Abstract
The COVID‐19 pandemic has presented many novel situations that have amplified the presence of moral distress in healthcare. With limited resources to protect themselves against the virus and strict safety regulations that alter the way they work, healthcare providers have felt forced to engage in work behaviours that conflicted with their professional and personal sense of right and wrong. Although many providers have experienced moral distress while being physically in the workplace, others suffered while at home. Some healthcare providers worked in facilities that were unable to open during the pandemic due to restrictions, which could contribute to a sense of powerlessness and guilt. The current study assessed whether the ability to see patients each week impacted the relationship between an employee's moral distress and their mental health strain, burnout, and maladaptive coping. A total of 378 healthcare providers responded to weekly surveys over the course of 7 months (April 2020–December 2020). Hierarchical linear modeling techniques were used to examine the study variables over time. Results showed that moral distress predicted an individual's mental health strain and burnout, even after controlling for the prior week. However, moral distress was not a significant predictor of maladaptive coping. Interestingly, there was not a significant difference between the average ratings of moral distress between those who were able, and those who were not able to see patients, meaning that both groups experienced symptoms of moral distress. However, cross‐level moderation results indicated that the ability to see patients magnified the relationships between moral distress and mental health strain and burnout over time. Implications of the results and recommendations for how moral distress should be addressed among healthcare providers are discussed.
Keywords: burnout, COVID‐19, maladaptive coping, mental health strain, moral distress
Introduction
Across the globe, healthcare workers have been challenged with increased demands and changes in work obligations due to the COVID‐19 pandemic (Dunham et al. 2020; Hesselink et al. 2021; Sheather & Fidler 2021; Williamson et al. 2020). While many hospital healthcare workers have been required to increase their work hours due to the limited personnel and increase in patient cases, other healthcare providers were considered ‘nonessential’ and had to standby as their workplaces shut down to prevent the spread of the virus (Gabler et al. 2020; Inglet 2020; Levy 2020). Researchers have assessed how changes at work due to epidemics have increased rates of physical and psychological stressors, whether employees are working directly with patients, such as with physicians and nurses, or indirectly such as laboratory technicians and respiratory therapists (see Preti et al. 2020, for review). Recent research has demonstrated the impact of COVID‐19 on healthcare workers' emotional stress (Cai et al. 2020), depression (Lai et al. 2020; Liang et al. 2020), sleep quality (Lai et al. 2020; Xiao et al. 2020), burnout (Kok et al. 2021; Plouffe et al. 2021), and anxiety (Lai et al. 2020; Xiao et al. 2020).
One type of stressor that has been highly discussed in research and popular press is moral distress. Moral distress refers to the emotional experience of feeling involuntarily complicit in an unethical act but have little power to act differently or change the situation (Corley 2002; Godshall 2021; Hamric & Epstein 2017; Jameton 1984). Healthcare workers can experience moral distress when they are prohibited by resource constraints, organizational protocols, or government requirements. Moral distress is conceptually similar to moral injury, where both involve the conflict between one's beliefs of the right course of action. However, moral distress results from individuals feeling ‘trapped’ by organizational constraints and moral injury involves trauma and atrocities that violate one's beliefs of what actions are necessary, typically referring to situations that involve violence or death (Jinkerson 2016; Papazoglou & Chopko 2017; Sugrue 2019; Wilson 2021). While both concepts may be present during the COVID‐19 pandemic, the focus of the current paper is on moral distress. Moral distress differs from other psychological stressors in that it involves witnessing or engaging in actions that are perceived as a violation of one's moral values, and the resulting guilt and shame associated with one's involvement in the event (Corley 2002).
The COVID‐19 pandemic has presented many nuanced situations for moral distress to occur, such as preventing family members from visiting the ill, inability to rest, forced decision‐making of life support, lack of resources, such as PPE and ventilators, few effective treatments, and the inability to practice as normal (Cacchione 2020; Daubman et al. 2020; Dunham et al. 2020; Hlubocky, et al. 2021; Morley et al. 2020; Vig 2021). Vig (2021) categorized the broad range of workplace factors into patient factors (e.g. suboptimal care due to the volume of patients), clinical factors (e.g. inadequate medical knowledge of reassigned positions), institutional factors (e.g. pressure to employ untested treatments), and policy factors (e.g. frequent guideline changes), demonstrating that circumstances that increase the likelihood of moral distress can surface from numerous places in the system. These factors have been endorsed globally in studies in France (Azoulay et al. 2020), Norway (Miljeteig et al. 2021), Netherlands (Donkers et al. 2021; Hesselink et al. 2021), United States (Butler et al. 2020; ffrench‐O'Carroll 2021; Hines et al. 2021; Wiener et al. 2021), Canada (Plouffe et al. 2021) Australia, Italy (Kreh et al. 2021), and United Kingdom (Petrella et al. 2021; Rosenwohl‐Mack et al. 2020).
Although moral distress was first observed among nurses (Jameton 1984), providers across all disciplines of healthcare, including physicians, respiratory therapists, social workers, and chaplains, experience moral distress (Whitehead et al. 2015). Researchers have found that moral distress ratings have varied due to an individual's occupation (Donkers et al. 2021; Dryden‐Palmer et al. 2020; Kok et al. 2021; Miljeteig et al. 2021; Petrella et al. 2021; Tan et al. 2020); however, these reports have been conducted primarily within hospital settings. While moral distress is evident for those on the ‘frontlines’ of the healthcare system, individuals who are prevented from working by regulations may also experience moral distress. As the pandemic began to spread more rapidly around the world, large institutions such as the Centers for Disease Control in the United States, British National Health Service, and British National Health Service (see Moletta et al. 2020 for review) recommended that healthcare systems minimize, postpone, or cancel elective, ‘nonessential’ procedures. These recommendations caused many healthcare providers', like specialists, lab techs, dentists, massage therapists, and support staff, work to come to a halt (Gabler et al. 2020; Inglet 2020; Levy 2020). Most of the published research on moral distress during COVID‐19 has been conducted within the hospital setting with nurses, physicians, and supporting staff (e.g. Donkers et al. 2021; Dryden‐Palmer et al. 2020; Hesselink et al. 2021; Kok et al. 2020; Miljeteig et al. 2021), with few researchers expanding to the providers affected outside of the hospital walls (Plouffe et al. 2021; ffrench‐O'Carroll 2021; Petrella et al. 2021). Tan et al. (2020) examined psychological distress among medically and ‘non‐medically trained’ hospital personnel (e.g. allied health professionals, pharmacists, and technicians) and found that the non‐frontline workers had higher prevalence of anxiety than the hospital workers. Tan et al.'s (2020) study promotes a need to investigate whether moral distress could follow the same trend.
In their recent review, Morley (2020) provided examples of the similar symptoms of moral conflict between those who were working by the bedside, and those who were sent home. Bedside caregivers were required to maintain their own safety by dressing in full PPE, however, abiding by strict protocols of safety led to providers feeling as though they are giving substandard care (e.g. taking additional time to put on PPE as a patient suddenly experiences cardiac arrest). Similarly, a psychologist, who has had to shut their office doors and adjust to telehealth practices, may also experience moral distress through perceiving their remote sessions as being a lower quality of connecting to the patient while needing to maintain social distancing precautions (Morley 2020). Other healthcare providers, like massage therapists and dental hygienists, who were unable to conduct telehealth visits, were either furloughed or permanently let go from their workplaces and may have felt a sense of powerlessness in the inability to use their skillset to combat the virus. Many media outlets have also highlighted how individuals are experiencing guilt regarding the perceived inability to contribute to the fight against the virus, while others experience guilt for knowing a patient's condition and not being able to address their needs (Angelos 2020; Covert 2021; Gabler et al. 2020; Rodger 2020).
Recent research has generally supported these claims, finding that workers on the frontline as well as those working in ‘their usual wards’ (e.g. oncology unit) experienced mental health symptoms during the pandemic (Lai et al. 2020; Wu et al. 2020). However, studies have neglected to assess healthcare workers who may be unable to see patients due to various circumstances of the pandemic. According to the Peterson‐KFF Health System Tracker (a U.S.‐based monitoring assessment; McDermott & Cox 2020), 1.57 million healthcare workers lost their jobs in March and April of 2020, with workers in ambulatory healthcare settings, like dental and physician's offices, accounting for more than half of the total healthcare job losses. Additionally, the American Massage Therapy Association (2020) indicated that as of April 2020 86% of massage therapists had stopped working. With many providers losing their ability to see patients, research is needed to understand the presence of moral distress for workers who were shut out of their offices and unable to work.
The repercussions of moral distress are important to consider for all job types, as the mental health and well‐being of healthcare providers can have damaging effects for when life goes back to ‘normal’ in the months to come. With the lack of research investigating the longitudinal effects of moral distress, organizations are unable to understand and provide the resources healthcare workers need to keep themselves and their work environment safe.
