Abstract
Objectives:
The study aimed to assess the functionality of labour rooms by evaluating the labour room infrastructure with reference to the standard guidelines, the status of the availability of human resources, the availability of essential equipment and consumables in the labour room and by documenting the knowledge of the healthcare provider in terms of labour room practices. The study also explored the facility parameters associated with its delivery load taking the facility as a unit of analysis.
Design:
A cross-sectional analytical study.
Setting:
India has realised the importance of improving the quality of care in public health facilities, and steps are being taken to make healthcare more responsive to women's needs. With an increase in the proportion of institutional deliveries in India, the outcome of the delivery process can be improved by optimising the health facility components.
Participants:
The study was conducted in 52 health facilities and healthcare providers involved in the delivery process in the selected facilities.
Results:
The infrastructure of the facilities was found to be the best for medical college followed by district hospitals, Community Health Centres (CHCs), Primary Health Centres (PHCs) and subcentres. Similar findings were observed in terms of the availability of equipment and consumables. Lack of healthcare providers was observed as only 20% of the posts for health personnel were fulfilled in CHCs followed by PHCs, subcentres and district hospitals where 43, 50 and 79% of the available vacancies were fulfilled. The level of knowledge of healthcare providers in terms of partograph, active management of the third stage of labour and post-partum haemorrhage ranged as per their designation. The specialists were the most knowledgeable while the Auxiliary Nurse Midwife (AMNs) were the least. All the components of structural capacity, i.e. infrastructure (r2 = 0.377, P value < 0.001), equipment and consumable (r2 = 0.606, P value < 0.001) and knowledge of healthcare providers (r2 = 0.456, P value < 0.001) along with the overall facility score were positively correlated with the average delivery load of the health facility. The results from multivariate linear regression depict significant relation between the delivery load and availability of equipment and consumables (t = 4.015, P < 0.01) and with the knowledge of healthcare providers (t = 2.129, P = 0.039).
Conclusions:
The higher facilities were better equipped to provide delivery and newborn care. A higher delivery load was found at high-level facilities which can be attributed to better infrastructure, adequate supply of equipment and consumables and availability of trained human resources.
Keywords: Childbirth, facility assessment, labour room, maternal health, quality of healthcare
Introduction
Every pregnant woman and her family wish to have a joyful birthing experience with a safe and healthy mother and newborn. Yet, it has been estimated that globally every day, 810 women die of preventable causes related to pregnancy and childbirth.[1] The provision of high-quality healthcare for pregnant women, once they reach the healthcare facilities, has emerged as a challenge. Low quality of care at the time of birth hampers the health outcome among the mothers and neonates.
In India, many guidelines were made to improve the quality of healthcare services, yet no heed was paid specifically for maternal and neonatal health until 2013 when the Ministry of Health and Family Welfare designed the Maternal and Newborn Health (MNH) Toolkit whose objective was to provide support and guidance to policymakers and programme officers to establish health facilities providing maternal and neonatal services to ensure quality services. These guidelines classified health facilities as Basic Emergency Obstetric Care (BEmOC) and Comprehensive Emergency Obstetric Care (CEmOC) based on the minimal healthcare services provided at the facility. It helped to design, organise and manage MNH services by defining 'Delivery points' and Maternal Child Health (MCH) centres by the level of care provided. The MNH Toolkit helped in identifying the underlying factors which led to maternal and neonatal deaths, provided information on the standard protocols for MNH services and provided assistance in designing and managing MNH services including specific requirements for infrastructure, equipment, supplies, human resources, recording and reporting at all levels of public health facilities.
In 2016, the Ministry of Health and Family Welfare (MoHFW) launched Guidelines for Standardisation of Labour Rooms at Delivery Points. The guideline objective was to upgrade the labour rooms for standardisation, i.e. constructing new labour rooms or reorganising the existing labour rooms. This guideline was an extension of the MNH Toolkit that focuses explicitly on the space, layout of labour rooms, human resource requirements, equipment and supplies, consumables and protocols specifically for the labour room.
To improve the quality of care in the labour rooms and maternity operation theatres in government medical colleges, district hospitals and other high-caseload health facilities, the MoHFW launched Labour Room Quality Improvement Initiative Guidelines (LaQshya) in 2017. The goal of the LaQshya programme was to reduce maternal and newborn mortality and morbidity associated with the care around delivery in the labour room and maternal OT and to ensure respectful maternity care (RMC). To reduce maternal and newborn mortality and morbidity due to antepartum haemorrhage (APH), postpartum haemorrhage (PPH), retained placenta, preterm, pre-eclampsia and eclampsia, obstructed labour, puerperal sepsis, newborn asphyxia and sepsis; improving the quality of care during and the immediate postpartum period, stabilisation of complications and ensuring timely referrals and finally enhancing the satisfaction of the beneficiaries by RMC, the LaQshya guidelines ensure strict adherence to clinical protocols for management and stabilisation of the complication before referral, reorganising labour room and maternity OT as per the “Labour Room Standardisation Guidelines” and “Maternal and Newborn Health Toolkit”.
After the implementation of various programmes and policies by the Government of India to decrease the maternal mortality rate (MMR) and neonatal mortality rate (NMR) by improving the accessibility and quality of care provided to the mothers and newborns, there has been a definite improvement in the target parameters. Similar results were observed in the study district, but there has been a decline in the percentage of institutional deliveries (public) to total antenatal care (ANC) registration from 80% (2016– 2017) to 61% (2017–2018).[2] Limited research material was available to explain this decline, hence, this study was planned and it aimed to assess the gaps in the quality of care being provided to the mothers and newborns in the labour rooms by evaluating whether the labour rooms of the primary healthcare facilities were capable of providing the basic delivery and newborn services. Also, knowledge of the available resources will help to suitably devise management and treatment strategies.
The functionality of the labour rooms in terms of the basic delivery and newborn services was evaluated by assessing the status of the labour room infrastructure regarding the standard guidelines, the status of the availability of human resources, the availability of essential equipment and consumables in the labour room and by documenting the knowledge of healthcare provider in terms of labour room practices. The study also explored the association of facility parameters with its delivery load taking the facility as a unit of analysis.
Methods
We conducted a cross-sectional analytical study in the western district of Uttar Pradesh from January 2019 to August 2020. The study was conducted in the government health facilities from all the eight blocks of the selected district. The study also collected data from the healthcare providers to assess their knowledge regarding the most common causes of maternal mortality among perinatal women.
Study population and sampling
There were a total of eight blocks in the study district and the medical needs of its residents were attended by a total of 231 government health facilities (HMIS 2016–2017). These 231 facilities included one tertiary care hospital, one district hospital, eight Community Health Centres (CHCs), 27 Primary Health Centres (PHCs) and 194 subcentres.[3]
Out of the total 231 health facilities, 66 facilities were conducting delivery and 52 government health facilities were selected for the study where at least 10 normal vaginal deliveries were conducted in the duration of 6 months (April 1, 2018, to September 30, 2018). This selection was made according to the list obtained from the Chief Medical Officer's office containing the number of normal vaginal deliveries performed in the individual facilities. These 52 facilities comprised of one medical college, one district hospital, seven CHCs, five PHCs and 38 sub-centres.
All the healthcare providers who had a role in conducting delivery were included in the study. To assess the knowledge, only those healthcare providers were interviewed who were posted at the facility during the time of the survey. The healthcare providers who were assessed for their knowledge were auxiliary nurse midwives (ANM) at the level of subcentres; medical officer-in-charge (MOIc) of PHCs and its staff nurses; MOIc of CHCs, specialists and staff nurses performing vaginal delivery in CHCs; the chief medical superintendent of the district hospital, specialists and staff nurses performing vaginal delivery in the district hospital; the head of the department of obstetrics and gynaecology in the medical college, specialists, residents and staff nurses performing vaginal delivery in the medical college. In the district hospital and medical college, the staff nurses posted in the labour room at the time of facility assessment were assessed for their knowledge.
