Abstract
Aim
During COVID‐19 restrictions, the paediatric clinic only accepted essential outpatient visits, schools closed, sports activities and social life were limited. Most employees worked at home. This quasi‐experiment evaluates how this affected glycaemic control and use of health services among children with diabetes.
Methods
Paired t‐tests were used to compare HbA1c‐values before, during and after lockdown. Sub‐analyses were stratified by pre‐lockdown HbA1c‐values.
Results
Overall mean HbA1c decreased from 58.3 to 56.9 mmol/mol (p = 0.025) from pre‐ to post‐lockdown, a decrease also seen during the same season the previous year. HbA1c decreased by −4.2 mmol/mol (p = 0.002) for patients with pre‐lockdown HbA1c > 59 mmol/mol, but increased slightly by 0.8 mmol/mol (p = 0.176) for patients with HbA1c < 52 mmol/mol. HbA1c measured 8 months post‐lockdown increased again, most pronounced for patients with lowest HbA1c. During lockdown, virtual contacts increased from 0.1 to 0.5 contacts/patient/month and stayed post‐lockdown at 0.3 contacts/patient/month.
Conclusion
Compared to 2019, overall the COVID‐19 restrictions did not influence the glycaemic control negatively. However, patients with pre‐lockdown HbA1c < 52 mmol/mol experienced a deterioration, whereas those with HbA1c > 59 mmol/mol experienced an improvement. Less stress and more contact with parents may contribute to the last‐mentioned finding. The lockdown enforced more virtual contacts between patients and the clinic.
Keywords: COVID‐19, diabetes type 1, HbA1c, metabolic control, virtual contacts
Abbreviations
- FGM
flash glucose monitors
- CGM
continuous glucose monitors
- COVID‐19
Corona Virus Disease 2019
Key notes.
Despite COVID‐19 restrictions, the overall metabolic control in the children and adolescents studied was unchanged during the lockdown compared to the previous year.
However, children with lower pre‐lockdown HbA1c had a minor deterioration and children with higher HbA1c a significant improvement in metabolic control.
The lockdown enforced more virtual contacts between patients and the diabetes clinic.
1. INTRODUCTION
Since the beginning of 2020, the World has experienced the consequences of the COVID‐19 pandemic. On March 11th 2020, this led the Danish government to announce several measures to reduce the spread of the COVID‐19. As a result, all schools and kindergartens closed. Restaurants, hairdressers and shopping centres were closed. As all employees not having an essential/critical function were forced not to meet physically at work whenever possible approximately 40% of all employees worked at home full‐ or part‐time during the initial national lockdown, 1 8% were send home temporarily. 2 Furthermore, the unemployment rate increased to 6%. 3 Thus, more than half of the Danish workforce was home full‐ or part‐time.
On April 15th, the kindergartens re‐opened, and children in grades 0–5 returned to school. Older pupils at elementary school came back on May 18th and at high schools on May 27th. The schools and kindergartens stayed open until beginning of 2021, when an increase in the number of COVID‐19 cases again prompted the health authorities to recommend them closed.
At the end of May 2020, the society began slowly to reopen. Still, employees were recommended/asked to work from home as much as possible and restrictions on social life, like participation in sports events, remained in effect to varying degrees for the rest of the year.
In March 2020, hospitals were directed to postpone operations and other non‐essential treatments to increase the capacity for treating COVID‐19 cases and to reduce the risk of infecting patients at the hospitals. Consequently, only essential outpatient visits were accepted at the Department of Paediatrics and Adolescent Medicine at Kolding Hospital from March 15th to May 15th.
The number of visits to diabetes clinics is a significant predictor of HbA1c, 4 and frequent attendance at outpatient clinics leads to improved glycaemic control. 5 , 6 Corroborating this, both reducing the number of clinical contacts and having a high rate of cancelations or no‐shows have been shown to lead to higher HbA1c levels, 7 , 8 , 9 , 10 and a strike among health staff at a diabetes clinic led to an increase in HbA1c levels, mainly in patients with better glycaemic control. 11
Due to the evidence of the importance of frequent and regular contact with the paediatric diabetic clinics, both the International Society for Paediatric and Adolescent Diabetes (ISPAD) and the Danish health authorities recommend that children and adolescents with diabetes be seen at least every 3 months. 12 , 13
To evaluate the impact of the COVID‐19 lockdown and the resulting restrictions and adjustments in health care on the glycaemic control of the children and adolescents with diabetes type 1, we made use of this natural quasi‐experiment and investigated the changes in HbA1c and the use of the services offered by the diabetes clinic before, during and after the nationwide lockdown.
