Abstract
During the COVID‐19 pandemic, many educational institutions followed the blended learning system. Using the participants' opinions, we evaluated the Blackboard (Bb) collaborate platform for online team‐based learning (TBL) sessions for undergraduate students from different medical programs in the KSA. The participants were students on the MBBS Program (157 year two and 149 year three), together with 53 students in year one of the Nursing Program, 25 in year two of the Doctor of Pharmacy Program, and 11 in year two of the Medical Laboratory Sciences Program in Fakeeh College for Medical Sciences, (FCMS) KSA. To assess students' recall, engagement, and satisfaction with the sessions, an online TBL plan was designed and reviewed by the Medical Education Department. The students completed an online survey at the end of each session. All responses in this study showed a statistically significant positive difference from the neutral mid‐point response (p < 0.05), reflecting high satisfaction. In the MBBS Program, the survey was completed by 40 students in year two and 76 in year three. The mean responses were 4.1 ± 0.3 and 3.9 ± 0.2 respectively (mean ± SD). In the BSN Program, 19 students completed the survey. The mean response was 4.6 ± 0.2. In the Pharm D Program, 10 students completed the survey. The mean response was 4.9 ± 0.12. In the MLS Program, eight students completed the survey. The mean response was 4.8 ± 0.12. It was concluded that online TBL using Bb collaborate is a successful anatomy‐learning tool among FCMS students on different programs.
Keywords: blackboard collaborate, blended learning, COVID‐19, medical education, online TBL
1. INTRODUCTION
In medical education, many institutions have realized the need to shift from conventional teaching strategies and discipline‐based curricula toward learner‐centered strategies and more integrated curricula (Vasan et al., 2008). Team‐based learning (TBL) is a flipped class teaching strategy based on the principles of collaborative learning (Parmelee et al., 2012). It encourages critical thinking while engaging learners in an active class (Parmelee & Michaelsen, 2010). Owing to its specific features making it suitable for medical education, TBL has been adopted by several medical schools (Parmelee, 2008).
In higher education, especially in medical sciences, TBL has achieved learning outcomes significantly different from other mixed active learning methods (Zingone et al., 2010). Many authors have reported that TBL results in improved student performances and favors perception (Al‐Meman et al., 2014; Chen et al., 2018; Rezaee et al., 2016). Moreover, its effect on recall, attention levels, and satisfaction among medical students was assessed; higher student engagement and satisfaction was demonstrated. It was recommended that TBL be applied in interprofessional educational programs and even preclinical courses using real clinical cases (Faezi et al., 2018).
The internet provides an additional learning tool. The potential of electronic learning (e‐learning) in medical education, a system based on electronic resources using computers and electronic devices, has quickly become popular (Bediang et al., 2013; Berners‐Lee et al., 1994). The COVID‐19 pandemic affected all educational systems worldwide. Most governments decided to close educational institutions temporarily to reduce the spread of the virus (UNESCO, 2020). Many institutions therefore followed the blended learning system, a style of education in which students learn via both traditional face‐to‐face teaching and electronic and online media. Blended learning is now widely implemented in Fakeeh College for Medical Sciences (FCMS), Jeddah, KSA. Most theoretical sessions are conducted virtually using the Blackboard (Bb) collaborate platform, while the remainder, along with all practical and clinical sessions, are conducted face‐to‐face in the College.
2. AIM OF THE STUDY
To our knowledge, few studies have been conducted to assess the effect of online TBL using a standard virtual learning environment. Our aim was therefore to evaluate the effect of online TBL on recall, engagement, and satisfaction among students in anatomy teaching on different programs at FCMS from the participants' point of view.
3. MATERIALS AND METHODS
3.1. Participants
The participants were students in FCMS, Jeddah, KSA on the MBBS Program (157 year two students, 101 females and 56 males, enrolled in the Foundation of Medicine A course; 149 year three students, 110 females and 39 males, enrolled in the Blood‐Cardiovascular & Respiratory Systems module). In addition we recruited students in the Nursing (BSN) Program enrolled in the Human Anatomy & Physiology course (53 females), year two students in the Doctor of Pharmacy (PharmD) Program enrolled in the Anatomy & Histology course (18 females and seven males), and year two students in the Medical Laboratory Sciences (MLS) Program enrolled in the Principles of Human Anatomy course (eight females and three males).
