Abstract
Background:
In an underdeveloped country like India where there are varied constraints in accessing healthcare, telemedicine can prove to be instrumental in providing access to the scant medical resources and infrastructures. The irony lies in its underutilization, which is multifactorial.
Objective:
The present research was planned to evaluate the level of awareness, knowledge, and attitude toward telemedicine among the faculty members of tertiary-care teaching centers in Chhattisgarh, India.
Methods:
A questionnaire-based survey was conducted to collect appropriate data, which were utilized for analysis as well as various intergroup analyses (among different designations, age groups, sex, and worksite). The data have been presented as median and percentage, while for intergroup comparison Mann-Whitney Test was performed.
Results:
Among the 115 respondents, only 34% were females. The mean age was around 40.7 years, and 58% were <40 years of age. Their median scores of awareness, knowledge, and attitude were estimated to be 06, 14, and +9, respectively. No statistically significant difference was observed in the awareness, knowledge, and attitude among the faculty members belonging to different designations, age groups, and worksites.
Conclusions:
Though, in general, the faculty members have demonstrated a favorable attitude toward the use of telemedicine yet most of them scored below the median mark. Furthermore, the estimated level of knowledge and awareness was also mediocre.
Keywords: e-health, tele-education, telemedicine
Introduction
The provision of medical information and services using telecommunication and information technology defines telemedicine.[1] While telehealth can be defined as “The delivery and facilitation of health and health-related services including medical care, provider and patient education, health information services, and self-care via telecommunications and digital communication technologies.”[2] Based on different modalities, the application of telemedicine can be classified (i) according to the mode of communication (audio and video), (ii) transmission of information (synchronous/asynchronous), (iii) the aim of the interaction (first consultation or follow-up), and (iv) interaction among the individuals (patient and healthcare worker; HCW; HCW-HCW).[3]
India started developing telemedicine facilities two decades back. From 2003 to 2004 onward, numerous telemedicine nodes were established throughout the country. Further, in 2009, the National Rural Telemedicine Network (NRTN) and National Medical College Network (NMCN) were conceived and started in 2012–2013. The National Knowledge Network (NKN), another initiative by the Government of India, was brought up to connect all academic institutions in the country. The aim is to integrate with the global scientific community. As of now, NKN has already interconnected 831 institutions, including 151 medical institutions.[4]
Telemedicine has wide applications in medical education and research. It helps deliver healthcare facilities using mobile health clinics, online consultation with the experts for diagnosis, screening, and management (including follow-up) of a disease. Comprehensive details of the uses of telemedicine can be found elsewhere.[5,6,7]
Considering the immense potential of telemedicine in delivering health services, India, along with other countries, has not been able to utilize its full potential.[8] The underutilization of services is multifactorial. From an administrative point of view, a lack of uniform policy for telemedicine practice, poor organizational structure, and regulation are significant factors contributing to inappropriate usage.[9] Professionally, a relative lack of knowledge and skills for the practice of telemedicine among physicians and other supporting staff with rapidly evolving information technology also contribute to inefficient utilization of telemedicine services.[10] As telemedicine requires a costly high-end setup of information and communication technology (ICT) with considerable technical expertise, it also hinders the uses of its full potential.[11] Due to a lack of guidelines regarding telemedicine practice, there are multiple legal issues regarding the patient's consent and privacy.[10] Lastly, reluctance toward the acceptability of telemedicine by physicians and patients is also responsible for its underutilization.[12] Telemedicine can only be fully utilized if the primary care physicians who are working in the periphery and remote areas are used to the technology as they are an important link between patients and higher centers.
In the current ongoing crisis of Coronavirus Disease (COVID-19), telemedicine seems to play a significant role in medical education and healthcare delivery. Further, remote consultation has also helped the patients, especially in chronic diseases where multiple follow-ups are required. Although the theoretical aspects of medical education have been covered nicely, telemedicine will have minimal utility in developing surgical and clinical skills, patient interaction/counseling.[13] In continuation, many issues need to be addressed regarding the practice of telemedicine. Telemedicine practice guidelines provide a regulatory framework for practicing telemedicine. The guidelines define the eligibility criteria of physicians, modes of communication, patient consent, confidentiality, data privacy, use of telemedicine in emergencies, types of drugs that can be prescribed, and responsibilities of the apex regulatory body.[14]
The accomplishment of any program relies on multiple factors like the knowledge about the concept, attitude toward implementation, and skills required for making it feasible. Telemedicine is an emerging technology in the Indian health sector that is still underutilized, so it requires studies to recognize the healthcare workers' and patients' knowledge, awareness, and attitude toward telemedicine. The current study was aimed to evaluate the knowledge, awareness, and attitude of the faculty members toward telemedicine in Chhattisgarh, India. The study outcomes will enable us to know the deficits among the professionals that may contribute to the underutilization of telemedicine services.
