Abstract
Background and Objectives:
The COVID-19 pandemic affected the mental health and psychosocial conditions of everyone worldwide according to the WHO. Public health emergencies affect college students and are expressed as anxiety, worry, and fear. The aim of this study was to assess the impact of COVID-19 on the psychological health and performance of medical students.
Design and Settings:
A cross-sectional study using an online survey was done.
Participants and Methods:
Participants were 1591 Saudi medical students. A predesigned questionnaire included questions on demographic characters, GPA, having a relative got COVID-19, how to face sad news and stressors, and satisfaction with online lectures. The Generalized Anxiety Disorder (GAD-7) scale was used that included seven items asking about the degree the participant was bothered by feeling anxious in the last 2 weeks.
Results:
A total of 59.4% of students had various degrees of anxiety. Participant age, unsteady family income, high grade point average (GPA,) satisfaction with the online lectures, and being female were associated with higher GAD-7 scores.
Conclusion:
Mental health of medical students was significantly affected by the COVID-19 pandemic. Psychological support programs for medical students during the pandemic and provision of high-quality distance learning is essential for psychological well-being during the pandemic.
Keywords: Academic, COVID-19, impact, medical, performance, psychological
Introduction
The novel coronavirus (COVID-2019) is an outbreak. It is viral pneumonia of unknown etiology, which originated at the end of December 2019 in Wuhan, China.[1,2,3] The pathogens of this illness were enveloped positive-stranded RNA viruses belonging to the coronavirus (CoV) family.[4,5] It is a highly contagious disease with a long incubation period; it is transmitted by respiratory droplets.[1,6] The main clinical manifestations of the disease are dry cough, dyspnea, fever (which occur in 99% of the affected persons), and patchy infiltration (bilateral upon imaging).[6,7]
Initially, there were no specific therapeutics or vaccines available; only supportive treatment was used.[4,8] All countries implemented social distancing, quarantine, and isolation to reduce the chance of contact between infected and noninfected persons.[9] Closure of the educational institutions was found to reduce the spread of the infectious disease in the community by breaking critical chains of transmission.[10,11,12] During the COVID-19 pandemic, many universities worldwide postponed or canceled all university activities and changed the education format from face-to-face to online courses.[13,14]
According to the World Health Organization (WHO) (2020), the COVID-19 pandemic can affect the mental health and psychosocial conditions of everyone.[10] Moreover, outbreaks can cause undesirable effects on the psychological health of students, which results in unfavorable effects on learning.[11,12] Similarly, some studies indicate that the psychological effects on college students by public health emergencies are expressed as anxiety, worry, and fear.[13]
Strict measures of isolation and delays in the starting dates of studies at colleges affected the mental health of students.[15] Quarantine increases the distance between people, which subsequently leads to the absence of interpersonal communication and affects student anxiety.[14]
The Kingdom of Saudi Arabia (KSA) started introducing decisive social distancing before the first case of COVID-19 was established. These measures ranged from the suspension of religious and sporting mass gatherings, entertainment, and events (e.g., the temporary closure of Umrah, mosques, educational establishments, and postponing all unnecessary meetings) to imposing a curfew.[10] A study was performed on students of the medical school of King Saud University in Riyadh in 2020 to investigate the impact of quarantine on the medical students' mental wellbeing and learning behavior. The above-mentioned study determined that medical students stated that quarantine caused them to feel emotionally detached from family, classmates, and friends and decrease their overall work and study performance. In addition, one-fourth of them felt disheartened during the quarantine period.[16]
To our knowledge, there are no studies available yet that assess the effect of COVID-19 on the psychological health and performance of medical students in KSA. Therefore, this study aimed to assess the effect of COVID-19 on the psychological health and performance of medical students.