2. METHODS
This natural quasi‐experiment took place at the diabetes outpatient clinic at the Department of Paediatrics and Adolescent Medicine at the University Hospital of Southern Denmark, Kolding. The clinic's routine is to offer patients with HbA1c ≥ 64 mmol/mol appointments at the outpatient clinic at least every 6 weeks and patients with HbA1c < 64 mmol/mol every 3 months. At every visit, HbA1c was measured on Afinion HbA1c DS 100 analyzers (Alere/Abbott). 14 Parents or patients could call the diabetes specialist nurses from 8.00 am to 15.00 pm on weekdays and if needed, extra appointments could be arranged.
Because of the COVID‐19 restrictions, only outpatient visits considered to be essential by the paediatrician or the diabetes specialist nurse were accepted at the department from March 15th to May 15th resulting in much less patients being invited to come physically to the clinic. Furthermore, even in these cases, some patients/parents cancelled the appointments, as they were afraid of contracting COVID‐19 at the hospital. During the lockdown period, the clinic offered telephone and video consultations as a replacement for face‐to‐face consultations.
The study population included patients with type 1 diabetes diagnosed before 2020 and not moving or being transferred to an adult diabetic clinic before November 1st 2020. Information on which patients used insulin pumps and continuous glucose monitors (CGM) and flash glucose monitors (FGM) were drawn from the patients' medical records.
The routinely measured HbA1c from just prior to lockdown (last measurement on or before March 14th 2020, but no earlier than December 15th 2019: HbA1c(3)) and just after the lockdown of the outpatient clinic (first measurement on or after May 15th but no later than August 14th 2020: HbA1c(4)) was registered. For comparison, the HbA1c measured in the same periods 1 year previously were used (December 15th 2018–March 14th 2019: HbA1c(1) and May 15th–August 14th 2019: HbA1c(2)). Finally, the last HbA1c measured before January 14th 2021, but no earlier than October 1th 2020 (HbA1c(5)), was registered (Figure 1).
FIGURE 1.
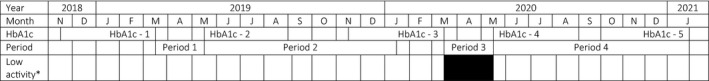
A timeline illustrating the time points of HbA1c measurements and the periods during which the number of contacts to the diabetes clinic were counted. For HbA1c(1), HbA1c(3) and HbA1c(5), the latest value in the interval was registered and for HbA1c(2) and HbA1c(4), the first value in the interval was registered
Furthermore, the number of physical consultations at the clinic and the number of virtual consultations by telephone or video registered in the periods March 15th to May 14th 2020 (period 3) and from May 15th 2020 to January 14th 2021 (period 4) were drawn from the hospital's registration system. For comparison, the same data were drawn for the corresponding periods 1 year before (March 15th to May 14th 2019 (period 1) and from May 15th 2019 to January 14th 2020 (period 2)) (Figure 1).
2.1. Data analysis
The main outcome was the difference between HbA1c(4) and HbA1c(3), considered as an indication of the change in glycaemic control during the lockdown period (period 3). The difference was compared to the change between HbA1c(1) and HbA1c(2), to investigate the effect of the lockdown taking a possible seasonal variation into account. Both analyses were stratified by pre‐lockdown HbA1c level (HbA1c(3) < 52 mmol/mol, 52–59 mmol/mol, and >59 mmol/mol) and patient pre‐lockdown age (0–11 years and 12–19 years).
Secondary outcomes were the change between HbA1c(5) and HbA1c(4) evaluating a possible effect of the reopening of the diabetes clinic during a period with continuous restrictions in the social life of the children. The analysis was stratified by pre‐lockdown HbA1c level. In addition, the difference between HbA1c(3) and HbA1c(5) was investigated to evaluate whether the glycaemic control 5–8 months after normalization of the operation of the clinic was comparable to the glycaemic control prior to lockdown.
Data were analysed using paired t‐test comparing mean HbA1c levels at the different time points of interest. Assumptions of normality were checked and found acceptable. Two outliers were detected on HbA1c(3) (HbA1c > 90 mmol/mol) and seven outliers were detected on the difference between HbA1c(3) and HbA1c(4) (HbA1c(4)‐(3) >20 or <−20 mmol/mol). Sensitivity analyses were performed to investigate the potential distorting effect from these outlying values. Patients with missing data on one or more variables of interest were left out from the respective analyses, and thus the number of analysed patients may vary across different models.
