Abstract
The objective of the present study is to investigate the incidence, characteristics and outcomes of patients who were readmitted to hospital emergency departments or required re‐hospitalisation following an index hospitalisation with a diagnosis of COVID‐19. A systematic review of PubMed, EMBASE and pre‐print websites was conducted between 1 January and 31 December 2020. Studies reporting on the incidence, characteristics and outcomes of patients with COVID‐19 who represent or require hospital admission were included. Two authors independently performed study selection and data extraction. Study quality was assessed with the Newcastle‐Ottawa Scale. Discrepancies were resolved by consensus or through an independent third reviewer. Data were synthesised according to the Preferred Reporting Items for Systematic Reviews guidelines. Six studies reporting on 547 readmitted patients were included. The overall incidence was 4.4%, most common in males (57.2%), and due to respiratory distress or prolonged COVID‐19. Readmitted patients had a shorter initial hospital length of stay (LOS) compared with those with a single hospitalisation (8.1 ± 10.6 vs 13.9 ± 10.2 days). The mean time to readmission was 7.6 ± 6.0 days; the mean LOS on re‐hospitalisation was 6.3 ± 5.6 days. Hypertension (odds ratio (OR) = 2.08; 95% confidence interval (CI) 1.69–2.55; P < 0.001; I 2 = 0%), diabetes mellitus (OR = 1.77; 95% CI 1.38–2.27; P < 0.001; I 2 = 0%) and chronic renal failure (OR = 2.37; 95% CI 1.09–5.14; P < 0.001; I 2 = 0%) were more common in these patients. Intensive care admission rates were similar between the two groups; 12.8% (22/172) of readmitted patients died. In summary, readmitted patients following an index hospitalisation for COVID‐19 were more commonly males with multiple comorbidities. Shorter initial hospital LOS and unresolved primary illness may have contributed to readmission.
Keywords: readmission, COVID‐19, rehospitalisation, mortality, systematic review, re‐presentation
Introduction
The Coronavirus disease 2019 (COVID‐19) pandemic, caused by the highly transmissible severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2), continues to be a worldwide health crisis, with many countries facing repeated surges in positive COVID‐19 cases, resulting in a rise in hospitalisations and ongoing strain on the healthcare system. 1 The clinical manifestation and outcomes of patients infected with COVID‐19 vary widely. 2 While the risk factors and characteristics of patients with COVID‐19 requiring hospitalisation are well documented, data pertinent to readmission rates in survivors are limited. Disease‐specific data on the outcomes for re‐hospitalised patients with COVID‐19 are essential to properly inform guidelines. Therefore, we conducted a rapid review to evaluate the incidence, characteristics and outcomes of patients who re‐presented to hospital emergency departments or required readmission following an index hospitalisation with a diagnosis of COVID‐19.
Methods
The present study was conducted in adherence with the Preferred Reporting Items for Systematic Reviews and Meta‐analyses (PRISMA) statement. 3 Figure 1 illustrates the consort flow diagram. We adopted the validated ‘rapid review’ methodology 4 while carrying out a literature search and pursuing through the relevant articles.
Figure 1.
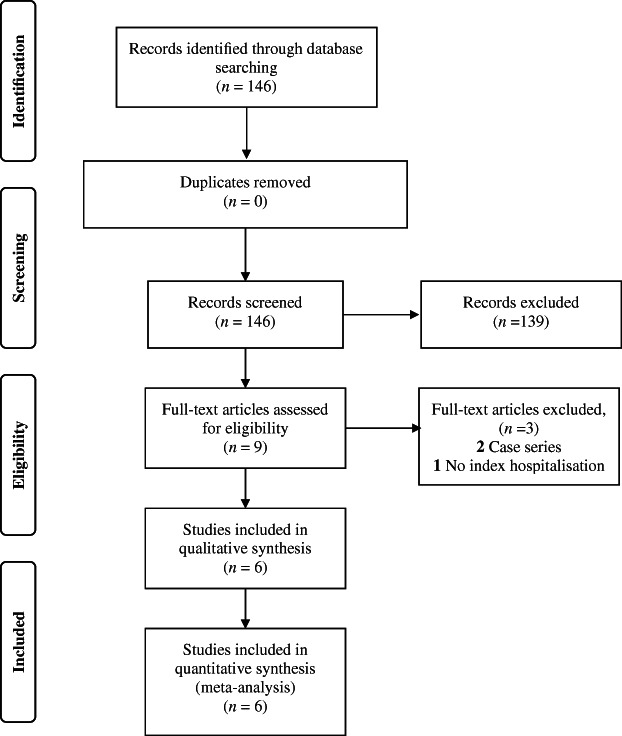
Preferred Reporting Items for Systematic Reviews and Meta‐analyses (PRISMA) consort flow diagra illustrating inclusion of studies for qualitative and quantitative analysis.
