Abstract
Background:
The rate of obesity in children is rising and it has become a growing epidemic worldwide; Childhood obesity is related to the high risk of obesity later in adult life. In the last 30 years the prevalence childhood obesity more than tripled. Overweight in paediatric population is suggested to be related to many cardio-metabolic risk factors such as metabolic syndrome, type 2 diabetes, hypertension, insulin resistance. Metabolic syndrome and dyslipidaemia and 70% obese children had first cardiovascular disease risk factor and 30% had second or more.
Aim:
To estimate the prevalence and correlates of obesity among children in Aseer region.
Methodology:
A descriptive cross-sectional survey was conducted in the schools of Abha and Khamis Mushayet Cities; Aseer region during the period from January to December 2019. The respondents were any of the parents of the child. After having permission from the school authority, self-administered questionnaires were distributed to a total of 300 children, with explanations about the questionnaire by the principal investigator and class teacher.
Results:
The study included 300 students with ages that ranged from 1 year up to 17 years and mean age was 8.6 years old. Exact of 55.3% of the students were males and 32% were at preschool age while 43.7% were at the primary level of education. Students' body mass index (BMI) distribution demonstrated that more than half of the children had overweight or obesity and 16.7% were with underweight. There was a significant relation between obesity among the children and some of their dietary habits including sweets, chocolate and fast food.
Conclusions and Recommendations:
In conclusion, the study revealed that nearly one-third of the children in the study group were overweight or obese with obesity more prevalent. Obesity was more recorded among old-aged children who frequently had unhealthy food. Improving the children lifestyle and dietary habits is mandatory to work against weight gain.
Keywords: Children, obesity, overweight
Background
Childhood obesity usually positively correlated with obesity in adulthood which in turn is a significant cardiovascular diseases risk factor such as hypertension, diabetes, and dyslipidaemia.[1,2] Recently, the prevalence of childhood overweight and obesity has increased significantly both in rich and poor countries.[3,4,5] Recent researches reported that this upward trend in childhood obesity is much more noticed in developing countries than in developed countries.[6] In the last 30 years, childhood obesity increased more than triple. Childhood overweight affects not only the physical health but there is many psychosocial drawbacks such as self-esteem and has negative consequences on cognitive and social development.[7] Generally, childhood obesity affects negatively the quality of life and life expectancy and accounts for billions of dollars in provision of health care.[8] Due to difficulty of dealing with obesity in young ages and the long-term serious adverse effects, the prevention of childhood obesity has been recognized as a public health priority.[9]
Till now, the primary cause of childhood obesity is unknown. It is a multidisciplinary disease that involves environment, genetics, and lifestyle factors. The one that play a significant role is a dietary outline.[10] It has been reported in several studies that childhood obesity has been related to the unhealthy dietary patterns as nutrition in children is associated with obesity, so first we should find the appropriate nutrition plan to prevent or treat obesity. Several studies have investigated the association between BMI and food habits, but the results have been unsatisfying.[11,12,13] In many developing countries, the A nutritional transition has been noticed which included diminution of the prevalence of nutritional deficiencies and the more significant recorded overweight and obesity, not only in the adult population, but also among children and adolescent. This transition was fundamentally related to changes in lifestyle and eating habits.[14,15]
The current study was conducted to assess the magnitude of obesity among children and to relate the children's weights to their dietary habits in Aseer region, Southern Saudi Arabia.