In addition, virtual contacts and visits at the diabetes clinic during the periods prior to the lockdown (periods 1 and 2), during the lockdown (period 3), and following the lockdown (period 4) were presented as descriptive statistics (median, minimum and maximum number of contacts/patient/month).
2.2. Ethics
According to the regional ethics committee of the Region of southern Denmark, no ethical approval was needed. Permission for evaluating the impact of the COVID‐19 restrictions on the outcome of the diabetes patients was according to guidelines granted by the hospital management (21.08.2020).
3. RESULTS
In January 2020, a total of 220 type‐1 diabetes patients were followed at the clinic. As 26 patients left the clinic before November 2020, 194 were included in the study. Among these, 23 patients got diabetes in 2019 and thus data are not available for that year. Of the patients included, 184 (94.8%) used insulin pumps and 182 (93.8%) used CGM or FGM. Basic characteristics of the study population are shown in Table 1.
TABLE 1.
Characteristics of the study population
| All | HbA1c level pre‐lockdown (HbA1C‐3) | ||||
|---|---|---|---|---|---|
| <52 mmol/mol | 52–59 mmol/mol | >59 mmol/mol | Missing | ||
| N (%) | 194 (100%) | 64 (33%) | 46 (24%) | 74 (38%) | 10 (5%) |
| Age pre‐lockdown, mean (min;max) | 13 (2;19) | 12 (3;18) | 12 (7;18) | 15 (2;19) | 10 (3;14) |
| Sex, N (%F) | 91 (47%) | 28 (44%) | 24 (52%) | 35 (47%) | 4 (40%) |
| Diagnosed in 2019, N (yes%) | 23 (12%) | 8 (13%) | 8 (17%) | 3 (4%) | 4 (40%) |
In paired t‐test, comparing mean HbA1c levels before and after lockdown (HbA1c(4)‐(3)) showed a mean HbA1c level of 58.3 ± 11.6 mmol/mol before and of 56.9 ± 12.2 mmol/mol after lockdown corresponding to a statistical significant decrease of −1.4 mmol/mol (95% CI −2.6–−0.2, p = 0.025). When stratifying by pre‐lockdown HbA1c, this difference was most pronounced among patients with HbA1c(3) > 59 mmol/mol showing a difference of −4.2 mmol/mol (95% CI −6.8–−1.7, p = 0.002) (Table 2). A sensitivity analysis excluding outliers showed similar results (data not shown). When stratified by pre‐lockdown age, the difference in HbA1c levels before and after lockdown was most pronounced among the 12–19‐year‐olds (HbA1c(3): 60.7 ± 12.3 and HbA1c(4): 58.6 ± 12.5, difference: −2.1 (95% CI −3.7–0.4), p = 0.013) compared to the 0–11‐year‐olds (HbA1c(3): 53.7 ± 8.5 and HbA1c(4): 53.6 ± 10.8, difference: −0.1 (95% CI −2.0–1.7), p = 0.867).
TABLE 2.
Paired t‐test comparing HbA1c levels before (HbA1c(3)) and after lockdown (HbA1c(4)) for all patients and stratified by pre‐lockdown HbA1c level (HbA1c(3))
| Mean HbA1c (mmol/mol) | Sd | 95% CI | p | |
|---|---|---|---|---|
| All patients (N = 172) | ||||
| HbA1c(4) | 56.9 | 12.2 | 55.1–58.7 | |
| HbA1c(3) | 58.3 | 11.6 | 56.6–60.1 | |
| Difference (HbA1c(4)‐(3)) | −1.4 | 8.2 | −2.6–−0.2 | 0.025 |
| Stratified analyses | ||||
| Pre‐lockdown HbA1c <52 mmol/mol (N = 60) | ||||
| HbA1c(4) | 47.9 | 6.0 | 46.4–49.5 | |
| HbA1c(3) | 47.1 | 4.4 | 46.0–48.2 | |
| Difference (HbA1c(4)‐(3)) | 0.8 | 4.6 | −0.4–2.0 | 0.176 |
| Pre‐lockdown HbA1c 52–59 mmol/mol (N = 44) | ||||
| HbA1c(4) | 55.6 | 6.4 | 53.7–57.6 | |
| HbA1c(3) | 55.7 | 2.0 | 55.1–56.3 | |
| Difference (HbA1c(4)‐(3)) | −0.1 | 6.2 | −1.9–1.8 | 0.942 |
| Pre‐lockdown HbA1c >59 mmol/mol (N = 68) | ||||
| HbA1c(4) | 65.7 | 13.0 | 62.5–68.8 | |
| HbA1c(3) | 69.9 | 8.3 | 67.9–71.9 | |
| Difference (HbA1c(4)‐(3)) | −4.2 | 10.6 | −6.8–−1.7 | 0.002 |
Investigating seasonal variation, a paired t‐test showed similar variation in mean HbA1c levels across 2019 and 2020 when comparing the difference between two yearly measurements in the same patient (HbA1c(2)‐(1): −1.5 ± 7.4 and HbA1c(4)‐(3): −1.7 ± 8.5, difference: 0.2 (95% CI −1.7–2.1), p = 0.832). Stratifying by pre‐lockdown HbA1c levels showed the variation being most stable among patients with HbA1c(3) 52–59 mmol/mol and with more variation in patients with HbA1c(3) <52 mmol/mol or >59 mmol/mol (Table 3). Stratifying by age showed similar results for seasonal variation in the two age groups (data not shown).