Eligibility criteria
Studies reporting on the incidence, characteristics and outcomes of consecutive patients with COVID‐19 who represent or require hospital admission were included.
Search strategy, information sources and study selection
Two authors (ZJL and AS) independently searched the publicly available COVID‐19 living systematic review. 5 This living systematic review is updated daily and provides a dynamic database of research papers related to COVID‐19 that are indexed by PubMed, EMBASE, MedRxiv, and BioRxiv. This has been validated in previously published COVID‐19‐related research. 6 Due to the rapidly evolving pandemic, preprint studies that were yet to be peer reviewed were included to capture as much data as possible. Studies were extracted between 1 January and 31 December 2020, using the search terms, ‘re‐admission’, ‘re‐present’ and ‘re‐admit’ with and without hyphenation within the title and the abstract columns of the systematic review list. These terms were combined with the Boolean operator ‘OR’. Preprint and non‐English language articles were included. The bibliography of each study was analysed to identify studies that may have been missed during the literature search.
Quality assessment and risk of bias in individual studies
The Newcastle‐Ottawa Scale (NOS) is a quality assessment tool used to evaluate non‐randomised studies based on an eight‐item score divided into three domains. 7 These domains assess selection, comparability and ascertainment of the outcome of interest. The Newcastle‐Ottawa Scale was used by the two reviewers (ZJL, MR) to independently evaluate the quality of included studies and assess for risk of bias. The same set of decision rules was used by each reviewer to score the studies. Any discrepancies from the NOS were reviewed and resolved by a third author (AS).
Data collection and analysis
Statistical analyses were conducted using Review Manager 5.4 (2020; The Cochrane Collaboration, London, UK). To enable an analysis of results between studies, median values were converted to means through an estimation formula (Supporting Information Table S1). 8 Categorical variables are presented as percentages, with between‐group differences compared using Fisher's exact tests. A two‐tailed P‐value <0.05 was considered significant. Equality of two proportions was evaluated using the Z‐test. The pooled prevalence and odds ratios (OR) were calculated across studies using random‐effects models of restricted maximum‐likelihood method. In the presence of heterogeneity (as expected and observed), random‐effect models have superior properties and are more conservative than fixed‐effect models. 9 Heterogeneity across the studies was evaluated using the Cochran Q test and quantified using I 2 statistic. Heterogeneity among studies was categorised as high (I 2: 76–100%), moderate (I 2: 26–75%) and low (I 2: 0–25%). 10 Subgroup analyses and meta‐regression were not conducted to explore the possible reasons of heterogeneity due to the relatively small number of studies and patients.
Results
A total of 146 studies were obtained from the living systematic review, with six studies across five countries (USA, South Korea, Spain, UK and Turkey) were included for qualitative and statistical analysis. 11 , 12 , 13 , 14 , 15 , 16 All studies were graded fair (Table S2).