Material and Methods
It was a cross-sectional questionnaire-based study for which due approval from the Institutional Ethics Committee (vide letter no. 718/IEC-AIIMSRPR/2019 dated 05.08.2019) was obtained. Chhattisgarh is situated in central India with over 30 million people.[15] Currently, in Chhattisgarh, there are 10 tertiary-care teaching hospitals in which around 1,000 faculty members are working at different designations. The sample size was obtained using the formula for finite population correction. Due to the lack of previous studies in this population, the proportion of telemedicine awareness knowledge, and attitude of 50%, gives us maximum variability with a 95% confidence interval with a relative precision of 10%.[16]
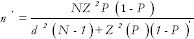
Where n′ = sample size, N = total population size,
Z = 1.96, P = expected proportion (P = 50%), and d = precision (d = 0.1)
The calculated sample size was 88. Our study planned to enroll a minimum of 100 faculty members (convenient sampling) from various institutions. Based on the sample size, the faculty members of different tertiary-care teaching hospitals were contacted. The faculty members, willing to fill the questionnaire, were considered to have consented to the study. The same was mentioned at the start of the questionnaire. Declined consent by the faculty members was the only exclusion criteria.
This questionnaire-based survey was carried out from August 2019 to April 2020, among the various faculty members of tertiary-care teaching hospitals of Chhattisgarh, India, after taking written permission from the heads of the respective institutes. A tertiary-care teaching hospital typically has two divisions, i.e. a medical college and an associated hospital.
The survey was conducted by two of the authors after physically visiting the institutes. The investigators visited the medical college and hospital with the facilitator provided by the respective institute. The faculty members were contacted, and a questionnaire was distributed. Along with the questionnaire, the faculty members were informed about the study's aims, and a volunteer information sheet was also provided. The questionnaire was collected. The data were preserved in the physical form as well as electronically.
This study was carried out to figure out the level of awareness, knowledge, and attitude toward telemedicine among the faculty members of tertiary-care teaching hospitals of Chhattisgarh.
The questionnaire was prepared by the contributors after a comprehensive review of the literature.[17,18,19,20,21] The questionnaire contents were assessed after consultation with the faculty of AIIMS Raipur and in charge of the telemedicine facility (expert consultation). Twenty-five faculty members from AIIMS Raipur were selected randomly for reviewing and rating the relevance of each parameter in the questionnaire, with a four-point Likert scale (1 = not relevant, 2 = somewhat relevant, 3 = relevant, 4 = very relevant). The Content Validity Index (CVI) was then estimated, and accordingly, the parameters were validated.[22]
This validated questionnaire used for the survey consists of four sections: (A) Demographic details; (B) Awareness about telemedicine; (C) Knowledge regarding telemedicine; (D) Attitude toward telemedicine.
In section A, personal and professional information was sought from the participants (name, age, sex, designation, qualification, subject, and institution). Section B was composed of eight statements to evaluate their awareness of telemedicine. Out of the eight statements, four statements were about the initiatives by the Government of India, and the other four were different terminologies of telemedicine. This section required a graded response on a three-point scale ranging from 0 to 2, i.e. '0,' '1,' and '2' for 'do not know,' 'heard of it, and 'know about it,' respectively (maximum score possible was 16).
Section C consisted of seven assertions to evaluate the knowledge of the respondents concerning telemedicine. The response was graded as 0 for 'NO, '1' for 'somewhat,' '2' for 'mediocre' and, '3' for 'expert' (maximum and minimum scores possible were 21 and 0, respectively). Section D consisted of eight statements that were formed to assess the attitude of the participants. This section also required a graded response, i.e. '-2' for strongly disagree, '-1' for disagree, '0' for undecided, '+1' for agree, and '+2' strongly agree (maximum and minimum scores possible were +16 and -16, respectively).
The reliability was assessed for the different domains of the questionnaire in 20 faculty members using Cronbach's α value.[23] Before conducting the survey, the questionnaire was validated, and the reliability score (Cronbach's α) for awareness, knowledge, and attitude was found to be 0.74, 0.93, and 0.85, respectively.
