Abstract
Background:
Medicaid expansion under the Affordable Care Act has improved access to screening and treatment for certain cancers. It is unclear how this policy has affected the diagnosis and management of pancreatic cancer.
Methods:
Using a quasi-experimental difference-in-differences (DID) approach, we analyzed Medicaid and uninsured patients in the National Cancer Data Base during two time periods: pre- (2011–12) and post-expansion (2015–16). We investigated changes in cancer staging, treatment decisions, and surgical outcomes.
Results:
In this national cohort, pancreatic cancer patients in expansion states had increased Medicaid coverage relative to those in non-expansion states (DID=17.49, p<0.01). Medicaid expansion also led to an increase in early-stage diagnoses (stage I/II, DID=4.71, p=0.03), higher comorbidity scores among surgical patients (Charlson/Deyo score 0: DID=−13.69, p=0.02), a trend toward more neoadjuvant radiation (DID=6.15, p=0.06), and more positive margins (DID=11.69, p=0.02). There were no differences in rates of surgery, postoperative outcomes, or overall survival.
Conclusion:
Medicaid expansion was associated with improved insurance coverage and earlier stage diagnoses for Medicaid and uninsured pancreatic cancer patients, but similar surgical outcomes and overall survival. These findings highlight both the benefits of Medicaid expansion and the potential limitations of policy change to improve outcomes for such an aggressive malignancy.
Keywords: pancreatic cancer, Medicaid expansion, healthcare policy
INTRODUCTION
Pancreatic cancer is the third-leading cause of cancer death in the United States; rates are on the rise, partially due to smoking and obesity, and over 57,000 people will be diagnosed this year1. Long-term survival is poor due to the aggressive biology of the disease and the high frequency of advanced presentation. However, advancements in medical and surgical therapy have improved the 5-year survival to 37% for patients with early stage disease1. Numerous studies have identified disparities in the management and outcomes of pancreatic cancer for patients based on race, income, and health insurance2.
The Affordable Care Act (ACA) was passed in 2010 with a goal of improving care and reducing costs through a variety of mechanisms, one of which was the expansion of public Medicaid insurance coverage to low-income non-elderly adults3. The process has been variable across states and politically contentious. While the majority of states have expanded Medicaid coverage, most in January 2014, a large proportion of states still have not4. This non-uniform adoption of the law has provided a natural experiment with which to study the impact of improved insurance coverage, and early studies have emphasized the reduced rate of uninsured patients as a result of the ACA5. There are suggestions of increased access to primary and preventative care, but the overall impact on health outcomes is unclear6. To date, no national studies have investigated the impact of Medicaid expansion on perioperative management and overall survival for pancreatic cancer.
Some studies have found increased screening and early-stage diagnosis, but these findings are at times small or inconsistent7–12. Findings specific to pancreatic cancer have also been mixed. One national study found no difference in early stage diagnoses in the years immediately following insurance expansion8. Studying Massachusetts health care reform, Loehrer et al found expanded insurance coverage led to increased admissions and surgical resection for pancreatic cancer13. However, Eguia et al found that Medicaid expansion in Iowa, Maryland, and New York increased admissions but not surgical resection for pancreatic cancer14.
The goal of the current study was to investigate the impact of Medicaid expansion on the diagnosis and management of pancreatic cancer at a national level. Using the National Cancer Data Base (NCDB), we analyzed a more granular set of patient and management characteristics than prior studies, using a larger and more heterogeneous cohort of patients, and across a longer time period. Our hypothesis was that state implementation of Medicaid expansion would be associated with increases in early-stage diagnoses and improvements in outcomes relative to trends in non-expansion states.
METHODS
Patient population
For this project we performed a retrospective analysis of the NCDB, a hospital-based cancer registry co-sponsored by the American College of Surgeons Commission on Cancer. This is a national cancer registry that receives information from over 1500 Commission-on-Cancer-accredited programs in the United States and captures approximately 70% of the incident cancer cases in the country15.
This analysis was performed using methods similar to a recent report on colon cancer using the NCDB16. We first selected all patients with pancreatic ductal adenocarcinoma, excluding benign and other histology. Next, we grouped patients based on the Medicaid expansion status of their home state. Although actual hospitals and locations are blinded, the NCDB recently included a field called “Medicaid Expansion Status State Group” which characterizes patients based on if/when their state expanded Medicaid coverage under the ACA. Categories include non-expansion states (AL, FL, GA, ID, KS, ME, MO, MS, NC, NE, OK, SC, SD, TN, TX, UT, VA, WI, WY), January 2014 expansion states (AR, AZ, CO, DE, HI, IA, IL, KY, MA, MD, ND, NM, NV, NY, OH, OR, RI, VT, WV), early expansion states (2010–2013; CA, CT, DC, MN, NJ, WA), and late expansion states (after January 2014; AK, IN, LA, MI, MT, NH, PA). In an effort to promote consistency we compared non-expansion states to January 2014 expansion states, which are the two largest categories (19 states each). Early and late expansion groups were excluded due to the heterogenous timelines with which these states expanded their insurance coverage.
We narrowed our patient cohort to two time periods: 2011–12 and 2015–16. Our goal was to compare the most recent possible cohort to a modern cohort prior to ACA Medicaid expansion. We excluded 2013 and 2014, the years directly before and after expanded Medicaid coverage, in order to eliminate any acclimation period.
Finally, we limited our analysis to patients age 40–64 who either had Medicaid coverage or were uninsured, excluding the ~75% of patients in the NCDB pancreatic cancer cohort with Medicare or private insurance16. Some studies have included all insurance types in their analysis8,10,13. Medicaid expansion was meant to improve coverage for patients without health insurance and should have little impact on cancer patients who are eligible for Medicare or have access to coverage through their employer17; the patients theoretically most affected by Medicaid expansion are those with Medicaid or no health insurance. While some uninsured patients with incomes above the Medicaid eligibility limit could have acquired private subsidized plans through ACA Marketplaces, this would have occurred across both expansion and non-expansion states. Further, the vast majority of private coverage is through employer-sponsored plans and there were no significant changes in the proportion of Medicare and privately insured patients in prior studies18 or in our analysis. Therefore, we chose to perform a more targeted analysis of only Medicaid and uninsured patients13,16. As Medicaid expansion status is suppressed for age 0–39 in the NCDB, only patients age 40–64 were included in this analysis.
