Abstract
Aim
To elucidate the impact of the coronavirus disease 2019 (COVID‐19) on the practice of high‐resolution manometry (HRM) and peroral endoscopic myotomy (POEM) in Japan.
Methods
We utilized a large‐scale database involving 14 high‐volume centers in Japan to investigate changes in the numbers of HRM and POEM procedures performed and outcomes of POEM between 2019 and 2020. A questionnaire survey was also conducted to analyze pandemic‐associated changes in the HRM and POEM protocols.
Results
Compared to that in 2019, the number of HRM and POEM procedures decreased by 17.2% (1587–1314) and 20.9% (630–498), respectively. These declines were prominent during the state of emergency from April to May 2020, particularly in pandemic areas. HRM and POEM in nonpandemic areas were relatively unaffected. From 2019 to 2020, there was a 0.4% (254–248) decrease in POEM cases within the prefecture, but the number outside the prefecture decreased by 33.6% (372–247). During the pandemic, the safety and efficacy of POEM were maintained. The implementation of personal protective equipment (PPE) measures varied among facilities, and PPE for POEM was relatively insufficient compared to that for HRM.
Conclusion
The COVID‐19 pandemic influenced HRM and POEM practices in Japan. It is necessary to establish a sufficient system for HRM and POEM in each hospital as well as countrywide to overcome the effects of the pandemic.
Keywords: achalasia, COVID‐19, esophageal motility disorder, high‐resolution manometry, peroral endoscopic myotomy
INTRODUCTION
On January 30, 2020, the World Health Organization declared the outbreak of the coronavirus disease 2019 (COVID‐19) a global pandemic. At that time, 7818 cumulative confirmed cases and 170 deaths had been documented globally in 19 countries across five continents. 1 The severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) is highly infectious, resulting in both community‐acquired and nosocomial infections among healthcare professionals and patients, and limiting nonemergent investigations in clinical practice.
High‐resolution manometry (HRM) is the gold standard for the diagnosis of esophageal motility disorders (EMDs), including achalasia, 2 of which peroral endoscopic myotomy (POEM) is a novel treatment. 3 Although HRM and POEM have been available since the 2000s, 4 achalasia is a rare, benign disease, with an incidence of 1.0 per 100,000 person‐years, 5 and facilities for the diagnosis and treatment are not widely distributed over Japan. In 2020, treatment with POEM could only be performed at limited facilities (and not necessarily in each prefecture) in Japan based on clinical practice guidelines published by the Japan Gastroenterological Endoscopy Society (JGES). 6 Therefore, patients with suspected EMDs often had to cross prefectures for diagnosis and treatment. It is considered that travel restrictions during the pandemic of COVID‐19 negatively affected these patients.
Although outpatient and endoscopy guidelines for gastrointestinal diseases during the COVID‐19 pandemic have already been published by the Japanese Society of Gastroenterology (JSGE) and JGES, there are no clinical data concerning HRM and POEM, or on the effect of the COVID‐19 pandemic on motility and achalasia interventions in Japan. 7 , 8 It is critical to understand these patients’ state of care during the pandemic of COVID‐19 to design effective future pandemic strategies. Therefore, we designed a multicenter study including 14 high‐volume EMD centers distributed over Japan in both COVID‐19 pandemic and nonpandemic areas to elucidate the state of care of patients with EMDs during the COVID‐19 pandemic.
METHODS
Study design
The 14 institutions included in this study were distributed from the Tohoku through the Kyushu area. POEM was implemented at all 14 facilities, and HRM was conducted at 13 of them. This study was approved by the Ethics Committees of all the institutions (Table S1) and was conducted following the Declaration of Helsinki. Informed consent was obtained in the form of an opt‐out system on a website.
COVID‐19’s effect on the number and outcome of HRM and POEM
Study‐1 was conducted to elucidate the effect of the COVID‐19 pandemic for the number of HRM and POEM procedures, as well as the outcomes of POEM.
First, a study‐specific Excel spreadsheet was made to collect validated case data from each facility. Survey items included age, sex, home prefecture, body mass index (BMI), HRM diagnosis, 2 type of achalasia (straight, sigmoid, and advanced sigmoid 9 ), esophageal dilation (grade I–III 9 ), history of a previous procedure, American Society of Anesthesiologists physical status (ASA‐PS) classification, 10 Eckardt score, date of HRM and POEM, and adverse events. The Eckardt score is composed of the sum of 4‐point scores for dysphagia, regurgitation, chest pain, and weight loss; 11 a higher score reflects more severe symptoms, while a lower score indicates milder symptoms. Clinical success was defined as a postoperative Eckardt score ≤3 in cases with a preoperative Eckardt score ≥4 or decreased Eckardt score in cases with a preoperative Eckardt score of <4, and no reinterventions. 12 The severity of adverse events was graded into seven types using the Clavien–Dindo classifications (I–V). 13
Using the large‐scale database, the numbers of HRM and POEM procedures per month between 2019 and 2020 were analyzed, and the numbers in the pandemic and nonpandemic areas were compared. Furthermore, the number of patients crossing their prefecture for POEM was also investigated. Finally, the outcomes of POEM were compared between 2019 and 2020.
