Abstract
Background:
High-risk pregnancy (HRP) puts current pregnancy at an increased risk of complications. In the absence of pre-existing HRP implementation model of the country, in collaboration with the Government of Himachal Pradesh, a new digital HRP model called the 'SEWA—A System E-approach for Women at risk' was developed. The current article demonstrates a model for the early identification and line listing of high-risk pregnant women (PW) with appropriate referrals and increased engagement with the healthcare workers using a digital tool in the form of the Android App.
Methods:
SEWA was implemented as a pilot intervention in two community development blocks of the Chamba district. The key implementation steps included finalizing protocols for the identification of HRPs, defining processes and roles, mapping health facilities, setting up the communication loop, and developing of digital solutions. The digital app, used by the auxiliary nurse midwife (ANM) and program officers, tracked PW for a year from October 19 to October 20 and recorded the ANC visits, referrals, and birth outcomes. A qualitative assessment was conducted among the health workers to find out their level of acceptance.
Results:
A total of 1,340 high-risk PW were identified. The intervention year saw a rise in the identification of HRP to 27.9% from 3.5% in the previous year. A total of 2,559 conditions were tagged to the identified 1,340 women categorized into current pregnancy (81%), previous pregnancy (16%), and any existing chronic illness (3%). A majority of the women who required urgent referrals were provided referrals. The application recorded 53% of the delivered HRP with a digital birth preparedness plan, prepared and shared with the PW and Accredited Social Health Activists (ASHA), by text message for compliance.
Conclusion:
The SEWA application is a feasible and sustainable solution to complement the competency of the care providers for early identification of the high-risk conditions and reduce the burden of preventable unprecedented deaths around the time of birth.
Keywords: Antenatal care, digital app, high-risk pregnancy, India, primary health care
Introduction
Pregnancy is a natural, physiological process, and yet, nearly 32,000 women are estimated to die annually in India during pregnancy and childbirth (NFHS 4). It also has one of the highest neonatal (28 per 1,000 live births) and early mortality rates (22 per 1,000 live births) along with a high and stagnant perinatal mortality of 26 per 1,000 live births.[1] High-risk pregnancy (HRP) is one which is complicated by factors that adversely affect the pregnancy outcome.[2] However, the exact proportion of HRPs in India is unknown. It is estimated that 20–30% of HRPs contribute to 75% of perinatal morbidity and mortality.[3] Considering the unpredictable nature of any pregnant woman becoming at risk at any time, the WHO (2016) recommended quality routine antenatal care (ANC) to every woman.
The Ministry of Health and Family Welfare (MoHFW) recommends at least four scheduled ANC visits.[4] However, the National Survey's (NFHS) report shows a continuous low coverage of ANC in the country. On average, only one in five pregnant women (PW) (21%) received all the ANC services with a wide variation in the ANCs across different states from as low as 2.3–65.9% (NFHS 4). Overall, about half of the PW (51.6%) had four or more ANC visits. The full ANC utilization can vary based on the womens' place of residence, their caste and educational level (NFHS4). (NFHS 4). A study in India found low levels of knowledge and practice of the management of high-risk pregnancy—only 35% of the staff at the primary health centers, and 51% at the community health centers, reported that they managed these conditions and the remaining staff referred most of such cases early in pregnancy.[5] The study also found that the healthcare staff desired skill-building and mentoring.
In 2013, the MoHFW launched the Reproductive, Maternal, Newborn, Child and Adolescent Health (RMNCH)+A strategic approach focusing on the needs of high-priority districts that have poor-performing RMNCH + A indicators. Since then, a significant number of policies and programs have been initiated to recognize early at-risk pregnancies like the Pradhan Mantri Surakshit Matritva Abhiyan,[6] New India 2022 Strategic Vision for Aspirational Districts Program (2018), and Surakshit Matritva Aashwasan (SUMAN, 2020).
Mhealth or the use of digital technology has gained considerable popularity as an education and service delivery platform (Chib et al., 2008; Lee et al., 2011).[7,8] Complex geography, caste or creed, education, economic status, intellectual capabilities, and unprecedented situations like the Coronavirus Disease 2019 (COVID-19) pandemic does not limit its reach (Varadraj et al., year). It offers 'One health'—an equitable inclusive approach facilitating the supply of standard evidence-based care delivery, improves patient engagement, and communication, real-time medication monitoring, and adherence support (Varadraj, 2017).