Data collection
The data were collected using two questionnaires; one for the health facility and the other for healthcare providers. Data were collected by making observations, record checking and interview method. The questionnaires were developed by taking literature from the WHO Standards for Improving Quality of Maternal and Newborn Care in Health Facilities, Labour Room Quality Improvement Initiative (LaQshya), MNH Toolkit, Guidelines for Standardisation of Labour Rooms at Delivery Points, DAKSHTA and other various studies conducted in the different states of India.[4,5,6,7]
The health facility questionnaire was categorised into three parts. The first part collected information on the infrastructure of the health facility, the second collected information on the availability of essential equipment and consumables while the third category assessed the availability of healthcare providers at the facility. The questionnaire for healthcare providers consists of closed-ended questions that assessed the knowledge of healthcare providers on topics like partograph, active management of the third stage of labour (AMTSL) and post-partum haemorrhage (PPH).
The questionnaire of healthcare providers was translated into the local language. In order to ensure that both the questionnaires, local language and English were conceptually equivalent, forward translation and back translation methods were implemented. A pilot study was conducted by assessing five health facilities and healthcare providers appointed in those facilities. Both the questionnaires depicted an excellent face validity, high internal consistency, Content Validity Index (CVI) greater than 0.8 and Cronbach's ranging from 0.7 to 0.8.[8,9] The data collected from the pilot study were not included in the study sample. Based on the results of the pilot study, necessary changes were made and the study proceeded.
Data analysis
The readiness of the labour rooms in a health facility was assessed based on two broad categories: Structural capacity of the health facility and knowledge of the healthcare providers providing delivery services in the respective health facilities.
Structural capacity
Structural capacity was assessed by evaluating the infrastructural parameters, staffing index and availability of essential equipment and consumables at the health facility.
Structural parameters of the labour rooms were evaluated under two broad headings: first, basic amenities in a health facility, and second, essential structural components of a labour room. Under these two headings, 15 components helped in computing an infrastructure score for every health facility (the details of the 15 components, scoring and calculation of the infrastructure score are listed in the online supplementary Appendix A1 and table A1).
The staffing index included the health personnel who were aiding in the delivery and newborn services. It was assessed based on the number of healthcare providers available versus the required per health facility. The information on the number of healthcare providers available at the facility was obtained from the facility in-charge while the healthcare providers required was calculated based on two guidelines: MNH and Labour Room Quality Improvement Initiative. Using these two pieces of information, the staffing index was calculated for each facility (the details of the scoring and staffing index calculation are listed in the online supplementary Appendix A2, table 2.1 and table 2.2).
To assess the availability of essential equipment and consumables, the facility in-charge and pharmacy in-charge were enquired along with visualisation of each item in the checklist. The assessment of the equipment and consumables was done under seven headings: diagnostic instruments, instruments for examination and monitoring, dressing material, protective equipment, newborn resuscitation, trays and records. Under these seven heading, 51 components helped in computing equipment and consumable score for every health facility (the details of the 51 components, scoring and calculation of equipment and consumable score are listed in online supplementary Appendix A3).
Knowledge of healthcare providers
The knowledge of healthcare providers on partograph, AMTSL and postpartum haemorrhage was assessed after enquiring if the healthcare providers attended any training session/received any information on partograph. A score was calculated for each facility based on the knowledge of the healthcare providers posted in the respective health facility (the details of the scoring and calculation of the score for knowledge of healthcare providers are listed in online supplementary Appendix A4)
The readiness of labour rooms of individual facilities was finally addressed as a percentage score for every health facility. It was calculated using the score percentages calculated for the four parameters: structural parameters, staffing index, availability of essential equipment and consumables at the health facility and knowledge of the healthcare providers. An average of all the facility scores of the individual facility was calculated for CHCs, PHCs and subcentres as more than one facility was evaluated in the study. The facility score percentage was graded as poor (0–50%), average (51–75%) and good (76–100%).
Statistical analysis
The collected forms were checked for completeness and quality, then the data were entered in Microsoft Excel. The entered data were checked, and in case of any incorrectness, they were matched with the respective questionnaire. The data were then analysed using the Statistical Package for Social Sciences (SPSS) version 24.0, IBM Inc. Chicago, USA software after coding it.
The availability of the assessed components and the knowledge of the healthcare providers were expressed in form of proportions while the scores computed for all the components (infrastructure, equipment and consumables, staff availability, healthcare provider knowledge and overall facility) were expressed in the form of mean ± standard deviation and percentages. The scores were depicted in the form of box plots describing the median, interquartile range and outliers. The correlation between the delivery load and various components assessed in the study was depicted as a scatter plot where P < 0.005 was considered significant. A multivariate linear regression analysis was performed to predict the effect of components like infrastructure, equipment and consumables, staff availability, healthcare provider knowledge and overall facility on the average delivery load of the facility.
Ethical consideration
The Ethical Committee of the institute granted ethical approval. Written permission was obtained from the Chief Medical Officer of the selected district to assess the facilities. Another written permission from the Medical Superintendent and Head of the Department of the Obstetrics and Gynaecology Department of the medical college was obtained. Informed written consent was made to be duly filled and signed by the healthcare providers interviewed.
Results
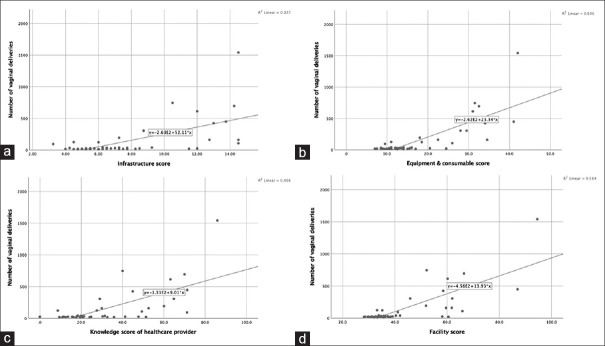
The data for this study were collected from the government health facilities in the study district. Among the 231 government health facilities, 66 (29%) facilities provided delivery and newborn services [Figure 1]. From the 66 facilities, 52 were selected according to the inclusion criteria. From the 52 facilities, 48 (one medical college, one district hospital, seven CHCs, five PHCs and 34 subcentres) proceeded for data collection as the remaining four health facilities were not conducting vaginal delivery. From the 48 health facilities, 117 healthcare providers were interviewed regarding their knowledge of delivery and newborn services [Figure 1]. The average delivery load in the health facilities was maximum for medical college (1,541) followed by CHCs (464), district hospital (448), PHCs (101) and subcentres (30).
Figure 1.
Flow diagram of the study.
Structural capacity
Infrastructure parameters
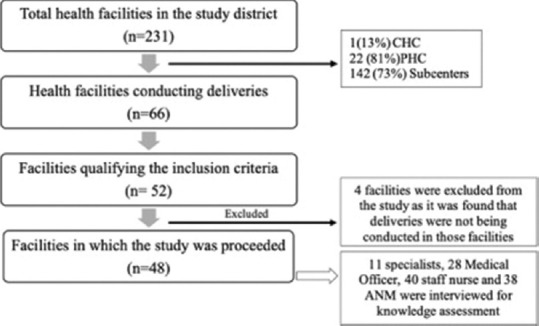
the infrastructure score percentage was the highest for medical college (96.6%) followed by district hospital (91.6%) while the average score for the CHC, PHC and subcentres was 77.8, 77.1 and 40%, respectively. The scores varied greatly amongst the facilities, particularly among the PHCs range: 48.3–96.6% [Figure 2].
Figure 2.
Infrastructure score across the different levels of primary healthcare facilities. Scores are presented as box plots describing the median, interquartile range and outliers (maximum infrastructure score 15).
