Abstract
Objective
We aimed to explore the impact of telehealth in the setting of COVID‐19 on patient access to ambulatory rheumatologic care at our academic public health system and to determine whether telemedicine visits had a beneficial impact on access to our rheumatology ambulatory clinics.
Methods
We compared completed, no‐show, and cancellation rates between in‐person clinic visits and telemedicine appointments over a 10‐week time period before Ohio's initial executive order responding to COVID‐19 (premandate period) and a 10‐week time period afterward (postmandate period). Scheduling and appointment data were retrospectively extracted from the medical center's electronic health record.
Results
During the premandate period, when all visits were in‐person, the total number of completed visits was 930. The percentages of cancellations, no‐shows, and completed appointments of all appointment activities were 31.43%, 13.12%, and 55.46%, respectively. During the postmandate period, when telemedicine visits were added, the overall total number of completed visits was 1038. The percentages of cancellations, no‐shows, and completed appointments of all appointment activities were 53.45%, 13.91%, and 32.64%, respectively, for in‐person appointments and 0.12%, 8.48%, and 91.39%, respectively, for telemedicine appointments.
Conclusion
Telemedicine during the COVID‐19 pandemic resulted in higher rates of completed appointments and lower rates of missed appointments in the rheumatology outpatient clinic compared with in‐person visits during and prior to the pandemic.
Significance & Innovation.
Telemedicine offerings led to less missed ambulatory clinic appointments.
We explore the importance of telehealth during the COVID‐19 pandemic in a population of patients with rheumatic diseases.
INTRODUCTION
The COVID‐19 pandemic has impacted nations globally. Governments have implemented several rules and regulations in an effort to minimize the spread of the virus and mitigate its burden. The health care sector has been substantially affected by the novel coronavirus pandemic (1). Emergency department visits, medical center inpatient admissions, and intensive care unit admissions have surged in impacted areas. In the spring of 2020, officials in the State of Ohio recommended delaying nonurgent in‐person outpatient visits with health care providers and placed a hold on elective procedures and surgeries (2). As a result, many patients with chronic illnesses had reduced access to health care. This prompted the need to provide alternative care delivery options for patients that ensured safety for both patients and health care providers (3).
The MetroHealth System is an academic safety‐net health care institution that services the population of Cuyahoga County and surrounding counties in northeast Ohio. Within 1 week of the State of Ohio issuing a statewide order limiting gatherings in March 2020, the MetroHealth System expanded its outpatient access modalities, with an emphasis on telehealth. Telemedicine visits by video or telephone replaced traditional in‐person, face‐to‐face visits, except when in‐office visits were deemed medically necessary. Anecdotally, rheumatology providers reported improved clinic show rates with telemedicine visits, prompting this study.
Our aim was to investigate and compare visit completion rates before and after the state mandate to determine whether telemedicine visits had a beneficial impact on access to rheumatology ambulatory clinics. To achieve this, we compared outpatient visit adherence between a 10‐week time period before Ohio's initial executive order responding to COVID‐19 and a 10‐week time period immediately following the issuance of the initial executive order.
MATERIALS AND METHODS
This was a retrospective study of rheumatology appointment statuses in the outpatient setting of our health care system. All outpatient appointments (telehealth or otherwise) during the study were included. Using an electronic data querying tool native to our electronic health record, we collected data pertaining to rheumatology outpatient appointments at the MetroHealth System between January 3 and May 29, 2020 (pandemic period). Data between March 18 and May 24, 2019, were collected as a reference period. Appointments were allocated into one of three categories: 1) canceled, 2) no‐show, or 3) completed appointments. Data were entered into a Microsoft Excel spreadsheet, with visits segmented into in‐person versus telemedicine (video and telephone visits) and stratified by weekly increments.
For analysis, the data were divided into two 10‐week periods: period 1, the premandate interval between January 3 and March 15, 2020, and period 2, the postmandate period between March 16 and May 29, 2020. During the premandate period, the only modality was in‐person visits, whereas during the postmandate period, telemedicine visits started taking place in addition to in‐person visits. Appointment behavior in period 1 was found to be similar to that in a prepandemic reference period 1 year prior to the study period (March 18 to May 24, 2019), with similar cancellation, no‐show, and completed appointment rates (Supplementary Table 1), suggesting that appointment hesitancy due to COVID‐19 was not pervasive in the study population during the premandate period.
