Abstract
Objective:
To describe how different key stakeholders (i.e., interprofessional clinical care team and patients) perceive their role in promoting in-hospital mobility by systematically synthesizing qualitative literature.
Data sources:
PubMed, Ovid Medline, Ovid PsychInfo, and CINAHL were searched using terms relevant to mobility, hospitalization and qualitative research. 510 unique articles were retrieved and screened for eligibility.
Study Selection:
Eligible qualitative studies included stakeholder perspectives on in-hospital mobility, including patients, nursing staff, rehabilitation staff, and physicians. Eleven articles remained after inclusion/exclusion criteria were applied.
Data extraction:
At least two authors independently read, coded, and derived themes from each study. We used a team-based inductive approach to thematic synthesis informed by critical realism and the socioecological model. Reciprocal translation unified convergent and divergent constructs across primary studies. Investigator triangulation enhanced interpretation
Data Synthesis.
Three primary themes emerged: (1) Patient, family, and clinician expectations shape roles in in-hospital mobility. (2) Stakeholders’ role in mobility depends on hospital environment, infrastructure, culture and resources, and (3) Teamwork creates successful in-hospital mobility, but lack of coordination and cooperation leads to delay in mobilizing. Studies suggested that while mobility is an essential construct in the professional role of clinicians and in the personal identity of patients, the ability of stakeholders to realize their role in mobility is highly dependent on the hospital physical and cultural environment, administrative support, clarity in professional roles, and teamwork.
Conclusions:
Interventions designed to address the problem of low-hospital mobility should take a systems approach and consider allocation of resources, clarity around professional responsibilities, and elevating patient and clinician expectations surrounding mobility.
Keywords: Exercise, physical therapists, physical activity, mobility limitation, nursing staff, hospital, qualitative research, frail elderly, inpatients
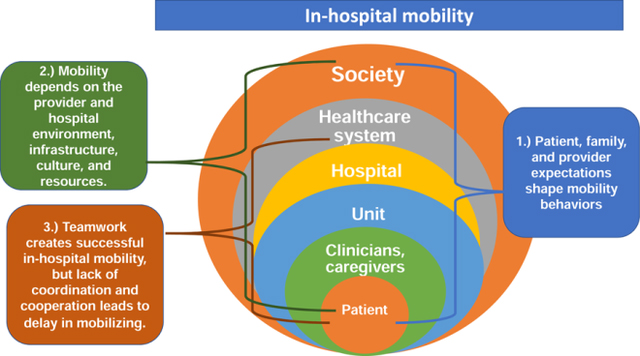
Graphical Abstract:
Introduction
Hospitalization is increasingly common with age: in the United States, seventeen percent of all older adults over 65 will experience a hospitalization over the next year.1 Hospitalized older adults often develop a dramatic loss of physical function2 and are 61 times more likely to develop deficiencies in Activities of Daily Living (ADLs) than their age-matched peers who are not hospitalized.3 Low mobility and high rates of sedentary behavior play a major role in the physical decline that occurs during a hospitalization2 and have been shown to predict development of hospital-associated deconditioning,2,4 rehospitalization5 and death.6
Previous studies demonstrate that older adults are highly sedentary during a hospital stay. A study conducted at an acute care for the elderly unit demonstrated that patients took an average of 740 steps per day,7 well below the 3,500–5,500 steps day considered normal for older adults with disabilities,8 and that on 12.9% of observation days, patients took no steps at all.7 Moreover, studies show that low mobility is closely linked to hospital readmissions5,9 and that lower step count per day predicts a longer length of stay.5 Collectively, these studies suggest that rehabilitation paradigms for hospitalized older adults do not include adequate dosage of mobility and that increasing mobility represents a critical target for reducing disability and preventing adverse events.
The interpersonal and environmental mechanisms behind persistent low mobility during a hospitalization are essential to understand, especially in the context of designing interventions to improve mobility. Qualitative studies have described the context around which many patients are largely sedentary while hospitalized from the perspectives of both clinicians and patients.10–13 These studies identified multiple factors that may impede mobility including difficulty identifying a team member responsible for mobilizing patients,11 patients’ dependence on staff to mobilize,10 lack of time for staff to assist patients,12 having symptoms such as pain, weakness, and fatigue,12 concerns about falling,12,13 and low patient motivation.12 However, these primary qualitative studies are limited in scope with small sample size and low geographic variability. This study seeks to provide a more complete examination of stakeholders’ perspectives on in-hospital mobility by using qualitative metasynthesis as a method to create a framework. This framework can inform interventions that facilitate patients and clinicians playing a larger role in promoting in-hospital mobility.
The socioecological model (SEM) is a theoretical framework that nests personal, interpersonal, community, and organizational levels in order to explain a phenomenon. 14 The SEM can be used to examine the interactions of levels within healthcare systems and their impact on health-related behaviors.15 In-hospital mobility can be influenced by multiple levels: patient-level factors (such as symptoms and health conditions), interpersonal factors (i.e. clinicians and caregivers), institutional factors, and healthcare system factors such as reimbursement structures. These levels interact in a way that can have a profound influence on in-hospital mobility. For example, in 2008, the Center for Medicare & Medicaid Services stopped reimbursing hospitals for costs related to inpatient falls (system level), which have lead hospitals to initiate stringent fall prevention programs (institution-level)16 that encourage staff to keep patients with fall risk in bed to prevent falls (interpersonal level). Therefore, the socioecological model provides valuable context for analyzing the roles of clinicians and patients in promoting (or discouraging) in-hospital mobility. Evaluating how stakeholders see their role in in-hospital mobility enables a modification of the SEM to provide a complete framework for person-environment interactions that play a role in the success or failure of a mobility program.