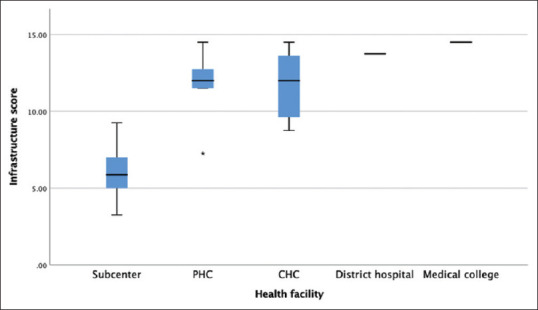
Communication and emergency transportation services were available at all the health facilities (100%), while among the least available items, hand hygiene station, protocol posters and focus light were available only in 4.1, 6.2, 8.3% of the facilities, respectively [Figure 3]. It was observed that all the infrastructure components were available at the medical college except for the focus lights. The district hospital was equipped with all the components except for focus lights and a hand hygiene station. Most of the components were available at the CHCs and PHCs except for the hand hygiene station. While in the subcentres, the hand hygiene station, buffer zone, focus lights, Newborn Care Corner (NBCC) and a computer with Internet services were unavailable at any of the subcentres [online supplementary Table S1].
Figure 3.
Availability of infrastructural components in different levels of primary healthcare facilities (n = 48)—medical college, district hospital, CHCs, PHCs and subcentres.
Staffing index
There was a gross shortage of healthcare providers and none of the vacancies was completely fulfilled [Table 1]. Based on the average delivery load, the medical college had adequate number of health personnel available at the facility. In the district hospital, the overall staffing index was 79% among which Obstetrics and Gyaecology (OBG)specialists, paediatricians and medical officer were available in the proportion of 80, 100 and 100%, respectively while the anaesthetists and staff nurses were deficient as they were occupying 60 and 75% of the positions available. The CHCs were most deficient in terms of the staffing index as only 20% of the positions were fulfilled [Figure 4]. None of the CHCs had paediatricians and anaesthetists while there was only 2.9% seats for OBG specialists, 27.8% for the staff nurse and 42.9% seats for the medical officers. The PHCs were primarily deficient in the availability of the staff nurses while there was a severe deficiency of ANM at the level of subcentres as only 50% of the ANMs were available [online supplementary Table S2].
Table 1.
Position of vacancies fulfilled against the available seats by the healthcare providers
| Designation | Total available | Total required | % Position fulfilled |
|---|---|---|---|
| Specialists | 53 | 23 | 43.4 |
| Medical officer | 40 | 34 | 85.0 |
| Staff nurse | 107 | 46 | 42.9 |
| ANM | 98 | 40 | 40.8 |
Figure 4.
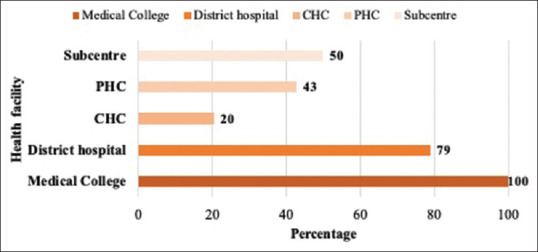
Position of vacancies fulfilled by the healthcare providers at different levels of primary care health facilities.
Equipment and consumables
the equipment score percentage at the medical college and district hospital was 96.1 and 91.37%, respectively. The availability of equipment and drugs was the weakest at the level of subcentres [Fig. 5]. All the equipment and consumables were available in the medical college and district hospital excluding eye cover. The diagnostic equipment (BP apparatus, stethoscope, thermometer) were available at all the CHCs and PHCs while the protective equipment like disposable gowns, face mask, caps, shoe covers and eye covers were only available at the medical college, district hospital and in less than half of the CHCs (42.9%). Items like the face masks, shoe covers, gowns and measuring tapes were absent in all the PHCs. In the subcentres most of the equipment and consumables were unavailable except for the measuring tape (14.7%), gown (2.9%) and sanitary napkin (2.9%). The availability of the newborn equipment and consumables was very poor. Only the weighing scale and cord clamp were available at more than 80% of the health facilities while the baby thermometer was unavailable at any of the facilities. Other equipment and consumables like the mucus extractor, IV cannula, mask of size 0 and 1, resuscitator bag, radiant warmer, oxygen catheter, oxygen cylinder, suction machine, and feeding tube were available in 66.7, 47.9, 22.9, 22.9, 18.8, 16.7, 16.7, 16.7 and 14.6% of the health facilities, respectively. In CHCs, only the feeding tube and mucus extractor were available in 57.1 and 71.4% of the facilities, respectively, while the rest of the consumables of the NBCC were available in more than 85% of the CHCs. The PHCs and subcentres were poorly equipped as a majority of the items were unavailable at the facilities. Except for medical college, none of the health facilities had the complete trays available. In the PHCs and subcentres only the delivery tray and baby tray were available at some health facilities, while the rest were unavailable. All the updated records and registers were available only at the medical college. Record maintaining was very poor at the subcentre and PHC levels [online supplementary Table S3].
Figure 5.
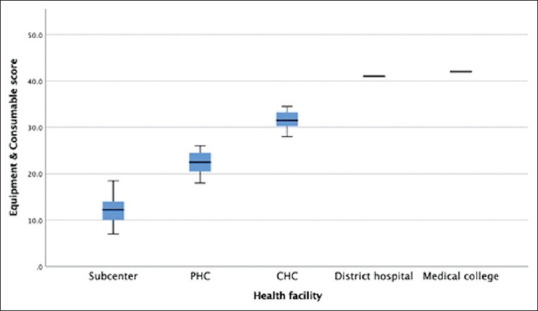
Equipment and consumable score across different levels of primary healthcare facilities. Scores are presented as box plots describing the median, interquartile range and outliers (maximum equipment and consumables score is 51 for all the facilities except for subcentre and PHC where the maximum score is 49).
Knowledge of healthcare providers
The knowledge of the healthcare providers regarding the components and use of partograph: 59.8–7.9% had correct knowledge while for AMTSL 91.4–11.9% of the healthcare providers had correct knowledge [Table 2]. Knowledge about PPH was poor as only 48.8–11.1% of the healthcare providers had correct knowledge. The specialists and medical officers were more knowledgeable in comparison to the staff nurses and the ANMs posted in the labour rooms. However, the maximum variation in the knowledge was reported amongst the staff nurses [Fig. 6].
Table 2.
Assessment of knowledge of healthcare providers in terms of partograph, active management of the third stage of labour and postpartum haemorrhage (n=117)
| Components | Correct response Frequency (%) |
|---|---|
| Partograph knowledge | 51.4 |
| Use of partograph | 27 (23.1) |
| When to begin plotting a partograph | 57 (48.8) |
| Parameters monitored every 30 min | 21 (17.9) |
| Parameters monitored every 4 hourly | 24 (20.6) |
| Normal foetal heart rate | 85 (72.6) |
| How long to measure a contraction | 74 (63.2) |
| Two lines marked in a partograph | 70 (59.8) |
| Importance of crossing of the alert line | 47 (40.1) |
| Importance of crossing of the action line | 46 (39.3) |
| Indications for referral | 21 (17.9) |
| AMTSL knowledge | 65.3 |
| Steps of AMTSL | 14 (11.9) |
| Drug of choice for AMTSL | 107 (91.4) |
| Other drugs used for AMTSL | 71 (60.7) |
| Route of oxytocin in AMTSL | 110 (94.1) |
| Route of misoprostol | 50 (42.7) |
| Steps for CCT | 17 (14.6) |
| PPH knowledge | 53.4 |
| Diagnosis of basis | 21 (17.9) |
| Causes of PPH | 31 (26.5 |
| Clinical features of PPH | 26 (22.2) |
| Estimation of blood loss | 13 (11.1) |
| Parameters monitored to assess PPH | 35 (29.9) |
| Non-surgical management of PPH | 24 (20.6) |
| Fluid recommended for PPH | 57 (48.8) |
| Uterotonics used for management of PPH | 44 (37.6) |
| Location to apply pressure for aortic compression | 39 (33.3) |
| Protocols followed before referring a case of PPH | 29 (24.8) |
Figure 6.