The incidence, characteristics and outcomes across these studies are detailed in Table 1. The forest plots analysing gender and intensive care unit (ICU) admission is illustrated in Figure 2. A total of 547 patients with COVID‐19 re‐presented to emergency or required hospital readmission, representing an overall incidence of 4.4%. Most (52.5%) patients were re‐hospitalised due to respiratory distress or prolonged COVID‐19, which is due to lingering symptoms recurring disease after initial recovery. 11 , 13 , 14 , 15 , 16 Mean age was similar at 65.2 ± 16.4 years among patients who had a single admission compared with 65.7 ± 16.2 years among patients who were re‐hospitalised. There were more male patients in the readmission group (57.2%, 95% CI 53.0–61.4) than those who had a single admission (45.7%; 95% CI 44.7–46.6; OR = 1.46; 95% CI 1.22–1.76; P < 0.001). Among patients with a single hospital admission, mean hospital length of stay (LOS) was 13.9 ± 10.2 days, compared with 8.1 ± 10.6 days among patients who had a subsequent hospital admission. All six studies reported a shorter hospital LOS among patients who were re‐hospitalised. The mean time to re‐hospitalisation was 7.6 ± 6.0 days among patients who were readmitted to hospital following hospital discharge. Mean LOS during the second admission was 6.3 ± 5.6 days.
Table 1.
Selected studies
| Atalla et al. 11 | Jeon et al. 12 | Parra et al. 13 , † | Rokadiya et al. 15 | Uyaroğlu et al. 16 | Somani et al. 14 | Total, n (%, 95% CI) | |
|---|---|---|---|---|---|---|---|
| Location | Rhode Island, USA | South Korea | Madrid, Spain | London, UK | Ankara, Turkey | New York, USA | — |
| Newcastle Ottawa Scale‡ | Fair | Good | Good | Fair | Good | Fair | — |
| Sample size | |||||||
| Nil readmission | 320 | 7262 | 61† | 391 | 143 | 2761 | 12021§ |
| Readmission | 19 | 328 | 61 | 25 | 11 | 103¶ | 547 |
| Readmission rate (%) | 5.6 | 4.3 | 5.1 | 6.0 | 7.1% | 3.6 | 4.4 |
| Age, median (IQR) (years) | |||||||
| Nil readmission | 61 (49–74) | NR | 66 (57–76) | 59 (48–76) | 44 (NR) | 65.9 (54.5–77.0) | — |
| Readmission | 58 (44–69) | NR | 67 (59–76) | 73 (58–82) | 49 (NR) | 66.1 (53.7–75.1) | — |
| Age, derived mean (SD) (years) | |||||||
| Nil readmission | 61.3 (18.6) | NR | 66.3 (14.4) | 61.0 (20.8) | NR | 65.8 (16.9) | 65.2 (16.4) |
| Readmission | 57.0 (20.0) | NR | 67.3 (12.9) | 71.0 (18.9) | NR | 65.0 (16.1) | 65.7 (16.2) |
| Male, n (%) | |||||||
| Nil readmission | 179 (55.9) | 2925 (40.3) | 45 (73.8) | NR | 71 (49.7) | 1598 (57.9) | 4818/10547 (45.7, 44.7–46.6) |