Questionnaire survey for HRM and POEM
In study‐2, a questionnaire survey was conducted to investigate the implementation of various protocols and infection control practices related to COVID‐19 by clinicians performing HRM and POEM in each facility. The questionnaire consisted of multiple questions in the following categories: (1) restriction on the number of HRM and POEM procedures, (2) period of restriction on the number of HRM and POEM procedures, (3) capacity of HRM and POEM at the time of restriction, (4) reasons for the decrease in the number of HRM and POEM procedures, (5) restriction on referral of patients receiving POEM from outside the prefecture, (6) COVID‐19 prescreening, (7) HRM performed in a room with or without negative pressure function, (8) extension of hospital stay, and (9) personal protective equipment (PPE) worn by clinicians performing HRM and POEM.
Statistics
Continuous variables are reported as the mean ± standard deviation and compared using the t‐test. Categorical variables are expressed as number (%) and compared using the Chi‐squared test (or Fisher’s exact test for small sample sizes). To compare the number of HRM and POEM procedures by region, pandemic areas were defined as prefectures with 15 or more new infections per 100,000 population, and nonpandemic areas were defined as prefectures with 14 or less new infections per 100,000 population in the last week during the state of emergency (Table S1). To evaluate clinical outcomes of POEM over COVID‐19 pandemic, we compared adverse events and clinical success of POEM between 2019 and 2020. We compared the numbers of HRM and POEM procedures in each month, and referral within or from out of the prefecture between 2019 and 2020 using a binomial test. P < 0.05 was considered statistically significant. Statistical analyses were performed using the SPSS v. 26.0 for Windows (SPSS, Tokyo, Japan).
RESULTS
COVID‐19 pandemic status in Japan
In Japan, the first wave of the COVID‐19 pandemic occurred from March to May 2020; the second from July to September 2020, and the third began in November 2020. The Japanese government declared a state of emergency from April 7 to May 25 in 2020, which required the public to stay at home and avoid nonessential outings and cross‐prefecture movements (Fig. 1a). 14
Figure 1.
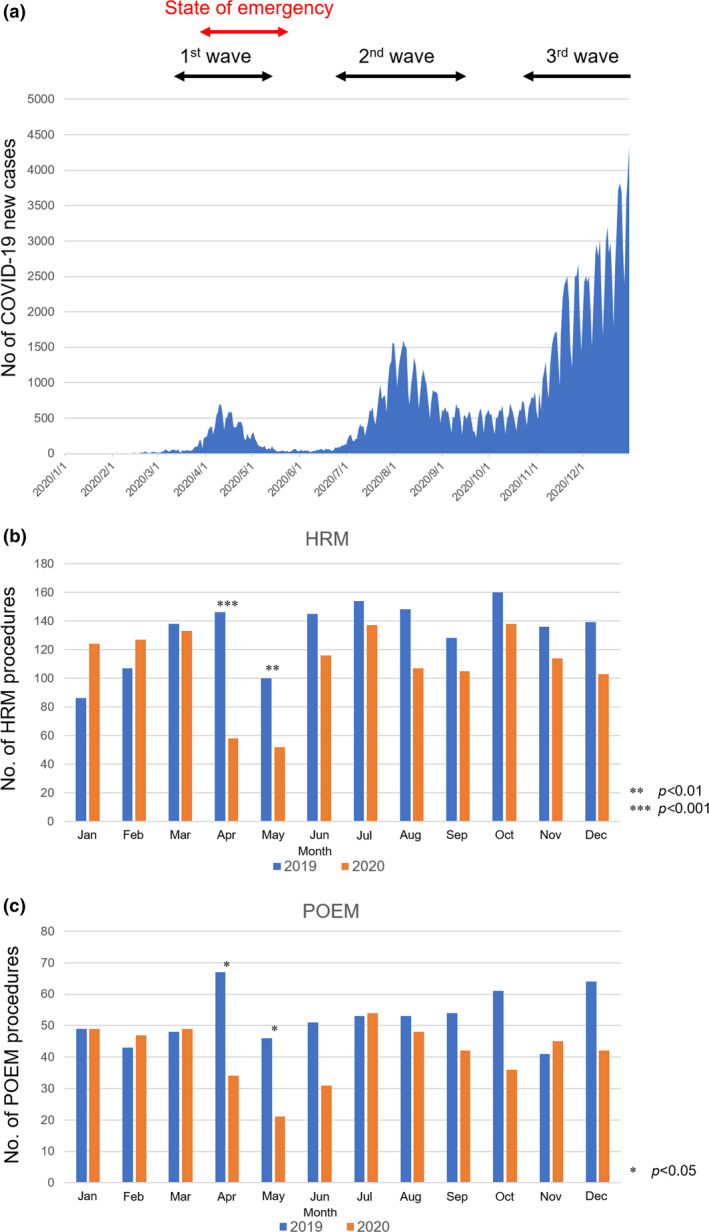
COVID‐19 pandemic status and the number of HRM and POEM procedures. (a) The number of infected people and definition of the term of the first to third wave and the state of emergency during the 2020 pandemic. (b) The number of HRM per month between 2019 and 2020. (c) The number of POEM per month between 2019 and 2020. Asterisk shows the months with a statistically significance difference in the numbers between 2019 and 2020. COVID‐19, coronavirus disease 2019; HRM, high‐resolution manometry; POEM, peroral endoscopic myotomy.