Methodology
A descriptive cross-sectional survey was conducted in the schools of Abha and Khamis Mushayet Cities Aseer region during the period from January to December 2019. The study approved on October 30, 2019 by the Ethics Committee of King Khalid University, Abha, Saudi Arabia, approval number (ECM#2019-69) - (HAPO-06-B-001). These are the biggest cities in the Aseer provenance as more than 80% of the schools were clustered there. A total of 50 schools were selected including primary, preparatory and secondary schools. The study population were schoolchildren at all phases from nursery to secondary grades, aged 4–13 years. The respondents were any of the parents of the child. Children with chronic health problem, endocrinal disorders or physical disability were excluded from the study as these conditions could affect their body weight. Two-stage stratified cluster random sampling performed. Schools were stratified into primary, preparatory or secondary. In the first stage, within each strata, randomly selected 5 out of the total 50 schools. In the second stage, two classes for each grade were included randomly in each school and enrolled all students. After having permission from the school authority, self-administered questionnaires were distributed to a total of 300 children, with explanations about the questionnaire by the principal investigator and class teacher. Each student received a separate request letter to the parents, prepared by the investigator with an informed consent. Then, questionnaires filled by parents collected at the school after two days, and the weight and height measurements of each child were taken using including all data regarding their children such as nutritional habits, lifestyle besides socio-demographic data. Weight and height measurements of each child recorded using a digital weighing machine and standard measuring tape respectively with recording to the nearest integer value. Body mass index (BMI) was defined as the ratio of body weight to body height squared, expressed as kg/m2.[16] Based on BMI, children and adolescents were classified according to thinness, normal weight, overweight or obesity using sets of age- and sex-specific cut-offs specified by WHO. A standard deviation score >1.04 for body mass index (above the 85th centile) was defined as overweight, and a standard deviation score >1.64 (above the 95th centile) was defined as obese.[17]
Statistical analysis
After data filtering for errors, it was fed to statistical package of social science (SPSS) version 24. All statistical methods based on two-tailed tests. A value of P < 0.05 was considered statistically significant. Descriptive analysis based on frequency and percent distribution was done for all variables including demographic data, dietary habits and obesity distribution. Univariate relations between children BMI categories and children's personal data and dietary habits were tested using Pearson Chi-square test.
Results
The study included 300 students with ages ranged from 1 year up to 17 years and mean age of 8.6 years old. Exact of 55.3% of the students were males and 32% were at preschool age while 43.7% were at the primary level of education.
Considering students body mass index (BMI) distribution, Figure 1 demonstrates that 49% of the children had normal weight for age and 16.7% were with underweight, 10% overweight while obesity was recorded among 24.3% of the sampled children.
Figure 1.
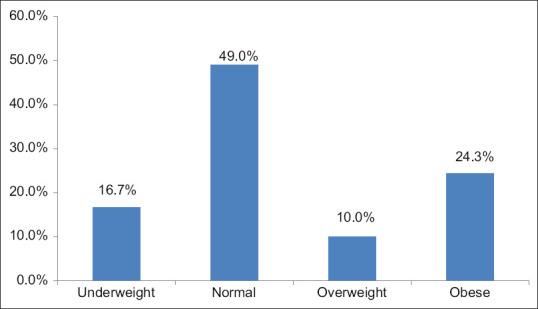
Weight for age among school students in Aseer region, Southern Saudi Arabia
As for distribution of the children BMI according to their personal data [Table 1], overweight and obesity were recorded among 51.4% of the children who aged 15 years or more compared to 34.7% of the children at pre-school age with recorded statistical significance (P = .001). With regard to gender, 35.8% of the female children were at overweight or obese compared to 33.1% of the students with no statistical significance (P = .741). Also, obesity was recorded among 52% of the students at secondary school compared to 33.3% of those who were at nursery (P = .001).
Table 1.
Body mass index distribution according to students personal data in Aseer region, Southern Saudi Arabia
| Personal data | Total No (%) | Body mass index | P | |||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Underweight | Normal | Overweight/Obese | ||||||
|
|
|
|
||||||
| No | % | No | % | No | % | |||
| Age in years | 0.001* | |||||||
| <6 years | 95 (31.7%) | 20 | 21.1% | 42 | 44.2% | 33 | 34.7% | |
| 6-10. | 95 (31.7%) | 26 | 27.4% | 46 | 48.4% | 23 | 24.2% | |
| 11-14 | 75 (25.0%) | 4 | 5.3% | 42 | 56.0% | 29 | 38.7% | |
| 15+ | 35 (11.7%) | 0 | 0.0% | 17 | 48.6% | 18 | 51.4% | |
| Gender | 0.741 | |||||||
| Male | 166 (55.3%) | 30 | 18.1% | 81 | 48.8% | 55 | 33.1% | |
| Female | 134 (44.7%) | 20 | 14.9% | 66 | 49.3% | 48 | 35.8% | |
| Educational stage | 0.001* | |||||||
| Nursery | 96 (32.0%) | 20 | 20.8% | 44 | 45.8% | 32 | 33.3% | |
| Primary | 131 (43.7%) | 30 | 22.9% | 67 | 51.1% | 34 | 26.0% | |
| Intermediate | 48 (16.0%) | 0 | 0.0% | 24 | 50.0% | 24 | 50.0% | |
| Secondary | 25 (8.3%) | 0 | 0.0% | 12 | 48.0% | 13 | 52.0% | |
P: Pearson χ2 test. *P<0.05 (significant)
Table 2 demonstrates that 65% of the obese children had fruits and vegetables only once weekly while 52.4% of those with normal weights had it 2–6 times/week with statistically significant difference (P = .001). Considering legumes, 70.9% of the children with overweight or obesity had it once weekly which is similar to those who had normal weights (74.1%) with no statistical significance (P = .941). Whole grains were taken daily among 38.8% of the children with overweight or obesity compared to 38.1% of those with normal weights (P = .958). Also milk and milk products were taken daily among 30.1% of obese children compared to 35.4% of those who had normal weights and 32% of those who had underweight with no significance (P = .727). Considering animal protein, it was taken daily among 21.4% of the obese children compared to 8.2% of those who had normal weights and only 2% of those who had underweight (P = .002). Fast food was taken nearly 2-6 times per week among 45.6% of the obese children compared to 34% of children with n normal weights (P = .049). Sweets and chocolate were taken daily among 20.4% of children with overweight or obesity compared to 14.3% of those with normal weights (P = .632). Soft drinks were taken 2–6 times per week among 74.8% of the obese children compared to 68% of children with normal weights (P = .027). Also chips and crunches were taken 2-6 times per week among 76.7% of the obese children compared to 56% of normal weighted children with recorded statistical significance (P = .005).