Methodology
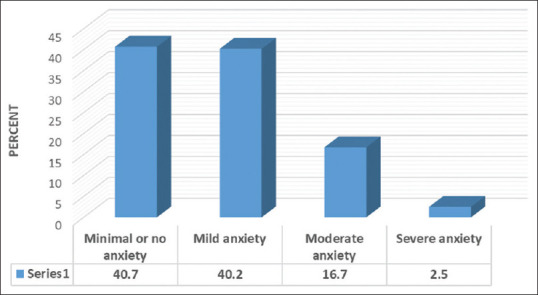
This study was a cross-sectional study that used an online-based survey from 22 May to 22 Jun 2020. The target sample size of participating medical students was determined using the formula:
In which, the estimated acceptable margin of error for proportion was 0.05, and 95% confidence level. So, the sample size was 379 students according to the formula. It increased according to the response of the participants to 1591 students. The inclusion criteria were all Saudi medical students who lived in Saudi Arabia, and the exclusion criteria were nonmedical students, nonSaudi medical students, Saudi medical students not living in Saudi Arabia. We used a predesigned questionnaire that had a first section containing items to collect data about the participants' demographic characters and their GPA in the 1st and 2nd semesters. The second section included items on having a relative or acquaintance got COVID-19, psychological questions such as how to face unwanted sad news, any of the related stressors, and their satisfaction with online lectures. The third section included the Generalized Anxiety Disorder (GAD-7) scale that was designed by Spitzer et al.[17] It is a scale of seven items that asks about the degree to which the participant was bothered by feeling anxious in the last 2 weeks. GAD7 is a patient health uestionnaire (PHQ)-generalized anxiety disorder item that was validated previously in a Saudi study where the Arabic version of the PHQ was approved to be a valid and reliable measure to screen depression, anxiety, somatic, and panic disorders in a Saudi sample.[18] Ethical approval was obtained from the Researchand Ethics committee of Taif University (Application no: 41-00188. The data were analyzed using the (SPSS) version 25, where qualitative data were expressed as numbers and percentages. Quantitative data were expressed as mean and standard deviation (Mean ± SD), where the Mann-Whitney (U) test and Kruskal Wallis tests were applied for nonparametric variables. Correlation analysis using Spearman's test was done, and a P value of <0.05 was considered as statistically significant.
Results
Table 1 shows that the mean age of the studied medical students was 23.36 ± 4.01 years. Of them, 55.1% were males, 29.7% were from the Western region of KSA, and 60.5% were senior students in the 4th, 5th and 6th grades. Of the participants, 81.55% had a steady family income, and 77.2% lived with parents.
Table 1.
Distribution of the studied participants according to their characters
| Variable | No. (%) |
|---|---|
| Age (mean±SD) | 23.36±4.01 |
| Gender | |
| Male | 876 (55.1) |
| Female | 715 (44.9) |
| Region | |
| Eastern | 254 (16) |
| Western | 472 (29.7) |
| Northern | 248 (15.6) |
| Southern | 259 (16.3) |
| Central | 358 (22.5) |
| Educational level | |
| Junior (1st-2nd-3rd) | 628 (39.5) |
| Senior (4th-5th-6th) | 963 (60.5) |
| Do you have a steady family income? | |
| Yes | 1296 (81.5) |
| No | 295 (18.5) |
| Do you live with your parents? | |
| Yes | 1228 (77.2) |
| No | 363 (22.8) |
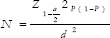
It was found that31.6% of the students knew a relative or acquaintance who got COVID-19 [Figure 1]. When we assessed the behavior of the students, it was found that49.3% of the participants faced unwanted bad news by thinking, 31.7% were worried about academic delays, and 57.1% thought that technology supports psychology [Table 2].
Figure 1.
Percentage of participants who know a relative (s) or acquaintance (s) infected with COVID-19
Table 2.
Distribution of the studied participants according to their behaviour
| Variable | No. (%) |
|---|---|
| How do you face unwanted bad news? | |
| Crying | 174 (10.9) |
| Carless | 371 (23.3) |
| Thinking | 785 (49.3) |
| Increase productivity | 261 (16.4) |
| Do you have any of these related stressors? | |
| Worry about academic influences | 440 (27.7) |
| Worry about academic delays | 505 (31.7) |
| Influence on daily life | 474 (29.8) |
| Social support | 172 (10.8) |
| Is technology supporting psychology? | |
| Yes | 908 (57.1) |
| No | 683 (42.9) |
| Score of Generalized Anxiety Disorder | 5.66±4.16 |
| Scale (GAD-7) (mean±SD) |
The table represents how the participants face bad news, type of stressors, having psychiatric illness, and their opinion of technology supporting psychology
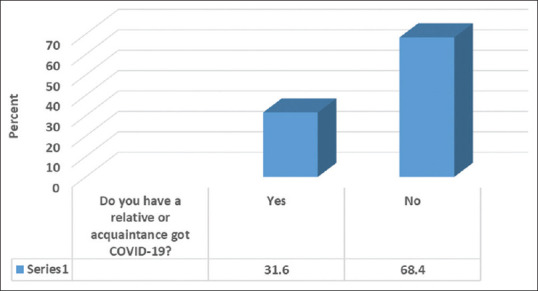
Table 3 shows that most of the students (59.6%) had a GPA of more than 3.5 in the 1st semester, compared to 62.3% in the 2nd semester. According to their satisfaction with the online lectures, 40.1% had moderate satisfaction, and 26.2% were not satisfied at all. On the other hand, 24.6% and 9.1% were so satisfied and very satisfied, respectively. The anxiety level of the students showed that 40.2%, 16.7%, and 2.5%, had mild, moderate, and severe anxiety respectively [Figure 2].