The study was carried out by the investigators personally visiting the institutes in different districts of Chhattisgarh. Accordingly, the bias that could have been encountered was interviewing only those faculty members available on the day of the visit.
The data were segregated and compared based on four parameters, i.e. designation, age, sex, and working site (hospital vs. medical college). The designation was chosen because the faculties at the higher post (professor) are involved in planning and implementing different projects in addition to their routine work, while the lower post (assistant professor) are commonly involved in routine works allotted to them. In between, the associate professors act as links between them. It is assumed that the younger ones are more technology-friendly, so the comparison was performed among the different age groups. Regarding the working site, the duties of the faculty vary as per the working site. The faculty working in the hospital is involved in patient care, teaching, and research, whereas medical colleges are involved in teaching, research, and lab services. Accordingly, they have a different distribution of working time.[24] The data were analyzed based on the median and percentage scores. Furthermore, intergroup comparisons were carried out by using the Mann–Whitney Test (wherein the P value < 0.05 was assumed statistically significant) using Microsoft Excel 2016.
Results
The study was conducted from August 2019 to April 2020, wherein all the tertiary-care teaching hospitals of Chhattisgarh, India, were contacted, and all had consented to participate except for one institute, where due permission could not be obtained. Eventually, the result discussed hereafter encompasses the data collected from the faculty members of nine tertiary-care teaching hospitals.
Population
Out of the 115 faculty members interviewed, 76 (66%) were males, and 39 (34%) were females, with the mean age of the participants being 40.7 years and 41.8% being above the age of 40 years. All the faculty members held a post-graduate degree in their respective fields and were either assistant professors (59), or associate professors (31), or Professors (25). Moreover, out of these 115 participants, 49 were deputed at the hospital, and the rest belonged to the medical college [Table 1].
Table 1.
Demographic and professional characteristics of faculty members
| Demographic Characteristics | |
|---|---|
| Age years (mean±SD) | 40.7±9.2 |
| Male: Female (Total) | 76 (66%):39 (34%) (115) |
| Assistant Professors | 59 (51.3%) |
| Associate Professors | 31 (27%) |
| Professors | 25 (21.7%) |
| Faculty members from Medical College | 65 (56.5%) |
| Faculty members from Hospital | 50 (43.5%) |
Attitude
The median score of 09 (-16 to + 16) reflected a positive attitude of the members toward the concept of telemedicine. Moreover, the same was validated with the observation that almost 90.4% of them agreed with the usefulness of telemedicine in improving access to healthcare facilities, even though 66.1% were concerned about the curtailed face-to-face communication and 53.9% were with the view that it will not be able to simulate in-person interaction. A considerable proportion (80.1%) appreciated the idea of remote communication as one of the added advantages. For better management and functionality of the telemedicine project, 95.7% acknowledged the importance of computers and information technology in healthcare, 93% agreed that regular CMEs and workshops should be held. On the other hand, 83.5% were ready to educate patients regarding the operational use of telemedicine, and 61.7% were willing to work in rural areas for the project [Table 2].
Table 2.
Attitude toward telemedicine among faculty members of different institutions
| Category | Strongly agree (%) | Agree (%) | Not sure (%) | Disagree (%) | Strongly disagree (%) |
|---|---|---|---|---|---|
| Reduction in face-to-face communication | 20.9 | 45.2 | 15.7 | 13.9 | 4.4 |
| Idea of remote communication | 44.4 | 35.7 | 13 | 5.2 | 1.7 |
| Willingness to educate patients for uses of Telemedicine | 35.7 | 47.8 | 9.6 | 5.2 | 1.7 |
| Medical colleges should organize CMEs | 70.4 | 22.6 | 2.6 | 2.6 | 1.7 |
| Computers has significant role in medicine and healthcare | 74.8 | 20.9 | 2.6 | 0.9 | 0.9 |
| Work in rural area for telemedicine project | 27.8 | 33.9 | 30.4 | 3.5 | 4.4 |
| Telemedicine will improve access to healthcare facilities | 48.7 | 41.7 | 7.8 | 00 | 1.7 |
| Telemedicine will be same as in-person interaction | 19.1 | 27 | 20 | 22.6 | 11.3 |
Knowledge
The scoring in terms of knowledge regarding various aspects of telemedicine was largely mediocre, which was ascertained by the median score as well 14 (0–21). Concerning the knowledge of computer-assisted learning, library computer catalogs, performing an online literature review, saving the webpages offline, and tele-education, 43.5, 40.9, 45.2, 40.9, and 47% of the participants, respectively, had mediocre scores. Nevertheless, concerning the knowledge of the routine use of e-mails (either in mobile or computer) and Microsoft Office, most of the faculty members had scores to an expert level (52.2 and 50.2%, respectively) [Table 3].