The present study
The current study aims to expand the literature on healthcare provider well‐being during the COVID‐19 pandemic in several ways. The first aim is to examine moral distress over time. Even prior to the pandemic, moral distress has not been evaluated longitudinally. In Oh and Gastmans' (2015) review of the literature, almost all studies that have been published on moral distress have been conducted cross‐sectionally. Other researchers have also critiqued the over‐reliance on cross‐sectional designs, limiting our ability to understand moral distress over time (Ando & Kawano 2018; Asgari et al. 2019; Elpern et al. 2005; Haghighinezhad et al. 2019). Moral distress has continued to be a hot topic of many editorials during the pandemic (e.g. Angelos 2020; Cacchione 2020; Fumis et al. 2017; Kok et al. 2020; Turale et al. 2020; White & Lo 2020); however, only a small number of studies have been published. Once more, the research continues to examine primarily healthcare workers in hospital settings during a single time point. With a lack of studies examining fluctuations in moral distress over time, researchers are unable to understand how frequent experiences of moral distress impact well‐being for different employees (Oh & Gastmans 2015).
The second goal of this study is to examine whether healthcare providers, including those outside of the hospital walls, also experience moral distress. Specifically, the current study will examine whether the relationship between moral distress (our predictor) and mental health strain, burnout, and maladaptive coping (our outcomes) is stronger for healthcare professionals when they are able to see patients (our moderator) using a global sample over the course of 7 months (see Fig. 1).
Fig. 1.
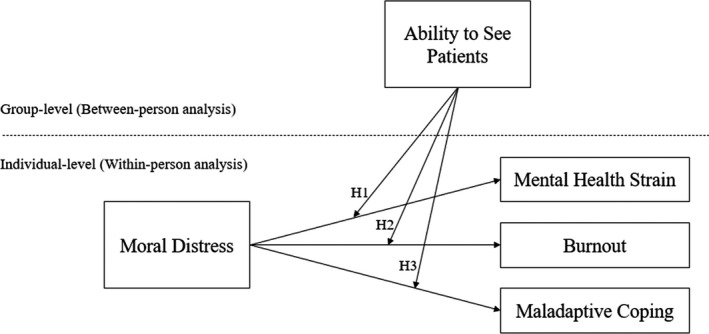
The hypothesized model.
The obligation to abide by extreme safety protocols, such as restricted patient access to family, limited resources, and knowledge of treatment for the COVID‐19 virus, may intensify workers' moral distress. Similarly, those healthcare workers who are bound by government or professional guidelines to shut down their businesses and are prohibited from providing care to their patients may also experience moral distress through the perception of ‘not being able to play their part’ (Rodger 2020, p.1). As healthcare workers, individuals work within an industry that helps diagnose and heal the sick, when unable to provide care and relief to their patients based on organizational constrains, moral distress may present itself. Thus, the current study aims to understand the following research question:
RQ1: When healthcare workers are able to see patients in a given week, do they experience more or less moral distress than the weeks they are not able to see patients?
Previous research has investigated the relationship between moral distress and well‐being, however, there is limited information on how this relationship exists over time. Throughout the pandemic, many practices have had to shut down completely, implement maximum patient capacities, or limit a worker's ability to provide care as they normally would. The inability to provide care in a way that a worker is trained to do may cause healthcare providers to feel guilt, shame, and powerlessness for the depersonalization of their work due to COVID‐19 restrictions (Sugrue 2019).
Previous research has shown the impact of powerlessness. In one study of veterinarians, over 70% of the sample felt that when they were prevented from providing appropriate care for which they were trained, the veterinarians reported increased rates of distress (Meltzer & Huckabay 2004). Similarly, in a qualitative study of emergency nurses, participants described that the profound feeling of not being able to provide patient care as they wanted to contributed to their experience of moral distress (Wolf et al. 2016). Prior to the pandemic, studies had linked moral distress and emotional exhaustion (Meltzer & Huckabay 2004) as well as psychological and physical well‐being (Elpern et al. 2005; Sanchez‐Reilly et al. 2013). These findings have persisted in recent studies including moral distress as a predictor of depression, anxiety, and PTSD (Plouffe et al. 2021). The changes in work design due to lack of resources, personnel, or protocols may increase the likelihood of moral distress and its relationship with mental health strain over time. Thus, the following hypothesis is presented:
Hypothesis 1: There will be a significant positive relationship between weekly assessments of moral distress and mental health strain, such that moral distress will predict current mental health strain and the following week's strain.
Additionally, the changing nature of work due to the pandemic has likely increased the symptoms of burnout for healthcare workers. There exists vast amount of research linking moral distress to burnout cross‐sectionally (Austin et al. 2017; Fernandez‐Parsons et al. 2013; Meltzer & Huckabay 2004; Ohnishi et al. 2010; Piers et al. 2012; Sundin‐Huard & Fahy 1999). This relationship is likely to be magnified during the current pandemic (Kok et al. 2021; Plouffe et al. 2021). The continuous rise in patient cases and lack of effective treatment may increase the symptoms related to exhaustion, depersonalization, and reduced sense of personal accomplishment.
Previous research states that burnout results from long‐term adaptive failure to resolve mismatches between job demands and worker resources (Maslach et al. 2001). Long‐term exposure to workplace demands that an individual feels powerlessness to control increases the likelihood of burnout (Demerouti et al. 2001; Maslach et al. 2001; Shirom 2003). Thus, healthcare providers' inability to prevent the spread of the virus and minimize the harm to their patient's well‐being contributes to the sense of helplessness. A recent study conducted by Barello et al. (2020) found that in their sample of 532 physicians, 92% of the participants reported that the pandemic put them more frequently in touch with other people's suffering, increasing symptoms of burnout. Additionally, the researchers found that responses to the items ‘the COVID‐19 emergency makes me take difficult decisions at work’ and ‘At work I usually do things I don't want to’ were most correlated with emotional exhaustion and psycho‐somatic distress (Barello et al. 2020). Thus, the following hypothesis is presented:
Hypothesis 2: There will be a significant positive relationship between weekly assessments of moral distress and burnout, such that moral distress will predict current burnout and the following weeks burnout.
Prior research has also shown that moral distress, due to the intensified guilt, has been associated with poor coping behaviours (Wolf et al. 2016). Previous research has shown experiencing increased emotional demands at work has been predictive of alcohol and drug use (Cunradi et al. 2003; Shepherd et al. 2019; Wolf et al. 2016). In one qualitative study of nurses who experienced moral distress, participants reported using maladaptive coping mechanisms including alcohol, food, or medications (Wolf et al. 2016). Nurses in this sample reported that the inability to perform the obligations of nursing due to a lack of unit support, limited patient interaction, and the perception of a distinct disconnection between the administration and the practitioners providing care were the main reasons for moral distress to occur. Individuals may acknowledge the precautions that are taken as necessary, however, feel guilt associated with the inability to nurture their patients as they normally would. Therefore, the guilt can cause individuals to pursue nonbeneficial coping behaviours such as alcohol, drug and sleeping pill use. Thus, the following hypothesis is presented:
Hypothesis 3: There will be a significant positive relationship between weekly assessments of moral distress and maladaptive coping, such that moral distress will predict poor coping and the following weeks coping.
Additionally, prior research has not examined whether the relationship between moral distress and these outcomes may differ due to one's ability to see patients. The COVID‐19 pandemic demonstrates a unique situation where healthcare workers may be employed, but unable to work, and this status may change over time. Government and professional regulations may impact whether a healthcare provider is able to serve their patients and clients in a regular capacity each week. When individuals are restricted from working due to personal, professional, or government policy, they are likely to experience moral distress due to feeling undervalued and unable to contribute. However, when individuals are able to see patients, the manner in which they operate is likely to have changed due to the many COVID‐19 restrictions. Individuals may be required to see patients via telehealth, enforce limited visitation, or be required to distance themselves from their patients in a way that conflicts with their professional training.
Although moral distress is likely to occur whether they are able to see patients or not, the relationship between moral distress and mental health outcomes may be stronger when providers are able to see patients in a given week. Moral distress experienced when individuals are seeing patients may be more likely to be translated into greater mental health symptoms as a result of the employee being actively confronted with the negative consequences of their action (or inaction). Circumstances where an individual's professional opinion of care may counter the COVID‐19 restrictions may intensify the experiences of strain, burnout, and maladaptive coping. Those who are unable to see patients in a week are less likely to see the negative consequences of the factors that gave rise to their moral distress. Participants in the current study report whether they were able to see patients in a given week, and if there is significant variability in a provider's ability to see patients over the course of the study, we examined the weekly changes in the providers' moral distress and predicted outcomes. If there is no significant variability, the ability to see patients will be treated as a Level 2 between‐participants variable. Therefore, the current study proposes:
Hypothesis 4: There will be a significant interaction between moral distress and the ability to see patients on mental health strain, burnout, and maladaptive coping. The relationship between the predictor of moral distress and the mental health outcomes will be stronger for providers who are able to see patients in a given week than for providers who are unable to see patients.
