Abstract
Objective
To assess existing evidence on the effects of COVID‐19 on healthcare workers (HCWs) using the health‐related productivity loss approach.
Methods
A systematic search of online databases including PubMed, Scopus, Ovid, Web of Science, and EMBASE was conducted up to 25 August 2020. Following two screening stages, studies related to the effects of COVID‐19 on healthcare workers were included in the study.
Results
82 studies were included in the analysis. The COVID‐19 related death rate among HCWs ranged from 0.00‐0.7%, while the positive test incidence varied between 0.00 and 24.4%. 39 evidences assessed psychological disorders. A wide range of psychological disorders observed among HCWs: 5.2 to 71.2% in anxiety, 1.00 to 88.3% in stress, 8.27 to 61.67% in insomnia, and 4.5 to 50.4% in depression.
Conclusions
The early evidence suggests that healthcare workers are one of the most vulnerable groups when it comes to positive COVID‐19 infection, mortality, and mental illness.
Keywords: absenteeism, COVID‐19, health care workers, presenteeism
1. INTRODUCTION & OBJECTIVES
A significant number of infections and even deaths among health care workers (HCWs) are caused by COVID‐19. 1 The loss of health professionals by healthcare systems, along with shortage problems in some countries, increases the severity of the problem. 2
Work absences and working while illness will lead to productivity losses for workers. 3 , 4 Health‐related productivity loss means productivity loss (PL) due to health problems. 5 In the Valuation of Lost Productivity Approach (VOLP) health‐related productivity loss appears to be driven by three variables: absenteeism (being absent from work), presenteeism (working while sick), and the inability to do unpaid work due to illness. 6 , 7
There are several ways COVID‐19 may impact health‐related productivity among HCWs. The first way involves the death of HCWs. Some studies have reported deaths among HCWs due to COVID‐19. 8 , 9 Healthcare systems have difficulty compensating for death of professionals in the field. Another way is to infect HCWs with COVID‐19. A COVID‐19 infection is most likely to cause productivity loss through absenteeism during the illness period and the quarantine period. As of 8 April 2020, the World Health Organization (WHO) reported that 2073 health care workers in 52 countries were infected with COVID‐19, however these numbers are based solely on reports that have been submitted to the WHO. According to this report, the incidence of COVID‐19 infection among HCWs was 3.8% in China and 11% in Italy among the entire infected population. 10 Third, HCWs are at risk for physical and psychological disorders. The main focus is on psychological disorders such as anxiety, depression, and insomnia. 11 , 12 , 13 A physical or psychological disorder may result in absenteeism or presenteeism among healthcare workers.
As a result of COVID‐19, death, infection, and physical and psychological disorders threaten productivity in healthcare settings, and these issues must be addressed separately.
The aim of this review is to:
Reaching out to a framework for Health‐related productivity loss among HCWs using Disability‐adjusted life year (DALY) approach.
Assess existing evidence about the effects of COVID‐19 on healthcare workers by physical and psychological disorders, quarantine due to infection and death.
2. METHODS
This systematic review conducted in August 2020 based on available evidences in scientific databases including published, accepted, and preprinted ones. This study conducted following the PRISMA‐ Preferred Reporting Items for Systematic Reviews and Meta‐Analyses statement based on the 27 items checklist.
2.1. Data sources and search strategy
To formulate search strategies, keywords selected based on the literature review.
The following terms were used for searching in titles, abstracts, and keywords in PubMed, Scopus, Web of Science, Ovid, and EMBASE from 20th August to 25th August:
#1: “COVID‐19” OR “Coronavirus” OR “SARS‐Cov‐2”
#2: “Health‐care worker” OR “Healthcare personnel” OR “Health professionals” OR “Nurse” OR “Medical staff”
#3: “Death” OR “Mortality” OR “physical disorder” OR “Psychological disorder” OR “Mental health” OR “Absenteeism” OR “Presenteeism” OR “Disability adjusted life years”
#4: #1 AND #2 AND #3 limited to 2020 and 2021. Some articles were published in 2021, so this year was also considered in the search. Different spellings of keywords were also considered. After the initial search, a total of 2922 articles were found. Details of the search procedure and the list of the final articles entered into the study are presented in Table 1.
TABLE 1.
Search features in scientific databases
| Keywords | Databases | Total articles | Initial article selection | Final articles |
|---|---|---|---|---|
| COVID‐19, Coronavirus, SARS‐Cov‐2, health‐care worker, healthcare personnel, health professionals, nurse, medical staff, death, mortality, physical disorder, psychological disorder, mental health, absenteeism, presenteeism, disability adjusted life years | PubMed | 409 | 650 | 82 |
| Scopus | 1406 | |||
| Ovid | 409 | |||
| EMBASE | 388 | |||
| Web of science | 310 |
Unrelated and duplicate studies eliminated. Reviewing the titles and abstracts of articles was done by two authors, and 1738 articles which were irrelevant to the objectives of the study excluded. Moreover, 534 articles were removed because they were duplicates. Finally, 650 articles assessed.
2.2. Inclusion and exclusion criteria
Inclusion criteria:
Available full text or at least English abstract;
Quantitative report based on primary data;
Letter to editors, commentaries, and the like with primary data;
Being specifically conducted among HCWs; and
Clear and specific sample size.
Exclusion criteria:
Qualitative studies, systematic reviews, and meta‐analysis; and
Reports based on the entire population or all infected cases in the country.
2.3. Study selection
Databases searched by one of the authors. Screening and assessing articles based on the inclusion and exclusion criteria performed by two independent authors. In the first stage of screening, the existing English abstract and quantitative reports assessed in terms of the inclusion and exclusion criteria based on primary data. Therefore, articles with secondary data (e.g., systematic review and meta‐analysis) and qualitative studies excluded. Articles that included primary data in letter to editors, editorials, commentaries, etc. were also considered. Based on the first stage of screening, 112 articles were excluded, and the 538 remaining articles were screened in the second stage. In the second stage, two inclusion criteria, that is, conducting research specifically among HCWs and specific sample size considered and studies reported based on the general population were excluded. At this stage, out of 538 articles, 82 articles were selected (Figure 1). Presenting the results of the selected articles assessed by two authors using STROBE (Strengthening the Reporting of Observational Studies in Epidemiology) checklist. The quality of the studies assessed with Critical Appraisal Skills Programme checklists (CASP). 14 These checklists review a variety of study designs. We used a general 10‐item checklist; each item scored from 0 to 5 (total score 0 to 50). The minimum acceptable score was 31. Manuscript Scores between 30 and 40 classified “good” and 41–50 “excellent”. 15
FIGURE 1.
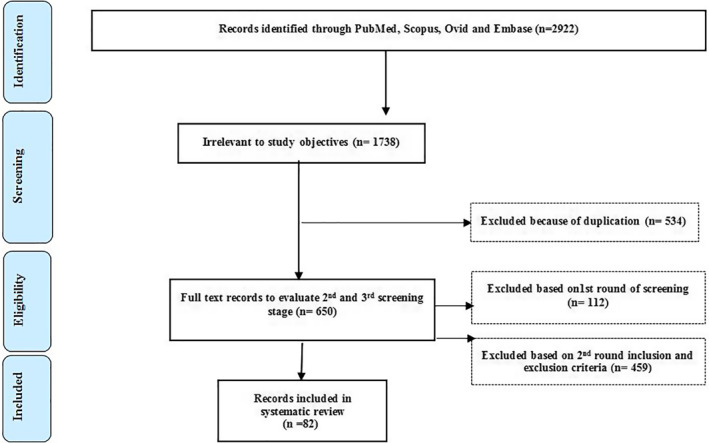
Flow chart of study selection process
2.4. Data extraction, variables and data analysis
All 82 articles scoped and summarized in terms of author/authors, country of the study, type of HCWs, sample size and their main findings using a data extraction form in MS Excel 2010. The effects of COVID‐19 on productivity loss (PL) of HCWs investigated in terms of several categories based on the conceptual framework presented in the Figure 2. In this study, the productivity loss of HCWs caused by COVID‐19 was combined with the Disability‐Adjusted Life Years (DALY) approach and categorized into four groups. The groups included deaths (YLLs), absenteeism due to quarantine, physical YLDs, and Mental YLDs.