In the absence of any pre-existing HRP implementation model of the country, project collaborated with the Government of Himachal Pradesh (HP) to develop a new digital HRP model which is called 'SEWA—A System E-approach for Women at risk' to strengthen the frontline health workers' capacities to adherence to the standard operating guidelines for improving the e-management of PW, identified with high-risk conditions, using mobile technology.
For piloting the intervention, two blocks of the aspirational Chamba district were considered, given their low rates of antenatal contacts, loss to follow-up of antenatal cases, and poor engagement between the providers and PW leading to low-continued care.
The SEWA application guides the auxiliary nurse midwife (ANM) on the systematic steps to how an antenatal care visit should be conducted routinely for every woman. During the process, it helps the ANM identify risk factors which could have implications on the woman's health and her unborn.
Methods
Objectives
SEWA was implemented as a pilot intervention from October 2019 to October 2020 and has since been continuing under the aegis of the state government. The overall objective of the intervention was to improve the ANC program management with a special, with the following specific objectives:
Early identification and line listing of the high-risk PW
Timely and appropriate referral of the high-risk PW for further management
Increase engagement between the high-risk PW and frontline workers
Mixed methods were used to study the efficacy of the SEWA intervention. Program data (baseline from the Health Management Information System [HMIS] and data reported from the intervention) and qualitative feedback from the users were taken to assess the effectiveness and acceptability of the App.
The implementation geography
The state of Himachal Pradesh is a predominantly mountainous state with heavy snowfall in the winter months in the higher altitudes making many areas inaccessible. The United States Agency for international development (USAID)-funded Vriddhi (scaling up RMNCH + A interventions) Project has been providing technical assistance to the state government and Chamba district, an aspirational district identified by the NITI Ayog, Government of India. The project conducted a desk review of the HMIS data for the year 2018–2019 and in consultation with the state, the National Health Mission (NHM) identified two community development blocks, Pukhri and Samote, with poor identification of HRP for the pilot intervention. The baseline data of the two blocks were found to be low (3.5%) in HRP identification (HMIS 2018–2019).
Operational framework
The VRIDDHI team worked with the state government in providing technical support for developing the operational framework and its roll-out. The key activities undertaken during the implementation phase include the following:
Finalizing protocols for identification of HRPs at the sub-centers and Pradhan Mantri Surakshit Matritva Abhiyan (PMSMA) clinics, i.e. the development of a standardized list of high-risk conditions with its trigger values. All relevant conditions were included. Several consultative meetings with decision-makers and technical experts were held to get the technical content validated and the operational plan finalized.
Defining process and roles for tracking HRPs—ANMs' role in the identification and line listing, ASHA to follow-up and mobilize families for follow-up actions and visits to health centers, birth preparedness planning, roles of line managers from block to the state level.
Mapping and setting up the communication loop between the community level to the facility to the referral center and back, support, and review mechanisms in consultation with the stakeholders.
Development of digital solutions—SEWA mobile application
The SEWA mobile application was developed in alignment with the principles of digital development (digitalprinciples.org).
-
(a)
Design with the user: The App was made with the User Interface (UI) like a file/folder/register used by the healthcare workers. The button colors and layouts were made keeping in mind the visual cues they have been used to regularly. The features specific to their needs were incorporated.
-
(b)
Understand the existing ecosystem: The offline feature in the App adapted to low the Internet availability in the snow-bound terrains.
-
(c)
Design for scale: By using a combination of an Elastic Cloud Storage Solution to host the application at the backend and by mapping each user to its geographical location cross-referenced by its health workers' assigned health center, it was ensured that the application can be scaled up either block-wise or district-wise without any further additional inputs or major structural changes.
-
(d)
Build for sustainability: The basic tools and minimalist UI are used to ensure that there is no redundancy and obsolete features as the application moves forward in the ecosystem.
-
(e)
Be data-driven: Multiple level filters—from the type of HRP condition and their subcategories which can be further filtered as per the geographical area or timeline/date range right up to the individual user level.
-
(f)
Open standards: The application is built on Android—which is one platform—and primarily an open-source. The web version has been built on the PHP platform, which is also an open-source, thus, promoting, open standards.