3.2. Design and procedure
An online TBL plan was designed including the following steps:
3.2.1. Prework
Teaching material including slides, assigned readings, or videos was uploaded to the Bb enabling students to review it in their own time, as done previously in face‐to‐face TBL sessions.
3.2.2. Individual readiness assurance test (IRAT)
Students joined the virtual Bb session at the agreed start time of the class, after which the instructor announced the start of the IRAT (Figure 1).
FIGURE 1.
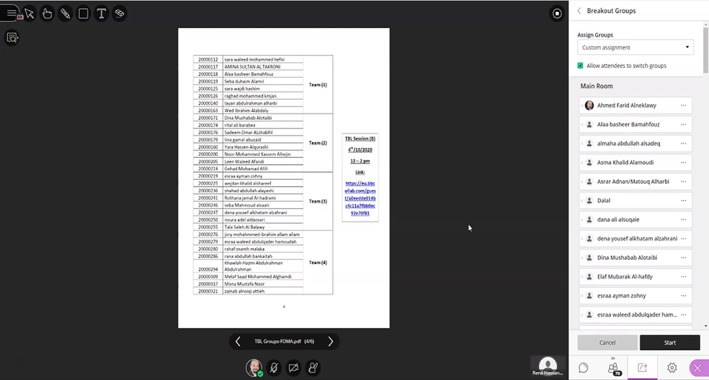
A screenshot from a virtual TBL session on Bb showing the distribution of teams. All participants are in the main room before starting the breakout groups. Bb, blackboard; TBL, team‐based learning
3.2.3. Team readiness assurance test (TRAT)
The Bb tool was used to create breakout rooms for each team so the teams could discuss their answers (Figures 2 and 3).
FIGURE 2.
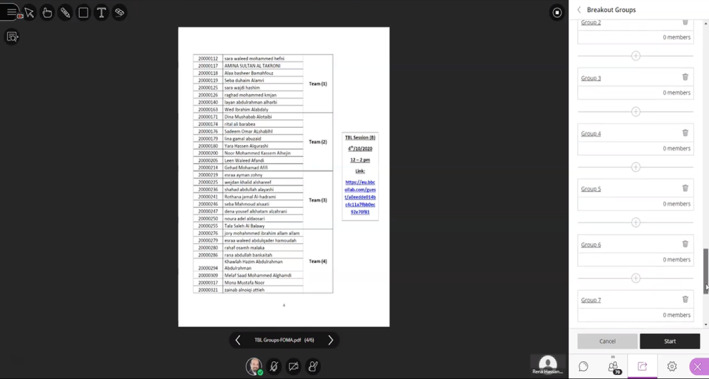
A screenshot from a virtual TBL session on bb showing different groups created by the instructor, the breakout groups ready to start. TBL, team‐based learning
FIGURE 3.
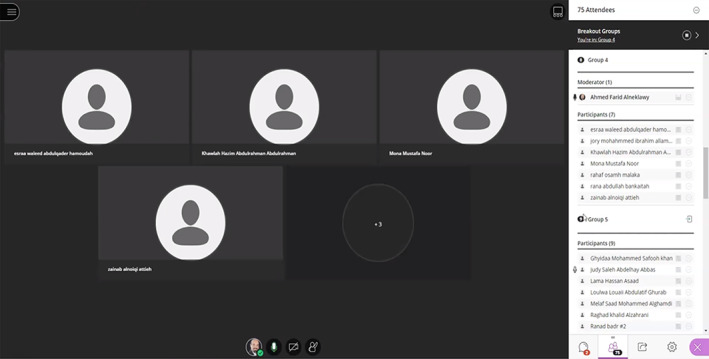
A screenshot from a virtual TBL session on bb showing the breakout groups and participants in each group. The instructor is in group 4 as he can join any group to follow‐up discussion among students. TBL, team‐based learning
Clarifications: the instructor stopped the breakout rooms to return to the main session room and asked students to flag any questions either by voicing them or by typing them into the chat box. The instructor also shared the item analyses from both IRAT and TRAT and discussed the most difficult points.