FIGURE 2.
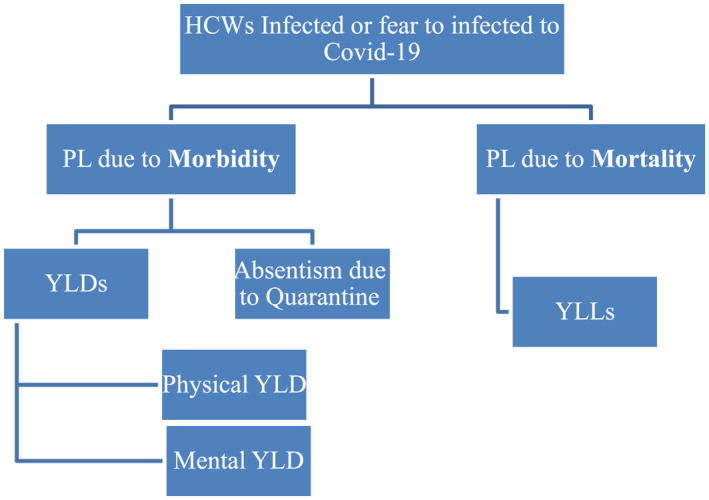
Conceptual framework of study. PL, productivity lost; YLD, years lost due to disability; YLL, years of life lost
3. RESULTS
Eighty two studies included in the analysis.
In evaluating the quality of the studies, out of 82 articles submitted, all studies obtained the minimum quality criteria. Quality of studies in 63 studies (76.8%) were excellent and 19 (23.2%) were good. The characteristics of the selected articles are depicted in Figure 3.
FIGURE 3.
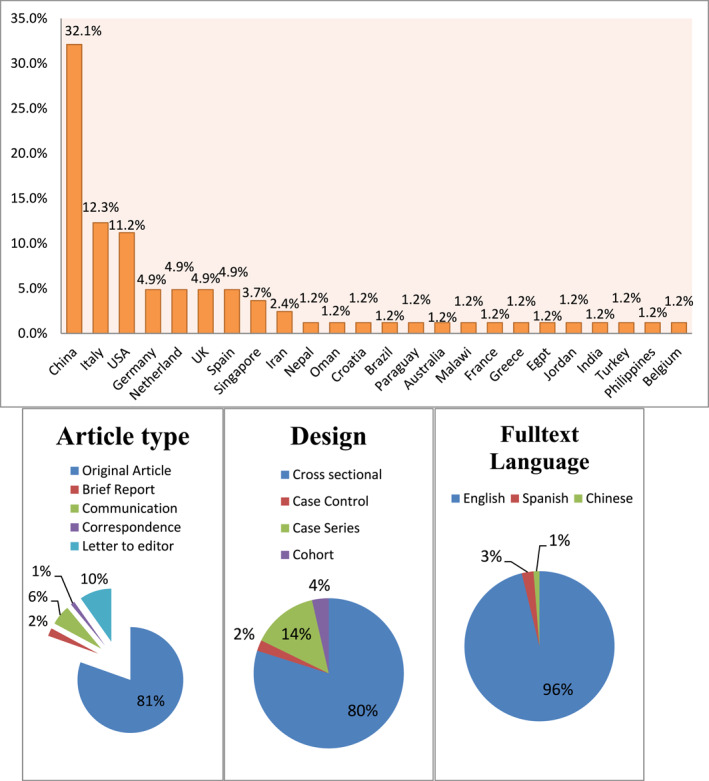
Characteristics of included articles
Summarizing and reporting were based on the conceptual framework. At first, HCWs morbidities related to physical and psychological disorders caused by COVID‐19 reported. After reporting the absence from work from COVID‐19 infection and quarantine, the mortality from COVID‐19 infection was reported.
3.1. Productivity lost due to morbidity
3.1.1. Years lost due to disability (YLDs)
Physical YLD
Few studies have focused specifically on physical disorders caused by COVID‐19 among HCWs. In order to determine the effects of COVID‐19 on HCWs physical conditions, it is necessary to wait for future reports. Results showed that skin problems were common among HCWs due to wearing masks and protective equipment (Table 2).
TABLE 2.
Physical disorders related to COVID‐19 among health care workers
| Authors | Country | HCWs types | Study sample & main outcome | CASP score |
|---|---|---|---|---|
| Lan et al. 16 | China | NA | 526 HCWs: Skin damages‐ dryness/tightness 370 (70.3%), tenderness 299 (56.8%), itching 276 (52.5%) and burning/pain 200 (38.0%) | 38 |
Abbreviations: CASP, critical appraisal skills programme checklists; HCW, health care workers.
Mental YLD
The diversity of mental disorders reported by HCWs due to COVID‐19 varies from fear and anxiety and loneliness to Post‐traumatic Stress Disorder (PTSD). The most commonly reported mental disorders included stress and anxiety, sleep disorders and depression (Table 3).
TABLE 3.
