Abstract
Aim
This study aims to clarify the construct and criterion‐related validity of the Questionnaire for Older Senior Citizens (QO) during the COVID‐19 pandemic.
Methods
This cross‐sectional study was conducted in Japan between November 11, 2020 and January 10, 2021. Of the 1645 (63.5%) older adults who responded, data from 900 participants were analyzed. First, we conducted an exploratory factor analysis (EFA) among older‐older adults (aged ≥75 years) and extracted the factors. Next, we conducted a confirmatory factor analysis (CFA) using structural equation modeling. We also conducted this analysis among younger‐older adults (aged ≥65 and <75 years) using the same model. Moreover, we compared each item of the QO with frailty status.
Results
Results of the EFA revealed six factors: social conditions and lifestyle, subjective conditions, cognitive functions, physical activity, oral functions, and physical functions. The results of the CFA were as follows: comparative fit index (CFI) = 0.971, adjusted goodness of fit index (AGFI) = 0.978, root mean square error of approximation (RMSEA) = 0.018, and standardized root mean square residual (SRMR) = 0.030. The results among the younger‐older adults were as follows: CFI = 0.880, AGFI = 0.940, RMSEA = 0.037, and SRMR = 0.048. Many QO items were significantly associated with frailty (P < 0.05).
Conclusions
Among the older‐older adults group, the model used for the QO has sufficient suitability and construct validity; among the younger‐older adults group, there also is sufficient questionnaire suitability. Moreover, the QO has criterion related validity with frailty. Geriatr Gerontol Int 2021; 21: 1018–1025.
Keywords: construct validity, COVID‐19, criterion‐related validity, frailty, Questionnaire for Older Senior Citizens
Introduction
Japan is an aging society, with 17.6 million (13.9%) people between 65 and 74 years old, and 18.0 million (14.2%) aged 75 or older. 1 The proportion of the population aged 65 or older is predicted to increase to 30% (reaching 35.3%) by 2040. This will affect healthcare systems, as they work differently for older adults (especially for those over 75 years old). For people over 75 years old, maintaining quality of life is particularly important, alongside providing treatments and preventing disease. Therefore, the Questionnaire for Older Senior Citizens (QO) was developed by the Japanese Ministry of Health, Labor, and Welfare 2 to comprehensively evaluate health conditions and lifestyles based on participant characteristics (e.g., frailty), in contrast to conventional questionnaires that assess metabolic syndromes. However, its validity and reliability have not yet been verified.
Frailty is considered relative to deficit accumulation 3 and has multidimensional issues related to its physical, 4 psychological, and social domains. 5 Physical frailty is used as a phenotype of frailty and is operationally defined based on weight loss, muscle weakness, increased fatigue, decreased walking ability, and a reduction in activity. 4 In the psychological and cognitive domain, frailty is defined when a person exhibits declining physical and cognitive functions, 6 while social frailty involves being without interaction with the local community, which may worsen life prognosis, similar to physical frailty. 7 Living alone and not leaving the house and/or interacting with other people also leads to a decline in physical functions. 8 In addition to these three domains, oral frailty is defined as poor oral status and is a strong predictor of physical frailty, sarcopenia, the need for long‐term care, and mortality. 9 Given this information, the QO may be useful for assessing the multidimensional aspects of frailty.
Although the QO has been a healthcare requirement for ascertaining conditions in older adults since April 2020, 10 the assessment process has been delayed because of the spread of coronavirus disease 2019 (COVID‐19). In Japan, the state of emergency was extended to all 47 prefectures on April 16, 2020. 11 Therefore, the validity of the QO has not yet been confirmed.
Clarifying the QO's validity is useful because it can guide policymakers and healthcare professionals regarding public health strategies in Japan. Although infection control was required, we conducted the QO among community‐dwelling older adults during the COVID‐19 pandemic through a survey. As such, this study aimed to clarify the construct and criterion‐related validity of the QO with frailty.
Methods
Study design and participants
This cross‐sectional study was conducted between November 11, 2020 and January 10, 2021 in Takasaki City, Gunma Prefecture, Japan. Eligible participants were 2590 community‐dwelling people aged 65 or above who lived in local housing in 14 community areas of Takasaki City and received regular support from local volunteers or support professionals. Those needing regular support were defined as such by supporters, based on their daily condition. Participants who had applied for long‐term care insurance or who had cancer or had suffered a stroke were excluded. Surveys, instructions, and written consent forms were distributed by local volunteers or support professionals, which were all returned by mail. In total, 1645 older adults returned the survey forms with written consent, a total response rate of 63.5%. Approximately 1387 older adults answered all items in the QO. The number of older adults who met the exclusion criteria (having applied to long‐term care insurance or having had a stroke or cancer) was 487. Therefore, 900 participants were included in the construct validity analysis (Fig. 1).
Figure 1.
