Abstract
Background:
Parents' of young children who frequently attend primary health care (PHC) services for mild health problems (MHPs) can present a complex and difficult challenge for staff. This phenomenon can expose the child to inappropriate overprescribing, unnecessary medical interventions and may impair the quality of life of parents and children.
Aim:
To define driving factors for frequent attenders (FAs) preschool children in PHC services in Kuwait.
Design and Setting:
An unmatched case-control study was conducted in the PHC setting in Kuwait.
Method:
A sample comprised of 300 parents from 10 PHC centres was selected. The top third children with higher frequency (FAs) visits to their family practitioners (FPs) were compared with the lower third with lower frequency (NFAs) visits to their FPs during the same duration. The Brief Illness Perception Questionnaire (Brief IPQ) was used to assess parents' response to their children's illness. The sociodemographic data for both groups were collected. Culture and background heath status for child and family were collected (order of the child in the family, if the family is living with the extended family and additional help received regarding childcare). The previous medical history of parent, child, and siblings was also included.
Results:
The mean number of consultations in FAs versus NFAs within the previous year was 15.5 ± 7.6 and 4.3 ± 2.1, respectively. There was no significant difference in means between the two groups of parents in responses to the questions of the adapted Brief IPQ. FAs were more likely to be the first-order child (odds ratio (OR) 2.4; 95% confidence interval (CI) =1.2–4.6), have chronic disease (OR 4.7; 95% CI = 2.1–10.6), and live with the extended family (OR 1.8; 95% CI = 1.1–3.3). They experienced an acute, potentially life-threatening episode previously (OR 2.6; 95% CI = 1.1–6.4), with the same applying to a sibling (OR 72.6; 1.2–6.2) or parent (OR 2.6; CI = 1.1–6.4).
Conclusion:
Identification of the hidden reasons that affect parents' decisions to consult their FPs frequently for their children's MHPs were important predictors for defining preschool FAs children in the PHC centres and can help the staff provide effective management plans to help them.
Keywords: Children, parents, primary health care
Introduction
General practitioners provide continuing medical care for patients (irrespective of age, sex, or health problems) in the community. They are usually a patient's first point of contact. Children up to the age of 14 formulate around 37% of the total population of Kuwait. This situation poses considerable challenges for general practice in Kuwait in meeting their health needs.
Dealing with child illness can be stressful for parents. When a child becomes ill, hidden influences, rather than personal characteristics, can affect their decision to seek medical care.
Many parents have previous health experiences, perceptions and interpretations that depend on a limited understanding of factors related to illness and disease.[1,2] Repeatedly, parents' concerns regarding their child's health are not consistent with the level of priority considered by family practitioners (FPs).[3] Subsequently, frequent attenders' (FAs) children phenomenon, with related consequences, occurs.
Previous studies reported that FAs children are more prone to unnecessary drug prescriptions and needless medical interventions.[4,5] Additionally, it interferes with the quality of life of children and parents.[6,7] Furthermore, previous reports showed that FAs are adding more cost and load onto health services.[8,9]
Identification of their characteristics is not enough to propose strategies to confront this problem. Discovering parents' motives behind this behavior can improve understanding of their difficulties and enhance communication.[10,11] Once clinicians understand these factors, they can develop accurate and targeted strategies to empower this group of parents. Additionally, it could help with the development of better health services and resources to help parents deal with their children's mild health problems (MHPs).[12,13]
It is important to investigate and highlight parents' hidden driving factors behind this behavior as little information is published about this subject in the Gulf region and throughout the globe.
The State of Kuwait, where this study has taken place, is situated in the northeast of the Arabian Peninsula. It is a high-income country and its economy ranks 10th (2016) and 5th (2018) according to gross national income per capita published by the World Bank.
Method
Study design
This is an unmatched case-control study for age and gender. It was designed to compare various variables that motivate parents to consult their FPs about their children's MHPs and measures that assess the cognitive and emotional impact of children's illnesses on parents. The sample was collected between January 2017 and August 2017.
The Medical Research Ethics Committee of the Ministry of Health in Kuwait approved the study protocol. Approval number is 216/361.