Method
Participants and procedure
Healthcare providers were self‐reported by the respondent considering himself or herself a healthcare provider. Healthcare professionals from over 16 different medical specialties and 6 countries participated in the study. A total of 771 participants responded to a baseline questionnaire and elected to continue in the study. A total of 378 participants responded to at least two weekly surveys (49% response rate) and were used as the study sample. On average, participants responded to 5 weekly surveys (SD = 4.53, range = 2–23), were 46 years old (SD = 11.68), and worked in their current profession for 15 years (SD = 9.47). The majority of participants were female (87%) and white (91%). The most common professions reported by participants were massage therapy (61%), nursing (12%), multi‐professional (9%), medicine (8%), occupational therapy (2%), mental health (1%), social work (1%), and allied health, dental, physical therapy, psychologist, respiratory therapists, and acupuncture were under 1% of our participants.
Data were collected over the course of 7 months (April 16 to December 4, 2020) as part of a larger study, Project COPE: Chronicling healthcare prOviders Pandemic Experiences. Participants were recruited from social media, professional newsletters, healthcare podcasts, and word of mouth. The project had a website, social media accounts, videos, and logo to engage participation in the study. Participants were provided informed consent which assured them the confidentiality and anonymity of their results. Participation was voluntary. Participants were provided a link to an initial survey which requested information pertaining to their current working status, demographics, and an invitation to participant in weekly assessments. Following the initial survey questionnaire, each week participants were sent a reminder email along with a URL link to participate in the weekly survey which contained the study variables. See Heavner et al. (2021) for details on the complete study methodology.
Measures
Moral distress
Moral distress was assessed using the single‐item Moral Distress Questionnaire by Rathert et al. (2016). Participants were provided a brief definition of moral distress; ‘Moral distress is the stress healthcare workers feel when they believe they know the “right” thing to do on the job, but something in the environment prevents them from being able to do it, such as law/policies, other team members/colleagues, patient/family members, etc’. Participants were then asked, ‘In the last week how often have you felt moral distress in relation to your job/profession?’ and provided a six‐point scale ranging from never (1) to four times a day or more (6). Previous authors have provided evidence for the justification of single‐item measures in occupational health research (Fisher et al. 2016). In the present case, the single moral distress item clearly assessed the construct of interest.
Mental health strain
Mental health strain was assessed through the Mayo Clinic Physician Well‐Being Index (PWBI), for which prior research has established construct and criterion validity and reliability (Dyrbye et al. 2013). Participants were provided seven items referring to their previous week's mental state (e.g. ‘Have you worried that your work is hardening you emotionally?’ or ‘Have you often been bothered by feeling down, depressed, or hopeless?’). Participants responded yes or no, and were assigned a sum score of the seven items ranging from low mental health strain (0) to high mental health strain (7; Dyrbye et al. 2013).
Burnout
Participants reported their current level of burnout using the single‐item burnout measure from the Mini Z burnout measure (Dolan et al. 2015). Participants were informed to consider their own definition of burnout and to select which of the options best applies to them ranging from ‘I enjoy my work. I have no symptoms of burnout (1)’ to ‘I feel completely burned out. I am at the point where I may need to seek help (5)’.
Maladaptive coping
Maladaptive coping was assessed using items similar to those found in the substance abuse subscale of the brief COPE (Carver, 1997). Participants were asked ‘Which of the following have you found helpful in the past week?’ and were provided a list of coping mechanisms. Five items were used to create the maladaptive coping variable: alcohol use, sleeping pill use, prescription medications, illicit substance use (i.e. marijuana), and tobacco use. Responses could range from no maladaptive coping (0) to high maladaptive coping (5).
Ability to see patients
Each week, participants responded to the question ‘Are you currently seeing patients/clients?’ The phrase ‘see patients’ was specifically used in contrast to ‘treat patients’ to reflect the diverse ways that healthcare providers work and to allow for virtual sessions (e.g. telehealth). Responses were limited to yes or no. The intent of this study was to assess weekly‐level data for how individuals experience moral distress when they are able and not able to see patients. Specifically, the researchers were interested in comparing the levels of moral distress during weeks that participants saw patients to when they did not see patients and how this impacted the outcome variables (i.e. within‐subjects analysis). However, only five (out of the 378) participants switched from seeing to not seeing patients (or vice versa) over the course of the weekly assessments. Therefore, the ability to see patients was adjusted in the model to reflect a Level 2 between‐subjects moderator of the within‐person relationship between moral distress and outcomes. Participants were classified as those who were seeing patients during all of their weekly assessments (24%) or who were not seeing patients (76%).
Results
Descriptive statistics on the measured variables
The means, standard deviations, and within‐person correlations are presented in Table 1. On average, participants experienced moral distress two to three times a week (SD = 1.49). Moral distress had a significant bivariate correlation with mental health strain and burnout but did not have a significant within‐person correaltion with maladatpive coping.
Table 1.
Means, standard deviations, and within‐person bivariate correlations among study variables
| Scale | M | SD | 1 | 2 | 3 | 4 | 5 | |
|---|---|---|---|---|---|---|---|---|
| 1. | TIME | 51.43 | 54.29 | |||||
| 2. | Moral Distress | 2.71 | 1.49 | −0.15** | ||||
| 3. | Mental Health Strain | 2.32 | 0.89 | 0.08** | 0.18** | |||
| 4. | Burnout | 2.65 | 1.79 | 0.14** | 0.13** | 0.51** | ||
| 5. | Maladaptive coping | 0.36 | 0.68 | 0.23** | −0.02 | 0.11** | 0.08** | |
All variables were assessed weekly, ability to see patients was assessed at Level 2 and, thus, there is no within‐person variability to model. TIME was coded as days since baseline. M and SD are used to represent mean and standard deviation, respectively. *P < 0.05. **P < 0.01.
Hierarchical linear modelling
Because of the nested structure of the weekly surveys, hierarchical linear modeling techniques were utilized in R (Bliese 2016) with restricted maximum‐likelihood estimation to test our hypotheses. Participants responded to their surveys at different rates; however, multilevel modeling allows for unequal spacing between time intervals and uneven number of occasions (Bliese et al. 2018; Kwok et al. 2008). The interclass correlations (ICC) indicated that 54% of variance in moral distress, 66% of variance in mental health strain, 65% of variance in burnout, and 51% of variance in maladaptive coping could be attributed to the participant, justifying the use of multilevel analyses to examine our hypotheses (Shrout & Fleiss 1979).
Our first research question addressed whether moral distress was higher or lower when participants reported seeing patients in a given week. Due to the lack of variability in participants switching whether they saw patients each week, this question was examined between‐persons rather than within‐persons. Results showed that both groups of individuals, those who were not able to see patients (M = 2.78, SD = 1.54) and those who were able to see patients (M = 2.49, SD = 1.24), reported experiencing moral distress each week. There was no significant difference in moral distress (t (368) = −0.75, n.s.) between the two groups.
To examine the hypotheses, a series of autoregressive lead and lag effects were examined (see Table 2). Lead and lag variables are a valuable tool to examine relationships among variables over time (Selig & Little 2012). Specifically, a lead–lag effect refers to analyses that account for a previous value of a (leading) variable (e.g. reported as the previous week's moral distress) and is cross‐correlated with the values of another lagging variable which occurs at a later time (e.g. reported as next week's outcomes; Dormann & Griffin 2015; Selig & Little 2012).
Table 2.
Multilevel estimates for weekly moral distress predicting the current week's outcomes controlling for prior week's outcomes (H1–3)
| Predictor | Mental Health Strain | Burnout | Maladaptive Coping | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Estimate | SE | t | Estimate | SE | t | Estimate | SE | t | |
| Intercept | 0.11 | 0.09 | 1.29 | 0.32 | 0.05 | 6.26** | 0.39 | 0.05 | 7.99** |
| Time | 0 | 0 | 3.03** | 0 | 0 | 3.11** | 0 | 0 | 2.77** |
| Prior Week | 0.7 | 0.02 | 34.28** | 0.73 | 0.02 | 37.20** | −0.04 | 0.02 | −1.65 |
| Moral Distress | 0.21 | 0.03 | 8.42** | 0.1 | 0.01 | 7.97** | 0.02 | 0.01 | 1.59 |
| Next Week's | Next Week's | Next Week's | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Mental Health Strain | Burnout | Maladaptive Coping | |||||||
| Estimate | SE | t | Estimate | SE | t | Estimate | SE | t | |
| Intercept | 0.15 | 0.07 | 1.92 | 0.24 | 0.04 | 5.48*** | 0.49 | 0.05 | 9.87** |
| Time | 0 | 0 | 2.09* | 0 | 0 | 2.05* | 0 | 0 | 2.22* |
| Prior Week | 0.86 | 0.02 | 50.36** | 0.85 | 0.02 | 48.80** | −0.05 | 0.03 | −2.04* |
| Moral Distress | 0.06 | 0.02 | 2.99** | 0.04 | 0.01 | 3.67** | −0.02 | 0.01 | −1.49 |
Prior week refers to measurement of the criterion that was assessed the week before moral distress and the criterion were measured (e.g. ‘The previous week's mental health strain’). *P < 0.05; **P < 0.01.