Outcomes of interest
The goal of this study was to investigate potential changes in pancreatic cancer presentation and management as a result of Medicaid expansion. Therefore, we analyzed three different groups of characteristics and outcomes in the NCDB based on specific patient groups. For all patients we compared sociodemographic characteristics, treatment facility details, timeliness of treatment, and stage at presentation. Next, we focused on early-stage patients (clinical stage I/II), all of whom should theoretically be surgical candidates. For this group we compared the proportion of early-stage patients within the whole cohort, rates of surgery, reasons for not having surgery, and rates of no treatment. Finally, we studied all patients who underwent surgical resection and compared their comorbidity scores, treatment facility characteristics, pathologic stage, surgical approach, use of neoadjuvant therapy (chemotherapy and/or radiation) and adjuvant chemotherapy, and surgical outcomes (margins, length of stay, readmission, mortality).
Difference-in-differences approach
In scenarios where a policy change creates a natural experiment with control and intervention groups, such as state Medicaid expansion under the ACA, a quasi-experimental difference-in-differences (DID) approach can be used to estimate the relative effects of the policy. This methodology has been used widely to study the impact of Medicaid expansion on insurance coverage and other patient characteristics8,10,16. For this study, the non-expansion states served as the “control” group and the January 2014 expansion states served as the “experimental” group. For any given variable, we first identified the change between time periods for the non-expansion states, described in absolute and relative terms.
We assumed we would have observed parallel trend in expansion states, if there was no Medicaid expansion treatment effect, and used the non-expansion rate of change to create a counterfactual end point, or an expected rate of change. Next, we calculated the change over time among expansion states and compared this difference to the change in non-expansion states, thus calculating a “difference-in-differences.”
Figure 1 demonstrates this technique used to analyze rates of Medicaid insurance coverage among our patient groups, a characteristic which was presumed to change significantly between groups based on policy and study design. Using rounded numbers, the proportion of Medicaid patients in the non-expansion cohort increased from 51% to 56% between time periods, a change of 5 percentage points. Based on this, the expectation would be for expansion states to increase their Medicaid proportion from 67% to 72%. However, the actual proportion increased to 90%, which was significantly higher than expected: an 18- point increase attributable to Medicaid expansion (treatment effect).
Figure 1.
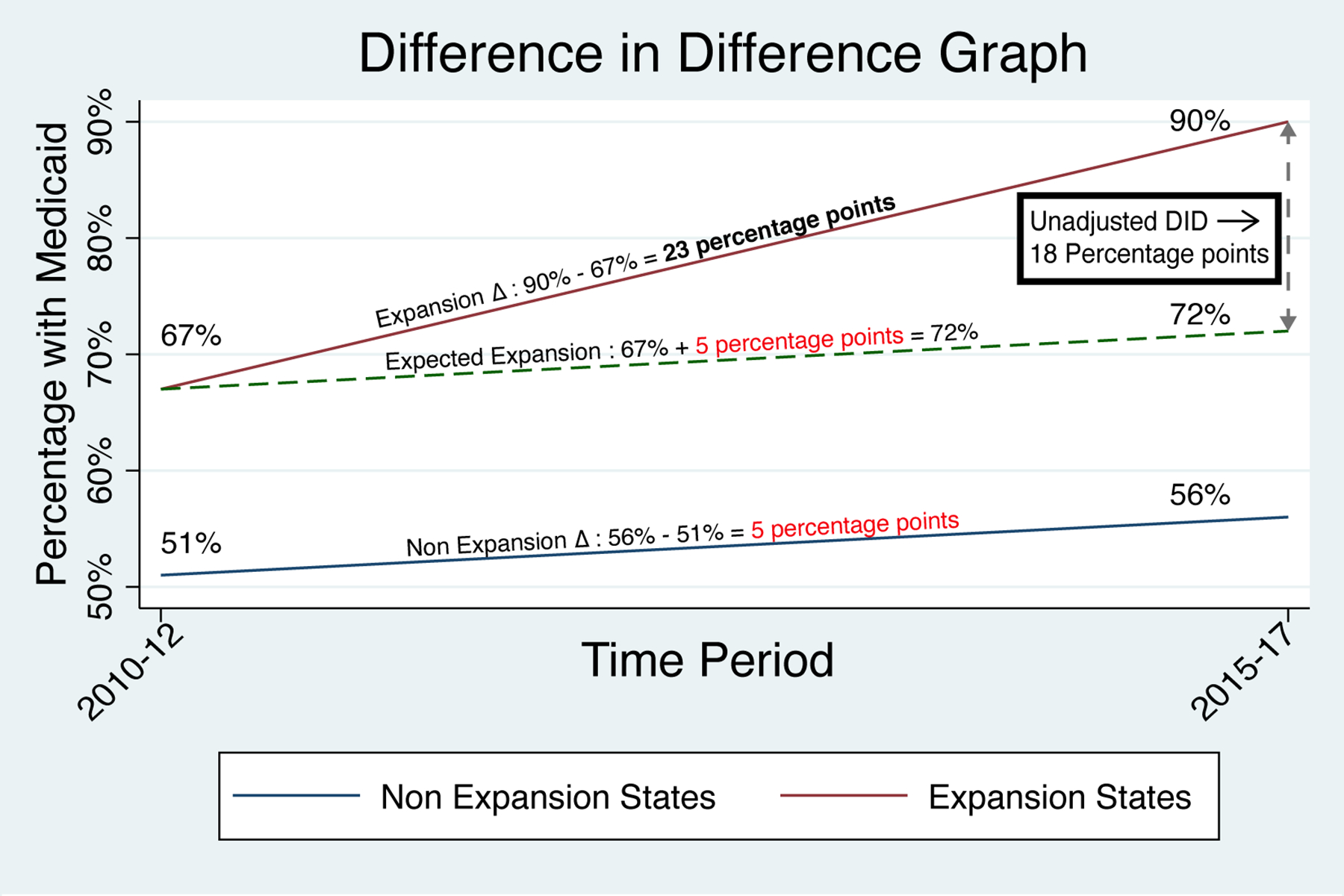
Graphical depiction of the difference-in-differences methodology. Changes in the proportions of patients who were uninsured (A) or had Medicaid (B) are shown for non-expansion states (blue line) and January 2014 expansion states (red line). Both groups showed parallel trends in the pre-expansion time period (2010–2013). Following Medicaid expansion in January 2014, expansion states showed a relative decrease in uninsured patients and increase in Medicaid coverage compared to non-expansion states.