Because cancellations often occur in advance of the actual appointment date, appointment activity denoted the sum of cancellations, no‐shows, and completed visits. On‐schedule appointment totals summed no‐shows and completed visits, offering a surrogate of what a provider may see on their schedule on the actual appointment date. Rates of cancellations, no‐shows, and completed visits, as well as in‐person versus telemedicine visits, were compared with appointment activity totals as well as on‐schedule totals during the pre‐ and postmandate periods.
The following State of Ohio executive orders are highlighted (4): mass gatherings limited and/or prohibited (March 14, 2020), order to cancel elective procedures requiring personal protective equipment (March 18, 2020), stay‐at‐home order unless engaged in essential work or activity (March 22, 2020), limited reopening of businesses (May 1, 2020), order allowing restaurant dine‐in (May 14, 2020), reopening of gyms and fitness centers (May 22, 2020), and reopening of childcare service facilities (May 29, 2020).
Appointments with a rheumatology provider at our institution can be requested telephonically through a centralized call center, telephonically via a rheumatology staff member, in‐person with a clinic staff after completion of an in‐person appointment, or by self‐service scheduling through the electronic health record patient portal. In response to the COVID‐19 pandemic during the study period, the following scheduling actions were taken:
-
‐March 18, 2020:
- Centralized call center only offered telemedicine appointments.
- Self‐service patient portal scheduling was placed on hold.
- All existing scheduled appointments were converted to telemedicine appointments (patients were contacted by rheumatology and clinic staff) unless an in‐person visit was approved by the patient's rheumatology provider.
- Rheumatology staff and clinic‐based schedulers only offered telemedicine appointments unless an in‐person appointment was approved by the patient's rheumatology provider.
-
‐April 24, 2020:
- In‐person appointments were offered to patients new to rheumatology.
-
‐May 4, 2020:
- Patients were offered either in‐person or telemedicine appointments.
Results
Results of the data collection are shown in Tables 1 and 2. During the premandate period, when all visits were in‐person, total appointment activity was 1677, of which 527 appointments were canceled (31.43% of appointment activity) (Figure 1A). Two hundred twenty patients did not show up to their appointment, accounting for a no‐show rate of 13.12% of all appointment activity and 19.13% of on‐schedule appointments (Figure 1B). Nine hundred thirty patients (55.46% of appointment activity and 80.87% of on‐schedule appointments) completed their clinic visits (Figure 1C).
