Abstract
Background
The COVID-19 pandemic has been highly disruptive for cancer care. Here, we examined the effect COVID-19 had on performance of the 62-day Cancer Waiting Time (CWT) target set by the National Health Service (NHS) in England.
Methods
Data were retrospectively obtained on COVID-19 hospitalisations and CWT for NHS hospitals in England (n = 121). We produced a ‘COVID-19 burden’ to describe the proportion of each provider’s beds occupied with COVID-19 patients. COVID-19 burden was examined against CWT performance for 1st April – 30th May 2020 (Wave 1), and 1st October – 30th November 2020 (Wave 2). Two-tailed Spearman correlations were used to identify relationships between COVID-19 burden and CWT performance amongst different referral (i.e., 2-week-wait (2 W W) and internal specialist) and tumour types. Significantly correlated variables were further examined using linear regression models.
Results
COVID-19 burden was negatively associated with the percentage of 2 W W pathway referrals that met the CWT target in Wave 1 (r= -0.30, p = 0.001) and Wave 2 (r= -0.21, p = 0.02). These associations were supported by the results from our linear regression models (B for wave 1: -0.71; 95 %CI: −1.03 to −0.40; B for wave 2: -0.38; 95 %CI: −0.68 to −0.07). No associations were found between COVID-19 burden and internal specialist referrals or tumour type.
Conclusion
Increased COVID-19 burden was associated with lower compliance with CWT targets amongst urgent referrals from primary care in England. This will likely be an ongoing issue due to the backlog of patients awaiting investigations and treatment.
Policy summary
As the number of cancer referrals improve, we highlight the need for changes to primary and secondary care to manage the backlog within cancer diagnostic services to alleviate the impact of COVID-19.
Keywords: COVID-19, Cancer care, NHS, Cancer waiting time
1. Background
The coronavirus SARS-CoV-2 (COVID-19) pandemic has had a profound impact on the management of cancer patients [1]. Healthcare organisations have made significant changes to their healthcare services aiming to face the challenges posed by the COVID-19 pandemic [2]. During the first wave of the pandemic starting in March 2020, national lockdowns were introduced across many countries across the globe to diminish exposure and reduce potential impact on health services, including the UK [3,4]. These guidelines lead to a decrease, or halting in some cases, of non-COVID-19 healthcare services including cancer care [5]. Real-world evidence has shown that the outbreak of the COVID-19 pandemic in March 2020 was followed by a substantial reduction in the number of overall cancer-related referrals [6,7]. In the UK, urgent primary care referrals for suspected cancers decreased by 56 % from March to April 2020, before increasing again throughout May to August, to then return to 2019 levels in September 2020 [7]. Delays in cancer referrals have also been reported in various other European countries, including Italy and France [[8], [9], [10], [11]]. Moreover, delays in cancer diagnoses and treatments have consistently been associated with poorer outcomes [4,12]. A recent meta-analysis by Hanna et al. found that a delay of even four weeks in cancer treatment was associated with significantly reduced survival rates [12].