Application exercises: the teams went again into their virtual breakout rooms to discuss and solve the application exercises. The instructor then stopped the breakout rooms and shared all the teams' responses with the students for discussion.
An orientation video was also uploaded to familiarize the students with the planned process of the virtual TBL session.
The Medical Education Department (MED) reviewed and approved the plan according to certain guidelines (Table 1). All approved guidelines were followed, and certain topics were selected from the anatomy curricula among different programs. The Bb collaborate was the learning management system (LMS) of choice in this study. A key criterion for the Bb collaborate is the ability to divide participants into teams during the virtual session.
TABLE 1.
Guidelines for developing an online TBL session
| Phase | Guidelines |
|---|---|
| Planning phase |
1. The material required by students for pre‐reading should be uploaded a week before the session. 2. The (IRAT/TRAT) and case application should be revised before conducting the session with the objectives of the session by the Medical Education Department. 3. The (IRAT/TRAT) comprises 10 cognitive MCQs aligned with the session objectives. 4. After revising the IRAT/TRAT and case application exercise, questions will be uploaded on Bb. 5. One case scenario is required with three related MCQs questions. 6. The students should be oriented about Online TBL. 7. Staff members should be orientated about Online TBL. |
| Implementation phase |
1. Online TBL session should be recorded. 2. Teams should be formed through randomization. 3. IRAT/TRAT will last for 15 min for each session (1.5 min/question). 4. Corrective instruction takes 15–20 min. 5. Case application takes 20 min. 6. Intra‐ and Inter‐team facilitated discussion takes 20 min. 7. Peer evaluation and feedback takes 10 min. 8. Grading of TBL sessions is weighted as 5% of the assessment plan and it is divided as follows:
9. At the end of the session the students complete the Online TBL satisfaction survey. |
Abbreviations: IRAT, individual readiness assurance test; TBL, team‐based learning; TRAT, team readiness assurance test.
3.3. Instrument
At the end of each TBL session, the students were invited to submit an online survey, which consisted of 30 Likert Scale questions using five degree points from “strongly disagree” to “strongly agree,” to assess students' recall, engagement, and satisfaction with the session (Table 2).
TABLE 2.
Survey instrument
| 1 | Online TBL helped me increase my understanding of the course material. |
| 2 | Online TBL helped me meet the course objectives. |
| 3 | Online TBL helped me to focus on core information. |
| 4 | I learned useful additional information during the online TBL sessions. |
| 5 | Online TBL allowed me to apply my knowledge |
| 6 | The online TBL format was helpful in developing my information and synthesizing skills. |
| 7 | Online TBL increase the quality of learning. |
| 8 | I was prepared well for online TBL. |
| 9 | I completed all required reading material for online TBL. |
| 10 | I felt prepared for IRAT. |
| 11 | The team readiness assurance test (TRAT) and case discussions allowed me to correct my mistakes and improve understanding of the concepts. |
| 12 | The instructor oriented us about TBL before the first session. |
| 13 | The instructor was helpful and responsive to my inquiries. |
| 14 | The instructor gave us clear corrective instruction. |
| 15 | The instructor gave us chance to appeal to any question. |
| 16 | I feel confident in speaking out my opinions during the TRAT and case discussions. |
| 17 | I am actively engaged in the TBL activities. |
| 18 | My teammates are actively engaged in the TBL activities. |
| 19 | My team worked well together. |
| 20 | I have a positive attitude about working with my peers. |
| 21 | The ability to collaborate with my peers is necessary if I am to be successful as a student. |
| 22 | I contributed meaningfully to the online TBL discussions. |
| 23 | I paid attention most of the time during the online TBL sessions. |
| 24 | There was mutual respect for other teammates' viewpoints during online TBL. |
| 25 | TRAT and case discussion were useful for my learning. |
| 26 | I learned better from small group discussion than in class setting. |
| 27 | Solving problems in a group was an effective way to practice what I have learned. |
| 28 | The TRAT and case discussions allowed me to correct my mistakes and improve understanding of the concepts. |
| 29 | Most students were attentive during online TBL sessions. |
| 30 | Overall, I was satisfied with online TBL experience. |
Abbreviations: IRAT, individual readiness assurance test; TBL, team‐based learning.