Table 3.
Distribution of the studied participants according to their GPA and their satisfaction with online lectures
| Variable | No. (%) |
|---|---|
| GPA in 1st semester | |
| <3 | 118 (7.4) |
| 3-3.5 | 525 (33) |
| >3.5 | 948 (59.6) |
| GPA in 2nd semester | |
| <3 | 122 (7.7) |
| 3-3.5 | 478 (30) |
| >3.5 | 991 (62.3) |
| Satisfaction about online lectures | |
| Not satisfied at all | 417 (26.2) |
| Moderate | 638 (40.1) |
| Satisfied | 391 (24.6) |
| Very satisfied | 145 (9.1) |
Figure 2.
Anxiety level of the participants
Table 4 shows that a significant positive correlation was found between the participants' age and their GAD-7 scores (r- 0.59, P = 0.01). GAD-7 score was significantly higher among female students, inhabitants of the eastern region, and those with unsteady family income (P=<0.05). However, a nonsignificant difference was found between the GAD scores and the participants' educational level or having a relative or acquaintance got COVID-19. Table 5 shows that the participants with a GPA score of (3–3.5) had a significantly higher GAD-7 score (P=<0.05). The participants who were very satisfied with online lectures had a significantly higher level of GAD-7 scores (<0.001).
Table 4.
Relationship between GAD-7 anxiety scores and the GPA of the participants
| Variable | GAD score (mean±SD) | Test | P |
|---|---|---|---|
| Age (mean±SD) | --- | 0.05* | 0.01 |
| Gender | |||
| Male | 5.38±4.05 | 2.74** | 0.006 |
| female | 6±4.27 | ||
| Region | |||
| Eastern | 7.36±3.84 | 4*** | < 0.001 |
| Western | 5.08±4.34 | ||
| Northern | 6.16±4.33 | ||
| Southern | 4.22±3.62 | ||
| Central | 5.91±3.9 | ||
| Educational level | |||
| Junior (1st-2nd-3rd) | 5.74±4.02 | 0.92** | 0.35 |
| Senior (4th-5th-6th) | 5.61±4.26 | ||
| Do you have a steady family income? | |||
| Yes | 5.54±4.14 | 2.59** | 0.009 |
| No | 6.2±4.24 | ||
| Do you live with your parents? | |||
| Yes | 5.35±4.08 | 5.67** | < 0.001 |
| No | 6.71±4.28 | ||
| Do you have a relative or acquaintance who got COVID-19? | |||
| Yes | 5.69±4.01 | 0.32** | 0.74 |
| No | 5.64±4.23 |
N.B.: * Spearman’s correlation ,**Mann-Whitney test ,***Kruskal Wallis Test,The table represents the relationship between GAD-7 anxiety scores and the GPA of the students in the 1st and 2nd semester and their and their satisfaction with online lectures
Table 5.