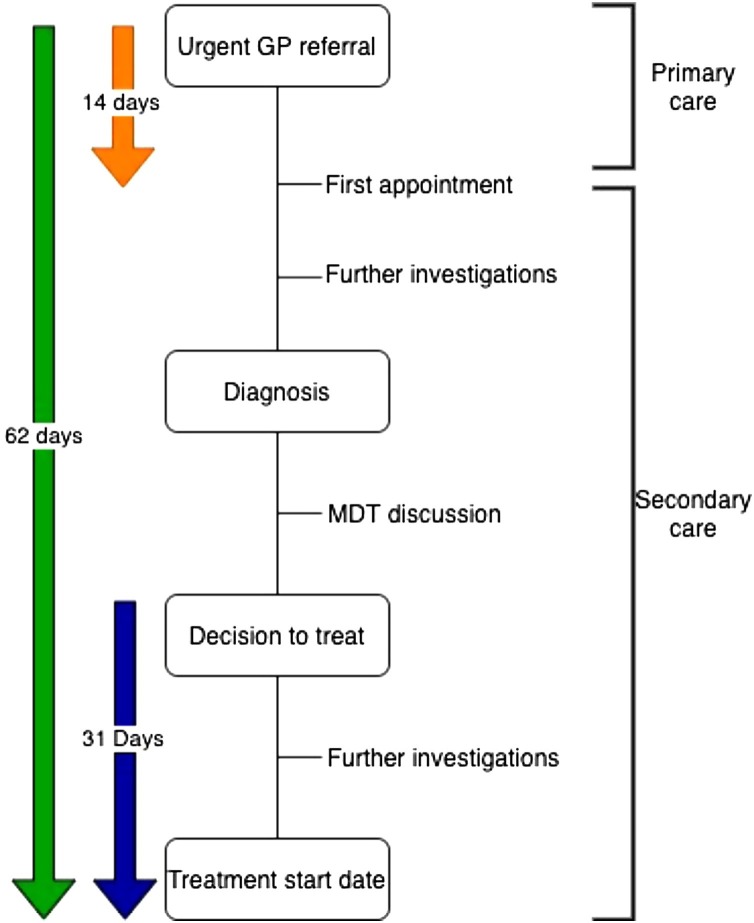
NHS England (NHSE) have provided a series of targets to support timely access to diagnostic and treatment services. These targets include the two week wait (2 W W) pathway, the 31-day target, and the 62-day Cancer Waiting Time (CWT). In the 2 W W pathway, patients are referred to a specialist by a general practitioner (GP) for further investigations and should have their first appointment within 14 days of referral. If a cancer is diagnosed, the case will be discussed at a Multi-disciplinary team (MDT, made up of a range of healthcare professionals) meeting, where a treatment decision will be made and presented to the patient. Once the specialist and patient have agreed on a treatment option (decision to treat), the treatment start date should be within a 31-day target. Lastly, all patients should receive treatment within 62-days of the initial referral date for a suspected cancer (Fig. 1 ) [13,14]. Furthermore, the COVID-19 pandemic has coincided with the lowest performance on this 62-day CWT target in the last 10 years, where 1 of 4 patients urgently referred from primary care between April 2020 and January 2021 did not receive treatment within 62 days [7]. However, no studies to our knowledge have looked at the definite effect a high COVID-19 burden within each hospital has had on its performance of the 62-day CWT target. In the current study we aimed to analyse the effect the COVID-19 pandemic has had on the provision of cancer services within a 62-day target.
Fig. 1.
Flowchart explaining the NHS two week wait (2 W W) pathway, the 31-day target, and the 62-day Cancer Waiting Time (CWT).
GP, general practitioner; MDT, multidisciplinary team.
2. Methods
2.1. Study design and data sources
The study had a retrospective, cross-sectional design which consisted of two separate analyses, each corresponding to the first and second waves of the COVID-19 pandemic in England. Data on daily number of patients in hospital for suspected COVID-19 were obtained for each individual NHS hospital trust in England, from Public Health England’s UK Coronavirus Dashboard [15], for two time periods within the first 2 waves of COVID-19: 1st April – 30th May 2020 (Wave 1), and 1st October – 30th November 2020 (Wave 2).
Data on CWT performance were obtained from NHS England, for all hospitals that reported this data, for June 2020 (Wave 1) and December 2020 (Wave 2). This approach was taken because we were interested in examining the burden of COVID-19 in the’ 62-day pathway’ from referral to treatment. The CWT performance metric used here therefore comprises the sum of the time taken to diagnose a cancer after referral, and the time taken to provide treatment from first suspicion of cancer [16].
Data were also obtained from NHS Digital on total overnight bed capacity for each hospital; and the percentage of patients seen by each provider that reside in geographical areas in the two most socially deprived quintiles (according to the Indices of Multiple Deprivation measure employed by the UK Government) [17]. Of 217 NHS hospital trusts in England in total, 131 hospital trusts delivered complete cancer-related care and thus, reported CWT data. Deprivation data were unavailable for 10 hospital trusts, and data on critical care bed capacity were unavailable for 1 provider, resulting in a sample of n = 120 hospitals.