-
(g)
Privacy and security: The Secure Sockets Layer (SSL) certificate for the web version, encryption of local database on the device, and encryption with masking of the data in the backend, IP blocking, and single-point access to the database, separate admin module of the App are there to ensure security and control over the users and accessibility.
The specifications for the App were made considering the health ecosystem with the aspects represented in Figure 1.
Figure 1.
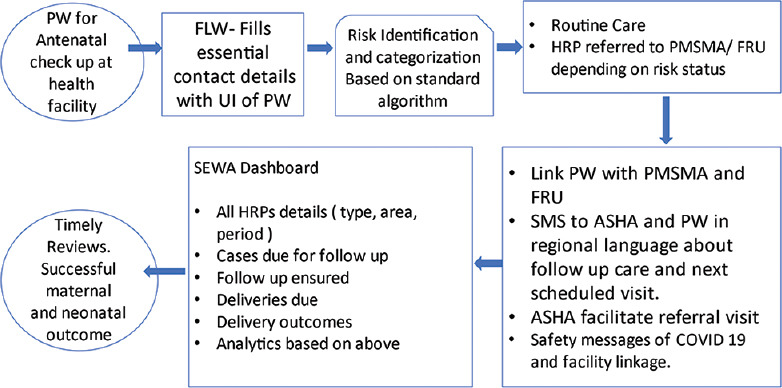
Flow design of the SEWA application.
The user acceptance testing was done with a sample of users in the implementation geography. The problems faced by the users and the suggested changes were incorporated before starting the pilot implementation.
Sensitization and capacity-building of the stakeholders: Posters and handouts were developed to train the frontline workers. These included guidance on clinical triggers for the risk conditions and action-required algorithms. The focus of the training was on the HRP conditions, and the use of the App to track PW with risk conditions. A total of 121 program officers and health workers (21 medical Officers, 96 staff nurses, and 4 counselors) were trained in three batches.
Implementation process
The users (ANMs and medical officers) started using the App immediately after the training. The ANMs from the health sub-centers started entering information of the PW in the App and tracking at-risk PW till the outcome.
Supportive supervision, monitoring, and review mechanisms
District monthly review meetings chaired by the Chief Medical Officer (CMO) constituted the main platform to review the progress of the intervention. Further, at the block level, block monthly review meetings with all the health workers and block medical officers were conducted. During these meetings, handholding of the frontline workers on the use of the App, improving identification with resolving issues and queries were done. Multiple supportive supervision visits were undertaken primarily by involving the first-line supervisors (health supervisors), block and district level officials along with the Vriddhi project team staff.
Qualitative assessment
Qualitative assessment of HRP tracking application was conducted with a structured questionnaire after 1 year of implementation. A total of 16 ANM and 4 male health workers were randomly selected (random draw of names from a bowl) from the two intervention blocks and were interviewed by three members from the national Vriddhi team. Due to the COVID situation, the interviews were conducted telephonically after obtaining informed consent.
Ethical review
Permission was granted by the state government of Himachal Pradesh to implement the pilot intervention. The state government was involved at every stage of the implementation as the intervention was integrated into the state health system. Routine health system data were used. For qualitative interviews, permission was obtained from the state NHM. The informed consent form was shared with the health workers who indicated their consent or otherwise in a WhatsApp message.
Data management and analysis
The data entered in the App were transferred to a project web portal. The indicators were tracked and periodic aggregation was conducted. The baseline data from the HMIS (2018–2019) were used to compare the number of PW identified with high-risk conditions. Qualitative information was entered into an excel sheet under the topic questions and content analysis was done. The attitude of the health workers toward the use of the HRP application was measured on a Likert Scale of 1–5 (1: strongly disagree, 2: disagree, 3: neutral, 4: agree, 5: strongly agree) on seven dimensions. The mean scores were computed.
Results
A total of 1,340 high-risk PW were identified in two blocks. Almost an equal number of women were identified from the two blocks. The majority of women were between 20 and 35 years. A lesser number of women were identified in the first trimester as compared to the second or third trimester [Table 1a].
Table 1a.