TABLE 3.
Paired t‐test comparing HbA1c(1) and HbA1c(2), in addition with paired t‐test investigating the seasonal variation in HbA1c levels in 2019 (HbA1c(2)‐(1)) and 2020 (HbA1c(4)‐(3)) for all patients and stratified by pre‐lockdown HbA1c (HbA1c(3))
| Mean HbA1c (mmol/mol) | Sd | 95% CI | p | |
|---|---|---|---|---|
| All patients (N = 155) | ||||
| HbA1c(2) | 59.1 | 11.8 | 57.2–60.9 | |
| HbA1c(1) | 60.4 | 11.8 | 58.5–62.2 | |
| Difference (HbA1c(2)‐(1)) | −1.3 | 7.4 | −2.5–−0.1 | 0.028 |
| All patients (N = 138) | ||||
| HbA1c(2)‐(1) (2019) | −1.5 | 7.4 | −2.7–−0.2 | |
| HbA1c(4)‐(3) (2020) | −1.7 | 8.5 | −3.1–0.2 | |
| Difference (HbA1c(2)‐(1))–(HbA1c(4)‐(3)) | 0.2 | 11.2 | −1.7–2.1 | 0.832 |
| Stratified analyses | ||||
| Pre‐lockdown HbA1c <52 mmol/mol (N = 45) | ||||
| HbA1c(2)‐(1) (2019) | −2.6 | 6.6 | −4.6–−0.6 | |
| HbA1c(4)‐(3) (2020) | 1.2 | 4.5 | −0.1–2.5 | |
| Difference (HbA1c(2)‐(1))–(HbA1c(4)‐(3)) | −3.8 | 7.2 | −6.0–−1.7 | 0.001 |
| Pre‐lockdown HbA1c 52–59 mmol/mol (N = 32) | ||||
| HbA1c(2)‐(1) (2019) | −1.9 | 7.4 | −4.6–0.8 | |
| HbA1c(4)‐(3) (2020) | −0.8 | 5.8 | −2.9–1.3 | |
| Difference (HbA1c(2)‐(1))–(HbA1c(4)‐(3)) | −1.1 | 7.8 | −3.9–1.7 | 0.433 |
| Pre‐lockdown HbA1c >59 mmol/mol (N = 61) | ||||
| HbA1c(2)‐(1) (2019) | −0.4 | 7.9 | −2.4–1.6 | |
| HbA1c(4)‐(3) (2020) | −4.3 | 11.0 | −7.1–−1.5 | |
| Difference (HbA1c(2)‐(1))–(HbA1c(4)‐(3)) | 3.9 | 13.9 | 0.3–7.4 | 0.034 |
Patients diagnosed in 2019 were excluded from the analyses.
Secondary analyses showed that when the diabetes clinic was back to normal operation, mean HbA1c levels increased (HbA1c(4): 57.6 ± 12.0 and HbA1c(5): 59.9 ± 11.5, difference: 2.2 (95% CI 0.7–3.8), p = 0.004) and returned to the mean HbA1c level before lockdown (HbA1c(3): 59.0 ± 11.5 and HbA1c(5): 59.9 ± 11.5, difference: 0.9 (95% CI −0.5–2.2), p = 0.227). When stratifying on pre‐lockdown HbA1c, the post‐lockdown increase was most pronounced in the subgroup with lowest pre‐lockdown HbA1c (<52 mmol/mol), (HbA1c(4): 48.8 ± 5.8 and HbA1c(5): 52.3 ± 7.5, difference: 3.5 (95% CI 1.3–5.6), p = 0.002), whereas for the subgroup with the highest pre‐lockdown HbA1c (HbA1c > 59 mmol/mol), the increase was less pronounced (HbA1c(4): 66.3 ± 13.2 and HbA1c(5): 67.4 ± 11.4, difference: 1.1 (95% CI −2.1–4.3), p = 0.50). For the group with intermediate values of HbA1c(3) (52–59 mmol/mol), an increase in between was found (HbA1c(4): 55.7 ± 6.5 and HbA1c(5): 57.8 ± 8.2, difference: 2.1 (95% CI −0.1–4.2), p = 0.065).