2.2. COVID-19 burden
We produced a ‘COVID-19 burden’ metric to find an approximated average percentage of each NHS hospital trust’s capacity that was occupied by patients with suspected COVID-19. For each of the two waves, daily COVID-19 data were used to calculate the mean number of patients in hospital with suspected COVID-19 at each hospital, across the first two months (1st April – 30th May 2020 for Wave 1; 1st October – 30th November 2020 for Wave 2). This statistic was divided by each hospitals overall general/acute and critical care bed capacity [18].
2.3. Cancer treatment delays
For each NHS hospital trust, CWT data were obtained for:
-
•
2 W W pathway referrals (i.e., urgent GP referrals for suspected cancer)
-
•
Internal specialist referral (i.e. when another specialist decides that the patient should be seen for suspected cancer [19])
-
•
Breast cancer referrals
-
•
Lower gastrointestinal (GI) cancer referrals
-
•
Lung cancer referrals
-
•
Skin cancer referrals
-
•
Urological cancer referrals
-
•
Other cancer referrals (i.e., any other cancer not stated above)
2.4. Statistical analysis
Preliminary analyses using two-tailed Spearman correlations were undertaken to establish whether the size of the hospital (i.e., general/acute bed capacity plus critical care bed capacity), and the deprivation score of the hospital was associated with COVID-19 burden. These analyses showed that COVID-19 burden was positively associated with deprivation score. No associations were found with the size of NHS hospital trust. Therefore, all our subsequent analyses included models adjusted for deprivation score as a possible confounder.
For our main analysis, two-tailed Spearman correlations were first examined to determine whether COVID-19 burden during the first two months of each wave (i.e., 1st April – 30th May 2020for Wave 1, and 1st October – 30th November 2020 for Wave 2) was associated with cancer treatment delays in the third month of each wave (i.e. June 2020 for Wave 1, and December 2020 for Wave 2). These analyses were performed for each of the following CWT metrics: 2 W W pathway referrals, and internal specialist referrals. In addition, we performed stratified analyses by cancer type including breast, lower GI, lung, skin, urological, and other cancer referrals. As the onset of the epidemic was accompanied by sharp decreases in referrals, correlations were also performed for the association between local COVID-19 burden and the total number of patients receiving cancer treatment locally.
Due to significant findings in our current study, correlations between COVID-19 burden and CWT performance at the p < 0.1 level were further examined using linear regression models. This was done to quantify associative relationships between COVID-19 burden and cancer treatment delays. For models examining all 2 W W referrals, separate linear regression models were constructed that included: 1) all NHS hospital trusts; 2) only those hospital trusts with >5% COVID-19 burden; and 3) only those hospital trusts with >10 % COVID-19 burden.
3. Results
3.1. Main analysis (Two-tailed spearman correlations)
Correlations between hospital-level COVID-19 burden and i) total number of treatments (i.e., overall, not only within the 62-day CWT), and ii) percentage treated within 62 days of suspected cancer referral (CWT target), for 2 W W pathway referrals and internal specialist referrals, for both Wave 1 and Wave 2 of the COVID-19 epidemic in England are summarized in Table 1 . An increased COVID-19 burden was associated with a lower percentage of 2 W W pathway referrals (i.e., urgent GP referrals for suspected cancer) treated within 62 days of cancer referral in both Wave 1 (r= -0.30, p = 0.001) and Wave 2 (r= -0.21, p = 0.02). High COVID-19 burden was also associated with a decrease in the total number of 2 W W pathway referrals treated (i.e., patients treated overall, not only within the 62-day CWT) within Wave 1 (r= -0.39, p < 0.001), no significant associations were found in Wave 2. When looking at internal specialist referrals (i.e., when another specialist decides that the patient should be seen for suspected cancer), no associations were found between the percentage of referrals meeting the 62-day CWT target and COVID-19 burden. However, an increased COVID-19 burden was associated with an increase in the total number of patients treated overall (i.e., not only within 62-day CWT) in both Wave 1 (r = 0.21, p = 0.03) and Wave 2 (r = 0.20, p = 0.03).
