Abstract
Coronavirus disease‐2019 (Covid‐19) disrupted the in‐person teaching format of anatomy. To study changes in gross anatomy education that occurred during August–December, 2020 compared to before the pandemic, an online survey was distributed to anatomy educators. The 191 responses received were analyzed in total and by academic program, geographic region, and institution type. Cadaver use decreased overall (before: 74.1 ± 34.1%, during: 50.3 ± 43.0%, P < 0.0001), as well as across allopathic and osteopathic medicine, therapy, undergraduate, and veterinary programs (P < 0.05), but remained unchanged for other programs (P > 0.05). Cadaver use decreased internationally and in the US (P < 0.0001), at public and private (P < 0.0001) institutions, and among allopathic medical programs in Northeastern, Central, and Southern (P < 0.05), but not Western, US geographical regions. Laboratories during Covid‐19 were delivered through synchronous (59%), asynchronous (4%), or mixed (37%) formats (P < 0.0001) and utilized digital resources (47%), dissection (32%), and/or prosection (21%) (P < 0.0001). The practical laboratory examination persisted during Covid‐19 (P = 0.419); however, the setting and materials shifted to computer‐based (P < 0.0001) and image‐based (P < 0.0001), respectively. In‐person lecture decreased during Covid‐19 (before: 88%, during: 24%, P = 0.003). When anatomy digital resources were categorized, dissection media, interactive software, and open‐access content increased (P ≤ 0.008), with specific increases in BlueLink, Acland's Videos, and Complete Anatomy (P < 0.05). This study provided evidence of how gross anatomy educators continued to adapt their courses past the early stages of the pandemic.
Keywords: coronavirus, Covid‐19, gross anatomy education, integrated curriculum, laboratory, lecture, medical education, online anatomy, remote teaching, stand‐alone course, virtual anatomy
INTRODUCTION
Since the acute respiratory syndrome coronavirus 2 and coronavirus disease‐2019 (Covid‐19) were first identified in December 2019 (Spiteri et al., 2020), the impact on the health of citizens globally has been unprecedented, with over 212 million cases and approximately 4 million deaths globally from Covid‐19 as of August 23, 2021 (Johns Hopkins, 2021). On December 1, 2020, over 997 million learners were affected by Covid‐19‐related closures (UNESCO, 2020). While this number is staggering, it is lower than the peak of approximately 1.5 billion affected learners reported in April, 2020 (UNESCO, 2020). As a result, health professions educators had to quickly adapt and continually evolve their curricula to be in compliance with local health mandates.
Health professions education has been uniquely impacted by Covid‐19‐related restrictions. Health professions' curricula rely heavily on in‐person mentorship (Burgess et al., 2018) and clinical training (Peters & ten Cate, 2014). On April 7, 2020, the Centers for Medicare and Medicaid Services issued a statement that recommended limiting all non‐essential planned surgeries and procedures and dental care indefinitely (CMS, 2020). This drastically reduced the opportunity for trainees to participate in common procedures in their respective fields, such as internal medicine (Alboraie et al., 2020; Shah et al., 2020), interventional radiology (Cahalane et al., 2020), otolaryngology (Guo et al., 2020), dentistry (Kathree et al., 2020), surgery (Khan & Mian, 2020), and manual therapy (MacDonald et al., 2020). Furthermore, many hospital systems and health professions schools elected to remove trainees from the clinical environment (Khan & Mian, 2020) due to insufficient supplies of personal protective equipment (PPE) and to limit Covid‐19 exposure and transmission (AACN, 2020; Khamees et al., 2020). Beyond the formal training, celebratory milestones in health sciences education, such as convocations (Grajek, 2020) and white coat ceremonies (Murphy, 2020), were forced to be reformatted as virtual or outdoor events.
Challenges were not unique to clinical training and institutional events; Covid‐19 made the traditional format(s) of foundational sciences education through in‐person lecture and laboratory‐based teaching no longer feasible. Gross anatomy, a foundational discipline in health professions education (Rizzolo, 2002; Drake et al., 2009; Sugand et al., 2010), was notably impacted due to its reliance on small group, in‐person instruction using human cadavers. Guidelines and information for body donor programs were published to address the safety of receiving human donors (Kramer et al., 2020; Lemos et al., 2021; Onigbinde et al., 2021a), and anatomy educators had to determine how to safely continue gross anatomy teaching (Onigbinde et al., 2021a). Ethical guidelines were published for anatomy educators who use cadaveric materials for online teaching (BACA, 2021). Even memorial services for human body donors needed to be redesigned for online delivery (Singal et al., 2021).
Data from the initial period of the pandemic (beginning March, 2020) indicated that anatomy laboratories were converted largely from in‐person sessions using cadaveric materials to remote virtual sessions leveraging digital teaching resources and other teaching modalities at individual institutions (Cuschieri & Calleja Agius 2020; Muñoz‐Leija et al., 2020; Naidoo et al., 2020; Herr & Nelson, 2021), within broader geographical regions, such as Western Europe (Brassett et al., 2020), the United Kingdom and Republic of Ireland (Longhurst et al., 2020), Australia and New Zealand (Pather et al., 2020), China (Cheng et al., 2021), and globally (Harmon et al., 2021). Simultaneously, lectures transitioned from predominantly in‐person to various remote mediums (Longhurst et al. 2020; Pather et al., 2020; Cheng et al., 2021; Harmon et al., 2021).
Several publications documented the immediate response to Covid‐19, highlighting the innovations and creative instruction that anatomy educators pursued. However, these reports were limited to single institutions (Cuschieri & Calleja Agius 2020; Naidoo et al. 2020; Srinivasan, 2020; Bond & Franchi, 2021; Harrell et al, 2021; Herr & Nelson, 2021) or institutions within a specific geographic region (Brassett et al. 2020; Longhurst et al. 2020; Pacheco et al., 2020; Pather et al., 2020; Cheng et al., 2021). Additionally, these studies were descriptive and did not present inferential statistics comparing gross anatomy education before and during Covid‐19. While the publications mentioned previously provided insight into the early adaptations to gross anatomy education during Covid‐19, to the authors' knowledge, there are no publications analyzing the curricular changes made beyond the early stages of the pandemic. While there were anecdotal calls for returning to the anatomy laboratory (Onigbinde et al., 2021b; Ross et al., 2021), quantification of such a return had not been done. It is unknown whether the initial curricular adaptations persisted, as anatomy educators were continuously requesting insight from their colleagues about how to teach during the pandemic.
Early in the pandemic, anatomy educators had many questions about teaching during Covid‐19 (Harmon et al., 2021). The number of relevant discussions on Anatomy Connected (2021), the American Association for Anatomy's (AAA) online member forum, served as an index of this uncertainty. Thirty‐five “open forum” posts generated 279 comments regarding the transition of anatomy teaching online or how to continue in‐person teaching safely between March 12 and July 31, 2020. The majority of this activity occurred in March/April (26 posts/240 comments). This large amount of discussion between anatomy educators led to the development of the “Virtual Anatomy During Covid‐19” survey (Harmon et al., 2021). The survey requested responses from programs teaching gross anatomy early in the pandemic (i.e., courses running between May to August, 2020) and later in the pandemic (i.e., courses running between August–December, 2020). Harmon et al. (2021) provided the first insight into how gross anatomy courses (e.g., methods of laboratory teaching, laboratory assessment, digital resources) were organized prior to Covid‐19 and how they changed across academic programs early in the pandemic, between March and August, 2020. While the majority of discussions among anatomy educators occurred between March and July, 2020, the conversations continued through December. Between August 1 and December 31, 2020, discussion in this community continued with seven open forum discussions involving 41 posts from 31 individuals. Discussion topics included: (i) A desire to know what instructional format(s) other schools were using (virtual vs. in‐person); (ii) practical implementation of, and/or planning for a return to in‐person teaching (including safety concerns regarding cadavers necessary for in‐person laboratories, and planning for longer practical examination days due to socially distanced/smaller examination cohorts); and (iii) bolstering virtual anatomy teaching (Anatomy Connected, 2021). It was evident that the uncertainty did not subside after the early stages of the pandemic, and anatomy educators were continuously looking for examples from other institutions.
The main purpose of this article was to continue the analysis of gross anatomy curricula before Covid‐19 and examine how the curricula changed between the months of August–December, 2020. The main purpose was assessed through two objectives. The first objective of this study was to determine the lecture and laboratory delivery methods among courses that ran between August ‐December, 2020 and to assess their changes by academic program, integrated compared to stand‐alone anatomy courses, institutional location, and private compared to public institutions. The final objective was to characterize the teaching adaptations by the anatomy educator community and explore assessment methods, anatomical modalities utilized for laboratory education, and digital and other resources utilized to aid in anatomy education during Covid‐19.
METHODS
Survey features
The study was classified as exempt by the Institutional Review Board at the University of California, San Francisco (protocol #20‐31300). The data compiled for this study were acquired from June 8, 2020 to November 1, 2020 for the academic period of August–December 2020. The data were collected through the distribution of the “Virtual Anatomy During Covid‐19 Survey” previously published by Harmon et al. (2021). Survey responses were collected electronically through Qualtrics XM (Qualtrics, Provo, UT). Survey development and piloting were conducted by the authors prior to distribution. Anatomy educators in higher education teaching in undergraduate and graduate programs in the United States (US) and internationally were the target population. Responses to all survey questions were optional.
The survey consisted of 20 unique questions. The first three questions of the survey asked respondents for general contact information (name, email, and institution). Following the questions on contact information, participants were asked if they are teaching anatomy between August–December 2020. If they selected “yes,” they were asked to select from the following list of programs in which they would teach: anatomy graduate, dental, allopathic medicine, osteopathic medicine, occupational therapy, physical therapy, physician assistant, undergraduate anatomy programs, and up to three “other” options where respondents could write in any program that was not listed. Participants were asked to complete the same series of 13 questions for each program that they selected. For example, if a participant selected allopathic medicine and occupational therapy programs, they would first complete the series of 13 questions on the allopathic medicine program followed by the same series of 13 questions on the occupational therapy program.
The 13 questions surveyed respondents on small group organization during Covid‐19, organization of the gross anatomy laboratory and lecture components of the course, and the utilization of gross anatomy digital resource(s) before and during Covid‐19. Respondents were asked to indicate the percentage of time utilizing dissection, prosection, plastinated specimens, plastic models, comparative anatomy models, and “other” teaching modalities in the gross anatomy laboratory. The current study defines prosections, plastinated specimens, and plastic models as follows: “prosections” are cadaveric materials that have been previously dissected to focus on a particular set of structures for direct teaching; “plastinated specimens” are prosections where the water and fat content have been replaced by a plastic material (von Horst et al., 2019); and “plastic models” are commercially purchased artistically‐rendered models made of plastic. Respondents were asked to select one of the following lecture delivery methods: in‐person lectures with a live stream, in‐person lectures without a live stream, previously recorded lectures, virtual live lectures, or “other” lecture formats. Following the laboratory and lecture‐specific questions, a series of narrative questions asked participants to provide a description of a “typical” laboratory session during Covid‐19, as well as their laboratory‐based assessment before and during Covid‐19.
Following the series of 13 questions for each program(s), three final questions asked participants to indicate the video conference platform(s) used by their institution to teach anatomy, to identify any non‐anatomy‐specific teaching tool(s) they planned to purchase to aid in teaching (e.g., camera tripod), and to select from a list of assessment software or technology that their institution used for gross anatomy (users could select all that applied and provide unlisted assessment software).
Survey distribution and data collection
Anatomy educators were recruited through various online mediums for professional associations and listservs including the AAA, the American Association of Clinical Anatomists, the American Physical Therapy Association, DR‐ED, and the Human Anatomy and Physiology Society. The authors also distributed the survey link through their professional Twitter (San Francisco, CA) accounts. Finally, AAA members were notified of the survey through forum posts on Anatomy Connected and through the Anatomy Now Weekly, the AAA's electronic newsletter. The recruitment of anatomy educators began on June 8, 2020. To collect the responses from anatomy educators teaching during August–December, 2020, the survey invitation was distributed through the same mediums during the week of September 23, 2020 and again two weeks later. Furthermore, the authors emailed the survey link to their professional networks.
The dataset was then exported and organized with Microsoft Excel (Microsoft Corp., Redmond, WA). All responses selected as “other” with a description were individually evaluated and classified into an existing category or designated as a unique response for further analysis by three authors (B.A.K., C.J.R., and D.C.B.).
Quantitative data
When data were available, respondent‐reported institutions were categorized as US or international. New US institutions that were not previously categorized as public or private by Harmon et al. (2021) were categorized as private or public by a single author (D.J.H.) using the name of the institution provided in the survey. The classification of public versus private and the US versus international was done by accessing each institutions' website to obtain the relevant information. Public and private institutions were defined according to the US Department of Homeland Security's website (DHS, 2013) as previously reported (Harmon et al., 2021). Additionally, survey responses for the US allopathic medical programs were categorized by geographical region (Northeastern, Central, Southern, and Western) by a single author (G.J.F.) according to the Association of American Medical Colleges (AAMC, 2021). Only US allopathic medical programs were classified by geographical region because of a robust sample size (i.e., >40) that contained institutional data.
To maximize the power for statistical analysis, selected survey response data were combined into groups. Responses from physical (n = 11), occupational (n = 2), chiropractic (n = 3), and radiation (n = 1) therapy formed a “therapy” group, while graduate programs in biomedical engineering (n = 1), medical physics (n = 1), organ donation science (n = 1), pharmacy (n = 1), podiatric medicine (n = 1), and psychology (n = 1) formed a “graduate health” group. A response indicating a program in dental hygiene (n = 1) was excluded only from the program‐specific analyses because a single response was received. All the other programs remained unchanged. Survey responses about teaching modalities utilized in anatomy laboratories were consolidated into three groups: “cadaver” (dissection and prosection), “plastic material” (plastinated specimens and anatomical models), and “other” (comparative specimens and other types) as established previously by Harmon et al. (2021). Similarly, responses about lecture delivery method(s) were consolidated into two groups: “in‐person lectures” (in‐person lectures with or without a live stream), “not in‐person” (lectures previously recorded or delivered remotely). Frequencies were calculated for digital resources, video conferencing software, assessment software, and non‐anatomy teaching tools.
Digital resource data were grouped into five categories by a single author (H.M.G.) and corroborated by a second author (K.M.H.). The categories included two‐dimensional (2D) illustrations, dissection media, interactive software, in‐house material, and open‐access content. 2D illustrations were defined as commercial products (e.g., image banks, atlases, and dissectors) whose image‐based content consists largely of illustrated renderings or photographs of anatomical structures. Dissection media were classified as commercial products containing dissection‐based images and/or videos showing cadaveric dissection but with limited or no interactivity other than viewing. Interactive software was delineated as commercial products that were mostly three‐dimensional (3D)‐based, allowed for cross‐sectional viewing, and/or offered interactivity for the user to manipulate anatomical structures. In‐house material was defined as non‐commercial, dissection‐based, image‐based, 2D, or 3D products produced within the respondents' University or program. Lastly, open‐access content was defined by free, non‐commercial products, such as dissection‐based, image‐based, 2D, or 3D content (e.g., University of Michigan Blue Link, University of Wisconsin School of Medicine and Public Health Dissection Videos, University of British Columbia Anatomy Videos), produced outside of the respondents' University or program. For each of the five categories, the number of respondents was calculated before and during Covid‐19 using Microsoft Excel.