All participants provided written informed consent
Participating centers
Kuwait had a population of approximately 4,225,705 of which about 1,305,722 million were Kuwaiti citizens (as of January 2016). The total number of Kuwaiti children from 1 to 5 years in this period was about 114,256. The current population of Kuwait is 4,254,445 as of Sunday, August 11, 2019, of which about 1,403,113 million were Kuwaiti citizens based on the latest United Nations estimates.
Kuwait is divided into five health regions with 97 primary health care (PHC) centres representing the first level of service. These centres refer patients as needed to five general area hospitals.
Cases were recruited from 10 PHC centres. Two criteria were required from participating PHC centres. First, at least one of the centre's doctors is a board-certified family physician. Second, the majority of patients attending the centre are Kuwaiti citizens. Twenty-six centres met these criteria, and from these, the largest two centres from each region, with at least 15,000 registered people, were selected to participate in the study.
The selected 10 centres were recruited using cluster sampling.
Sample size
There are no preceding studies comparing the parents' perception of their children's MHPs between FAs and NFAs children. We estimated the sample size in accordance with previous research investigating the relationship between maternal knowledge of vaccines and its impact on infant immunisation rates in Karachi, Pakistan.[14] The sample size is 270 participants, which has been calculated by using the Sample Size Calculation for Unmatched Case–Control Studies of the software open Epi.[15] Our assumptions are 80% power, 5% alpha, 30% of controls have unfavorable illness perception (have overall sum score above 40) and 50% of cases have unfavorable illness perception (have an overall score above 40).
The collected sample was 300 accompanying parents of children (aged 1–5 years) from 10 centres. The additional 30 participants were included in the final sample size calculation and analysis.
Sampling procedure
A consecutive series of eligible parents from each of the 10 clinics were included until the required number was achieved (30 parents from each clinic).
Of all parents invited to participate in the study, only 13 declined citing shortage of their time.
All parents were Kuwaiti (21–55 years). Parents were excluded if they had any documented psychiatric health problems or personality disorders. Previous reports documented the relationship of these problems with the increased frequency of visits to the health services.[16,17]
There is no agreed or precise definition for FAs patients, especially in children.[4,16,17,18,19] Some studies considered FAs as the top 10%, 25%, 30% or the top 33.3% of consulting patients during a 1-year period.
We considered the top third (100 children) with higher frequency of visits to their FPs for MHPs in the year prior to data collection as the study arm. The lower third with lower frequency visits within the same duration (100 children) was considered as the control group. This ensures enough sample size for analysis and comparison.
Parents were invited after finishing their visits to FPs.
Their children must be currently well and without fever, injuries, or any moderate or serious conditions that necessitate urgent interference.
No incentives were provided to participants.
Data collection
One FP was appointed as an investigator from each participating centre. A meeting was held with the study coordinator to discuss the purpose, design, recruitment criteria and logistics of data collection. They were trained to identify and invite study participants according to the specified inclusion and exclusion criteria.
A questionnaire that assesses the cognitive and emotional representations of illness was completed by the parent in a separate room in the clinic. The completed questionnaires were sent to the coordinator's office for data entry and analysis.
The instrument
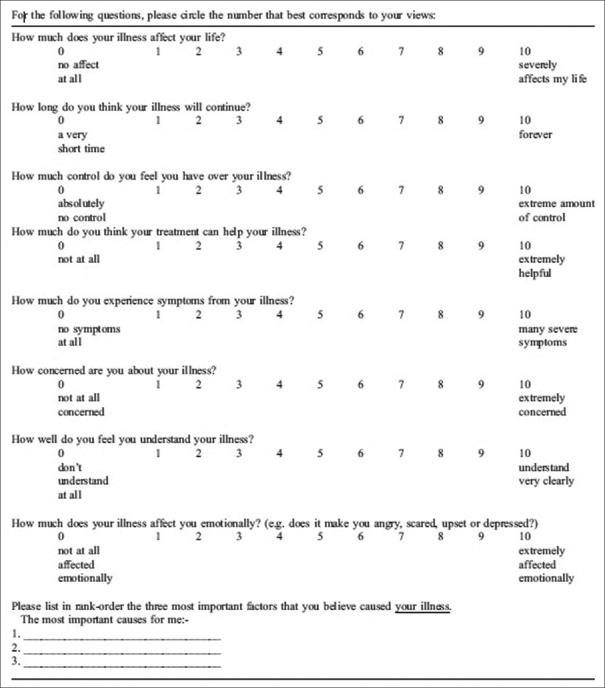
Brief IPQ [Figure 1] was adapted, after obtaining permission to use it. The questions were redirected to explore the parents' cognitive and emotional representation towards their children's illness.