| Readmission | 12 (63.2) | 170 (51.8) | 45 (73.8) | 15 (60.0) | 6 (54.5) | 65 (63.1) | 313/547 (57.2, 53.0–61.4) |
| Congestive heart failure, n (%) | |||||||
| Nil readmission | 30 (9.4) | 44 (0.6) | NR | NR | 7 (4.9) | NR | 240/10486 (2.3, 2.0–2.6) |
| Readmission | 2 (10.5) | 3 (0.9) | NR | NR | 0 (0.0) | NR | 13/461 (2.8, 1.5–4.8) |
| Ischaemic heart disease, n (%) | |||||||
| Nil readmission | NR | 143 (2.0) | 12 (19.7) | NR | NR | 220 (8.0) | 375/10084 (3.7, 3.4–4.1) |
| Readmission | NR | 7 (2.1) | 16 (26.2) | NR | NR | 12 (11.7) | 35/492 (7.1, 5.0–9.8) |
| Hypertension, n (%) | |||||||
| Nil readmission | 141 (44.1) | 890 (12.3) | 24 (39.3) | NR | 20 (14.0) | 610 (22.1) | 1685/10547 (16.0, 15.3–16.7) |
| Readmission | 13 (68.4) | 73 (22.3) | 34 (55.7) | 16 (64.0) | 5 (45.5) | 36 (35.0) | 177/547 (32.4, 28.5–36.5) |
| Diabetes mellitus, n (%) | |||||||
| Nil readmission | 103 (32.2) | 558 (7.7) | 10 (16.4) | NR | 17 (11.9) | 420 (15.2) | 1108/10547 (10.5, 9.9–11.1) |
| Readmission | 11 (57.9) | 46 (14.0) | 14 (23.0) | 6 (24.0) | 2 (18.2) | 19 (18.4) | 98/547 (17.9, 14.8–21.4) |
| Obesity, n (%) | |||||||
| Nil readmission | 125 (39.1) | NR | 5 (8.2) | NR | NR | NR | 130/381 (34.1, 29.4–39.1) |
| Readmission | 10 (52.6) | NR | 6 (9.8) | NR | NR | NR | 16/80 (20.0, 11.9–30.4) |
| COPD/asthma, n (%) | |||||||
| Nil readmission | 41 (12.8) | 712 (9.8) | 12 (19.7) | NR | 13 (9.1) | NR | 778/7786 (10.0, 9.3–10.7) |
| Readmission | 11 (57.9) | 42 (12.8) | 12 (19.7) | NR | 0 (0.0) | NR | 65/419 (15.5, 12.2–19.3) |
| Chronic renal failure, n (%) | |||||||
| Nil readmission | 32 (10.0) | 38 (0.5) | NR | NR | NR | NR | 70/7582 (0.9, 0.7–1.2) |
| Readmission | 4 (21.1) | 4 (1.2) | NR | NR | NR | NR | 8/347 (2.3, 1.0–4.5) |
| Liver disease, n (%) | |||||||
| Nil readmission | 8 (2.5) | 341 (4.7) | NR | NR | NR | NR | 349/7582 (4.6, 4.1–5.1) |
| Readmission | 3 (15.8) | 11 (3.4) | NR | NR | NR | NR | 14/347 (4.0, 2.2–6.7) |
| Cancer, n (%) | |||||||
| Nil readmission | 23 (7.2) | 266 (3.7) | 12 (19.7) | NR | 3 (2.1) | NR | 304/7786 (3.9, 3.5–4.4) |
| Readmission | 4 (21.1) | 16 (4.9) | 12 (19.7) | NR | 2 (18.2) | NR | 34/419 (8.1, 5.7–11.2) |
| ICU admission, n (%) | |||||||
| Nil readmission | 110 (34.4) | 758 (10.4) | 5 (8.2) | NR | NR | 524 (19.0) | 1397/10404 (13.4, 12.8–14.1) |
| Readmission | 6 (31.6) | 38 (11.6) | 3 (4.9) | 2 (8.0) | NR | 6 (5.8) | 55/511 (10.8, 8.2–13.8) |
| Mechanical ventilation, n (%) | |||||||
| Nil readmission | 64 (20.0) | NR | NR | NR | NR | 293 (10.6) | 357/3081 (11.6, 10.5–12.8) |
| Readmission | 3 (15.8) | NR | NR | NR | NR | 1 (0.97) | 4/122 (3.3, 0.9–8.2) |