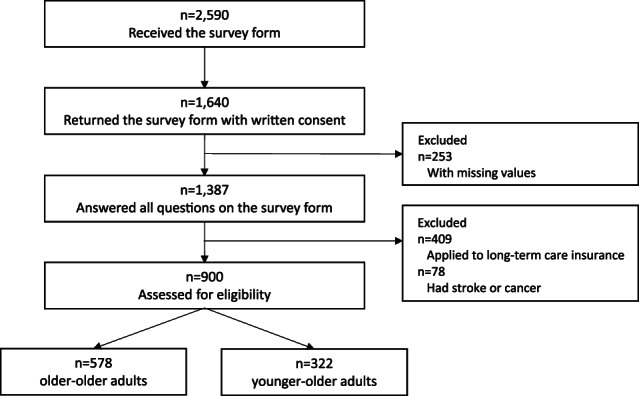
Flow diagram of the participants enrolled in the study.
This study was approved by the Research Ethics Committee of Takasaki University of Health and Welfare (approval number 2009) and was conducted in accordance with the Declaration of Helsinki. The purpose and the handling of the information were explained to all participants, and signed written consent was obtained. This study was registered with the University Hospital Medical Information Network (UMIN000040335).
Measurements
The survey included the following: sociodemographic characteristics (e.g., age, sex, morbidity, living arrangements [with cohabitant or alone]) and the QO. Responses were either yes/no or ratings on a 3‐ to 5‐point Likert scale. 2 Frailty was assessed using the Frailty Screening Index (FSI) 12 via a questionnaire and did not require face‐to‐face measurement. Frailty status was based on the participant's score: a score of ≥3 was defined as frail, 1 to 2 as pre‐frail, and 0 as robust.
Statistical analysis
Participants were divided into the older‐older adults group (aged 75 years and over) and the younger‐adults group (aged 65 to 74 years) and an older‐older adults group (aged 75 years or over), because the QO was developed to assess health conditions of people aged 75 years and older.
Descriptive statistics were run on sociodemographics and results from the QO. First, an exploratory factor analysis (EFA) was conducted on the older‐older adults group to identify dimensionality among the QO items. A principal axis factor analysis with a Promax rotation method with Kaiser normalization was used. The Kaiser–Guttman eigenvalue‐greater‐than‐one rule was used to select the number of factors to be extracted. As the QO was structured using multidimensional frailty concepts that had been previously established, items could not be dropped. Therefore, items with a factor loading of >0.20 were adopted.
Second, among the older‐ and younger‐older adults groups, a confirmatory factor analysis (CFS) using structural equation modeling (SEM) was conducted on the QO model using EFA. To evaluate model fit, a comparative fit index (CFI), adjusted goodness of fit index (AGFI), root mean square error of approximation (RMSEA), and standardized root mean square residual (SRMR) were used.
To indicate criterion‐related validity with frailty, the association between the QO and frailty status among the older‐ and younger‐older adults groups was assessed. Because the QO was not developed for calculating a total score with all items, each of the QO response items was compared with frailty status using a chi‐square test or Fisher's exact test. QO items 6, 7, and 9 are part of the FSI; therefore, these items were excluded from the analysis for criterion‐related validity with frailty.
Statistical analyses were performed using IBM SPSS Statistics Version 26 for Windows (IBM Corp., Armonk, NY, USA), IBM SPSS Amos 24.0, (IBM Corp., Armonk, NY, USA), and R version 4.0.0, with P < 0.05 indicating statistical significance.
Results
Table 1 shows the participants' sociodemographic data. The mean age for the older‐older adults group (n = 578) was 81.1 ± 4.4 years, and 451 participants (78.0%) were women. The most common disease was hypertension (n = 272, 47.0%), followed by dyslipidemia (n = 88, 15.2%), osteoporosis (n = 84, 14.5%), and heart disease (n = 84, 14.5%). A total of 192 participants had multimorbidity (33.2%), and 349 were living alone (60.4%). The mean age of the younger‐older adults group (n = 322) was 71.0 ± 2.4 years, and 231 participants (71.7%) were women. The most common disease was hypertension (n = 129, 40.1%), followed by dyslipidemia (n = 55, 17.1%) and diabetes mellitus (n = 35, 10.9%). A total of 79 participants had multimorbidity (24.5%), and 123 were living alone (38.2%).
Table 1.
Participants' sociodemographic characteristics
| Characteristics | Total n = 900 | Older‐older adults n = 578 | Younger‐older adults n = 322 |
|---|---|---|---|
| Age, mean ± SD (years) | 77.5 ± 6.2 | 81.1 ± 4.4 | 71.0 ± 2.4 |
| Female, n (%) | 682 (74.5) | 451 (78.0) | 231 (71.7) |
| Morbidity, n (%) | |||
| Hypertension | 401 (45.3) | 272 (47.1) | 129 (40.1) |
| Osteoporosis | 110 (14.6) | 84 (14.5) | 26 (8.1) |
| Heart disease | 114 (13.8) | 84 (14.5) | 30 (9.3) |
| Dyslipidemia | 143 (13.8) | 88 (15.2) | 55 (17.1) |
| Diabetes mellitus | 108 (13.3) | 73 (12.6) | 35 (10.9) |
| Multimorbidity, n (%) | 271 (35.8) | 192 (33.2) | 79 (24.5) |
| Living, n (%) | |||
| With cohabitant | 428 (44.7) | 229 (39.6) | 199 (61.8) |
| Alone | 472 (55.3) | 349 (60.4) | 123 (38.2) |
Multimorbidity was considered when a participant had more than one chronic disease.