Relationship between GAD-7 anxiety scores and the GPA of the participants including Kruskal Wallis test
| Variable | GAD score (mean±SD) | Kruskal Wallis Test | P |
|---|---|---|---|
| GPA in 1st semester | |||
| <3 | 4.67±4.39 | 2 | 0.004 |
| 3-3.5 | 5.84±3.8 | ||
| >3.5 | 5.68±4.31 | ||
| GPA in 2nd semester | |||
| <3 | 4.77±4.84 | 2 | 0.004 |
| 3-3.5 | 5.94±3.84 | ||
| >3.5 | 5.63±4.34 | ||
| Satisfaction about online lectures | |||
| Not satisfied at all | 5.19±4.2 | 3 | < 0.001 |
| Moderate | 5.55±4.08 | ||
| Satisfied | 5.83±3.9 | ||
| Very satisfied | 7.05±4.79 |
-Relationship between GAD-7 anxiety scores and the GPA of the students in the 1st and 2nd semester and their and their satisfaction with online lectures
Discussion
Health is a state of physical, mental, and social prosperity and not only the absence of illness.[19] The COVID-19 outbreak has initiated a worldwide mental wellbeing emergency; simultaneously, it is a tremendous psycho-social experiment.[20] The COVID-19 pandemic has caused stress and changes within the learning behaviors of medical students.[16]
Globally, the prevalence of anxiety among medical students is higher than that among the general population, which globally ranges from 29.2% to 38.7% and is 17% in KSA.[21] Medical students were determined to be more susceptible to academic stress owing to academic requirements.[16,22,23] High stress among medical students impairs the learning ability that may eventually affect the quality of patient care they provide after graduation.[24]
The main goal of this study was to assess the impact of COVID-19 on the psychological and academic performance of medical students. This survey indicated that 59.4% of the studied students had anxiety because of the COVID-19 pandemic. Of these students, 2.5% experienced severe anxiety, 16.7% experienced moderate anxiety, and 40.2% experienced mild anxiety. Recent studies have also reported a significant association between COVID-19 and anxiety level.[21,25,26]
This study identified a significant positive correlation between the age of medical students and their GAD-7 scores. In contrast, other studies done on Brazilian students did not consider age as a predictor for psychological distress. The first study found that medical students will be affected more than intern students due to the health knowledge of the medical interns which was considered a protective factor. And in the second study, a nonsignificant difference was present between age and anxiety score.[27] In this study, the female students had a significantly higher score of GAD compared to the males; this result has been confirmed by other studies.[28] These studies demonstrate that women have a higher prevalence of anxiety among the general population as well as among medical students. However, a study done in China showed there is no difference between gender.[29] This could be due to the frequent exposure of the Chinese people to natural disasters.[30]
In the present study, the students who lived in the eastern region had more anxiety scores than others who lived in the western, northern, southern, and central regions. In our opinion, this might be because the first cases discovered in Saudi Arabia were in the eastern region, a matter that can affect anxiety scores.[31] The stability of family income showed a significant correlation with anxiety scores during the COVID-19 crisis, because students who did not have a steady family income had a higher GAD-7 scores compared to students who had a steady family income. A previous study showed that students who had higher income had less stress than students who had lower income because financial constraints could be a source of stress among students.[24,25]
The results of this study identified a positive correlation between anxiety and a high GPA. In contrast to a previous study, there was a negative correlation between academic achievement and student stress, as when the level of stress increases, academic performance decreases.[24] This can be explained by the considerable efforts exerted by the Arab ministries of higher education by proving e-learning teaching facilities and by starting various campaigns to promote distance learning/online classes.[32]
Regarding the online lectures, 24.6% and 9.1% of the students were satisfied and very satisfied with them, respectively; 40.1% had moderate satisfaction, and 26.2% were not satisfied. A previous study revealed that in Arab countries, there was unreadiness and incompetence associated with pandemic e-learning that might compromise education. Staying home leads to problems such as pandemic-related stress, anxiety, depression, domestic violence, and preventing students and teachers from learning and teaching.[32] Another study performed in Saudi Arabia determined that many students complained about coursework and described it as very difficult and not possible to be self-studied. In addition, they reported that many assignments were pending owing to the lack of study materials.[33]
The pandemic of COVID-19 has had an impact on the psychological health of all university students (medical and nonmedical). One of the most crucial roles to enabling people to cope with their anxiety about the virus was the role of primary health care, which correct misperception in addition to the early diagnosis for its significance. As well as, it reduces their need for hospitalization in huge numbers. Which reflected positively to the country's response to the pandemic.
Limitations
This study had some limitations. Firstly, the study used a cross-sectional design, which usually cannot offer strong affirmation for causality. Secondly, the authors were enforced to use an online survey in this pandemic and the lockdown circumstances and the commitment to the precautionary measures. Finally, one of the major restriction points is that we did not have a recorded baseline data about medical student's psychological health in our region. So, if we want to consider this study for the assessment of the accurate medical student situation, we must recognize other variables affecting their psychological health with consideration to the COVID-19 pandemic.