Statistical comparisons were made for the total number of responses and by the program (as defined above), type of gross anatomy course (integrated and stand‐alone), region (US and international), type of institution (public and private), and geographical location of allopathic US medical school (as defined above) before and during Covid‐19. All data were assessed for parametric or nonparametric distribution using the Shapiro‐Wilk test and histograms. Continuous data that did not meet parametric standards were log‐transformed (all data are presented as non‐transformed) to reduce its skewness. For continuous data, Wilcoxon signed‐rank test, Mann–Whitney U test, and Kruskal–Wallis H test with Dunn's post hoc analysis were used to compare responses across groups (type of program, gross anatomy course, location, and institution) and time‐points (before and during Covid‐19). When appropriate, a Bonferroni post hoc adjustment for multiple comparisons was performed. Comparisons between groups as well as comparisons before and during Covid‐19 were analyzed using the Chi‐square test of independence or the McNemar's test for unpaired and paired categorical data, respectively. The response rate (= number of responses/viewed or started survey) for the survey was calculated. Internal consistency was assessed with Cronbach alpha according to the criteria published by (Taber, 2018). The significance level was set a priori at α < 0.05. All statistical analyses were performed using SPSS statistical package, version 26 (IBM Corp., Armonk, NY).
Narrative data
Open‐ended responses describing the methods used in anatomy laboratory teaching and assessment methods before and during Covid‐19 were each coded by a team of two researchers (M.B., J.F.D. and S.M.A., K.M.B., respectively). Descriptive codes were applied to the data to summarize the content (Saldaña, 2016), with the coding structure, determined a priori according to previously published methods (Harmon et al., 2021). Three categories of codes were applied to each laboratory setting used: (1) delivery modality (i.e., type of synchrony); (2) format of laboratory practice (i.e., dissection, prosection); (3) the format of student groups. Three categories of codes were applied to each assessment: (1) setting of the assessment (i.e., where it took place), (2) format of the assessment, and (3) the material used for the question (e.g., cadaver, medical imaging, plastic model). The first coders for each team (J.F.D. and K.M.B.) coded the data in Microsoft Excel. The second coders for each team (M.B. and S.M.A.) reviewed the coded dataset and coding discrepancies were discussed and reconciled with the first coder. Code frequencies within each category were tabulated using Microsoft Excel.
RESULTS
Descriptive characteristics and sample sizes are presented in Table 1. Of the 187 respondents who indicated the type of gross anatomy course, use of a stand‐alone anatomy course was reported by 64% of the anatomy graduate, 60% of the graduate health, 64% of the dental, 60% of the nursing, 100% of the physician assistant, 33% of the veterinary, 83% of the therapy, 19% of the allopathic medicine, 50% of the osteopathic medicine, and 65% of the undergraduate programs (P < 0.001). Alternatively, the use of an integrated anatomy curriculum was reported by 36% of the anatomy graduate, 40% of the graduate health, 36% of the dental, 40% of the nursing, 0% of the physician assistant, 67% of the veterinary, 17% of the therapy, 81% of the allopathic medicine, 50% of the osteopathic medicine, and 35% of the undergraduate programs (P < 0.001). Fifty‐two percent of the surveyed private institutions and 64% of the public institutions reported using an integrated anatomy course (P > 0.05), whereas 48% of private institutions and 36% of public institutions used a stand‐alone anatomy course (P > 0.05). With regard to the type of course at the United States and international institutions, 58% of the surveyed US institutions and 32% of the international institutions reported using an integrated anatomy course (P = 0.006), and 42% of the US institutions and 68% of international institutions used a stand‐alone anatomy course (P = 0.013). A total of 62 US allopathic medical programs were categorized by region with 34% in the Northeastern, 27% in the Central, 26% in the Southern, and 13% in the Western US (P = 0.026; Table 1).
TABLE 1.
Descriptive characteristics and sample sizes for survey responses regarding adaptations to teaching anatomy during Covid‐19 (August–December, 2020)
| Variable | n (%) |
|---|---|
| Programs (n = 191) | |
| Allopathic medicine | 71 (37) |
| Undergraduate | 40 (21) |
| Anatomy graduate | 19 (10) |
| Therapy a | 17 (9) |
| Dental | 11 (6) |
| Osteopathic medicine | 11 (6) |
| Graduate health b | 6 (3) |
| Nursing | 6 (3) |
| Physician assistant | 6 (3) |
| Veterinary | 3 (2) |
| Dental hygiene | 1 (0) |
| Type of anatomy course (n = 187) | |
| Stand‐alone course | 95 (51) |
| Integrated anatomy course | 92 (49) |
| Did not reply to prompt | 4 |
| United States and International Institution (n = 172) | |
| United States | 140 (81) |
| International | 32 (19) |
| Unclear or unreported | 19 |
| Type of institution (United States institutions only) (n = 140) | |
| Private | 62 (44) |
| Public | 78 (56) |
| Geographical location of United States allopathic medical programs c (n = 62) | |
| Northern | 21 (34) |
| Central | 17 (27) |
| Southern | 16 (26) |
| Western | 8 (13) |
| International or unreported institution data | 9 |
| Variable | n |
|---|---|
| Teaching delivery, assessment, and digital resources | |
| Teaching delivery in the anatomy laboratory | 179 |
| Assessment software | 262 |
| Assessment Setting, Structure, And Material | 186 |
| Anatomy digital resources | 200 |
| Other anatomy teaching tools | 133 |
| Video communication software | 206 |
Therapy includes physical (n = 11), occupational (n = 2), and radiation (n = 1) therapy and chiropractic (n = 3) programs.
Graduate health includes engineering (n = 1), medical physics (n = 1), organ donation science (n = 1), pharmacy (n = 1), podiatric medicine (n = 1), and psychology (n = 1) graduate programs.
United States allopathic medical programs were categorized by geographical regions according to the Association of American Medical Colleges (AAMC, 2021).
The response rate was 76% and the Cronbach alpha coefficient was 0.73, suggesting the survey instrument measured with acceptable internal consistency (Taber, 2018).
Laboratory teaching
Overall, a significantly greater percentage of respondents used cadavers for in‐laboratory teaching before Covid‐19 as compared to during Covid‐19 (before: 74.1 ± 34.1% and during: 50.3 ± 43.0%, P < 0.0001). The transition away from cadaver‐based instruction aligned with a simultaneous significant decrease of “plastics” (before: 19.1 ± 27.7% and during: 15.0 ± 25.2%, P = 0.009) and a statistically significant increase of “other” laboratory modalities (before: 6.7 ± 18.6% and during: 33.7 ± 42.3%, P < 0.0001).
Academic programs
Figure 1 shows the percentage of laboratory time using cadaver, plastic, and “other” teaching modalities before and during Covid‐19 by the academic program.
FIGURE 1.
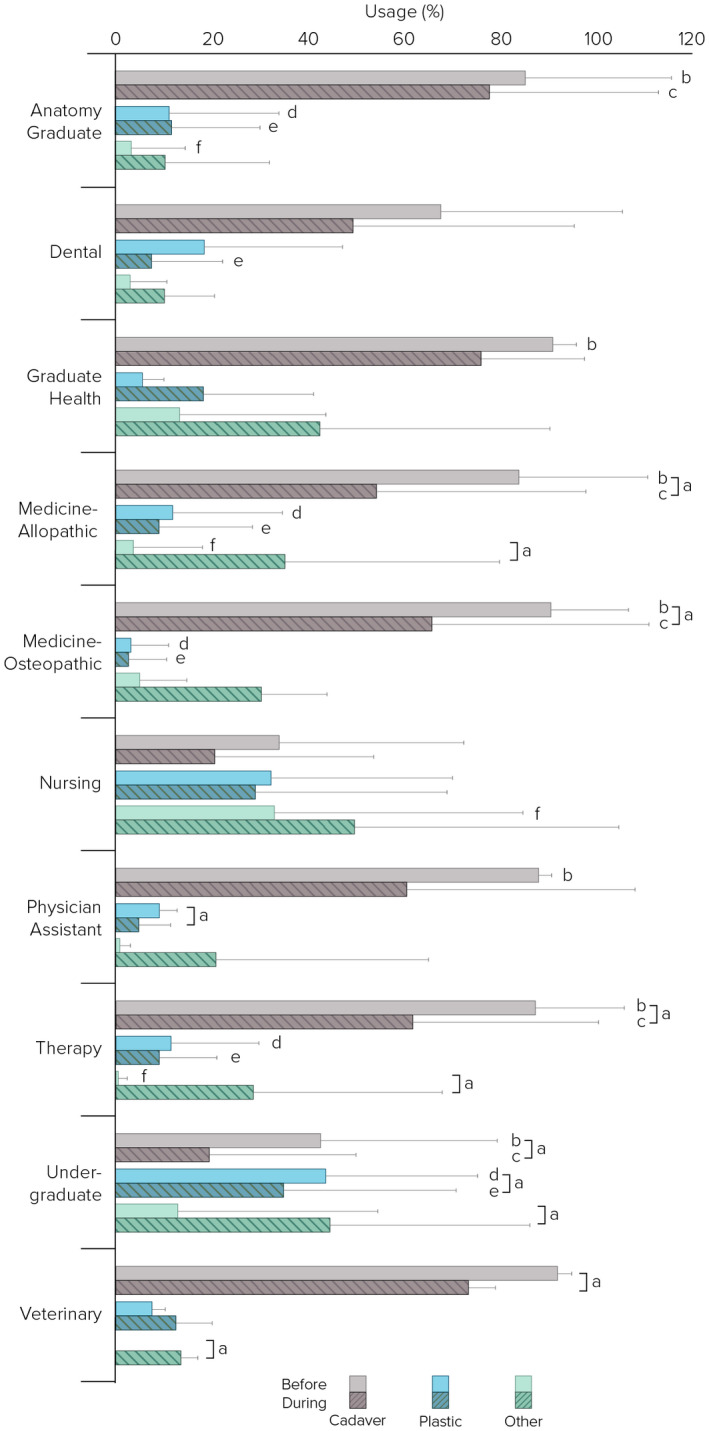
Percentage of laboratory time using cadaver, plastic, and “other” teaching modalities before and during Covid‐19 pandemic (August–December 2020) by academic program (n = 190; anatomy graduate, n = 19; dental, n = 11; graduate health, n = 6; allopathic medicine, n = 71; osteopathic medicine, n = 11; nursing, n = 6; physician assistant, n = 6; therapy, n = 17; undergraduate n = 40; veterinary, n = 3). Cadaver includes dissection and prosection; plastic includes plastic models and plastinated specimens. aPercent time using cadaver, plastic, and “other” were significantly different before and during Covid‐19 (P ≤ 0.045); bPercent time using cadavers was significantly different across programs before Covid‐19 (Kruskal–Wallis test H, P < 0.0001). Dunn's post hoc analysis showed that cadaver usage was significantly less in the undergraduate versus anatomy graduate (P = 0.001), allopathic (P < 0.0001) and osteopathic (P < 0.0001) medicine, physician assistant (P = 0.019), therapy (P < 0.0001), and graduate health (P = 0.047) programs. Similarly, cadaver usage was significantly less in the nursing versus anatomy graduate (P = 0.010), allopathic (P = 0.004) and osteopathic (P = 0.007) medicine, and therapy (P = 0.008) programs; cPercent time using cadavers was significantly different across programs during Covid‐19 (Kruskal–Wallis test H, P < 0.0001). Dunn's analysis showed that cadaver usage was significantly less in the undergraduate versus anatomy graduate (P < 0.0001), allopathic (P = 0.001) osteopathic (P = 0.027) medicine, and therapy (P = 0.016) programs; dPercent time using plastics was significantly different across programs before Covid‐19 (Kruskal–Wallis test H, P < 0.0001). Dunn's analysis showed that plastics usage was significantly greater in the undergraduate versus anatomy graduate (P < 0.0001), allopathic (P < 0.0001) and osteopathic (P < 0.0001) medicine, and therapy (P < 0.0001) programs; ePercent time using plastics was significantly different across programs during Covid‐19 (Kruskal–Wallis test H, P < 0.0001). Dunn's analysis showed that cadaver usage was significantly less in the undergraduate versus anatomy graduate (P = 0.017), dental (P = 0.026), allopathic (P < 0.0001) and osteopathic (P < 0.003) medicine, and therapy (P = 0.010) programs; fPercent time using “other” was significantly different across programs before Covid‐19 (Kruskal–Wallis test H, P = 0.006). Dunn's analysis showed that cadaver usage was significantly greater in the nursing versus anatomy graduate (P = 0.018), allopathic medicine (P = 0.006), and therapy (P = 0.010) programs
Cadaver use was significantly reduced during Covid‐19 across allopathic (before: 84.3 ± 26.7% and during: 54.5 ± 43.6%, P < 0.0001) and osteopathic (before: 91.2 ± 15.7% and during: 66.3± 44.9%, P = 0.033) medicine, therapy (before: 87.7 ± 18.2% and during: 62.1 ± 38.7%, P = 0.016), undergraduate (before: 42.9 ± 36.5% and during: 19.5 ± 30.4%, P < 0.0001), and veterinary (before: 92.3 ± 2.5% and during: 73.7 ± 5.5%, P = 0.010) programs. Alternatively, cadaver use did not significantly change (P > 0.05) during Covid‐19 for anatomy graduate (before: 85.5 ± 30.7% and during: 77.95 ± 35.3%), graduate health (before: 91.3 ± 4.8% and during: 76.3 ± 21.6%), dental (before: 67.9 ± 37.8% and during: 49.6 ± 46.1%), nursing (before: 34.2 ± 38.5% and during: 20.8 ± 32.9%), and physician assistant (before: 88.3 ± 2.6% and during: 60.8 ± 47.4%) programs.
With respect to plastics use, the only programs to significantly reduce their usage during Covid‐19 were the physician assistant (before: 9.2 ± 3.8% and during: 5.0 ± 6.3%, P = 0.045) and undergraduate (before: 43.9 ± 31.3% and during: 35.1 ± 35.7%, P = 0.033) programs. No significant changes (P > 0.05) were observed concerning plastic usage for anatomy graduate (before: 11.2 ± 22.9% and during: 11.8 ± 18.3%), graduate health (before: 5.7 ± 4.5% and during: 18.4 ± 23.1%), dental (before: 18.6 ± 29.0% and during: 7.6 ± 14.8%), allopathic (before: 12.0 ± 23.0% and during: 9.10 ± 19.5%) and osteopathic (before: 3.5 ± 7.4% and during: 3.0 ± 7.5%) medicine, nursing (before: 32.5 ± 37.7% and during: 29.2± 39.8%), therapy (before: 11.7 ± 18.3% and during: 9.2 ± 12.0%), and veterinary (before: 7.7 ± 2.5% and during: 12.7 ± 7.5%) programs.
Alternatively, allopathic medicine (before: 3.8 ± 14.4% and during: 35.5± 44.6%, P < 0.0001), therapy (before: 0.63 ± 1.7% and during: 28.8 ± 39.1%, P = 0.012), undergraduate (before: 13.0 ± 20.8% and during: 44.8 ± 41.4%, P < 0.0001), and veterinary (before: 0.0 ± 0.0% and during: 13.7 ± 3.2%, P = 0.018) programs all significantly increased their use of “other” resources during Covid‐19. No significant changes (P > 0.05) were observed concerning “other” resources for anatomy graduate (before: 3.3 ± 11.5% and during: 10.3 ± 21.8%), dental (before: 13.5 ± 30.4% and during: 42.7 ± 47.8%), graduate health (before: 3.1 ± 7.6% and during: 5.0 ± 10.3%), osteopathic medicine (before: 5.4 ± 9.9% and during: 30.7 ± 13.6%), nursing (before: 33.3 ± 51.6% and during: 50.0 ± 54.8%), and physician assistant (before: 1.0 ± 2.2% and during: 21.0 ± 44.2%) programs.