Unadjusted DID coefficients were determined from the interaction term between Medicaid expansion and time period in a linear probability model. Additionally, we estimated multivariable DID models that adjusted for age, gender, race, urban/rural location, Charlson/Deyo comorbidity score, income, AJCC clinical cancer stage, regional facility location, and year of diagnosis.
To assess the validity of the parallel trends assumption, we examined pre-2014 trends in expansion and non-expansion states. We first qualitatively assessed for pre-expansion similarities by visually examining pre-2014 trends in diagnosis, insurance status, and management between groups. We then formally assessed the parallel trends assumption by regressing a year-by-expansion interaction on outcomes in the pre-expansion period. Nonsignificant adjusted year-by-expansion interaction terms in the pre-expansion period support the assumption of parallel trends.
Reported p-values were 2-tailed with a value <0.05 considered statistically significant. All statistical analysis was performed using STATA 16MP (StataCorp LP, College Station, TX).
RESULTS
Insurance coverage
First, we examined changes in all types of health insurance. Medicaid expansion led to significant changes in insurance coverage when considering all types of health insurance (Table 1). Relative to non-expansion states, Medicaid expansion states demonstrated an increase in Medicaid coverage (DID=2.00, p<0.001) and decrease in their uninsured proportion (DID=−0.64, p=0.004) among patients with pancreatic cancer. There was also a relative reduction in private insurance coverage (DID=−1.12, p=0.03). When parallel trends were examined for rates of Medicaid and uninsured patients over the pre-expansion years, we found no difference in trends between expansion and non-expansion states (all p>0.05).
Table 1.
Difference-in-differences analysis of health insurance for pancreatic cancer patients in the pre- and post-expansion time periods in non-expansion and January 2014 expansion states.
| Non-Expansion States | Expansion States | Unadjusted | Adjusted | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2011–12 | 2015–16 | AD | RC (%) | 2011–12 | 2015–16 | AD | RC (%) | DID | p value | DID | p value | |
| All patients (n) | 25,871 | 33,031 | 21,186 | 26,915 | ||||||||
| Insurance Types (%) | ||||||||||||
| Private | 30.16 | 27.95 | −2.21 | −7.32 | 31.32 | 28.53 | −2.79 | −8.91 | −0.58 | 0.30 | −1.12 | 0.03 * |
| Medicare | 58.18 | 61.81 | 3.63 | 6.25 | 59.01 | 61.64 | 2.63 | 4.45 | −1.01 | 0.10 | −0.31 | 0.54 |
| Medicaid | 5.04 | 4.44 | −0.60 | −11.85 | 5.95 | 7.57 | 1.62 | 27.29 | 2.22 | <0.001 * | 2.00 | <0.001 * |
| Other Governmental | 1.91 | 2.13 | 0.22 | 11.41 | 0.96 | 1.22 | 0.27 | 28.00 | 0.05 | 0.75 | 0.06 | 0.72 |
| Uninsured | 4.72 | 3.67 | −1.05 | −22.22 | 2.76 | 1.04 | −1.73 | −62.47 | −0.68 | 0.002 * | −0.64 | 0.004 * |
AD=absolute difference (%); DID=difference-in-differences; RC=relative change (% change between time periods).
indicates statistical significance.
All patients
There were a total of 6,698 pancreatic cancer patients in the final dataset: 3,819 patients from non-expansion states and 2,879 patients from expansion states (Table 2). Similar to the larger cohort, expansion states in this group showed a relative increase in Medicaid coverage (DID=17.49, p<0.001) and reduction in uninsured patients (DID=−17.49, p<0.001) (Figure 1). Expansion states had a relative increase in the days from diagnosis to starting treatment (DID=5.31, p=0.01), but there were no differences in distance travelled, stage at diagnosis, or hospital type.
Table 2.
Difference-in-differences analysis of Medicaid and uninsured patients with pancreatic cancer. Comparison is between pre- and post-expansion time periods in non-expansion and January 2014 expansion states.