COVID‐19 pandemic reduced the number of HRM and POEM procedures
The numbers of HRM and POEM procedures performed are summarized in Figure 1b,c, respectively. These numbers decreased dramatically in April and May 2020 as compared to the numbers in the same months in 2019. From April 2019 to April 2020, the number of HRM procedures decreased from 146 to 58 (–60.3%; P < 0.001). From May 2019 to May 2020, the number of HRM procedures decreased from 100 to 52 (–48.0%; P = 0.001). Similarly, from April 2019 to April 2020, the number of POEM procedures decreased from 67 to 34 (–49.3%; P = 0.016). From May 2019 to May 2020, the number of POEM procedures decreased from 46 to 21 (–54.3%; P = 0.037). The number of HRM and POEM procedures also declined during the second and third waves, but not as drastically as during the first wave. There was no rebound in the number of HRM and POEM after the state of emergency was lifted.
The total number of HRM and POEM at all facilities in 2020 decreased by 17.2% (1587–1314) and 20.9% (630–498), respectively, compared to that in 2019 (P < 0.001 and P < 0.001, respectively) (Fig. 2a,b). The rate of decrease in the number of HRM in pandemic areas was significantly higher than that in nonpandemic areas (1238–980 [–20.8%] vs. 349–334 [–4.3%], respectively; P = 0.030). The rate of decrease in the number of POEM in pandemic areas was also significantly higher than that in nonpandemic areas (488–358 [–26.6%] vs. 142–140 [–1.4%], respectively; P = 0.032).
Figure 2.
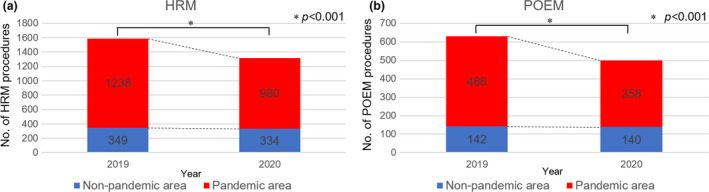
The total number of HRM and POEM procedures. (a) The total number of HRM procedures in pandemic and nonpandemic areas. (b) The total number of POEM procedures in pandemic and nonpandemic areas. In the pandemic area, the numbers of HRM and POEM procedures significantly decreased from 2019 to 2020, although the nonpandemic area had no statistical significance. HRM, high‐resolution manometry; POEM, peroral endoscopic myotomy.
COVID‐19 severely affected patients with achalasia crossing the prefecture
From 2019 to 2020, the decrease in POEM cases within the prefecture was 0.4% (254–248), but the number of cases referred from outside the prefecture decreased by 33.6% (372–247) (P < 0.001). The relative rate of cases referred from outside the prefecture decreased from 59.1% in 2019 to 49.6% in 2020 (P < 0.001), while the rate of cases within the prefecture increased from 40.3% in 2019 to 49.8% in 2020 (P = 0.823) (Table 1).
Table 1.
The impact of the coronavirus disease 2019 pandemic on peroral endoscopic myotomy referral within and from outside of the prefecture
| 2019 | 2020 | Year‐on‐year rate | P‐value | |
|---|---|---|---|---|
| Total | 630 | 498 | –132 (–21.0%) | <0.001 |
| Referral within the prefecture | 254 (40.3%) | 248 (49.8%) | –6 (–0.4%) | 0.823 |
| Referral from outside of the prefecture | 372 (59.1%) | 247 (49.6%) | –125 (–33.6%) | <0.001 |
The number of missing values for patients’ address was four (0.6%) in 2019, and three (0.6%) in 2020.