Demographic characteristics of pregnant women identified through the HRP App
| Characteristics | Number | Percentage |
|---|---|---|
| Block Pukhri | 710 | 53% |
| Block Samote | 630 | 47% |
| Age <20 years | 79 | 6% |
| Age 20-35 years | 1208 | 90% |
| Age >35 years | 53 | 4% |
| 1st trimester (Gestation 1-13 weeks) | 302 | 23% |
| 2nd trimester (Gestation 14-26 weeks) | 634 | 47% |
| 3rd trimester (Gestation above 26 weeks) | 404 | 30% |
The intervention year saw a rise in the identification of women with high-risk conditions [Table 1b]. The risk conditions were categorized into current pregnancy, previous pregnancy, and any existing chronic illness. In these three categories, a total of 2,559 conditions were tagged to the identified 1,340 PW [Table 2]. The current pregnancy complications were the most common (81%), followed by previous pregnancy complications (16%), and pre-existing chronic illness (3%).
Table 1b.
Identification of HRP in the intervention year (October 2019-October 2020) and the previous year (April 2018-March 2019)
| HRP App Oct 19 to Oct 20 | HMIS Baseline Apr 2018-Mar 2019 | |||||
|---|---|---|---|---|---|---|
|
|
|
|||||
| Pukhri | Samote | Total | Pukhri | Samote | Total | |
| PW registered for ANC | 2038 | 2773 | 4811 | 1823 | 2281 | 4104 |
| Total HRP identified | 710 | 630 | 1340 | 101 | 44 | 145 |
| HRP % out of the total ANC registration | 34.8% | 22.7% | 27.9% | 5.5% | 1.9% | 3.5% |
Table 2.
High-risk conditions of pregnant women (n=1340)
| Current pregnancy complications | |||
|---|---|---|---|
| HRP Diagnosis | Cases | Total | % of total conditions |
| Anemia in pregnancy (Sev. anemia-25, Moderate anemia-916) | 941 | 2068 | 81% |
| Pregnancy-induced hypertension (pih) | 52 | ||
| Hypothyroidism | 30 | ||
| Gestational diabetes mellitus | 68 | ||
| Ante-partum hemorrhage (aph)/accidental hemorrhage | 9 | ||
| Mal presentation | 97 | ||
| Low weight/Too thin | 352 | ||
| Other | 519 | ||
| Existing chronic illness | |||
| Tuberculosis | 15 | 79 | 3% |
| Diabetes mellitus | 2 | ||
| Rh-negative | 42 | ||
| Thyroid disorder | 12 | ||
| Infertility (under treatment) | 4 | ||
| Other | 4 | ||
| Previous pregnancy complications: Obstetric history | |||
| Abortion | 170 | 412 | 16% |
| Severe anemia | 14 | ||
| Pregnancy-induced hypertension (pih)/eclampsia | 8 | ||
| C-section operation | 144 | ||
| Still birth or neonatal death | 44 | ||
| Others | 32 | ||
| Total identified conditions in line listed 1340 PW | 2559 | ||
The ANC visits average 2.4 for all women after registration in the App while visits recorded for those who delivered were 3 [Table 3]. The women who required urgent referral based on their conditions were 28.9% of the total PW with high-risk conditions. The majority accessed referrals [Table 4]. The outcomes of 49% of the total identified women were known as the rest were still in the early stages of pregnancy. The application recorded 53% of delivered HRPs with a digital birth preparedness plan (BPP), prepared and shared with the PW and ASHA by text message for compliance. A total of 94.7% women safely delivered while the rest (5.3%) were abortion cases. With regard to institutional delivery, 79.2% were institutional and 70% were delivered in First Referral Unit (FRU) with Comprehensive emergency obstetric care (CEmOC) services as per the birth preparedness counseling by Health workers (HW) [Table 5].
Table 3.
Antenatal attendance
| Cases | Average attendance recorded | |
| All HRP cases | 1340 | 2.4 |
| Delivered cases | 625 | 3 |
Table 4.
Referral of pregnant women as per the birth preparedness plan (n=1340)
| Outcomes | Number (%) |
|---|---|
| Pregnant women required referral | 405 (28.9%) |
| Pregnant women referred | 332 (82%) |
Table 5.