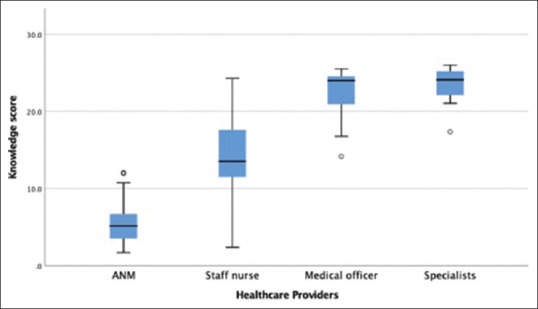
The knowledge score of the healthcare providers from all primary care health facilities. Scores are presented as box plots describing the median, interquartile range and outliers (maximum knowledge score is 26).
Overall facility score
Based on the individual facility scores, all the subcentres were graded under the 'poor' category in contrast to the medical college and district hospital which were categorised into 'good' grades [Fig. 7]. A few (14.3%) CHCs were falling under the 'poor' category while all the PHCs were categorised in 'average' grades.
Figure 7.
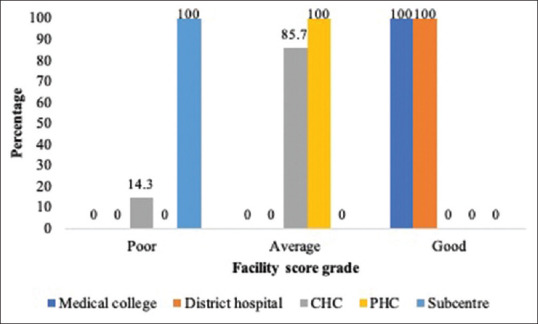
Distribution of health facilities based on the overall facility score.
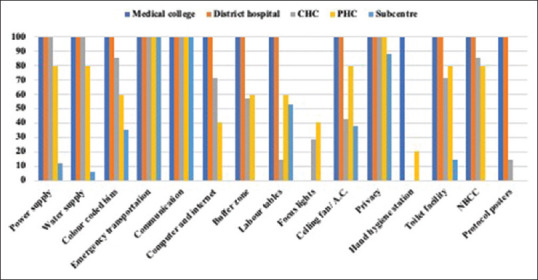
Relationship between average delivery load and structural capacity
All the components of structural capacity, i.e. infrastructure, equipment and consumables and knowledge of healthcare providers along with the overall facility score were positively correlated with the average delivery load of the health facility. Implying that as the scores of the facility will increase the delivery load of the facility will also increase [Fig. 8]. On multivariate linear regression, equipment and consumable along with healthcare provider knowledge depicted a statistically significant relationship with the average delivery load at the facility [Table 2]. The results from multivariate linear regression depict a significant relation between the delivery load and availability of equipment and consumables (t = 4.015, P < 0.01) and with the knowledge of healthcare providers (t = 2.129, P = 0.039) [Table 3].
Figure 8.
Correlation between the average number of deliveries conducted at the health facilities with the (a) infrastructure score (Pearson correlation = 0.377, P value 0.001) (b) equipment and consumable score (Pearson correlation = 0.606, P value 0.001) (c) knowledge score of healthcare providers (Pearson correlation = 0.456, P value 0.001) (d) the overall facility score (Pearson correlation = 0.584, P value 0.001).
Table 3.
Multivariate linear regression showing the relation between the average delivery load and components assessed for the health facility (infrastructure, equipment and consumables and healthcare provider knowledge)
| B | β | t | P | 95% Confidence interval | |
|---|---|---|---|---|---|
| Infrastructure | -2.840 | -0.223 | -1.266 | 0.212 | -7.361-1.682 |
| Equipment and consumables | 10.452 | 0.793 | 4.015 | <0.001 | 5.206-15.698 |
| Knowledge of healthcare providers | 3.464 | 0.260 | 2.129 | 0.039 | 0.184-6.743 |
Discussion
The evaluation of healthcare quality started with the work of Avedis Donabedian. In 1966, he proposed a framework for quality-of-care assessment that described quality in terms of structure, process and outcome.[10] Based on this broad concept, the present study provides evidence from the primary care health facilities of a district in western Uttar Pradesh about the structural and functional capacity of the labour rooms in these facilities. The study helps in identifying the gaps in terms of basic infrastructure, availability of equipment and consumables, staffing capacity and knowledge of healthcare providers. The study also explores the association of facility parameters with its delivery load taking the facility as a unit of analysis.
Despite the continuous efforts of the government to improve the availability of maternal and child health services, more than two-thirds of the facilities in the district were not providing delivery and newborn care among which the leading were the PHCs followed by the subcentres who did not offer any childbirth services. These findings were substantially high when compared with the results of Sharma J et al. (2017).[11] The discrepancy could either be due to the large sample size or it could be due to negligence in terms of maternal and newborn policy implementation. In the present study, the infrastructural capacity of the medical college and district hospital was better than CHCs and PHCs. Also, large gaps were observed in terms of structural components in the subcentres. These observations were consistent with the results stated in the study by Kaur J et al. (2019)[12] where the district hospitals were better in terms of structural capacity when compared to the PHCs. The study identified a lack of hand hygiene stations in a majority of the facilities in spite of it being an important component of infection control. Similarly, poster protocols were not being followed in most of the health facilities. Similar results were reported in a study conducted in Gujarat and Bihar which reported suboptimal infection control methods in many delivery units.[13,14] the availability of NBCC was very poor in the present study. It was reported only in one-fourth of the facilities, however, other states like Odisha were at par where only 13% of the facilities had no separate newborn corner within the labour room.[15]
The trends of the availability of the equipment and consumables were similar to the structural capacity of the present study, as with no surprise, the higher-level facilities were better equipped than the others. As studies have cited that lack of supplies is one of the major reasons for not performing the basic obstetric emergency care (Sabde et al., 2015[16]), it is important to improve the availability of the equipment and consumables in order to improve the quality of care for mothers and their newborns.
the results in this study were similar to various other studies that have stated that infrastructure, availability of medicine, ambulance, trained providers were prioritised by beneficiaries and these factors have also emerged as important determinants of good care.[17,18,19,20] This study suggests that a better infrastructure setup can increase the deliveries load of the facility as the infrastructure score was significantly correlated to the average deliveries conducted at the facility and this finding was in line with the previous studies (Singh A et al., 2016,[21] Kumar D et al., 2014[22]). Across the 48 facilities in this study, the delivery load was significantly correlated to the availability of equipment and consumables and this finding was consistent with the results of the study conducted by Spector JM et al.[23] (2013) according to which, the presence of gaps in the availability of essential childbirth-related consumables significantly reduced the birth volumes in the facilities. the availability of supplies and medicines along with the availability of medical and paramedical staff were found to be positively associated with institutional delivery and these were some of the major reasons for choosing a public health facility for delivery.[22,24]
The present study has several strengths. It contributes to the scant literature on the effect of facility parameters on institutional delivery in the districts of Uttar Pradesh. This study can lay the foundation for the ongoing studies in the district and help in comparing results from other districts and states in order to improve the quality of care provided in the labour rooms. As the study was conducted in a community setting it has more external validation. The collection of data for the study were conducted by a single observer, hence, eliminating observer bias. The estimation of the outcome using the binomial regression model adds to the strength of study results of this study. Among the topmost limitations is the inference of causality as it a cross-sectional study. It is possible that the facilities with a higher delivery load receive more resources or vice-versa.