Psychological disorders related to COVID‐19 among health care workers
| Authors | Country | HCWs types | Study sample & main outcome | CASP score |
|---|---|---|---|---|
| Labrague & santos 17 | Philippines | Nurses | 325 nurses: Dysfunctional levels of anxiety 123 (37.8%) | 43 |
| Gupta et al. 18 | Nepal | Nursing staff, faculty members and other | 150 HCWs: Anxiety disorder 56 (37.3%), depression 12 (8%) | 47 |
| Zandifar et al. 19 | Iran | NA | 892 HCWs: Depression 41.7%, anxiety 51.2%, stress 33.9% | 46 |
| Salopek‐Žiha et al. 20 | Croatia | All | 124 HCWs: 11% moderate to very‐severe depression, 17% moderate to extremely‐severe anxiety, 10% moderate to extremely‐severe stress | 38 |
| Badahdah et al. 21 | Oman | Physician and nurses | 509 physician and nurses: High anxiety 132 (25.9), high stress 287 (56.4%) | 46 |
| Luceño‐Moreno et al. 22 | Spain | All | 1422 HCWs: Posttraumatic stress disorder (PTSD) 56.6%, anxiety disorder 58.6%, depressive disorder 46%, feel emotionally drained 41.1% | 43 |
| Dal’BoscoI et al. 23 | Brazil | Nurses | 88 nurses: Anxiety (48.9%) and depression (25%) | 49 |
| Samaniego et al. 24 | Paraguay | NA | 126 HCWs: Moderate and severe depression 32.2%, anxiety 41.3%, insomnia 27.8%, distress 38.9%, fatigue 64.3% | 45 |
| Giusti et al. 25 | Italy | NA | 330 health professionals: 235 (71.2%) anxiety above the clinical cutoff, 88 (26.8%) clinical levels of depression, 103 (31.3%) of anxiety, 113 (34.3%) of stress, 121 (36.7%) of post‐traumatic stress. | 36 |
| Rossi et al. 26 | Italy | Nurse, GP, assistant, laboratory, radiology, physiotherapists | 1379 HCWs: (PTSS) 681 (49.38%), depression 341 (24.73%), anxiety 273 (19.80%), insomnia 114 (8.27%), High perceived stress 302 (21.90%) | 47 |
| Magnavita et al. 27 | Italy | Physician, nurse, technician, clerk, other | 595 HCWs: Anxiety (16.6%), depression (20.3%) | 46 |
| De sio et al. 28 | Italy | Physicians | 695 physicians: Distress of (93.8%), poor well‐being (58.9%) | 47 |
| Ni et al. 29 | China | NA | 214 HCWs: Anxiety 47 (22.0%), depression 41 (19.2%) | 42 |
| Zhou et al. 30 | China | NA | 1931 HCWs: Poor sleep quality (18.4%) | 41 |
| Que et al. 31 | China | Physicians, medical residents, nurses, technicians and public health | 2285 HCWs: Anxiety (46.04%), depression (44.37%), insomnia (28.75%) and the overall psychological problems (56.59%) | 41 |
| Song et al. 32 | China | Medical staff nurses | 14825HCWs: Depressive symptoms (25.2%), post‐traumatic stress disorder (PTSD) (9.1%) | 44 |
| Tu et al. 33 | China | Nurses | 100 nurses: Poor sleep quality (60%), depression symptoms (46%), anxiety symptoms (40%) | 48 |
| Tian et al. 34 | China | Frontline health professionals (76.8% nurses) | 845 HCWs: Moderate to severe stress level (60.8%), depression (45.6%), anxiety (20.7%), insomnia symptoms (27%) | 47 |
| Jin et al. 35 | China | Medical staffs, nurses, medical technicians | 103 HCWs: Psychological stress or emotional changes during their isolation period after infection (88.3%) | 33 |
| Li et al. 36 | China | Women HCW | 4369 women HCWs: Depression 621 (14.2%), anxiety 1101 (25.2%), acute stress symptoms 1382 (31.6%) | 46 |
| Zhan et al. 37 | China | Nurses | 2667 nurses: 935 (35.06%) in the fatigue status | 46 |
| Wang et al. 38 | China | Doctors and nurses | 274 HCWs: Combined prevalence of anxiety, depression and insomnia of staff backing Hubei reached as high as (38%) | 39 |
| Dong et al. 39 | China | All | 4618 HCWs: 24.2% high levels of anxiety or/and depressive symptoms | 43 |
| Zhang et al. 40 | China | Medical staffs | 1563 medical staffs: 564 (36.1%)insomnia symptoms | 41 |
| Wang et al. 41 | China | All | 2737 HCWs: Sleep problems (61.6%), anxiety (22.6%), depressive symptoms (35%) | 45 |
| Huang et al. 42 | China | Medical staffs | 230 medical staffs: 53 (23.04%) anxiety | 46 |
| Wu & Wei 43 | China | Medical staffs | 120 medical staffs: Moderate insomnia (61.67%), severe insomnia (26.67%) | 37 |
| Liu et al. 44 | China | Medical staffs | 2031 medical staffs: Depression (14.81%), anxiety (18.3%), stress symptoms (9.98%) | 48 |
| Lai et al. 13 | China | All | 1257 HCWs: Depression 634 (50.4%), anxiety 560 (44.6%), insomnia 427 (34%), distress 899 (71.5%) | 44 |
| Yin et al. 45 | China | All | 377 HCWs: Posttraumatic stress symptoms‐ PTSS (3.8%) | 42 |
| Cai et al. 46 | China | Frontline and non‐frontline medical workers | 1173 frontline and 1173 non‐frontline medical workers: Mental problem (52.6% vs. 34.0%), anxiety symptoms (15.7% vs. 7.4%), depressed mood (14.3% vs. 10.1%) and insomnia (47.8% vs. 29.1) among frontline and non‐frontline medical workers. | 38 |
| Zhao et al. et al. 47 | China | All | 972 frontline staff: Anxiety 438 (45.1%), depressive symptoms 313 (32.2%), insomnia 380 (39.1%) | 35 |
| Wang et al. 48 | China | Nurses | 202 nurses: Post‐traumatic stress disorder (PTSD) (16.83%) | 42 |
| Leng et al. 49 | China | Nurses | 90 nurses: Post‐traumatic stress disorder (PTSD) 5 (5.6%) | 46 |
| Zhang et al. 50 | China | Medical health workers | 927 medical health workers: Insomnia (38.4%), anxiety (13%), depression (12.2%), somatization (1.6%), obsessive‐compulsive symptoms (5.3%) | 39 |
| Shechter et al. 51 | USA | Physicians, advanced practice providers, residents/fellows, and nurses | 657 HCW: Acute stress (57%), depressive (48%), anxiety symptoms (33%) | 41 |
| Civantos et al. 52 | USA | Physician | 349 physicians: Anxiety 167 (47.9%), distress 210 (60.2%), burnout 76 (21.8%), depression 37 (10.6%) | 47 |
| Tan et al. 53 | Singapore | Physician, nurse, allied healthcare, technician, Clerical staff, administrator, maintenance worker | 470 HCWs: Depression (8.93%), anxiety (14.46%), stress (6.59%), PTSD (7.65%) | 45 |
| Chew et al. 54 | Singapore | Doctors, nurses, allied healthcare, administrators, clerical staff and maintenance workers | 906 HCWs: Moderate to very‐severe depression (5.3%), moderate to extremely‐severe anxiety (8.7%), moderate to extremely‐severe stress (2.2%), moderate to severe levels of psychological distress (3.8%). | 46 |
| Chew et al. 55 | Multi countries | Physician, nurse, technician, Clerical staff/executive, administrator, maintenance worker, allied professional | 1146 HCWs: Depression (4.5%), anxiety (5.2%), stress (1.0%), PTSD (7.9%) | 45 |
Abbreviations: CASP, critical appraisal skills programme checklists; HCW, health care workers.
3.1.2. Absenteeism due to quarantine
Any case of COVID‐19 and long absence from work will affect productivity, and it will not be possible to use infected HCWs until full recovery. For different study populations, COVID‐19 incidences among HCWs range from 0.00% to about 25% (Table 4).
TABLE 4.