Clinical outcomes of POEM during the COVID‐19 pandemic
The clinical outcomes of POEM are summarized in Table 2. There were no significant differences in patient characteristics for POEM between 2019 and 2020. Adverse events were observed in 33 patients (5.2%) in 2019 and 37 patients (7.4%) in 2020 (P = 0.137). The clinical success of POEM was comparable between 2020 and 2019 (92.9% vs. 93.9%; P = 0.504). Three patients underwent a semi‐emergent POEM due to exacerbation of achalasia‐related symptoms during the state of emergency. There were no patients for whom the polymerase chain reaction (PCR) test for SARS‐CoV‐2 was positive and POEM was postponed.
Table 2.
Clinical outcomes of peroral endoscopic myotomy during the coronavirus disease 2019 pandemic
| 2019 (n = 630) | 2020 (n = 498) | P‐value | |
|---|---|---|---|
| Age, years, mean ± SD | 53.6 ± 17.4 | 53.1 ± 17.2 | 0.645 |
| Sex | 0.489 | ||
| Female | 304 (48.3%) | 230 (46.2%) | |
| Male | 326 (51.7%) | 268 (53.8%) | |
| BMI, kg/m2, mean ± SD | 21.6 ± 4.1 | 21.5 ± 4.0 | 0.770 |
| HRM diagnosis | 0.430 | ||
| Type I achalasia | 265 (42.1%) | 250 (50.2%) | |
| Type II achalasia | 189 (30.0%) | 126 (25.3%) | |
| Type III achalasia | 36 (5.7%) | 21 (4.2%) | |
| EGJOO | 19 (3.0%) | 14 (2.8%) | |
| Jackhammer esophagus | 12 (1.9%) | 8 (1.6%) | |
| Distal esophageal spasm | 13 (2.1%) | 9 (1.8%) | |
| Others* | 96 (15.2%) | 70 (14.1%) | |
| Type of achalasia | 0.775 | ||
| Straight | 469 (74.4%) | 367 (73.7%) | |
| Sigmoid | 125 (19.9%) | 107 (21.5%) | |
| Advanced sigmoid | 36 (5.7%) | 24 (4.8%) | |
| Esophageal dilation | 0.051 | ||
| Grade I | 326 (51.8%) | 226 (45.4%) | |
| Grade II | 273 (43.3%) | 252 (50.6%) | |
| Grade III | 31 (4.9%) | 20 (4.0%) | |
| History of previous procedure | 0.169 | ||
| None | 502 (79.7%) | 417 (83.7%) | |
| Pneumatic dilation | 103 (16.3%) | 64 (12.9%) | |
| Heller or Heller‐Dor operation | 22 (3.5%) | 12 (2.4%) | |
| POEM | 3 (0.5%) | 5 (1.0%) | |
| ASA‐PS classification | 0.876 | ||
| I/II | 610 (96.8%) | 483 (97.0%) | |
| ≥III | 20 (3.2%) | 15 (3.0%) | |
| Eckardt score, mean ± SD | 6.1 ± 2.2 | 5.9 ± 2.1 | 0.114 |
| Adverse events | 33/630 (5.2%) | 37/498 (7.4%) | 0.137 |
| Clinical success | 562/598 (93.9%) | 326/351 (92.9%) | 0.504 |
Others include achalasia‐related esophageal motility disorders diagnosed by endoscopy and esophagography. Adverse events were defined by Clavien–Dindo classification grades I–V.
Statistical analysis for HRM diagnosis was conducted between type I–III achalasia and other esophageal motility disorders. Statistical analysis for the type of achalasia was performed between the straight type and the sigmoid type (including the advanced sigmoid type). Statistical analysis for esophageal dilation was performed between Grade I and Grade II–III.
ASA‐PS, American Society of Anesthesiologists physical status; BMI, body mass index; COVID‐19, coronavirus disease 2019; EGJOO, esophagogastric outflow obstruction; HRM, high‐resolution manometry; POEM, peroral endoscopic myotomy; SD, standard deviation.