SPSS statistical program version 17 (IBM Corporation, New York, USA) was used for statistical analysis of the survey responses. The mean values and SD were calculated, and one way ANOVA followed by t‐tests was used to determine the statistical differences between the mean responses of students on different programs. A p value less than 0.05 was considered significant.
3.4. Ethical considerations
The experimental design and protocols accorded with the guidelines of the Scientific Research Unit (SRU), FCMS, Jeddah, KSA.
3.5. Results (Table 3 and Figure 4)
TABLE 3.
Mean responses on each question among different programs
| Question number | Year 2 MBBS | Year 3 MBBS | Year 1 BSN | Year 2 PharmD | Year 2 MLS |
|---|---|---|---|---|---|
| 1 | 3.6 | 3.8 | 4.3 | 4.9 | 4.9 |
| 2 | 3.9 | 3.8 | 4.4 | 4.6 | 4.8 |
| 3 | 3.8 | 3.8 | 4.7 | 4.6 | 4.8 |
| 4 | 3.8 | 3.9 | 4.5 | 4.6 | 4.9 |
| 5 | 3.8 | 3.8 | 4.7 | 4.9 | 4.9 |
| 6 | 3.8 | 3.8 | 4.5 | 5.0 | 4.8 |
| 7 | 3.6 | 3.7 | 4.4 | 4.7 | 4.9 |
| 8 | 4.2 | 3.9 | 4.8 | 4.9 | 4.8 |
| 9 | 4.2 | 4.0 | 4.7 | 4.8 | 4.8 |
| 10 | 4.0 | 3.9 | 4.5 | 4.9 | 4.8 |
| 11 | 4.2 | 4.0 | 4.6 | 4.9 | 4.5 |
| 12 | 4.4 | 4.1 | 4.7 | 5.0 | 4.8 |
| 13 | 4.4 | 4.2 | 4.7 | 5.0 | 4.8 |
| 14 | 4.5 | 4.2 | 4.7 | 4.9 | 4.8 |
| 15 | 4.4 | 4.2 | 4.8 | 4.7 | 4.8 |
| 16 | 4.4 | 4.2 | 4.6 | 5.0 | 4.8 |
| 17 | 4.4 | 4.1 | 4.6 | 4.9 | 4.8 |
| 18 | 4.2 | 4.0 | 4.7 | 5.0 | 4.6 |
| 19 | 4.4 | 4.0 | 4.8 | 5.0 | 4.5 |
| 20 | 4.4 | 4.1 | 4.4 | 5.0 | 4.5 |
| 21 | 4.3 | 4.1 | 4.5 | 5.0 | 4.8 |
| 22 | 4.2 | 4.1 | 4.6 | 4.9 | 4.8 |
| 23 | 4.3 | 4.1 | 4.6 | 4.9 | 4.8 |
| 24 | 4.5 | 4.2 | 4.7 | 4.9 | 4.8 |
| 25 | 4.2 | 4.1 | 4.4 | 4.9 | 4.8 |
| 26 | 3.5 | 3.9 | 4.3 | 4.9 | 4.5 |
| 27 | 4.2 | 4.1 | 4.4 | 4.9 | 4.8 |
| 28 | 4.2 | 4.0 | 4.4 | 4.9 | 4.6 |
| 29 | 3.8 | 3.9 | 4.5 | 4.9 | 4.6 |
| 30 | 3.9 | 3.9 | 4.7 | 4.9 | 4.8 |
| Overall mean | 4.1 a | 3.9 a | 4.6 a | 4.9 a | 4.8 a |
Positive significant difference from the neutral mid‐point response M = 3, p < 0.005.