Number and percentage of infection (positive cases) related to COVID‐19 among HCWs
| Authors | Country | HCWs type | Study sample & main outcome | CASP score |
|---|---|---|---|---|
| Behrens et al. 56 | Germany | NA | 217 HCWs: 45 (21%) infected | 45 |
| Brandstetter et al. 57 | Germany | NA | 201 HCWs: 31 (15.4%) infected | 48 |
| Korth et al. 58 | Germany | NA | 316 HCWs: 5 (1.6%) infected | 43 |
| Schmidt et al. 59 | Germany | All | 406 HCWs: 2.7% infected | 39 |
| Kempker et al. 60 | USA | NA | 283 HCWs: 51 (18%) infected | 48 |
| Mani et al. 61 | USA | All | 3477 HCWs: 185 (5.3%) infected | 46 |
| Demmer et al. 62 | USA | All | 489 HCWs: 0 (0.00%) infected | 45 |
| Cummings et al. 63 | USA | NA | 4689 HCWs: 387 (8%) infected | 43 |
| Stubblefield et al. 64 | USA | Nurses, providers, radiology technicians, others | 249 HCWs: 19 (7.6%) infected | 47 |
| Hartmann et al. 65 | USA | All | 56,855 HCWs: 5458 (9.6%) infected | 47 |
| Reusken et al. 66 | Netherland | NA | 1097 HCW: 45 (4.1%) infected | 34 |
| Tostmann et al. 67 | Netherland | NA | 803 HCWs: 90 (11.2%) infected | 39 |
| Sikkema et al. 68 | Netherland | NA | 1796 HCWs: 96 (5%) infected | 37 |
| Kluytmans‐van den bergh et al. 69 | Netherland | All | 9075 HCWs: 85 (1%) infected | 43 |
| Martin et al. 70 | Belgium | Physicians, nurses, paramedical staff, stretcher‐bearers and cleaners, administrative employees | 326 HCWs: 37 (11.3%) infected | 36 |
| Garcia‐Basteiro et al. 71 | Spain | All | 578 HCWs: 65 (11.2%) infected | 49 |
| Moreno‐Casbas et al. 72 | Spain | NA | 2230 HCWs: 275 (12.3%) infected | 45 |
| Alvarez Gallego et al. 73 | Spain | Surgeons | 50 surgeons: 12 (24.4%) infected | 39 |
| Zheng et al. 74 | China | All | 117,100 HCWs: 2457 (2.09%) infected | 41 |
| Lai et al. 75 | China | Medical staffs | 9684 medical staffs: 110 (1.1%) infected | 45 |
| Brown et al. 76 | UK | All | 1152 HCWs: 23 (2.0%) infected | 47 |
| Bampoe et al. 77 | UK | Anaesthetists, midwives and obstetricians | 200 HCWs: 29 (14.5%) infected | 47 |
| Keeley et al. 78 | UK | NA | 1533 HCW: 282 (18%) infected | 48 |
| Felice et al. 79 | Italy | All | 388 HCWs: 18 infected | 38 |
| Lombardi et al. 80 | Italy | All | 1573 HCWs: 139 (8.8%) infected | 47 |
| Paderno et al. 81 | Italy | All staffs of otolaryngology unit | 58 HCWs: 5 (9%) infected | 41 |
| Garzaro et al. 82 | Italy | NA | 830 HCWs: 80 (9.6%) infected | 43 |
| Lahner et al. 83 | Italy | All | 2057 HCWs: 58 (2.7%) infected | 43 |
| Magnavita et al. 27 | Italy | Physician, nurse, technician, clerk, other | 595 HCWs: 82 (13.78%) infected | 48 |
| Muhi et al. 84 | Australia | NA | 1160 HCWs: 11 (0.94%) infected | 42 |
| Gheysaradeh et al. 85 | Iran | Nurses | 125 nurses: 5 (4%) infected | 34 |
| Chibwana et al. 86 | Malawi | All | 500 HCWs: 12.3% infected | 47 |
| Wee et al. 87 | Singapore | NA | 1642 HCWs: 9 (0.54%) infected. | 47 |
| Contejean et al. 88 | France | All | 1344 HCWs: 373 (28%) infected | 46 |
| Maltezou et al. 89 | Greece | All | 3398 HCWs: 66 (1.9%) infected | 32 |
| Kassem et al. 90 | Egypt | Physician, nurse, patient transporters/cleaners, administrative employees | 74 HCWs: 10 (13.5%) infected | 45 |
| Al‐zoubi et al. 91 | Jordan | All | 370 HCWs: 0 (0.00%) infected | 35 |
| Jha et al. 92 | India | NA | 1113 HCWs: 20 (1.8%) infected | 46 |
| Çelebi et al. 93 | Turkey | Physicians nurses cleaning personnel other occupations | 703 HCWs: 50 (7.1%) infected. Physicians 6.3%, nurses 8.0%, Cleaning personnel 9.1% and the other occupations 2.6%. | 43 |
Abbreviations: CASP, critical appraisal skills programme checklists; HCW, health care workers.
3.2. Productivity lost due to mortality
3.2.1. Years of life lost (YLLs)
HCWs dying from COVID‐19 can impact PL because these workers are highly valued, education and deployment are costly, and replacement is hard. The situation is worse in countries with a high shortage of health care workers. Based on the results, the mortality rate among HCWs ranges from 0.00 to 0.7%. Based on the PL approach, even one case of mortality among HCWs can significantly reduce productivity (Table 5).
TABLE 5.
Number and percentage of Death related to COVID‐19 among HCWs
| Authors | Country | HCWs type | Study Sample & main outcome | CASP score |
|---|---|---|---|---|
| CDC COVID‐19 response Team 94 | USA | NA | 9282 HCWs: 27 (0.29%) death | 46 |
| Hartmann et al. 65 | USA | All | 56,855 HCWs: 398 (0.7%) death | 48 |
| Çelebi et al. 93 | Turkey | Physicians, nurses, cleaning personnel,Other occupations | 703 HCWs: 0 (0.00%) death | 47 |
| Levene et al. 95 | UK | Doctor, nurse and others | 147 HCW death: 19.1% doctors (n = 28, including 10 GPs), 42.9%nurses (n = 63), and other HCWs 38.1% (n = 56). The cumulative mortality rates for doctors 0.15 per 1000, nurses 0.17 per 1000 nurses, and 0.10 per 1000 other HCWs | 41 |
| Contejean et al. 88 | France | All | 1344 HCWs: 0 (0.00%) death | 48 |
| Lapolla et al. 96 | Italy | All | 205 HCWs deaths: Medical staffs 119 (57.8%), nurses 34 (16.5%), nurse aides 17 (8.3%), dentists 12 (5.8%), pharmacists 10 (4.9%) | 43 |
Abbreviations: CASP, critical appraisal skills programme checklists; HCW, health care workers.
4. DISCUSSION
In this study, the productivity loss of HCWs due to COVID‐19 categorized into four groups: deaths (YLLs), absenteeism due to quarantine, physical YLDs, and mental YLDs.
The quality of the studies included in the present study is generally an important issue for systematic review. Although quality assessment is limited in cases where results are reported quickly due to urgency in COVID‐19, none of articles excluded. Quality assessment may reflect the incompleteness of the report to some extent, and poor reporting remains a widespread problem. There are no homogeneous and accurate statistics on the death rate among HCWs due to COVID‐19. In some studies, HCWs mortality reported among the entire population. Some studies specifically report the death rate among HCWs, while others only report the general number of deaths. The main point is that HCWs lose their lives because of COVID‐19. In addition to the invaluable sacrifices made by HCWs during the COVID‐19 outbreak, their absence can cause many problems for healthcare systems. This issue can become more complicated in developing countries dealing with various shortages. 97
A systematic review reported presenteeism productivity losses ranging from 2000 USD to 15,541 USD per healthcare employee annually. Moreover, absenteeism costs were higher than presenteeism (463 vs. 340 USD per person). These estimates were based on a general calculation and not related to a specific disease. 2 Although presenteeism is more prevalent among HCWs, the monetary value of absenteeism is higher. 98 In Nurchis et al. (2020), the burden of COVID‐19 for the Italian population calculated by DALY and the human capital approach and mortality and disability caused by COVID‐19 were considered. According to Nurchis et al., the permanent and temporary productivity loss estimated around 300 million € and 100 million €, respectively. 99 In South Korea, the DALY of COVID‐19 estimated for the total population, accounting for 10.3% of YLLs and 89.7% of YLDs. 100 These studies show that despite lower mortalities than disabilities, the monetary value of YLLs is higher than that of YLDs, with greater impact on productivity loss.