Immature PPE for HRM
The results of the questionnaire survey on HRM are shown in Table 3. During the COVID‐19 pandemic, eight of 13 facilities restricted the number of HRM procedures. The restriction period differed in each facility, ranging from April 1 to August 16 (median 57.5 days). The median capacity of HRM was reduced 35% (0–50%). The number of HRMs were mainly decreased due to the hospitals’ management policy (75.0%), postponement or cancellation of nonurgent examinations (25.0%), and lack of PPE (25.0%). Body temperature prescreening was performed at all facilities. Most HRMs were performed in an endoscopy room (92.3%), followed by a fluoroscopy room (7.7%) and a procedure room (7.7%), all of which lacked negative pressure functions. Common PPEs included a cap (46.2%), goggles (46.2%) or face shield (46.2%), surgical mask (92.3%), long‐sleeve gown (76.9%), and a single pair of gloves (92.3%). Conversely, 53.8% wore no cap, 7.7% did not wear a goggles or face shield, and 23.1% wore a short‐sleeved gown. Yet no healthcare professionals were infected with SARS‐CoV‐2 during the practice of HRM and POEM in 2020.
Table 3.
Questionnaire survey on high‐resolution manometry for healthcare professionals (n = 13)
| Restriction on the number of HRM procedures | 61.5% (8/13) |
| Period of restriction on the number of HRM procedures* | 57.5 days (29–131) |
| Capacity of HRM procedures at the time of restriction* | 35% (0–50) |
| Reasons for the decrease in the number of HRM a | |
| Management policy of the hospital | 75.0% (6/8) |
| Postponement or cancellation of nonurgent examinations | 25.0% (2/8) |
| Lack of PPE | 25.0% (2/8) |
| Lack of medical staff due to COVID‐19 medical treatment | 0% (0/8) |
| COVID‐19 screening before examination | |
| Body temperature | 100.0% (13/13) |
| Symptoms related to COVID‐19 | 92.3% (12/13) |
| Exposure to patients with COVID‐19 or traveling to a high‐risk area | 76.9% (10/13) |
| Implementation location a | |
| Endoscopy room b | 92.3% (12/13) |
| Fluoroscopy room b | 7.7% (1/13) |
| Procedure room b | 7.7% (1/13) |
| PPE | |
| Cap | 46.2% (6/13) |
| No use of cap | 53.8% (7/13) |
| Goggles | 46.2% (6/13) |
| Face shield | 46.2% (6/13) |
| No use of goggles or face shield | 7.7% (1/13) |
| Surgical mask | 92.3% (12/13) |
| N95 mask | 7.7% (1/13) |
| Long‐sleeved gown | 76.9% (10/13) |
| Short‐sleeved gown | 23.1% (3/13) |
| Gloves (single pair) | 92.3% (12/13) |
| Gloves (double pair) | 7.7% (1/13) |
Median (range).
Duplicate answers are allowed.
Without negative pressure function.
COVID‐19, coronavirus disease 2019; HRM, high‐resolution manometry; PPE, personal protective equipment.
POEM during the COVID‐19 pandemic
The results of the questionnaire survey on POEM are shown in Table 4. During the COVID‐19 pandemic, eight of 14 facilities restricted the number of POEMs. The restriction period differed in each facility, ranging from March 25 to August 16 (median 50 days). The median capacity of POEM was reduced to 10% (0–50%). The number of POEMs primarily decreased due to the hospitals’ management policy (100.0%) and lack of PPE (12.5%). Prescreening for COVID‐19 was performed via PCR (92.9%), chest X‐ray (35.7%), and chest computed tomography (21.4%). Only one facility (7.1%) required a 1‐day prior hospitalization for COVID‐19 screening. The most common PPE used included cap (100.0%), goggles (42.9%), surgical mask (100.0%), long‐sleeve gown (78.6%), and a single pair of gloves (92.9%). The minimum PPE reported was no goggles or face shield (28.6%) and no gown (7.1%).
Table 4.
Questionnaire survey on peroral endoscopic myotomy for healthcare professionals (n = 14)
| Restriction on the number of POEM procedures | 57.1% (8/14) |
| Period of restriction on the number of POEM procedures* | 50 days (27–126) |
| Capacity of POEM procedures at the time of restriction* | 10% (0–50) |
| Reasons for the decrease in the number of POEM procedures | |
| Management policy of the hospital | 100.0% (8/8) |
| Lack of PPE | 12.5% (1/8) |
| Lack of medical staff due to COVID‐19 medical treatment | 0% (0/8) |
| Restriction on referral of patients from outside the prefecture | 35.7% (5/14) |
| COVID‐19 screening before POEM | |
| PCR | 92.9% (13/14) |
| Chest X‐ray | 35.7% (5/14) |
| Chest CT | 21.4% (3/14) |
| Hospitalization ahead of schedule due to screening for COVID‐19 | 7.1% (1/14) |
| Days of hospitalization ahead of schedule due to screening for COVID‐19* | 0 days (0–1) |
| PPE | |
| Cap | 100.0% (14/14) |
| Goggles | 42.9% (6/14) |
| Face shield | 28.6% (4/14) |
| No use of goggles or face shield | 28.6% (4/14) |
| Surgical mask | 100.0% (14/14) |
| N95 mask | 0% (0/14) |
| Long‐sleeved gown | 78.6% (11/14) |
| Short‐sleeved gown | 14.3% (2/14) |
| No use of gown | 7.1% (1/14) |
| Gloves (single pair) | 92.9% (13/14) |
| Gloves (double pair) | 7.1% (1/14) |
Median (range).