Conclusion
The study has an important role in policy implications as the government can make changes in the facilities to improve the quality of maternal and child services provided. The study results indicate that the strengthening of labour rooms in the CHCs and PHCs and making the parameters meet the required guidelines would be an important step in achieving more institution-based deliveries. The role of the subcentres in providing the delivery and newborn services has been put into question after the results of this study. Catalytic capacity-building and quality improvement initiatives have resulted in an overall improvement; hence, they can be used for improving the quality of maternal and newborn services.[25,26]
Key Results
Around two-thirds of the primary care health facilities are not providing delivery and newborn services
The scores varied greatly amongst the facilities, particularly among the PHCs
the communication and emergency transportation services were available at all the health facilities
The CHCs were most deficient in terms of availability of health personnel
the availability of equipment and drugs was the weakest at the level of the subcentres
Record maintaining was very poor at the subcentre and PHC levels
The healthcare providers had inadequate knowledge on the PPH and partograph
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
This study received no specific grants from any funding agency in the public, commercial or not profit sectors.
Conflicts of interest
There are no conflicts of interest.
Acknowledgements
We would like to acknowledge the in charge of the facilities observed for their kind cooperation during the study process.
Appendix A1
The assessment of labour room infrastructure was done under two broad headings: first, the basic amenities in a health facility, and second, the essential structural components of a labour room. Under these two headings, 15 components helped in computing an infrastructure score for every health facility. In order to calculate the infrastructure score, a score out of 1 was assigned for each of the 15 components. These scores were added and divided by the total components, i.e. 15, which was then converted into a percentage by multiplying by 100. The score, hence, derived was the infrastructure score for the health facility.
To compute the score for power/electricity, a value of 1 was assigned to the facility with continuous power supply 24 × 7 throughout the year, a value of 0.5 was assigned to the facilities that faced occasional or regular disruption of power and a value of 0 to the facilities that reported no power supply. In any case, where a working power backup was available at the health facility, the score was replaced by 1. For water supply, a score of 1 was assigned for the availability of 24 × 7 running water, 0.5 for occasional availability of running water and 0 for no arrangement of water supply in the health facility. A score of 1 was assigned if all the four colour-coded (red, yellow, white and blue) bins were available at the facility and 0 if even any one of them was found to be missing. The facility was assigned a score of 1 on the availability of up-to-date protocols and awareness material on cleaning and disinfection, hand hygiene, safe waste management and maintenance of hygiene in the facility. A score of 0.25 or 0 was assigned per component, either on the availability or unavailability of the component, respectively. For emergency transportation, a score of 1 was assigned if the service was available in the health facility and 0 if it was not. For communication/telephone connection, a value of 1 was assigned if any means of communication were available at the health facility be it the mobile phones by the healthcare workers of the facility, else 0. For computer and the Internet connection, a score of 0.5 was assigned if the facility was provided with a computer and an additional 0.5 was assigned if the Internet connection was available. The facility with a buffer zone before entering the labour room was assigned a score of 1. In the absence of a buffer zone, the facility was assigned 0. The labour tables were assigned a score of 1 if they were adequate, 0.5 if inadequate and 0 if absent. The adequacy of the number of labour tables was calculated by reviewing the average number of deliveries conducted in the past 3 months from the time of data collection in the health facility.
Table A1.
Recommended number of labour tables per health facility based on the delivery load6
| Criteria | Number of table(s) |
|---|---|
| <20 deliveries/month | 1 |
| 20-99 deliveries/month | 2 |
| 100-199 deliveries/month | 4 |
| 200-499 deliveries/month | 6 |
| >500 deliveries/month | To be calculated as per the given formula for LDR or conventional labour room concept* |
No. of LDR beds= {(Projected LDR events in a year) * (Average length of stay))/{(365) *(occupancy rate))
For focus light, a score of 1 was given if one focus light was present for every labour table present, 0.5 if the focus light was present and 0 if it was absent. A score of 1 was given if the labour table was accompanied by one mounted ceiling fan, 0.5 if the ceiling fan was present in the labour room and 0 if the ceiling fan was present. A score of 1 was assigned even in the absence or in case of inadequate number of fans per labour table if the labour room was air-conditioned. For privacy in the labour room, a score of 1 was given if the doors and windows were in proper condition and providing adequate privacy while a score of 0 was assigned if either or both doors and windows were not in proper condition. A total score of 1 was assigned for the hand hygiene station as each component were given an equal weight of 0.25. The components of the hand hygiene station were marked as either 0.25 or 0 in the availability or unavailability of the items, respectively. The assessment of the toilet facility was based on four components: available— if the door of the toilet was unlocked, functional—if the hole/pit was not blocked and water was available for pour/flush, private—if the toilet had doors or screen that could be closed when needed and accessible—if it could be accessed without stairs or steps and it had handrails for support. When all four components were available, the toilet facility was marked as 1. If any one of the components was absent, the toilet facility was marked as 0. If there was the presence of a newborn care corner in the labour room or if it was reachable within 5 s, a score of 1 was assigned else 0 was assigned.
Appendix A2
The status of the human resource was assessed based on the number of human resources available versus the number of human resources required per health facility. The information on the number of healthcare workers posted in the facility was obtained from the facility in-charge. Then, the number of human resources required per facility was calculated based on two guidelines, one from the MNH Toolkit which was based on the level of facility and the other from the Labour Room Quality Improvement Initiative which was based on the delivery load.
Table A2.1.
Requirement of an adequately trained human resource based on the level of facility5
| Level 1 (SC/Non 24 × 7 PHC) | Level 2 (24 × 7 PHC/Non-FRU CHC) | Level 3 (FRU CHC/DH) |
|---|---|---|
| 2 ANM 1 parttime female sweeper |
1-2 MO Minimum 4 staff nurses/ANM each for the labour room and maternity ward Sweeper 3 |
Specialists including gynaecologist/EmOC, anaesthetist/LSAS, paediatrician Medical officers Staff nurse |
For a subcentre to provide quality care to the maternal and newborn care services, 2 ANM were required per facility. For a PHC, 1–2 medical officers and 4 staff nurses/ANM were required. To calculate the adequacy of the human resource posted in a CHC, district hospital and medical college, the average number of deliveries performed in the last 3 months from the time of facility assessment was calculated. Depending upon the delivery load, the human resource required was assessed from Table 2b.
Table A2.2.
Recommended minimum human resource for labour room in CHC/DH/Medical college based on the delivery load6
| No. of deliveries (per month) | Staff nurse | Other staff |
|---|---|---|
| 100-200 | 8 | 4 MO, 1 OBG/EmOC, 1 anaesthesia/LSAS, 1 paediatrician |
| 200-500 | 12 | 4 MO, 1 OBG (mandatory), 4 OBG/EmOC, 1 anaesthesia, 4 LSAS, 1 paediatrician |
| >500 | 16 | 4 MO, 3 OBG (mandatory), 4 EmOC, 1 anaesthesia, 4 LSAS, 1 paediatrician |
Appendix A3
The assessment of the equipment and consumables was done under seven headings: diagnostic instruments, instruments for examination and monitoring, dressing material, protective equipment, newborn resuscitation, trays and records. To assess the availability of the essential equipment and consumables, the facility in-charge and pharmacy in-charge were enquired along with the visualisation of each item in the checklist.