Hypothesis 1 was supported; moral distress predicted both the current week's mental health strain, as well as the following week's mental health strain after controlling for the prior week's mental health strain. Hypothesis 2 was also supported; after controlling for the previous week's burnout, moral distress predicted the same week's burnout and the following week's burnout. However, Hypothesis 4 was not supported; after controlling for the previous week's maladaptive coping, there was not a significant relationship between moral distress and the current week's maladaptive coping or the following week's maladaptive coping. Although 30% of the sample reported using at least one of the maladaptive coping mechanisms each week, the use of the coping strategies was not related to experienced moral distress.
The final set of hypotheses examined the cross‐level interaction between moral distress and the ability to see patients predicting the outcome variables (see Table 3. An interaction occurs when the relationship between the predictor and outcome variable changes at different degrees of the moderator Mackinnon & Luecken 2008). After controlling for the previous week's mental health strain and main effects, the interaction between moral distress and the ability to see patients was a significant predictor of the current week's mental health strain; however, the interaction did not predict the following week's mental health strain. Simple slope analyses revealed that the relationship between moral distress and the current week's strain was significant for both those who were seeing patients (γ = 0.34, t = 4.63, P < 0.01) and for those who were not seeing patients (γ = 0.20, t = 7.63, p < 0.01). The relationship between moral distress and strain was stronger for those seeing patients than those who were not (See Fig. 2).
Table 3.
Multilevel estimates for the interaction between weekly moral distress and the ability to see patients predicting the current week's outcomes controlling for prior week's outcomes (H4)
| Predictor | Mental Health Strain | Burnout | Maladaptive Coping | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Estimate | SE | t | Estimate | SE | t | Estimate | SE | t | |
| Intercept | 0.14 | 0.09 | 1.45 | 0.37 | 0.06 | 6.80** | 0.36 | 0.06 | 6.81** |
| Time | 0 | 0 | 3.08** | 0 | 0 | 3.14** | 0 | 0 | 2.69** |
| Prior Week | 0.69 | 0.02 | 33.60** | 0.71 | 0.02 | 35.26** | −0.03 | 0.02 | −1.37 |
| Moral Distress | 0.2 | 0.03 | 7.65** | 0.09 | 0.01 | 7.24** | 0.02 | 0.01 | 1.37 |
| Patient Status | −0.18 | 0.21 | −0.86 | −0.13 | 0.11 | −1.26 | 0.07 | 0.11 | 0.58 |
| MD × PS | 0.15 | 0.08 | 1.89* | 0.11 | 0.04 | 2.88** | 0.01 | 0.03 | 0.35 |
| Next Week's | Next Week's | Next Week's | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Mental Health Strain | Burnout | Maladaptive Coping | |||||||
| Estimate | SE | t | Estimate | SE | t | Estimate | SE | t | |
| Intercept | 0.06 | 0.07 | 0.8 | 0.3 | 0.05 | 6.33** | 0.5 | 0.06 | 8.49** |
| Time | 0 | 0 | 1.96* | 0 | 0 | 2.26* | 0 | 0 | 2.29* |
| Prior Week | 0.88 | 0.02 | 55.07** | 0.81 | 0.02 | 43.60** | −0.05 | 0.03 | −2.28* |
| Moral Distress | 0.06 | 0.02 | 3.09** | 0.04 | 0.01 | 3.43** | −0.02 | 0.01 | −1.51 |
| Patient Status | 0.18 | 0.02 | 1.09 | −0.09 | 0.1 | −1.01 | 0.1 | 0.13 | 0.78 |
| MD × PS | −0.02 | 0.06 | −0.35 | 0.07 | 0.04 | 2.16* | 0.01 | 0.04 | 0.38 |
Prior week refers to measurement of the criterion that was assessed the week before moral distress and the criterion were measured (e.g. ‘The previous week's mental health strain’). MD × PS refers to the interaction term of moral distress*patient status. *P < 0.05; **P < 0.01.
Fig. 2.
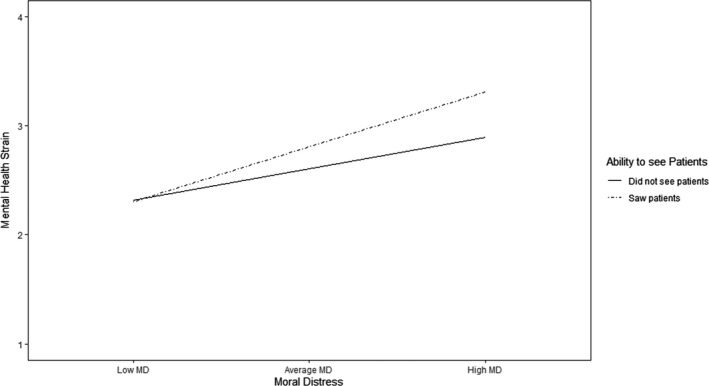
The interaction between moral distress and the ability to see patients predicting the same week's mental health strain after controlling for the prior week's stain.
Additionally, the ability to see patients moderated the relationship between moral distress and burnout. After controlling for the previous week's burnout and main effects, the interaction between seeing patients and moral distress was significant in predicting the current week's burnout and the following week's burnout. Simple slope analyses revealed that the relationship predicting burnout in a given week was significant for both those seeing patients (γ = 0.20, t = 5.55, P < 0.01) and those who were not able to see patients (γ = 0.09, t = 7.24, P < 0.01). Similarly, the interaction was significant in predicting next week's burnout for those who were able to see patients (γ = 0.11, t = 3.37, P < 0.01), and those who were not able to see patients (γ = 0.04, t = 3.45, P < 0.01). The relationship between moral distress and both weeks' burnout was stronger for those seeing patients than those who were not (See Figs 3 and 4).
Fig. 3.
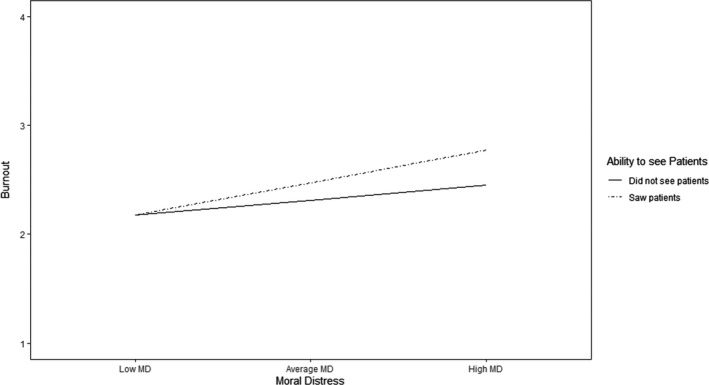
The interaction between moral distress and the ability to see patients predicting the same week's burnout after controlling for the prior week's strain.
Fig. 4.
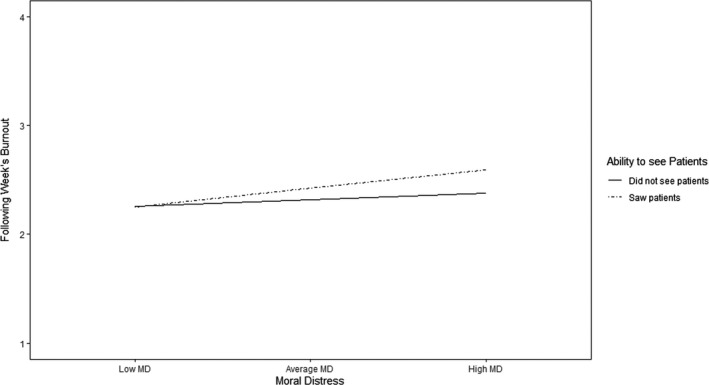
The interaction between moral distress and the ability to see patients predicting the following week's burnout after controlling for the prior week's burnout.
The interaction between moral distress and the ability to see patients was not a significant predictor of maladaptive coping. Seeing patients did not moderate the relationship between moral distress and predicting the current week's maladaptive coping or the following week's maladaptive coping after controlling for the prior week's maladaptive coping.