Table 2 shows the results for each QO item. For each item, the higher the number, the worse the respondent's condition; for the number of responses, see Table 2. EFA for the QO was performed using principal axis factor analysis with a Promax rotation method in the older‐older adults group. Six factors with an eigenvalue of >1.0 were extracted based on the Kaiser–Guttman rule. The Kaiser–Meyer–Olkin measure of sampling adequacy was calculated at 0.609, and Bartlett's test of sphericity was significant (P < 0.001). We confirmed that all communalities were between 0 and 1, and there was no Heywood case. Factor loadings >0.20 were assigned to each factor (Table 3). Factor 1 included four items: 3, 12, 14, and 15 (social conditions and lifestyle); Factor 2 involved items 1 and 2 (subjective conditions); Factor 3 involved items 10 and 11 (cognitive functions); Factor 4 involved items 9 and 13 (physical activity); Factor 5 involved items 4 and 5 (oral functions); and Factor 6 involved items 6, 7, and 8 (physical functions).
Table 2.
Results for the Questionnaire for Older Senior Citizens, n (%)
| No | Item | Response | Total | Older‐older adults | Younger‐older adults |
|---|---|---|---|---|---|
| n = 900 | n = 578 | n = 322 | |||
| 1 | How is your health? | 1. Good | 160 (17.8) | 98 (17.0) | 62 (19.3) |
| 2. Fairly good | 238 (26.4) | 150 (26.0) | 88 (27.3) | ||
| 3. Normal | 431 (47.9) | 275 (47.6) | 156 (48.5) | ||
| 4. Not very good | 64 (7.1) | 48 (8.3) | 16 (5.0) | ||
| 5. Bad | 7 (0.8) | 7 (1.2) | 0 (0.0) | ||
| 2 | Are you satisfied with your daily life? | 1. Satisfied | 352 (39.1) | 234 (40.5) | 118 (36.6) |
| 2. Somewhat satisfied | 460 (51.1) | 292 (50.5) | 168 (52.2) | ||
| 3. Somewhat dissatisfied | 82 (9.1) | 48 (8.3) | 34 (10.6) | ||
| 4. Dissatisfied | 6 (0.7) | 4 (0.7) | 2 (0.6) | ||
| 3 | Do you consistently eat three meals a day? | 1. Yes | 845 (93.9) | 549 (95.0) | 296 (91.9) |
| 2. No | 55 (6.1) | 29 (5.0) | 26 (8.1) | ||
| 4 | Has it become more difficult to eat hard food than it was 6 months ago? | 1. No | 663 (73.7) | 402 (69.5) | 261 (81.1) |
| 2. Yes | 237 (26.3) | 176 (30.5) | 61 (18.9) | ||
| 5 | Do you sometimes choke on tea or soup? | 1. No | 691 (76.8) | 440 (76.1) | 251 (78.0) |
| 2. Yes | 209 (23.2) | 138 (23.9) | 71 (22.1) | ||
| 6 | Have you lost 2–3 kg or more in the past 6 months? | 1. No | 827 (91.9) | 525 (90.8) | 302 (93.8) |
| 2. Yes | 73 (8.1) | 53 (9.2) | 20 (6.2) | ||
| 7 | Do you think you walk slower than before? | 1. No | 461 (51.2) | 251 (43.4) | 210 (65.2) |
| 2. Yes | 439 (48.8) | 327 (56.6) | 112 (34.8) | ||
| 8 | Have you fallen in the past year? | 1. No | 747 (83.0) | 481 (83.2) | 266 (82.6) |
| 2. Yes | 153 (17.0) | 97 (16.8) | 56 (17.4) | ||
| 9 | Do you take a walk to exercise at least once a week? | 1. Yes | 675 (75.0) | 431 (74.6) | 244 (75.8) |
| 2. No | 225 (25.0) | 147 (25.4) | 78 (24.2) | ||
| 10 | Are you told that you are forgetful, with comments such as “You are always telling me the same thing”? | 1. No | 806 (89.6) | 512 (88.6) | 294 (91.3) |
| 2. Yes | 94 (10.4) | 66 (11.4) | 28 (8.7) | ||
| 11 | Do you sometimes forget what day and month it is that day? | 1. No | 724 (80.4) | 458 (79.2) | 266 (82.6) |
| 2. Yes | 176 (19.6) | 120 (20.8) | 56 (17.4) | ||
| 12 | Do you smoke cigarettes? | 1. No, I do not smoke | 743 (82.6) | 499 (86.3) | 244 (75.8) |
| 2. I quit smoking | 99 (11.0) | 53 (9.2) | 46 (14.3) | ||
| 3. Yes, I smoke | 58 (6.4) | 26 (4.5) | 32 (9.9) | ||
| 13 | Do you go out at least once a week? | 1. Yes | 865 (96.1) | 548 (94.8) | 317 (98.5) |
| 2. No | 35 (3.9) | 30 (5.2) | 5 (1.6) | ||
| 14 | Are you normally in close contact with family and friends? | 1. Yes | 843 (93.7) | 548 (94.8) | 295 (91.6) |
| 2. No | 57 (6.3) | 30 (5.2) | 27 (8.4) | ||
| 15 | Do you have anyone to talk to if you feel unwell? | 1. Yes | 850 (94.4) | 547 (94.6) | 303 (94.1) |
| 2. No | 50 (5.6) | 31 (5.4) | 19 (5.9) |
Table 3.