The diagnostic instruments were assigned a score of 1 each if they were available at the facility, otherwise, they were marked as 0. Among the instruments for examination and monitoring, the BP apparatus, adult thermometer, handheld foetal doppler and wall clock were marked as 1 each if they were available in a working condition while they were marked as 0 if they were available and not functional or were absent. Other items in instruments for examination and monitoring were assigned a score of 1 if they were available and 0 if they were not available. All the items under the dressing material and protective equipment excluding the hub cutter and autoclave were marked as 1 each if they were present at the time of the assessment and their supply was also maintained throughout the year. If an item was present and the supply was not maintained throughout the year, then the item was scored as 0.5 and if an item was unavailable at the time of assessment, it was marked as 0. If the hub cutter was available at the facility, it was marked as 1 otherwise 0. For autoclave, a score of 1 was assigned if it was present and functional otherwise a score of 0 was assigned if either it was present and not functional or absent. In the newborn resuscitation list, a score of 1 each was assigned for the baby weighing scale, baby thermometer, radiant warmer, suction machine, oxygen cylinder if they were available in a functioning form. These items were marked as 0 if either they were present and not functional or absent. Other items in the list like the paediatric resuscitator bag, mask (size 0, 1), mucus extractor, feeding tube, oxygen catheter, cord clamps and IV cannula 24 G/26 G were marked as 1 if they were present and 0 if they were absent. All the items in the trays were assessed and a score of 1 each was assigned if the tray was present and complete, 0.5 if the tray was present but incomplete and 0 if the tray was absent. To assess the case sheets, one case sheet was randomly chosen from the discharged patients of the previous month. If there were no filled case sheets available at the facility, then a score of 0 was assigned and if the case sheets were available, then they were marked out of 1, each of the headings under the case sheets was to be assessed over 0.2 each. If the details were mentioned in the case sheets, then a score of 0.2 was assigned else 0. The score was added up and a final score out of 1 was assigned to the case sheets. For the registers, a score of 1 was assigned if the register was present and updated, 0.5 if the register was present but not updated and 0 if the register was unavailable.
To calculate the equipment and consumable score, an average was calculated after adding up scores from all the 51 items (49 items for PHC and subcentre as two trays are not recommended for these facilities) in the list, and then, the percentage was calculated.
Appendix A4
The knowledge of the healthcare providers on the partograph was assessed after enquiring if they had attended any training session/received any information on the partograph. The knowledge on the partograph was assessed based on nine questions each of which were given a score of 1. The first four options on the use of partograph were each given a score of 0.25 totalling up to 1. A score of 0.25 was added up for each marked option while 0 was imparted if the healthcare provider had no knowledge on the use of partograph. A score of 1 was allotted if the participant marked option 2 for the time when plotting should begin in a partograph while a score of 0 was allotted if option 1 or option 3 was chosen. A score of 0.25 each was allotted for options from 1–4 while a score of 0 was allotted for option 5 for parameters that should be monitored every 30 min and parameters that should be monitored every 4 hourly. A final score was obtained after adding up all the scores for different options. For the lines marked in a partograph, option 1 alert line was allotted a score of 0.5, option 2 action line was allotted a score of 0.5, option 3 alert and action line were allotted a score of 1 and a score of 0 was allotted for no knowledge. A score of 1 was allotted if the healthcare provider had the knowledge on foetal heart rate, i.e. 120–160 beats per min else 0 was allotted for options 1 and 3. A score of 1 was allotted if the healthcare provider has the knowledge to monitor contractions for 10 min otherwise a score of 0 was allotted for options 1 and 3. A score of 1 was allotted if the indication of the alert line was marked as abnormal/prolonged labour and the indication for the action line was marked as the time for an intervention. For other options, a score of 0 was allotted to both the questions. For indications of referral, all options from 1 to 4 were correct and a score of 0.25 each was allotted for every option. The scores were added up for indications for referral based on the response of the healthcare provider. A score out of 10 was calculated for the knowledge of the healthcare provider on the partograph.
The knowledge of the healthcare providers on AMTSL was assessed after enquiring if they had attended any training session/received any information on AMTSL. A total of six questions were framed for assessing the knowledge each of which was awarded a score of 1. A score of 0 was awarded for each question if the healthcare provider has no knowledge about that particular question. The first question was about the steps followed in AMTSL which were three in number, hence, a score of 1/3 was awarded for each of the options and the total was calculated out of 1. The second question was regarding the drug used in AMTSL whose answer was oxytocin, a score of 1 was awarded for correct answer. The next question was on the other drugs which can be used in AMTSL whose correct answer was misoprostol for which a score of 1 was awarded for the correct answer. The fourth question was on the route used to administer oxytocin whose answer was the intramuscular route for which a score of 1 was awarded for the correct answers. The next question was to enquire the route of administration of misoprostol whose correct answer was the enteral route, a score of 1 was awarded for the correct answer. The last question was to enquire about the suitable conditions which should be followed before performing the control cord traction. All four options were awarded a score of ¼ each and the total score for the question was calculated by adding up all the correct answers. A score out of 6 was calculated for the knowledge of the healthcare provider on AMTSL.
The knowledge of the healthcare providers on PPH was assessed after enquiring if they had attended any training session/received any information on PPH. A total of 10 questions were framed for assessing the knowledge—each of which was awarded a score of 1. A score of 0 was awarded for each question if the healthcare provider had no knowledge about that particular question. The first question was regarding the methods for diagnosing PPH for which all three options were awarded a score of 1/3 each and the total score for the question was calculated by adding up the score. The second question was on the causes of PPH with four options with a score of ¼ awarded to each. The third question was on the clinical features of PPH which had five options with a score of 1/5 awarded to each. The fourth question was on the methods to assess blood loss with four options and a score of ¼ awarded to each. The fifth question was regarding the parameters which need to be measured during the management of PPH. It had three correct options with a score of 1/3 awarded to each. The next question enquired about the non-surgical method that can be used to manage a case of PPH. It had five correct options with a score of 1/5 awarded to each. The next question was about the IV recommended in a case of PPH. The correct answer was ringer lactate and a score of 1 was awarded for the correct answer. The eighth question was about the drugs that used to contract the uterus in case of atonic PPH to prevent bleeding. It had two correct options, one oxytocin, the other misoprostol. A score of ½ was awarded to each of the correct options. The ninth question was to assess the location where the aorta should be compressed in order to minimise bleeding in a case of PPH. The correct answer was towards the left of the umbilicus and it carries a score of 1 for the correct answer. The last question was on the measure to be undertaken before referring to a case of PPH. It had five correct options with a score of 1/5 awarded to each. A score out of 10 was calculated for the knowledge of the healthcare provider on PPH.1
Supplementary data
Table S1.
Distribution of infrastructure components at different levels of health facilities
| Infrastructure component | Medical college (n=1) n (%) | District hospital (n=1) n (%) | CHC (n=7) n (%) | PHC (n=5) n (%) | Subcentre (n=34) n (%) | Total (n=48) n (%) |
|---|---|---|---|---|---|---|
| Power supply | 1 (100.0) | 1 (100.0) | 7 (100.0) | 4 (80.0) | 4 (11.8) | 17 (35.4) |
| Water supply | 1 (100.0) | 1 (100.0) | 7 (100.0) | 4 (80.0) | 2 (5.9) | 15 (31.2) |
| Colour-coded bins | 1 (100.0) | 1 (100.0) | 6 (85.7) | 3 (60.0) | 12 (35.3) | 23 (47.9) |
| Emergency transportation | 1 (100.0) | 1 (100.0) | 7 (100.0) | 5 (100.0) | 34 (100.0) | 48 (100.0) |
| Communication | 1 (100.0) | 1 (100.0) | 7 (100.0) | 5 (100.0) | 34 (100.0) | 48 (100.0) |
| Computer and the Internet | 1 (100.0) | 1 (100.0) | 5 (71.4) | 2 (40.0) | 0 (0.0) | 9 (18.7) |
| Buffer zone | 1 (100.0) | 1 (100.0) | 4 (57.1) | 3 (60.0) | 0 (0.0) | 9 (18.7) |
| Labour tables | 1 (100.0) | 1 (100.0) | 1 (14.2) | 3 (60.0) | 18 (52.9) | 24 (50.0) |
| Focus light | 0 (0.0) | 0 (0.0) | 2 (28.6) | 2 (40.0) | 0 (0.0) | 4 (8.3) |
| Ceiling fan/air conditioner | 1 (100.0) | 1 (100.0) | 3 (42.9) | 4 (80.0) | 13 (38.2) | 22 (45.8) |
| Privacy | 1 (100.0) | 1 (100.0) | 7 (100.0) | 5 (100.0) | 30 (88.2) | 44 (91.6) |
| Hand hygiene station | 1 (100.0) | 0 (0.0) | 0 (0.0) | 1 (20.0) | 0 (0.0) | 2 (4.1) |
| Toilet facility | 1 (100.0) | 1 (100.0) | 5 (71.4) | 4 (80.0) | 5 (14.7) | 16 (33.3) |
| NBCC | 1 (100.0) | 1 (100.0) | 6 (85.7) | 4 (80.0) | 0 (0.0) | 12 (25.0) |
Table S2.