Table 2.
Body mass index distribution according to students dietary habits in Aseer region, Southern Saudi Arabia
| Dietary habits | Total | Body mass index | P | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||
| Underweight | Normal | Overweight/Obese | ||||||||
|
|
|
|
|
|||||||
| No | % | No | % | No | % | No | % | |||
| Fruits and vegetables | Once weekly | 146 | 48.7% | 16 | 32.0% | 63 | 42.9% | 67 | 65.0% | 0.001* |
| 2-6/week | 139 | 46.3% | 29 | 58.0% | 77 | 52.4% | 33 | 32.0% | ||
| Daily | 15 | 5.0% | 5 | 10.0% | 7 | 4.8% | 3 | 2.9% | ||
| Legumes | Once weekly | 219 | 73.0% | 37 | 74.0% | 109 | 74.1% | 73 | 70.9% | 0.941 |
| 2-6/week | 79 | 26.3% | 13 | 26.0% | 37 | 25.2% | 29 | 28.2% | ||
| Daily | 2 | 0.7% | 0 | 0.0% | 1 | 0.7% | 1 | 1.0% | ||
| Whole grains | Once weekly | 12 | 4.0% | 2 | 4.0% | 7 | 4.8% | 3 | 2.9% | 0.958 |
| 2-6/week | 174 | 58.0% | 30 | 60.0% | 84 | 57.1% | 60 | 58.3% | ||
| Daily | 114 | 38.0% | 18 | 36.0% | 56 | 38.1% | 40 | 38.8% | ||
| Milk and milk products | Once weekly | 30 | 10.0% | 4 | 8.0% | 17 | 11.6% | 9 | 8.7% | 0.727 |
| 2-6/week | 171 | 57.0% | 30 | 60.0% | 78 | 53.1% | 63 | 61.2% | ||
| Daily | 99 | 33.0% | 16 | 32.0% | 52 | 35.4% | 31 | 30.1% | ||
| Animal protein | Once weekly | 42 | 14.1% | 8 | 16.3% | 24 | 16.4% | 10 | 9.7% | 0.002* |
| 2-6/week | 221 | 74.2% | 40 | 81.6% | 110 | 75.3% | 71 | 68.9% | ||
| Daily | 35 | 11.7% | 1 | 2.0% | 12 | 8.2% | 22 | 21.4% | ||
| Sea food | Once weekly | 264 | 88.0% | 40 | 80.0% | 130 | 88.4% | 94 | 91.3% | 0.254 |
| 2-6/week | 35 | 11.7% | 10 | 20.0% | 16 | 10.9% | 9 | 8.7% | ||
| Daily | 1 | 0.3% | 0 | 0.0% | 1 | 0.7% | 0 | 0.0% | ||
| Fast food | Once weekly | 158 | 52.7% | 33 | 66.0% | 77 | 52.4% | 48 | 46.6% | 0.049* |
| 2-6/week | 128 | 42.7% | 17 | 34.0% | 64 | 43.5% | 47 | 45.6% | ||
| Daily | 14 | 4.7% | 0 | 0.0% | 6 | 4.1% | 8 | 7.8% | ||
| Sweets and chocolate | Once weekly | 48 | 16.0% | 6 | 12.0% | 24 | 16.3% | 18 | 17.5% | 0.632 |
| 2-6/week | 201 | 67.0% | 35 | 70.0% | 102 | 69.4% | 64 | 62.1% | ||
| Daily | 51 | 17.0% | 9 | 18.0% | 21 | 14.3% | 21 | 20.4% | ||
| Soft drinks | Once weekly | 80 | 26.7% | 19 | 38.0% | 43 | 29.3% | 18 | 17.5% | 0.027* |
| 2-6/week | 205 | 68.3% | 28 | 56.0% | 100 | 68.0% | 77 | 74.8% | ||
| Daily | 15 | 5.0% | 3 | 6.0% | 4 | 2.7% | 8 | 7.8% | ||
| Chips and crunches | Once weekly | 58 | 19.3% | 15 | 30.0% | 31 | 21.1% | 12 | 11.7% | 0.005* |
| 2-6/week | 217 | 72.3% | 28 | 56.0% | 110 | 74.8% | 79 | 76.7% | ||
| Daily | 25 | 8.3% | 7 | 14.0% | 6 | 4.1% | 12 | 11.7% | ||
P: Pearson χ2 test. *P<0.05 (significant)
Discussion
Obesity is considered as the disease of twenty-first century due to its impact on morbidity and mortality, quality of life and health care costs. According to WHO, obesity is defined as a Body Mass Index (BMI) is equal to or greater than 30, obtained by dividing weight in kilograms by height in meters squared.[18,19] The main feature of obesity is the excessive accumulation of fat or general hypertrophy of adipose tissue in the body. Obesity is multifactorial diseases including genetic, biological, behavioural and cultural factors.[10] Obesity in children and adolescents can be related to many factors including binging which means losing the ability to stop overeating, physical inactivity, endocrine or neurological problems, exposure to life stressors such as separations, divorce, moves, deaths of family members, family problems, low self-esteem, depression or other emotional problems besides family history of obesity.[5,20,21]