Discussion
While popular press articles have speculated over the long‐term psychological effects of COVID‐19 on healthcare workers (e.g. Angelos 2020; Cabarkapa et al. 2020; Cacchione 2020; Dunham et al. 2020; White & Lo 2020), little research to date has demonstrated the impact of moral distress over the course of the pandemic. While recent studies have reported the rates of moral distress among frontline workers (e.g. Donkers et al. 2021; Miljeteig et al. 2021; Plouffe et al. 2021), few have been able to capture the trends in moral distress beyond a single time point (Hines et al. 2021; Kok et al. 2021). The current study provides empirical data to demonstrate the prevalence of moral distress on a weekly basis over the course of 23 weeks.
The results revealed that weekly moral distress predicted both the current week's mental health strain (Hypothesis 2) and burnout (Hypothesis 3) over time. The findings remained significant even after controlling for the previous week's outcomes. The results support previous theory that moral distress can have cumulative effects (Epstein & Hamric 2009), such that even after controlling for the prior week's outcomes, endorsement of moral distress predicted increased mental health strain and burnout each week. These findings extend the work of previous researchers who have found that moral distress was a significant predictor of burnout, depression, anxiety, and PTSD (Kok et al. 2021; Plouffe et al. 2021).
The current study also sheds light on those who were unable to provide care during the pandemic. Reports from massage therapists, dentists, and acupuncturists, indicate that frontline healthcare providers were not alone and that moral distress is an industry‐wide experience. These findings support prior research stating that all healthcare‐related fields experience moral distress to some degree (ffrench‐O'Carroll et al. 2021; Whitehead et al. 2015). The current study expands the literature on moral distress to include the perspective of those providers who were unable to provide care during the pandemic. Although the causes for moral distress may differ between providers who were able to see patients and those who were not, the impact on mental health and burnout is notable. Initial analyses indicated that there was no significant difference in the general experience of moral distress between providers who were able and providers who were unable to see patients. In other words, on average, healthcare workers who were not seeing patients reported statistically similar ratings of moral distress to those who were on the frontlines. While some providers exhibited symptoms due to the inability help their patients directly, other providers who are unable to see patients exhibited symptoms through the guilt of feeling responsible for the patient's hindered recovery (Covert 2021; Rodger 2020). This finding is novel in that the pandemic has provided a unique circumstance where some providers were unable to continue their work, despite feeling as though they should be (Covert 2021; Rodger 2020).
While the average moral distress values did not differ overall, weekly reports of mental health strain and burnout were significantly impacted by the ability to see patients. The interaction between moral distress and the ability to see patients demonstrated that seeing patients magnified the relationships between moral distress and the outcomes of mental health strain and burnout (Hypothesis 4). The results indicated that providers who were directly seeing patients each week experienced increased rates of moral distress compared to those who were not seeing patients. These results contrast the findings from other researchers who found that those not on the frontline had higher frequency of burnout (Wu et al. 2020), higher prevalence of anxiety (Tan et al. 2020), and vicarious traumatization (Li et al. 2020) than those on the frontline. The current sample included workers who were not on the frontline and unable to go into their workplaces, whereas the prior research included providers who were actively seeing patients in non‐COVID‐19 units. Future research is needed to investigate this area further.
Moral distress was a significant predictor of next week's burnout but not mental health strain in the lagged effects model. This finding was distinctive in that mental health strain tends to be a precursor to burnout symptoms. The researchers rationalize these findings in that the mental health items tend to inquire about general mental states, whereas the burnout item specifically refers to at work emotions and experiences. It is likely that because moral distress refers to specific situations at work, this would be a stronger predictor of other work‐related indices.
Despite significant correlations between moral distress and maladaptive coping in the between‐subjects analysis, when examining the relationships within‐persons, moral distress was not a significant predictor of maladaptive coping (Hypothesis 3). Moral distress did not influence whether individuals used alcohol, tobacco, or drugs. These results are surprising as previous work has suggested that strain and burnout can increase maladaptive health behaviours (Cunradi et al. 2003; Shepherd et al. 2019). However, ffrench‐O'Carroll et al. (2021) found that there was low use of substance abuse within their sample of participants, but did find that those who reported increased moral distress and use of maladaptive coping strategies were predictive of PTSD risk. Shepherd et al. (2019) found that while emotional demands were predictive of drinking behaviours, the relationship was contingent on the level of psychological detachment from work during non‐work time suggesting that recovery experiences were important to mitigate the use of alcohol. Thus, the relationship between moral distress and maladaptive coping may be offset by other coping mechanisms.
The current study expanded the literature of moral distress to those who are unable to work and contribute their skillset to helping their patients. Previous research has examined workers, at work. During ‘normal’ operation, these limitations make sense; however, due to national closures and restrictions imposed by government and professional organizations, those who were unable to see patients due to various circumstances are important to consider. Employees, whether furloughed or taking a step down due to personal concerns, can still experience adverse effects that have implications for when they return to work. Future research should evaluate the impact of the inability to see patients on providers' mental health as they return to work as the pandemic comes to an end.
Relevance for clinical practice
Moral distress is an inevitable by‐product of patient care, and while it cannot be eliminated completely from the work environment, there are some strategies organizations can utilize to mitigate the negative effects such as burnout (Cabarkapa et al. 2020; Morley et al. 2020; Vig 2021). Plouffe et al. (2021) found that workplace resource adequacy, positive work life impact, managerial and organizational leadership, and perceptions of an ethical work environment were associated with decreased ratings of moral distress for healthcare workers during the pandemic. The researchers also found that moral distress was positively related to COVID‐19 risk perception.
Leaders can monitor the workplace climate to acknowledge ethical concerns and the treatment of those individuals who are struggling. Being preventative and proactive in addressing situations of moral distress can reduce the presence and impact of moral distress on employees. One strategy is to implement peer support programs (Benishek et al. 2020; Helmers et al. 2020). Morley et al. (2020) noted that the repeated nature of moral distress can occur across a work team, and through active listening, providing resources and transparency in work design changes to help employees could foster a psychologically safe work environment among their team members. Moral Distress Reflective Dialogues and Debriefs (MDRD) and Caring for Caregivers are some of the professional resources facilitated through experts to provide caregivers a safe space to reflect on moral events. Similarly, Davis and Batcheller (2020) tested these strategies in an intervention where the authors proposed a ‘resiliency bundle’ that incorporated a multifaceted approach which was shown to statistically increase group resilience and decrease moral distress. Researchers and practitioners must provide healthcare workers with awareness of moral distress and provide the support needed to counter these occurrences. Future research must examine whether these evidence‐based strategies apply to providers who are not on the frontlines (Tan et al. 2020).
Additionally, organizations may not be responsible for preventing healthcare providers from working during regular operations, however, managers should consider ways to keep employees involved, provide training (to transfer), and prepare employees to come back as soon as possible in order to diminish the long‐term effects of moral distress for their employees. While the pandemic shutdowns have been a nuanced experience, other events like natural disasters could simulate similar occurrences where employees are unable to provide care as they normally would.
Limitations and future directions
While the current study addressed gaps in the literature, it did not go without limitations. First, the single‐item assessment of moral distress may have contributed to a limited scope of the construct. Although this was a validated measure, the reported moral distress could have been improved by asking specific situations where moral distress occurred and the degree to which distress was felt. Future research should examine whether these dimensions expand understanding of the proposed relationships; knowing what types of situations cause moral distress for which professions could provide insight into the resources and interventions needed to mitigate the effects of moral distress. Additionally, research often refers to moral distress and moral injury interchangeably; however, the current study intentionally focused on moral distress. Participants may have been more affected by moral injury during the pandemic due to the large amount of pain and suffering that was witnessed, and, thus, future research should evaluate whether the relationships found in the current study are strengthened for moral injury.
Our main research question aimed to assess how the relationship between moral distress and the study outcomes would be affected by the provider's ability to see patients during the pandemic. In many industries, such as retail and food, employees have been in and out of operation due to local guidelines. However, it was unclear whether similar fluctuations would apply to healthcare professionals. While hospital and clinical practices may be less likely to have these changes, professions, such as massage therapists, dentist and others, were likely to be caught in the yo‐yo effect of operations. However, initial analysis indicated that the majority of the sample maintained the same patient status throughout the study collection period. Because there was no within‐person variability in the patient status variable, it was treated as a Level 2 variable, analysing how differences between providers in the ability to see patients affected the relationships between moral distress and the study outcomes. This approach reduced the sample size for analyses involving the ability to see patient variables, which likely reduced the power to detect significant effects.
Finally, the participant sample was not evenly distributed across professional specialities. While the goal of the study was to be inclusive of all regions and occupations, the methods relied on convenience sampling. Participants were recruited through online social media engagement, radio interviews, professional listservs, or word of mouth. The reliance of self‐selection into the study may have led to bias in our sample. Future research should seek out ways to engage a randomized group of individuals from evenly represented specialities.