| Non-Expansion States | Expansion States | Unadjusted | Adjusted | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2011–12 | 2015–16 | AD | RC (%) | 2011–12 | 2015–16 | AD | RC (%) | DID | p value | DID | p value | |
| All Patients (n) | 1,972 | 1,847 | 1,311 | 1,568 | ||||||||
| Insurance (%) | ||||||||||||
| Medicaid | 51.12 | 56.47 | 5.35 | 10.47 | 66.97 | 90.24 | 23.27 | 34.75 | 17.92 | <0.001 * | 17.49 | <0.001 * |
| Uninsured | 48.88 | 43.53 | −5.35 | −10.95 | 33.03 | 9.76 | −23.27 | −70.46 | −17.92 | <0.001 * | −17.49 | <0.001 * |
| Distance travelled (miles) | 35.91 | 28.80 | −7.11 | −19.81 | 27.27 | 24.00 | −3.27 | −12.00 | 3.84 | 0.39 | 2.31 | 0.60 |
| Diagnosis to treatment (days) | 32.00 | 32.68 | 0.68 | 2.12 | 28.46 | 34.18 | 5.72 | 20.08 | 5.04 | 0.01 * | 5.31 | 0.01 * |
| Treatment at academic program | 43.31 | 41.42 | −1.89 | −4.36 | 58.05 | 56.82 | −1.22 | −2.11 | 0.66 | 0.79 | −0.02 | 1.00 |
| AJCC Clinical Stage (%) | ||||||||||||
| 1 | 9.91 | 11.08 | 1.17 | 11.79 | 9.49 | 12.88 | 3.38 | 35.64 | 2.22 | 0.17 | 1.92 | 0.24 |
| 2 | 21.22 | 19.40 | −1.82 | −8.57 | 17.86 | 18.39 | 0.53 | 2.98 | 2.35 | 0.25 | 2.32 | 0.26 |
| 3 | 13.10 | 11.66 | −1.44 | −10.97 | 13.94 | 12.40 | −1.54 | −11.05 | −0.10 | 0.95 | −0.06 | 0.97 |
| 4 | 55.66 | 57.80 | 2.14 | 3.85 | 58.54 | 56.27 | −2.27 | −3.88 | −4.41 | 0.09 | −4.12 | 0.11 |
| Early stage (I-II) patients (n) | 556 | 520 | 314 | 454 | ||||||||
| Proportion of all patients (%) | 28.19 | 28.15 | −0.04 | −0.15 | 23.95 | 28.95 | 5.00 | 20.89 | 5.04 | 0.02 * | 4.71 | 0.03 * |
| Diagnosis to treatment (days) | 31.45 | 34.04 | 2.58 | 8.21 | 27.09 | 36.08 | 8.99 | 33.17 | 6.40 | 0.08 | 6.18 | 0.09 |
| Reason for no surgery (%) | ||||||||||||
| Surgery performed | 42.63 | 38.65 | −3.97 | −9.32 | 49.68 | 43.61 | −6.07 | −12.22 | −2.10 | 0.66 | −1.57 | 0.74 |
| Not part of first planned treatment | 45.50 | 49.81 | 4.30 | 9.46 | 35.99 | 42.07 | 6.08 | 16.90 | 1.78 | 0.71 | 1.61 | 0.74 |
| Patient risk factors | 5.94 | 5.19 | −0.74 | −12.52 | 7.96 | 8.81 | 0.85 | 10.66 | 1.59 | 0.51 | 1.06 | 0.66 |
| Patient died | 0.72 | 0.19 | −0.53 | −73.27 | 0.00 | 0.00 | 0.00 | 0.00 | 0.53 | 0.29 | 0.46 | 0.36 |
| Patient refused | 1.62 | 2.50 | 0.88 | 54.44 | 2.23 | 1.32 | −0.91 | −40.72 | −1.79 | 0.17 | −1.72 | 0.19 |
| No treatment (%) | 13.13 | 13.85 | 0.72 | 5.46 | 9.87 | 10.13 | 0.26 | 2.63 | −0.46 | 0.88 | 0.160 | 0.96 |
| Stage IV patients (n) | 994 | 986 | 672 | 817 | ||||||||
| Proportion of all patients (%) | 55.66 | 57.80 | 2.14 | 3.85 | 58.54 | 56.27 | −2.27 | −3.88 | −4.41 | 0.09 | −4.12 | 0.11 |
| Systemic therapy (%) | 53.22 | 57.51 | 4.29 | 8.05 | 54.76 | 60.83 | 6.07 | 11.09 | 1.78 | 0.60 | 2.31 | 0.49 |
| Surgery (%) | 1.31 | 0.41 | −0.90 | −68.98 | 0.89 | 0.61 | −0.28 | −31.46 | 0.62 | 0.31 | 0.62 | 0.31 |
| Palliative care (%) | 23.54 | 22.82 | −0.72 | −3.07 | 28.42 | 29.74 | 1.32 | 4.65 | 2.04 | 0.50 | 1.65 | 0.58 |
| No treatment (%) | 31.39 | 29.41 | −1.98 | −6.30 | 29.76 | 25.58 | −4.18 | −14.05 | −2.20 | 0.48 | −2.61 | 0.40 |
AD=absolute difference (in days, miles, or %); AJCC=American Joint Committee on Cancer; DID=difference-in-differences; RC=relative change (% change between time periods).
indicates statistical significance.
Stage-specific treatment
Next, we analyzed patients diagnosed with early stage (stage I/II) pancreatic cancer (Table 2). Medicaid expansion was associated with a relative increase in early-stage diagnoses (DID=4.71, p=0.03), but no difference in treatment for these patients. Rates of surgery, reasons for no surgery, and timeliness of treatment were unchanged with Medicaid expansion.
The proportion of patients presenting with metastatic disease was not associated with Medicaid expansion (Table 2). Also, the treatments these patients received was not uniquely changed in Medicaid expansion states; there was no relative difference in chemotherapy, palliative care, or lack of treatment for metastatic patients following Medicaid expansion.
Patients receiving surgery
Medicaid expansion was not associated with a change in the proportion of patients in the sample undergoing surgery for pancreatic cancer (Table 3). Also, there were few observed differences in this cohort of patients. Medicaid expansion was associated with an increase in medical comorbidities among surgical patients (Charlson/Deyo score 0: DID=−13.69, p=0.02). However, there was no difference in cancer stage, facility characteristics, or time to treatment.
Table 3.
Difference-in-differences analysis of all Medicaid and uninsured patients who underwent surgery for pancreatic cancer. Comparison is between pre- and post-expansion time periods in non-expansion and January 2014 expansion states.