Figure 1.
Brief Illness Perception Questionnaire (IPQ)
Brief IPQ is a nine-item self-report scale measuring the patient's cognitive and emotional representations of their illness including consequences, timeline, personal control, treatment, control, identity, coherence, concern, emotional response and causes. The Brief IPQ has been proven to be reliable and valid.[20]
The original English questionnaire was translated into Arabic by a bilingual FP. Translation back into English was independently performed by another bilingual FP, and its retranslation back into Arabic independently carried out by an Arabic language senior tutor. The study investigators then reviewed the two Arabic versions and agreed that they were equivalent.
The Arabic questionnaire was pretested on 20 subjects to uncover any difficulties in understanding the questions and to estimate the time needed to complete it. Subsequently, minor adjustments were made to the wording of some questions.
The adapted Brief IPQ was completed by enrolled parents. Additional information was collected and completed by the investigators. This included parent's marital status, number of living siblings, order of the child in the family, education level, occupation, if the family is living with the extended family and additional help received regarding childcare. The previous medical history of parent, the child or siblings was included.
Statistical analysis
Various descriptive statistics (mean and standard deviation) were used to describe the difference between the two groups, regarding the number of children visits for MHPs during the previous year.
Chi-squared test was conducted to assess the differences between FAs and NFAs groups with respect to sociodemographic characteristics.
Independent t-test was used to compare mean scores between the two groups in response to the adapted Brief IPQ questions.
The crude odds ratios (ORs) and their 95% confidence interval (CI) were calculated for different influencing factors separately.
A significance level of 5% was used for all analyses.
The statistical package for Social Sciences SPSS 23.0 was used for data processing.
Results
The mean number of consultations in FAs within the previous year was 15.5 (range 8–45) ±7.6, compared with 4.3 (range 0–7) ±2.1 in NFAs.
Table 1 shows the sociodemographic data of participating parents with their accompanying children. It shows no significant difference regarding basic background information between FAs and NFAs groups (parents' age, gender, marital status, educational level and occupational status), as well as in the gender and age of accompanying children.
Table 1.
Sociodemographic characteristics of FAs and NFAs children (1-5 years) in PHC offices
| Characteristics | FAs No=100 | NFAs No=100 | P |
|---|---|---|---|
| Parent’s age | |||
| 21-45 years | 97 | 96 | 0.700 |
| >45-<65 | 3 | 4 | |
| Parent gender | |||
| Male | 35 | 29 | 0.363 |
| Female | 65 | 71 | |
| Marital status | |||
| Married | 98 | 98 | 1.00 |
| Divorced | 2 | 2 | |
| Widow/widower | 0 | 0 | |
| Educational level | |||
| Nonilliterate | 3 | 1 | 0.231 |
| Primary school | 1 | 1 | |
| Junior | 13 | 6 | |
| Secondary | 29 | 25 | |
| College and above | 42 | 58 | |
| Others | 12 | 9 | |
| Occupation | |||
| Working | 79 | 82 | 0.395 |
| Not working | 17 | 17 | |
| Retired | 4 | 1 | |
| Number of children in family | |||
| 1 | 19 | 7 | 0.052 |
| 2 | 30 | 27 | |
| 3 | 24 | 29 | |
| >3 | 27 | 37 | |
| Child gender | |||
| Male | 58 | 59 | 0.589 |
| Female | 42 | 41 | |
| Child age (years) | |||
| 1≥2 | 30 | 29 | 0.422 |
| 2≤3 | 21 | 14 | |
| 3≥4 | 19 | 27 | |
| 4-5 | 30 | 30 |
Single-child families slightly dominated in FAs (19%) versus NFAs (7%), however, with no significant difference.