Table 1.
Weekly data for office visits pre‐COVID‐19 and during the COVID‐19 pandemic
| Week | Total visits | Office visit | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | Comp + NS | Total % | Canceled | Canceled % | NS | NS % | NS % per on schedule | Comp | Comp % | Comp % per on schedule | ||
| Week 1 | 165 | 165 | 96 | 100.00 | 69 | 41.82 | 25 | 15.15 | 26.04 | 71 | 43.03 | 73.96 |
| Week 2 | 130 | 130 | 89 | 100.00 | 41 | 31.54 | 18 | 13.85 | 20.22 | 71 | 54.62 | 79.78 |
| Week 3 | 178 | 178 | 114 | 100.00 | 64 | 35.96 | 22 | 12.36 | 19.30 | 92 | 51.69 | 80.70 |
| Week 4 | 182 | 182 | 131 | 100.00 | 51 | 28.02 | 22 | 12.09 | 16.79 | 109 | 59.89 | 83.21 |
| Week 5 | 177 | 177 | 119 | 100.00 | 58 | 32.77 | 23 | 12.99 | 19.33 | 96 | 54.24 | 80.67 |
| Week 6 | 184 | 184 | 127 | 100.00 | 57 | 30.98 | 23 | 12.50 | 18.11 | 104 | 56.52 | 81.89 |
| Week 7 | 160 | 160 | 113 | 100.00 | 47 | 29.38 | 20 | 12.50 | 17.70 | 93 | 58.13 | 82.30 |
| Week 8 | 160 | 160 | 122 | 100.00 | 38 | 23.75 | 21 | 13.13 | 17.21 | 101 | 63.13 | 82.79 |
| Week 9 | 159 | 159 | 116 | 100.00 | 43 | 27.04 | 16 | 10.06 | 13.79 | 100 | 62.89 | 86.21 |
| Week 10 | 182 | 182 | 123 | 100.00 | 59 | 32.42 | 30 | 16.48 | 24.39 | 93 | 51.10 | 75.61 |
| Total | 1677 | 1677 | 1150 | 100.00 | 527 | 31.43 | 220 | 13.12 | 19.13 | 930 | 55.46 | 80.87 |
| Average | 0 | 31.37 | 13.11 | 55.52 | ||||||||
| SD | 0 | 5.00 | 1.76 | 6.07 | ||||||||
| Week 11 | 312 | 192 | 63 | 61.54 | 129 | 67.19 | 31 | 16.15 | 49.21 | 32 | 16.67 | 50.79 |
| Week 12 | 149 | 33 | 5 | 22.15 | 28 | 84.85 | 2 | 6.06 | 40.00 | 3 | 9.09 | 60.00 |
| Week 13 | 157 | 50 | 16 | 31.85 | 34 | 68.00 | 5 | 10.00 | 31.25 | 11 | 22.00 | 68.75 |
| Week 14 | 142 | 46 | 12 | 32.39 | 34 | 73.91 | 4 | 8.70 | 33.33 | 8 | 17.39 | 66.67 |
| Week 15 | 167 | 66 | 18 | 39.52 | 48 | 72.73 | 6 | 9.09 | 33.33 | 12 | 18.18 | 66.67 |
| Week 16 | 138 | 55 | 21 | 39.86 | 34 | 61.82 | 7 | 12.73 | 33.33 | 14 | 25.45 | 66.67 |
| Week 17 | 181 | 111 | 67 | 61.33 | 44 | 39.64 | 12 | 10.81 | 17.91 | 55 | 49.55 | 82.09 |
| Week 18 | 163 | 115 | 63 | 70.55 | 52 | 45.22 | 18 | 15.65 | 28.57 | 45 | 39.13 | 71.43 |
| Week 19 | 151 | 100 | 70 | 66.23 | 30 | 30.00 | 17 | 17.00 | 24.29 | 53 | 53.00 | 75.71 |
| Week 20 | 135 | 102 | 70 | 75.56 | 32 | 31.37 | 19 | 18.63 | 27.14 | 51 | 50.00 | 72.86 |
| Total | 1695 | 870 | 405 | 51.33 | 465 | 53.45 | 121 | 13.91 | 29.88 | 284 | 32.64 | 70.12 |
| Average | 50.21 | 57.11 | 12.61 | 30.28 | ||||||||
| SD | 18.94 | 19.38 | 4.19 | 16.31 | ||||||||
Abbreviations: Comp, completed; NS, no‐show.
Table 2.
Weekly data for telemedicine visits pre‐COVID‐19 and during the COVID‐19 pandemic
| Week | Telemedicine | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | Comp + NS | Total % | Canceled | Canceled % | NS | NS % | NS % per on schedule | Comp | Comp % | Comp % per on schedule | |