Descriptive statistics on number of visits and virtual contacts to the diabetes clinic showed that the median number of visits were 0.5 visits per patient per month in the periods before (periods 1 and 2) and after lockdown (period 4). During the lockdown (period 3), the median number of visits at the clinic was 0 while virtual contacts was 0.5 indicating a higher number of virtual contacts during lockdown (Figure 2).
FIGURE 2.
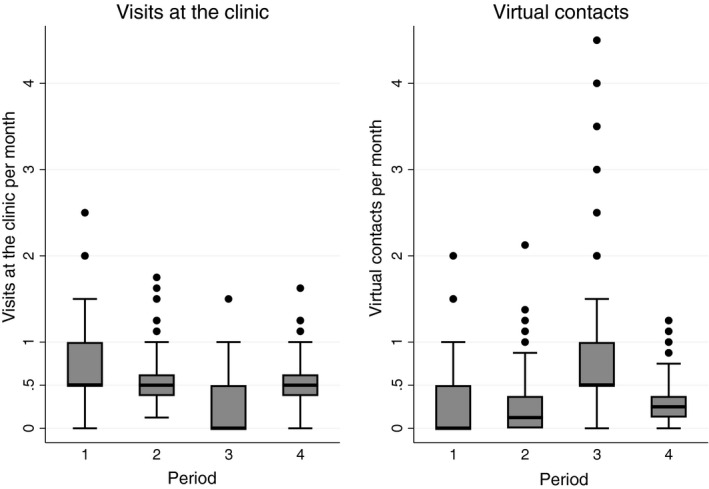
Box and whiskers plots displaying the distribution of visits at the diabetes clinic and virtual contacts in the four periods under study
4. DISCUSSION
The importance of patients with diabetes being seen regularly has been confirmed by many studies. 4 , 5 , 6 , 7 , 8 , 9 , 10 , 11 . We therefore expected that the reduced availability to the paediatric diabetes team would have caused deterioration in the glycaemic control. However, overall we found a significant improvement in mean HbA1c from before until after the period with restricted access to the diabetic clinic. As the lockdown took place during spring, the improvement in HbA1c could be explained by seasonal changes, which was confirmed by a comparison with the changes in HbA1c during the same period in 2019, indicating that overall the metabolic control of the patients followed at the clinic did not change due to the lockdown.
We have previously shown that the better the glycaemic control, the greater the negative effect of reducing the availability to the diabetic clinic. 11 Corroborating these results, children with pre‐lockdown HbA1c‐values of <52 mmol/mol had a slight increase in mean HbA1c during the lockdown as opposed to a significant decrease during the same season the previous year. Children with pre‐lockdown HbA1c ≥ 59 mmol/mol had an improved glycaemic control during lockdown contrasting unchanged values the previous year. In both years, a minor improvement in glycaemic control was seen for children with pre‐lockdown HbA1c‐values between 52 and 59 mmol/mol. The finding that the higher the HbA1c, the greater the positive effect of the lockdown could be partly explained by a ‘regression towards the mean’ effect. However, a tendency of regression towards the mean was not observed in 2019 where the better the glycaemic control, the greater the positive effect of the season.
A Spanish study in adults found an improvement during lockdown mainly in patients with poorer baseline control. 15 One of the few studies in children and adolescents comparing HbA1c from before until after lockdown also found an improvement, which was inversely correlated with HbA1c values measured just before lockdown. 16 A brief report from Sweden found an unchanged HbA1c during the first 7 months of 2020 compared to 2019. 17 Other studies comparing CGM or FGM readings in adults 18 , 19 , 20 and in children 21 , 22 have shown overall improvements in glycaemic control during lockdown. However, as these studies did not take season into consideration, the improvement could be due to season.