Conclusion
Previous research has provided vast evidence of the frequency and effects of moral distress for healthcare providers under normal circumstances. However, during the COVID‐19 pandemic, many workers experienced new situations that compromised a worker's sense of right and wrong. The current study demonstrated that moral distress increased provider's mental health strain and burnout symptoms and this was stronger for those seeing patients. The present study contributes to the growing body of literature demonstrating the impact of COVID‐19 on healthcare workers who are not directly treating COVID‐19 patients (ffrench‐O'Carroll et al. 2021; Tan et al. 2020). The findings of this study demonstrate the need for organizations to provide care for those who are caring.
Data Availability Statement
This study contains data from a larger on‐going study, and thus the data is not yet publicly available. A subset of the data including only the variables in this study can be made available by contacting the corresponding author.
Acknowledgements
The project has been partially funded by a seed grant from the Prisma Health System. This study is part of a larger project which includes a number of other researchers and research assistants and all need to be thanked for their contributions to Project COPE: Chronicling healthcare prOviders' Pandemic Experiences. Those individuals include: Niki Munk, PhD, LMT from IUPUI; Shannon Stark Taylor, PhD from Prisma Health; Sarah Griffin, MHD, PhD from Clemson University; Molly Benedum, MD from Appalachian Regional Healthcare System; Marissa Shuffler, PhD from Clemson University; Rebecca Russ‐Sellers PhD from University of South Carolina School of Medicine Greenville; Kendal Dean from University of South Carolina School of Medicine Greenville; Kemi Balogun from University of South Carolina School of Medicine Greenville.
Declaration of conflict of interest: All authors have certified that they have no affiliations with or involvement in any organization or entity with any financial interest in the subject matter or materials discussed in this manuscript.
Funding Statement: The project has been partially funded by a seed grant from the Prisma Health System.
Authorship Statement: Chloe Wilson: Conceptualization, Methodology, Investigation, Data Curation, Formal analysis, Writing – Original Draft. Hannah Metwally: Resources, Visualization. Smith Heavner: Conceptualization, Investigation, Methodology, Supervision. Ann Blair Kennedy: Conceptualization, Investigation, Writing – Review & Editing, Methodology, Supervision. Thomas W. Britt: Conceptualization, Methodology, Writing ‐ Review & Editing.
References
- American Massage Therapy Association . (2020). Massage Therapy Industry Fact Sheet | AMTA. American Massage Therapy Association. [Cited 7 July 2021]. Available from: URL: https://www.amtamassage.org/publications/massage‐industry‐fact‐sheet/
- Ando, M. & Kawano, M. (2018). Relationships among moral distress, sense of coherence, and job satisfaction. Nursing Ethics, 25 (5), 571–579. 10.1177/0969733016660882 [DOI] [PubMed] [Google Scholar]
- Angelos, P. (2020). Surgeons, ethics, and COVID‐19: Early lessons learned. Journal of the American College of Surgeons, 230 (6), 1119–1120. 10.1016/j.jamcollsurg.2020.03.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asgari, S. , Shafipour, V. , Taraghi, Z. & Yazdani‐Charati, J. (2019). Relationship between moral distress and ethical climate with job satisfaction in nurses. Nursing Ethics, 26 (2), 346–356. 10.1177/0969733017712083 [DOI] [PubMed] [Google Scholar]
- Austin, C.L. , Saylor, R. & Finley, P.J. (2017). Moral distress in physicians and nurses: Impact on professional quality of life and turnover. Psychological Trauma: Theory, Research, Practice, and Policy, 9 (4), 399–406. 10.1037/tra0000201 [DOI] [PubMed] [Google Scholar]
- Azoulay, E. , Cariou, A. , Bruneel, F. et al. (2020). Symptoms of anxiety, depression, and peritraumatic dissociation in critical care clinicians managing patients with COVID‐19. A Cross‐Sectional Study. American Journal of Respiratory and Critical Care Medicine, 202 (10), 1388–1398. 10.1164/rccm.202006-2568OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barello, S. , Palamenghi, L. & Graffigna, G. (2020). Stressors and resources for healthcare professionals during the Covid‐19 pandemic: Lesson Learned From Italy. Frontiers in Psychology, 11, 2179. 10.3389/fpsyg.2020.02179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benishek, L.E. , Kachalia, A. , Daugherty Biddison, L. & Wu, A.W. (2020). Mitigating health‐care worker distress from scarce medical resource allocation during a public health crisis. Chest, 158 (6), 2285–2287. 10.1016/j.chest.2020.07.073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bliese, P.D. (2016). Multilevel modelling in R (2.6). A Brief Introduction to R, the Multilevel Package and the Nlme Package.
- Bliese, P.D. , Maltarich, M.A. & Hendricks, J.L. (2018). Back to basics with mixed‐effects models: Nine take‐away points. Journal of Business and Psychology, 33 (1), 1–23. 10.1007/s10869-017-9491-z [DOI] [Google Scholar]
- Butler, C.R. , Wong, S.P. , Wightman, A.G. & O'Hare, A.M. (2020). US clinicians' experiences and perspectives on resource limitation and patient care during the COVID‐19 pandemic. Journal of American Medicine Association Network Open, 3 (11), e2027315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cabarkapa, S. , Nadjidai, S.E. , Murgier, J. & Ng, C.H. (2020). The psychological impact of COVID‐19 and other viral epidemics on frontline healthcare workers and ways to address it: A rapid systematic review. Brain, Behavior, & Immunity ‐ Health, 8, 100144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cacchione, P.Z. (2020). Moral distress in the midst of the COVID‐19 pandemic. Clinical Nursing Research, 29 (4), 215–216. 10.1177/1054773820920385 [DOI] [PubMed] [Google Scholar]
- Cai, H. , Tu, B. , Ma, J. et al. (2020). Psychological impact and coping strategies of frontline medical staff in Hunan between January and March 2020 during the outbreak of coronavirus disease 2019 (COVID‐19) in Hubei, China. Medical Science Monitor: International Medical Journal of Experimental and Clinical Research, 26, e924171–e924181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carver, C.S. (1997). You want to measure coping but your protocol's too long: Consider the brief cope. International Journal of Behavioral Medicine, 4 (1), 92–100. [DOI] [PubMed] [Google Scholar]
- Corley, M.C. (2002). Nurse moral distress: A proposed theory and research agenda. Nursing Ethics, 9 (6), 636–650. 10.1191/0969733002ne557oa [DOI] [PubMed] [Google Scholar]
- Covert, B. (2021). ‘They Just Feel That They've Been Violated.’ The Atlantic. [Cited 7 December 2021]. Available from: URL: https://www.theatlantic.com/health/archive/2021/04/the‐pandemic‐broke‐americas‐health‐care‐workers/618600/
- Cunradi, C.B. , Greiner, B.A. , Ragland, D.R. & Fisher, J.M. (2003). Burnout and alcohol problems among urban transit operators in San Francisco. Addictive Behaviors, 28 (1), 91–109. 10.1016/S0306-4603(01)00222-2 [DOI] [PubMed] [Google Scholar]
- Daubman, B.R. , Black, L. & Goodman, A. (2020). Recognizing moral distress in the COVID‐19 pandemic: Lessons from global disaster response. Journal of Hospital Medicine, 15 (11), 696–698. [DOI] [PubMed] [Google Scholar]
- Davis, M. & Batcheller, J. (2020). Managing moral distress in the workplace: Creating a resiliency bundle. Nurse Leader, 18 (6), 604–608. 10.1016/j.mnl.2020.06.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Demerouti, E. , Bakker, A.B. , De Jonge, J. , Janssen, P.P. & Schaufeli, W.B. (2001). Burnout and engagement at work as a function of demands and control. Scandinavian Journal of Work, Environment & Health, 279–286. [DOI] [PubMed] [Google Scholar]
- Dolan, E.D. , Mohr, D. , Lempa, M. et al. (2015). Using a single item to measure burnout in primary care staff: A psychometric evaluation. Journal of General Internal Medicine, 30 (5), 582–587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dormann, C. & Griffin, M.A. (2015). Optimal time lags in panel studies. Psychological Methods, 20 (4), 489. [DOI] [PubMed] [Google Scholar]