Known outcomes of pregnancy (n=660)
| Outcomes | Cases | Percentage |
|---|---|---|
| Delivered | 625 | 94.7% |
| Inst. deliveries | 495 | 79.2% |
| Delivered at FRU | 435 | 69.6% |
| Abortion | 35 | 5.3% |
| Maternal death | 0 | 0.0% |
| Still birth | 14 | 2.2% |
| Neonatal death | 3 | 0.5% |
Findings of qualitative assessment
Qualitative assessment with 20 randomly selected users of the App was done and 80% of the health workers responded that the App is easy to use as, in the words of one ANM,
“Inclusion criteria of this application are very good; they helps us to correctly identify the HRP cases, and messages being sent to pregnant women PW and ASHA workers. Sometimes, we forget to deliver these important messages but as it is inbuilt in the App, it always sends the messages.” (ANM ID 3)
There were four (20%) HWs who reported difficulty in using the App. They cited poor connectivity, the App hanging up, or inability to enter old data.
On the question of the purpose of the App, the most common response was that it helped in reducing Maternal mortality ratio (MMR) by HRP identification and facilitated timely ANC and pregnancy management.
“The App helps to identify high-risk cases, provides knowledge about ANC, refers patients in a timely manner, and ensures follow-up of ANC check-ups.” (ANM ID 4)
According to the health workers, the average time taken to enter the HRP case during their first visit is 11 min and an average of 6 min during each subsequent visit, which according to them was appropriate and did not increase their burden. All the 20 respondents reported that the HRP tracking application was helping them to track the high-risk PW till their pregnancy outcome. As regards connectivity, 15 (75%) users had no problem while 5 (25%) of them reported some connectivity issue in the subcenter. Out of the 20 respondents, 15 reported that they were able to use it in the offline mode. Ninety percent of the respondents were aware of how the application can be synced after using it offline; 65% reported that the sync has to be done manually, and 35% reported that the application synced by itself.
Discussing the usefulness of messaging, all the 20 participants reported that SMS to PW and ASHA had helped them in tracking or HRP women. In their view, SMS to PW
“helps in reminder for follow-up to both PW and workers. PW are happy to receive messages—makes them feel somebody is taking care.” (ANM ID 11)
Also, in their view, SMS to ASHA “helps ASHA on social mobilization—taking PW to the health center, planning on when to go to the health center, prioritize visits to HRP, informs PW about birth preparedness plan, helps remind women about the next visit.” (ANM, ID 2)
On suggestions for improvement, while 60% said they had no problems and were fully satisfied with the App, others mentioned drawbacks and ways to improve. Back-dated entry was a common problem; Internet connectivity was another limitation. Among the suggestions for improvement was that it should work properly on ANMOL, the App should not stop working, and the user interface should not hang. Other suggestions were that the applications should come in one page and that the Reproductive and Child Health (RCH) portal of the Government of India and HRP should be synchronized in one app to avoid duplication.
An overall mean score of 4.5 was obtained, indicating that satisfaction with the App was on the higher side [Figure 2].
Figure 2.
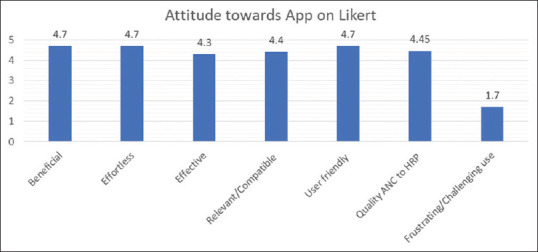
Attitude toward the use of the HRP App.
Discussion
The use of digital solutions for HRP was not only a technology upgradation—it was intended to enhance the operational scope, improve efficiency, and ensure greater equity in the delivery of the MNCH services. The use of the HRP App overcomes the natural challenges posed by the snowbound geographical terrains and takes advantage of the rising number of mobile users of the area. In addition, the digital solution seems to be easier and sustainable as the ANMs were already using the digital tool 'ANMOL' (ANM online) tablets provided by the state government.