Reponses to the adapted Brief IPQ showed no significant difference in means between the two groups of parents for the first eight questions [Table 2].
Table 2.
Response of the two groups to adapted IPQ
| Questions | FAs Mean (SD) | NFA Mean (SD) | P | 95% CI |
|---|---|---|---|---|
| How much does your child’s illness affect your life? | 5.03 (3.26) | 5.74 (3.46) | 0.137 | -1.648-0.228 |
| How long do you think your child’s illness will continue? | 3.20 (1.97) | 3.18 (2.17) | 0.951 | -0.561-0.597 |
| How much control do you feel you have over your child’s illness? | 6.88 (3.07) | 6.79 (2.97) | 0.833 | -0.753-0.933 |
| How much do you think your treatment can help your child’s illness? | 7.58 (2.55) | 8.05 (2.43) | 0.183 | -1.164-0.224 |
| How much do you experience symptoms from your child’s illness? | 7.54 (2.52) | 8.01 (2.33) | 0.173 | -1.147-0.207 |
| How concerned are you about your child’s illness? | 9.02 (1.66) | 9.11 (1.64) | 0.700 | -0.550-0.370 |
| How well do you feel you understand your child’s illness? | 8.09 (2.34) | 8.33 (2.40) | 0.474 | -0.900-0.420 |
| How much does your child’s illness affect you emotionally? | 6.61 (3.07) | 6.31 (2.83) | 0.479 | -0.529-1.123 |
SD: Standard Deviation, CI: Confidence Interval
Brief IPQ question 9 analysis showed that most parents reported changes in weather as the main cause of their children's illness (65.5%). Some reported contagious causes (38.0%) and 33.5% reported other causes (e.g. excess consumption of ice cream and cold drinks, wearing light dress, etc.).
Table 3 shows different important factors that may affect visit frequency of children to their FPs. In the group of FAs, there is a highly significant number of children with chronic health problems (OR 4.7; 95% CI = 2.1–10.6), and who are living with extended family (OR 1.8; 95% CI = 1.1–3.3). This is also seen in first-order children (OR 2.4; 95% CI = 1.2–4.6). The history of potentially life-threatening illness early in life, whether in the child, siblings or parents, was significantly higher in FAs versus NFAs children (OR 2.6; 95% CI = 1.1–6.4, OR 1.5; 95% CI = 0.7–3.1, OR 2.6; 95% CI = 1.1–6.4, respectively). Parents (22%) and siblings (21%) with a history of chronic disease is higher in the FA children; however, this is statistically not significant.
Table 3.
Variables that may affect the frequency of annual visits to PHC physicians’ offices among children (1-5 years old)
| Variables | FAs, n (%) | NAs, n (%) | OR (95% CI) | P |
|---|---|---|---|---|
| Child information | ||||
| If the child is the first order | 33 (33) | 17 (17) | 2.4 (1.2-4.6) | <0.009** |
| If the child has chronic disease | 32 (32) | 9 (9) | 4.7 (2.1-10.6) | <0.000** |
| If child had potentially life-threatening illness early in life | 19 (19) | 8 (8) | 2.6 (1.1-6.4) | <0.023* |
| Sibling information | ||||
| sibling has chronic disease | 21 (21) | 15 (15) | 1.5 (0.7-3.1) | 0.269 |
| sibling had potentially life-threatening illness early in life | 21 (21) | 9 (9) | 2.6 (1.2-6.2) | <0.017* |
| The accompanying parent information | ||||
| If received addition care | 97 (97) | 98 (98) | 1.5 (0.2-9.2) | 0.651 |
| living with extended family | 67 (67) | 52 (52) | 1.8 (1.1-3.3) | <0.031* |
| If parent has chronic disease | 22 (22) | 14 (14) | 1.7 (0.8-3.6) | 0.141 |
| If parent had potentially life-threatening illness early in life | 19 (19) | 8 (8) | 2.6 (1.1-6.4) | <0.023* |
OR=Odds ratio, CI: Confidence Interval, *Significant at <0.050 level, **Significant at <0.010 level
Discussion
PHC physicians often see parents whose worries regarding their child's vulnerability to disease or safety issues seem out of proportion to the child's actual health status. This phenomenon leads to frequent visits to PHC services with unfavourable effects on the services, children and their parents.