Result on exploratory factor analysis for the Questionnaire for Older Senior Citizens
| No | Item | Factors | |||||
|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | ||
| 14 | Are you normally in close contact with family and friends? | 0.915 | 0.019 | −0.085 | 0.013 | 0.087 | −0.023 |
| 15 | Do you have anyone to talk to if you feel unwell? | 0.546 | −0.085 | 0.045 | −0.014 | 0.008 | −0.005 |
| 3 | Do you consistently eat three meals a day? | 0.317 | 0.172 | 0.102 | 0.023 | −0.251 | 0.111 |
| 12 | Do you smoke cigarettes? | 0.231 | 0.017 | 0.119 | −0.013 | −0.071 | −0.045 |
| 1 | How is your health? | −0.027 | 0.695 | −0.007 | 0.046 | 0.168 | −0.098 |
| 2 | Are you satisfied with your daily life? | 0.008 | 0.611 | −0.019 | −0.110 | −0.092 | 0.084 |
| 11 | Do you sometimes forget what day and month it is that day? | 0.105 | −0.002 | 0.697 | 0.027 | 0.047 | −0.103 |
| 10 | Are you told that you are forgetful, with comments such as “You are always telling me the same thing”? | −0.028 | −0.044 | 0.363 | −0.047 | 0.119 | 0.158 |
| 9 | Do you take a walk to exercise at least once a week? | −0.055 | −0.036 | −0.001 | 0.661 | −0.054 | 0.000 |
| 13 | Do you go out at least once a week? | 0.182 | −0.083 | −0.001 | 0.272 | −0.016 | 0.093 |
| 5 | Do you sometimes choke on tea or soup? | 0.002 | −0.021 | 0.058 | −0.119 | 0.303 | 0.136 |
| 4 | Has it become more difficult to eat hard food than it was 6 months ago? | −0.029 | 0.018 | 0.077 | 0.015 | 0.255 | −0.047 |
| 8 | Have you fallen in the past year? | −0.007 | −0.022 | −0.009 | 0.015 | 0.082 | 0.368 |
| 7 | Do you think you walk slower than before? | −0.052 | 0.145 | 0.052 | 0.112 | 0.213 | 0.245 |
| 6 | Have you lost 2–3 kg or more in the past 6 months? | −0.035 | 0.162 | −0.050 | 0.048 | −0.103 | 0.202 |
A principal axis factor analysis with a rotation method of Promax with Kaiser normalization was used.
We structured the QO model to comprehensively assess health conditions, assuming that the six factors extracted by the EFA were components of health conditions. The results of the CFA using SEM among the older‐older adults group were as follows: CFI = 0.971, AGFI = 0.978, RMSEA = 0.018, and SRMR = 0.030 (Fig. 2a). Meanwhile, the results for the younger‐older adults group were as follows: CFI = 0.880, AGFI = 0.940, RMSEA = 0.037, and SRMR = 0.048 (Fig. 2b).
Figure 2.
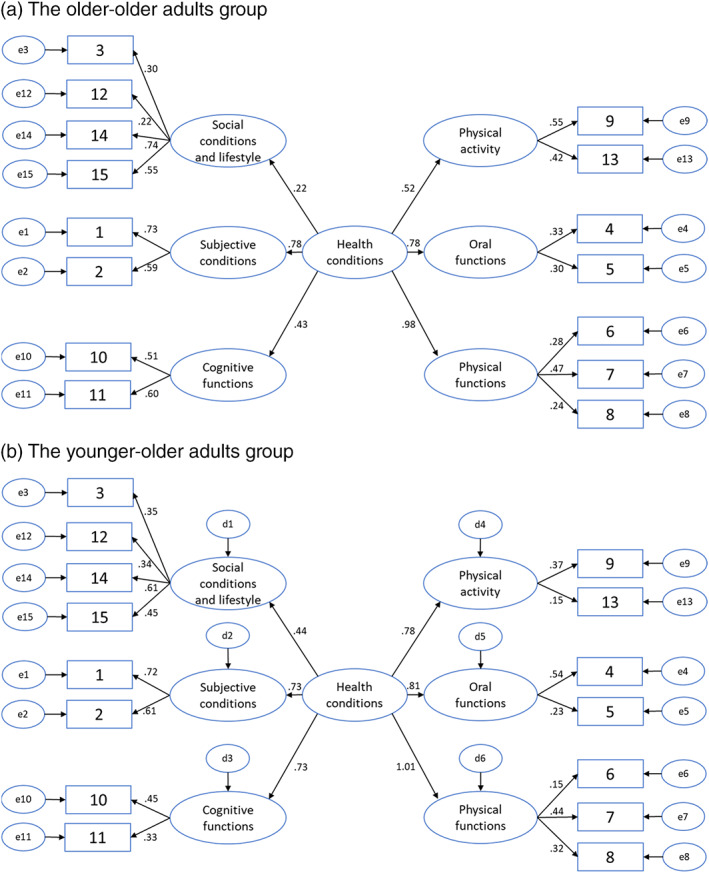
Confirmation factor analysis using structural equation modeling for the Questionnaire for Older Senior Citizens. (a) Among the older‐older adults group, the results of the CFA using SEM were as follows: CFI = 0.971, AGFI = 0.978, RMSEA = 0.018, SRMR = 0.030. (b) Among the younger‐older adults group, the results of the CFA using SEM were as follows: CFI = 0.880, AGFI = 0.940, RMSEA = 0.037, and SRMR = 0.048. CFA, confirmatory factor analysis; SEM, structural equation modeling.