| Week 1 | 0 | 0 | 0.00 | 0 | 0.00 | 0 | 0.00 | 0.00 | 0 | 0.00 | 0.00 |
| Week 2 | 0 | 0 | 0.00 | 0 | 0.00 | 0 | 0.00 | 0.00 | 0 | 0.00 | 0.00 |
| Week 3 | 0 | 0 | 0.00 | 0 | 0.00 | 0 | 0.00 | 0.00 | 0 | 0.00 | 0.00 |
| Week 4 | 0 | 0 | 0.00 | 0 | 0.00 | 0 | 0.00 | 0.00 | 0 | 0.00 | 0.00 |
| Week 5 | 0 | 0 | 0.00 | 0 | 0.00 | 0 | 0.00 | 0.00 | 0 | 0.00 | 0.00 |
| Week 6 | 0 | 0 | 0.00 | 0 | 0.00 | 0 | 0.00 | 0.00 | 0 | 0.00 | 0.00 |
| Week 7 | 0 | 0 | 0.00 | 0 | 0.00 | 0 | 0.00 | 0.00 | 0 | 0.00 | 0.00 |
| Week 8 | 0 | 0 | 0.00 | 0 | 0.00 | 0 | 0.00 | 0.00 | 0 | 0.00 | 0.00 |
| Week 9 | 0 | 0 | 0.00 | 0 | 0.00 | 0 | 0.00 | 0.00 | 0 | 0.00 | 0.00 |
| Week 10 | 0 | 0 | 0.00 | 0 | 0.00 | 0 | 0.00 | 0.00 | 0 | 0.00 | 0.00 |
| Total | 0 | 0 | 0 | 0 | 0.00 | 0 | 0.00 | ||||
| Average | 0 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | |||||
| SD | 0 | 0.00 | 0.00 | 0.00 | 0.00 | ||||||
| Week 11 | 120 | 120 | 38.46 | 0 | 0.00 | 10 | 8.33 | 8.33 | 110 | 91.67 | 91.67 |
| Week 12 | 116 | 115 | 77.85 | 1 | 0.86 | 10 | 8.62 | 8.70 | 105 | 90.52 | 91.30 |
| Week 13 | 107 | 107 | 68.15 | 0 | 0.00 | 15 | 14.02 | 14.02 | 92 | 85.98 | 85.98 |
| Week 14 | 96 | 96 | 67.61 | 0 | 0.00 | 5 | 5.21 | 5.21 | 91 | 94.79 | 94.79 |
| Week 15 | 101 | 101 | 60.48 | 0 | 0.00 | 1 | 0.99 | 0.99 | 100 | 99.01 | 99.01 |
| Week 16 | 83 | 83 | 60.14 | 0 | 0.00 | 7 | 8.43 | 8.43 | 76 | 91.57 | 91.57 |
| Week 17 | 70 | 70 | 38.67 | 0 | 0.00 | 7 | 10.00 | 10.00 | 63 | 90.00 | 90.00 |
| Week 18 | 48 | 48 | 29.45 | 0 | 0.00 | 8 | 16.67 | 16.67 | 40 | 83.33 | 83.33 |
| Week 19 | 51 | 51 | 33.77 | 0 | 0.00 | 3 | 5.88 | 5.88 | 48 | 94.12 | 94.12 |
| Week 20 | 33 | 33 | 24.44 | 0 | 0.00 | 4 | 12.12 | 12.12 | 29 | 87.88 | 87.88 |
| Total | 825 | 824 | 48.67 | 1 | 0.12 | 70 | 8.48 | 8.50 | 754 | 91.39 | 91.50 |
| Average | 49.79 | 0.09 | 8.98 | 90.93 | |||||||
| SD | 18.94 | 0.27 | 4.52 | 4.52 | |||||||
Abbreviations: Comp, completed; NS, no‐show.
Figure 1.
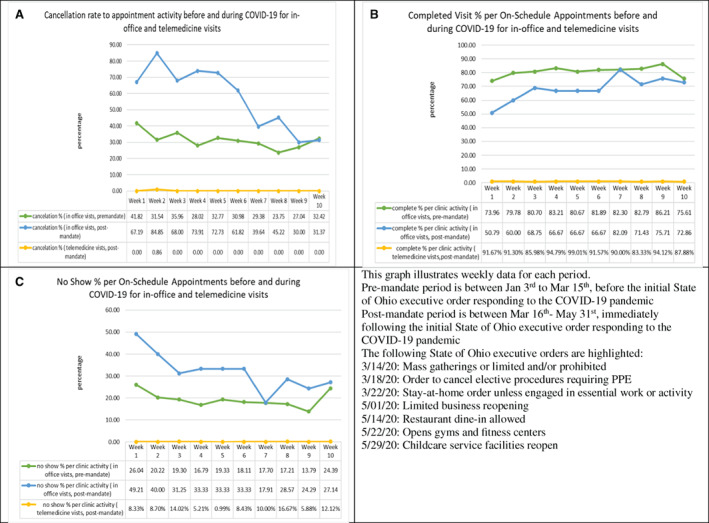
Weekly data for each period. A, Cancellation rate to appointment activity before and during COVID‐19 for in‐office and telemedicine visits. B, Completed visit percentage per on schedule appointment before and during COVID‐19 for in‐office and telemedicine visits. C, No show percentage per on schedule appointments before and during COVID‐19 for in‐office and telemedicine visits. PPE, personal protective equipment.
During the postmandate period, the total appointment activity was 1695, with an in‐person appointment activity of 857 (51.33%) and a telemedicine appointment activity of 825 (48.67%). This resulted in 1229 total on‐schedule appointments, of which 405 (33.0%) were in‐person and 824 (67.1%) were telemedicine appointments.