COVID‐19, coronavirus disease 2019; CT, computed tomography; PCR, polymerase chain reaction; POEM, peroral endoscopic myotomy; PPE, personal protective equipment.
DISCUSSION
This multicenter study found that during the COVID‐19 pandemic, the number of HRM and POEM procedures in Japan decreased by nearly 20%, especially during the state of emergency. Furthermore, accessibility to POEM was impaired for patients needing to cross prefectures. The use of PPE for HRM and POEM varied among regions and facilities.
Clinical practices of HRM and POEM are considered nonemergent and have a high risk of splash and aerosol contamination of COVID‐19 to healthcare professionals. 15 , 16 The American Neurogastroenterology and Motility Society Task Force and European Society for Neurogastroenterology and Motility provided guidelines on the indications and clinical qualifiers that elevate the typically elective esophageal physiologic procedures to semi‐urgent or emergent status during the COVID‐19 pandemic. 17 , 18 , 19 They recommended that patients with significant dysphagia and an inability to maintain hydration and nutrition be prioritized, and procedures for patients with mild symptoms be postponed. It is presumed that each facility restricted the number of HRM procedures according to the spread of infection and the state of emergency in accordance with these recommendations.
Similarly, the American Society of Gastrointestinal Endoscopy, European Society of Gastrointestinal Endoscopy, and JSGE recommended that endoscopic procedures be postponed or performed electively according to their priority and the COVID‐19 pandemic status. 8 , 20 , 21 According to the United Kingdom’s National Endoscopy Database, the total number of endoscopic procedures during the lockdown period was 87.8% lower than that before COVID‐19. 22 Even the number of therapeutic endoscopy procedures, such as endoscopic submucosal dissection and endoscopic mucosal resection for gastrointestinal neoplasia, were reduced by 60% during the lockdown. 23 It is difficult to compare the validity of clinical care between the Western countries and Japan, because the numbers of infected patients and medical‐care provision systems are totally different between the two; however, it is considered that HRM and POEM were relatively well managed in Japan. Furthermore, even when the performance of POEM was limited during the state of emergency, semi‐emergent POEM was performed for cases with acute exacerbation of symptoms. Alternatively, balloon dilatation may be effective during the short period of time, and can be followed by POEM under a safer setting. However, laparoscopic Heller myotomy may be more difficult to perform during the pandemic due to the requirement of more staff and longer hospital stays. 6 , 24 , 25
Interestingly, the numbers of HRM and POEM procedures were strongly affected in pandemic areas, where human behavior was restricted, but not in nonpandemic areas. Furthermore, the number of POEM for patients outside the prefecture decreased significantly. Unnecessary and nonurgent access to pandemic areas was particularly restricted during the COVID‐19 pandemic, and patients living in prefectures without high‐volume EMD centers had greatly impaired access to POEM, which requires further consideration, as accessibility to medical care should be equal for every patient.
Jan et al. reported that more than 90% of facilities in Europe majorly reduced or froze their capacity for HRM during the COVID‐19 pandemic. 17 Mori et al. reported that, compared to Europe, the restrictions on HRM capacity were less stringent in Asia, where the COVID‐19 transmission and mortality rates were relatively low. 26 , 27 In our study, 61.5% of facilities restricted the number of HRMs, and there was a considerable discrepancy in the restriction of HRM cases between facilities in nonpandemic and pandemic areas, as those in the latter implemented restriction similar to those in Europe. 17 In most facilities, HRM was performed in the endoscopy room without negative pressure function, as previously reported. 17 Currently, the recommended standard PPE for HRM is caps, surgical masks or N95 masks, goggles or face shield, long‐sleeved gown, and a single pair of gloves, 17 but 53.8% of the facilities in this study did not meet these requirements. Each facility was unable to respond to the unprecedented situation of the COVID‐19 pandemic, particularly during the first to second wave.