Availability of healthcare providers at different levels of health facilities
| Healthcare providers | Medical college | District hospital | CHC | PHC | Subcentre |
|---|---|---|---|---|---|
| OBG specialist | 100% | 80% | 2.9% | - | - |
| Paediatrician | 100% | 100% | 0 | - | - |
| Anaesthetist | 100% | 60% | 0 | - | - |
| Medical officer | 100% | 100% | 42.9% | 100% | - |
| Staff nurse | 100% | 75% | 27.8 | 25% | - |
| ANM | - | - | - | 25% | 50% |
Table S3.
Availability of the consumables and equipment in different levels of health facilities
| Consumables and equipment | Medical college (n=1) n (%) | District hospital (n=1) n (%) | CHC (n=7) n (%) | PHC (n=5) n (%) | Subcentre (n=34) n (%) | Total (n=48) n (%) |
|---|---|---|---|---|---|---|
| Glucometer | 1 (100.0) | 1 (100.0) | 2 (28.6) | 4 (80.0) | 0 (0.0) | 8 (16.7) |
| Protein kit | 1 (100.0) | 1 (100.0) | 6 (85.7) | 3 (60.0) | 18 (52.9) | 29 (60.4) |
| Haemoglobin kit | 1 (100.0) | 1 (100.0) | 3 (42.9) | 4 (80.0) | 31 (91.2) | 40 (83.3) |
| HIV kit | 1 (100.0) | 1 (100.0) | 4 (57.1) | 3 (60.0) | 0 (0.0) | 9 (18.8) |
| BP apparatus | 1 (100.0) | 1 (100.0) | 7 (100.0) | 5 (100.0) | 9 (26.5) | 23 (47.9) |
| Stethoscope | 1 (100.0) | 1 (100.0) | 7 (100.0) | 5 (100.0) | 5 (14.7) | 19 (39.6) |
| Thermometer | 1 (100.0) | 1 (100.0) | 7 (100.0) | 5 (100.0) | 24 (70.6) | 38 (79.2) |
| Foetal doppler | 1 (100.0) | 1 (100.0) | 4 (57.1) | 3 (60.0) | 0 (0.0) | 9 (18.8) |
| Fetoscope | 1 (100.0) | 1 (100.0) | 1 (14.3) | 0 (0.0) | 19 (55.9) | 22 (45.8) |
| Measuring tape | 1 (100.0) | 1 (100.0) | 3 (42.9) | 0 (0.0) | 5 (14.7) | 10 (20.8) |
| Wall clock | 1 (100.0) | 1 (100.0) | 7 (100.0) | 5 (100.0) | 21 (61.8) | 35 (72.9) |
| Gauze piece | 1 (100.0) | 1 (100.0) | 7 (100) | 4 (80.0) | 20 (58.8) | 33 (68.7) |
| Cotton swab | 1 (100.0) | 1 (100.0) | 6 (85.7) | 4 (80.0) | 22 (64.7) | 34 (70.8) |
| Sanitary pads | 1 (100.0) | 1 (100.0) | 2 (85.7) | 3 (60.0) | 12 (35.3) | 19 (39.6) |
| Sanitary napkin | 1 (100.0) | 1 (100.0) | 2 (28.6) | 3 (60.0) | 1 (2.9) | 8 (16.7) |
| Antiseptic solution | 1 (100.0) | 1 (100.0) | 7 (100.0) | 5 (100.0) | 17 (50) | 31 (64.6) |
| Surgical blade | 1 (100.0) | 1 (100.0) | 7 (100.0) | 5 (100.0) | 11 (32.4) | 25 (52.1) |
| Hub cutter | 1 (100.0) | 1 (100.0) | 6 (85.7) | 4 (80.0) | 31 (91.2) | 43 (89.6) |
| Autoclave | 1 (100.0) | 1 (100.0) | 7 (100.0) | 4 (80.0) | 0 (0.0) | 13 (27.1) |
| Sterile gloves | 1 (100.0) | 1 (100.0) | 6 (85.7) | 5 (100.0) | 18 (52.9) | 31 (64.6) |
| Gown | 1 (100.0) | 1 (100.0) | 3 (42.9) | 0 (0.0) | 1 (2.9) | 6 (12.5) |
| Face masks | 1 (100.0) | 1 (100.0) | 2 (28.6) | 0 (0.0) | 0 (0.0) | 4 (8.3) |
| Caps | 1 (100.0) | 1 (100.0) | 3 (42.9) | 0 (0.0) | 0 (0.0) | 5 (10.4) |
| Shoe cover | 1 (100.0) | 1 (100.0) | 3 (42.9) | 0 (0.0) | 0 (0.0) | 5 (10.4) |
| Eye cover | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Weighing scale | 1 (100.0) | 1 (100.0) | 6 (85.7) | 5 (100.0) | 28 (82.4) | 41 (85.4) |
| Baby thermometer | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Radiant warmer | 1 (100.0) | 1 (100.0) | 7 (100.0) | 0 (0.0) | 0 (0.0) | 9 (18.8) |
| Suction machine | 1 (100.0) | 1 (100.0) | 6 (85.7) | 0 (0.0) | 0 (0.0) | 8 (16.7) |
| Oxygen cylinder | 1 (100.0) | 1 (100.0) | 6 (85.7) | 0 (0.0) | 0 (0.0) | 8 (16.7) |
| Resuscitator bag | 1 (100.0) | 1 (100.0) | 7 (100.0) | 2 (40.0) | 0 (0.0) | 11 (22.9) |
| Mask (size 0, 1) | 1 (100.0) | 1 (100.0) | 7 (100.0) | 2 (40.0) | 0 (0.0) | 11 (22.9) |
| Mucus extractor | 1 (100.0) | 1 (100.0) | 5 (71.4) | 3 (60.0) | 22 (64.7) | 32 (66.7) |
| Feeding tube | 1 (100.0) | 1 (100.0) | 4 (57.1) | 1 (20.0) | 0 (0.0) | 7 (14.6) |
| Oxygen catheter | 1 (100.0) | 1 (100.0) | 6 (85.7) | 0 (0.0) | 0 (0.0) | 8 (16.7) |
| Cord clamp | 1 (100.0) | 1 (100.0) | 7 (100.0) | 5 (100.0) | 25 (73.6) | 39 (81.3) |
| IV cannula 24 G | 1 (100.0) | 1 (100.0) | 7 (100.0) | 3 (60.0) | 11 (32.4) | 23 (47.9) |
| Delivery tray | 1 (100.0) | 1 (100) | 6 (85.7) | 2 (40.0) | 3 (8.8) | 13 (27.0) |
| Episiotomy tray | 1 (100.0) | 1 (100) | 3 (42.9) | 0 (0.0) | 0 (0.0) | 5 (10.4) |
| Baby tray | 1 (100.0) | 1 (100) | 4 (57.1) | 1 (20.0) | 1 (2.9) | 8 (16.7) |
| Medicine tray | 1 (100.0) | 0 (0.0) | 3 (42.9) | 0 (0.0) | 0 (0.0) | 4 (8.3) |
| Emergency tray | 1 (100.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (2.1) |
| MVA/EVA tray | 1 (100.0) | 1 (100.0) | 2 (28.6) | 0 (0.0) | - | 4 (8.3) |
| PPIUCD tray | 1 (100.0) | 1 (100.0) | 3 (42.9) | 0 (0.0) | - | 5 (10.4) |
| Case sheets | 1 (100.0) | 0 (0.0) | 2 (28.6) | 0 (0.0) | 0 (0.0) | 3 (6.2) |
| Labour room register | 1 (100.0) | 1 (100.0) | 7 (100.0) | 5 (100.0) | 21 (61.8) | 35 (72.9) |
| MTP register | 1 (100.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | - | 1 (2.0) |
| Interval and PPIUCD register | 1 (100.0) | 1 (100.0) | 0 (0.0) | 0 (0.0) | - | 2 (4.1) |
| Maternal and infant death register | 1 (100.0) | 1 (100.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 2 (4.1) |
| Referral in/out register | 1 (100.0) | 1 (100.0) | 2 (28.6) | 2 (40.0) | 0 (0.0) | 6 (12.5) |
| Stock register | 1 (100.0) | 1 (100.0) | 5 (71.4) | 4 (80.0) | 8 (23.5) | 19 (39.6) |
References
- 1.Maternal mortality. World Health Organization. 2019. [[Last accessed on 2021 Jan 21]]. published online September 19. Available from: https://www.who.int/news-room/fact-sheets/detail/maternal-mortality .