In the digital health ecosystem, the plethora of mHealth initiatives has also seen technical challenges as identified by Gurupur and Wan which include usability, system integration, data security and privacy, network access, and reliability.[9] The HRP App is found to address these challenges to a reasonable extent. The usability of the App was high as evident by the improved line listing, increased birth preparedness planning, and as indicated by a high mean score on the attitude scale. In terms of system integration, the application has a provision of the integration of data from the existing portal of RCH currently used by governments. Data security is ensured through an SSL certificate for the web version, encryption of the local database on the device, and encryption with masking of data in the backend. The App allows only one point of contact approach for the addition of new users to the system. According to a Cochrane review, the main challenges the health workers in the primary health settings experienced were poor network connections.[10] In our intervention, just a quarter of the HWs interviewed reported not having the Internet coverage, further, the offline feature of the application helped HWs to save and complete their work when the work was relatively low. The HRP App is, in addition, reliable as evidenced by our finding that all the HWs in the qualitative piece reported that the application was helping them to track the high-risk pregnant woman till her pregnancy outcome. The SMS was also helpful in maintaining contact during the COVID lockdown. Our finding on the SMS reminders echoes other studies that text messaging reminders increase attendance at healthcare appointments.[11]
Ease of use has been reported as a major benefit of the App. The available literature has pointed out the importance of the ease of use of the software and applications.[12,13,14,15,16,17] Indeed, applications that were not user-friendly made HWs reluctant to use them (Schoen 2017).[14,17,18] For ease of the users, the App identifies PW by face and name rather than a random number, button colors. The layouts had visual cues used by Health Care Professionals (HCPs) routinely. The web version of the application enables use in the browser on any device, and mapping of each user to the geographical location to help with follow-up care. For reporting purposes, inputs were taken from the administrative and managerial user groups on the type of reports and filters they would need to generate meaningful information.
After the introduction of the digital application, a significant jump was seen in the HRP identification rate from the previous year in the two blocks. However, the increase should be treated with caution. In the previous year, the HRP data consisted of very few risk conditions while our intervention broadened them to include a high number of risks. Nevertheless, the App did manage to overcome the technical limitation that the health workers used to face about the identification of the HRP condition and deciding appropriate levels of care for PW. Lack of confidence among the health workers and the need to increase focus on the immediate care for complications, appropriate decision-making for referral, and improving referral communication for high-risk PW has been reported.[5]
Our findings on the risk conditions of the PW highlights the prevalence of anemia—70% of the identified women suffered from severe or moderate anemia. Globally, anemia is found to be one of the major indirect causes accounting for about one-fifth of maternal deaths (WHO, 2000–2010 decade report). Focused attention was being able to be delivered to these women by the ANM and ASHA following the standard protocol of GoI. Moreover, the women could now be categorized into having moderate and severe anemia and receive appropriate care as per their gestational age. Similar treatment protocols were followed with the other conditions, consistent with other studies that mobile technology helped HWs in following standard guidelines and protocol.[19] The majority of women who required referrals were referred echoing studies that referrals improved through digital referral coordinated systems.[20,21] Referral management and coordination is not an isolated process. Orton et al. pointed to the limitations to the degree to which patient referrals can truly be coordinated.[22] As referral compliance was added later to the system, one of the limitations is that we do not have the number of women who complied with the referrals. In the future roll-out of the App, this outcome would be an important addition.
Among those women who delivered, they had three ANC visits on average which is recorded after being registered in the App. As we did not analyze the average gestation at which the PW registered in the App, we cannot conclusively say whether this was a good or poor outcome. As a clinical decision support aid, the HRP App has not only increased the quality of care provided to the PW but also facilitated appropriate linkages to care and management at the facility level, consistent with a study finding in Tanzania.[23] In high-income countries, mobile support in clinical diagnosis and management to providers is found to show benefits.[11]
In terms of birth preparedness and complication readiness, the digital application recorded 53% of the delivered high-risk PW with BPP. However, one of the reasons for BPP not being recorded for the rest 47% of the women was that it was not entered in the system. Not all data were entered regularly or timely by HW, something to be noted for improvement in the future. Supervision and regular review of data are important to ensure updation and timely entry. The stillbirth and newborn deaths that occurred among this cohort could be a result of low preparedness at the tertiary level of the healthcare facilities. It could also be a result of some of the women not actually visiting referral facilities during their pregnancy. Ascertaining the level of preparedness to receive such HRPs at Comprehensive Obstetric and Newborn Care Service (CEmONC) level of healthcare facility was beyond the scope of this intervention.
The HRP tracking process with a digital tool will improve the ANC program management in the respective community of the primary care physicians. This will empower their frontline workers for early identification of any high-risk condition, provide customized women-centric care with facilitated decision-making for appropriate referrals, and increased follow-ups with easy data entry. For primary care physicians, this will streamline a systems-based mechanism for detection and management of high-risk pregnancies by integrating data, providing critical case-related information, and linking all the levels of stakeholders for concerted action. It will also help the primary care physicians to tailor the treatment/intervention as per the condition identified in the PW.