| Hospital length of stay, median (IQR) (days) | |||||||
| Nil readmission | 8 (4–15) | 17 (10–24) | 9 (6–14) | 7 (4–11) | 4 (1–28) | 6.7 (3.5–11.5) | — |
| Readmission†† | 6 (3–12) | 9 (1–18) | 6 (4–14) | 6 (1–9) | 3 (2.5–5.5) | 4.7 (2.9–9.1) | — |
| Time to readmission | 5 (3–13) | NR | 6 (3–10) | 10 (6–15) | 8 (4–11.5) | 4.5 (NR) | — |
| Readmission‡‡ | 7 (4–9) | NR | NR | NR | 3 (1.5–4) | NR | — |
| Hospital length of stay, derived mean (SD) (days) | |||||||
| Nil readmission | 9 (8.2) | 17 (10.4) | 9.7 (6.1) | 7.3 (5.2) | 9.3 (5.1) | 7.2 (5.9) | 13.9 (10.2) |
| Readmission†† | 7 (5.6) | 9.3 (12.7) | 8 (7.6) | 5.3 (6.3) | 5.5 (6.9) | 5.6 (4.7) | 8.1 (10.6) |
| Time to readmission | 7.7 (6.1) | NR | 6.3 (5.3) | 10.3 (7.1) | 8.2 (5.2) | NR | 7.6 (6.0) |
| Readmission‡‡ | 7.9 (6.1) | NR | NR | NR | 3.5 (3.0) | NR | 6.3 (5.6) |
| Reason for admission, n (%) | |||||||
| Respiratory distress/prolonged COVID‐19 | 8 (42.1) | NR | 34 (55.7) | 14 (56.0) | 8 (72.7) | 51 (49.5) | 115/219 (52.5, 45.7–59.3) |
| Cardiac: heart failure, chest pain, AMI | NR | NR | 7 (11.5) | NR | NR | 6 (5.8) | 13/164 (7.9, 4.3–13.2) |
| Thrombotic episode | 2 (10.5) | NR | 10 (16.4) | NR | NR | NR | 12/80 (15.0, 8.0–24.7) |
| Fall/trauma | 1 (5.3) | NR | NR | NR | NR | 5 (4.9) | 6/122 (4.9, 1.8–10.4) |
| Others | 8 (42.1) | NR | 10 (16.4) | 11 (44.0) | 3 (27.3) | 41 (39.8) | 73/219 (33.3, 27.1–40.0) |
| Outcomes following readmission, n (%) | |||||||
| Death | 2 (10.5) | NR | 9 (14.7) | 6 (24.0) | 2 (18.2) | 3 (5.4)§§ | 22/172 (12.8, 8.2–18.7) |
| Still admitted | 1 (5.3) | NR | NR | 3 (12.0) | 0 (0.0) | 2 (3.6)§§ | 6/111 (5.4, 2.0–11.4) |
| Recovered | 16 (84.2) | NR | NR | 16 (64.0) | 9 (81.8) | 51 (91.1)§§ | 92/111 (82.9, 74.6–89.4) |
Parra et al.13 reported a matched (1:1) cohort. A total of 1144 patients had an initial admission but no hospital readmission.
Please refer Table S2 for Individual study quality by NOS score that was performed independently by two authors.
Total includes 1144 patients from Parra et al.,14 who had an initial admission but no hospital readmission.
Among 103 patients who re‐presented to hospital.
Length of stay during first hospital admission.
Length of stay during second hospital admission.
Among 56 patients who were admitted to hospital.
AMI, acute myocardial infarction; COPD, chronic obstructive pulmonary disease; ICU, intensive care unit; IQR, interquartile range; SD, standard deviation.
Figure 2.
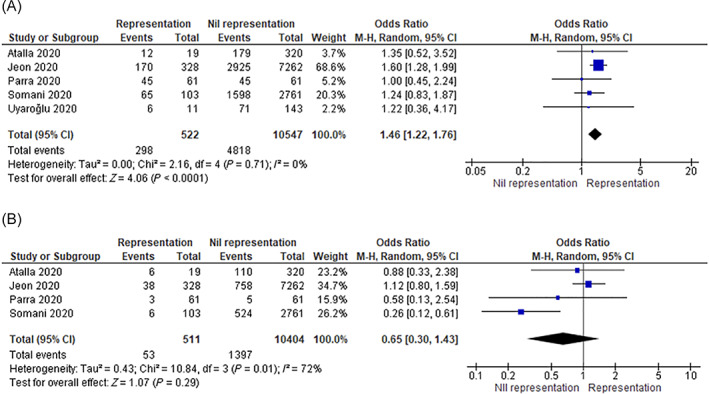
Forest plots representing characteristics in (A) male patients and (B) intensive care unit (ICU) admission. CI, confidence interval.