Conclusion
Of the studied medical students, 59.4% had anxiety during the COVID-19 pandemic. The age of the participant, unsteady family income, high GPA, satisfaction with the online lectures, and being female were associated with higher GAD-7 scores. So, the mental health of medical students was significantly affected by the pandemic. The study calls colleges, health authorities, and the ministry of education to establish psychological support programs for medical students during the pandemic. In addition, the collaboration between them to resolve this problem to provide a high quality of learning and psychological well-being during the timely crisis is suggested.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
The authors gratefully acknowledge the cooperation of all data collectors and participants. Also, the authors would like to thank Falcon Scientific Editing (https://falconediting.com) for proofreading the English language in this paper.
References
- 1.Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382:727–33. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chahrour M, Assi S, Bejjani M, Nasrallah AA, Salhab H, Fares MY, et al. A bibliometric analysis of COVID-19 research activity: A call for increased output. Cureus. 2020;12:e7357. doi: 10.7759/cureus.7357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bao Y, Sun Y, Meng S, Shi J, Lu L. 2019-nCoV epidemic: Address mental health care to empower society. Lancet. 2020;395:e37–8. doi: 10.1016/S0140-6736(20)30309-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shaker MS, Oppenheimer J, Grayson M, Stukus D, Hartog N, et al. COVID-19: Pandemic contingency planning for the allergy and immunology clinic. J Allergy Clin Immunol Pract. 2020;8:1477–88.e5. doi: 10.1016/j.jaip.2020.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Habibzadeh P, Stoneman EK. The novel coronavirus: A bird's eye view. Int J Occup Environ Med. 2020;11:65–71. doi: 10.15171/ijoem.2020.1921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Huang CL, Wang YM, Li XW, Ren LL, Zhao JP, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lai CC, Shih TP, Ko WC, Tang HJ, Hsueh PR. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and corona virus disease-2019 (COVID-19): The epidemic and the challenges? Int J Antimicrob Agents. 2020;55:105924. doi: 10.1016/j.ijantimicag.2020.105924. doi: 10.1016/j.ijantimicag. 2020.105961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zimmermann P, Curtis N. Coronavirus Infections in Children Including COVID-19: An overview of the epidemiology, clinical features, diagnosis, treatment and prevention options in children. Pediatr Infect Dis J. 2020;39:355–68. doi: 10.1097/INF.0000000000002660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wilder-Smith A, Freedman DO. Isolation, quarantine, social distancing and community containment: Pivotal role for old-style public health measures in the novel coronavirus (2019-nCoV) outbreak. J Travel Med. 2020;27:1–4. doi: 10.1093/jtm/taaa020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kawano S, Kakehashi M. Substantial impact of school closure on the transmission dynamicsduring the pandemic flu H1N1-2009 in Oita, Japan. PLoS One. 2015;10:e0144839. doi: 10.1371/journal.pone.0144839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Luca GD, Kerckhove KV, Coletti P, Poletto C, Bossuyt N, Hens N, et al. The impact of regular school closure on seasonal influenza epidemics: A data-driven spatial transmission model for Belgium. BMC Infect Dis. 2018;18:29–45. doi: 10.1186/s12879-017-2934-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wheeler CC, Erhart LM, Jehn ML. Effect of school closure on the incidence of influenzaamong school-age children in Arizona. Public Health Rep. 2010;125:851–9. doi: 10.1177/003335491012500612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gewin V. Five tips for moving teaching online as COVID-19 takes hold. Nature. 2020;580:295–6. doi: 10.1038/d41586-020-00896-7. [DOI] [PubMed] [Google Scholar]
- 14.Lau J, Yang B, Dasgupta R. Will the coronavirus make online education go viral? 2020. [[Last accessed 2020 Mar 24]]. Available from: https://www.timeshighereducation.com/features/will-coronavirusmake-online-educationgo-viral .