As seen in Table 1, the children with poorer glycaemic control before lockdown were older, which agrees with the fact that glycaemic control often deteriorates during the teenage years. We have previously shown that shortening the interval between visits to the diabetes clinic helped the children with higher HbA1c to improve their glycaemic control. 6 Nevertheless, for children with the poorer glycaemic control, HbA1c decreased from 69.9 to 65.7 mmol/mol despite of not being seen at the clinic. Even though many children achieve the ability of self‐care by the age of around 12 years, non‐adherence is particularly an issue with adolescents. 23 During lockdown, the schools were closed for the children of approximately 12 years and above, and social activity outside the closest family was almost non‐exciting. As around every second adult either worked from home full‐ or part‐time or was unemployed, 1 , 2 , 3 most children and adolescents spend much more time than usual with one or both parents. The more regular lifestyle, the more regular and for some probably better quality meals combined with the possibility of more support and help from parents could explain the significant improvement in glycaemic control for this group of patients despite of probably less physical activity.
In contrast to the patients with the poorer glycaemic control, the children with the better glycaemic control did not improve their HbA1c during lockdown, if anything a slight deterioration was seen. For these patients, the positive effect of spending more time with a parent was probably less, as they were younger and therefore tended to get more support at school and to have less social challenges and demands. 24 , 25 We have previously seen a negative effect of not offering consultations during a period of 2 months for the children with better control. 11 Therefore, we speculate that the lack of physical consultations at the clinic could have had a negative effect on these patients, even though the number of virtual contacts increased considerably.
However, other factors were at play, one of the most important being the reduced opportunity for physical activity. Regular physical activity is recommended for all patients with diabetes, 26 and a meta‐analysis has shown a significant reduction in HbA1c as a consequence of physical activity. 27 After the services at the hospital returned to normal and schools reopened, restrictions continued to varying degrees for the rest of 2020 hampering social life and limiting the possibility to participate in sport activities. 28 In fact, 8 months after the reopening, the mean HbA1c had increased significantly and had returned to or slightly above the pre‐lockdown value while one would have expected the glycaemic control to continue to improve as has happened during recent years. 7 , 29
The patients with the worse glycaemic control pre‐lockdown not only had the best outcome during the initial lockdown period; they also had the smallest increase in HbA1c post‐lockdown. One can hypothesise that even though the restrictions imposed on their lives had a negative effect on physical activity, the more regular daily life and the more regular contact with the parents due to many still working at least part‐time at home had the opposite effect and overall resulted in only a slight increase in HbA1c post lockdown. 22 Actually, these patients ended up having a better glycaemic control after the first 10 months of the pandemic than they had pre‐lockdown.
The patients with the better pre‐lockdown HbA1c‐values had the largest increase post‐lockdown, which may indicate that the restrictions imposed on their daily lives had a negative impact on the glycaemic control, where the lack of physical activity could be one of the factors. 27 The better opportunity of getting support from the diabetes clinic and of having closer contact to the parents might thus have been less important for this group of patients. This corroborate a recent Danish study finding that children with HbA1c < 59 mmol/mol indicated having sufficient support from teachers and fellow students. 25
Before March 2020, the patients had a median of 0.5 face‐to‐face consultations per months, which corresponds to what has previously been seen at the clinic. 7 As expected, very few consultations were performed during the lockdown period. It has been anticipated that the experience obtained in using telephone and video consultations during the COVID‐19 pandemic will cause some face‐to‐face contacts to change to virtual contacts. 30 That the number of physical consultations after re‐opening increased to pre‐lockdown levels could be due to the patients and the clinicians going back to old habits, but is more likely due to a backlog following the 2 months closure of the clinic. Prior to lockdown, the number of virtual contacts was approximately 0.1 per patient per month 7 ; this increased to approximately 0.5 during lockdown, and decreased only slightly during the following 8 months indicating that a change in the contact pattern might actually have taken place. Considering the experience from the lockdown period and with the increased use of diabetes technologies, more face‐to‐face contacts could be expected to be replaced by telemedicine consultations. 30 However, we need to be cautious as face‐to‐face contacts between healthcare providers and patients are invaluable, especially when dealing with children and adolescents. 17 , 25
A methodological strength of the study is the relatively high number of observations and the long follow‐up time. A limitation is that HbA1c was measured using Afinion HbA1c DS 100 analyzers with a measurement variation of 2%. 14 However, we expect the measurement error to be random, and thus the precision is improved by investigating group means. In addition, we depended on HbA1c measurements from visits to the clinic why the intervals from which we accepted values are between 3–4 months. Furthermore, the number of included patients was predetermined by the number of patients followed at the clinic. Therefore, sub‐analyses were performed with reduced power.