When analysing the comorbidities in patients who were readmitted in comparison to those who had a single admission, the frequency of ischaemic heart disease, hypertension, diabetes mellitus, chronic obstructive pulmonary disease or asthma, and cancer were higher and statistically significant among patients who were re‐hospitalised. Hypertension (OR = 2.08; 95% CI 1.69–2.55; P < 0.001; I 2 = 0%), diabetes mellitus (OR = 1.77; 95% CI 1.38–2.27; P < 0.001; I 2 = 0%) and chronic renal failure (OR = 2.37; 95% CI 1.09–5.14; P < 0.001; I 2 = 0%) were significantly more frequent among patients who were readmitted (Table 1, Fig. 3). The frequency of ICU admission was similar between both groups (OR = 0.65; 95% CI 0.30–1.43; P = 0.29) (Fig. 2). Across five studies, a total of 22 (12.8%) of 172 patients died following readmission. 11 , 13 , 14 , 15 , 16
Figure 3.
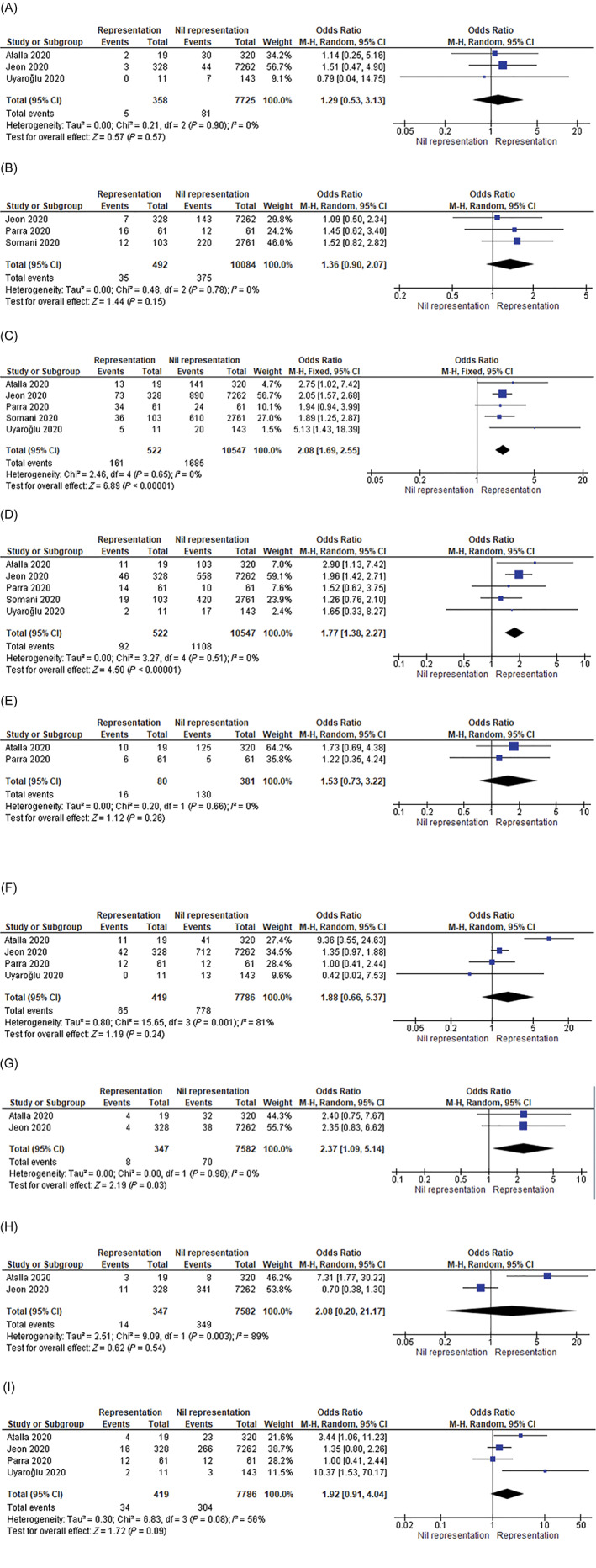
Forest plots comparing the comorbidities among patients who were readmitted compared with those with a single indexed admission. (A) Congestive heart failure; (B) ischaemic heart disease; (C) hypertension; (D) diabetes; (E) obesity; (F) chronic obstructive pulmonary disease (COPD)/asthma; (G) renal failure; (H) liver disease; and (I) cancer. CI, confidence interval.