To indicate criterion‐related validity with frailty, 888 participants who were able to fully complete the FSI were analyzed. The association between the QO and frailty status is presented in Table 4. For the older‐ and younger‐older adults groups, many items of the QO had significant associations with frailty (P < 0.05). The items for choking, smoking, and having someone to talk to if feeling unwell had no statistically significant association with frailty.
Table 4.
Association between the Questionnaire for Older Senior Citizens and frailty status, n (%)
| No | Item | Response | Older‐older adults n = 568 | Younger‐older adults n = 320 | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Robust | Pre‐frail | Frail | P‐value | Robust | Pre‐frail | Frail | P‐value | |||
| n = 173 | n = 344 | n = 51 | n = 146 | n = 157 | n = 17 | |||||
| 1 | How is your health? | 1. Good | 48 (27.8) | 47 (13.7) | 0 (0.0) | 0.000 | 44 (30.1) | 17 (10.8) | 0 (0.0) | 0.000 |
| 2. Fairly good | 51 (29.5) | 82 (23.8) | 14 (27.5) | 36 (24.6) | 49 (31.2) | 3 (17.6) | ||||
| 3. Normal | 72 (41.6) | 182 (52.9) | 20 (39.2) | 62 (42.5) | 85 (54.1) | 8 (47.1) | ||||
| 4. Not very good | 2 (1.2) | 30 (8.7) | 13 (25.5) | 4 (2.7) | 6 (3.8) | 6 (35.3) | ||||
| 5. Bad | 0 (0.0) | 3 (0.9) | 4 (7.8) | 0 (0.0) | 0 (0.0) | 0 (0.0) | ||||
| 2 | Are you satisfied with your daily life? | 1. Satisfied | 82 (47.4) | 137 (39.8) | 9 (17.6) | 0.001 | 64 (43.8) | 51 (32.5) | 2 (11.8) | 0.000 |
| 2. Somewhat satisfied | 83 (48) | 174 (50.6) | 33 (64.7) | 74 (50.7) | 85 (54.1) | 9 (52.9) | ||||
| 3. Somewhat dissatisfied | 8 (4.6) | 31 (9.0) | 8 (15.7) | 8 (5.5) | 21 (13.4) | 4 (23.5) | ||||
| 4. Dissatisfied | 0 (0) | 2 (0.6) | 1 (2.0) | 0 (0.0) | 0 (0.0) | 2 (11.8) | ||||
| 3 | Do you consistently eat 3 meals a day? | 1. Yes | 168 (97.1) | 327 (95) | 45 (88.2) | 0.037 | 135 (92.5) | 145 (92.4) | 14 (82.3) | 0.336 |
| 2. No | 5 (2.9) | 17 (4.9) | 6 (11.8) | 11 (7.5) | 12 (7.6) | 3 (17.6) | ||||
| 4 | Has it become more difficult to eat hard food than it was 6 months ago? | 1. No | 135 (78.0) | 230 (66.9) | 32 (62.7) | 0.017 | 127 (87.0) | 124 (79) | 8 (47.1) | 0.000 |
| 2. Yes | 38 (22.0) | 114 (33.1) | 19 (37.3) | 19 (13.0) | 33 (21) | 9 (52.9) | ||||
| 5 | Do you sometimes choke on tea or soup? | 1. No | 136 (78.6) | 259 (75.3) | 37 (72.5) | 0.584 | 119 (81.5) | 119 (75.8) | 11 (64.7) | 0.200 |
| 2. Yes | 37 (21.4) | 85 (24.7) | 14 (27.5) | 27 (18.5) | 38 (24.2) | 6 (35.3) | ||||
| 8 | Have you fallen in the past year? | 1. No | 150 (86.7) | 284 (82.5) | 37 (72.5) | 0.059 | 132 (90.4) | 119 (75.8) | 13 (76.5) | 0.003 |
| 2. Yes | 23 (13.3) | 60 (17.4) | 14 (27.5) | 14 (9.6) | 38 (24.2) | 4 (23.5) | ||||
| 10 | Are you told that you are forgetful, with comments such as “you are always telling me the same thing”? | 1. No | 163 (94.2) | 300 (87.2) | 39 (76.5) | 0.001 | 140 (95.9) | 138 (87.9) | 14 (82.3) | 0.020 |
| 2. Yes | 10 (5.8) | 44 (12.8) | 12 (23.5) | 6 (4.1) | 19 (12.1) | 3 (17.6) | ||||
| 11 | Do you sometimes forget what day and month it is that day? | 1. No | 153 (88.4) | 264 (76.7) | 33 (64.7) | 0.000 | 124 (84.9) | 128 (81.5) | 12 (70.6) | 0.306 |
| 2. Yes | 20 (11.6) | 80 (23.3) | 18 (35.3) | 22 (15.1) | 29 (18.5) | 5 (29.4) | ||||
| 12 | Do you smoke cigarettes? | 1. No, I do not smoke | 154 (89) | 291 (84.6) | 45 (88.2) | 0.628 | 115 (78.8) | 115 (73.3) | 12 (70.6) | 0.326 |
| 2. I quit smoking | 14 (8.1) | 34 (9.9) | 4 (7.8) | 22 (15.1) | 21 (13.4) | 3 (17.6) | ||||
| 3. Yes, I smoke | 5 (2.9) | 19 (5.5) | 2 (3.9) | 9 (6.2) | 21 (13.4) | 2 (11.8) | ||||
| 13 | Do you go out at least once a week? | 1. Yes | 170 (98.3) | 322 (93.6) | 46 (90.2) | 0.026 | 143 (97.9) | 156 (99.4) | 16 (94.1) | 0.138 |
| 2. No | 3 (1.7) | 22 (6.4) | 5 (9.8) | 3 (2.1) | 1 (0.6) | 1 (5.9) | ||||
| 14 | Are you normally in close contact with family and friends? | 1. Yes | 167 (96.5) | 324 (94.2) | 47 (92.2) | 0.368 | 139 (95.2) | 141 (89.8) | 13 (76.5) | 0.017 |