Beliefs, social and cultural factors may contribute to parents seeking medical advice frequently.
This study explored several specific factors that influence the parents' decision to consult their FPs more frequently when their children develop minimal symptoms of illness. Many of these motivations are related to the child's social and chronic health status, culture factors and previous medical events in the family, rather than parents' personal characteristics.
There are no previous studies to directly compare our results with.
The first born children were more likely to be FAs. In accordance with the reports of previous studies,[21,22] they are seen as more vulnerable to serious illness. This can be explained by the lack of experience of parents with symptoms of MHPs and how to deal with them.
Children with chronic diseases such as bronchial asthma, eczema, etc., were observed to be more frequently visiting their FPs when they developed MHPs. These children are perceived by their parents as vulnerable[23] causing parents to behave in a more controlling, protective or intrusive manner[24], leading to frequent visits to health services.
In accordance with previous reports,[4,24] children were perceived by their parents as medically susceptible if they experienced an acute, potentially life-threatening illness early in life even after full recovery. Thus, traumatic experience leads to an exaggerated response to minor symptoms. Previous history of issues in the family, whether experienced by the parent or siblings, leads to the same effect. The unpleasant incident has subconscious effect on the parents driving them to seek medical advice early for MHPs in previously healthy children.
Living with extended families is a sociocultural habit, especially for young adults in the gulf countries. We found an association between those who are living with extended families and frequent attendance. There are no similar studies to compare with our findings in this aspect directly. However, our result is not consistent with previous reports that showed positive effects on the health of children receiving care from grandparents.[25,26] According to these studies, it is expected that children who are receiving ancestral care visit health care services less frequently. Our explanation is that parents living with extended family might obtain advice and sometimes face pressure from other family members to consult their FPs when their child develops any symptoms, even mild ones.
In our study, all parents' cognitive and emotional response toward their children's illness was the same between the two groups. This is expected, as the selection of the participating parents excluded those with any psychiatric disorders. Previous studies[7,27] reported the strong relation of these problems with a high frequency of attendance to the health services. Parents with these problems were excluded to avoid bias in the outcomes.
Implications for research and practice
PHC providers dealing with children need to explore the social, cultural and psychological status of families and consider expected factors that render children to be counted as FAs. Communication with parents can be improved and be more successful, especially with the understanding of the hidden fears and family circumstances.
Children regularly attend well baby clinics and scheduled visits for vaccination. This provides a good opportunity for delivering purposeful and culturally appropriate health education programmes for this group of parents.
Identifying and describing the characteristics of FAs is insufficient in planning suitable educational programmes. More studies are required from different cultures and societies to further explore the hidden motives for frequent unnecessary visits, especially for children, to PHC services. This will enrich researchers' discussions and promote suggestions of appropriate solutions.
Strengths and limitations
This is the first study to investigate the problem of FAs children to PHC services in the Middle East. Additionally, after the meticulous exclusion of psychiatric problems and personality disorders among parents, the authors investigated social, as well as current and previous medical experiences of children, parents, siblings and the possibility of their influence on frequent unnecessary visits to PHC services.
This study has limitations. The study included Kuwaiti parents and children only. In Kuwait, non-national populations constitute about two thirds of Kuwait's inhabitants. A great portion of the non-Kuwaiti residents work as drivers, builders, or in service occupations. These populations have different background social factors and health beliefs, therefore were excluded from the study. The addition of the non-Kuwaiti population may add biases to the results. Another limitation is that some families are consulting private health facilities thus records of previous health visits are unknown. However, the majority of the population consult national health services.