Table 1.
Correlations between provider-level COVID-19 burden and i) total number of treatments, and ii) percentage treated within 62 days of suspected cancer referral, for 2 week-wait (2 W W) referrals and internal specialist referrals, for both Wave 1 and Wave 2 of the COVID-19 epidemic in England.
| Total number treated |
Proportion treated within 62-day CWT target |
|||||
|---|---|---|---|---|---|---|
| NHS hospital trusts (n) | r | p-value | NHS hospital trusts (n) | r | p-value | |
| Wave 1 | ||||||
| 2 W W pathway referrals | ||||||
| 120 | −0.39 | <0.001 | 121 | −0.30 | 0.001 | |
| Internal specialist referral | ||||||
| 115 | 0.21 | 0.03 | 116 | 0.07 | 0.44 | |
| Wave 2 | ||||||
| 2 W W pathway referrals | ||||||
| 120 | −0.14 | 0.13 | 120 | −0.21 | 0.02 | |
| Internal specialist referral | ||||||
| 116 | 0.20 | 0.03 | 116 | −0.14 | 0.14 | |
NHS, National Health System; 2 W W, 2 week-wait; CWT, Cancer Waiting Time.
Moreover, after performing stratified analyses by tumour type, we found that an increase in COVID-19 burden was linked to an decrease in the total number of patients treated during Wave 1 across all tumour types (i.e., breast, lower GI, lung, skin, urological, and ‘other’ tumour sites). No other significant associations were found by tumour type (Table 2 ).
Table 2.
Correlations between provider-level COVID-19 burden and i) total number of treatments, and ii) percentage treated within 62 days of suspected cancer referral, for breast, lower gastrointestinal, lung, skin, urological, or other cancers for both Wave 1 and Wave 2 of the COVID-19 epidemic in England.
| Total number treated |
Proportion treated within 62-day CWT target |
|||||
|---|---|---|---|---|---|---|
| NHS hospital trusts (n) | r | p-value | NHS hospital trusts (n) | r | p-value | |
| Wave 1 | ||||||
| Breast | ||||||
| 115 | −0.25 | <0.01 | 115 | 0.03 | 0.78 | |
| Lower GI | ||||||
| 117 | −0.25 | <0.01 | 117 | −0.11 | 0.22 | |
| Lung | ||||||
| 116 | −0.32 | 0.001 | 116 | −0.09 | 0.36 | |
| Skin | ||||||
| 110 | −0.43 | <0.001 | 110 | −0.17 | 0.08 | |
| Urological | ||||||
| 120 | −0.29 | 0.001 | 120 | −0.09 | 0.34 | |
| Other tumour sites | ||||||
| 120 | −0.22 | 0.02 | 120 | −0.17 | 0.06 | |
| Wave 2 | ||||||
| Breast | ||||||
| 117 | 0.01 | 0.98 | 117 | 0.08 | 0.38 | |
| Lower GI | ||||||
| 120 | −0.13 | 0.17 | 120 | −0.13 | 0.15 | |
| Lung | ||||||
| 116 | −0.05 | 0.57 | 116 | 0.06 | 0.55 | |
| Skin | ||||||
| 113 | −0.19 | 0.05 | 113 | 0.05 | 0.59 | |
| Urological | ||||||
| 118 | −0.07 | 0.43 | 118 | −0.10 | 0.27 | |
| Other tumour sites | ||||||
| 120 | −0.11 | 0.23 | 120 | −0.25 | <0.01 | |
NHS, National Health System; CWT, Cancer Waiting Time; GI, gastrointestinal.