- 2.Health Management Information system. National Health Mission. Ministry of Health and Family Welfare, Government of India. [[Last accessed on 2021 Jan 21]]. Available from: https://hmis.nhp.gov.in/#!/aboutus .
- 3.Directorate of Census Operations. District Census Handbook Etawah. Lucknow: Directorate of Census Operations; 2011. p. 17. [Google Scholar]
- 4.Government of India. Labour Room Quality Improvement Initiative- National Health Mission. Ministry of Health and Family Welfare. 2017. [[Last accessed on 2021 Jan 21]]. Available from: https://nhm.gov.in/index1.php?lang=1&level=3&sublinkid=1307&lid=690 .
- 5.Government of India. Maternal and Newborn Health Toolkit- Maternal Health Division, Ministry of Health and Family Welfare. 2013. Jan, [[Last accessedon 2021 Jan 21]]. Available from: http://www.dkhfw.in/wp-content/uploads/2017/07/Maternal_Newborn_Health_Toolkit.pdf .
- 6. [[Last accessed on 2021 Jan 21]];Government of India. Standardization of Labour room at delivery point- Maternal Health Division, Ministry of Health and Family Welfare. 2016 April; https:// nhm.gov.in/images/pdf/programmes/maternal-health/guidelines/Labor_Room%20Guideline.pdf. [Google Scholar]
- 7.World Health Organization. Standards for improving quality of maternal and newborn care in health facilities. World Health Organization. 2016. [[Last accessed on 2021 Jan 21]]. Available from: https://apps.who.int/iris/bitstream/handle/10665/249155/9789241511216-eng.pdf; jsessionid=658D138DBA4D903F3150942D174F80E6?sequence=1 .
- 8.Yusoff MS. ABC of content validation and content validity index calculation. Educ Med J. 2019;11:49–54. [Google Scholar]
- 9.Valim MD, Marziale MH, Hayashida M, Rocha FL, Santos JL. Validity and reliability of the questionnaire for compliance with standard precaution. Rev Saude Publica. 2015;49:87. doi: 10.1590/S0034-8910.2015049005975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Donabedian A. Evaluating the quality of medical care. Milbank Q. 1966;44:166–206. [PubMed] [Google Scholar]
- 11.Sharma J, Leslie HH, Regan M, Nambiar D, Kruk ME. Can India's primary care facilities deliver. A cross-sectional assessment of the Indian public health system's capacity for basic delivery and newborn services? BMJ open. 2018;8:e020532. doi: 10.1136/bmjopen-2017-020532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kaur J, Franzen SR, Newton-Lewis T, Murphy G. Readiness of public health facilities to provide quality maternal and newborn care across the state of Bihar, India: A cross-sectional study of district hospitals and primary health centres. BMJ Open. 2019;9:e028370. doi: 10.1136/bmjopen-2018-028370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mehta R, Mavalankar DV, Ramani KV, Sharma S, Hussein J. Infection control in delivery care units, Gujarat state, India: A needs assessment. BMC Pregnancy Childbirth. 2011;11:1–8. doi: 10.1186/1471-2393-11-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.State Health Society, Bihar. Assessment of Labour Rooms in Public Health Facilities of Bihar. Department of Health and Family Welfare. Government of Bihar. 2012. [[Last accessed on 2021 Jan 21]]. Available from: http://statehealthsocietybihar.org/pip2011-12/statepip-2011-12/BHR%20SPIP%2011-12%20_Final-April%202011_12.pdf .
- 15.Orissa Technical Management Support Team. State Specific Comprehensive Procurement and distribution Reform Strategy for Drugs, equipment and Other Medical Supplies. Department of Health and Family Welfare. Government of Orrisa. [[Last accessed on 2021 Jan 21]]. Available from: http://nhmodisha.gov.in/writereaddata/Upload/Documents/State%20Specific%20Comprehensive%20Procurement%20and.pdf .
- 16.Sabde Y, Diwan V, Randive B, Chaturvedi S, Sidney K, Salazar M, et al. The availability of emergency obstetric care in the context of the JSY cash transfer programme in Madhya Pradesh, India. BMC Pregnancy Childbirth. 2016;16:1–3. doi: 10.1186/s12884-016-0896-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Andaleeb SS. Service quality perceptions and patient satisfaction: A study of hospitals in a developing country. Soc Sci Med. 2001;52:1359–70. doi: 10.1016/s0277-9536(00)00235-5. [DOI] [PubMed] [Google Scholar]
- 18.Duong DV, Binns CW, Lee AH, Hipgrave DB. Measuring client-perceived quality of maternity services in rural Vietnam. Int J Qual Health Care. 2004;16:447–52. doi: 10.1093/intqhc/mzh073. [DOI] [PubMed] [Google Scholar]
- 19.Dzomeku MV. Maternal satisfaction with care during labour: A case study of the Mampong-Ashanti district hospital maternity unit in Ghana. Intern J Nursing Midwifery. 2011;3:30–4. [Google Scholar]
- 20.George A. Quality of reproductive care in private hospitals in Andhra Pradesh. Womens Perception Econ Polit Wkly. 2002;37:1686–92. [Google Scholar]
- 21.Singh A. Supply-side barriers to maternal health care utilization at health sub-centers in India. PeerJ. 2016;4:e2675. doi: 10.7717/peerj.2675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kumar S, Dansereau E. Supply-side barriers to maternity-care in India: A facility-based analysis. PLoS One. 2014;9:e103927. doi: 10.1371/journal.pone.0103927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Spector JM, Reisman J, Lipsitz S, Desai P, Gawande AA. Access to essential technologies for safe childbirth: A survey of health workers in Africa and Asia. BMC Pregnancy Childbirth. 2013;13:1–7. doi: 10.1186/1471-2393-13-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bhattacharyya S, Srivastava A, Saxena M, Gogoi M, Dwivedi P, Giessler K. Do women's perspectives of quality of care during childbirth match with those of providers. A qualitative study in Uttar Pradesh, India? Glob Health Action. 2018;11:1527971. doi: 10.1080/16549716.2018.1527971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Das MK, Chaudhary C, Mohapatra SC, Srivastava VK, Khalique N, Kaushal SK, et al. Improvements in essential newborn care and newborn resuscitation services following a capacity building and quality improvement program in three districts of Uttar Pradesh, India. Indian J Community Med. 2018;43:90–6. doi: 10.4103/ijcm.IJCM_132_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Makene CL, Plotkin M, Currie S, Bishanga D, Ugwi P, Louis H, et al. Improvements in newborn care and newborn resuscitation following a quality improvement program at scale: Results from a before and after study in Tanzania. BMC Pregnancy Childbirth. 2014;14:381. doi: 10.1186/s12884-014-0381-3. [DOI] [PMC free article] [PubMed] [Google Scholar]