Table 3.
Self-perceived knowledge of telemedicine among faculty members of different institutions
| Knowledge | ||||
|---|---|---|---|---|
| Category | No (%) | Somewhat (%) | Mediocre (%) | Expert (%) |
| Computer-assisted learning | 6.1 | 22.6 | 43.5 | 27.8 |
| Library computer catalog | 13.9 | 33.9 | 40.9 | 11.3 |
| Performing online literature review | 3.5 | 13 | 45.2 | 38.3 |
| Offline saving of webpage | 6.9 | 16.5 | 40.9 | 35.7 |
| Microsoft Office | 3.5 | 13 | 33 | 50.4 |
| Routine use of e-mails in both mobile and computers | 1.7 | 7.8 | 38.3 | 52.2 |
| Tele-education* | 6.9 | 23.5 | 47 | 21.7 |
*Digital lecture theater room for Continuous Medical Education for Medical Persons, training of Para Medical staff, sharing of surgical, and interventional skills.
Awareness
The questions about awareness about the various telemedicine projects initiated by the Government of India and about the application of telemedicine were grouped. The median score for awareness 06 (0–16) indicated that most participants (59.1 and 57.4%, respectively) had only heard about the aforementioned themes.
Comparison among Groups
The pooled median score for the awareness, knowledge, and attitude among the recruited faculty members was 06, 14, and 09, respectively, as represented earlier. The authors observed that the median score for awareness and attitude was comparatively lower in the group of assistant professors, while the median score of knowledge was higher in the associate professors' group. Within the group of professors, the median score for awareness was better than the pooled median, while the opposite held for the median score of attitude.
On the other hand, the faculty from the medical colleges had a lower median score of awareness. Similarly, those faculty members who were aged ≥40 years demonstrated a better median awareness score as against those who were <40 years, though they had a better knowledge score. Among the respondents, the males had a better awareness and attitude score as compared to the females [Table 4]. The number of faculty members who scored below median was found to be 69 (60%), 60 (52%), and 63 (54.8%) for attitude, knowledge, and awareness, respectively. The critical finding of this study was that no statistically significant difference was observed when the intergroup comparison among faculty members belonging to different designations was performed. Except for the comparison between professors and assistant professors, a statistically significant difference was found regarding the awareness score (P = 0.01).
Table 4.
Representation of median score of awareness, knowledge, and attitude among the faculty members toward telemedicine
| Subgroups | Awareness (16) | Knowledge (21) | Attitude (16) |
|---|---|---|---|
| Pooled Median (115) | 6 | 14 | 9 |
| Assistant Professor (59) | 5 | 14 | 8 |
| Associate Professors (31) | 6 | 16 | 9 |
| Professors (25) | 8 | 14 | 8 |
| Faculty from Hospital (50) | 6.5 | 13.5 | 9 |
| Faculty from Medical College (65) | 5 | 14 | 9 |
| Faculty ≥40 years (48) | 7 | 13.5 | 9 |
| Faculty <40 years (67) | 5 | 15 | 9 |
| Males (76) | 6.5 | 14 | 9 |
| Females (39) | 5 | 15 | 8 |
Furthermore, in another comparison between the associate and assistant professors, statistically significant results were found regarding the knowledge score (P = 0.03). However, no statistically significant difference for the same framework was observed among the faculty members who were ≥40 or <40 years of age. Moreover, a similar trend was noticed among the faculty members who were either males or females or belonged to the hospital or medical college [Table 5].
Table 5.
