9(12):33988. doi: 10.1136/bmjopen-2019-033988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Holm S. A simple sequentially rejective multiple test procedure on JSTOR. Scand J Stat. 1979;6(2):65‐70. Accessed June 17, 2021. https://www.jstor.org/stable/4615733 [Google Scholar]
- 29.Team RC. R: A language and environment for statistical computing. Published online 2020. https://www.r‐project.org/
- 30. Venables WN, Ripley BD. Modern applied statistics with S. 4th edn. Springer; 2002. [Google Scholar]
- 31.General Data Protection Regulation (GDPR) Compliance Guidelines. Accessed March 17, 2021. https://gdpr.eu/
- 32. Bray MJC, Daneshvari NO, Radhakrishnan I, et al. Racial differences in statewide suicide mortality trends in maryland during the coronavirus disease 2019 (COVID‐19) pandemic. JAMA Psychiatry. 2021;78(4):444. doi: 10.1001/jamapsychiatry.2020.3938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Center for Selvmordsforskning. Accessed March 24, 2021. https://statistik.selvmordsforskning.dk/
- 34. Helweg‐Larsen K. The Danish register of causes of death. Scand J Public Health. 2011;39(7):26‐29. doi: 10.1177/1403494811399958. [DOI] [PubMed] [Google Scholar]
- 35.The Ministry of Health and the Elderly. Committee on Health and the Eldery, The Danish Parliament, Answer to Quesiton 510. 2021; https://www.ft.dk/samling/20201/almdel/suu/spm/510/svar/1741735/2327521.pdf?fbclid=IwAR2r_2MsGVgYQFGKoEG8qJEqn7Ud5eW1Rhkl4e_opx6G5x7CrAZ_2LsQnXA
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Material
Data Availability Statement
All presented data are available to Danish researchers after approval of access from the data accessor authorities.