3.2. Secondary analysis (linear regression)
Results of further analyses using linear regression examining the associations between COVID-19 burden and the 62-day CWT target for 2 W W pathway referrals are shown in Table 3 . A high COVID-19 burden at hospital level was associated with a decline in the proportion of 2 W W pathway referrals (i.e., urgent GP referrals for suspected cancer) treated within the 62-day target during Wave 1 (B: -0.71; 95 %CI: −1.03 to −0.40) and Wave 2 (B: -0.38; 95 %CI: −0.68 to −0.07). Models examining the association between absolute numbers of patients treated within the target (adjusted for total of patients treated) also showed that an increased COVID-19 burden was associated with a decrease in the number of patients treated within the 62-day CWT target in both waves. The association appeared to be stronger in the analyses which only included hospitals who had a higher COVID-19 burden (i.e., >5 and >10 % COVID-19 burden) in both waves except for those NHS hospital trusts with only >10 % COVID-19 burden in wave 2 where no significant association was found. For instance, the B statistic in the regression models represents the difference in CWT performance when COVID-19 burden is increased by 1 absolute percentage point. Thus, hospitals with only 5% COVID-19 burden were associated with a 3.6 % absolute decrease in referrals meeting the 62-day target in wave 1; and a 1.9 % absolute decrease in wave 2.
Table 3.
Linear regression models depicting associations between local COVID-19 burden, and compliance with the 62-day Cancer Waiting Times (CWT) target amongst 2 W W pathway referral, for both Wave 1 and Wave 2 of the COVID-19 epidemic in England. 2 W W, 2-week-wait; CWT, cancer Waiting Times; n, number. * Adjusted for total number treated.
| NHS hospital trusts (n) | Total number of patients treated per hospital trust | Proportion treated within 62-day CWT target |
Number treated in target* |
|||
|---|---|---|---|---|---|---|
| Median (range) | B | 95 % CI | B | 95 % CI | ||
| Wave 1 | ||||||
| 2 W W pathway referrals: All treatments | ||||||
| All hospital trusts | 120 | 70 (15 ‒ 211.5) | −0.71 | (-1.03‒-0.40) | −0.50 | (-0.77‒-0.23) |
| Mean COVID burden >5% only | 113 | −0.76 | (-1.11‒-0.41) | −0.55 | (-0.86‒-0.25) | |
| Mean COVID burden >10 % only | 79 | −1.04 | (-1.55‒-0.54) | −0.61 | (-1.00‒-0.22) | |
| Wave 2 | ||||||
| 2 W W pathway referrals: All treatments | ||||||
| All providers | 120 | 97 (13.5 ‒ 231) | −0.38 | (-0.68‒-0.07) | −0.50 | (-0.88‒-0.13) |
| Mean COVID burden >5% only | 86 | −0.53 | (-0.94‒-0.13) | −0.71 | (-1.21‒-0.22) | |
| Mean COVID burden >10 % only | 45 | 0.14 | (-0.71‒0.98) | −0.30 | (-1.30‒0.71) | |
2WW, 2 week-wait; NHS, National Health System; CWT, Cancer Waiting Time; CI, confidence interval.
4. Discussion
The results from our analyses have shown that a high local COVID-19 burden was associated with lower compliance with CWT targets amongst 2 W W pathway referrals. These urgent referrals from primary care comprised most of the suspected cancer caseload, during both waves of the COVID-19 pandemic in England. When looking at internal specialist referrals (i.e. when another specialist decides that the patient should be seen for suspected cancer), no significant associations were found between compliance with CWT targets and COVID-19 burden. Our results also indicate that although 62-day CWT performance was not affected by a high COVID-19 burden for various tumour types, we did observe a decrease in total number of patients treated during the first wave of COVID-19.
The analysis presented here is consistent with the anecdotal experiences of many clinicians working in England’s NHS, in which cancer diagnostics and treatments for some patients have had to be delayed due to safety and capacity issues arising from the SARS-CoV-2 epidemic. Quantifying this impact serves as an important step in understanding the effects of the pandemic on cancer services.