Analysis with Kruskal–Wallis H demonstrated that before Covid‐19, the largest percentage of laboratory teaching time was devoted to cadaveric materials, although this differed significantly across academic programs (P < 0.0001; Figure 1). Post hoc analysis showed that cadaver usage before Covid‐19 was significantly less in the undergraduate programs as compared to the anatomy graduate (P < 0.0001), allopathic (P < 0.0001) and osteopathic (P < 0.0001) medicine, therapy (P < 0.0001), physician assistant (P = 0.019), and graduate health (P = 0.047) programs. Similarly, cadaver usage before Covid‐19 was significantly less in nursing programs as compared to anatomy graduate (P = 0.010), allopathic (P = 0.004) and osteopathic (P = 0.007) medicine, therapy (P = 0.008), and physician assistant (P = 0.045) programs. Use of cadaveric material during Covid‐19, significantly differed across academic programs (P < 0.0001), with undergraduate programs using significantly less than anatomy graduate programs (P < 0.0001), allopathic (P = 0.001) and osteopathic (P = 0.027) medicine, and therapy (P = 0.016) programs. All other post hoc findings concerning cadaver use across programs before and during Covid‐19 did not reach statistical significance (P > 0.05).
Before Covid‐19, the laboratory time allocated to teaching with plastics significantly differed across the academic programs (P < 0.0001; Figure 1). Post hoc examination identified that plastic usage was significantly greater in undergraduate programs as compared to anatomy graduate (P < 0.0001), allopathic (P < 0.0001) and osteopathic (P < 0.0001) medicine, and therapy (P < 0.001) programs. Similarly, during Covid‐19, plastic usage within the academic programs also significantly differed across programs (P < 0.0001) with undergraduate programs devoting significantly more teaching time toward plastics as compared to anatomy graduate (P = 0.017), dental (P = 0.026), allopathic (P < 0.0001) and osteopathic (P = 0.003) medicine, and therapy (P = 0.010) programs. All other post hoc findings concerning plastic use across programs before and during Covid‐19 did not reach statistical significance (P > 0.05).
The percentage of laboratory time devoted to “other” teaching modalities during Covid‐19 was not significantly different across academic programs (P = 0.172); however, before Covid‐19, it was significantly different across programs (P = 0.006; Figure 1). Post hoc analysis showed that “other” usage was significantly greater in nursing programs as compared to anatomy graduate (P = 0.018), allopathic medicine (P = 0.006), and therapy (P = 0.008) programs. All other post hoc findings concerning “other” teaching modalities across programs before and during Covid‐19 did not reach statistical significance (P > 0.05).
Type of gross anatomy course
Figure 2 shows the percentage of laboratory time using cadaver, plastic, and “other” teaching modalities before and during Covid‐19 by type of gross anatomy course. Stand‐alone (before: 76.2 ± 31.0% and during: 51.4 ± 42.9%, P < 0.0001) and integrated (before: 73.1 ± 35.9% and during: 51.4 ± 43.0%, P < 0.0001) anatomy courses saw a significant decrease in cadaver use during Covid‐19. A significant increase in “other” teaching modalities during Covid‐19 were observed in stand‐alone (before: 5.1 ± 14.6% and during: 32.1 ± 42.1%, P < 0.0001) and integrated anatomy (before: 6.5 ± 17.5% and during: 32.6 ± 41.3%, P < 0.0001) courses. Plastic usage significantly decreased in integrated anatomy courses (before: 20.4 ± 30.4% and during: 14.9 ± 25.0%, P = 0.021), while changes in stand‐alone courses did not reach statistical significance (before: 18.0 ± 25.2% and during: 15.7 ± 25.9%, P = 0.263).
FIGURE 2.
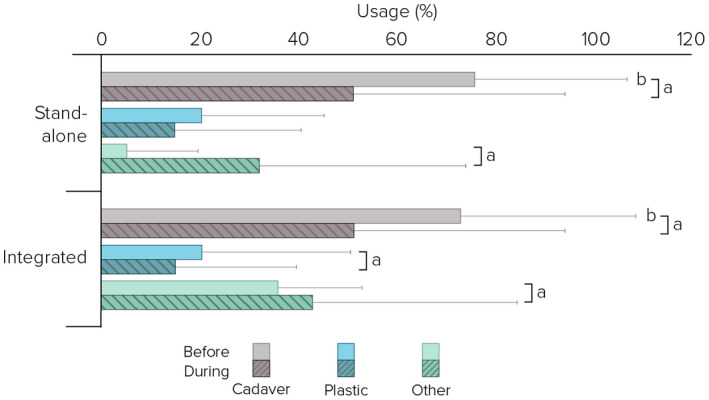
Percentage of laboratory time using cadaver, plastic, and “other” teaching modalities before and during Covid‐19 pandemic (August–December 2020) by type of gross anatomy course (n = 187; stand‐alone, n = 95; Integrated, n = 92). Cadaver includes dissection and prosection; plastic includes plastic models and plastinated specimens. aPer cent time using cadaver, plastic, and “other” were significantly different before and during Covid‐19 (Wilcoxon signed‐rank, P ≤ 0.021); bPercent time using cadavers was significantly greater in stand‐alone versus integrated courses before Covid‐19 (Mann–Whitney U, P = 0.046)
Before Covid‐19, stand‐alone anatomy courses spent a significantly greater percentage of in‐laboratory time using cadaveric materials relative to integrated anatomy courses (P = 0.046; Figure 2). No other significant differences were found (P > 0.05).
United States and international institutions
Figure 3 demonstrates the percentage of laboratory time using cadaver, plastic, and “other” teaching modalities before and during Covid‐19 by international and US institutions. A significant decrease in cadaver use during Covid‐19 was observed at both international (before: 60.0 ± 38.4% and during: 31.3 ± 38.3%, P < 0.0001) and US (before: 76.5 ± 32.6% and during: 53.4 ± 42.8%, P < 0.0001) institutions, while a significant increase in “other” use during Covid‐19 was found at both international (before: 11.5 ± 22.7% and during: 50.6 ± 43.2%, P < 0.0001) and US (before: 6.2 ± 18.6% and during: 30.8 ± 41.2%, P < 0.0001) institutions. Regarding plastic usage, there was a significant decrease in international institutions (before: 28.5 ± 31.4% and during: 18.1 ± 26.8%, P = 0.042), although US institutions did not reach a statically significant decrease (before: 17.0 ± 25.8% and during: 14.9 ± 25.1%, P = 0.144).
FIGURE 3.
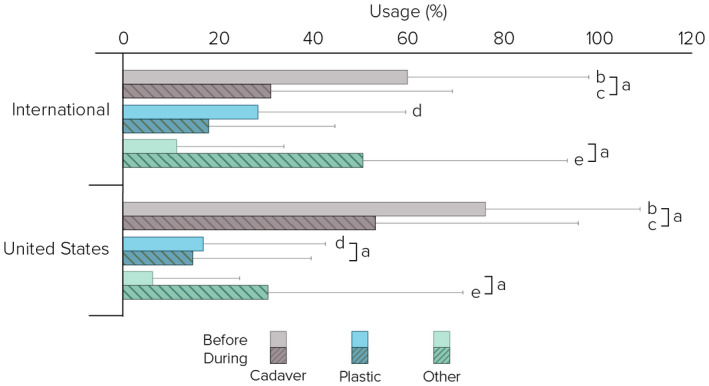
Percentage of laboratory time using cadaver, plastic, and “other” teaching modalities before and during Covid‐19 pandemic (August–December 2020) by US and International Institutions (n = 172; international, n = 32; US n = 140). Cadaver includes dissection and prosection; plastic includes plastic models and plastinated specimens. aPercent time using cadaver, plastic, and “other” were significantly different before and during Covid‐19 (Wilcoxon signed‐rank, P ≤ 0.042); bPercent using cadaver was significantly greater in US institutions versus international institutions before Covid‐19 (Mann–Whitney U, P = 0.030); cPercent using cadaver was significantly greater in US institutions versus international institutions during Covid‐19 (Mann–Whitney U, P = 0.006); dPercent using plastic was significantly greater in international versus US institutions before Covid‐19 (Mann–Whitney U, P = 0.031); ePercent using “other” was significantly greater in international versus US institutions during Covid‐19 (Mann–Whitney U, P = 0.021)
Before (P = 0.030) and during (P = 0.006) Covid‐19, US institutions spent a significantly greater percentage of in‐laboratory time using cadaveric materials relative to international (Figure 3). In contrast, compared to US institutions, international institutions spent a significantly greater percentage of time in the laboratory using plastic and “other” teaching modalities before (P = 0.031) and during (P = 0.021) Covid‐19, respectively (Figure 3).
Type of institution
Figure 4 exhibits the percentage of laboratory time using cadaver, plastic, and “other” teaching modalities before and during Covid‐19 by the US public and private institutions. A significant decrease in cadaver use during Covid‐19 was observed at both public (before: 72.4 ± 35.6% and during: 46.9 ± 43.5%, P < 0.0001) and private (before: 82.5 ± 27.4% and during: 63.2 ± 40.7%, P < 0.0001) institutions. Alternatively, a significant increase in “other” use during Covid‐19 was found at both public (before: 8.4 ± 23.0% and during: 36.3 ± 43.7%, P < 0.0001) and private (before: 3.3 ± 9.9% and during: 22.9 ± 36.7%, P < 0.0001) institutions. Regarding plastic usage, private institutions (before: 14.1 ± 23.6% and during: 12.7 ± 23.2%, P = 0.604) did not reach a statistically significant decrease. However, public institutions trended toward a significant decrease (before: 19.0 ± 27.2% and during: 16.3 ± 26.4%, P = 0.066).
FIGURE 4.
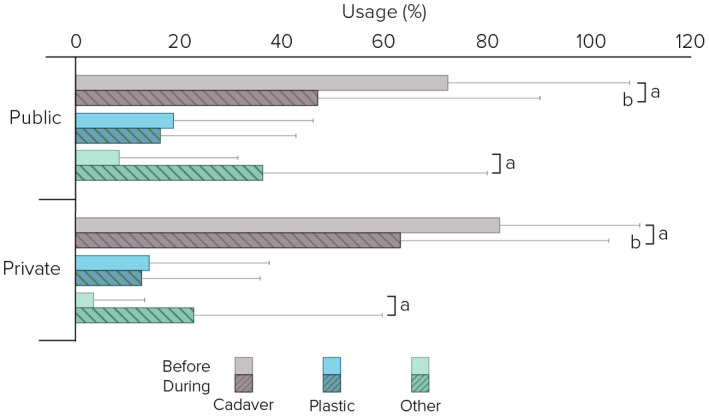
Percentage of laboratory time using cadaver, plastic, and “other” teaching modalities before and during Covid‐19 pandemic (August–December 2020) by type of institution (n = 140; private, n = 62; public n = 78). Cadaver includes dissection and prosection; plastic includes plastic models and plastinated specimens. aPercent time using cadaver and “other” were significantly different before and during Covid‐19 (Wilcoxon signed‐rank, P ≤ 0.004); bPercent using cadaver was significantly greater in private versus public institutions during Covid‐19 (Mann–Whitney U, P = 0.035)
The percentage of laboratory time spent using cadaveric materials during Covid‐19 was significantly greater at private institutions relative to public institutions (P = 0.024). Before and during Covid‐19, the percentage of time using plastic and “other” laboratory modalities did not reach statistically significant differences at public versus private institutions (P = 0.058 and P = 0.062), respectively (Figure 4).
Geographical location of United States allopathic medical programs
Figure 5 demonstrates the percentage of laboratory time using cadaver, plastic, and “other” teaching modalities before and during Covid‐19 by geographical region of US allopathic medical programs. Cadaver usage among US allopathic medical programs in Northeastern (before: 88.2 ± 19.0% and during: 50.6 ± 44.7%, P = 0.001), Central (before: 87.1 ± 23.3% and during: 57.7 ± 45.4%, P = 0.011), and Southern (before: 88.6 ± 24.2% and during: 66.3 ± 39.8%, P = 0.027), but not Western (before: 82.9 ± 33.7% and during: 60.6 ± 47.7%, P = 0.177), geographical regions significantly decreased during Covid‐19. During Covid‐19, the use of “other” laboratory teaching material significantly increased across Northeastern (before: 3.8 ± 13.6% and during: 38.1 ± 46.1%, P = 0.003), Central (before: 5.9 ± 24.3% and during: 35.3 ± 49.3%, P = 0.020), and Southern (before: 0.94 ±2.5% and during: 27.1 ± 37.9%, P = 0.016) allopathic medical program, while Western allopathic programs did not significantly increase (before: 0.71 ± 1.9% and during: 28.3 ± 45.8%, P = 0.165). Changes in plastic usage did not meet statistical significance during Covid‐19 in Northeastern (before: 8.0 ± 14.8% and during: 11.3 ± 25.9%, P = 0.197), Central (before: 7.0 ± 6.4% and during: 7.1 ± 12.6%, P = 0.982), Southern (before: 10.5 ± 24.5% and during: 6.6 ± 12.6%, P = 0.260), and Western (before: 16.5 ± 34.0% and during: 2.1 ± 3.6%, P = 0.281) allopathic medical programs (Figure 5). Additionally, when evaluating the data with Kruskal–Wallis test, no significant differences were observed between US regions before Covid‐19 as well as during Covid‐19 regarding percentage of time teaching with cadaver, plastic, or “other” materials (P > 0.05).
FIGURE 5.
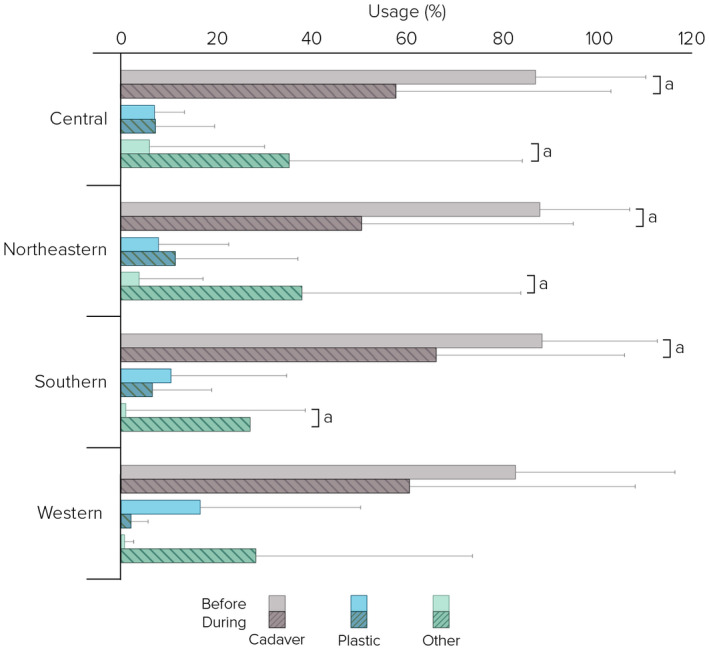
Percentage of laboratory time using cadaver, plastic, and “other” teaching modalities before and during Covid‐19 pandemic (August–December 2020) by geographical location of United States allopathic medical programs (n = 62; northern, n = 21; central, n = 17; southern, n = 16; western, n = 8). Cadaver includes dissection and prosection; plastic includes plastic models and plastinated specimens. aPercent time using cadaver and “other” were significantly different before and during Covid‐19 (Wilcoxon signed‐rank, P = 0.027)
Lecture teaching
The percentage of respondents who relied on in‐person lectures for content delivery before Covid‐19 significantly decreased during Covid‐19 (before: 88% and during: 24%, P = 0.003), while not in‐person lecture delivery significantly increased during Covid‐19 compared to before Covid‐19 (before: 12% and during: 76%, P = 0.003). Some respondents provided examples of their lecture format during Covid‐19: “Lecture with 1/2 cohort physically in lecture, 1/2 virtually live,” “Taught the content virtually over the summer doing Zoom lectures,” and “Class meets for 2.5 hours twice weekly for lecture and lab. The lecture will move to online.”