- Donkers, M.A. , Gilissen, V.J.H.S. , Candel, M.J.J.M. , van Dijk, N.M. , Kling, H. , Heijnen‐Panis, R. , Pragt, E. , van der Horst, I. , Pronk, S.A. & van Mook, W.N.K.A. (2021). Moral distress and ethical climate in intensive care medicine during COVID‐19: A nationwide study. BMC Medical Ethics, 22 (1), 73. 10.1186/s12910-021-00641-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dryden‐Palmer, K. , Moore, G. , McNeil, C. et al. (2020). Moral distress of clinicians in Canadian pediatric and neonatal ICUs. Pediatric Critical Care Medicine, 21 (4), 314–323. [DOI] [PubMed] [Google Scholar]
- Dunham, A.M. , Rieder, T.N. & Humbyrd, C.J. (2020). A bioethical perspective for navigating moral dilemmas amidst the COVID‐19 pandemic. The Journal of the American Academy of Orthopaedic Surgeons, 28, 471–476. 10.5435/JAAOS-D-20-00371 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dyrbye, L.N. , Satele, D. , Sloan, J. & Shanafelt, T.D. (2013). Utility of a brief screening tool to identify physicians in distress. Journal of General Internal Medicine, 28 (3), 421–427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elpern, E.H. , Covert, B. & Kleinpell, R. (2005). Moral distress of staff nurses in a medical intensive care unit. American Journal of Critical Care, 14 (6), 523–530. 10.4037/ajcc2005.14.6.523 [DOI] [PubMed] [Google Scholar]
- Epstein, E.G. & Hamric, A.B. (2009). Moral distress, moral residue, and the crescendo effect. Journal of Clinical Ethics, 20 (4), 330–342. [PubMed] [Google Scholar]
- Fernandez‐Parsons, R. , Rodriguez, L. & Goyal, D. (2013). Moral distress in emergency nurses. Journal of Emergency Nursing, 39 (6), 547–552. 10.1016/j.jen.2012.12.009 [DOI] [PubMed] [Google Scholar]
- ffrench‐O'Carroll, R. , Feeley, T. , Tan, M.H. et al. (2021). Psychological impact of COVID‐19 on staff working in paediatric and adult critical care. British Journal of Anaesthesia, 126 (1), e39–e41. 10.1016/j.bja.2020.09.040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher, G.G. , Matthews, R.A. & Gibbons, A.M. (2016). Developing and investigating the use of single‐item measures in organizational research. Journal of Occupational Health Psychology, 21 (1), 3–23. 10.1037/a0039139 [DOI] [PubMed] [Google Scholar]
- Fumis, R.R.L. , Junqueira Amarante, G.A. , de Fátima Nascimento, A. & Vieira Junior, J.M. (2017). Moral distress and its contribution to the development of burnout syndrome among critical care providers. Annals of Intensive Care, 7 (1), 71. 10.1186/s13613-017-0293-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gabler, E. , Montague, Z. & Ashford, G. (2020). During a pandemic, an unanticipated problem: Out‐of‐work health workers. The New York times. [Cited 12 September 2020]. Available from: URL: https://www.nytimes.com/2020/04/03/us/politics/coronavirus‐health‐care‐workers‐layoffs.html
- Godshall, M. (2021). Coping with moral distress during COVID‐19. Nursing 2021, 51 (2), 55–58. [DOI] [PubMed] [Google Scholar]
- Haghighinezhad, G. , Atashzadeh‐Shoorideh, F. , Ashktorab, T. , Mohtashami, J. & Barkhordari‐Sharifabad, M. (2019). Relationship between perceived organizational justice and moral distress in intensive care unit nurses. Nursing Ethics, 26 (2), 460–470. [DOI] [PubMed] [Google Scholar]
- Hamric, A.B. & Epstein, E.G. (2017). A health system‐wide moral distress consultation service: Development and evaluation. HEC Forum, 29 (2), 127–143. [DOI] [PubMed] [Google Scholar]
- Heavner, S. , Stuenkel, M. , Russ‐Sellers, R. et al. (2021). “I Don't Want to Go to Work”: A Mixed Methods Analysis of Healthcare Worker Experiences from the Front‐ and Side‐Lines of COVID‐19. Unpublished Manuscript. [DOI] [PMC free article] [PubMed]
- Helmers, A. , Palmer, K.D. & Greenberg, R.A. (2020). Moral distress: Developing strategies from experience. Nursing Ethics, 27 (4), 1147–1156. 10.1177/0969733020906593 [DOI] [PubMed] [Google Scholar]
- Hesselink, G. , Straten, L. , Gallée, L. et al. (2021). Holding the frontline: A cross‐sectional survey of emergency department staff well‐being and psychological distress in the course of the COVID‐19 outbreak. BMC Health Services Research, 21 (1), 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hines, S.E. , Chin, K.H. , Glick, D.R. & Wickwire, E.M. (2021). Trends in moral injury, distress, and resilience factors among healthcare workers at the beginning of the COVID‐19 pandemic. International Journal of Environmental Research and Public Health, 18 (2), 488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hlubocky, F.J. , Symington, B.E. , McFarland, D.C. et al. (2021). Impact of the COVID‐19 pandemic on oncologist burnout, emotional well‐being, and moral distress: Considerations for the cancer organization's response for readiness, mitigation, and resilience. JCO Oncology Practice, 17 (2), 1–11. 10.1200/OP.20.00937 [DOI] [PubMed] [Google Scholar]
- Inglet, M. (2020). Some Boise healthcare workers laid off after COVID‐19 cuts back number of non‐emergency surgeries. Ktvb.Com. [Cited 7 June 2021]. Available from: URL: https://www.ktvb.com/article/news/health/coronavirus/some‐boise‐nurses‐laid‐off‐after‐covid‐19‐cuts‐back‐number‐of‐non‐emergency‐surgeries/277‐30c17b25‐3802‐4981‐96f5‐ac08e1fb4c67
- Jameton, A. (1984). Nursing Practice: The ethical issues. Englewood Cliffs, NJ: Prentice Hall. [Google Scholar]
- Jinkerson, J.D. (2016). Defining and assessing moral injury: A syndrome perspective. Traumatology, 22 (2), 122. [Google Scholar]
- Kok, N. , van Gurp, J. , Teerenstra, S. et al. (2021). Coronavirus disease 2019 immediately increases burnout symptoms in ICU professionals: A longitudinal cohort study. Critical Care Medicine, 49 (3), 419–427. [DOI] [PubMed] [Google Scholar]
- Kok, N. , Hoedemaekers, A. , van der Hoeven, H. , Zegers, M. & van Gurp, J. (2020). Recognizing and supporting morally injured ICU professionals during the COVID‐19 pandemic. Intensive Care Medicine, 46 (8), 1653–1654. 10.1007/s00134-020-06121-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kreh, A. , Brancaleoni, R. , Magalini, S.C. et al. (2021). Ethical and psychosocial considerations for hospital personnel in the Covid‐19 crisis: Moral injury and resilience. PLoS One, 16 (4), e0249609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kwok, O.‐M. , Underhill, A.T. , Berry, J.W. , Luo, W. , Elliott, T.R. & Yoon, M. (2008). Analyzing longitudinal data with multilevel models: An example with individuals living with lower extremity intra‐articular fractures. Rehabilitation Psychology, 53 (3), 370–386. 10.1037/a0012765 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lai, J. , Ma, S. , Wang, Y. et al. (2020). Factors associated with mental health outcomes among health care workers exposed to Coronavirus Disease 2019. Journal of the American Medical Association Network Open, 3 (3), e203976. 10.1001/jamanetworkopen.2020.3976 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levy, M. (2020). A mounting casualty of coronavirus crisis: Health care jobs. AP NEWS. [Cited 7 June 2021]. Available from: URL: https://apnews.com/article/financial‐markets‐us‐news‐ap‐top‐news‐pennsylvania‐virus‐outbreak‐811b2057ad110605fa70a2745e5e0ee4
- Li, Z. , Ge, J. , Yang, M. et al. (2020). Vicarious traumatization in the general public, members, and non‐members of medical teams aiding in COVID‐19 control. Brain, Behavior, and Immunity, 88, 916–919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liang, Y. , Chen, M. , Zheng, X. & Liu, J. (2020). Screening for Chinese medical staff mental health by SDS and SAS during the outbreak of COVID‐19. Journal of Psychosomatic Research, 133, 110102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKinnon, D.P. & Luecken, L.J. (2008). How and for whom? Mediation and moderation in health psychology. Health Psychology : Official Journal of the Division of Health Psychology, American Psychological Association, 27 (2 Suppl), S99. 10.1037/0278-6133.27.2(Suppl.).S99 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maslach, C. , Schaufeli, W.B. & Leiter, M.P. (2001). Job burnout. Annual Review of Psychology, 52 (1), 397–422. [DOI] [PubMed] [Google Scholar]
- McDermott, D. & Cox, C. (2020). What impact has the coronavirus pandemic had on healthcare employment? Peterson‐KFF Health System Tracker. https://www.healthsystemtracker.org/chart‐collection/what‐impact‐has‐the‐coronavirus‐pandemic‐had‐on‐healthcare‐employment/
- Meltzer, L.S. & Huckabay, L.M. (2004). Critical care nurses' perceptions of futile care and its effect on burnout. American Journal of Critical Care, 13 (3), 202–208. 10.4037/ajcc2004.13.3.202 [DOI] [PubMed] [Google Scholar]