The total number of canceled in‐person appointments was 465 (59.45% of total in‐person appointment activity), compared with only one telemedicine appointment that was canceled during the same period (0.12% of total telemedicine appointment activity) (Figure 1A). The total number of no‐shows was 121 for the in‐person appointments (13.91% of total in‐person appointment activity, 29.88% of total in‐person on‐schedule appointments), compared with 70 telemedicine appointments no‐shows (8.48% of total telemedicine appointment activity, 8.50% of total telemedicine on‐schedule appointments) (Figure 1B). The total number of completed in‐person appointments was 284 (32.64% of total in‐person appointment activity, 70.12% of total in‐person on‐schedule appointments), compared with 754 completed telemedicine appointments (91.39% of total telemedicine appointment activity, 91.50% of total telemedicine on‐schedule appointments) (Figure 1C).
The total number of completed appointments increased to 1038 in the postmandate period, when both in‐person and telemedicine appointments were offered, in comparison with the 930 completed visits in the premandate period, when only in‐person visits were available. Of the 1038 completed appointments, in‐person appointments numbered 284 (27.40% of all completed visits during the postmandate period), compared with 754 telemedicine appointments (72.60% of all completed visits during the postmandate period).
The average percentage of completed visits per appointment activity decreased during the postmandate period for in‐person visits (30.28%) but increased for telemedicine visits (90.93%) compared with the premandate period (55.52%) and the reference period (62.07%).
The average percentage of no‐show visits per appointment activity was similar during all studied periods (12.61%‐13.11%) for in‐person visits but was lower for telemedicine visits during the postmandate period (8.89%).
Cancellations were highest for in‐person visits during the postmandate period, with an average of 57% per appointment activity, compared with 31% during the premandate period and 24% during the reference period. The cancellation rate was almost zero for telemedicine visits during the COVID‐19 pandemic.
Discussion
The COVID‐19 pandemic prompted the rapid implementation of telemedicine visits in MetroHealth's rheumatology division. Starting in March 2020, hospital systems across the country moved to postpone procedures and cancel face‐to‐face visits because of the potential risk of infection with the novel coronavirus. However, pandemics pose an increased demand for medical care (5). Patients with rheumatic diseases may have to weigh risks and benefits of travelling to medical facilities for care, exposing themselves to crowds and sick individuals, because many patients face an increased risk for infection due to immunosuppressive medications as well as immune system dysfunction related to their diseases (6). It was noted early in the pandemic that patients with connective tissue disease were avoiding medical care and interrupting their disease‐modifying antirheumatic drugs without medical guidance from their physicians because of fear of contracting the virus (7). Although a “business as usual” approach with in‐person visits may place patients at risk for contracting the virus, delaying care can increase the risk for disease flares and the potential need for hospitalization. The rheumatology patient population often requires close clinical and laboratory monitoring to maintain optimal health, and telemedicine provides a means to maintain necessary follow‐up while reducing risk.
Telemedicine has been practiced even before the COVID‐19 pandemic; almost 15% of physicians in the United States have worked in practices that offer telehealth (8). This has been applied in critically ill patients and in palliative care settings (3), as well as in the context of stroke through telestroke and mobile stroke units that allow providers to remotely assess and manage patients who have had strokes (8, 9). Telehealth was successfully implemented in Sichuan Province in Western China February 1, 2020, as a response to the COVID‐19 pandemic, where patients were offered consultations, drug prescriptions, and delivery remotely (5). In the United States, restrictions on telemedicine services for Medicare part B beneficiaries were waived in response to the COVID‐19 pandemic (1135 Waiver) (10).
The offering of telemedicine visits had seemingly favorable impacts on access to rheumatology ambulatory clinics at our academic public health system. Telemedicine appointment cancellations were nearly zero (1 of 825 telemedicine appointments offered) during the postmandate period compared with the premandate period, during which 527 appointments were canceled out of 1677 appointments offered, all in‐person appointments. No‐shows also trended down in the postmandate period; there were 191 no‐shows (121 in‐person and 70 telemedicine) versus 220 no‐shows in the premandate period (all in‐person). This led to a slight increase in completed visits during the postmandate period, when there were 1038 completed appointments (754 telemedicine and 284 in‐person); whereas premandate, there were only 930 completed in‐person appointments.