A poor diet with high levels of fat or sugar and few nutrients lead to gain weight quickly. Fast food, candy, and soft drinks are common offenders. The U.S. Department of Health and Human Services (HHS) reports that 32 percent of adolescent girls and 52 percent of adolescent boys in the United States drink 24 ounces of soda – or more – per day.[22] Convenience foods, such as frozen dinners, salty snacks, and canned pastas, can also be considered. Many parents don't know how to choose or prepare healthy foods for their children which in turn helps in child weight gain. Other families may not be able to easily afford fresh fruits, vegetables, and meats.
The current study aimed to assess the prevalence of obesity among children in Aseer region and its relation with their dietary habits. The study revealed that about one-third of the children were overweight or obese as obesity itself recorded among nearly each fourth child. Overweight and obesity were more recorded among old-aged children (15 years or more) who were at the secondary schools. This may be due to the children at this age are away of parents control with more liability of fast food intake, beverages, and outdoor meals. This may be justified by that fast food was recorded for 2-6 times per week among 42.7% of the sampled children besides sweets and chocolate (67%), soft drinks (68.3%). Obesity was more recorded among these categories of children with more frequent unhealthy food and among those who and less fruits and vegetables weekly.
Kuźbicka K et al. conducted a literature review concerned with bad eating habits as the main cause of obesity among children.[23] The researchers reported that the problem recorded increasing trend especially among children. About 10% of world's school-aged children have an overweight and a 25% of these children are obese. In Europe one out of each five school-aged child suffers from an excess body weight. The review reported that low frequency of meals, skipping breakfast, eating in front of TV screen; drinking sugar sweetened beverages, eating without hunger, and eating out were the main factors behind weight gain. Another study was conducted in Canada to present recent overweight and obesity prevalence rates for 11–16-year-old Canadian youth and to examine associations between overweight and obesity with dietary habits and leisure-time physical activities.[24] The study revealed that 15% of Canadian youth were overweight and 4.6% were obese in 2002. Obesity was more prevalent among males but did not vary according to age. There were no clear associations observed between dietary habits and measures of overweight and obesity.