Comparison among different groups by Mann-Whitney Test regarding awareness, knowledge, and attitude
| Groups | Awareness (P) | Knowledge (P) | Attitude (P) |
|---|---|---|---|
| Assistant Professor and Associate Professor | 0.39 | 0.03* | 0.71 |
| Assistant Professor and Professor | 0.01* | 0.86 | 0.20 |
| Professor and Associate Professor | 0.14 | 0.12 | 0.41 |
| Faculty ≥40 and Faculty <40 years | 0.21 | 0.15 | 0.11 |
| Faculty Medical College and Hospital | 0.87 | 0.45 | 0.88 |
| Male and Female | 0.31 | 0.45 | 0.84 |
*Statistically significant
Discussion
The study was conducted in nine tertiary-care teaching hospitals of Chhattisgarh. The female representation among the participants for this survey was comparatively less (34%) against the male representation (66%). This corroborates the fact that among modern medicine practitioners, the percentage of women is low (16.8%).[25] However, in tertiary-care teaching hospitals, this ratio seems to be better. Among the faculty members, most of them were at the assistant professor designation, which could be attributed to the recruitment trend as advised by the National Medical Commission.[26] Akin to the previous study wherein only 27% of hospital-based faculty had participated, in our study as well, only 43.5% of the faculty belonging to the hospital had participated.[27] The hospital site's plausible reasons for this modest participation could be fixed outpatient days (as investigators visited only outpatient departments), higher patient load making the interaction complex, and reluctance for participation. Most of the participants (58.3%) in our study were <40 years of age [Table 4], which is also similar to the previous studies.[16,27]
Similar to previous studies, in the present study, most of the faculty members showed a favorable attitude toward the utility and relevance of telemedicine in medical education and patient care. A critical study by Demartines et al., 2000[18] showed a positive attitude among 71% of the surgeons toward telemedicine in surgical teaching. The study results conducted by George et al., 2007,[20] were also not different as 71% of the doctors opined telemedicine as a potential tool in future healthcare delivery. In another study, 90.9% of the doctors had the view that telemedicine is essential.[21,28] Likewise, in other studies, most of the doctors interviewed had a favorable attitude toward the real-life utilization of telemedicine.[16,29,30] But the study conducted by Ashfaq et al. 2020[31] concluded differently as 28.1% of the participants opined that telemedicine might help provide medical care. In the same study, 42.9% opined that telemedicine might disrupt the doctor–patient relationship; this finding has also been reported in our study [Table 2]. The importance of telemedicine for improving access to health care was recognized by medical students of France, resident doctors of India, and health care workers of Libya.[32,33,34]
Even though the teaching physicians have a positive attitude toward the utilization of telemedicine in real-world scenarios, their technical knowledge for the same is sketchy. The cause could be their average proficiency in information technology (IT), which is not their primary domain, though telemedicine can be practiced with this much level of information.[35] The studies conducted on a similar pattern concluded with similar findings as ours, i.e. less than 50% of the participating respondents had a sound technical knowledge of telemedicine.[16,18,20,21] In another study, 43% of the healthcare professionals reported a lack of knowledge about IT.[36] Similarly, different investigators from different countries have reported the limited knowledge of telemedicine technology.[31,32,34]
The authors also assessed awareness about different projects initiated by the Government of India and the application of telemedicine. It was interesting to observe that more than 50% of the participants reportedly were aware of telemedicine.[18,21] But there were a few studies that concluded with contrasting results. The studies conducted by Sheikhtaheri et al.,[29] 2016, Ghafari et al. 2019,[30] and Ullah et al. 2020[36] reported that 43.7, 35.5, and 46% of the participants, respectively, were aware of telemedicine.
Intergroup comparisons for awareness, knowledge, and attitude were also made among faculties at different designations, age, sex, and worksite, and, no significant difference was apparent, except for in two settings (mentioned in results). The professors were more aware of telemedicine than the assistant professors, which could be linked up to their work profile, as being senior faculties, they have higher chances of getting involved in planning and implementing national projects.[24]
The insignificant difference among the faculty members between different work sites is not similar to the previous study.[34] In the author's opinion, the significant difference in the level of knowledge among the assistant and associate professors observed could be a coincidence, as they usually belong to a similar age group without much difference in their experience and job profile.[37]
As discussed earlier in this article, telemedicine's total utilization depends on multifactorial components, and with this study, we could reflect on the potential areas of improvement on the user's professional front. If this study is further extended to district hospitals, community health centers, and rural health centers, a broader picture of doctors' and para-medics acceptability toward telemedicine in routine use can be gained. Furthermore, studies investigating the availability of resources for telemedicine would add up in eliminating the deficiencies which hinder its actual world utilization. Being a low-middle income country with a vast population, India grossly lacks both financial and workforce resources.[38] Add on to that the budget allocated to health and related services in India is only 1.6% of its GDP, which is not only less but also adversely affected because of the COVID-19 crisis.[39,40] Under these circumstances, the implementation of telemedicine facilities is likely to be further delayed. Another valuable after-effect of this study could be that since most of the data collection was done before the ongoing COVID-19 crisis, it provides baseline data that could later be compared with a similar survey post-COVID-19 pandemic.