Laboratory and small group formats
A significantly greater percentage of respondents indicated a hybrid in‐person and virtual anatomy laboratory (37%) during Covid‐19, compared to other responses that indicated virtual‐only (25%), in‐person only (23%), they did not know the format (14%), or anatomy laboratory was completely canceled (1%) (P = 0.006). The percentage of respondents indicating virtual small groups (46%) trended toward a significant difference compared to those that conducted in‐person (15%) small groups or did not respond (39%) (P = 0.065).
Laboratory teaching structure
Analysis of the narrative comments specific to how anatomy laboratory teaching was delivered between August–December, 2020 centered around three categories: (1) delivery modality, (2) format of laboratory practice, and (3) format of student groups (Table 2). Although the level of detail included in the responses varied, attributes for each of the three categories were readily identified. In addition, 11 subcategories were identified during the coding process (Table 2). Forty‐eight responses were coded as “unclear, unreported, or undetermined” for laboratory teaching structure. The remaining responses in each category are presented in Table 2. Representative comments are provided verbatim.
TABLE 2.
Laboratory delivery modality, format of laboratory practice, and format of student groups during Covid‐19 (August–December, 2020)
| Category | Subcategories | n (%) a | χ 2 | P‐value |
|---|---|---|---|---|
| Delivery modality | Synchronous in‐person | 52 (40.9) | 74.2 | <0.0001 |
| Synchronous not in‐person | 23 (18.1) | |||
| Asynchronous not in‐person | 5 (3.9) | |||
| Mixed: synchronous & asynchronous not in‐person | 16 (12.6) | |||
| Mixed: synchronous in‐person & asynchronous not in‐person | 27 (21.3) | |||
| Mixed: synchronous in‐person & asynchronous not in‐person | 4 (3.1) | |||
| Total | 127 (100) | |||
| Format of laboratory practice | Dissection | 41 (32.3) | 20.7 | 0.0001 |
| Prosection b | 27 (21.3) | |||
| Anatomy digital resource(s) c | 59 (46.5) | |||
| Total | 127 (100) | |||
| Format of student groups | Small group | 50 (76.9) | 18.8 | <0.0001 |
| Large group | 15 (23.1) | |||
| Total | 65 (100) |
Total number of respondents (n = 179); Chi‐square test, P < 0.05.
Responses coded as unclear, undetermined, or unreported were not included in the analysis (n = 48).
Denotes prosection as faculty‐ or student‐led and is distinct from anatomy digital resources.
Commercial and/or in‐house anatomy digital resources were included in the comments.
Delivery modality
The most frequent statements addressed the delivery of laboratory teaching content. Responses emphasized the use of synchronous, asynchronous, mixed delivery, or were unclear/undetermined. In the current study, these terms are defined as follows: “synchronous” refers to educational activities that take place in real‐time (Allen et al., 2019); “asynchronous” does not occur at the same time (Allen et al., 2019); and “mixed delivery” involves elements of both types of synchrony (Harmon et al., 2021). The delivery modality responses were separated into those who reported information that could be analyzed further into subcategories (71%), and those who had not yet determined their laboratory delivery format or their response was unclear or unreported (29%).
Based on the 71% of respondents who provided information on their laboratory delivery modality, the use of synchronous and mixed formats were varied and sub‐categories for these formats were identified: Synchronous in‐person, Synchronous not in‐person, Mixed: Synchronous in‐person and Asynchronous not in‐person, Mixed: Synchronous and asynchronous not in‐person, and Mixed: Synchronous in‐person and Synchronous not in‐person.
Analysis of synchronous laboratory sessions revealed two subcategories specific to the synchronous delivery modality: Synchronous in‐person and Synchronous not in‐person. These reflected different institutions electing to return to campus or continue with virtual teaching. A large proportion of institutions had returned to Synchronous in‐person sessions (40.9%) incorporating faculty‐ or student‐led dissection or prosection sessions (see “format of laboratory practice”). Responses reflected the need for reduced capacity and scheduling enough time in the laboratory for all students in the course/cohort:
While most lectures will be given live virtually, the laboratory component will be face‐to‐face instruction with faculty members. Students will wear PPE, practice social distancing, and be limited to two students per cadaveric specimen […] Right now, we will have to run the lab sessions in two separate groups either 90 minutes each or find additional times where the students can enter the labs for instruction.
Few institutions reported the use of Synchronous not in‐person laboratories (18.1%). In these responses, teaching methods similar to Synchronous in‐person were emphasized but this occurred via video conferencing platforms (e.g., Zoom) to permit not in‐person delivery. Overall, review of anatomy digital resources, small group “breakout” sessions, and/or live streaming of faculty‐led dissection or prosection reviews were frequently modeled in this example:
The plan is for students to have access ad libitum to virtual anatomy software that they have purchased, with scheduled real‐time smaller group sessions with instructors and TAs, and assigned weekly exercises and/or quizzes for course credit.
Analysis of the respondents that provided insight into their mixed laboratory sessions revealed three sub‐categories specific to the type of blending of modalities used for delivery: Synchronous in‐person and Asynchronous not in‐person, Synchronous and asynchronous not in‐person, and Synchronous in‐person and Synchronous not in‐person. The most frequent subcategory was Synchronous in‐person & Asynchronous not in‐person (21.3%) and was best characterized by laboratory sessions utilizing on campus, in‐person laboratories, complemented by an asynchronous, not in‐person component typically used for review of digital, pre‐laboratory resources, or a laboratory module.
The structure of the anatomy laboratory session during Covid‐19 involves bringing students on campus in small groups (12–14 students) for an hour (1:30–4:30, 3 groups rotate through lab) per region (back, shoulder region, upper limb, etc.) in the lab to view prosected donors. The remainder of laboratory instruction is via independent and asynchronous viewing of the posted materials. Due to Covid[‐19] restrictions, some students may not be able to attend a session and are offered an additional make‐up session. The lab visits, however, are supplemental learning as all testable material is provided online in the learning platform.
The mixed, Synchronous and asynchronous not in‐person (12.6%) type of delivery activities were also described:
The students are provided pre‐lab modules that explain the dissection approach (had they been in lab) and hyperlinks to the 4D Anatomy and VH Dissector software. Students are expected to review the pre‐lab and work through the links prior to attending lab. We scheduled 2‐hours blocks of time via zoom. During this time, the delivery varies by faculty member, but has included either of the following two options: (1) 30 minutes of lecture/concept review with 1 hour of live/streaming prosection review or (2) live, active dissection (1.5–2 hours) by the faculty member. A second faculty member or student TA is working as the Zoom jockey to relay incoming questions/comments to the faculty member leading the lab session. In the prosection review and active dissection, the faculty members are relaying important concepts, reviewing structure/function/innervation, and noting clinical relevance, when applicable.
The final sub‐category of mixed laboratory delivery was the Synchronous in‐person and Synchronous not in‐person format. This was the least frequently used of the mixed delivery modalities (3.1%), but incorporated remote, synchronous sessions to complement synchronous in‐person laboratories with reduced student capacity. For example:
Half of the class attends a 2‐hours lab: 1‐hour prosections; 1‐hour dry lab (bones, models, clinical content). Half of the class receives virtual interactive lab modules with the same content—completed on one day (2.5 hours protected time) and followed up with TA tutorial (1.5 hours) for consolidation and Q&A.
Only 3.9% of respondents utilized Asynchronous not in‐person laboratory sessions.
Format of laboratory practice
A number of respondents elaborated on the format of laboratory practice. The laboratory practice responses were divided into two broad categories: Those who reported information that could be analyzed further into dissection, prosection, and/or digital resources (71%), and those who had not yet determined their format of laboratory practice or their response was unclear or unreported (29%).
Based on the 71% of respondents who provided information on their format of laboratory practice, they described dissection (student‐led), prosection (faculty‐ and student‐led), and the utilization of commercial and/or in‐house anatomical digital resources. Thirty‐two percent of respondents that provided information about their laboratory practice indicated that dissection was part of their laboratory format. For example:
Class is split into four cohorts (~50 students each) and student lab groups of four (e.g., two students in Cohort 1, and two students in Cohort 2). Students work in groups of two to dissect as usual (2 hours lab at quarter‐capacity) then meet virtually on Zoom or Teams to discuss with their group members in the other cohort. The other two students go to the next lab (2 hours lab at quarter‐capacity) and dissect as usual. After all four students in each lab group have participated in the lab, they meet on Zoom or Teams to discuss the anatomy and reflect on the laboratory experience.
Responses denoting the utilization of prosection (21.3%) during anatomy laboratory teaching emphasized faculty‐led prosection reviews, often with the involvement of teaching assistants, followed by a student‐led component for practice and self‐assessment. For example:
Sign‐up sheet for prosection viewing with faculty and MS4 TAs present in rotating shifts to answer questions and guide students through the prosections; weekly quizzes and Q&As to make sure students are staying on track and asking questions when needed; prosections structure ID videos and lab review PPTs will be provided to the students to study prior to coming to the lab so they are familiar with the material beforehand.
Responses denoting the utilization of anatomy digital resources (46.5%) during anatomy laboratory teaching emphasized the utilization of interactive software. An example of how these digital resources were used is below:
Students meet virtually on Zoom in small groups (~20) with an instructor to review dissection videos and engage in a virtual dissection using the Complete Anatomy app. At the end of each session, there is an informal quiz involving identifying structures on cadaver images and a discussion of a clinical correlate posed as a “question of the day.”
Format of student groups
The final category identified the format of student groups (i.e., small groups, large groups) utilized during laboratory sessions. The responses about student groups were divided into two categories: respondents who reported information that could be analyzed further into small and large groups (69.3%), and those who had not yet determined their format of student groups or their response was unclear or unreported (30.7%). Based on the 69.3% of respondents who provided information on their format of student groups, descriptions of small groups (76.9%) outnumbered the large group format (23.1%). Small groups were typically indicative of not in‐person anatomy sessions where small groups were used in “breakout rooms” for students to meet with each other and/or faculty to review laboratory‐related concepts. Most small group interactions were limited to virtual, not in‐person learning, but there were instances in which in‐person small groups were utilized for dissection hand‐off and updating other team members, for example:
Students will be in their anatomy lab groups (six students/group) and all lab groups are within a larger Microsoft Teams Session. Faculty move between lab groups and confirm their identification of structures on photographs within PPT. They also cover radiology with a radiologist, as appropriate.
Small group usage complemented the large group sessions. Typically, large groups were used to allow faculty to review and present the assigned laboratory topic, with small groups used for review as well as for the presentation of case studies for students to work through with their peers:
9–9:15 am: Course director provides an introduction to the laboratory in a large Zoom room; 9:15–11:00 a.m. students are preassigned to Breakout Rooms for their lab groups where they work on instructor‐created lab guides; 11:00–12 p.m. livestream dissections and/or prosections, bones, and models in the laboratory through Zoom.
Thirty‐three percent of respondents noted various methods to minimize the spread of Covid‐19, such as maintaining physical distancing and the utilization of PPE for their in‐person laboratory‐based activities. For example:
The laboratory component will be face‐to‐face instruction with faculty members. Students will wear PPE, practice social distancing, and be limited to two students per cadaveric specimen […] We will have to run the lab sessions in two separate groups either 90 minutes each or find additional times where the students can enter the labs for instruction. If lectures are held face‐to‐face, it will be following a 50% room capacity guideline, wearing PPE, and social distancing.
Gross anatomy assessment and assessment software
Examsoft (ExamSoft Worldwide, Inc., Dallas, TX), Canvas (Instructure, Inc., Salt Lake City, UT), and “others” accounted for 58% of the responses related to assessment software utilized by anatomy educators during Covid‐19 (Supporting Information File 1). Narrative data for how students were assessed in the gross anatomy laboratory between August–December, 2020 were coded within three categories: (1) assessment setting; (2) assessment format; and (3) material used for the assessment (Table 3). The number of responses coded as “unclear, unreported, or undetermined” for setting was 28 before and 43 during, for format were 30 before and 41 during, and for material were 45 before and 48 after. The remaining responses that provided data within each category are shown in Table 3. Overall, assessment in the laboratory setting significantly decreased (P < 0.0001), whereas the computer‐based setting significantly increased (P < 0.0001) during Covid‐19. There was a significant increase in the use of written assessments (P = 0.002) during Covid‐19. Use of cadaveric materials (P < 0.0001) and bones, models, and plastinates significantly decreased (P = 0.001) while the use of images significantly increased (P < 0.0001) during Covid‐19. No other findings were significant (P > 0.05; Table 3).
TABLE 3.
Comparison of assessment setting, structure, and material used before and during Covid‐19 (August–December, 2020)
| Category | Code | Covid‐19 | χ 2 | P‐value | |
|---|---|---|---|---|---|
| Before n (%) a | During n (%) a | ||||
| Setting | Laboratory | 158 (93) | 70 (41) | 33.9 | <0.0001 |
| Computer | 6 (4) | 95 (56) | 78.4 | <0.0001 | |
| None | 6 (4) | 6 (4) | 0 | 1 | |
| Totals | 170 (100) | 171 (100) | 0.002 | 0.957 | |
| Assessment | Practicals | 136 (61) | 123 (54) | 0.653 | 0.419 |
| Oral assessments | 17 (8) | 14 (6) | 0.29 | 0.59 | |
| Written assessments | 18 (8) | 42 (18) | 9.6 | 0.002 | |
| Skill and/or dissection completion | 10 (5) | 8 (3) | 0.222 | 0.637 | |
| Other assessments b | 34 (15) | 35 (15) | 0.014 | 0.904 | |
| None | 7 (3) | 7 (3) | 0 | 1 | |
| Totals | 222 (100) | 229 (100) | 0.109 | 0.742 | |
| Material | Cadaveric dissection/prosection | 155 (61) | 60 (26) | 42 | <0.0001 |
| Bones, models, plastinates | 41 (16) | 15 (6) | 12.1 | 0.001 | |
| Imaging c | 36 (14) | 127 (54) | 50.8 | <0.0001 | |
| Other d | 16 (6) | 23 (10) | 1.26 | 0.262 | |
| Not applicable | 4 (2) | 4 (2) | 0 | 1 | |
| None | 4 (2) | 5 (2) | 0.111 | 0.739 | |
| Totals | 256 (100) | 234 (100) | 0.988 | 0.32 | |
Total number of respondents (n = 186); McNemar's test, P < 0.05.
Data that were coded as unclear, undetermined, or unreported were not included in the analysis (n = 235).
Examples include assignments, integrated assessments, quizzes.
Examples of images include medical imaging, photographs of cadaveric material, textbook images.
Examples include 3D virtual models, video, and virtual reality.