Limitations
A major limitation observed during the implementation is the availability of suitable and updated hardware with the Internet connectivity to the health worker. The government had provided the health workers with ANMOL tabs, but the functionality and availability to some extent is a challenge because of the lack of a sustainable mechanism to ensure updating of the hardware. A limitation was seen in the synching of the application in the background with the existing portal used by the health system for the auto-populated basic identification details and the total number of concurrent ANC visits. Better data management needs to be ensured. Another limitation was the initially designed login credential being health-worker specific, with his/her mobile number, which becomes a challenge in the dynamic nature of the health worker posting to a particular geography. The solution being the login to be facility-specific rather than person-specific. Furthermore, there is a limitation with respect to the list of high-risk conditions. It needs to be limited to key conditions to increase the focus on the at-risk cases. Although the high-risk conditions were taken from a variety of sources including a draft HRP guideline of the Government of India (GoI), they need to be amended according to the global and regional evidence. The mapping of the health facilities at all levels in geography must be more stringent, in consultation with the stakeholders. The lack of the feature in the App to update case records of PWs by the facility visited for referred ANC or institutional delivery and the access of the PW case record to the treating physician became the limiting factor for a complete referral loop. Future scale-up will need to consider these limitations for further improvement.
Conclusion
The SEWA application is a feasible and sustainable solution to complement the competency of the care providers for the early identification of high-risk conditions.
The digital application has overall helped to bring women under a safe institutional cover. However, to achieve the ultimate goal of reducing preventable deaths, the intervention has to strengthen the referral loop and quality of care at the referral facilities.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
This work was made possible by the support of the American people through the United States Agency for International Development under the terms of Cooperative Agreement Number AID 386 A 14 00001. The contents of this paper represent the views of the authors and do not reflect the views of the US Government.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Sankar MJ, Neogi SB, Sharma J, Chauhan M, Srivastava R, Prabhakar PK, et al. State of newborn health in India. J Perinatol. 2016;36((s3)):S3–S8. doi: 10.1038/jp.2016.183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jaideep KC, Prashant D, Girija A. Prevalence of high risk among pregnant women attending antenatal clinic in rural field practice area of Jawaharlal Nehru Medical College, Belgavi, Karnataka, India. Int J Community Med Public Health. 2017:1257. [Google Scholar]
- 3.Kulshreshtha S, Babel M. A prospective study of causes and outcome of high-risk pregnancies in referred patients in a tertiary health care centre of southern Rajasthan. J Obstet Gynecol. 2019;5:141–6. [Google Scholar]
- 4.Ministry of Health and Family Welfare, Government of India. Guidelines for Antenatal Care and Skilled Attendance at birth by ANM/LHV/SNs. Maternal Health Division. 2010. Apr, Available from: https://nhm.gov.in/images/pdf/programmes/maternal-health/guidelines/sba_guidelines_for_skilled_attendance_at_birth.pdf .