As far as telemedicine in India is concerned, it is in the primitive stage as detailed guidelines for the same were approved in March 2020. As per the data from NMCN to date, 6,433 sessions mainly for academic purpose have been conducted since 2009.[41] Regarding the establishment of infrastructure to connect the different strata of healthcare, the process is in the initial stages of development.[42] Most of the practice of telemedicine in the previous years was involving HCW to HCW. The significant factors that direct acceptability are age, sex, profession, and education.[43] The delivery of e-health directly to the patient will ultimately remain dependent on acceptability by patients and HCWs. Further, it was hard to find any scientifically sound study that could estimate physicians practicing e-health; however, reports indicate an expected rise of telemedicine practice in India.[44] This age-old technology is likely to bridge the healthcare gap, especially in small towns, supported by the growing number of Internet users in India.[44] With this current COVID-19 pandemic situation, the necessity of a proper setup for telemedicine has been understood. The significant limitations include relatively smaller sample size and the involvement from tertiary-care teaching hospitals only. The skill required to practice telemedicine has also not been assessed.
Conclusion
The current study gives a general idea of awareness, knowledge, and attitude toward telemedicine in Chhattisgarh. This study informs us that faculty members have a positive attitude and appropriate knowledge. The study indicates that despite telemedicine having started in early 2000, it still has to go a long way as about 28% of the medical institutions are connected via NKN/NMCN. Probably, the lack of infrastructure and proper guidelines, telemedicne is underutilized. These all are organizational factors and are correctable. Concerning the enormous potential of its use in the field of medicine, it still stands very far.
Key Messages
The study finds a favorable attitude of the faculty members with decent knowledge and awareness toward telemedicine.
No significant difference in awareness, knowledge, and attitude in the faculty members of different designations, age groups, sex, and worksites was observed.
The study suggests that the optimum utilization of telemedicine requires more efforts from the administration by improving awareness and knowledge required to practice telemedicine.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
Authors wish to thank Dr. Ekta Khandelwal (In-charge Telemedicine) for valuable inputs.
References
- 1.Field MJ. Telemedicine: A Guide to Assessing Telecommunications in Health Care. Washington (DC): National Academies Press (US); 1996. [PubMed] [Google Scholar]
- 2.Global Health Observatory (GHO) data. 2016. [[Last accessed on 2021 May 10]]. Available from: https://www.who.int/gho/goe/telehealth/en/
- 3.WHO Global Observatory for eHealth. Telemedicine: Opportunities and developments in Member States: Report on the second global survey on eHealth. World Health Organization. 2010. [[Last accessed on 2021 May 10]]. Available from: https://apps.who.int/iris/handle/10665/44497 .
- 4.Evolution of Telemedicine in India: Brief Summary. 2020. [[Last accessed on 2021 May 10]]. Available from: https://www.nhm.gov.in/images/pdf/Telemedicine/Telemedicine.pdf .
- 5.Chellaiyan VG, Nirupama AY, Taneja N. Telemedicine in India: Where do we stand? J Family Med Prim Care. 2019;8:1872–6. doi: 10.4103/jfmpc.jfmpc_264_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Agarwal N, Jain P, Pathak R, Gupta R. Telemedicine in India: A tool for transforming health care in the era of COVID-19 pandemic. J Educ Health Promot. 2020;9:190. doi: 10.4103/jehp.jehp_472_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Garshnek V, Burkle FM., Jr Applications of telemedicine and telecommunications to disaster medicine: Historical and future perspectives. J Am Med Inform Assoc. 1999;6:26–37. doi: 10.1136/jamia.1999.0060026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Surya Bali (December 5th 2018). Barriers to Development of Telemedicine in Developing Countries, Telehealth, Thomas F. Heston, IntechOpen. DOI: 10.5772/intechopen.81723. Available from: https://www.intechopen.com/books/telehealth/barriers-to-development-oftelemedicine-in-developing-countries .