Program‐specific analyses demonstrated that the use of the laboratory setting for assessment significantly decreased for allopathic medicine (before: 93% and during: 36%, P < 0.0001) and undergraduate (before: 97% and during: 33%, P = 0.001) programs. There were significant increases in the computer‐based setting for anatomy graduate (before: 0% and during: 43%, P = 0.014), allopathic medicine (before: 7% and during: 63%, P < 0.0001), osteopathic medicine (before: 0% and during: 31%, P = 0.046), undergraduate (before: 3% and during: 56%, P < 0.0001), dental (before: 0% and during: 33%, P = 0.046), and therapy (before: 0% and during: 41%, P = 0.008) programs. The use of written assessments significantly increased for allopathic medicine (before: 14% and during: 28%, P = 0.016). There were significant decreases in the use of cadaveric materials for allopathic medicine (before: 52% and during: 20%, P < 0.0001) and undergraduate (before: 69% and during: 22%, P = 0.0002) programs. In allopathic medicine only, there was a significant decrease in the use of bones, models, and plastinates (before: 20% and during: 9%, P = 0.016). The use of images significantly increased in anatomy graduate (before: 0% and during: 36%, P = 0.046), allopathic medicine (before: 25% and during: 65%, P < 0.0001), undergraduate (before: 2% and during: 53%, P < 0.0001), and dental (before: 0% and during: 44%, P = 0.046) programs. No other findings were significant (P > 0.05).
Gross anatomy digital and other teaching resources
Anatomy digital resources used for teaching before and during Covid‐19 are presented in Table 4. The utilization of digital teaching resources for anatomy increased during Covid‐19 (P < 0.0001). In‐house content created at the respondent's institution was the most frequently reported anatomy digital resource used during Covid‐19 (P > 0.05; Table 4). There were a number of anatomical teaching resources that were specifically and frequently identified including the University of Michigan's BlueLink (Alsup & Fox, 2021), Acland's Video Atlas of Anatomy (Acland, 2021), Clinically Oriented Anatomy Images (Moore et al., 2017), Complete Anatomy software (Complete Anatomy, 2021), and “other” digital resources. However, only BlueLink, Acland's Videos, and Complete Anatomy significantly increased during Covid‐19 (P < 0.05; Table 4). In addition, respondents reported a significant increase in the use of Anatomy.TV during Covid‐19 (P = 0.001), while the Thieme Dissector trended toward a significant decrease (P = 0.056). When digital resource data were categorized by group, dissection media (before: 16.6% and during: 18%, P = 0.007), interactive software (before: 19.4% and during: 25.1%, P < 0.0001), and open‐access content (before: 12.2% and during: 18.2%, P < 0.0001) significantly increased, while 2D illustrations (before: 35.4% and during: 27.1%, P = 0.666) and in‐house content (before: 16.4% and during: 14.5%, P = 0.222) decreased, but not significantly.
TABLE 4.
Anatomy digital resources utilized before and during Covid‐19 (August–December 2020)
| Resources | Before Covid‐19 n (%) | During Covid‐19 n (%) | χ 2 | P‐value |
|---|---|---|---|---|
| In‐house content created at your institution | 69 (15) | 85 (13) | 1.66 | 0.197 |
| University of Michigan BlueLink (Alsup & Fox, 2021) | 28 (6) | 69 (11) | 17.30 | <0.0001 |
| Acland's Video Atlas of Anatomy (Acland, 2021) | 33 (7) | 58 (9) | 6.90 | 0.009 |
| Clinically Oriented Anatomy Images (Moore et al., 2017) | 48 (10) | 52 (8) | 0.16 | 0.689 |
| Other | 33 (7) | 50 (8) | 3.48 | 0.062 |
| Complete Anatomy (Complete Anatomy, 2021) | 27 (6) | 48 (7) | 5.90 | 0.0153 |
| Netter Presenter Atlas of Human Anatomy (Netter, 2020) | 40 (9) | 41 (6) | 0.01 | 0.912 |
| Gray's Anatomy Images (Drake et al., 2020) | 28 (6) | 34 (5) | 0.58 | 0.446 |
| Anatomy: A Photographic Atlas (Rohen et al., 2015) | 26 (6) | 34 (5) | 1.10 | 0.302 |
| A&P Revealed (Schneider et al., 2021) | 16 (3) | 25 (4) | 2.00 | 0.160 |
| Essential Clinical Anatomy Images (Moore et al., 2014) | 20 (4) | 23 (3) | 0.21 | 0.647 |
| Grant's Dissector Videos (Detton, 2016) | 19 (4) | 21 (3) | 0.10 | 0.752 |
| Visible Body (Visible Body, 2021) | 10 (2) | 20 (3) | 3.33 | 0.068 |
| Anatomy.TV (Anatomy.TV, 2021) | 1 (0) | 14 (2) | 11.30 | 0.0008 |
| University of Wisconsin School of Medicine and Public Health Dissection Videos (University of Wisconsin, 2021) | 10 (2) | 14 (2) | 0.67 | 0.414 |
| University of British Columbia Anatomy Videos (Krebs et al., 2020) | 9 (2) | 13 (2) | 0.72 | 0.394 |
| VH Dissector for Medical Education (VH Dissector, 2021) | 7 (2) | 13 (2) | 1.80 | 0.18 |
| Thieme MyCourse/Dissector (Gould et al., 2015) | 20 (4) | 10 (2) | 3.33 | 0.068 |
| Dartmouth Geisel School of Medicine Anatomy Resources (Lyons et al., 2021) | 3 (1) | 7 (1) | 1.60 | 0.206 |
| The BioDigital Human (The Biodigital Human, 2021) | 2 (0) | 6 (1) | 2.00 | 0.157 |
| Kenhub Human Anatomy (Kenhub, 2021) | 4 (1) | 5 (1) | 0.11 | 0.739 |
| Stanford Medicine Bassett Collection of Stereoscopic Images of Human Anatomy (Bassett et al., 2021) | 1 (0) | 4 (1) | 1.80 | 0.18 |
| VIVED Anatomy Videos (Vived Anatomy, 2019) | 3 (1) | 4 (1) | 0.14 | 0.705 |
| 3D Organon (3D Organon, 2021) | 2 (0) | 3 (1) | 0.20 | 0.655 |
| University of Arkansas for Medical Sciences Anatomy Resources (UAMS, 2009) | 3 (1) | 3 (0) | 0.00 | 1 |
| Autopsy.online (Margolis, 2021) | 1 (0) | 2 (0) | 0.33 | 0.564 |
| Netter3D Anatomy powered by CyberAnatomy 3D (Netter3D, 2018) | 3 (1) | 2 (0) | 0.20 | 0.655 |
| Georgetown University Medical Center Videos (Georgetown University, 2021) | 2 (0) | 2 (0) | 0.00 | 1 |
| OsiriX Dicom Viewer (Rosset & Heuberger, 2021) | 1 (0) | 2 (0) | 0.33 | 0.563 |
| AnatomyTOOL (Anatomy Tool, 2021) | 0 (0) | 1 (0) | 1.00 | 0.317 |
| BodyViz 3D Anatomy (Bodyviz, 2020) | 2 (0) | 1 (0) | 0.33 | 0.564 |
| A.D.A.M. Interactive Anatomy (A.D.A.M., 2021) | 1 (0) | 0 (0) | 1.00 | 0.317 |
| TOTAL | 472 (100) | 666 (100) | 33.10 | P < 0.0001 |
Total number of respondents n = 207, with several individuals indicating ≥1 resource. McNemer's test, P < 0.05.
Camera and camera‐related accessories were the most commonly reported (30%) non‐anatomy tools that were purchased by respondents to support teaching during Covid‐19, while less than 10% of respondents reported the remaining choices (Supporting Information File 2). Zoom (Zoom Voice Communications Inc., San Jose, CA) was the dominant video conferencing platform used by the majority of respondents (55%) followed by Blackboard Collaborate (Blackboard Inc., Washington, DC) (11%), whereas the remaining choices were used by 10% or less of the respondents (Supporting Information File 3).
DISCUSSION
Together with the findings from May to August 2020 by Harmon et al. (2021), and the current study of August–December, 2020, this body of work is the first to provide a comprehensive picture, using inferential statistics, of the differences in gross anatomy teaching before and during Covid‐19. The collective data provide insight into laboratory modalities, lecture and laboratory delivery format, laboratory assessment, anatomy digital resource utilization, and communication software usage.
The current study assessed differences between programs, integrated and stand‐alone courses, institutional locations, as well as private and public US institutions, with respect to gross anatomy laboratory and lecture teaching. The predominant changes occurred in the setting of laboratory instruction and in the utilization of laboratory modalities before and during Covid‐19. The anatomy laboratory delivery format shifted significantly from in‐person instruction to not in‐person (i.e., remote). Consequently, cadaver‐based modalities decreased significantly while the use of “other” materials increased significantly.
Laboratory teaching
When the data were assessed collectively, there was a significant decrease in the use of cadaver‐based and plastic modalities, and an increase in “other” modalities during Covid‐19 compared to before. Laboratory sessions that ran between August andDecember, 2020 with decreased cadaver usage corroborated findings from the literature that reported on the early months of the pandemic at individual institutions (Cuschieri & Calleja Agius, 2020; Muñoz‐Leija et al., 2020; Naidoo et al., 2020; Herr & Nelson, 2021) and in broader geographical regions (Brasset et al., 2020; Longhurst et al., 2020; Pather et al., 2020; Cheng et al., 2021; Harmon et al., 2021). However, the proportion of programs using cadaveric modalities between August–December (50.3 ± 43.0%) was notably larger than the proportions reported in May–August (34.0 ± 42.6%; Harmon et al., 2021). Indeed, 65% of respondents that provided insight into their laboratory delivery modality indicated that at least a portion of it was in‐person. One possible explanation is the Environmental Protection Agency's recommendation (EPA, 2020) to utilize educational spaces with high ventilation, and anatomy laboratories have consistently high ventilation compared to other spaces on campus (OSHA, 1990; Trelease, 2006). Additionally, anatomy educators in countries that provided Covid‐19 vaccinations for students in the latter half of 2020 (Barash et al., 2021) may have felt safe to resume in‐person laboratories. Anatomy educators may also have been eager to return to in‐person cadaver‐based laboratories due to their long‐standing beliefs that learning is facilitated by hands‐on experiences, and that working with body donors fosters humanistic personal growth (Harmon et al., 2021) and the formation of professional identity (Barash et al., 2021). Concurrently, with the increase of cadaveric modalities during August–December compared to during May–August (Harmon et al., 2021), there was a decrease in the utilization of “other” modalities from 50.5% to 33.7%, but the use of plastic modalities was consistent (May–August: 15.1% vs. August–December: 15.0%).
Before Covid‐19, the majority of health professions programs (allopathic medicine, graduate health, physician assistant, osteopathic medicine, and therapy), anatomy graduate, and veterinary medicine allocated over 80% of their laboratory teaching time to cadaver‐based instruction, while undergraduate and nursing programs allocated less than 50%. The lower utilization of cadaver‐based instruction in undergraduate and nursing programs corresponds with their higher proportion allocated to plastic (at least 33%) and “other” (at least 13%) modality usage compared to other programs before Covid‐19. A possible explanation for this is that undergraduate and nursing programs may not be able to support the associated costs of offering cadaver‐based instruction due to their relatively high number of enrolled students (Jonas Philanthropies, 2015), compared to programs like allopathic medicine (Kalter, 2019). However, undergraduate and nursing programs may choose to utilize plastic and “other” modalities due to lower costs and long‐term continued use. This disparity of cadaveric usage for undergraduate and nursing programs remained during Covid‐19. The programs that experienced the smallest decrease in allocated time to cadaver‐based modalities were anatomy graduate, dental, physician assistant, nursing, and graduate health. Most of these programs typically have a lower enrollment (i.e., less than 100 students on average) (Brokaw & O’Loughlin, 2015; Kolomitro et al., 2018; PAEA, 2019; CODA, 2020) than medical schools and undergraduate programs as a whole (Schutte, 2016; Attardi et al., 2018; AAMC, 2020), allowing for proper physical distancing, which may explain why the decrease in cadaver‐based modalities was not as extreme.
In addition to program‐specific comparisons, laboratory teaching modality was used to compare integrated versus stand‐alone anatomy courses, US versus international institutions, US private versus public institutions, and allopathic medicine programs in the US by region. Before Covid‐19, programs with stand‐alone gross anatomy courses spent a significantly greater percentage of their laboratory time utilizing cadaveric materials compared to integrated courses. An explanation for this finding is that stand‐alone gross anatomy courses typically have more hours of instruction compared to integrated (Brooks et al., 2015; McBride & Drake, 2018; Rockarts et al., 2020). During Covid‐19, regardless of the type of anatomy course, cadaver usage decreased while the usage of “other” modalities significantly increased. Only integrated courses saw a significant decrease in plastic usage during Covid‐19.
Before Covid‐19, US institutions allocated a significantly greater percentage of their laboratory time to cadaveric materials compared to international institutions. Conversely, international institutions allocated a significantly greater amount of time to plastic and “other” teaching modalities. During Covid‐19, regardless of institutional location, cadaver usage decreased while usage of “other” modalities significantly increased. However, during Covid‐19, the United States continued to allocate a significantly greater amount of time to cadaveric materials and international institutions continued to allocate a significantly greater amount of time to plastic and “other” modalities. One reason why international institutions may devote less time to cadaver‐based modalities could be due to global variations on the availability and sourcing of human body donors (Habicht et al., 2018).
In the United States, before Covid‐19 there was no difference in the percentage of laboratory teaching time for cadaver‐based, plastic, and “other” modalities between private and public institutions. During Covid‐19, regardless of institution type, cadaver usage decreased while usage of “other” modalities significantly increased for both the current study and as presented in Harmon et al. (2021). However, during Covid‐19, private institutions allocated a significantly greater percentage of their laboratory time to cadaveric modalities compared to public institutions, but there were no significant differences in the utilization of plastic and “other” modalities. As noted in Harmon et al. (2021), and confirmed by the larger sample size in the current study, private institutions typically have more flexibility in educational decisions compared to public institutions as they are typically not government funded. In the future, this difference could continue due to the high cost associated with operating a human dissection laboratory (McLachlan et al., 2004; McMenamin et al., 2014; Simpson, 2014), which may be more feasible for private institutions to fund.
As stated previously, allopathic medical programs significantly decreased their percentage of laboratory teaching time allocated for cadaver‐based modalities while increasing their time for “other” modalities. Further examination into the US geographical regions revealed that this pattern of decreased cadaveric use and increased use of “others” was consistent within the Northeastern, Central, and Southern groups, but was not significant for the Western region. Regardless of the changes due to Covid‐19, there were no significant differences in the allocation of time for the different laboratory modalities between regions before or during Covid‐19. An explanation for the lack of significant changes to laboratory modalities in the Western region was the relatively small number of respondents in this region compared to the other three regions.