Conclusion
Summary
Repeated unnecessary visits, especially for children, to PHC centers have unfavourable effects on the child and PHC providers. Exploring motives and addressing them is extremely important in minimizing this phenomenon.
Cultural demographics, psychosocial intentions, and health experiences of parents of the children are strong motivating factors for repeatedly visiting PHC services unnecessarily. These issues need to be seriously investigated and addressed to avoid suffering unnecessary medical interventions and the possible iatrogenic risks associated, and to save health resources.
There is very little research done on this topic regarding FAs children in PHC setting. This limits the dimensions of the foundation for understanding the study problem, therefore necessitating further development in this area of study.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
We would like to acknowledge all FPs who were appointed as an investigators from the participating centres. We are also grateful to the participating parents in this study.
References
- 1.Saunders NR, Tennis O, Jacobson S, Gans M, Dick PT. Parents' responses to symptoms of respiratory tract infection in their children. CMAJ. 2003;168:25–30. [PMC free article] [PubMed] [Google Scholar]
- 2.Kelly M, Sahm LJ, Shiely F, O’Sullivan R, Brenner M, Larkin P, et al. The knowledge, attitudes and beliefs of carers (parents, guardians, healthcare practitioners, crèche workers) around fever and febrile illness in children aged 5 years and under: Protocol for a qualitative systematic review. Syst Rev. 2015;4:27. doi: 10.1186/s13643-015-0021-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Reijneveld SA, de Meer G, Wiefferink CH, Crone MR. Parents' concerns about children are highly prevalent but often not confirmed by child doctors and nurses. BMC Public Health. 2008;8:124. doi: 10.1186/1471-2458-8-124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Stojanović-Spehar S, Blazeković-Milaković S, Bergman-Marković B, Matijasević I. Preschool children as frequent attenders in primary health care in Croatia: Retrospective study. Croat Med J. 2007;48:852–9. doi: 10.3325/cmj.2007.6.852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Riva B, Clavenna A, Cartabia M, Bortolotti A, Fortino I, Merlino L, et al. Emergency department use by paediatric patients in Lombardy Region, Italy: A population study? BMJ Paediatr Open. 2018;2:e000247. doi: 10.1136/bmjpo-2017-000247. doi: 10.1136/bmjpo-2017-000247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kersnik J, Svab I, Vegnuti M. Frequent attenders in general practice: Quality of life, patient satisfaction, use of medical services and GP characteristics. Scand J Prim Health Care. 2001;19:174–7. doi: 10.1080/028134301316982405. [DOI] [PubMed] [Google Scholar]
- 7.Patel S, Kai J, Atha C, Avery A, Guo B, James M, et al. Clinical characteristics of persistent frequent attenders in primary care: Case-control study. Fam Pract. 2015;32:624–30. doi: 10.1093/fampra/cmv076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Neal RD, Heywood PL, Morley S, Clayden AD, Dowell AC. Frequency of patients' consulting in general practice and workload generated by frequent attenders: Comparisons between practices. Br J Gen Pract. 1998;48:895–8. [PMC free article] [PubMed] [Google Scholar]
- 9.Morriss R, Kai J, Atha C, Avery A, Bayes S, Franklin M, et al. Persistent frequent attenders in primary care: Costs, reasons for attendance, organisation of care and potential for cognitive behavioural therapeutic intervention. BMC Fam Pract. 2012;13:39. doi: 10.1186/1471-2296-13-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kai J. Parents' difficulties and information needs in coping with acute illness in preschool children: A qualitative study. BMJ. 1996;313:987–90. doi: 10.1136/bmj.313.7063.987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kai J. What worries parents when their preschool children are acutely ill, and why: A qualitative study. BMJ. 1996;313:983–6. doi: 10.1136/bmj.313.7063.983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Walsh A, Edwards H, Fraser J. Influences on parents' fever management: Beliefs, experiences and information sources. J Clin Nurs. 2007;16:2331–40. doi: 10.1111/j.1365-2702.2006.01890.x. [DOI] [PubMed] [Google Scholar]
- 13.Kallestrup P, Bro F. Parents' beliefs and expectations when presenting with a febrile child at an out-of-hours general practice clinic. Br J Gen Pract. 2003;53:43–4. [PMC free article] [PubMed] [Google Scholar]
- 14.Owais A, Hanif B, Siddiqui AR, Agha A, Zaidi AK. Does improving maternal knowledge of vaccines impact infant immunization rates. A community-based randomized-controlled trial in Karachi, Pakistan? BMC Public Health. 2011;11:239. doi: 10.1186/1471-2458-11-239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Open Epi. Sample size calculation for unmatched case-control studies. 2014. [[Last accessed on 2016 Dec 07]]. Version 3.03.17. Available from: https://www.openepi.com/SampleSize/SSCC.htm .