In the field of rheumatology, the patient population includes older patients and very ill patients; many among them may have barriers to accessing in‐person, on‐facility health care because of transportation or other issues. Video and telephone visits that do not require patients to be on‐site at the medical facility offer patient convenience and may reduce barriers to accessing health care. Also, some rheumatology concerns may be less reliant on the need for a physical examination, such as titrating medication to reach a particular uric acid level when treating gout. Conversely, visits that require diagnostic or therapeutic procedures, such as joint injection or ultrasound, will always require in‐person visits, and physical examinations are essential when establishing new diagnoses or adjusting therapies for patients with active disease.
This study suggests that telemedicine visits increased patient adherence to their clinic appointments through their adherence to telemedicine appointments. Completed visit volume trended up during the intervention time period (postmandate) compared with the preintervention time period (premandate), and there were also lower no‐show rates in telemedicine compared with face‐to‐face visits. Although in‐person visits cannot always be replaced by phone or video visits, we believe that telemedicine's potential to increase the accessibility and convenience of health care makes it an essential component to the future of medicine.
According to the above findings, we encourage examining the incorporation of telemedicine in our routine clinic visits to improve patient's appointment adherence. More studies are needed to investigate telemedicine's impact on other parameters, including patient experience, access to technology, provider experience and decision‐making, patient and provider satisfaction, health outcomes based on traditional disease measurements, and other variables.
AUTHOR CONTRIBUTIONS
All authors were involved in drafting the article or revising it critically for important intellectual content, and all authors approved the final version to be published. Dr. Alkilany had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study conception and design
Alkilany, Hong.
Acquisition of data
Alkilany, Tarabichi.
Analysis and interpretation of data
Alkilany, Tarabichi, Hong.
Supporting information
Disclosure Form
Supplementary material: Table 1 (weekly data for office visits pre COVID‐19 pandemic during the year 2019 (Mar18th‐may24th)
ACKNOWLEDGMENTS
We would like to acknowledge Dr. Mustafa Abdulsada for his valuable input and substantial contribution to data analysis and revising the article.
No potential conflicts of interest relevant to this article were reported.
Author disclosures are available at https://onlinelibrary.wiley.com/action/downloadSupplement?doi=10.1002%2Facr2.11372&file=acr211372‐sup‐0001‐Disclosureform.pdf.
REFERENCES
- 1. Gadzinski AJ, Gore JL, Ellimoottil C, Odisho AY, Watts KL. Implementing telemedicine in response to the COVID‐19 pandemic. J Urol 2020;204:14–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. DeWine M. Executive order 2020‐01D. March 2020. URL: https://governor.ohio.gov/wps/portal/gov/governor/media/executive‐orders/executive‐order‐2020‐01‐d.
- 3. Calton B, Abedini N, Fratkin M. Telemedicine in the time of coronavirus. J Pain Symptom Manage 2020;60:e12–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Ohio Department of Health . Public health orders. URL: https://coronavirus.ohio.gov/wps/portal/gov/covid‐19/resources/public‐health‐orders/public‐health‐orders.
- 5. Hong Z, Li N, Li D, Li J, Li B, Xiong W et al. Telemedicine during the COVID‐19 pandemic: experiences from western China. J Med Internet Res 2020;22:e19577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Cron RQ, Chatham WW. The rheumatologist's role in COVID‐19. J Rheumatol 2020;47:639–42. [DOI] [PubMed] [Google Scholar]
- 7. George MD, Venkatachalam S, Banerjee S, Baker JF, Merkel PA, Gavigan K, et al. Concerns, healthcare use, and treatment interruptions in patients with common autoimmune rheumatic diseases during the COVID‐19 pandemic. J Rheumatol 2021;48:603–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Dorsey ER, Topol EJ. Telemedicine 2020 and the next decade. Lancet 2020;395:859. [DOI] [PubMed] [Google Scholar]
- 9. Hollander JE, Carr BG. Virtually perfect? Telemedicine for Covid‐19. N Engl J Med 2020;382:1679–81. [DOI] [PubMed] [Google Scholar]
- 10. Centers for Medicare & Medicaid Services . Medicare telemedicine health care provider fact sheet. 2020. URL: https://www.cms.gov/newsroom/fact‐sheets/medicare‐telemedicine‐health‐care‐provider‐fact‐sheet.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Disclosure Form
Supplementary material: Table 1 (weekly data for office visits pre COVID‐19 pandemic during the year 2019 (Mar18th‐may24th)