| 2. No | 6 (3.5) | 20 (5.8) | 4 (7.8) | 7 (4.8) | 16 (10.2) | 4 (23.5) | ||||
| 15 | Do you have anyone to talk to if you feel unwell? | 1. Yes | 165 (95.4) | 325 (94.5) | 47 (92.2) | 0.671 | 141 (96.6) | 145 (92.4) | 16 (94.1) | 0.281 |
| 2. No | 8 (4.6) | 19 (5.5) | 4 (7.8) | 5 (3.4) | 12 (7.6) | 1 (5.9) | ||||
Item 6, 7, and 9 were excluded from analysis for criterion‐related validity with frailty.
Discussion
The EFA for the QO extracted six factors: (1) social conditions and lifestyle, (2) subjective conditions, (3) cognitive functions, (4) physical activity, (5) oral functions, and (6) physical functions. The model for the QO involved all 15 items that were assumed to form part of a health condition assessment. The model's CFA demonstrated high suitability among the older‐ and younger‐older adults groups.
Factors 2 to 6 were structured using homogeneous items. The QO was proposed to assess frailty in older adults. It has been suggested that frailty has three domains: physical, psychological, and social; 13 , 14 the current study model included all three. Factor 4 (physical activity) and Factor 6 (physical functions) were related to the physical domain; Factor 2 (subjective conditions) and Factor 3 (cognitive functions) were related to the psychological domain; and Factor 1 addressed the social domain through factors such as eating (item 3), smoking (item 12), and social activities (items 14 and 15). Recently, oral frailty, which strongly predicts the onset of adverse health outcomes including mortality, has also been proposed. 9 Therefore, Factor 5 (oral functions) was assessed by asking about item 4, which asked about difficulty in eating food, and item 5, which asked about choking on tea or soup. Each factor in this model had a different significance, thereby indicating health conditions that were associated with the three domains of frailty or oral frailty. This indicated that the QO could comprehensively assess health conditions related to frailty.
Four items in Factor 1 were positively related to each other based on their factor loadings (i.e., if the participants consistently ate three meals a day, were able to communicate with others or supporters, or did not smoke). In a meta‐analysis, smokers in 15 countries consumed more calories, although this was not the case in Japan. 15 There was no association between smoking and caloric consumption in this context, 16 and female smokers actually consumed fewer calories. 17 The question about meals was included in the QO because greater dietary variety helps in maintaining physical performance among older adults, 18 and the smoking question was included because smoking is associated with life prognosis. 19 However, as these lifestyle choices were unlikely to be directly related to the social conditions of items 14 and 15, combining these four items into Factor 1 would result in a spurious correlation.
Regarding the results of the CFA using SEM among the older‐older adults group, the CFI and AGFI were over 0.95, RMSEA was 0.018, and SRMR was 0.030. Both the CFI and AGFI, with values greater than 0.90 and 0.95, respectively, typically reflected acceptable and excellent fits to the data. 20 , 21 RMSEA was recommended to be lower than 0.06, and SRMR lower than 0.08. 22 Therefore, we conclude that the model assumed for the QO based on the EFA is suitable, indicating that the QO has construct validity. Although there might be room for improvement in the model with a CFI of 0.880, the model among the younger‐older adults group generally had sufficient suitability, despite the CFI. The QO prepared for the older‐older adults group could also have been useful for the younger‐older adults. In the model for both the older‐ and younger‐older adults groups, the factor with the strongest correlation with health conditions was Factor 6 (i.e., physical functions). Thus, an older adult's health condition might be related to physical frailty, such as the ability or inability to walk.