- 15.Yezli S, Khan A. COVID-19 social distancing in the Kingdom of Saudi Arabia: Bold measures in the face of political, economic, social and religious challenges? Travel Med Infect Dis. 2020;21:101692. doi: 10.1016/j.tmaid.2020.101692. doi: 10.1016/j.tmaid.2020.101692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Meo SA, Abukhalaf AA, Alomar AA, Sattar K, Klonoff DC. COVID-19 Pandemic: Impact of quarantine on medical students' mental wellbeingand learning behaviors. Pak J Med Sci. 2020;36:S43–8. doi: 10.12669/pjms.36.COVID19-S4.2809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Spitzer RL, Kroenke K, Williams JBW, Löwe B. A brief measure for assessing generalized anxiety disorder: The GAD-7. Arch Intern Med. 2006;166:1092–7. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- 18.AlHadi AN, AlAteeq DA, Al-Sharif E, Bawazeer HM, Alanazi H, Al Shomrani AT, et al. An arabic translation, reliability, and validation of patient health questionnaire in a Saudi sample. Ann Gen Psychiatry. 2017;6:32–41. doi: 10.1186/s12991-017-0155-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.WHO. WHO remains firmly committed to the principles set out in the preamble to the Constitution. Available from: https://www.who.int/about/who-we-are/constitution .
- 20.WHO. Mental health and psychosocial considerations during the COVID-19 outbreak. 2020. Mar, Available from: https://www.who.int/docs/default-source/coronaviruse/mental-health-considerations.pdf?sfvrsn=6d3578af_2 .
- 21.Ezmeirlly HA, Farahat FM. Illness anxiety disorder and perception of disease and distress among medical students in western Saudi Arabia. Saudi Med J. 2019;40:1144–9. doi: 10.15537/smj.2019.11.24654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Quek TT, Tam WW, Tran BX, Zhang M, Zhang Z, Ho CS, et al. The global prevalence of anxiety among medical students: A meta-analysis. Int J Environ Res Public Health. 2019;16:2735. doi: 10.3390/ijerph16152735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.von Krakauer Hübner C, de Lima Bruscatto M, Lima RD. Distress among Brazilian university students due to the Covid-19 pandemic: Survey results and reflections. medRxiv. 2020 doi: 10.1101/2020.06.19.20135251. [Google Scholar]
- 24.Melaku L, Mossie A, Negash A. Stress among medical students and its association with substance use and academic performance. J Biomed Educ. 2015;2015:1–9. [Google Scholar]
- 25.Cao W, Fang Z, Hou G, Han M, Xu X, Dong J, et al. The psychological impact of the COVID-19 epidemic on college students in China? Psychiatry Res. 2020;287:112934. doi: 10.1016/j.psychres.2020.112934. doi: 10.1016/j.psychres. 2020.112934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ullah R, Amin S. The psychological impact of COVID-19 on medical students? Psychiatry Res. 2020;288:113020. doi: 10.1016/j.psychres.2020.113020. doi: 10.1016/j.psychres. 2020.113020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Baaleis MAS, Ali SA. Impact of usage of different coping strategies on academic performance of female students in college of medicine, Al-Ahsa. Egypt J Hosp Med. 2018;73:7883–91. [Google Scholar]
- 28.de Sousa JM, Moreira CA, Telles-Correia D. Anxiety, depression and academic performance: A study amongst Portuguese medical students versus non-medical students. Acta Med Port. 2018;31:454–62. doi: 10.20344/amp.9996. [DOI] [PubMed] [Google Scholar]
- 29.McLean CP, Asnaani A, Litz BT, Hofmann SG. Gender differences in anxiety disorders: Prevalence, course of illness, comorbidity and burden of illness. J Psychiatr Res. 2011;45:1027–35. doi: 10.1016/j.jpsychires.2011.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kessler RC, McLaughlin KA, Koenen KC, Petukhova M, Hill ED WHO World Mental Health Survey Consortium. The importance of secondary trauma exposure for post-disaster mental disorder. Epidemiol Psychiatr Sci. 2012;21:35–45. doi: 10.1017/s2045796011000758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Saudi ministry of health (MOH). Ministry of Health Reports 15 New Cases of Coronavirus“. Available from: https://covid19.moh.gov.sa/
- 32.Al Lily AE, Ismail AF, Abunasser FM, Alqahtani RH. Distance education as a response to pandemics: Coronavirus and Arab culture? Technol Soc. 2020;29:101317. doi: 10.1016/j.techsoc.2020.101317. doi: 10.1016/j.techsoc. 2020.101317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Tanveer M, Bhaumik A, Hassan S, Haq UI. Covid-19 pandemic, outbreak educational sector and students online learning in Saudi Arabia. J Entrep Educ. 2020;23:1–14. [Google Scholar]