| Non-Expansion States | Expansion States | Unadjusted | Adjusted | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2011–12 | 2015–16 | AD | RC (%) | 2011–12 | 2015–16 | AD | RC (%) | DID | p value | DID | p value | |
| Surgical patients (n) | 350 | 305 | 240 | 301 | ||||||||
| Proportion of all patients (%) | 17.75 | 16.51 | −1.24 | −6.96 | 18.31 | 19.20 | 0.89 | 4.86 | 2.13 | 0.26 | 2.05 | 0.28 |
| Charlson/Deyo Score (%) | ||||||||||||
| 0 | 60.29 | 69.18 | 8.89 | 14.75 | 67.08 | 60.47 | −6.62 | −9.87 | −15.51 | 0.01 * | −13.69 | 0.02 * |
| 1 | 30.86 | 22.62 | −8.23 | −26.68 | 27.50 | 28.57 | 1.07 | 3.90 | 9.31 | 0.07 | 8.11 | 0.13 |
| 2 | 6.86 | 3.61 | −3.25 | −47.40 | 4.17 | 4.65 | 0.48 | 11.63 | 3.74 | 0.14 | 3.16 | 0.22 |
| 3+ | 2.00 | 4.59 | 2.59 | 129.51 | 1.25 | 6.31 | 5.06 | 404.98 | 2.47 | 0.25 | 2.42 | 0.27 |
| AJCC clinical stage (%) | ||||||||||||
| 1 | 37.01 | 39.15 | 2.14 | 5.79 | 37.13 | 42.34 | 5.22 | 14.05 | 3.07 | 0.65 | 0.09 | 0.99 |
| 2 | 55.12 | 54.25 | −0.87 | −1.58 | 53.29 | 46.40 | −6.90 | −12.94 | −6.02 | 0.38 | −4.28 | 0.55 |
| 3 | 3.54 | 5.19 | 1.65 | 46.44 | 5.99 | 9.01 | 3.02 | 50.45 | 1.38 | 0.67 | 2.16 | 0.52 |
| 4 | 3.54 | 1.42 | −2.13 | −60.06 | 3.59 | 2.25 | −1.34 | −37.31 | 0.79 | 0.73 | 1.20 | 0.60 |
| Distance travelled (miles) | 46.28 | 35.77 | −10.51 | −22.71 | 27.16 | 25.90 | −1.26 | −4.63 | 9.25 | 0.24 | 7.42 | 0.33 |
| Diagnosis to treatment (days) | 20.67 | 23.92 | 3.24 | 15.69 | 18.33 | 26.56 | 8.22 | 44.85 | 4.98 | 0.12 | 3.68 | 0.26 |
| Treatment at academic program | 50.00 | 49.18 | −0.82 | −1.64 | 65.83 | 58.14 | −7.69 | −11.69 | −6.87 | 0.23 | −8.15 | 0.16 |
| AJCC pathologic stage (%) | ||||||||||||
| 0 | 0.91 | 0.34 | −0.57 | −62.34 | 0.91 | 0.00 | −0.91 | −100.00 | −0.34 | 0.69 | −0.23 | 0.80 |
| 1 | 8.16 | 12.97 | 4.81 | 58.99 | 9.55 | 8.77 | −0.77 | −8.10 | −5.59 | 0.12 | −6.35 | 0.08 |
| 2 | 84.89 | 82.25 | −2.64 | −3.11 | 83.18 | 85.96 | 2.78 | 3.35 | 5.42 | 0.22 | 5.71 | 0.20 |
| 3 | 2.11 | 2.05 | −0.07 | −3.17 | 3.18 | 1.75 | −1.43 | −44.86 | −1.36 | 0.44 | −0.93 | 0.61 |
| 4 | 3.93 | 2.39 | −1.54 | −39.17 | 3.18 | 3.51 | 0.33 | 10.28 | 1.87 | 0.39 | 1.80 | 0.41 |
| MIS approach (%) | 13.42 | 24.81 | 11.38 | 84.81 | 15.31 | 23.39 | 8.08 | 52.75 | −3.31 | 0.51 | −1.55 | 0.76 |
| Negative margin (R0, %) | 73.14 | 78.69 | 5.55 | 7.58 | 83.33 | 77.08 | −6.26 | −7.51 | −11.80 | 0.02 * | −11.69 | 0.02 * |
| Length of stay (days) | 11.54 | 8.92 | −2.61 | −22.66 | 11.48 | 10.09 | −1.39 | −12.09 | 1.23 | 0.32 | 0.79 | 0.53 |
| 30-day readmission (%) | 6.86 | 6.56 | −0.30 | −4.37 | 12.08 | 8.31 | −3.78 | −31.26 | −3.48 | 0.28 | −4.55 | 0.16 |
| 30-day mortality (%) | 2.00 | 1.64 | −0.36 | −18.03 | 3.33 | 0.66 | −2.67 | −80.07 | −2.31 | 0.14 | −2.19 | 0.17 |
| 90-day mortality (%) | 4.86 | 3.93 | −0.92 | −19.00 | 6.67 | 2.33 | −4.34 | −65.12 | −3.42 | 0.15 | −3.59 | 0.14 |
| Neoadjuvant therapy (%) | 12.29 | 28.85 | 16.57 | 134.85 | 10.42 | 31.89 | 21.48 | 206.18 | 4.91 | 0.29 | 5.34 | 0.25 |
| Adjuvant chemotherapy (%) | 61.14 | 59.02 | −2.13 | −3.48 | 61.67 | 64.78 | 3.12 | 5.06 | 5.24 | 0.36 | 2.53 | 0.66 |
AD=absolute difference (in miles, days, or %); AJCC=American Joint Committee on Cancer; DID=difference-in-differences; MIS=minimally invasive surgery; RC=relative change (% change between time periods).
indicates statistical significance.
Surgical outcomes were largely unchanged. There was reduction in margin-negative resections with Medicaid expansion (DID=−11.69, p=0.02), but there was no difference in the use of minimally invasive surgery or other surgical outcomes such as length of stay, readmission, or mortality. Both groups of states demonstrated a substantial increase in the use of neoadjuvant therapy; Medicaid expansion was associated with a near-significant increase in neoadjuvant radiation (DID=6.15, p=0.06) but no difference in the use of neoadjuvant chemotherapy.
Survival analysis
Finally, we analyzed survival based on Medicaid expansion status for all patients and then localized (stage I-III) and metastatic (stage IV) patients (Table 4). The median overall survival for the entire cohort was 7.36 months (95% CI 7.06–7.69). Survival improved over time for all patient groups, and survival was higher in Medicaid expansion states compared to non-expansion states in each of the time periods for each of the patient groups (i.e. 2011–2012, all stages: 7.20 vs 6.51 months, p<0.05). However, Medicaid expansion was not associated with a significant change in survival relative to non-expansion states.
Table 4.