Implementation of PPE for POEM was more lenient than that for HRM in this study, as some facilities reported that no goggles, face shield, or gown were worn. However, Chan et al. reported that aerosols were generated during the initial intubation of the endoscope and output of electric knife during POEM under general anesthesia. 28 Even with endotracheal intubation, the healthcare professional may inhale the aerosol during the endoscopic procedure. Furthermore, a meta‐analysis reported that up to 54% of COVID‐19 patients may initially show false‐negative PCR results. 29 We recommend surgical mask, goggles, cap, long‐sleeve isolation gown, and gloves as PPE for POEM, regardless of whether a COVID‐19 screening test can be performed. Only one facility mandated a 1‐day extended hospital stay during the pandemic, and additional medical costs against COVID‐19 were mostly for screening tests and PPE.
There are several limitations in this study. First, factors other than the COVID‐19 pandemic may be associated with the change in the number of HRM and POEM. However, at the 14 facilities included the numbers are increasing annually (data not shown), so we consider that the negative influence of COVID‐19 may be underestimated. Second, the number of SARS‐CoV‐2‐positive patients in Japan was smaller compared to that in the United States and Europe. Further, the state of emergency in Japan was a mild lockdown compared to that in Western countries. Therefore, the data in this study may not apply to countries where COVID‐19 numbers were staggering and severe lockdowns were declared. In Japan, further studies are required to compare the change in the number of POEM procedures for benign diseases and of endoscopic treatment such as endoscopic submucosal dissection for neoplasia to clarify the position of POEM during the COVID‐19 pandemic. Third, adverse events in postponed cases, which may have been followed up in other hospitals, could not be analyzed completely.
In conclusion, the COVID‐19 pandemic influenced the practices of HRM and POEM in Japan. The total number of HRM and POEM procedures decreased by ~20%, and access to facilities in pandemic areas from outside the prefecture was severely restricted during the state of emergency. Although there were differences in management for medical care and infection among regions and facilities, the safety and effectiveness of POEM were maintained throughout.
CONFLICT OF INTEREST
Author H.I. is the president of the Japan Gastroenterological Endoscopy Society. The other authors declare no conflict of interest for this article.
FUNDING INFORMATION
This study was partially supported by JGA Clinical Research Grants (grant number: 2021‐1). The funding played no role in the study design, analysis, or decision to publish the article.
Supporting information
Table S1 Affiliations and Ethics Committee approval numbers for the 14 participating facilities.
ACKNOWLEDGMENT
We thank Editage [http://www.editage.com] for editing and reviewing this article for English.
References
- 1. World Health Organization . Coronavirus Disease 2019 (COVID‐19) Situation Report‐10 [Internet]. Geneva: World Health Organization; 2020. [cited 2021 Jun 30]. Available from: https://www.who.int/docs/default‐source/coronaviruse/situation‐reports/20200130‐sitrep‐10‐ncov.pdf?sfvrsn=d0b2e480_2. [Google Scholar]
- 2. Kahrilas PJ, Bredenoord AJ, Fox M et al. The Chicago Classification of esophageal motility disorders, v3.0. Neurogastroenterol Motil 2015; 27: 160–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Inoue H, Minami H, Kobayashi Y et al. Peroral endoscopic myotomy (POEM) for esophageal achalasia. Endoscopy 2010; 42: 265–71. [DOI] [PubMed] [Google Scholar]
- 4. Sato H, Takahashi K, Mizuno KI et al. Esophageal motility disorders: New perspectives from high‐resolution manometry and histopathology. J Gastroenterol 2018; 53: 484–93. [DOI] [PubMed] [Google Scholar]
- 5. Sato H, Yokomichi H, Takahashi K et al. Epidemiological analysis of achalasia in Japan using a large‐scale claims database. J Gastroenterol 2019; 54: 621–7. [DOI] [PubMed] [Google Scholar]
- 6. Inoue H, Shiwaku H, Iwakiri K et al. Clinical practice guidelines for peroral endoscopic myotomy. Dig Endosc 2018; 30: 563–79. [DOI] [PubMed] [Google Scholar]
- 7. Japanese Society of Gastroenterology . Points to note in gastrointestinal disease treatment for new coronavirus infection (COVID‐19) [Internet]. Tokyo: Japanese Society of Gastroenterology; 2020 [cited 2021 Jun 30]. Available from: https://www.jsge.or.jp/news/archives/287. Japanese.
- 8. Furuta T, Irisawa A, Matsumoto T et al. Clinical Questions and Answers on Gastrointestinal Endoscopy during the Novel Coronavirus Disease 2019 pandemic. Dig Endosc 2020; 32: 651–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Japan Esophageal Society. Descriptive rules for achalasia of the esophagus, June 2012: 4th edition. Esophagus 2017; 14: 275–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. American Society of Anesthesiologists . ASA physical status classification system [Internet] . Illinois: American Society of Anesthesiologists; 2020 [cited 2021 Jun 30]. Available from: https://www.asahq.org/standards‐and‐guidelines/asa‐physical‐status‐classification‐system.