Discussion
This is the first systematic review to examine the incidence, characteristics and outcomes of patients who re‐present to hospital following initial hospital discharge. Overall, patients who re‐presented were more likely male, and suffer from various comorbidities with hypertension, chronic renal failure and cancer being the most common.
Notably, patients who re‐presented to the hospital had an overall shorter initial hospital LOS, with COVID‐19‐related respiratory symptoms as the most common reason for re‐presentation. The reason for readmission may be due to an unresolved primary illness, potentially premature hospital discharges in the context of significant demand for hospital beds due to a surge in patients with COVID‐19, 17 limited patient care post‐discharge, 14 or repeat manifestation of disease again with symptoms or redetection following repeat testing. 12 Long‐term rehabilitation care for COVID‐19 survivors may aid in reducing both the incidence and mortality following hospital representation. 18
The overall hospital re‐presentation rate of 4.4% was lower compared with studies investigating the readmission rate for patients with seasonal influenza, where the readmission rate ranged from 10.2 to 14%. 19 , 20 This could be due to either saturated hospitals bed capacity or hospitals limiting admissions to preserve resources and limit exposure risk. In contrast, the mortality rate of 12.8% reported in this review was considerably higher when compared with 6.5–7% among patients with influenza. 19 , 20 In keeping with our findings, a recent study also identified the re‐hospitalisation rates or death were higher among patients with COVID‐19 than those with pneumonia or heart failure during the first 10 days after discharge following COVID‐19 hospitalisation, suggesting a period of heightened risk of clinical deterioration. 21 While the exact reason for the higher mortality rate is unclear, the potential biphasic illness course of COVID‐19 may have contributed to the increased mortality. 22
The present study has a few limitations that need to be addressed. First, the lack of age and disease stratification of COVID‐19, and overall small sample size of patients who were re‐hospitalised. Second, we could not describe the pooled difference of in‐hospital mortality between the patients with COVID‐19 who were re‐hospitalised with those patients who had a single admission. Additionally, the eventual outcome of patients who had one admission was not investigated in this review, where they may have died prior to re‐hospitalisation or presented to another hospital where the readmission was not captured in the reported study. The analysed re‐presentation time period was variable among studies, ranging 14−30 days. A more consistent evaluation over a 30‐day re‐presentation period is needed to effectively compare the re‐presentation rates with other known diseases.
Conclusion
This review identified that patients with COVID‐19 who re‐present to hospital following an index hospitalisation for COVID‐19 were more likely to be of male sex and suffer multiple comorbidities. Even though the re‐presentation rate was lower than that reported for seasonal influenza, mortality was much higher. Shorter initial hospital LOS and unresolved primary illness may have contributed to re‐presentation. Equally, patients might be presenting late, which leads to the higher mortality. Future studies are required to examine the reasons behind the higher mortality rate seen in patients who re‐present to hospitals following an index admission of COVID‐19.
Supporting information
Table S1 Equation used to calculate mean and standard deviation from median and interquartile range.
Table S2 Individual study quality by Newcastle Ottawa Scale (NOS) score.
Funding: K. Shekar acknowledges research support from Metro North Hospital and Health Service.
Conflict of interest: None.