- 9.Zanaboni P, Lettieri E. Institutionalizing telemedicine applications: The challenge of legitimizing decision-making. J Med Internet Res. 2011;13:e72. doi: 10.2196/jmir.1669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Alghatani KM. Telemedicine implementation: Barriers and recommendations. J Sci Res Stud. 2016;3:140–5. [Google Scholar]
- 11.'Using Telemedicine to Treat Patients in Underserved Areas: Health Telemedicine Case World Bank Group. https://www.innovationpolicyplatform.org/www.innovationpolicyplatform.org/system/files/2_%20Health%20Telemedicine%20Case_Jun15/index.pdf. [Google Scholar]
- 12.Alaboudi A, Atkins A, Sharp B, Balkhair A, Alzahrani M, Sunbul T. Barriers and challenges in adopting Saudi telemedicine network: The perceptions of decision makers of healthcare facilities in Saudi Arabia. J Infect Public Health. 2016;9:725–33. doi: 10.1016/j.jiph.2016.09.001. [DOI] [PubMed] [Google Scholar]
- 13.Sharma D, Bhaskar S. Addressing the Covid-19 burden on medical education and training: The role of telemedicine and tele-education during and beyond the pandemic. Front Public Health. 2020;8:589669. doi: 10.3389/fpubh.2020.589669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Telemedicine Practice Guidelines. 2020. [[Last accessed on 2021 May 10]]. Available from: https://www.mohfw.gov.in/pdf/Telemedicine.pdf .
- 15.Chhattisgarh Population 2011 – 2021. 2021. [[Last accessed on 2021 May 10]]. Available from: https://www.census2011.co.in/census/state/chhattisgarh.html .
- 16.Biruk K, Abetu E. Knowledge and attitude of health professionals toward telemedicine in resource-limited settings: A cross-sectional study in North West Ethiopia? J Healthc Eng. 2018;2018:2389268. doi: 10.1155/2018/2389268. doi: 10.1155/2018/2389268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bryson M, Tidy N, Smith M, Levy S. An online survey of nurses' perceptions, knowledge, and expectations of the National Health Service modernization programme. J Telemed Telecare. 2005;11((1_Suppl)):64–6. doi: 10.1258/1357633054461732. [DOI] [PubMed] [Google Scholar]
- 18.Demartines N, Freiermuth O, Mutter D, Heberer M, Harder F. Knowledge and acceptance of telemedicine in surgery: A survey. J Telemed Telecare. 2000;6:125–31. doi: 10.1258/1357633001935167. [DOI] [PubMed] [Google Scholar]
- 19.Ibrahim MIM, Phing CW, Palaian S. Evaluation on knowledge and perception of Malaysian health professionals toward telemedicine. J Clin Diag Res. 2010;3:2052–7. [Google Scholar]
- 20.George JT, Rozariow KS, Abraham A. A survey in India of doctors' knowledge, attitudes, and practice regarding telemedicine and e-health. J Telemed Telecare. 2007;13:322. doi: 10.1258/135763307781644924. [DOI] [PubMed] [Google Scholar]
- 21.Meher SK, Tyagi RS, Chaudhry T. Awareness and attitudes to telemedicine among doctors and patients in India. J Telemed Telecare. 2009;15:139–41. doi: 10.1258/jtt.2009.003011. [DOI] [PubMed] [Google Scholar]
- 22.Lynn MR. Determination and quantification of content validity. Nur Res. 1986;35:382–5. [PubMed] [Google Scholar]
- 23.Mondal H, Mondal S. Calculation of Cronbach's alpha in spreadsheet: An alternative to costly statistics software. J Sci Soc. 2017;44:117–8. [Google Scholar]
- 24.Work standards for faculty of autonomous institutions of medical education under the department of health and family welfare, Government of India. 2012. [[Last accessed on 2021 May 10]]. Available from: https://www.aiims.edu/aiims/committee/Sneh%20Barghava%20Commitee%20%20Report.PDF .
- 25.Anand S, Fan V. The Health Workforce in India. 2016. [[Last accessed on 2021 May 10]]. Available from: https://www.who.int/hrh/resources/16058health_workforce_India.pdf .
- 26.National Medical Commission. 2020. [[Last accessed on 2021 May 10]]. Available from: https://www.nmc.org.in/rules-regulations/minimum-requirementsfor-annual-m-b-b-s-admissions-regulation2020 .