- 11. Eckardt VF. Clinical presentations and complications of achalasia. Gastrointest Endosc Clin N Am 2001; 11: 281–92, vi. [PubMed] [Google Scholar]
- 12. Shiwaku H, Inoue H, Sato H et al. Peroral endoscopic myotomy for achalasia: A prospective multicenter study in Japan. Gastrointest Endosc 2020; 91: 1037–44.e2. [DOI] [PubMed] [Google Scholar]
- 13. Dindo D, Demartines N, Clavien PA. Classification of surgical complications: A new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 2004; 240: 205–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Ministry of Health, Labour and Welfare . COVID‐19 Opendata [Internet]. Tokyo: Ministry of Health, Labour and Welfare; c2020‐2021 [cited 2021 Jun 30]. Available from: https://www.mhlw.go.jp/stf/covid‐19/open‐data.html. Japanese.
- 15. Huang C, Wang Y, Li X et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020; 395: 497–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Gu J, Han B, Wang J. COVID‐19: Gastrointestinal manifestations and potential fecal‐oral transmission. Gastroenterology 2020; 158: 1518–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Tack J, Schol J, Geeraerts A et al. A survey on the impact of the COVID‐19 pandemic on motility and functional investigations in Europe and considerations for recommencing activities in the early recovery phase. Neurogastroenterol Motil 2020; 32: e13926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Baker JR, Moshiree B, Rao S et al. American Neurogastroenterology and Motility Society Task Force recommendations for resumption of motility laboratory operations during the COVID‐19 pandemic. Am J Gastroenterol 2020; 115: 1575–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Tack J, Vanuytsel T, Serra J et al. European Society for Neurogastroenterology and Motility recommendations for conducting gastrointestinal motility and function testing in the recovery phase of the COVID‐19 pandemic. Neurogastroenterol Motil 2020; 32: e13930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. American Society for Gastrointestinal Endoscopy . Joint GI society message: COVID‐19 clinical insights for our community of gastroenterologists and gastroenterology care providers [Internet] . Downers Grove: American Society for Gastrointestinal Endoscopy; c2020‐2021 [cited 2021 Jun 30]. Available from: https://www.asge.org/home/joint‐gi‐society‐message‐covid‐19.
- 21. Gralnek IM, Hassan C, Beilenhoff U et al. ESGE and ESGENA Position Statement on gastrointestinal endoscopy and COVID‐19: An update on guidance during the post‐lockdown phase and selected results from a membership survey. Endoscopy 2020; 52: 891–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Rutter MD, Brookes M, Lee TJ, Rogers P, Sharp L. Impact of the COVID‐19 pandemic on UK endoscopic activity and cancer detection: A national endoscopy database analysis. Gut 2021; 70: 537–43. [DOI] [PubMed] [Google Scholar]
- 23. Rodriguez‐Carrasco M, Albeniz E, Bhandari P et al. COVID‐19 and endoscopic management of superficial gastrointestinal neoplastic lesions: A multinational cross‐sectional survey. Endoscopy 2021; 53: 173–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Khashab MA, Vela MF, Thosani N et al. ASGE guideline on the management of achalasia. Gastrointest Endosc 2020; 91: 213–27.e6. [DOI] [PubMed] [Google Scholar]
- 25. Oude Nijhuis RAB, Zaninotto G, Roman S et al. European guidelines on achalasia: United European Gastroenterology and European Society of Neurogastroenterology and Motility recommendations. United Eur Gastroenterol J 2020; 8: 13–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Mori H, Schol J, Geeraerts A et al. The impact of COVID‐19 on gastrointestinal motility testing in Asia and Europe. J Clin Med 2020; 9: 3189–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Mori H, Tack J, Suzuki H. Statements for conducting high‐resolution manometry during the COVID‐19 pandemic. J Clin Biochem Nutr 2020; 67: 114–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Chan SM, Ma TW, Chong MK, Chan DL, Ng EKW, Chiu PWY. A proof of concept study: Esophagogastroduodenoscopy is an aerosol‐generating procedure and continuous oral suction during the procedure reduces the amount of aerosol generated. Gastroenterology 2020; 159: 1949–51.e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Arevalo‐Rodriguez I, Buitrago‐Garcia D, Simancas‐Racines D et al. False‐negative results of initial RT‐PCR assays for COVID‐19: A systematic review. PLoS One 2020; 15: e0242958. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1 Affiliations and Ethics Committee approval numbers for the 14 participating facilities.