HCWs infection during COVID‐19 is one of the contributing factors to absenteeism. There are various statistics on the infection rates. The length of the quarantine, receiving treatment, and absence from work affect productivity loss due to the number of days it takes a person to return to work. The number of days it takes for a person to return to work estimated around 10‐14 days. 101 In Gianino et al. (2019), absenteeism due to seasonal influenza calculated among 5041 HCWs, and the results showed over 11,100 working days/year lost, costs were approximately 1.7 million euros, and the average work loss valued around €327/person. 102 The study carried out by Gianino et al. shows the level of productivity loss due to viral infections.
In this study, presenteeism categorized to physical and psychological disorders. Presenteeism is highly prevalent among HCWs. In a study in Saudi Arabia among physicians, nurses, dentists, pharmacists, and other professionals at a tertiary center, 74% of employees reported having sickness presenteeism during the year. 103 In a study in Turkey among HCWs, the monetary value of presenteeism productivity loss estimated at 19.92 to 315.57 TRY for two weeks and 478.08 to 7573.68 TRY for one year. 104
Physical disorders among HCWs caused by COVID‐19 have been reported in a limited number of studies, and there is a need for further research. Based on the results, skin damage due to COVID‐19 observed. In case of eczema mentioned in the results, Van der Meer et al. (2013) showed that 12% of HCWs had eczema and 3.1% of HCWs reported high levels of presenteeism due to eczema during the year. 105
Results of the current study showed that mental disorders caused by COVID‐19 were relatively high among HCWs. Mental illnesses after chronic low back pain have the highest rate of daily productivity loss among HCWs 106 which was the most important factor affecting YLDs. 107 Studies on stress among HCWs in China showed that there was a significant relationship between stress and presenteeism in a way that with increasing stress, presenteeism also increased. 108 , 109 These problems increase the risk of burnout among HCWs. 110 A study conducted among nurses in Croatia showed a significant relationship between stress and presenteeism; however, this relationship was not significant for absenteeism. 111 All these studies show the importance and effects of psychological disorders on productivity loss.
Diversity of reported outcomes in physical and psychological disorders, infection rate based on symptoms and serology tests and death rate for meta‐analysis made the authors not to expand the results. Also, studies which were at risk of bias may lead to misleading analysis. Our study was limited in these ways.
5. CONCLUSION
According to the results, HCWs are one of the most vulnerable groups in COVID‐19 outbreak in terms of infection, mortalities, and disabilities. As a result, they become patients, fail to show up at work, or have ineffective performances at work. These issues among HCWs can lead to absenteeism and presenteeism and they can cause productivity loss due to health problems among healthcare providers. Therefore, planning in terms of helping HCWs to continue service delivery, proper shifting schedule and psychological counselling should be implemented.
CONFLICT OF INTEREST
The authors declare that there is no conflict of interest regarding the publication of this article.
ETHICS STATEMENT
The ethics committee of the Baqiyatallah University of Medical Sciences (BUMS) approved this study (Approval ID: IR. BMSU.REC.1399.411).
AUTHORS' CONTRIBUTIONS
MY and MMA were equally involved in study design and conception, data collection, analysis and interpretation. MS is the MSc student, who was involved in data collection as well as drafting the manuscript.
CONSENT FOR PUBLICATION
All authors have seen and approved the final version of the articles for publication.
ACKNOWLEDGEMENTS
We thanks to the efforts and support of the Health Management Research Center. This study conducted with no financial support.
Yaghoubi M, Salimi M, Meskarpour‐Amiri M. Systematic review of productivity loss among healthcare workers due to Covid‐19. Int J Health Plann Mgmt. 2022;37(1):94‐111. doi: 10.1002/hpm.3351
DATA AVAILABILITY STATEMENT
The datasets generated and/or analysed during the current study are available from the corresponding author upon reasonable request.
REFERENCES
- 1. Behzadnia MJ, Saboori F. COVID‐19 outbreak management in hospitals of Iran; strengths and weaknesses. Journal Mil Med. 2020;22(2):203‐204. [Google Scholar]
- 2. Lui JNM, Andres EB, Johnston JM. Presenteeism exposures and outcomes amongst hospital doctors and nurses: A systematic review. BMC Health Serv Res. 2018;18(1):985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Zhang W, Bansback N, Boonen A, Severens JL, Anis AH. Development of a composite questionnaire, the valuation of lost productivity, to value productivity losses: Application in rheumatoid arthritis. Value Health. 2012;15(1):46‐54. [DOI] [PubMed] [Google Scholar]
- 4. Sadatsafavi M, Rousseau R, Chen W, Zhang W, Lynd L, FitzGerald JM. The preventable burden of productivity loss due to suboptimal asthma control: A population‐based study. Chest. 2014;145(4):787‐793. [DOI] [PubMed] [Google Scholar]
- 5. Rocha APR, Turi‐Lynch BC, Morais LCd, et al. Association between osteoporosis, health‐related productivity loss and use of hospital services in outpatients of the Brazilian National Health System. Motriz, Rio Claro. 2017;23(3):1‐7. doi: 10.1590/s1980-6574201700030004 [DOI] [Google Scholar]
- 6. Zhang W, Bansback N, Sun H, Pedersen R, Kotak S, Anis AH. Estimating the monetary value of the annual productivity gained in patients with early rheumatoid arthritis receiving etanercept plus methotrexate: Interim results from the PRIZE study. RMD Open. 2015;1(1):e000042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Zhang W, Bansback N, Boonen A, Severens JL, Anis AH. Development of a composite questionnaire, the valuation of lost productivity, to value productivity losses: Application in rheumatoid arthritis. Value Health. 2012;15(1):46‐54. doi: 10.1016/j.jval.2011.07.009 [DOI] [PubMed] [Google Scholar]
- 8. Zhan M, Qin Y, Xue X, Zhu S. Death from Covid‐19 of 23 health care workers in China. N Engl J Med. 2020;382(23):2267‐2268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Ing EB, Xu QA, Salimi A, Torun N. Physician deaths from corona virus (COVID‐19) disease. Occup Med (London); 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. WHO . Coronavirus disease 2019 (COVID‐19): Situation report, 82. 2020. [Google Scholar]
- 11. Bansal P, Bingemann TA, Greenhawt M, et al. Clinician wellness during the COVID‐19 pandemic: extraordinary times and unusual Challenges for the allergist/immunologist. J Allergy Clin Immunol Pract. 2020;8(6):1781‐1790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Blake H, Bermingham F, Johnson G, Tabner A. Mitigating the psychological impact of COVID‐19 on healthcare workers: a digital learning package. Int J Environ Res Publ Health. 2020;17(9):17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Lai J, Ma S, Wang Y, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open. 2020;3(3):e203976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Ma LL, Wang YY, Yang ZH, Huang D, Weng H, Zeng XT. Methodological quality (risk of bias) assessment tools for primary and secondary medical studies: what are they and which is better? Military Medical Research. 2020;7(1):7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Shafiee S, Rajabzadeh Ghatari A, Hasanzadeh A, Jahanyan S. Studying the effect of IT on sustainable development of tourism destinations toward developing smart tourism destinations (based on the meta synthetize approach). New Marketing Research Journal. 2018;7(4):95‐115. doi:10.22108/nmrj.2017.103939.1247 [Google Scholar]