FIGURE 4.
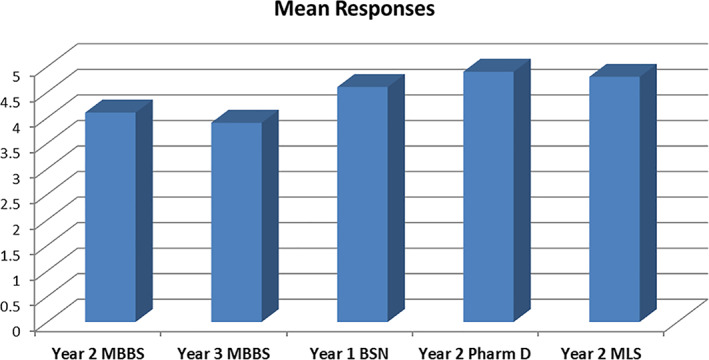
Likert scale of students' overall evaluation
On the MBBS Program, 40 third level students responded to the survey (26% response rate). The mean response was 4.1 ± 0.3 (mean ± SD). Seventy‐six fifth level students responded to the survey (52% response rate). The mean response was 3.9 ± 0.2. In the BSN Program, 19 students responded to the survey (36% response rate). The mean response was 4.6 ± 0.2. In the PharmD Program, 10 students responded to the survey (40% response rate). The mean response was 4.9 ± 0.12. In the MLS Program, eight students responded to the survey (73% response rate). The mean response was 4.8 ± 0.12. All responses in this study showed a statistically significant positive difference from the neutral mid‐point response (p < 0.05). There were no significant differences among the mean responses of students on different programs for any question in the survey (p > 0.05).
4. DISCUSSION
To our knowledge, the present study is the first trial of an online TBL session for different medical sciences students in Saudi Arabia using the Bb collaborate platform with a survey evaluating the session from the participants' point of view. The study did not aim at comparative analysis of outcomes either between traditional teaching strategies and TBL or between on‐site and online TBL. However, many studies have reported that TBL yields significant differences in learning outcomes from other teaching strategies.
Although the TBL sessions in this study were conducted online among students on different medical programs, all responses showed statistically significant positive differences from the neutral response, reflecting the satisfaction and success of the experiment in the participants' opinions. This agrees with many studies that have evaluated face‐to‐face TBL sessions.
More than 10 years ago, Zingone et al. (2010) reported that TBL gave learning outcomes significantly different from other mixed active learning methods in pharmaceutical education. A few years later, Al‐Meman et al. (2014) concluded that a successfully developed TBL module resulted in improved students' performance and favored perception in different pharmacy practice courses in Saudi Arabia. As regards medical students, Rezaee et al. (2016) and Faezi et al. (2018) stated that the TBL approach created an active learning environment that contributed to improving students' recall, attention level, satisfaction, and performances in both hospital organization and management and rheumatology courses. Moreover, Chen et al. (2018) concluded that TBL seemed more effective than traditional lecture‐based learning in improving knowledge, skills, and attitudes of students in China, providing evidence of the implementation of TBL in medical education in China.
In FCMS, the TBL strategy has been approved and encouraged to the extent that it is included in the assessment plans for different courses.
Prior to the COVID‐19 pandemic, the sessions were conducted face‐to‐face in the TBL studio in the main campus of the college. Thereafter, the blended learning system was implemented and most of the theoretical sessions were conducted using the Bb collaborate platform.