Difference-in-differences analysis of overall survival for Medicaid and uninsured patients with pancreatic cancer. Comparison is between pre- and post-expansion time periods in non-expansion and January 2014 expansion states.
| Non-expansion States | Expansion States | Unadjusted | Adjusted | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2011–12 | 2015–16 | AD | RC (%) | 2011–12 | 2015–16 | AD | RC (%) | DID | p value | DID | p value | |
| All patients (n) | 1,972 | 1,847 | 1,311 | 1,568 | ||||||||
| All stages | ||||||||||||
| Median survival (months)# | 6.51 (6.21–6.93) |
8.18 (7.16–9.07) |
7.20 (6.60–7.89) |
9.72 (8.41–11.10) |
||||||||
| 1-year survival (%) | 28.70 | 53.55 | 24.85 | 86.59 | 33.26 | 58.29 | 25.03 | 75.26 | 0.19 | 0.94 | −1.85 | 0.41 |
| 2-year survival (%) | 12.27 | 40.01 | 27.74 | 226.04 | 15.56 | 43.62 | 28.06 | 180.34 | 0.32 | 0.88 | −0.83 | 0.69 |
| Stage I-III | ||||||||||||
| Median survival (months)# | 11.47 (10.48–12.42) |
13.77 (12.75–15.54) |
13.04 (11.7–15.15) |
16.89 (14.62–19.09) |
||||||||
| 1-year survival (%) | 46.62 | 67.67 | 21.04 | 45.14 | 51.69 | 70.09 | 18.40 | 35.60 | −2.64 | 0.47 | −3.27 | 0.37 |
| 2-year survival (%) | 21.53 | 46.94 | 25.41 | 117.98 | 26.40 | 50.57 | 24.17 | 91.52 | −1.24 | 0.72 | −1.45 | 0.68 |
| Stage IV | ||||||||||||
| Median survival (months)# | 3.38 (3.15–3.84) |
3.80 (3.40–4.47) |
3.91 (3.45–4.40) |
4.93 (4.11–5.95) |
||||||||
| 1-year survival (%) | 13.56 | 42.19 | 28.62 | 211.03 | 18.58 | 47.78 | 29.20 | 157.13 | 0.58 | 0.85 | −0.54 | 0.86 |
| 2-year survival (%) | 4.65 | 34.23 | 29.58 | 635.56 | 5.90 | 37.13 | 31.23 | 529.28 | 1.65 | 0.52 | 0.82 | 0.75 |
AD=absolute difference (in %); DID=difference-in-differences; RC=relative change (% change between time periods). Median overall survival presented with 95% confidence intervals.
Statistically significant difference (p<0.05) in median overall survival between non-expansion and expansion states for each time period.
DISCUSSION
This analysis of uninsured and Medicaid patients in the NCDB found that Medicaid expansion under the ACA may have caused several changes in the presentation and management of pancreatic cancer. States that expanded Medicaid coverage demonstrated shifts toward earlier presentation and higher comorbidity scores, but there were no differences in rates of surgery or most surgical outcomes in the cohort examined. This is the first study to investigate pancreatic cancer survival after Medicaid expansion, and we found no association between survival and state Medicaid expansion status.
We have recently reported a similar analysis of colon cancer diagnosis and management using the NCDB16. In that study, Medicaid expansion correlated with earlier diagnosis, more travel and less delays for care, less urgent surgery, more minimally invasive surgery, and more palliative care for stage IV patients. These studies highlight the possibilities and limitations of insurance expansion. Due to accurate screening tests, expanded insurance coverage and enhanced health care access can improve the diagnosis and management of colon cancer. Conversely, pancreatic cancer presents symptomatically and progresses rapidly. While most aspects of pancreatic cancer diagnosis and management were unchanged, there were a few differences associated with Medicaid expansion.
Existing studies are mixed on the association between insurance expansion and early-stage cancer diagnoses. Soni et al found more early stage diagnoses in a heterogeneous cohort of malignancies11. When analyzing the NCDB for the years 2011–2014, Jemal et al found increased early stage diagnoses for several malignancies in Medicaid expansion states, but these trends were not significant in adjusted analyses8. Our study is different in that we analyzed a more recent post-ACA cohort (2015–16) and focused on Medicaid and uninsured patients. Our results showed minimal change in early-stage diagnoses in non-expansion states compared to a 5% increase in expansion states. This suggests that Medicaid expansion contributed to earlier diagnosis of pancreatic cancer among the group of Medicaid and uninsured patients. Reasons for this finding are unclear, as pancreatic cancer has no effective screening mechanism. This may be a result of improved access to health care and more timely workup of vague symptoms, or perhaps this reflects an increase in incidental diagnoses. It may also be related to broader changes in the health care infrastructure of Medicaid expansion states. Future studies with access to more granular data may help elucidate these findings.
We also found a shift toward higher comorbidity scores among surgical patients in expansion states. This finding has not been described elsewhere and could have several explanations. One goal of Medicaid expansion was improved access to primary care and other non-urgent services. It is possible that patients in expansion states were more likely to have seen a physician and identified comorbid conditions prior to their pancreatic cancer diagnosis. It may also represent more expanded surgical patient selection in these states. Importantly, this shift towards increased illness among surgical patients did not correlate with increased postoperative mortality or readmissions rates.
Two other findings suggest expanded surgical patient selection associated with Medicaid expansion. Expansion states demonstrated a 6% increase in positive surgical margins which was statistically different from non-expansion states. Since other surgical outcomes were similar, this is likely not explained by a deterioration in surgical quality across expansion states. Also, the use of neoadjuvant radiation among surgical patients in the sample doubled in expansion states, while this therapy did not change in non-expansion states. Neoadjuvant radiation is controversial and may offer the most benefit for patients with borderline or locally advanced tumors that respond favorably to treatment and ultimately undergo surgical resection19,20. The relative increases in preoperative radiation and positive surgical margins suggest that more patients, beyond those with straightforward resectable tumors, were undergoing curative-intent treatments following Medicaid expansion.