In Saudi Arabia, a study was conducted by Alqarni S et al., 2018[25] to assess childhood obesity trend in Saudi Arabia between years 1992 to 2022. The study reported that there will be increase in the obesity rate from 12% in 1992 to 60% at 2022. A review study was conducted by Hammad S, 2017[26] to examine prevalence, nutrition and activity, and overweight and obesity prevention and management in Saudi Arabia. The review included 32 studies regarding overweight and obesity. Studies showed that the range of overweight and obesity were greater in males (19.3% to 35.6%) than in females (11.8% to 19.2%). Male obesity is dominant as males had outdoor life than females exposing them to unhealthy outdoor meals. The study also assessed the effect of life style concluding that Lifestyle factors provide some specifics on the growing problem of childhood obesity in Saudi Arabia. However, cultural norms may vary from one region to another in Saudi society. One study in Abha found that 72% of children aged 8 to 18 years reported frequent consumption of breakfast, and only 28% reported skipping breakfast.[27] In contrast, a study in Jeddah found missing breakfast among more than half (54%) of the sample of children aged 13 to 18 years.[28] Healthier feeding behaviours were also seen in more urban areas than in less urban areas. These findings could aid in designing programs suited for different regions of the country.
Limitation of the study
The study depended on self-administered questionnaire from the children or their parents to report their anthropometric measures and dietary habits which is somewhat subjective and may give some bias in estimating children obesity status. Physical activity assessment was not included due to the high variety in age group of sampled children.
Conclusions and Recommendations
In conclusion, the study revealed that nearly one third of the children were overweight or obese with obesity more prevalent. Obesity was more recorded among old-aged children who frequently had unhealthy food including sweets and chocolate, and crunches. Also dietary habits were variable between healthy and unhealthy but fruits and vegetables intake was questionable. Health education sessions regarding healthy food and life style should be held for both children and their parents to improve their life style and dietary habits. Periodic screening programs for obesity are also wanted for early detection of any weight deviations from normality to avoid subsequent life-threatening complications and minimize the medical care cost.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Geiss HC, Parhofer KG, Schwandt P. Parameters of childhood obesity and their relationship to cardiovascular risk factors in healthy prepubescent children. Int J Obes. 2001;25:830–7. doi: 10.1038/sj.ijo.0801594. [DOI] [PubMed] [Google Scholar]
- 2.Lobstein T, Baur L, Uauy R. Obesity in children and young people: A crisis in public health. Obes Rev. 2004;5:4–85. doi: 10.1111/j.1467-789X.2004.00133.x. [DOI] [PubMed] [Google Scholar]
- 3.Herouvi D, Karanasios E, Karayianni C, Karavanaki K. Cardiovascular disease in childhood: The role of obesity. Eur J Pediatr. 2013;172:721–32. doi: 10.1007/s00431-013-1932-8. [DOI] [PubMed] [Google Scholar]
- 4.Wang Y, Lobstein TI. Worldwide trends in childhood overweight and obesity. Int J Pediatr Obes. 2006;1:11–25. doi: 10.1080/17477160600586747. [DOI] [PubMed] [Google Scholar]
- 5.Karnik S, Kanekar A. Childhood obesity: A global public health crisis. Int J Prev Med. 2012;3:1–7. [PMC free article] [PubMed] [Google Scholar]
- 6.De Onis M, Blössner M, Borghi E. Global prevalence and trends of overweight and obesity among preschool children. Am J Clin Nutr. 2010;92:1257–64. doi: 10.3945/ajcn.2010.29786. [DOI] [PubMed] [Google Scholar]
- 7.Puder JJ, Munsch S. Psychological correlates of childhood obesity. Int J Obes (Lond) 2010;34:S37–43. doi: 10.1038/ijo.2010.238. [DOI] [PubMed] [Google Scholar]
- 8.Katzmarzyk PT, Janssen I. The economic costs associated with physical inactivity and obesity in Canada: An update. Can J Appl Physiol. 2004;29:90–115. doi: 10.1139/h04-008. [DOI] [PubMed] [Google Scholar]