- 16. Lan J, Song Z, Miao X, et al. Skin damage among health care workers managing coronavirus disease‐2019. J Am Acad Dermatol. 2020;82(5):1215‐1216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Labrague LJ, de Los Santos J. COVID‐19 anxiety among frontline nurses: predictive role of organisational support, personal resilience and social support. J Nurs Manag. 2020;28(7):1653‐1661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Gupta AK, Mehra A, Niraula A, et al. Prevalence of anxiety and depression among the healthcare workers in Nepal during the COVID‐19 pandemic. Asian journal of psychiatry. 2020;54:102260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Zandifar A, Badrfam R, Mohammadian Khonsari N, et al. COVID‐19 and medical staff's mental health in educational hospitals in Alborz Province, Iran. Psychiatr Clin Neurosci. 2020;74:499‐501. doi:10.1111/pcn.13098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Salopek‐Žiha D, Hlavati M, Gvozdanović Z, et al. Differences in distress and coping with the COVID‐19 stressor in nurses and physicians. Psychiatr Danub. 2020;32(2):287‐293. [DOI] [PubMed] [Google Scholar]
- 21. Badahdah A, Khamis F, Al Mahyijari N, et al. The mental health of health care workers in Oman during the COVID‐19 pandemic. Int J Soc Psychiatry. 2021;67(1):90‐95. doi: 10.1177/0020764020939596 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Luceño‐Moreno L, Talavera‐Velasco B, García‐Albuerne Y, Martín‐García J. Symptoms of posttraumatic stress, anxiety, depression, levels of resilience and burnout in Spanish health personnel during the COVID‐19 pandemic. Int J Environ Res Publ Health. 2020;17(15). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Dal'Bosco EB, Floriano LSM, Skupien SV, Arcaro G, Martins AR, Anselmo ACC. Mental health of nursing in coping with COVID‐19 at a regional university hospital. Rev Bras Enferm. 2020;73(Suppl 2):e20200434. [DOI] [PubMed] [Google Scholar]
- 24. Samaniego A, Urzúa A, Buenahora M, Vera‐Villarroel P. Sintomatología asociada a trastornos de salud mental en trabajadores sanitarios en Paraguay: efecto COVID‐19. Revista Interamericana de Psicología/Interamerican J Psychol. 2020;54(1):1298‐1317. doi: 10.30849/ripijp.v54i1.1298 [DOI] [Google Scholar]
- 25. Giusti EM, Pedroli E, D'Aniello GE, et al. The psychological impact of the COVID‐19 outbreak on health professionals: a cross‐sectional study. Front Psychol. 2020;11:1684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Rossi R, Socci V, Pacitti F, et al. Mental health outcomes among frontline and second‐line health care workers during the coronavirus disease 2019 (COVID‐19) pandemic in Italy. JAMA Netw Open. 2020;3(5):e2010185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Magnavita N, Tripepi G, Di Prinzio RR. Symptoms in health care workers during the COVID‐19 epidemic. A cross‐sectional survey. Int J Environ Res Publ Health. 2020;17(14). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. De Sio S, Buomprisco G, La Torre G, et al. The impact of COVID‐19 on doctors' well‐being: results of a web survey during the lockdown in Italy. Eur Rev Med Pharmacol Sci. 2020;24(14):7869‐7879. [DOI] [PubMed] [Google Scholar]
- 29. Ni MY, Yang L, Leung CMC, et al. Mental health, risk factors, and social media use during the COVID‐19 epidemic and Cordon sanitaire among the community and health professionals in wuhan, China: Cross‐sectional survey. JMIR Ment Health. 2020;7(5):e19009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Zhou Y, Yang Y, Shi T, et al. Prevalence and demographic Correlates of poor sleep quality among frontline health professionals in liaoning province, China during the COVID‐19 outbreak. Front Psychiatr. 2020;11:520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Que J, Shi L, Deng J, et al. Psychological impact of the COVID‐19 pandemic on healthcare workers: a cross‐sectional study in China. Gen Psychiatr. 2020;33(3):e100259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Song X, Fu W, Liu X, et al. Mental health status of medical staff in emergency departments during the Coronavirus disease 2019 epidemic in China. Brain Behav Immun. 2020;88:60‐65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Tu Z‐h, He J‐w, Zhou N. Sleep quality and mood symptoms in conscripted frontline nurse in Wuhan, China during COVID‐19 outbreak: A cross‐sectional study. Medicine. 2020;99(26):e20769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Tian T, Meng F, Pan W, et al. Mental health burden of frontline health professionals treating imported patients with COVID‐19 in China during the pandemic. Psychol Med. 2020:1‐2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Jin YH, Huang Q, Wang YY, et al. Perceived infection transmission routes, infection control practices, psychosocial changes, and management of COVID‐19 infected healthcare workers in a tertiary acute care hospital in Wuhan: A cross‐sectional survey. Mil Med Res. 2020;7(1):24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Li G, Miao J, Wang H, et al. Psychological impact on women health workers involved in COVID‐19 outbreak in Wuhan: A cross‐sectional study. J Neurology, Neurosurg Psychiatry. 2020;91(8):895‐897. [DOI] [PubMed] [Google Scholar]
- 37. Zhan Y‐X, Zhao S‐Y, Yuan J, et al. Prevalence and influencing factors on fatigue of first‐line nurses Combating with COVID‐19 in China: A descriptive cross‐sectional study. Current Medical Science. 2020;40(4):625‐635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Wang L‐Q, Zhang M, Liu G‐M, et al. Psychological impact of coronavirus disease (2019) (COVID‐19) epidemic on medical staff in different posts in China: A multicenter study. J Psychiatric Res. 2020;129:198‐205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Dong Z‐Q, Ma J, Hao Y‐N, et al. The social psychological impact of the COVID‐19 pandemic on medical staff in China: A cross‐sectional study. Eur Psychiatry. 2020;63(1):e65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Zhang C, Yang L, Liu S, et al. Survey of insomnia and related social psychological factors among medical staff involved in the 2019 novel coronavirus disease outbreak. Front Psychiatr. 2020;11:306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Wang W, Song W, Xia Z, et al. Sleep disturbance and psychological profiles of medical staff and non‐medical staff during the early outbreak of COVID‐19 in Hubei province, China. Front Psychiatr. 2020;11:733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Huang JZ, Han MF, Luo TD, Ren AK, Zhou XP. [Mental health survey of medical staff in a tertiary infectious disease hospital for COVID‐19]. Zhonghua Lao Dong Wei Sheng Zhi Ye Bing Za Zhi. 2020;38(3):192‐195. [DOI] [PubMed] [Google Scholar]
- 43. Wu K, Wei X. Analysis of psychological and sleep status and exercise rehabilitation of front‐line clinical staff in the fight against COVID‐19 in China. Med Sci Monit Basic Res. 2020;26:e924085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Liu Y, Wang L, Chen L, Zhang X, Bao L, Shi Y. Mental health status of paediatric medical workers in China during the COVID‐19 outbreak. Front Psychiatry. 2020;11(702). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Yin Q, Sun Z, Liu T, et al. Posttraumatic stress symptoms of health care workers during the corona virus disease 2019. Clin Psychol Psychotherapy. 2020;27(3):384‐395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Cai Q, Feng H, Huang J, et al. The mental health of frontline and non‐frontline medical workers during the coronavirus disease 2019 (COVID‐19) outbreak in China: a case‐control study. J Affect Disord. 2020;275:210‐215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Zhao K, Zhang G, Feng R, et al. Anxiety, depression and insomnia: a cross‐sectional study of frontline staff fighting against COVID‐19 in Wenzhou, China. Psychiatr Res 2020;15:92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Wang Y‐X, Guo H‐T, Du X‐W, Song W, Lu C, Hao W‐N. Factors associated with post‐traumatic stress disorder of nurses exposed to corona virus disease 2019 in China. Medicine. 2020;99(26):e20965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Leng M, Wei L, Shi X, et al. Mental distress and influencing factors in nurses caring for patients with COVID‐19. Nurs Crit Care. 2021;26(2):94‐101. doi: 10.1111/nicc.12528 [DOI] [PubMed] [Google Scholar]