A limitation of this natural experiment is the potential risk of bias from residual confounding especially from dietary habits and physical activity, which we assume is associated with both lockdown and change in HbA1c‐level from time point (3) to (4). However, information on these parameters was not available. Another limitation is that the analyses did not include download data from insulin pumps and CGM or FGM, which could have given detailed information on the changes in the daily handling of the diabetes (number of insulin doses taken, the total insulin dosage, the time in range, number of scans and carbohydrates entered), whereas HbA1c gives an overall indication of the metabolic control. However, the day‐to‐day variation in handling of the diabetes was beyond the scope of this paper.
5. CONCLUSION
The overall decrease in HbA1c during lockdown corresponded to the decrease observed the previous year. However, despite all patients being subject to the same restrictions during the COVID‐19 lockdown, the influence on their glycaemic control varied. For children with the better pre‐lockdown HbA1c levels, the lack of face‐to‐face contacts in the diabetes clinic and the limited possibilities for doing sport and having a social life outside the family might have influenced their metabolic control negatively, whereas patients with the worse glycaemic control improved their HbA1c levels, which might have been due to a more structured daily life, less daily stress and better and easier contact with parents.
The experience gained by patients, parents and staff using telemedicine during the lockdown seemed to be used also during the initial 8 months following the normalisation of the diabetic clinic and could be expected to have an impact on future consultations.
CONFLICT OF INTEREST
None.
ACKNOWLEDGEMENTS
We thank Hans Jørn Refsgaard Jørgensen, specialist consultant, Lillebaelt Hospital, University Hospital of Southern Denmark, for helping draw data from the hospital registration system.
Kofoed P‐E, Timm S. The impact of COVID‐19 lockdown on glycaemic control and use of health services among children followed at a Danish diabetes clinic. Acta Paediatr.2022;111:368–375. doi: 10.1111/apa.16128
REFERENCES
- 1. Danmarks Statistik . NYT: Hjemmearbejde fordoblet i 2020 – Danmarks. https://www.dst.dk/da/Statistik/nyt/NytHtml?cid=32435. Accessed March 14, 2021.
- 2. Erhvervsstyrelsen . Statistik for kompensationsordninger | erhvervsstyrelsen.dk. https://erhvervsstyrelsen.dk/statistik‐kompensationsordninger. Accessed March 14, 2021.
- 3. Kommunernes Landsforening . Ledighedsstigningen i coronakrisen rammer meget forskelligt i landets kommuner. https://www.kl.dk/nyheder/makro‐analyseenheden/nyt‐om‐dansk‐oekonomi/ledighedsstigningen‐i‐coronakrisen‐rammer‐meget‐forskelligt‐i‐landets‐kommuner/. Accessed March 14, 2021.
- 4. Kaufman FR, Halvorson M, Carpenter S. Association between diabetes control and visits to a multidisciplinary pediatric diabetes clinic. Pediatrics. 1999;103:948‐951. [DOI] [PubMed] [Google Scholar]
- 5. Rhee MK, Slocum W, Ziemer DC, et al. Patient adherence improves glycemic control. Diabetes Educ. 2005;31:240‐250. [DOI] [PubMed] [Google Scholar]
- 6. Kofoed P‐E, Pedersen C, Thomsen J. Do more frequent visits at the outpatient clinic improve glycaemic control in children and adolescents with a high HcA1c? Pediatr Diabetes. 2008;9:29.18211634 [Google Scholar]
- 7. Kofoed PE, Thomsen J. Leaving the responsibility of booking appointments to parents in a paediatric diabetes outpatient clinic resulted in a deterioration of glycaemic control. Pediatr Diabetes. 2020;21:390‐394. [DOI] [PubMed] [Google Scholar]
- 8. Fortin K, Pries E, Kwon S. Missed medical appointments and disease control in children with type 1 diabetes. J Pediatr Health Care. 2016;30:381‐389. [DOI] [PubMed] [Google Scholar]
- 9. Markowitz JT, Volkening LK, Laffel LM. Care utilization in a pediatric diabetes clinic: cancellations, parental attendance, and mental health appointments. J Pediatr. 2014;164:1384‐1389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Fisher E, Lazar L, Shalitin S, et al. Association between glycemic control and clinic attendance in emerging adults with type 1 diabetes: a tertiary center experience. J Diabetes Res. 2018;2018:9572817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Kofoed P‐E, Thomsen J, Ammentorp J. An unplanned delay between control visits influences the metabolic status in children with diabetes. An observational study. Acta Paediatrica. 2010;99:774‐777. [DOI] [PubMed] [Google Scholar]
- 12. The Danish National Board of Health . http://www.endocrinology.dk/Kliniske%20retningslinier%20‐%20Diabetes%20hos%20boern%20og%20unge.pdf. Accessed March 14, 2021.