- 27.Zayapragassarazan Z, Kumar S. Awareness, knowledge, attitude, and skills of telemedicine among health professional faculty working in teaching hospitals. J Clin Diagn Res. 2016;10:JC01–4. doi: 10.7860/JCDR/2016/19080.7431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Malhotra P, Ramachandran A, Chauhan R, Soni D, Garg N. Assessment of knowledge, perception, and willingness of using telemedicine among medical and allied healthcare students studying in private institutions. Telehealth Med Today. 2020;5 doi: 10.30953/tmt.v5.228. [Google Scholar]
- 29.Sheikhtaheri A, Sarbaz M, Kimiafar K, Ghayour M, Rahmani S. Awareness, attitude and readiness of clinical staff toward telemedicine: A study in Mashhad, Iran. Stud Health Technol Inform. 2016;228:142–6. [PubMed] [Google Scholar]
- 30.Ghafari SF, Mahdizadeh J, Valinejadi A, Mehraeen E, Mohammadpour A, Bouraghi H, et al. Iranian physicians' expectations of telemedicine development and implementation infrastructures in teaching hospitals. AIMS Public Health. 2019;6:514–22. doi: 10.3934/publichealth.2019.4.514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ashfaq A, Memon SF, Zehra A, Barry S, Jawed H, Akhtar M, et al. Knowledge and attitude regarding telemedicine among doctors in Karachi. Cureus. 2020;12:e6927. doi: 10.7759/cureus.6927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Yaghobian S, Ohannessian R, Iampetro T, Riom I, Salles N, de Bustos EM, et al. Knowledge, attitudes, and practices of telemedicine education and training of French medical students and residents? J Telemed Telecare. 2020 doi: 10.1177/1357633X20926829. doi: 10.1177/1357633X20926829. [DOI] [PubMed] [Google Scholar]
- 33.Das N, Narnoli S, Kaur A, Sarkar S, Balhara Y. Attitude to telemedicine in the times of COVID-19 pandemic: Opinion of medical practitioners from India. Psychiatry Clin Neurosci. 2020;74:560–2. doi: 10.1111/pcn.13109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Elhadi M, Elhadi A, Bouhuwaish A, Bin Alshiteewi F, Elmabrouk A, Alsuyihili A, et al. Telemedicine awareness, knowledge, attitude, and skills of health care workers in a low-resource country during the COVID-19 pandemic: Cross-sectional study. J Med Internet Res. 2021;23:e20812. doi: 10.2196/20812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Going Digital: The Essential Guide to Getting Started in Telemedicine. 2020. Aug 03, [[Last accessed on 2021 May 10]]. Available from: https://www.hcplive.com/view/going-digital-the-essential-guideto-getting-started-in-telemedicine .
- 36.Ullah S, Maghazil AM, Qureshi AZ, Tantawy S, Moukais IS, Aldajani AA. Knowledge and attitudes of rehabilitation professional toward telerehabilitation in Saudi Arabia: A cross-sectional survey. Telemed J E Health. 2021;27:587–91. doi: 10.1089/tmj.2020.0016. [DOI] [PubMed] [Google Scholar]
- 37.Aggarwal R, Gogtay N, Kumar R, Sahni P. The revised guidelines of the Medical Council of India for academic promotions: Need for a rethink. Indian Heart J. 2016;68((Suppl 2)):S1–3. doi: 10.1016/j.ihj.2016.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Low and middle income countries. 2021. [[Last accessed on 2021 May 10]]. Available from: https://data.worldbank.org/country/XO .
- 39.Health-care Industry in India. 2021. [[Last accessed on 2021 May 10]]. Available from: https://www.ibef.org/industry/healthcare India.aspx#:~:text=The%20Government%20has%20announced%20Rs, Product%20(GDP)%20by%202022 .
- 40.Current health expenditure. 2018. [[Last accessed on 2021 May 10]]. Available from: https://data.worldbank.org/indicator/SH.XPD.CHEX.GD.ZS .
- 41.National Telemedicne Portal. 2021. [[Last accessed on 2021 May 10]]. Available from: https://nmcn.in/totalsessions.php .
- 42.E-health and telemedicine. 2021. [[Last accessed on 2021 May 10]]. Available from: https://main.mohfw.gov.in/Organisation/departments-health-andfamily-welfare/e-Health-Telemedicine .
- 43.Haluza D, Naszay M, Stockinger A, Jungwirth D. Prevailing opinions on connected health in Austria: Results from an online survey. Int J Environ Res Public Health. 2016;13:813. doi: 10.3390/ijerph13080813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Telemedicine Startups Ride On Regulatory Clarity To Tap Demand Surge. https://inc42.com/features/telemedicinestartups-ride-on-regulatory-clarity-to-tap-demand-surge/