From the beginning of the pandemic, essential cancer diagnostic services were suspended or operating at reduced capacity due to both the risk of exposure to COVID-19 and the redeployment of staff towards the management of patients with COVID-19 [20]. From June 2020, these services re-initiated their activities with continued substantial delays in routine and rapid referral pathways (i.e., 2-week-wait pathways). The findings of a decrease in the proportion of patients treated within the 62-day week target amongst urgent referrals from primary care in both COVID-19 waves in the current study, is consistent with both the anecdotal experiences of many clinicians working in England’s NHS, and previous epidemiological studies [6,21,22].
As previously mentioned, various publications have found that delays in cancer treatments of even 4 weeks are associated with inferior outcomes, including two modelling studies which have found significant increase in deaths due to cancer up to 5 years after diagnosis because of treatment delays in England [4,5,12]. However, the increase in delays of cancer care pathways in England during the first two waves of the pandemic cannot necessarily be translated into clinical harm due to the risk prioritisation strategies that were implemented in response to reduced service capacity. In addition, NHSE made available “interim treatment options” to allow for greater flexibility in the management of cancer patients during the COVID-19 pandemic. These treatment options are clinically assessed against a set of criteria to protect patients from becoming seriously ill, reduce their exposure, and make better use of clinical capacity [23]. Furthermore, GP referrals for suspected cancer decreased by more than 50 % at the onset of the pandemic and returned to 2019 levels in September 2020 [13]. Following this, at the end of the second wave of the COVID-19 pandemic (January 2021), the backlog of patients with suspected cancer awaiting diagnostic investigations (and subsequent treatment) in England was still substantially larger than the comparable period before the pandemic (approximately 65 % larger) [7].
As lockdown measures are being relaxed, the number of cancer referrals are now improving but remain lower than before the COVID-19 pandemic [2,24]. It is expected that the number of patients referred from primary care via the 2 W W pathway will continue to increase, saturating the demand for diagnostic services [25]. Moreover, preliminary analyses showed that COVID-19 burden was positively associated with deprivation score. This is in line with previous studies which have found that people residing in an area of socioeconomic deprivation apprear to be at greater risk of critical illness due to COVID-19 and thus, have higher COVID-19 burden [[26], [27], [28]].
In the current study, no associations were found between COVID-19 burden and compliance with the 62-day CWT target amongst internal specialist referrals. This may be explained by the direct contact between specialist teams which may have allowed for faster communication and therefore, faster treatment start dates. However, we did see a positive association between the total number of patients treated and COVID-19 burden within both wave 1, and wave 2. This may be associated with the prioritization of treatments for cancer patients diagnosed previous to the onset of the COVID-19 pandemic.
Furthermore, while we found that an increase in COVID-19 burden was associated with a decrease in the number of patients treated within all cancer types (i.e., breast, lower GI, lung, skin, urological, and ‘other’ cancer) during the first wave of COVID-19 (1st April – 30th May 2020), no associations were found for wave 2 (1st October – 30th November 2020. This may be explained by the implementation of ‘safe COVID-19 pathways’ for treatment and assessment of patients, carried out by site-specific cancer services as lockdown measures were being relaxed [2,29].
To our knowledge, this is one of the first studies to analyse the effect COVID-19 has had on the delays of cancer care in England, using real-world data. However, it should be noted that the analysis presented above is a broad quantification of the relationship between the spread of SARS-CoV-2 in the population and operational capacity of cancer services. It therefore does not provide a more granular analysis of the variability in the organisational characteristics of healthcare providers in England, and how these different providers responded to their COVID-19 caseloads. In addition, further studies are required to understand the differences between the impact of COVID-19 burden on internal specialist referrals and urgent referrals from primary care (i.e., 2 W W pathway referrals).
5. Conclusion
The current study adds to the body of evidence suggesting the impact the COVID-19 pandemic has had on the timely provision of cancer care in England. This is likely to be an ongoing issue due to the currently vast backlog of patients with suspected cancer awaiting diagnostic investigations and treatment. As the number of cancer-related referrals are steadily improving, changes to both primary and secondary care are necessary to manage the overwhelming backlog within diagnostic services to alleviate the impact of COVID-19 on cancer services.