E‐learning has quickly become popular in medical education (Bediang et al., 2013). It has also been reported that web‐based learning can provide greater motivation and learning success for students (Gallagher et al., 2005). Moreover, the use of social media, namely Twitter and Facebook, in higher education has been documented as an additional tool enhancing the learning process and increasing students' engagement (Ebner et al., 2010; Evans, 2014; Junco et al., 2011). In the field of anatomy education, many authors have documented that e‐learning is a successful learning tool that improves the students' engagement and learning experience by enhancing their communication with teachers (Al‐Neklawy, 2017; Hennessy et al., 2016; Jaffar, 2014).
The Bb platform was used in the present study as it is the official LMS approved by FCMS. It provides the top principles of successful e‐learning (Anderson & McCormick, 2005). Also, the Bb collaborate enables participants to be divided into teams during the virtual sessions. In this study, the overall students' responses ranged from 3.9 to 4.9 with a statistically significant positive difference from the neutral response. These results provide evidence of successful implementation of the virtual TBL sessions among students on different medical programs in Saudi Arabia using the Bb collaborate platform.
Moreover, evidence was obtained of successful e‐learning in conducting challenging interactive teaching strategies such as TBL. This, in turn, adds a new clue for improving blended learning and agrees with previous studies that demonstrated the positive effect of blended learning on health professional learners, which could be more effective than, or at least as effective as, non‐blended instruction for knowledge acquisition (Liu et al., 2016).
5. LIMITATIONS OF THE STUDY
Although the results of this study were informative about the success of the online TBL strategy, it has certain limitations. To our knowledge, it is the first study of online TBL among students in different medical sciences in Saudi Arabia. It was conducted to evaluate the success of this strategy from the student's point of view without measuring overall academic improvement in terms of total scores. It included only certain topics of anatomy among the participating students of FCMS; the students' responses could differ from those of students elsewhere. Moreover, there was a low‐response rate to the survey.
6. CONCLUSION
Online TBL using the Bb collaborate appears to be a successful anatomy learning tool among FCMS students on different programs. It is strongly recommended that further studies be conducted on different medical curricula to enhance the knowledge gain and engagement among students.
CONFLICT OF INTEREST
The authors declare that they have no conflict of interest, intention to make financial gain, or commercial associations regarding this research.
ACKNOWLEDGMENTS
The authors would like to thank FCMS Management, All Program Directors, Medical Education Department, Quality Unit, and Research Unit for their continuous support and encouraging innovations. They would also like to thank Anatomy staff members at FCMS (Professor Sherif Zaki and Dr. Mohammed Elshafey) for their great help in preparing and conducting the sessions for MBBS students. Ms. Maha Darandary and Ms. Kholoud Nazer are thanked for their efforts in improving the English in this manuscript.
Al‐Neklawy, A. F. , & Ismail, A. S. A. (2022). Online anatomy team‐based learning using blackboard collaborate platform during COVID‐19 pandemic. Clinical Anatomy, 35(1), 87–93. 10.1002/ca.23797
REFERENCES
- Al‐Meman, A. , Al‐Worafi, Y. , & Saleh, M. (2014). Team‐based learning (TBL) as a new learning strategy in pharmacy college, Saudi Arabia. UJP, 03(03), 57–65. [Google Scholar]
- Al‐Neklawy, A. F. (2017). Online embryology teaching using learning management systems appears to be a successful additional learning tool among Egyptian medical students. Annals of Anatomy, 214, 9–14. [DOI] [PubMed] [Google Scholar]