- Miljeteig, I. , Forthun, I. , Hufthammer, H.O. , Engelund, I.E. , Schanche, E. , Schaufel, M. & Onarheim, K.H. (2021). Priority‐setting dilemmas, moral distress and support experienced by nurses and physicians in the early phase of the COVID‐19 pandemic in Norway. Nursing ethics, 28 (1), 66–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moletta, L. , Pierobon, E.S. , Capovilla, G. et al. (2020). International guidelines and recommendations for surgery during Covid‐19 pandemic: A systematic review. International Journal of Surgery, 79, 180–188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morley, G. , Sese, D. , Rajendram, P. & Horsburgh, C.C. (2020). Addressing caregiver moral distress during the COVID‐19 pandemic. Cleveland Clinic Journal of Medicine, 10.3949/ccjm.87a.ccc047 [DOI] [PubMed] [Google Scholar]
- Oh, Y. & Gastmans, C. (2015). Moral distress experienced by nurses: A quantitative literature review. Nursing Ethics, 22 (1), 15–31. 10.1177/0969733013502803 [DOI] [PubMed] [Google Scholar]
- Ohnishi, K. , Ohgushi, Y. , Nakano, M. et al. (2010). Moral distress experienced by psychiatric nurses in Japan. Nursing Ethics, 17 (6), 726–740. 10.1177/0969733010379178 [DOI] [PubMed] [Google Scholar]
- Papazoglou, K. & Chopko, B. (2017). The role of moral suffering (moral distress and moral injury) in police compassion fatigue and PTSD: An unexplored topic. Frontiers in Psychology, 8, 1999. 10.3389/fpsyg.2017.01999 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petrella, A.R. , Hughes, L. , Fern, L.A. et al. (2021). Healthcare staff well‐being and use of support services during COVID‐19: A UK perspective. General Psychiatry, 34 (3), e100458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piers, R.D. , Van den Eynde, M. , Steeman, E. , Vlerick, P. , Benoit, D.D. & Van Den Noortgate, N.J. (2012). End‐of‐life care of the geriatric patient and nurses' moral distress. Journal of the American Medical Directors Association, 13 (1), 80.e7–80.e13. 10.1016/j.jamda.2010.12.014 [DOI] [PubMed] [Google Scholar]
- Plouffe, R.A. , Nazarov, A. & Forchuk, C.A. et al. (2021). Impacts of morally distressing experiences on the mental health of Canadian health care workers during the COVID‐19 pandemic. Psychiatry and Clinical Psychology [preprint]. 10.1101/2021.04.06.21254800 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preti, E. , Di Mattei, V. , Perego, G. et al. (2020). The psychological impact of epidemic and pandemic outbreaks on healthcare workers: Rapid Review of the Evidence. Current Psychiatry Reports, 22 (8), 43. 10.1007/s11920-020-01166-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rathert, C. , May, D.R. & Chung, H.S. (2016). Nurse moral distress: A survey identifying predictors and potential interventions. International Journal of Nursing Studies, 53, 39–49. 10.1016/j.ijnurstu.2015.10.007 [DOI] [PubMed] [Google Scholar]
- Rodger, S. (2020). “Nurses are feeling guilty about not being at work.” Nursing Times. [Cited 7 December 2021]. Available from: URL: https://www.nursingtimes.net/opinion/sian‐rodger/nurses‐are‐feeling‐guilty‐about‐not‐being‐at‐work‐23‐03‐2020/
- Rosenwohl‐Mack, S. , Dohan, D. , Matthews, T. , Batten, J.N. & Dzeng, E. (2020). Understanding experiences of moral distress in end‐of‐life care among US and UK physician trainees: A comparative qualitative study. Journal of General Internal Medicine, 36 (7), 1890–1897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanchez‐Reilly, S. , Morrison, L.J. , Carey, E. et al. (2013). Caring for oneself to care for others: Physicians and their self‐care. The Journal of Supportive Oncology, 11 (2), 75–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Selig, J.P. & Little, T.D. (2012). Autoregressive and cross‐lagged panel analysis for longitudinal data. In: Laursen B., Little T.D. & Card N.A. (Eds). Handbook of Developmental Research Methods (pp. 265–278). United Kingdom: Guilford Publications: The Guilford Press. [Google Scholar]
- Sheather, J. & Fidler, H. (2021). Covid‐19 has amplified moral distress in medicine. BMJ, 372 (28), 1–2. 10.1136/bmj.n28 [DOI] [PubMed] [Google Scholar]
- Shepherd, B.R. , Fritz, C. , Hammer, L.B. , Guros, F. & Meier, D. (2019). Emotional demands and alcohol use in corrections: A moderated mediation model. Journal of Occupational Health Psychology, 24 (4), 438–449. 10.1037/ocp0000114 [DOI] [PubMed] [Google Scholar]
- Shirom, A. (2003). Job‐related burnout: A review. In J. C. Quick & L. E. Tetrick (Eds.), Handbook of occupational health psychology (pp. 245–264). American Psychological Association. 10.1037/10474-012 [DOI]
- Shrout, P.E. & Fleiss, J.L. (1979). Intraclass correlations: Uses in assessing rater reliability. Psychological Bulletin, 86 (2), 420. [DOI] [PubMed] [Google Scholar]
- Sugrue, E. (2019). Understanding the effect of moral transgressions in the helping professions: In search of conceptual clarity. Social Service Review, 93 (1), 4–25. 10.1086/701838 [DOI] [Google Scholar]
- Sundin‐Huard, D. & Fahy, K. (1999). Moral distress, advocacy and burnout: Theorizing the relationships. International Journal of Nursing Practice, 5 (1), 8–13. [DOI] [PubMed] [Google Scholar]
- Tan, B.Y. , Chew, N.W. , Lee, G.K. et al. (2020). Psychological impact of the COVID‐19 pandemic on health care workers in Singapore. Annals of Internal Medicine, 173 (4), 317–320. 10.7326/M20-1083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turale, S. , Meechamnan, C. & Kunaviktikul, W. (2020). Challenging times: Ethics, nursing and the COVID‐19 pandemic. International Nursing Review, 67 (2), 164–167. 10.1111/inr.12598 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vig, E.K. (2021). As the Pandemic Recedes, Will Moral Distress Continue to Surge? American Journal of Hospice and Palliative Medicine, 1–5. 10.1177/10499091211030456 [DOI] [PubMed] [Google Scholar]
- White, D.B. & Lo, B. (2020). A framework for rationing ventilators and critical care beds during the COVID‐19 pandemic. Journal of the American Medical Association, 323 (18), 1773. 10.1001/jama.2020.5046 [DOI] [PubMed] [Google Scholar]
- Whitehead, P.B. , Herbertson, R.K. , Hamric, A.B. , Epstein, E.G. & Fisher, J.M. (2015). Moral distress among healthcare professionals: Report of an institution‐wide survey. Journal of Nursing Scholarship, 47 (2), 117–125. [DOI] [PubMed] [Google Scholar]
- Wiener, L. , Rosenberg, A.R. , Pennarola, B. , Fry, A. & Weaver, M. (2021). Navigating the terrain of moral distress: Experiences of pediatric end‐of‐life care and bereavement during COVID‐19. Palliative & supportive care, 19 (2), 129–134. 10.1017/S1478951521000225 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williamson, V. , Murphy, D. & Greenberg, N. (2020). COVID‐19 and experiences of moral injury in front‐line key workers. Occupational Medicine, 70 (5), 317–319. 10.1093/occmed/kqaa052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson, C.A. (2021). Trauma or trapped: Conceptualizing moral suffering and the impact of occupational stigma. Available from Dissertations & Theses @ Clemson University; ProQuest Dissertations & Theses Global. (2539294698).
- Wolf, L.A. , Perhats, C. , Delao, A.M. , Moon, M.D. , Clark, P.R. & Zavotsky, K.E. (2016). “It's a burden you carry”: Describing moral distress in emergency nursing. Journal of Emergency Nursing, 42 (1), 37–46. 10.1016/j.jen.2015.08.008 [DOI] [PubMed] [Google Scholar]
- Wu, Y. , Wang, J. , Luo, C. et al. (2020). A comparison of burnout frequency among oncology physicians and nurses working on the frontline and usual wards during the COVID‐19 epidemic in Wuhan, China. Journal of Pain and Symptom Management, 60 (1), e60–e65. 10.1016/j.jpainsymman.2020.04.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiao, H. , Zhang, Y. , Kong, D. , Li, S. & Yang, N. (2020). The effects of social support on sleep quality of medical staff treating patients with coronavirus disease 2019 (COVID‐19) in January and February 2020 in China. Medical Science Monitor: International Medical Journal of Experimental and Clinical Research, 26, e923549–e923551. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
This study contains data from a larger on‐going study, and thus the data is not yet publicly available. A subset of the data including only the variables in this study can be made available by contacting the corresponding author.