Author contributions
Conceptualization: LF, AA, RS, MVH; Data curation: LF; Formal analysis: LF, MM; Supervision: RS, MVH, AA, KH, AP, JS, SP, AR, SD; Writing – original draft: MM, LF; Writing – review & editing: LF, MM, AA, KH, AP, JS, SP, AR, SD, RS, MVH.
Data availability
Data will be made available on request.
Declaration of Competing Interest
The authors declare no conflict of interest.
References
- 1.Raymond E., Thieblemont C., Alran S., Faivre S. Impact of the COVID-19 outbreak on the management of patients with cancer. Target. Oncol. 2020;15(3):249–259. doi: 10.1007/s11523-020-00721-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Monroy-Iglesias M.J., Tagliabue M., Dickinson H., Roberts G., De Berardinis R., Russell B., et al. Continuity of Cancer care: the surgical experience of two large cancer hubs in London and Milan. Cancers (Basel) 2021;13(7) doi: 10.3390/cancers13071597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Government U. 2021. Staying at Home and Away From Others (Social Distancing)https://www.gov.uk/government/publications/full-guidance-on-staying-at-home-and-away-from-others [Available from: [Google Scholar]
- 4.Maringe C., Spicer J., Morris M., Purushotham A., Nolte E., Sullivan R., et al. The impact of the COVID-19 pandemic on cancer deaths due to delays in diagnosis in England, UK: a national, population-based, modelling study. Lancet Oncol. 2020;21(8):1023–1034. doi: 10.1016/S1470-2045(20)30388-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sud A., Torr B., Jones M.E., Broggio J., Scott S., Loveday C., et al. Effect of delays in the 2-week-wait cancer referral pathway during the COVID-19 pandemic on cancer survival in the UK: a modelling study. Lancet Oncol. 2020;21(8):1035–1044. doi: 10.1016/S1470-2045(20)30392-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Morris E.J.A., Goldacre R., Spata E., Mafham M., Finan P.J., Shelton J., et al. Impact of the COVID-19 pandemic on the detection and management of colorectal cancer in England: a population-based study. Lancet Gastroenterol. Hepatol. 2021;6(3):199–208. doi: 10.1016/S2468-1253(21)00005-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cancer Waiting Times [Available from: https://www.england.nhs.uk/statistics/statistical-work-areas/cancer-waiting-times/.
- 8.Ricciardiello L., Ferrari C., Cameletti M., Gaianill F., Buttitta F., Bazzoli F., et al. Impact of SARS-CoV-2 pandemic on colorectal Cancer screening delay: effect on stage shift and increased mortality. Clin. Gastroenterol. Hepatol. 2021;19(7):1410–1417. doi: 10.1016/j.cgh.2020.09.008. e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Santoro G.A., Grossi U., Murad-Regadas S., Nunoo-Mensah J.W., Mellgren A., Di Tanna G.L., et al. DElayed COloRectal cancer care during COVID-19 Pandemic (DECOR-19): global perspective from an international survey. Surgery. 2021;169(4):796–807. doi: 10.1016/j.surg.2020.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tsibulak I., Reiser E., Bogner G., Petru E., Hell-Teutsch J., Reinthaller A., et al. Decrease in gynecological cancer diagnoses during the COVID-19 pandemic: an Austrian perspective. Int. J. Gynecol. Cancer. 2020;30(11):1667–1671. doi: 10.1136/ijgc-2020-001975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lamblin G., Golfier F., Peron J., Moret S., Chene G., Nohuz E., et al. Impact of the COVID-19 Outbreak on the management of patients with gynecological cancers. Gynecol. Obstet. Fertil. Senol. 2020;48(11):777–783. doi: 10.1016/j.gofs.2020.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hanna T.P., King W.D., Thibodeau S., Jalink M., Paulin G.A., Harvey-Jones E., et al. Mortality due to cancer treatment delay: systematic review and meta-analysis. BMJ. 2020;371:m4087. doi: 10.1136/bmj.m4087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cancer Waiting Times [Available from: https://www.england.nhs.uk/statistics/statistical-work-areas/cancer-waiting-times/.