- Anderson, J. , & McCormick, R. (2005). Ten pedagogic principals for e‐learning insight: Observatory for new technologies and education. European Schoolnet. [Google Scholar]
- Bediang, G. , Stoll, B. , Geissbuhler, A. , Klohn, A. M. , Stuckelberger, A. , Nko'o, S. , & Chas‐tonay, P. (2013). Computer literacy and e‐learning perception in Cameroon: The case of Yaounde faculty of medicine and biomedical sciences. BMC Medical Education, 13, 57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berners‐Lee, T. , Cailliau, R. , Luotonen, A. , Nielsen, H. F. , & Secret, A. (1994). The world‐wide web. Communications. ACM, 37(August 8), 76–82. [Google Scholar]
- Chen, M. , Ni, C. , Hu, Y. , Wang, M. , Liu, L. , Ji, X. , Chu, H. , Wu, W. , Lu, C. , Wang, S. , Wang, S. , Zhao, L. , Li, Z. , Zhu, H. , Wang, J. , Xia, Y. , & Wang, X. (2018). Meta‐analysis on the effectiveness of team‐based learning on medical education in China. BMC Medical Education, 18, 77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ebner, M. , Lienhardt, C. , Rohs, M. , & Meyer, I. (2010). Microblogs in higher education—Achance to facilitate informal and process‐orientated learning? Computers in Education, 55, 92–100. [Google Scholar]
- Evans, C. (2014). Twitter for teaching: Can social media be used to enhance the processof learning? British Journal of Educational Technology, 45, 902–915. [Google Scholar]
- Faezi, S. T. , Moradi, K. , Ghafar Rahimi Amin, A. , Akhlaghi, M. , & Keshmiri, F. (2018). The effects of team‐based learning on learning outcomes in a course of rheumatology. Journal of Advances in Medical Education & Professionalism, 6(1), 22–30. [PMC free article] [PubMed] [Google Scholar]
- Gallagher, J. E. , Dobrosielski‐Vergona, K. A. , Wingard, R. G. , & Williams, T. M. (2005). Web‐based vs. traditional classroom instruction in gerontology: A pilot study. Journal of Dental Hygiene, 79(3), 7. [PubMed] [Google Scholar]
- Hennessy, C. M. , Kirkpatrick, E. , Smith, C. F. , & Border, S. (2016). Social media andanatomy education: Using twitter to enhance the student learning experiencein anatomy. American Association for Anatomy, 9, 505–515. [DOI] [PubMed] [Google Scholar]
- Jaffar, A. A. (2014). Exploring the use of a Facebook page in anatomy education. American Association for Anatomy, 7, 199–208. [DOI] [PubMed] [Google Scholar]
- Junco, R. , Heibergert, G. , & Loken, E. (2011). The effect of twitter on college studentengagement and grades. Journal of Computer Assisted Learning, 27, 119–132. [Google Scholar]
- Liu, Q. , Peng, W. , Zhang, F. , Hu, R. , Li, Y. , & Yan, W. (2016). The effectiveness of blended learning in health professions: Systematic review andmeta‐analysis. Journal of Medical Internet Research, 18(1), e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parmelee, D. , Michaelsen, L. K. , Cook, S. , & Hudes, P. D. (2012). Team‐based learning: A practical guide: AMEE guide no. 65. Medical Teacher, 34, e275–e287. [DOI] [PubMed] [Google Scholar]
- Parmelee, D. X. (2008). Team‐based learning in health professions education. Team‐Based Learning for Health Professions Education, 23(1), 47–48. [Google Scholar]
- Parmelee, D. X. , & Michaelsen, L. K. (2010). Twelve tips for doing effective team‐based learning (TBL). Medical Teacher, 32, 118–122. [DOI] [PubMed] [Google Scholar]
- Rezaee, R. , Moadeb, N. , & Shokrpour, N. (2016). Team‐based learning: A new approach toward improving education. Acta Medica Iranica, 54, 678–682. [PubMed] [Google Scholar]
- UNESCO . (2020). COVID‐19 educational disruption and response.
- Vasan, N. S. , DeFouw, D. O. , & Holland, B. K. (2008). Modified use of team‐based learning for effective delivery of medical gross anatomy and embryology. Anatomical Sciences Education, 1(1), 3–9. [DOI] [PubMed] [Google Scholar]
- Zingone, M. M. , Franks, A. S. , Guirguis, B. , George, C. M. , Howard‐Thompson, A. , & Heidel, R. E. (2010). Comparing team‐based and mixed active‐learning methods in an ambulatory care elective course. American Journal of Pharmaceutical Education, 74(9) Article 160. [DOI] [PMC free article] [PubMed] [Google Scholar]