- 16.Kivelä K, Elo S, Kääriäinen M. Frequent attenders in primary health care: A concept analysis. Int J Nurs Stud. 2018;86:115–24. doi: 10.1016/j.ijnurstu.2018.06.003. [DOI] [PubMed] [Google Scholar]
- 17.Luciano JV, Fernández A, Pinto-Meza A, Luján L, Bellón JA, García-Campayo J, et al. Frequent attendance in primary care: Comparison and implications of different definitions. Br J Gen Pract. 2010;60:49–55. doi: 10.3399/bjgp10X483139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rifel J, Svab I, Selič P, Rotar Pavlič D, Nazareth I, Car J. Association of common mental disorders and quality of life with the frequency of attendance in Slovenian family medicine practices: Longitudinal study? PLoS One. 2013;8:e54241. doi: 10.1371/journal.pone.0054241. doi: 10.1371/journal.pone. 0054241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Welzel FD, Stein J, Hajek A, König HH, Riedel-Heller SG. Frequent attenders in late life in primary care: A systematic review of European studies. BMC Fam Pract. 2017;18:104. doi: 10.1186/s12875-017-0700-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Broadbent E, Petrie KJ, Main J, Weinman J. The brief illness perception questionnaire. J Psychosom Res. 2006;60:631–7. doi: 10.1016/j.jpsychores.2005.10.020. [DOI] [PubMed] [Google Scholar]
- 21.van den Bosch WJ, Huygen FJ, van den Hoogen HJ, van Weel C. Morbidity in early childhood, sex differences, birth order and social class. Scand J Prim Health Care. 1992;10:118–23. doi: 10.3109/02813439209014047. [DOI] [PubMed] [Google Scholar]
- 22.Thomasgard M, Metz WP. Parental overprotection and its relation to perceived child vulnerability. Am J Orthopsychiatry. 1997;67:330–5. doi: 10.1037/h0080237. [DOI] [PubMed] [Google Scholar]
- 23.Houtzager BA, Möller EL, Maurice-Stam H, Last BF, Grootenhuis MA. Parental perceptions of child vulnerability in a community-based sample: Association with chronic illness and health-related quality of life. J Child Health Care. 2015;19:454–65. doi: 10.1177/1367493514530954. [DOI] [PubMed] [Google Scholar]
- 24.Chambers PL, Mahabee-Gittens EM, Leonard AC. Vulnerable child syndrome, parental perception of child vulnerability, and emergency department usage. Pediatr Emerg Care. 2011;27:1009–13. doi: 10.1097/PEC.0b013e318235bb4f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pulgaron ER, Marchante AN, Agosto Y, Lebron CN, Delamater AM. Grandparent involvement and children's health outcomes: The current state of the literature. Fam Syst Health. 2016;34:260–9. doi: 10.1037/fsh0000212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wellard S. Grandparents: An underestimated resource for children's health development. J Fam Health Care. 2010;20:150–2. [PubMed] [Google Scholar]
- 27.Pymont C, Butterworth P. Longitudinal cohort study describing persistent frequent attenders in Australian primary healthcare? BMJ Open. 2015;5:e008975. doi: 10.1136/bmjopen-2015-008975. doi: 10.1136/bmjopen-2015-008975. [DOI] [PMC free article] [PubMed] [Google Scholar]