- 50. Zhang WR, Wang K, Yin L, et al. Mental health and psychosocial problems of medical health workers during the COVID‐19 epidemic in China. Psychother Psychosom. 2020;89(4):242‐250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Shechter A, Diaz F, Moise N, et al. Psychological distress, coping behaviors, and preferences for support among New York healthcare workers during the COVID‐19 pandemic. Gen Hosp Psychiatr. 2020;66:1‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Civantos AM, Byrnes Y, Chang C, et al. Mental health among otolaryngology resident and attending physicians during the COVID‐19 pandemic: national study. Head Neck. 2020;42(7):1597‐1609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Tan BYQ, Chew NWS, Lee GKH, et al. Psychological impact of the COVID‐19 pandemic on health care workers in Singapore. Ann Intern Med. 2020;173(4):317‐320. doi: 10.7326/m20-1083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Chew NWS, Lee GKH, Tan BYQ, et al. A multinational, multicentre study on the psychological outcomes and associated physical symptoms amongst healthcare workers during COVID‐19 outbreak. Brain Behav Immun. 2020;88(4):559‐565. doi:10.1016/j.bbi.2020.04.049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Chew NWS, Ngiam JN, Tan BY, et al. Asian‐Pacific perspective on the psychological well‐being of healthcare workers during the evolution of the COVID‐19 pandemic. BJPsych Open. 2020;6(6):e116. doi:10.1192/bjo.2020.98 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Behrens GMN, Cossmann A, Stankov MV, et al. Perceived versus proven SARS‐CoV‐2‐specific immune responses in health‐care professionals. Infection. 2020;48(4):631‐634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Brandstetter S, Roth S, Harner S, et al. Symptoms and immunoglobulin development in hospital staff exposed to a SARS‐CoV‐2 outbreak. Pediatr Allergy Immunol. 2020;31(7):841‐847. [DOI] [PubMed] [Google Scholar]
- 58. Korth J, Wilde B, Dolff S, et al. SARS‐CoV‐2‐specific antibody detection in healthcare workers in Germany with direct contact to COVID‐19 patients. J Clin Virol. 2020;128:104437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Schmidt SB, Grüter L, Boltzmann M, Rollnik JD. Prevalence of serum IgG antibodies against SARS‐CoV‐2 among clinic staff. PLoS One. 2020;15(6):e0235417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Kempker RR, Kempker JA, Peters M, et al. Loss of Smell and Taste Among Healthcare Personnel Screened for Coronavirus 2019. Clin Infect Dis. 2021;72(7):1244‐1246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Mani NS, Budak JZ, Lan KF, et al. Prevalence of COVID‐19 Infection and Outcomes Among Symptomatic Healthcare Workers in Seattle. Washington: Clinical Infectious Diseases; 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Demmer RT, Ulrich AK, Wiggen T, et al. Severe acute respiratory coronavirus virus 2 (SARS‐CoV‐2) screening among symptom‐free healthcare workers. Infect Control Hosp Epidemiol; 2021;1‐4. doi: 10.1017/ice.2021.81 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Cummings DA, Radonovich LJ, Gorse GJ, et al. Risk factors for healthcare personnel infection with endemic Coronaviruses (HKU1, OC43, NL63, 229E): results from the respiratory protection effectiveness clinical trial (ResPECT). Clinical Infectious Diseases; 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Stubblefield WB, Talbot HK, Feldstein L, et al. Seroprevalence of SARS‐CoV‐2 among frontline healthcare personnel during the first month of caring for COVID‐19 patients ‐ nashville, Tennessee. Clin Infect Dis. 2021;72(9):1645‐1648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Hartmann S, Rubin Z, Sato H, OYong K, Terashita D, Balter S. Coronavirus 2019 (COVID‐19) Infections Among Healthcare Workers, Los Angeles County. Clinical Infectious Diseases; 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Reusken CB, Buiting A, Bleeker‐Rovers C, et al. Rapid assessment of regional SARS‐CoV‐2 community transmission through a convenience sample of healthcare workers, The Netherlands, March 2020. Euro Surveill. 2020;25(12). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Tostmann A, Bradley J, Bousema T, et al. Strong associations and moderate predictive value of early symptoms for SARS‐CoV‐2 test positivity among healthcare workers, The Netherlands, March 2020. Euro Surveill. 2020;25(16). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Sikkema RS, Pas SD, Nieuwenhuijse DF, et al. COVID‐19 in health‐care workers in three hospitals in the south of The Netherlands: a cross‐sectional study. Lancet Infect Dis. 2020;20(11):1273‐1280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Kluytmans‐van den Bergh MFQ, Buiting AGM, Pas SD, et al. Prevalence and clinical presentation of health care workers with symptoms of coronavirus disease 2019 in 2 Dutch hospitals during an early phase of the pandemic. JAMA Network Open. 2020;3(5):e209673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Martin C, Montesinos I, Dauby N, et al. Dynamic of SARS‐CoV‐2 RT‐PCR positivity and seroprevalence among high‐risk health care workers and hospital staff. J Hosp Infect. 2020;106(1):102‐106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Garcia‐Basteiro AL, Moncunill G, Tortajada M, et al. Seroprevalence of antibodies against SARS‐CoV‐2 among health care workers in a large Spanish reference hospital. Nat Commun. 2020;11(1):3500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Moreno‐Casbas MT. Factors Related to SARS‐CoV‐2 Infection in Healthcare Professionals in Spain. The SANICOVI Project. Enferm Clin; 2020;30(6):360‐370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Álvarez Gallego M, Gortázar de Las Casas S, Pascual Migueláñez I, et al. SARS‐CoV‐2 pandemic on the activity and professionals of a General Surgery and Digestive Surgery Service in a tertiary hospital. Cir Esp. 2020;98(6):320‐327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Zheng L, Wang X, Zhou C, et al. Analysis of the infection status of the health care workers in Wuhan during the COVID‐19 outbreak: a cross‐sectional study. Clin Infect Dis. 2020;71(16):2109‐2113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Lai X, Wang M, Qin C, et al. Coronavirus disease 2019 (COVID‐2019) infection among health care workers and implications for prevention measures in a tertiary hospital in wuhan, China. JAMA Netw Open. 2020;3(5):e209666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Brown CS, Clare K, Chand M, et al. Snapshot PCR surveillance for SARS‐CoV‐2 in hospital staff in England. J Infect. 2020;81(3):427‐434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Bampoe S, Lucas DN, Neall G, et al. A cross‐sectional study of immune seroconversion to SARS‐CoV‐2 in frontline maternity health professionals. Anaesthesia. 2020;75(12):1614‐1619. [DOI] [PubMed] [Google Scholar]
- 78. Keeley AJ, Evans C, Colton H, et al. Roll‐out of SARS‐CoV‐2 testing for healthcare workers at a large NHS Foundation Trust in the United Kingdom, March 2020. Euro Surveill. 2020;25(14). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Felice C, Di Tanna GL, Zanus G, Grossi U. Impact of COVID‐19 outbreak on healthcare workers in Italy: results from a national E‐survey. J Community Health. 2020;45(4):675‐683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Lombardi A, Consonni D, Carugno M, et al. Characteristics of 1573 healthcare workers who underwent nasopharyngeal swab testing for SARS‐CoV‐2 in Milan, Lombardy, Italy. Clin Microbiol Infect. 2020;26(10):1413.e9‐1413.e13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Paderno A, Fior M, Berretti G, et al. SARS‐CoV‐2 Infection in Health Care Workers: Cross‐Sectional Analysis of an Otolaryngology Unit. Otolaryngol Head Neck Surg; 2020. [DOI] [PubMed] [Google Scholar]