- 13. Pihoker C, Forsander G, Fantahun B, et al. The delivery of ambulatory diabetes care to children and adolescents with diabetes. Pediatr Diabetes. 2018;2018(Suppl 27):84‐104. [DOI] [PubMed] [Google Scholar]
- 14. Wood JR, Kaminski BM, Kollman C, et al. Accuracy and precision of the Axis‐Shield Afinion hemoglobin A1c measurement device. J Diabetes Sci Technol. 2012;6:380‐386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Fernández E, Virginia A, Bellido V. Impact of COVID‐19 lockdown on glycemic control in patients with type 1 diabetes. Diabetes Res Clin Pract. 2020;166:108348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Marigliano M, Maffeis C. Glycemic control of children and adolescents with type 1 diabetes improved after COVID‐19 lockdown in Italy. Acta Diabetol. 2021;58:661‐664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Ludvigsson J. Effect of COVID‐19 pandemic on treatment of Type 1 diabetes in children. Acta Paediatr. 2021;110:933‐934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Dover AR, Ritchie SA, McKnight JA, et al. Assessment of the effect of the COVID‐19 lockdown on glycaemic control in people with type 1 diabetes using flash glucose monitoring. Diabet Med. 2021;38(1):e14374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Capaldo B, Annuzzi G, Creanza A, et al. Blood glucose control during lockdown for COVID‐19: CGM metrics in Italian adults with type 1 diabetes. Diabetes Care. 2020;43(8):e88‐e89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Mesa A, Viñals C, Pueyo I, et al. The impact of strict COVID‐19 lockdown in Spain on glycemic profiles in patients with type 1 Diabetes prone to hypoglycemia using standalone continuous glucose monitoring. Diabetes Res Clin Pract. 2020;167:108354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Predieri B, Leo F, Candia F, et al. Glycemic control improvement in Italian children and adolescents with type 1 diabetes followed through telemedicine during lockdown due to the COVID‐19 pandemic. Front Endocrinol (Lausanne). 2020;11:595735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Schiaffini R, Barbetti F, Rapini N, et al. School and pre‐school children with type 1 diabetes during Covid‐19 quarantine: the synergic effect of parental care and technology. Diabetes Res Clin Pract. 2020;166:108302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Bratina N, Forsander G, Annan F, et al. ISPAD Clinical Practice Consensus Guidelines 2018: management and support of children and adolescents with type 1 diabetes in school. Pediatr Diabetes. 2018;19(Suppl 27):287‐301. [DOI] [PubMed] [Google Scholar]
- 24. Bixo Ottosson A, Åkesson K, Ilvered R, Forsander G, Särnblad S. Self‐care management of type 1 diabetes has improved in Swedish schools according to children and adolescents. Acta Paediatr. 2017;106:1987‐1993. [DOI] [PubMed] [Google Scholar]
- 25. Eriksen TM, Gaulke A, Thingholm PR, Svensson J, Skipper N. Association of type 1 diabetes and school wellbeing: a population‐based cohort study of 436,439 Danish schoolchildren. Diabetologia. 2020;63(11):2339‐2348. [DOI] [PubMed] [Google Scholar]
- 26. Colberg SR, Sigal RJ, Yardley JE, et al. Physical activity/exercise and diabetes: a position statement of the American Diabetes Association. Diabetes Care. 2016;39(11):2065‐2079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. MacMillan F, Kirk A, Mutrie N, Matthews L, Robertson K, Saunders DH. A systematic review of physical activity and sedentary behavior intervention studies in youth with type 1 diabetes: study characteristics, intervention design, and efficacy. Pediatr Diabetes. 2014;15(3):175‐189. [DOI] [PubMed] [Google Scholar]
- 28. Chen P, Mao L, Nassis GP, Harmer P, Ainsworth BE, Li F. Coronavirus disease (COVID‐19): the need to maintain regular physical activity while taking precautions. J Sport Health Sci. 2020;9(2):103‐104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. https://www.sundhed.dk/content/cms/87/4687_aarsrapport_diabetes_2019_20_endelig_praksis.pdf. Accessed March 14, 2021.
- 30. Nørgaard K. Telemedicine consultations and diabetes technology during COVID‐19. J Diabetes Sci Technol. 2020;14:767‐768. [DOI] [PMC free article] [PubMed] [Google Scholar]