- 14.Trust KGHNF . 2021. 62 Day Pathway.https://www.kgh.nhs.uk/62-day-pathway/ [Available from: [Google Scholar]
- 15.UK Coronavirus summary [Available from: https://coronavirus.data.gov.uk/.
- 16.England N. NHS; 2021. Cancer Waiting Times.https://www.england.N.hs.uk/statistics/statistical-work-areas/cancer-waiting-times/ [Available from: [Google Scholar]
- 17.Digital N. 2021. SHMI Deprivation Contextual Indicators.https://digital.N.hs.uk/data-and-information/publications/statistical/shmi/2020-10/deprivation [Available from: [Google Scholar]
- 18.England N. NHSE; 2021. Bed Availability and Occupancy.https://www.england.N.hs.uk/statistics/statistical-work-areas/bed-availability-and-occupancy/bed-data-overnight/ [Available from: [Google Scholar]
- 19.Dictionary NDMa . 2021. Consultant Upgrade.https://datadictionary.nhs.uk/nhs_business_definitions/consultant_upgrade.html [Available from: [Google Scholar]
- 20.The Lancet Gastroenterology H Resuming bowel cancer screening post-COVID-19. Lancet Gastroenterol. Hepatol. 2020;5(8):711. doi: 10.1016/S2468-1253(20)30200-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rutter M.D., Brookes M., Lee T.J., Rogers P., Sharp L. Impact of the COVID-19 pandemic on UK endoscopic activity and cancer detection: a National Endoscopy Database Analysis. Gut. 2021;70(3):537–543. doi: 10.1136/gutjnl-2020-322179. [DOI] [PubMed] [Google Scholar]
- 22.Papautsky E.L., Hamlish T. Patient-reported treatment delays in breast cancer care during the COVID-19 pandemic. Breast Cancer Res. Treat. 2020;184(1):249–254. doi: 10.1007/s10549-020-05828-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.England N. NICE; 2021. NHS England Interim Treatment Options During the COVID-19 Pandemic.https://www.nice.org.uk/guidance/ng161/resources/interim-treatment-change-options-during-the-covid19-pandemic-endorsed-by-nhs-england-pdf-8715724381 [Available from: [Google Scholar]
- 24.Greenwood E., Swanton C. Consequences of COVID-19 for cancer care - a CRUK perspective. Nat. Rev. Clin. Oncol. 2021;18(1):3–4. doi: 10.1038/s41571-020-00446-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hamilton W. Cancer diagnostic delay in the COVID-19 era: what happens next? Lancet Oncol. 2020;21(8):1000–1002. doi: 10.1016/S1470-2045(20)30391-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lone N.I., McPeake J., Stewart N.I., Blayney M.C., Seem R.C., Donaldson L., et al. Influence of socioeconomic deprivation on interventions and outcomes for patients admitted with COVID-19 to critical care units in Scotland: A national cohort study. Lancet Reg Health Eur. 2021;1 doi: 10.1016/j.lanepe.2020.100005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wendel Garcia P.D., Fumeaux T., Guerci P., Heuberger D.M., Montomoli J., Roche-Campo F., et al. Prognostic factors associated with mortality risk and disease progression in 639 critically ill patients with COVID-19 in Europe: initial report of the international RISC-19-ICU prospective observational cohort. EClinicalMedicine. 2020;25 doi: 10.1016/j.eclinm.2020.100449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Statistics OoN . 2021. Death Involving COVID-19 by Local Area and Socioeconomic Deprivation.https://www.ons.gov.uk/peoplepopulatio-nandcommunity/birthsdeathsandmarriages/deaths/bulletins/deathsinvolving-covid19bylocalareasanddeprivation/deathsoccurringbetween1marchand [Available from: [Google Scholar]
- 29.Archer S., Calanzani N., Honey S., Johnson M., Neal R., Scott S.E., et al. Impact of the COVID-19 pandemic on cancer assessment in primary care: a qualitative study of GP views. Bjgp Open. 2021;5(4) doi: 10.3399/BJGPO.2021.0056. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data will be made available on request.