- 82. Garzaro G, Clari M, Ciocan C, et al. COVID‐19 infection and diffusion among the healthcare workforce in a large university‐hospital in northwest Italy. Med Lav. 2020;111(3):184‐194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Lahner E, Dilaghi E, Prestigiacomo C, et al. Prevalence of sars‐Cov‐2 infection in health workers (HWs) and diagnostic test performance: the experience of a teaching hospital in Central Italy. Int J Environ Res Publ Health. 2020;17(12). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Muhi S, Irving LB, Buising KL. COVID‐19 in Australian health care workers: early experience of the Royal Melbourne Hospital emphasises the importance of community acquisition. Med J Aust. 2020;213(1):44‐e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Gheysarzadeh A, Sadeghifard N, Safari M, et al. Report of five nurses infected with severe acute respiratory syndrome coronavirus 2 during patient care: case series. New Microbes New Infect. 2020;36:100694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Chibwana MG, Jere KC, Kamng'ona R, et al. High SARS‐CoV‐2 seroprevalence in health care workers but relatively low numbers of deaths in urban Malawi. Wellcome Open Res; 2020;5(8):199‐214 doi: 10.12688/wellcomeopenres.16188.1 [DOI] [Google Scholar]
- 87. Wee LE, Sim XYJ, Conceicao EP, et al. Containment of COVID‐19 cases among healthcare workers: The role of surveillance, early detection, and outbreak management. Infect Control Hosp Epidemiol. 2020;41(7):765‐771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Contejean A, Leporrier J, Canouï E, et al. Comparing dynamics and determinants of severe acute respiratory syndrome coronavirus 2 transmissions among healthcare workers of adult and pediatric settings in central Paris. Clin Infect Dis. 2021;72(2):257‐264. doi: 10.1093/cid/ciaa977 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Maltezou HC, Dedoukou X, Tseroni M, et al. SARS‐CoV‐2 infection in healthcare personnel with high‐risk occupational exposure: evaluation of seven‐day exclusion from work policy. Clin Infect Dis. 2020;71(12):3182‐3187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Kassem AM, Talaat H, Shawky S, et al. SARS‐CoV‐2 infection among healthcare workers of a gastroenterological service in a tertiary care facility. Arab J Gastroenterology. 2020;21(3):151‐155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Al‐zoubi NA, Obeidat BR, Al‐Ghazo MA, et al. Prevalence of positive COVID‐19 among asymptomatic health care workers who care patients infected with the novel coronavirus: a retrospective study. Annals of Medicine and Surgery. 2020;57:14‐16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Jha S, Soni A, Siddiqui S, et al. Prevalence of flu‐like symptoms and COVID‐19 in healthcare workers from India. J Assoc Phys India. 2020;68(7):27‐29. [PubMed] [Google Scholar]
- 93. Çelebi G, Pişkin N, Bekleviç A, et al. Specific risk factors for SARS‐CoV‐2 transmission among health care workers in a university hospital. Am J Infect Control. 2020;48(10):1225–1230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. CDC‐COVID‐19Response‐Team . Characteristics of health care personnel with COVID‐19 ‐ United States, february 12‐april 9, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(15):477‐481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Levene LS, Coles B, Davies MJ, Hanif W, Zaccardi F, Khunti K. COVID‐19 cumulative mortality rates for frontline healthcare staff in England. Br J general Pract J R Coll General Pract. 2020;70(696):327‐328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Lapolla P, Mingoli A, Lee R. Deaths from COVID‐19 in healthcare workers in Italy‐What can we learn? Infect Control Hosp Epidemiol. 2021;42(3):364‐365. doi: 10.1017/ice.2020.241 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Bahadori M, Arab M, Sadeghifar J, Ahmadi B, Salimi M, Yghoubi M. Estimation of nursing staff in selected hospitals of ilam and ahvaz provinces, Western Iran. Nurs Midwifery Stud. 2013;2(2):217‐225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Rantanen I, Tuominen R. Relative magnitude of presenteeism and absenteeism and work‐related factors affecting them among health care professionals. Int Arch Occup Environ Health. 2011;84(2):225‐230. [DOI] [PubMed] [Google Scholar]
- 99. Nurchis MC, Pascucci D, Sapienza M, et al. Impact of the burden of COVID‐19 in Italy: results of disability‐adjusted life years (DALYs) and productivity loss. Int J Environ Res Publ Health. 2020;17(12). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100. Jo MW, Go DS, Kim R, et al. The burden of disease due to COVID‐19 in Korea using disability‐adjusted life years. J Kor Med Sci. 2020;35(21):e199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101. Wang J, Lee YF, Zhou M. What is the best timing for health care workers infected with COVID‐19 to return to work? Am J Infect Control. 2020;48(9):1128‐1129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102. Gianino MM, Politano G, Scarmozzino A, et al. Cost of sickness absenteeism during seasonal influenza outbreaks of medium intensity among health care workers. Int J Environ Res Publ Health. 2019;16(5). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103. Al Nuhait M, Al Harbi K, Al Jarboa A, et al. Sickness presenteeism among health care providers in an academic tertiary care center in Riyadh. J Infect Public Health. 2017;10(6):711‐715. [DOI] [PubMed] [Google Scholar]
- 104. Aysun K, Bayram S. Determining the level and cost of sickness presenteeism among hospital staff in Turkey. Int J Occup Saf Ergon. 2017;23(4):501‐509. [DOI] [PubMed] [Google Scholar]
- 105. van der Meer EW, Boot CR, van der Gulden JW, Jungbauer FH, Coenraads PJ, Anema JR. Hand eczema among healthcare professionals in The Netherlands: prevalence, absenteeism, and presenteeism. Contact Dermat 2013;69(3):164‐171. [DOI] [PubMed] [Google Scholar]
- 106. Allen D, Hines EW, Pazdernik V, Konecny LT, Breitenbach E. Four‐year review of presenteeism data among employees of a large United States health care system: a retrospective prevalence study. Hum Resour Health. 2018;16(1):59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107. Whiteford HA, Degenhardt L, Rehm J, et al. Global burden of disease attributable to mental and substance use disorders: findings from the Global Burden of Disease Study 2010. Lancet. 2013;382(9904):1575‐1586. [DOI] [PubMed] [Google Scholar]
- 108. Yang T, Guo Y, Ma M, Li Y, Tian H, Deng J. Job stress and presenteeism among Chinese healthcare workers: the mediating effects of affective Commitment. Int J Environ Res Publ Health. 2017;14(9). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109. Yang T, Ma M, Zhu M, et al. Challenge or hindrance: does job stress affect presenteeism among Chinese healthcare workers? J Occup Health. 2018;60(2):163‐171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110. Allemann A, Siebenhüner K, Hämmig O. Predictors of presenteeism among hospital employees‐A cross‐sectional questionnaire‐based study in Switzerland. J Occup Environ Med. 2019;61(12):1004‐1010. [DOI] [PubMed] [Google Scholar]
- 111. Brborovic H, Brborovic O, Mustajbegovic J. Looking for the possible association between stress, presenteeism and absenteeism among Croatian nurses: A cross‐sectional study. Iran J Psychiatry Behav Sci. 2016;10(4):4587‐4594. doi: 10.17795/ijpbs-4587 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated and/or analysed during the current study are available from the corresponding author upon reasonable request.