Several studies have shown that pancreatic cancer patients receive surgery and other expected therapies at surprisingly low rates21–24. One thoughtful analysis of the Surveillance, Epidemiology, and End Results database highlighted the stepwise association of lower patient socioeconomic status with reduced receipt of surgery of early stage gastrointestinal cancers23. Patient race has also been suggested to influence the receipt of surgery for pancreatic cancer, with minority race predicting a lower likelihood of surgery21,24,25. There are many patient factors that may influence management that are not immediately improved by expanded insurance coverage.
An analysis of Massachusetts health reform found that expanded insurance coverage did increase the use of surgery for pancreatic cancer, which the authors attributed to earlier detection13. In our study, while Medicaid expansion led to more early-stage diagnoses, these patients did not receive higher rates of surgery. This is perhaps a result of our broader and more heterogenous analysis including 19 expansion states of various sizes and characteristics. This may also be a result of the increased use of neoadjuvant therapy in recent years, as seen in Table 3, which allows more time to assess patients prior to surgery. Indeed, a study of early stage pancreatic cancer patients at our institution showed that 57% of patients received surgery while the majority who did not were either deemed medically unfit or had disease progression that prohibited curative surgery26. While pancreatic surgery has become much safer in recent years, it is still a major physiologic stress that is not suitable for many patients. These unfortunate disease characteristics will not be modified by expanded insurance coverage.
Our findings did not demonstrate increases in specific treatments among patients in our cohort. For example, stage IV patients in expansion states showed a slight increase in palliative care and decrease in no treatment compared to non-expansion states, but these findings were not statistically significant. We recently found that patients with stage IV colon cancer were more likely to receive palliative care services following Medicaid expansion.16 One explanation is the relatively small number of patients in this study, which limits statistical power to detect changes. Also, if Medicaid expansion led to more patients being treated at Commission-on-Cancer hospitals and thus improved access to these services, we would be unable to study that using the NCDB. Regardless, our findings may highlight a limitation of insurance expansion when it comes to addressing disparities in treatment for low income cancer patients, and more work is needed to better address these issues.
There are limitations to this study. Due to the blinding of NCDB data we are limited in our ability to stratify certain variables or to link to other datasets which may help understand other hospital or geographic characteristics. The NCDB collects 70% of cancer diagnoses in the country, but it is based on Commission-on-Cancer hospitals and not population-based, which limits generalizability. We are unable to assess whether Medicaid expansion influenced the proportion of patients receiving care at Commission-on-Cancer-institutions. While the NCDB provides standardized oncologic data, there is limited information regarding courses of treatment and postoperative outcomes. Most significantly, we could not analyze long-term survival due to inadequate follow-up for the post-ACA cohorts, and some of our adjusted analyses may have been limited by sample size. Also, despite the quasi-experimental nature of the study design, we can only assess changes associated with Medicaid expansion and cannot rule out the potential that unobserved differences across states contribute to these findings. We also cannot comment on insurance coverage in the overall population or among patients with other types of cancer based on our results, as we are limited to those with pancreatic cancer captured by the NCDB in this analysis. There could also be broader population dynamics at work in certain states that may have skewed our results.
Finally, while we limited our analysis to Medicaid and uninsured patients to focus on low-income patients and those most likely affected by expanded Medicaid coverage, it is possible that we excluded patients who may have otherwise benefitted from the ACA. For example, improved insurance coverage through the ACA Marketplace, changes in care due to cost sharing subsidies, and other aspects of the ACA may have affected all patients rather than just those in Medicaid expansion states. We chose to narrow our patient cohort (uninsured and Medicaid patients only, excluding early and late expansion states) to more specifically study the effect of Medicaid expansion and maximize the ability to observe changes associated with the policy. However, this may limit the generalizability of our findings.
CONCLUSION
At this time, it appears that increased insurance coverage in Medicaid expansion states led to more early-stage pancreatic cancer diagnoses and perhaps expanded surgical patient selection among a population of Medicaid and uninsured patients. In contrast, most aspects of pancreatic cancer management in this cohort were unaffected by Medicaid expansion. Perhaps this indicates that treatment decisions for pancreatic cancer are generally made independent of a patient’s ability to pay. Moreover, socioeconomic characteristics such as income and education likely influence health care disparities more than insurance coverage and are unaffected by the ACA. This study highlights limitations of certain health care policies to improve outcomes for aggressive cancers. More work is needed to understand and improve the management of these vulnerable patients.
Synopsis:
In this analysis of the National Cancer Data Base, Medicaid expansion was associated with more early-stage diagnoses but no significant changes in outcomes or overall survival for patients with pancreatic cancer. This study highlights the benefits and limitations of health insurance policy to affect treatment for certain malignancies.
Funding:
University of Pittsburgh Department of Surgery
Footnotes
Disclosures: none
REFERENCES
- 1.American Cancer Society. (www.cancer.org).
- 2.Noel M, Fiscella K. Disparities in Pancreatic Cancer Treatment and Outcomes. Health Equity 2019;3(1):532–540. (In eng). DOI: 10.1089/heq.2019.0057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Patient Protection and Affordable Care Act. 2010.