- 9.Wang Y, Monteiro C, Popkin BM. Trends of obesity and underweight in older children and adolescents in the United States, Brazil, China, and Russia. Am J Clin Nutr. 2002;75:971–7. doi: 10.1093/ajcn/75.6.971. [DOI] [PubMed] [Google Scholar]
- 10.Sahoo K, Sahoo B, Choudhury AK, Sofi NY, Kumar R, Bhadoria AS. Childhood obesity: Causes and consequences. J Family Med Prim Care. 2015;4:187–92. doi: 10.4103/2249-4863.154628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Epstein LH, Valoski A, Wing RR, McCurley J. Ten-year follow-up of behavioral, family-based treatment for obese children. JAMA. 1990;264:2519–23. [PubMed] [Google Scholar]
- 12.Flodmark CE, Ohlsson T, Rydén O, Sveger T. Prevention of progression to severe obesity in a group of obese schoolchildren treated with family therapy. Pediatrics. 1993;91:880–4. [PubMed] [Google Scholar]
- 13.Nowicka P. Dietitians and exercise professionals in a childhood obesity treatment team. Acta Paediatr Suppl. 2005;94:23–9. doi: 10.1111/j.1651-2227.2005.tb02125.x. [DOI] [PubMed] [Google Scholar]
- 14.Hanley AJ, Harris SB, Gittelsohn J, Wolever TM, Saksvig B, Zinman B. Overweight among children and adolescents in a Native Canadian community: Prevalence and associated factors. Am J Clin Nutr. 2000;71:693–700. doi: 10.1093/ajcn/71.3.693. [DOI] [PubMed] [Google Scholar]
- 15.Katzmarzyk PT, Barreira TV, Broyles ST, Champagne CM, Chaput JP, Fogelholm M, et al. Relationship between lifestyle behaviors and obesity in children ages 9–11: Results from a 12-country study. Obesity (Silver Spring) 2015;23:1696–702. doi: 10.1002/oby.21152. [DOI] [PubMed] [Google Scholar]
- 16.Prentice AM. Body mass index standards for children. BMJ. 1998;317:1401–2. doi: 10.1136/bmj.317.7170.1401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Onis MD, Onyango AW, Borghi E, Siyam A, Nishida C, Siekmann J. Development of a WHO growth reference for school-aged children and adolescents. Bull World Health Organ. 2007;85:660–7. doi: 10.2471/BLT.07.043497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.James PT. Obesity: The worldwide epidemic. Clin Dermatol. 2004;22:276–80. doi: 10.1016/j.clindermatol.2004.01.010. [DOI] [PubMed] [Google Scholar]
- 19.World Health Organization. Obesity Preventing and Managing the Global Epidemic, Report of a WHO Consultation on Obesity. Geneva: WHO; 1998. pp. 17–40. Global prevalence and secular trends in obesity. [PubMed] [Google Scholar]
- 20.Papoutsi GS, Drichoutis AC, Nayga RM., Jr The causes of childhood obesity: A survey. J Econ Surv. 2013;27:743–67. [Google Scholar]
- 21.Gurnani M, Birken C, Hamilton J. Childhood obesity: Causes, consequences, and management. Pediatr Clin North Am. 2015;62:821–40. doi: 10.1016/j.pcl.2015.04.001. [DOI] [PubMed] [Google Scholar]
- 22.Childhood obesity. [Achieved at 10/02/2020]. Available from: https://www.healthline.com/health/weight-loss/weight-problems-in-children .
- 23.Kuźbicka K, Rachoń D. Bad eating habits as the main cause of obesity among children. Pediatr Endocrinol Diabetes Metab. 2013;19:106–10. [PubMed] [Google Scholar]
- 24.Janssen I, Katzmarzyk PT, Boyce WF, King MA, Pickett W. Overweight and obesity in Canadian adolescents and their associations with dietary habits and physical activity patterns. J Adolesc Health. 2004;35:360–7. doi: 10.1016/j.jadohealth.2003.11.095. [DOI] [PubMed] [Google Scholar]
- 25.Alqarni S. Prevention of childhood obesity in Saudi Arabia. J Child Obes. 2018;3:S2–002. [Google Scholar]
- 26.Hammad SS, Berry DC. The child obesity epidemic in Saudi Arabia: A review of the literature. J Transcult Nurs. 2017;28:505–15. doi: 10.1177/1043659616668398. [DOI] [PubMed] [Google Scholar]
- 27.Farghaly NF, Ghazali BM, Al-Wabel HM, Sadek AA, Abbag FI. Life style and nutrition and their impact on health of Saudi school students in Abha, Southwestern region of Saudi Arabia. Saudi Med J. 2007;28:415–21. [PubMed] [Google Scholar]
- 28.Washi SA, Ageib MB. Poor diet quality and food habits are related to impaired nutritional status in 13-to 18-year-old adolescents in Jeddah. Nutr Res. 2010;30:527–34. doi: 10.1016/j.nutres.2010.07.002. [DOI] [PubMed] [Google Scholar]