Lecture teaching
With respect to lecture‐based teaching, in‐person delivery significantly decreased and not in‐person delivery significantly increased during August–December, 2020 compared to before Covid‐19. These results were consistent with reports from anatomy educators early during the pandemic individual institutions (Alkhowailed et al., 2020; Cuschieri & Calleja Agius, 2020; Naidoo et al., 2020; Herr & Nelson, 2021) and in broader geographical regions (Brasset et al., 2020; Longhurst et al., 2020; Pather et al., 2020; Cheng et al., 2021; Harmon et al., 2021). As was reported by Harmon et al. (2021) specifically, this was likely due to the international and US stay‐at‐home orders and physical distancing requirements. Globally, country‐wide closures peaked at 163 in early May and were reduced to nine closures by late December, 2020 (UNESCO, 2020). This trend was consistent in the US, with the vast majority of states lifting their shelter‐in‐place or stay‐at‐home orders before or during May–August, 2020 (Finra, 2020). Regardless of the stay‐at‐home orders, the Centers for Disease Control and Prevention classified in‐person educational activities, where students and faculty interact freely, as a component of the highest risk category (CDC, 2021). As a result, anatomy educators have continued to use the not in‐person lecture format; however, there was a notable increase in the percentage of respondents in the current study who utilized in‐person lectures (24%), compared to the May–August respondents (8%) (Harmon et al., 2021). Gross anatomy educators were uniquely prepared to deliver not in‐person lectures due to a well‐documented history of using this format before the pandemic, both synchronously (Attardi & Rogers, 2015) and asynchronously (Nieder & Nagy, 2002; Bacro et al., 2010, 2013; Nieder & Borges, 2012; Trelease, 2015; Farkas et al., 2016; Zureick et al., 2018)
Gross anatomy laboratory assessment
Before Covid‐19, gross anatomy assessment typically took place in‐person in a laboratory setting. The practical examination (i.e., “bellringer”) was the predominant testing format with cadavers representing the majority of testing materials and a small proportion allotted to bones, models, plastinates, and images. During Covid‐19, institutions transitioned their laboratory assessments to a computer‐based setting, and because of that, images represented the majority of testing materials used. This pattern aligns with the decrease in the time allotted to cadaver‐based modalities during Covid‐19 presented in the current report. It is consistent with the assessment adaptations anatomy educators made during the early pandemic (Harmon et al., 2021), with most of the respondents offering practical examinations (May–August: 62% vs. August–December: 54%) in a computer‐based setting (May–August: 61% vs. August–December: 56%) using images as testing materials (May–August: 51% vs. August–December: 54%). The findings of the current study also align with assessment adaptations observed in other studies of anatomy education during the early pandemic (Longhurst et al., 2020; Cheng et al, 2021; Herr & Nelson, 2021). In addition, there was a significant increase in the use of anatomy laboratory questions incorporated into a program's typical written examinations (i.e., term test or end‐of‐block examination). However, this finding was largely driven by allopathic medical programs as all other programs did not have a significant increase in written assessments.
Gross anatomy digital and other resources
The respondents from gross anatomy programs between August and December, 2020 indicated an increased utilization of gross anatomy digital resources during Covid‐19. Adoption of gross anatomy digital resources both early in the pandemic (May–August, 2020) and later in the pandemic (August–December, 2020) followed a similar pattern. The University of Michigan BlueLink, a free resource, and Complete Anatomy, a commercial resource, had the largest increase of adoption throughout the current study and Harmon et al. (2021). The use of Complete Anatomy was noted in other published studies of gross anatomy education during Covid‐19 (Brassett et al., 2020; Longhurst et al., 2020; Pather et al., 2020). In addition to the University of Michigan BlueLink and Complete Anatomy, Acland's Video Atlas of Anatomy and Anatomy.TV also saw a significant increase in adoption in the current study. The additional significant increase of these resources may be due to the longer planning period afforded to gross anatomy educators teaching during the August–December compared to May–August, 2020.
The sustained increase in digital resource usage for gross anatomy education during Covid‐19 was particularly pronounced for interactive software, open‐access resources, and dissection media that allowed educators to mimic features of a dissection laboratory. Despite the significant increase of commercial anatomy digital resources, the most commonly selected digital resource was in‐house content, both before and during Covid‐19, used by nearly half of the respondents. However, the comparison between before and during Covid‐19 was not significant due to the high pre‐pandemic usage of in‐house content. This may be due to the fact that utilizing in‐house content that was previously created is considerably less expensive than purchasing new digital resources. Anatomists have continuously developed digital resources independently, even prior to the pandemic (Attardi & Rogers, 2015; Yammine & Violato, 2015; Swinnerton et al., 2017; Leung et al., 2020). For example, a member of the AAA posted on Anatomy Connected a curated collection of 46 open‐access digital resources and hosted the list freely online for gross anatomy educators to utilize, most of which were created in‐house (Flaherty, 2021). It is important for digital resources to be readily available in the event that anatomy education faces future lockdowns (Das & Al Mushaiqri, 2021).
Regardless of the specific resources used, there was an overall significant increase in the adoption of digital resources to teach gross anatomy between August and December, 2020 compared to before Covid‐19. This rapid shift in adopting both commercial and free digital resources are likely to drive the future of innovation in anatomy education. It remains unknown if the current findings are transient Covid‐19‐related changes or if they will persist long‐term. A number of publications have recently discussed the concern of the broad transition to digital resource teaching for gross anatomy instruction during Covid‐19 and how this could lead to a continued decrease of cadaveric utilization beyond the pandemic (Franchi, 2020; Pearson, 2020; Jones, 2021; Ross et al., 2021) in an effort to reduce institutional costs (Evans & Pawlina, 2021).
Communication software
Zoom was the dominant video conferencing software used by 55% of respondents for tele‐education, which is consistent with the findings of Harmon et al. (2021) during the May–August, 2020 period (57%). This software dominated the market share for video conferencing in the higher education sector (Menard, 2020) as well as across sectors (Datanyze, 2021) during the pandemic. Interestingly, Zoom is not specific to the education sector compared to products like Blackboard Collaborate, which had a much lower adoption rate in this study. Similar to the changes with digital resource adoption and laboratory content changes, it remains to be seen how didactic instruction will be conducted after the pandemic. Future studies will need to examine whether the utilization of video conferencing as a predominant medium for lecture instruction will continue or if institutions will transition back fully to in‐person instruction. Previous research has indicated that screen time is associated with less happiness and could contribute to the declining mental health experienced by the current generation of students (Twenge, 2017). Therefore, it will be important to assess the mental health of students based on their concentration of screen time in their curriculum.
The future of gross anatomy education
Together with Harmon et al (2021), this body of research has demonstrated the dramatic changes undertaken by gross anatomy educators in response to Covid‐19 during May–December, 2020. This paradigm‐shifting pedagogy in gross anatomy and across higher education (García‐Morales et al., 2021; Pokhrel & Chhetri, 2021) during 2020 forced educators in gross anatomy (Evans et al., 2020) as well as other basic medical science disciplines (Bzowyckyj et al., 2021; Seitz & Rediske, 2021; Zhang et al., 2021) to reassess the best ways to deliver higher education. It is unknown whether the changes will become a common practice after Covid‐19 is better controlled or vanquished. However, numerous sources suggest that some of the new delivery formats introduced in 2020 offer an improved educational experience for students and educators alike. For example, broadening the population of guest speakers available to students (Schapiro, 2021), flexible work arrangements for staff (Schapiro, 2021), improving accessibility to resources and experiences for students with disabilities and low‐income status (Larson, 2021), and the development of new online courses (Nworie, 2021). It is unknown what the future holds for gross anatomy education, but what is certain is that anatomy education will likely change as a result of Covid‐19. Anatomy educators were required to become experts in multiple new technologies (e.g., video communication software and gross anatomy digital resources) in a short period of time (Smith & Pawlina, 2021). This forced adoption of new technologies will certainly change the perspective as to what is “possible” for teaching gross anatomy in higher education moving forward.
Limitations of the study
This study is not without limitations. Participation in the survey was voluntary, introducing self‐selection bias to the sample of respondents. For example, while international participation was sought, the majority of the sample population was from the United States. Second, several programs had small samples which may have created the opportunity of a type 2 error; however, the study overall had a robust sample of 191 respondents. Programs with small samples sizes were combined with other groups where possible. Consequently, the groups were categorized differently from the groups in Harmon et al. (2021), which made direct comparisons difficult between May–August and August–December, 2020. Third, interpretation of the narrative data introduced researcher bias; however, this was mitigated by the use of at least two independent coders and multiple reviews, which is known to improve the reliability of the analysis (Mays & Pope, 1995). Last, while descriptive accounts of anatomy curriculum strategies were presented, student outcomes were not included. At the time of participant recruitment, outcomes data were not available because the courses had not yet concluded.
Future directions
Although the pandemic challenged every facet of gross anatomy education, it has been described as a “positive disruption” that should inspire anatomy educators to evaluate which newly adopted pedagogies would be beneficial for students after Covid‐19 (Evans & Pawlina, 2021). In the future, the authors plan to compare student outcomes before, during, and after Covid‐19. It will also be of interest for researchers to study the mental well‐being of students enrolled in gross anatomy curricula as a result of the pandemic, due to the increased social isolation, increased screen time, and fears of contracting Covid‐19. In addition, the authors plan to track the state of anatomy curricula (e.g., laboratory modalities, delivery format, assessment) after Covid‐19 to determine which educational practices for anatomy will revert back to before Covid‐19, and which Covid‐19 adaptations will persist and continue to evolve.
CONCLUSION
This is the first study of its magnitude to provide granular, location‐ and program‐specific details about gross anatomy curricula, both before and during Covid‐19. The data provided inferential evidence for how anatomy educators transitioned their curricula during August–December, 2020 as a result of Covid‐19. Lectures continued to be predominantly not in‐person, while nearly two‐thirds of respondents had at least some form of in‐person laboratory activities. Regardless, most academic programs saw a decrease in the use of cadaveric materials from before Covid‐19 to during August–December, while “other” laboratory modalities increased, with this effect being most pronounced in allopathic medicine and undergraduate gross anatomy programs. Laboratory assessments shifted from a traditional in‐person environment to computer‐based, necessitating the use of images over cadaveric materials, bones, models, and plastinated specimens. However, the practical (“bell‐ringer”) examination persisted as the dominant laboratory assessment format from before Covid‐19, through the May–August period (Harmon et al., 2021), and into the August–December period. In addition, the use of gross anatomy digital resources significantly increased during Covid‐19, with in‐house content remaining the most commonly indicated. This study demonstrates how gross anatomy educators pursued several approaches to maintain educational continuity past the early stages of the Covid‐19 pandemic. These findings provide gross anatomy educators with data on innovative approaches that can be used in future gross anatomy curricula.
CONFLICTS OF INTEREST
Dr. Derek J. Harmon serves on an Advisory Board for Elsevier. All the other authors attest that they have no financial or other conflicts of interest.
Supporting information
Supplementary Material
Supplementary Material
Supplementary Material
ACKNOWLEDGMENTS
The authors would like to thank all the individuals who have completed the survey. They are also grateful to the AAA and the staff at the AAA for supporting the dissemination of both the survey and its data. The authors are grateful for critical survey feedback and support by Joan T. Richtsmeier, PhD, as well as the technical assistance provided by Joseph R. Macher in analyzing the narrative data and by Audrey Bell in formatting the figures.
Biographies
Stefanie M. Attardi, Ph.D., is an assistant professor in the Department of Foundational Medical Studies at Oakland University William Beaumont School of Medicine in Rochester, Michigan. She teaches histology and gross anatomy to medical students. Her research focuses on online education and curricular integration involving the anatomical sciences.
Derek J. Harmon, Ph.D., is an associate professor of anatomy in the Department of Anatomy at the University of California, San Francisco in San Francisco, California. He teaches medical students, residents, fellows, and clinicians. His research interests are in technology‐based educational innovations and developing low‐cost, high‐quality clinical simulation models.
Malli Barremkala, M.B.B.S., is an associate professor in the Department of Foundational Medical Studies at Oakland University William Beaumont School of Medicine in Rochester, Michigan. He teaches gross anatomy and embryology to medical students. He has a strong interest in developing resources to enhance anatomy learning and medical instructional simulation.
Danielle C. Bentley, Ph.D., is an assistant professor, teaching stream, in the Division of Anatomy, Faculty of Medicine, University of Toronto in Toronto, Canada. She teaches gross anatomy and embryology to undergraduate, graduate, and medical students. She has an interest in research design and is currently investigating student assessments.
Kirsten M. Brown, Ph.D., M.A., is an associate professor in the Department of Anatomy & Cell Biology at the George Washington University School of Medicine & Health Sciences in Washington, D.C. She teaches anatomy to a variety of student populations. Her research focuses on various aspects of anatomy education.
Jennifer F. Dennis, Ph.D., is an associate professor of anatomy in the Department of Anatomy at Kansas City University College of Osteopathic Medicine in Joplin, Missouri. She teaches embryology, histology, and neuroanatomy to medical students. Her research interests include anatomy education and assessment outcomes.
Haviva M. Goldman, Ph.D., is a professor in the Department of Neurobiology and Anatomy at Drexel University College of Medicine. She is Vice Chair for Medical Education and teaches gross anatomy and microanatomy to medical students. Her research interests include anatomical sciences integration, e‐learning module development, and bone biology.
Kelly M. Harrell, Ph.D., M.P.T., is an associate professor in the Department of Anatomy and Neurobiology at Virginia Commonwealth University School of Medicine. She teaches gross anatomy, embryology, and neuroscience across multiple programs. Her research interest is in medical education and utility of technology in the classroom and laboratory.
Barbie A. Klein, Ph.D., is an assistant professor in the Department of Anatomy at the University of California, San Francisco in San Francisco, California. She teaches health professional and graduate‐level learners. Her research focuses on integrating technology and interprofessional collaboration in anatomy education.
Christopher J. Ramnanan, Ph.D., is an associate professor in the Division of Clinical and Functional Anatomy, Department of Innovation of Medical Education at the University of Ottawa in Ottawa, Canada. He teaches anatomy to medical students. His research interests include optimizing anatomy education in the context of student‐centered approaches.
Gary J. Farkas, Ph.D., is a postdoctoral associate in the Department of Physical Medicine and Rehabilitation at the University of Miami in Miami, Florida. His research focuses on obesity‐induced comorbidities after spinal cord injury and anatomy education. He is the recipient of the 2020–2021 AAA Postdoctoral Fellowship.
Attardi SM, Harmon DJ, Barremkala M, Bentley DC, Brown KM, Dennis JF, Goldman HM, Harrell KM, Klein BA, Ramnanan CJ, Farkas GJ. 2022. An analysis of anatomy education before and during Covid‐19: August–December 2020. Anat Sci Educ 15:5–26. 10.1002/ase.2152
Drs Stefanie M. Attardi and Derek J. Harmon contributed equally to the writing of this manuscript.