It was not surprising that many QO items had a statistically significant association with frailty, as QO was developed to evaluate the characteristics of frailty. 2 Although we could not assess the criterion‐related validity of the QO's total score, we found that many QO items had criterion‐related validity with frailty. Choking (item 5) was one of the oral status items and its decline was associated with oral frailty. 9 Oral frailty 9 and smoking habits 23 (item 12) have been reported to be predictors of frailty. However, in the present study, these factors had no cross‐sectional association with frailty. The opportunity to talk to people (item 14) was related to social frailty. 24 Having someone to talk to if feeling unwell (item 15), which had no statistically significant association with frailty, might differ from opportunities to talk to people, as item 15 relates more to social support. During the QO development, item 15 was included because lack of social support was significantly associated with psychological distress. 25 Therefore, we suggest that lack of social support has a strong psychological dimension and a weak relationship with frailty, or frailty assessed by the FSI has strong physical and cognitive aspects and weak psychological and social aspects.
The model of the current study, developed during the COVID‐19 pandemic, is an appropriate measure of frailty. As a result of COVID‐19 restrictions, the more frailty older adults had, the less subjective physical activity and smaller meal size they had. 26 Time for physical activity decreased compared with what was possible before the COVID‐19 pandemic. 27 The lifestyle of the older adults may have changed during this study. Health conditions during the pandemic might have differed from those in non‐pandemic times, which could have affected the findings. In particular, the opportunity for exercise and physical activities may relate to frailty differently compared with in non‐pandemic times. How the finding for the QO structure might differ in pandemic and non‐pandemic times should be examined in future studies.
This study has several limitations. First, the QO was developed using health guidance for older adults based on their answers to each item, and the spurious structure was not considered. Second, the Japanese Ministry of Health, Labor and Welfare suggested 10 domains for the QO, 2 and the Japanese Geriatrics Society categorized the 15 items into six groups based on frailty domains. 28 As the QO might have several models, the association between the factors of the QO and clinical anchors ought to be investigated further. Third, this study was conducted in a limited area. Generalizability, by including results from other areas or participants, should be assessed in future studies.
In conclusion, we have suggested a QO model that is structured by six factors (social conditions and lifestyle, subjective conditions, cognitive functions, physical activity, oral functions, and physical functions) and includes frailty domains. The CFA using SEM for the older‐older adults group found that CFI = 0.971, AGFI = 0.978, RMSEA = 0.018, and SRMR = 0.030. The CFA using SEM for the younger‐older adults group found that CFI = 0.880, AGFI = 0.940, RMSEA = 0.037, and SRMR = 0.048. The QO model could evaluate health conditions among the older‐older adults groups as it has sufficient suitability and the QO has construct validity. Similarly, the QO generally has sufficient suitability for the younger‐older adults group. Moreover, many QO items has criterion‐related validity with frailty.
Disclosure statement
The authors declare no conflict of interest.
Acknowledgements
We would like to express our sincere gratitude to Kenichi Sudo, Munehisa Sudo, Atsushi Kuwabara, Satoshi Tanaka, Chieko Mesaki, Junko Ishii, Kumi Aoki, Norie Torizuka, Miyuki Ogawa, Yumi Ino, Seiichi Asanuma, Izumi Tsutsumi, Susumu Shimomura, Nobuko Kaseda, Kazuaki Kuwabara, Yuriko Yoshiara, Ryo Koike, Masaaki Arai, Ayako Yamazaki, and all the district welfare commissioners who cooperated with us. This work was supported by the Nippon Life Insurance Foundation (Grant 2020‐0203‐04) and the Japanese Society for the Promotion of Science KAKENHI (Grant 19K19712). We would like to thank Editage (www.editage.com) for English language editing and for supporting COVID‐19 research.
Shinohara T, Saida K, Tanaka S, Murayama A, Higuchi D. Construct validity of the Questionnaire for Older Senior Citizens based on a confirmatory factor analysis: A study during the period of self‐restraint to prevent the spread of coronavirus disease 2019. Geriatr. Gerontol. Int. 2021;21:1018–1025. 10.1111/ggi.14285
Data availability statement
Only the authors can access to the study data in accordance with the contract with the participants.
References
- 1.Cabinet Office. Annual report on the ageing society [Summary] FY 2019 [Cited 5 March 2021]. Available from URL: https://www8.cao.go.jp/kourei/english/annualreport/2019/pdf/2019.pdf
- 2.Ministry of Health, Labour and Welfare. Explanation and notes for the Questionnaire for Older Senior Citizens.
- 3. Rockwood K, Mitnitski A. Frailty in relation to the accumulation of deficits. J Gerontol A Biol Sci Med Sci 2007; 62: 722–727. [DOI] [PubMed] [Google Scholar]
- 4. Fried LP, Tangen CM, Walston J et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci 2001; 56: M146–M156. [DOI] [PubMed] [Google Scholar]
- 5. Gobbens RJ, Luijkx KG, Wijnen‐Sponselee MT, Schols JM. Toward a conceptual definition of frail community dwelling older people. Nurs Outlook 2010; 58: 76–86. [DOI] [PubMed] [Google Scholar]
- 6. Kelaiditi E, Cesari M, Canevelli M et al. Cognitive frailty: rational and definition from an (I.A.N.A./I.A.G.G.) international consensus group. J Nutr Health Aging 2013; 17: 726–734. [DOI] [PubMed] [Google Scholar]
- 7. Garre‐Olmo J, Calvó‐Perxas L, López‐Pousa S, de Gracia Blanco M, Vilalta‐Franch J. Prevalence of frailty phenotypes and risk of mortality in a community‐dwelling elderly cohort. Age Ageing 2013; 42: 46–51. [DOI] [PubMed] [Google Scholar]
- 8. Makizako H, Shimada H, Tsutsumimoto K et al. Social frailty in community‐dwelling older adults as a risk factor for disability. J Am Med Dir Assoc 2015; 16: 1003.e7‐11. [DOI] [PubMed] [Google Scholar]
- 9. Tanaka T, Takahashi K, Hirano H et al. Oral frailty as a risk factor for physical frailty and mortality in community‐dwelling elderly. J Gerontol A Biol Sci Med Sci 2018; 73: 1661–1667. [DOI] [PubMed] [Google Scholar]
- 10.Ministry of Health, Labour and Welfare. The changes for the Questionnaire used in the health checkup of medical insurance for older‐older adults.