References
- 1. Remuzzi A, Remuzzi G. COVID‐19 and Italy: what next? Lancet 2020; 395: 1225–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID‐19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA 2020; 323: 1239–42. [DOI] [PubMed] [Google Scholar]
- 3. Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta‐analyses: the PRISMA statement. BMJ 2009; 339: b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Tricco AC, Antony J, Zarin W, Strifler L, Ghassemi M, Ivory J et al. A scoping review of rapid review methods. BMC Med 2015; 13: 224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. COVID‐19 Open Access Project . Living evidence on COVID‐19. 2020. [cited 2021 February 12]. Available from URL: https://ispmbern.github.io/covid-19/living-review/
- 6. Wynants L, Van Calster B, Collins GS, Riley RD, Heinze G, Schuit E et al. Prediction models for diagnosis and prognosis of covid‐19: systematic review and critical appraisal. BMJ 2020; 369: m1328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Wells GA, Shea B, O'Connell D, Peterson J, Welch V, Losos M et al. The Newcastle‐Ottawa Scale (NOS) for Assessing the Quality of Nonrandomised Studies in Meta‐Analyses. [cited 2021 February 12]. Available from URL: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp
- 8. Wan X, Wang W, Liu J, Tong T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol 2014; 14: 135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Nyaga VN, Arbyn M, Aerts M. Metaprop: a Stata command to perform meta‐analysis of binomial data. Arch Public Health 2014; 72: 39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta‐analyses. BMJ 2003; 327: 557–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Atalla E, Kalligeros M, Giampaolo G, Mylona EK, Shehadeh F, Mylonakis E. Readmissions among patients with COVID‐19. Int J Clin Pract 2021; 75: e13700. [DOI] [PubMed] [Google Scholar]
- 12. Jeon WH, Seon JY, Park SY, Oh IH. Analysis of risk factors on readmission cases of COVID‐19 in the Republic of Korea: using nationwide health claims data. Int J Environ Res Public Health 2020; 17: 5844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Parra LM, Cantero M, Morras I, Vallejo A, Diego I, Jiménez‐Tejero E et al. Hospital readmissions of discharged patients with COVID‐19. Int J Gen Med 2020; 13: 1359–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Somani SS, Richter F, Fuster V, De Freitas JK, Naik N, Sigel K et al. Characterization of patients who return to hospital following discharge from hospitalization for COVID‐19. J Gen Intern Med 2020; 35: 2838–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Rokadiya S, Gil E, Stubbs C, Bell D, Herbert R. COVID‐19: outcomes of patients with confirmed COVID‐19 re‐admitted to hospital. J Infect 2020; 81: e18–e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Uyaroğlu OA, Başaran NÇ, Özişik L, Dİzman GİTİ, EroĞlu İ, Şahİn TK et al. Thirty‐day readmission rate of Covid‐19 patients discharged from a tertiary care university hospital in Turkey: an observational, single‐center study. Int J Qual Health Care 2020; 33: mzaa144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Oliver D. Covid‐19: hospital discharges during pandemic were often chaotic, says watchdog. BMJ 2020; 371: m4155. [DOI] [PubMed] [Google Scholar]
- 18. Halpin SJ, McIvor C, Whyatt G, Adams A, Harvey O, McLean L et al. Postdischarge symptoms and rehabilitation needs in survivors of COVID‐19 infection: a cross‐sectional evaluation. J Med Virol 2021; 93: 1013–22. [DOI] [PubMed] [Google Scholar]
- 19. Dobrzynski DM Jr, Ndi DN, Zhu Y, Markus T, Schaffner W, Talbot HK. Hospital readmissions after laboratory‐confirmed influenza hospitalization. J Infect Dis 2020; 222: 583–9. [DOI] [PubMed] [Google Scholar]
- 20. Yandrapalli S, Aronow WS, Frishman WH. Readmissions in adult patients following hospitalization for influenza: a nationwide cohort study. Ann Transl Med 2018; 6: 318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Donnelly JP, Wang XQ, Iwashyna TJ, Prescott HC. Readmission and death after initial hospital discharge among patients with COVID‐19 in a large multihospital system. JAMA 2021; 325: 304–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Lescure F‐X, Bouadma L, Nguyen D, Parisey M, Wicky P‐H, Behillil S et al. Clinical and virological data of the first cases of COVID‐19 in Europe: a case series. Lancet Infect Dis 2020; 20: 697–706. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1 Equation used to calculate mean and standard deviation from median and interquartile range.
Table S2 Individual study quality by Newcastle Ottawa Scale (NOS) score.