REFERENCES
- 3D Organon . 2021. 3D Organon: Virtual Reality Anatomy Atlas. Metis Media Pty Ltd., Gold Coast, Queensland, Australia. URL: https://www.3dorganon.com/ [accessed 24 March 2021]. [Google Scholar]
- AACN . 2020. American Association of Colleges of Nursing. Considerations for COVID‐19 preparedness and response in U.S. schools of nursing. American Association of Colleges of Nursing, Washington, DC. URL: https://www.aacnnursing.org/News‐Information/COVID‐19/AACN‐Recommendations [accessed 16 March 2021]. [Google Scholar]
- AAMC . 2020. Association of American Medical Colleges. U.S. medical school applications and matriculants by school, state of legal residence, and sex, 2020‐2021. Association of American Medical Colleges, Washington, DC. URL: https://www.aamc.org/data‐reports/students‐residents/interactive‐data/2020‐facts‐applicants‐and‐matriculants‐data [accessed 22 February 2021]. [Google Scholar]
- AAMC. Association of American Medical Colleges . 2021. State by state graduate medical education data. Association of American Medical Colleges, Washington, DC. URL: https://www.aamc.org/advocacy‐policy/state‐state‐graduate‐medical‐education‐data [accessed 18 March 2021]. [Google Scholar]
- Acland RD. 2021. Acland's Video Atlas of Human Anatomy® . Wolters Kluwer Health Inc./Lippincott, Williams & Wilkins, Baltimore, MD. URL: http://aclandanatomy.com/ [accessed 24 March 2021]. [Google Scholar]
- A.D.A.M . 2021. A.D.A.M. Interactive Anatomy. EBIX Inc., Atlanta, GA. URL: adameducation.com/aiaonline [accessed 24 March 2021]. [Google Scholar]
- Alboraie M, Piscoya A, Tran QT, Mendelsohn RB, Butt AS, Lenz L, Alavinejad P, Emara MH, Samlani Z, Altonbary A, Monged A, Lemmers A, Sudovykh I, Ho DQD, Ghazanfar S, Kamau E, Iqbal S, Tan DMY, Liao W‐C, Vignesh S. 2020. The global impact of COVID‐19 on gastrointestinal endoscopy units: An international survey of endoscopists. Arab J Gastroenterol 21:156–161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alkhowailed MS, Rasheed Z, Shariq A, Elzainy A, El Sadik A, Alkhamiss A, Alsolai AM, Alduraibi SK, Alduraibi A, Alamro A, Alhomaidan HT, Al Abdulmonem W. 2020. Digitalization plan in medical education during COVID‐19 lockdown. Inform Med Unlocked 20:100432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allen M, Omori K, Cole AW, Burrell N. 2019. Distance learning and student satisfaction. In: Moore MG, Diehl WC (Editors). Handbook of Distance Education. 4th Ed. New York, NY: Routledge. p 122–132. [Google Scholar]
- Alsup BK, Fox G. 2021. BlueLink Images. University of Michigan Medical School, Ann Arbor, MI. URL: https://sites.google.com/a/umich.edu/bluelink/resources/bluelink [accessed 24 March 2021]. [Google Scholar]
- Anatomy Connected . 2021. American Association for Anatomy, Rockville, MD. URL: https://anatomyconnected.anatomy.org/home [accessed 18 March 2021]. [Google Scholar]
- AnatomyTOOL . 2021. Anatomy TOOL (Topic Oriented Open Learning platform). Leiden University Medical Center, Leiden, The Netherlands; Maastricht University, Maastricht, The Netherlands. URL: https://anatomytool.org/ [accessed 24 March 2021]. [Google Scholar]
- Anatomy.TV . 2021. Anatomy.TV Interactive Anatomy. Primal Pictures Ltd., London, UK. URL: www.anatomy.tv/ [accessed 22 September 2020]. [Google Scholar]
- Attardi SM, Barbeau ML, Rogers KA. 2018. Improving online interactions: Lessons from an online anatomy course with a laboratory for undergraduate students. Anat Sci Educ 11:592–604. [DOI] [PubMed] [Google Scholar]
- Attardi SM, Rogers KA. 2015. Design and implementation of an online systemic human anatomy course with laboratory. Anat Sci Educ 8:53–62. [DOI] [PubMed] [Google Scholar]
- BACA . 2021. British Association of Clinical Anatomists. Guidance for institutions/anatomists when utilising cadaveric material for online teaching sessions. British Association of Clinical Anatomists, Swansea, UK. URL: https://drive.google.com/file/d/133eX64YGTLfJjik8Bo9v‐ow0J_vxZe0Z/view [accessed 12 March 2021]. [Google Scholar]
- Bacro TR, Gebregziabher M, Ariail J. 2013. Lecture recording system in anatomy: Possible benefit to auditory learners. Anat Sci Educ 6:376–384. [DOI] [PubMed] [Google Scholar]
- Bacro TR, Gebregziabher M, Fitzharris TP. 2010. Evaluation of a lecture recording system in a medical curriculum. Anat Sci Educ 3:300–308. [DOI] [PubMed] [Google Scholar]
- Barash A, Dickman N, Karasik D. 2021. Educating future doctors in Covid‐19 times: Anatomists lead the way! Anat Sci Educ 14:426–427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bassett DL, Gruber WA, O’Neill H, Ogren R, Segal L. 2021. Bassett Collection of Stereoscopic Images of Human Anatomy. Stanford School of Medicine, Stanford, CA. URL: http://lane.stanford.edu/biomed‐resources/bassett/index.html [accessed 24 March 2021]. [Google Scholar]
- Biodigital . 2021. The Biodigital Human powering the world's understanding of the human body. Biodigital, New York, NY. URL: https://www.biodigital.com/ [accessed 24 March 2021]. [Google Scholar]
- Brooks WS, Woodley KT, Jackson JR, Hoesley CJ. 2015. Integration of gross anatomy in an organ system‐based medical curriculum: Strategies and challenges. Anat Sci Educ 8:266–274. [DOI] [PubMed] [Google Scholar]
- BodyViz . 2020. BodyViz 6.0: 3D Anatomy Dissection Labs for Online/Remote Learning Environments. Visual Medical Solutions, LLC., Clive, IA. URL: https://www.bodyviz.com/ [accessed 24 March 2021]. [Google Scholar]
- Bond G, Franchi T. 2021. Resuming cadaver dissection during a pandemic. Med Educ Online 26:1842661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brassett C, Cosker T, Davies DC, Dockery P, Gillingwater TH, Lee TC, Milz S, Parson SH, Quondamatteo F, Wilkinson T. 2020. COVID‐19 and anatomy: Stimulus and initial response. J Anat 237:393–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brokaw JJ, O'Loughlin VD. 2015. Implementation of an education‐focused PhD program in anatomy and cell biology at Indiana University: Lessons learned and future challenges. Anat Sci Educ 8:258–265. [DOI] [PubMed] [Google Scholar]
- Burgess A, van Diggele C, Mellis C. 2018. Mentorship in the health professions: A review. Clin Teach 15:197–202. [DOI] [PubMed] [Google Scholar]
- Bzowyckyj AS, Blake E, Crabtree B, Edwards KL, Franks AM, Gonyeau M, Rospond R, Turner K, Gandhi N, Ragucci KR. 2021. Advancing pharmacy education and workforce development amid the Covid‐19 pandemic: Report of the 2020‐2021 AACP Academic Affairs Committee. Am J of Pharm Educ 85:8716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cahalane AM, Cui J, Sheridan RM, Thabet A, Sutphin PD, Palmer WE, Hirsch JA, Kalva SP. 2020. Changes in interventional radiology practice in a tertiary academic center in the United States during the coronavirus disease 2019 (COVID‐19) pandemic. J Am Coll Radiol 17:873–877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CDC . 2021. Centers for Disease Control and Prevention. Operating schools during COVID‐19: CDC's considerations. Centers for Disease Control and Prevention, Atlanta, GA. URL: https://www.cdc.gov/coronavirus/2019‐ncov/community/schools‐childcare/schools.html [accessed 24 March 2021]. [Google Scholar]
- Cheng X, Chan LK, Pan SQ, Cai H, Li YQ, Yang X. 2021. Gross anatomy education in China during the Covid‐19 pandemic: A national survey. Anat Sci Educ 14:8–18. [DOI] [PubMed] [Google Scholar]
- CMS . 2020. Centers for Medicare and Medicaid Services. CMS Adult Elective Surgery and Procedures Recommendations: Limit all Non‐Essential Planned Surgeries and Procedures, Including Dental, until Further Notice. 1st Ed. Baltimore, MD: Centers for Medicare and Medicaid Services. 2 p. URL: https://www.cms.gov/files/document/covid‐elective‐surgery‐recommendations.pdf [accessed 16 March 2021]. [Google Scholar]
- CODA . 2020. Commission on Dental Accreditation. Survey of dental education 2019‐20. Commission on Dental Accreditation, Chicago, IL. URL: https://www.ada.org/en/coda/find‐a‐program/program‐surveys [accessed 23 February 2021]. [Google Scholar]
- Complete Anatomy . 2021. The world's most advanced 3D anatomy platform. 3D4Medical. Elsevier, Dublin, Ireland. URL: https://3d4medical.com/ [accessed 22 September 2020]. [Google Scholar]
- Cuschieri S, Calleja Agius J. 2020. Spotlight on the shift to remote anatomical teaching during Covid‐19 pandemic: Perspectives and experiences from the University of Malta. Anat Sci Educ 13:671–679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Das S, Al Mushaiqri M. 2021. Anatomy online teaching during Covid‐19 pandemic: The need for responsive anatomy learning ecosystem. Anat Sci Educ 14:428–429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Datanyze . 2021. Market share, web conferencing, Zoom. Datanyze, Durham, NC. URL: https://www.datanyze.com/market‐share/web‐conferencing‐‐52/zoom‐market‐share [accessed 30 March 2021]. [Google Scholar]
- Detton A. 2016. Grant's Dissector Videos for Grant's Dissector. 16th Ed. Philadelphia, PA: Wolters Kluwer, Lippincott, Williams & Wilkins. 323 p. [Google Scholar]
- DHS . 2013. United States Department of Homeland Security. What is a public university? What is a private university?. United States Department of Homeland Security, Washington, DC. URL: https://studyinthestates.dhs.gov/2013/01/what‐public‐university‐what‐private‐university [accessed 18 March 2021]. [Google Scholar]
- Drake RL, McBride JM, Lachman N, Pawlina W. 2009. Medical education in the anatomical sciences: The winds of change continue to blow. Anat Sci Educ 2:253–259. [DOI] [PubMed] [Google Scholar]
- Drake R, Vogl AW, Mitchell A, Tibbitts R, Richardson P. 2020. Gray's Atlas of Anatomy. 3rd Ed. Philadelphia, PA: Elsevier. 648 p. [Google Scholar]
- EPA . 2020. United States Environmental Protection Agency. Ventilation and Coronavirus (COVID‐19). United States Environmental Protection Agency, Washington, DC. URL: https://www.epa.gov/coronavirus/ventilation‐and‐coronavirus‐covid‐19 [accessed 22 March 2021]. [Google Scholar]
- Evans DJ, Bay BH, Wilson TD, Smith CF, Lachman N, Pawlina W. 2020. Going virtual to support anatomy education: A STOPGAP in the midst of the Covid‐19 pandemic. Anat Sci Educ 13:279–283. [DOI] [PubMed] [Google Scholar]
- Evans DJ, Pawlina W. 2021. Effects of Covid‐19‐the need to assess the real value of anatomy education. Anat Sci Educ 14:129–131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farkas GJ, Mazurek E, Marone JR. 2016. Learning style versus time spent studying and career choice: Which is associated with success in a combined undergraduate anatomy and physiology course? Anat Sci Educ 9:121–131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- FINRA . 2020. Financial Industry Regulatory Authority. State “shelter‐in‐place” and “stay‐at‐home” orders. Financial Industry Regulatory Authority, Washington, DC. URL: https://www.finra.org/rules‐guidance/key‐topics/covid‐19/shelter‐in‐place [accessed 10 February 2021]. [Google Scholar]
- Flaherty K. 2021. Free online anatomy resources. Augustana College, Rock Island, IL. URL: https://sites.google.com/view/anatomy‐resources/home [accessed 22 March 2021]. [Google Scholar]
- Franchi T. 2020. The impact of the Covid‐19 pandemic on current anatomy education and future careers: A student's perspective. Anat Sci Educ 13:312–315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Georgetown University . 2021. Georgetown University Medical Center Gross Anatomy Videos. Georgetown University, Washington, DC. URL: https://dml.georgetown.edu/gross‐anatomy‐videos/ [accessed 24 March 2021]. [Google Scholar]
- García‐Morales VJ, Garrido‐Moreno A, Martín‐Rojas R. 2021. The transformation of higher education after the COVID disruption: Emerging challenges in an online learning scenario. Front Psychol 12:616059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grajek S. 2020. EDUCAUSE COVID‐19 quickpoll results: 2020 Commencement plans. EDUCAUSE Review, 30 March 2021. EDUCAUSE, Denver, CO. URL: https://er.educause.edu/blogs/2020/3/educause‐covid‐19‐quickpoll‐2020‐commencement‐plans [accessed 18 August 2021]. [Google Scholar]
- Gould DJ, Franklin SR, MacPherson BR. 2015. Thieme MyCourse. Thieme Medical Publishers Inc., New York, NY. URL: https://mycourse.thieme.com/pages/Home [accessed 24 March 2021]. [Google Scholar]
- Guo T, Kiong KL, Yao CM, Windon M, Zebda D, Jozaghi Y, Zhao X, Hessel AC, Hanna EY. 2020. Impact of the COVID‐19 pandemic on otolaryngology trainee education. Head Neck 42:2782–2790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Habicht JL, Kiessling C, Winkelmann A. 2018. Bodies for anatomy education in medical schools: An overview of the sources of cadavers worldwide. Acad Med 93:1293–1300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harmon DJ, Attardi SM, Barremkala M, Bentley DC, Brown KM, Dennis JF, Goldman HM, Harrell KM, Klein BA, Ramnanan CJ, Richtsmeier JT, Farkas GJ. 2021. An Analysis of Anatomy Education before and During Covid‐19: May‐August 2020. Anat Sci Educ 14:132–147. [DOI] [PubMed] [Google Scholar]
- Harrell KM, McGinn MJ, Edwards CD, Warren Foster K, Meredith MA. 2021. Crashing from cadaver to computer: Covid‐driven crisis‐mode pedagogy spawns active online substitute for teaching gross anatomy. Anat Sci Educ 14:536–551. [DOI] [PubMed] [Google Scholar]
- Herr MJ, Nelson RJ. 2021. Administering a stay‐at‐home dental gross anatomy practical during COVID‐19. J Dent Educ 85:S939–S940. [DOI] [PubMed] [Google Scholar]
- Johns Hopkins . 2021. Coronavirus resource center. Global map. Johns Hopkins University and Medicine, Baltimore, MD. URL: https://coronavirus.jhu.edu/map.html [accessed 19 April 2021]. [Google Scholar]
- Jonas Philanthropies . 2015. New AACN data confirms enrollment surge in schools of nursing. Jonas Philanthropies, New York, NY. URL: https://jonasphilanthropies.org/new‐aacn‐data‐confirms‐enrollment‐surge‐in‐schools‐of‐nursing/ [accessed 19 March 2021]. [Google Scholar]
- Jones DG. 2021. Anatomy in a post‐Covid‐19 world: Tracing a new trajectory. Anat Sci Educ 14:148–153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalter L. 2019. U.S. medical school enrollment rises 30%. Association of American Medical Colleges, Washington, DC. URL: https://www.aamc.org/news‐insights/us‐medical‐school‐enrollment‐rises‐30 [accessed 19 March 2021]. [Google Scholar]
- Kathree BA, Khan SB, Ahmed R, Maart R, Layloo N, Asia‐Michaels W. 2020. COVID‐19 and its impact in the dental setting: A scoping review. PLoS One 15:e0244352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kenhub . 2021. Kenhub Anatomy. Kenhub GmbH, Leipzig, Germany. URL: https://www.kenhub.com/en/library/anatomy [accessed 24 March 2021]. [Google Scholar]
- Khamees D, Brown CA, Arribas M, Murphey AC, Haas MRC, House JB. 2020. In crisis: Medical students in the COVID‐19 pandemic. AEM Educ Train 4:284–290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khan S, Mian A. 2020. Medical education: COVID‐19 and surgery. Br J Surg 107:e269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kramer B, Billings B, Moxham B, Winkelmann A. 2020. IFAA Best Practice Guidelines for Body Donation Programmes During the novel Coronavirus Pandemic. 1st Ed. Johannesburg, South Africa: International Federation of Associations of Anatomists. 7 p. URL: http://www.ifaa.net/wp‐content/uploads/2020/05/IFAA‐Staement‐on‐COVID‐19_‐final‐v2.pdf [accessed 16 March 2021]. [Google Scholar]