- 11. Looi MK. Covid‐19: Japan prepares to extend state of emergency nationwide as “untraceable” cases soar. BMJ 2020; 369: m1543. [DOI] [PubMed] [Google Scholar]
- 12. Yamada M, Arai H. Predictive value of frailty scores for healthy life expectancy in community‐dwelling older Japanese adults. J Am Med Dir Assoc 2015; 16: 1002.e7‐11. 10.1016/j.jamda.2015.08.001. [DOI] [PubMed] [Google Scholar]
- 13. Gobbens RJ, van Assen MA, Luijkx KG, Wijnen‐Sponselee MT, Schols JM. The Tilburg frailty indicator: psychometric properties. J Am Med Dir Assoc 2010; 11: 344–355. [DOI] [PubMed] [Google Scholar]
- 14. Op het Veld LP, van Rossum E, Kempen GI, de Vet HC, Hajema K, Beurskens AJ. Fried phenotype of frailty: cross‐sectional comparison of three frailty stages on various health domains. BMC Geriatr 2015; 15: 77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Dallongeville J, Marécaux N, Fruchart JC, Amouyel P. Cigarette smoking is associated with unhealthy patterns of nutrient intake: a meta‐analysis. J Nutr 1998; 128: 1450–1457. [DOI] [PubMed] [Google Scholar]
- 16. Dyer AR, Elliott P, Stamler J et al. Dietary intake in male and female smokers, ex‐smokers, and never smokers: the INTERMAP study. J Hum Hypertens 2003; 17: 641–654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Yaguchi‐Tanaka Y, Ishikawa H, Shao L, Sasaki S, Fukao A. Association between smoking status and nutrient and food group intakes among community‐dwelling Japanese adults. J Jpn Soc Nutr Food Sci 2011; 64: 159–167. [Google Scholar]
- 18. Yokoyama Y, Nishi M, Murayama H et al. Dietary variety and decline in lean mass and physical performance in community‐dwelling older Japanese: a 4‐year follow‐up study. J Nutr Health Aging 2017; 21: 11–16. [DOI] [PubMed] [Google Scholar]
- 19. Murakami Y, Miura K, Okamura T, Ueshima H, EPOCH‐JAPAN Research Group . Population attributable numbers and fractions of deaths due to smoking: a pooled analysis of 180,000 Japanese. Prev Med 2011; 52: 60–65. [DOI] [PubMed] [Google Scholar]
- 20. Marsh HW, Lüdtke O, Muthén B et al. A new look at the big five factor structure through exploratory structural equation modeling. Psychol Assess 2010; 22: 471–491. [DOI] [PubMed] [Google Scholar]
- 21. Schermelleh‐Engel K, Moosbrugger H, Müller H. Evaluating the fit of structural equation models: tests of significance and descriptive goodness‐of‐fit measures. Methods Psychol Res Online 2003; 8: 23–74. [Google Scholar]
- 22. Hu LT, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equat Model 1999; 6: 1–55. [Google Scholar]
- 23. Kojima G, Iliffe S, Walters K. Smoking as a predictor of frailty: a systematic review. BMC Geriatr 2015; 15: 131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Kojima G, Taniguchi Y, Kitamura A, Fujiwara Y. Is living alone a risk factor of frailty? A systematic review and meta‐analysis. Ageing Res Rev 2020; 59: 101048. [DOI] [PubMed] [Google Scholar]
- 25. Kuriyama S, Nakaya N, Ohmori‐Matsuda K et al. Factors associated with psychological distress in a community‐dwelling Japanese population: the Ohsaki cohort 2006 study. J Epidemiol 2009; 19: 294–302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Shinohara T, Saida K, Tanaka S, Murayama A. Association between frailty and changes in lifestyle and physical or psychological conditions among older adults affected by the coronavirus disease 2019 countermeasures in Japan. Geriatr Gerontol Int 2021; 21: 39–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Yamada M, Kimura Y, Ishiyama D et al. Effect of the COVID‐19 epidemic on physical activity in community‐dwelling older adults in Japan: a cross‐sectional online survey. J Nutr Health Aging 2020; 24: 948–950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. The Japan Geriatrics Society. Response Manual for the Questionnaire for Older Senior Citizens.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Only the authors can access to the study data in accordance with the contract with the participants.