- 5.Singh S, Doyle P, Campbell OM, Murthy GV. Management and referral for high-risk conditions and complications during the antenatal period: knowledge, practice and attitude survey of providers in rural public healthcare in two states of India. Reprod Health. 2019;16:100. doi: 10.1186/s12978-019-0765-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ministry of Health and Family Welfare, Government of India. Pradhan Mantri Surakshit Matritva Abhiyan. National Health Portal. 2016. Available from: https://pmsma.nhp.gov.in/
- 7.Florez-Arango JF, Iyengar MS, Dunn K, Zhang J. Performance factors of mobile rich media job aids for community health workers. J Am Med Inform Assoc. 2011;18:131–7. doi: 10.1136/jamia.2010.010025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Braun R, Catalani C, Wimbush J, Israelski D. Community health workers and mobile technology: A systematic review of the literature. PLoS One. 2013;8:e65772. doi: 10.1371/journal.pone.0065772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gurupur VP, Wan TT. Challenges in implementing mHealth interventions: A technical perspective. Mhealth. 2017;3:32. doi: 10.21037/mhealth.2017.07.05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Odendaal WA, Anstey Watkins J, Leon N, Goudge J, Griffiths F, Tomlinson M, et al. Health workers' perceptions and experiences of using mHealth technologies to deliver primary healthcare services: A qualitative evidence synthesis. Cochrane Database Syst Rev. 2020;3:CD011942. doi: 10.1002/14651858.CD011942.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Free C, Phillips G, Watson L, Galli L, Felix L, Edwards P, et al. The effectiveness of mobile-health technologies to improve health care service delivery processes: A systematic review and meta-analysis. PLoS Med. 2013;10:e1001363. doi: 10.1371/journal.pmed.1001363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ginsburg AS, Tawiah Agyemang C, Ambler G, Delarosa J, Brunette W, Levari S, et al. mPneumonia, an innovation for diagnosing and treating childhood pneumonia in low-resource settings: A feasibility, usability and acceptability study in Ghana. PLoS One. 2016;11:e0165201. doi: 10.1371/journal.pone.0165201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Khan NU, Rasheed S, Sharmin T, Ahmed T, Mahmood SS, Khatun F, et al. Experience of using mHealth to link village doctors with physicians: Lessons from Chakaria, Bangladesh. BMC Med Inform Decis Mak. 2015;15:1–9. doi: 10.1186/s12911-015-0188-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kolltveit BH, Gjengedal E, Graue M, Iversen MM, Thorne S, Kirkevold M. Conditions for success in introducing telemedicine in diabetes foot care: A qualitative inquiry. BMC Nurs. 2017;16:1–10. doi: 10.1186/s12912-017-0201-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lodhia V, Karanja S. Acceptability, usability, and views on deployment of Peek, a mobile phone mHealth intervention for eye care in Kenya: Qualitative study. JMIR Mhealth Uhealth. 2016;4(:e30. doi: 10.2196/mhealth.4746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Praveen D, Patel A. SMARTHealth India: Development and field evaluation of a mobile clinical decision support system for cardiovascular diseases in rural India. JMIR Mhealth Uhealth. 2014;2:e54. doi: 10.2196/mhealth.3568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rothstein JD, Jennings L, Moorthy A, Yang F, Gee L, Romano K, et al. Qualitative assessment of the feasibility, usability, and acceptability of a mobile client data app for community-based maternal, neonatal, and child care in rural Ghana? Int J Telemed Appl. 2016;2016:1–14. doi: 10.1155/2016/2515420. doi: 10.1155/2016/2515420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ramirez M, Wu S, Ryan G, Towfighi A, Vickrey BG. Using beta-version mHealth technology for team-based care management to support stroke prevention: An assessment of utility and challenges. JMIR Res Protoc. 2017;6:e94. doi: 10.2196/resprot.7106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jones CO, Wasunna B, Sudoi R, Githinji S, Snow RW, Zurovac D. ''Even if you know everything you can forget'': Health worker perceptions of mobile phone text-messaging to improve malaria case-management in Kenya. PLoS One. 2012;7:e38636. doi: 10.1371/journal.pone.0038636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mbuagbaw L, Thabane L, Ongolo-Zogo P, Lester RT, Mills EJ, Smieja M, et al. The cameroon mobile phone SMS (CAMPS) trial: A randomized trial of text messaging versus usual care for adherence to antiretroviral therapy. PLoS One. 2012;7:e46909. doi: 10.1371/journal.pone.0046909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kabakyenga J, Barigye C, Brenner J, Maling S, Buchner D, Nettle-Aquirre A, et al. A demonstration of mobile phone deployment to support the treatment of acutely ill children under five in Bushenyi district, Uganda. Afr Health Sci. 2016;16:89–96. doi: 10.4314/ahs.v16i1.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Orton M, Agarwal S, Muhoza P, Vasudevan L, Vu A. Strengthening delivery of health services using digital devices. Glob Health Sci Pract. 2018;6((Suppl 1)):S61–71. doi: 10.9745/GHSP-D-18-00229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Agarwal S, Lasway C, L'Engle K, Homan R, Layer E, Ollis S, et al. Family planning counseling in your pocket: A mobile job aid for community health workers in Tanzania. Glob Health Sci Pract. 2016;4:300–10. doi: 10.9745/GHSP-D-15-00393. [DOI] [PMC free article] [PubMed] [Google Scholar]