- Krebs C, Fejtek M, Mordhorst A. 2020. Clinical Anatomy Website. University of British Columbia, Vancouver, Canada. URL: http://clinicalanatomy.ca/ [accessed 24 March 2021]. [Google Scholar]
- Kolomitro K, MacKenzie LW, Wiercigroch D, Godden L. 2018. The design and evaluation of a master of science program in anatomical sciences at Queen's University Canada. Anat Sci Educ 11:613–622. [DOI] [PubMed] [Google Scholar]
- Larson S. 2021. Virtual medical school admissions: Making the process accessible for all. EDUCAUSE Review, 27 July 2021. EDUCAUSE, Denver, CO. URL: https://er.educause.edu/articles/2021/7/virtual‐medical‐school‐admissions‐making‐the‐process‐accessible‐for‐all [accessed 19 August 2021]. [Google Scholar]
- Lemos GA, Araújo DN, de Lima FJ, Bispo RF. 2021. Human anatomy education and management of anatomic specimens during and after COVID‐19 pandemic: Ethical, legal and biosafety aspects. Ann Anat 233:151608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leung BC, Williams M, Horton C, Cosker TDA. 2020. Modernising anatomy teaching: Which resources do students rely on? J Med Educ Curr Dev 7:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Longhurst GJ, Stone DM, Dulohery K, Scully D, Campbell T, Smith CF. 2020. Strength, weakness, opportunity, threat (SWOT) analysis of the adaptations to anatomical education in the United Kingdom and Republic of Ireland in response to the Covid‐19 pandemic. Anat Sci Educ 13:301–311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lyons V, McNulty N, Catlin B, Swenson R. 2021. Human Anatomy Learning Modules. Geisel School of Medicine at Dartmouth Dartmouth, Hanover, NH. URL: https://www.dartmouth.edu/~anatomy/HAE/index.html [accessed 24 March 2021]. [Google Scholar]
- MacDonald CW, Lonnemann E, Petersen SM, Rivett DA, Osmotherly PG, Brismée JM. 2020. COVID 19 and manual therapy: International lessons and perspectives on current and future clinical practice and education. J Man Manip Ther 28:134–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Margolis B. 2021. Autopsy.Online. Autopsy Center of Chicago, Chicago, IL. URL: https://autopsy.online/ [accessed 24 March 2021]. [Google Scholar]
- Mays N, Pope C. 1995. Rigour and qualitative research. Br Med J 311:109–112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McBride JM, Drake RL. 2018. National survey on anatomical sciences in medical education. Anat Sci Educ 11:7–414. [DOI] [PubMed] [Google Scholar]
- McLachlan JC, Bligh J, Bradley P, Searle J. 2004. Teaching anatomy without cadavers. Med Educ 38:418–424. [DOI] [PubMed] [Google Scholar]
- McMenamin PG, Quayle MR, McHenry CR, Adams JW. 2014. The production of anatomical teaching resources using three‐dimensional (3D) printing technology. Anat Sci Educ 7:479–486. [DOI] [PubMed] [Google Scholar]
- Menard J. 2020. Video conferencing systems used in higher education. LISTedTECH, Ottawa, ON, Canada. URL: https://www.listedtech.com/blog/video‐conferencing‐systems‐used‐in‐higher‐education [accessed 30 March 2020]. [Google Scholar]
- Moore KL, Agur AM, Dalley AF II. 2014. Essential Clinical Anatomy. 5th Ed. Baltimore, MD: Wolters Kluwer. 712 p. [Google Scholar]
- Moore KL, Dalley AF II, Agur AM. 2017. Clinically Oriented Anatomy. 8th Ed. Philadelphia, PA: Wolters Kluwer. 1168 p. [Google Scholar]
- Muñoz‐Leija MA, Zarate‐Garza PP, Jacobo‐Baca G, Quiroga‐Garza A, Salinas‐Alvarez Y, Martinez‐Garza JH, Elizondo‐Omaña RE, Guzmán‐López S. 2020. Modifications to the delivery of a gross anatomy course during the COVID‐19 pandemic at a Mexican medical school. Eur J Anat 24:507–512. [Google Scholar]
- Murphy B. 2020. Limited by pandemic precautions, white‐coat ceremonies take new forms. American Medical Association, Chicago, IL. URL: https://www.ama‐assn.org/residents‐students/medical‐school‐life/limited‐pandemic‐precautions‐white‐coat‐ceremonies‐take‐new [accessed 19 August 2021]. [Google Scholar]
- Naidoo N, Akhras A, Banerjee Y. 2020. Confronting the challenges of anatomy education in a competency‐based medical curriculum during normal and unprecedented times (COVID‐19 pandemic): Pedagogical framework development and implementation. JMIR Med Educ 6:e21701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Netter FH. 2020. The Netter Presenter: Human Anatomy Collection, Version 2.0. Elsevier, Philadelphia, PA. URL: https://www.netterimages.com/book‐presenter‐anatomy‐9781929007221.html [accessed 23 September 2020]. [Google Scholar]
- Netter 3D . 2018. Netter 3D Anatomy Powered by CyberAnatomy. Elsevier Inc. Cyber Anatomy Corporation, Philadelphia, PA. URL: http://netter3danatomy.com/ [accessed 16 April 2021]. [Google Scholar]
- Nieder GL, Borges NJ. 2012. An eight‐year study of online lecture use in a medical gross anatomy and embryology course. Anat Sci Educ 5:311–320. [DOI] [PubMed] [Google Scholar]
- Nieder GL, Nagy F. 2002. Analysis of medical students' use of web‐based resources for a gross anatomy and embryology course. Clin Anat 15:409–418. [DOI] [PubMed] [Google Scholar]
- Nworie J. 2021. Beyond COVID‐19: What's next for online teaching and learning in higher education? EDUCAUSE Review, 19 May 2021. EDUCAUSE, Denver, CO. URL: https://er.educause.edu/articles/2021/5/beyond‐covid‐19‐whats‐next‐for‐online‐teaching‐and‐learning‐in‐higher‐education [accessed 19 August 2021]. [Google Scholar]
- Onigbinde OA, Ajagbe AO, Oyeniran OI, Chia T. 2021a. Post‐COVID‐19 pandemic: Standard operating procedures for gross anatomy laboratory in the new normal. Morphologie 105:196–203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Onigbinde OA, Chia T, Oyeniran OI, Ajagbe AO. 2021b. The place of cadaveric dissection in post‐COVID‐19 anatomy education. Morphologie 105:259–266. [DOI] [PubMed] [Google Scholar]
- OSHA . 1990. Occupational Safety and Health Administration. Standard interpretations. Application of the formaldehyde standard, 1910.1048, to private medical school personnel. Occupational Safety and Health Administration, United States Department of Labor, Washington, DC. URL: https://www.osha.gov/laws‐regs/standardinterpretations/1990‐05‐16 [accessed 14 March 2021]. [Google Scholar]
- Pacheco LF, Noll M, Mendonça CR. 2020. Challenges in teaching human anatomy to students with intellectual disabilities during the Covid‐19 pandemic. Anat Sci Educ 13:556–557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- PAEA . 2019. Physician Assistant Education Association. PAEA Research. Program Report 34: By the Numbers | Data from the 2018 Program Survey. 1st Ed. Washington, DC: Physician Assistant Education Association. 54 p. URL: https://paeaonline.org/wp‐content/uploads/imported‐files/program‐report‐34‐20191002‐1.pdf [accessed 19 March 2021]. [Google Scholar]
- Pather N, Blyth P, Chapman JA, Dayal MR, Flack NAMS, Fogg QA, Green RA, Hulme AK, Johnson IP, Meyer AJ, Morley JW, Shortland PJ, et al. 2020. Forced disruption of anatomy education in Australia and New Zealand: An acute response to the Covid‐19 pandemic. Anat Sci Educ 13:284–300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearson S. 2020. Anatomy: Beyond the COVID‐19 pandemic. Acad Med 96:e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peters M, ten Cate O. 2014. Bedside teaching in medical education: A literature review. Perspect Med Educ 3:76–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pokhrel S, Chhetri R. 2021. A literature review on impact of COVID‐19 pandemic on teaching and learning. High Educ Future 8:133–141. [Google Scholar]
- Rizzolo LJ. 2002. Human dissection: An approach to interweaving the traditional and humanistic goals of medical education. Anat Rec 269:242–248. [DOI] [PubMed] [Google Scholar]
- Rockarts J, Brewer‐Deluce D, Shali A, Mohialdin V, Wainman B. 2020. National survey on Canadian undergraduate medical programs: The decline of the anatomical sciences in Canadian medical education. Anat Sci Educ 13:378–386. [DOI] [PubMed] [Google Scholar]
- Rohen JW, Yokochi C, Lutjen‐Drecoll E. 2015. Anatomy: A Photographic Atlas. 8th Ed. Philadelphia, PA: Wolters Kluwer. 560 p. [Google Scholar]
- Ross CF, Pescitelli MJ, Smith HF, Williams JM. 2021. Teaching anatomy with dissection in the time of COVID‐19 is essential and possible. Clin Anat 34:1135–1136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosset A, Heuberger J. 2021. OsiriX DICOM Viewer, Pixmeo SARL, Geneva, Switzerland. URL: https://www.osirix‐viewer.com/ [accessed 24 March 2021]. [Google Scholar]
- Saldaña J. 2016. The Coding Manual for Qualitative Researchers. 3rd Ed. Thousand Oaks, CA: SAGE Publications Ltd. 368 p. [Google Scholar]
- Seitz H, Rediske A. 2021. Impact of covid‐19 curricular shifts on learning gains on the microbiology for health sciences concept inventory. J Microbiol Biol Educ 22:22.1.73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singal A, Sahni D, Chaudhary P, Singh H. 2021. Virtual thanks giving to a cadaver by medical students exposed to learning anatomy before and amidst COVID‐19 pandemic. Surg Radiol Anat 43:523–527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schapiro MO. 2021. Let's not return to normal when the ‘new normal’ finally arrives. The Chronicle of Higher Education, 29 July 2021. The Chronicle of Higher Education Inc., Washington, DC. URL: https://www.chronicle.com/article/lets‐not‐return‐to‐normal‐when‐the‐new‐normal‐finally‐arrives [accessed 19 August 2021]. [Google Scholar]
- Schneider R, Morse DE, Bennett‐Clarke C, Hankin M. 2021. Anatomy & Physiology Revealed 4.0: An Interactive Cadaver Dissection Experience. McGraw Hill, New York, NY. URL: https://www.mheducation.com/highered/explore/apr.html/ [accessed 24 March 2021]. [Google Scholar]
- Schutte AF. 2016. Who is repeating anatomy? Trends in an undergraduate anatomy course. Anat Sci Educ 9:171–178. [DOI] [PubMed] [Google Scholar]
- Shah S, Castro‐Dominguez Y, Gupta T, Attaran R, Byrum GV III, Taleb A, Pettyjohn A, Bartel RC, Szerlip M, Henry TD, Mahmud E. 2020. Impact of the COVID‐19 pandemic on interventional cardiology training in the United States. Catheter Cardiovasc Interv 96:997–1005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simpson JS. 2014. An economical approach to teaching cadaver anatomy: A 10‐year retrospective. Am Biol Teach 76:42–46. [Google Scholar]
- Smith CF, Pawlina W. 2021. A Journey Like No Other: Anatomy 2020! Anat Sci Educ 14:5–7. [DOI] [PubMed] [Google Scholar]
- Spiteri G, Fielding J, Diercke M, Campese C, Enouf V, Gaymard A, Bella A, Sognamiglio P, Sierra Moros MJ, Riutort AN, Demina YV, Mahieu R, Broas M, Bengnér M, Buda S, Schilling J, Filleul L, Lepoutre A, Saura C, Mailles A, Levy‐Bruhl D, Coignard B, Bernard‐Stoecklin S, Behillil S, van der Werf S, Valette M, Lina B, Riccardo F, Nicastri E, Casas I, Larrauri A, Salom Castell M, Pozo F, Maksyutov RA, Martin C, Van Ranst M, Bossuyt N, Siira L, Sane J, Tegmark‐Wisell K, Palmérus M, Broberg EK, Beauté J, Jorgensen P, Bundle N, Pereyaslov D, Adlhoch C, Pukkila J, Pebody R, Olsen S, Ciancio BC. 2020. First cases of coronavirus disease 2019 (COVID‐19) in the WHO European Region, 24 January to 21 February 2020. Euro Surveill 25:2000178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Srinivasan DK. 2020. Medical students' perceptions and an anatomy teacher's personal experience using an e‐learning platform for tutorials during the Covid‐19 crisis. Anat Sci Educ 13:318–319. [DOI] [PubMed] [Google Scholar]
- Sugand K, Abrahams P, Khurana A. 2010. The anatomy of anatomy: A review for its modernization. Anat Sci Educ 3:83–93. [DOI] [PubMed] [Google Scholar]
- Swinnerton BJ, Morris NP, Hotchkiss S, Pickering JD. 2017. The integration of an anatomy massive open online course (MOOC) into a medical anatomy curriculum. Anat Sci Educ 10:53–67. [DOI] [PubMed] [Google Scholar]
- Taber KS. 2018. The use of Cronbach's alpha when developing and reporting research instruments in science education. Res Sci Educ 48:1273–1296. [Google Scholar]
- Trelease R. 2006. Anatomy meets architecture: Designing new laboratories for new anatomists. Anat Rec 289B:241–251. [DOI] [PubMed] [Google Scholar]
- Trelease RB. 2015. Essential e‐learning and m‐learning methods for teaching anatomy. In: Chan LK, Pawlina W (Editors). Teaching Anatomy: A Practical Guide. 1st Ed. New York, NY: Springer International Publishing. p 247–258. [Google Scholar]
- Twenge JM. 2017. iGen: Why Today's Super‐Connected Kids Are Growing Up Less Rebellious, More Tolerant, Less Happy‐‐and Completely Unprepared for Adulthood‐‐and What That Means for the Rest of Us. 1st Ed. New York, NY: Atria Books. 342 p. [Google Scholar]
- UNESCO . 2020. United Nations Educational, Scientific and Cultural Organization Education. From disruption to recovery. The United Nations Educational, Scientific and Cultural Organization, Paris, France. URL: https://en.unesco.org/covid19/educationresponse [accessed 16 March 2021]. [Google Scholar]
- UAMS . 2009. University of Arkansas for Medical Sciences. Anatomy Resource. University of Arkansas, Fayetteville, AR. URL: http://anatomy.uams.edu/gross_atlas.html [24 March 2021]. [Google Scholar]
- University of Wisconsin . 2021. Video Library. University of Wisconsin School of Medicine and Public Health, University of Wisconsin School of Medicine and Public Health. Madison, WI. URL: http://videos.med.wisc.edu/events/65/videos/ [accessed 24 March 2020]. [Google Scholar]
- VH Dissector . 2021. VH Dissector for Medical Education. Touch of Life Technologies, Aurora, CO. URL: https://www.toltech.net/anatomy‐software/solutions/vh‐dissector‐for‐medical‐education [accessed 24 March 2021]. [Google Scholar]
- Visible Body . 2021. Visible Body Human Anatomy Atlas. Argosy Publishing Inc., Newton, MA. URL: https://www.visiblebody.com/ [accessed 24 March 2020]. [Google Scholar]
- Vived Anatomy . 2019. VIVED Anatomy, VIVED Learning, Coatsville, IA. URL: https://vivedlearning.com/vivedanatomy/ [accessed 29 March 2019]. [Google Scholar]
- von Horst C, von Hagens R, Sora CM, Henry RW. 2019. History and development of plastination techniques. Anat Histol Embryol 8:512–517. [DOI] [PubMed] [Google Scholar]
- Yammine K, Violato C. 2015. A meta‐analysis of the educational effectiveness of three‐dimensional visualization technologies in teaching anatomy. Anat Sci Educ 8:525–538. [DOI] [PubMed] [Google Scholar]
- Zhang X, Al‐Mekhled D, Choate J. 2021. Are virtual physiology laboratories effective for student learning? A systematic review. Adv Physiol Educ 45:467–480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zureick AH, Burk‐Rafel J, Purkiss JA, Hortsch M. 2018. The interrupted learner: How distractions during live and video lectures influence learning outcomes. Anat Sci Educ 11:366–376. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Material
Supplementary Material
Supplementary Material