- 4.KFF. Status of State Action on the Medicaid Expansion Decision. Kaiser Family Foundation. (https://www.kff.org/health-reform/state-indicator/state-activity-around-expanding-medicaid-under-the-affordable-care-act/?currentTimeframe=0&sortModel=%7B%22colId%22:%22Location%22,%22sort%22:%22asc%22%7D). [Google Scholar]
- 5.Obama B United States Health Care Reform: Progress to Date and Next Steps. JAMA 2016;316(5):525–32. (In eng). DOI: 10.1001/jama.2016.9797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gruber J, Sommers BD. The Affordable Care Act’s Effects on Patients, Providers, and the Economy: What We’ve Learned So Far. Journal of Policy Analysis and Management 2019;38(4):1028–1052. [Google Scholar]
- 7.Han X, Yabroff KR, Ward E, Brawley OW, Jemal A. Comparison of Insurance Status and Diagnosis Stage Among Patients With Newly Diagnosed Cancer Before vs After Implementation of the Patient Protection and Affordable Care Act. JAMA Oncol 2018;4(12):1713–1720. (In eng). DOI: 10.1001/jamaoncol.2018.3467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jemal A, Lin CC, Davidoff AJ, Han X. Changes in Insurance Coverage and Stage at Diagnosis Among Nonelderly Patients With Cancer After the Affordable Care Act. J Clin Oncol 2017;35(35):3906–3915. (In eng). DOI: 10.1200/JCO.2017.73.7817. [DOI] [PubMed] [Google Scholar]
- 9.Han X, Zhao J, Ruddy KJ, Lin CC, Sineshaw HM, Jemal A. The impact of dependent coverage expansion under the Affordable Care Act on time to breast cancer treatment among young women. PLoS One 2018;13(6):e0198771. (In eng). DOI: 10.1371/journal.pone.0198771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sabik LM, Tarazi WW, Hochhalter S, Dahman B, Bradley CJ. Medicaid Expansions and Cervical Cancer Screening for Low-Income Women. Health Serv Res 2018;53 Suppl 1:2870–2891. (In eng). DOI: 10.1111/1475-6773.12732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Soni A, Simon K, Cawley J, Sabik L. Effect of Medicaid Expansions of 2014 on Overall and Early-Stage Cancer Diagnoses. Am J Public Health 2018;108(2):216–218. (In eng). DOI: 10.2105/AJPH.2017.304166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zhao J, Mao Z, Fedewa SA, et al. The Affordable Care Act and access to care across the cancer control continuum: A review at 10 years. CA Cancer J Clin 2020. (In eng). DOI: 10.3322/caac.21604. [DOI] [PubMed] [Google Scholar]
- 13.Loehrer AP, Chang DC, Hutter MM, et al. Health Insurance Expansion and Treatment of Pancreatic Cancer: Does Increased Access Lead to Improved Care? J Am Coll Surg 2015;221(6):1015–22. (In eng). DOI: 10.1016/j.jamcollsurg.2015.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Eguia E, Cobb AN, Kothari AN, et al. Impact of the Affordable Care Act (ACA) Medicaid Expansion on Cancer Admissions and Surgeries. Ann Surg 2018;268(4):584–590. (In eng). DOI: 10.1097/SLA.0000000000002952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mohanty S, Bilimoria KY. Comparing national cancer registries: The National Cancer Data Base (NCDB) and the Surveillance, Epidemiology, and End Results (SEER) program. J Surg Oncol 2014;109(7):629–30. (In eng). DOI: 10.1002/jso.23568. [DOI] [PubMed] [Google Scholar]
- 16.Hoehn RS, Rieser CJ, Phelos H, et al. Association Between Medicaid Expansion and Diagnosis and Management of Colon Cancer. J Am Coll Surg 2020. (In eng). DOI: 10.1016/j.jamcollsurg.2020.10.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.KFF. Health Insurance Coverage of the Total Population. (https://www.kff.org/other/state-indicator/total-population/?currentTimeframe=0&sortModel=%7B%22colId%22:%22Location%22,%22sort%22:%22asc%22%7D).
- 18.Gan T, Sinner HF, Walling SC, et al. Impact of the Affordable Care Act on Colorectal Cancer Screening, Incidence, and Survival in Kentucky. J Am Coll Surg 2019;228(4):342–353.e1. (In eng). DOI: 10.1016/j.jamcollsurg.2018.12.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Versteijne E, Suker M, Groothuis K, et al. Preoperative Chemoradiotherapy Versus Immediate Surgery for Resectable and Borderline Resectable Pancreatic Cancer: Results of the Dutch Randomized Phase III PREOPANC Trial. J Clin Oncol 2020;38(16):1763–1773. (In eng). DOI: 10.1200/JCO.19.02274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Oba A, Ho F, Bao QR, Al-Musawi MH, Schulick RD, Del Chiaro M. Neoadjuvant Treatment in Pancreatic Cancer. Front Oncol 2020;10:245. (In eng). DOI: 10.3389/fonc.2020.00245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lutfi W, Zenati MS, Zureikat AH, Zeh HJ, Hogg ME. Health Disparities Impact Expected Treatment of Pancreatic Ductal Adenocarcinoma Nationally. Ann Surg Oncol 2018;25(7):1860–1867. (In eng). DOI: 10.1245/s10434-018-6487-5. [DOI] [PubMed] [Google Scholar]
- 22.McGhan LJ, Etzioni DA, Gray RJ, Pockaj BA, Coan KE, Wasif N. Underuse of curative surgery for early stage upper gastrointestinal cancers in the United States. J Surg Res 2012;177(1):55–62. (In eng). DOI: 10.1016/j.jss.2012.03.013. [DOI] [PubMed] [Google Scholar]
- 23.Swords DS, Mulvihill SJ, Brooke BS, Firpo MA, Scaife CL. Size and Importance of Socioeconomic Status-Based Disparities in Use of Surgery in Nonadvanced Stage Gastrointestinal Cancers. Ann Surg Oncol 2019. (In eng). DOI: 10.1245/s10434-019-07922-7. [DOI] [PubMed] [Google Scholar]
- 24.Tohme S, Kaltenmeier C, Bou-Samra P, Varley PR, Tsung A. Race and Health Disparities in Patient Refusal of Surgery for Early-Stage Pancreatic Cancer: An NCDB Cohort Study. Ann Surg Oncol 2018;25(12):3427–3435. (In eng). DOI: 10.1245/s10434-018-6680-6. [DOI] [PubMed] [Google Scholar]
- 25.Shapiro M, Chen Q, Huang Q, et al. Associations of Socioeconomic Variables With Resection, Stage, and Survival in Patients With Early-Stage Pancreatic Cancer. JAMA Surg 2016;151(4):338–45. (In eng). DOI: 10.1001/jamasurg.2015.4239. [DOI] [PubMed] [Google Scholar]
- 26.Miller-Ocuin JL, Zenati MS, Ocuin LM, et al. Failure to Treat: Audit of an Institutional Cancer Registry Database at a Large Comprehensive Cancer Center Reveals Factors Affecting the Treatment of Pancreatic Cancer. Ann Surg Oncol 2017;24(8):2387–2396. (In eng). DOI: 10.1245/s10434-017-5880-9. [DOI] [PubMed] [Google Scholar]