The purpose of this study was to describe how different key stakeholders (i.e., interprofessional clinical care team and patients) perceive their role in promoting in-hospital mobility by systematically synthesizing qualitative literature. Examining this concept will allow us to revise the SEM to create a framework that better guides interventions that aim to promote in-hospital mobility.
Methods
Study design
Qualitative metasynthesis is a rigorous method used to understand a phenomenon in a specific context from the perspective of multiple investigations and diverse study subjects.17,18 The goal is to fill a gap in the literature related to a clinical need by examining individual primary studies to extrapolate a broader meaning.19 Previous studies have used qualitative metasynthesis to examine the construct of physical activity in the intensive care unit (ICU) setting20 and with other special populations such as dysvascular amputation,21 and stroke.22 This study was conducted using a critical realist approach, examining experiences and phenomenon within participants’ truth and reality while acknowledging that individuals experience the same reality in different ways.18 We used interpretation, conceptual synthesis and reciprocal translation to extrapolate, compare and synthesize themes as reported by Thomas and Harden.23 Qualitative metasynthesis unifies convergent and divergent constructs across primary studies, creating new concepts and analytical themes.24 We followed the Enhancing Transparency in Reporting the Synthesis of Qualitative Research statement to guide the report of our study.25
Systematic Search Strategy
The primary author (JS) conducted a systematic search strategy with PubMed, Ovid Medline, Ovid PsychInfo, and CINAHL. The search terms aimed to discover all relevant qualitative studies examining in-hospital mobility were: (“qualitative” OR “qualitative research”) AND (“inpatient” OR “inpatients” OR “acute care” OR “hospitalized” OR “hospitalization”) AND (“exercise” OR “physical activity” OR “Physical activities” OR exercises OR walking OR ambulation OR mobility OR “Mobility limitation” OR “activities of daily living”). Articles were also hand-searched to find additional relevant studies. Studies were reviewed if they were published between 2002 and the time of search (October 2019). Studies met the following inclusion criteria: 1.) Primary qualitative research study examining perceptions of mobility from the perspectives of patients and/or clinicians and 2.) published in English. Studies were excluded if they focused on the ICU setting and post-acute care/rehabilitation setting as these settings have key differences in a professional environment than general acute care. Studies were also excluded if they focused exclusively on special populations such as stroke or dementia, as these populations have differences related to disease process, physical and cognitive symptoms, and adjustment than older adults in the general inpatient setting. If there was a disagreement about the inclusion or exclusion of a manuscript, it was discussed with the team to reach a consensus.
Critical appraisal
Studies were appraised for quality using the McMaster University Tool,26 which was selected as it comprehensively reviews methodologies and scientific rigor. No studies were excluded based on insufficient quality because there is no consensus on using a critical appraisal to exclude qualitative studies; Journals’ space requirements can exclude details about methodological rigor. Critical appraisal and discrepancies in the evaluation were discussed until team members reached an agreement.
Thematic Synthesis
Thematic analysis was performed in a continuous, iterative process from October 2019 to December 2019. Using an inductive strategy of constant comparison, we extracted primary codes and themes to create and synthesize new analytical themes derived within and across studies.24,27 At least two authors independently extracted themes from each primary study, using both direct quotes from participants and narratives written within studies. Each text segment was considered for meaning and insights related to our research question. All texts were coded line by line within the results and discussion sections of each article, and codes were grouped together to form descriptive themes. This process was repeated for each article and then compared across all articles in comparison to one another. Using the process of reciprocal translation, we constructed an evidentiary matrix that mapped primary study themes to themes derived from interpreting all studies. In an iterative process, the study team interpreted themes to further synthesize and streamline the data, creating primary themes and subthemes.24 The SEM guided our analysis, as we mapped our interpreted themes to patient, clinician/caregiver, unit, hospital, healthcare system, and societal levels.
Scientific rigor
The primary author guided the study, and the study team held regular discussions to agree upon evaluation, interpretations, and synthesis of primary study themes. A team-based analytic toolkit was used including inductive, deductive and abductive reasoning, reflexivity and researcher triangulation.31 The study team maintained a written audit trail to record decisions. The study team consisted of three nurses, two PTs and a hospitalist/geriatrician. A Ph.D.-prepared qualitative researcher (JJ) oversaw methodological aspects of the study.
Results
Study Selection results
The systematic search yielded 483 articles after the removal of duplicates. After the screening process, eleven primary qualitative studies were included in the analysis (Figure 1 and Table 1). Studies were published between 2007 and 2019. A total of 349 individuals participated in these studies: 80 patients, 52 nursing assistants, 168 nurses, 13 physicians, and 36 PTs. No studies interviewed caregivers, occupational therapists (OTs) or hospital administrators. Studies were from a variety of countries including the United States, Sweden, Australia, Denmark, Norway, and Singapore and used various qualitative design approaches: descriptive/interpretative, phenomenology, grounded theory, and ethnography.
Figure 1:
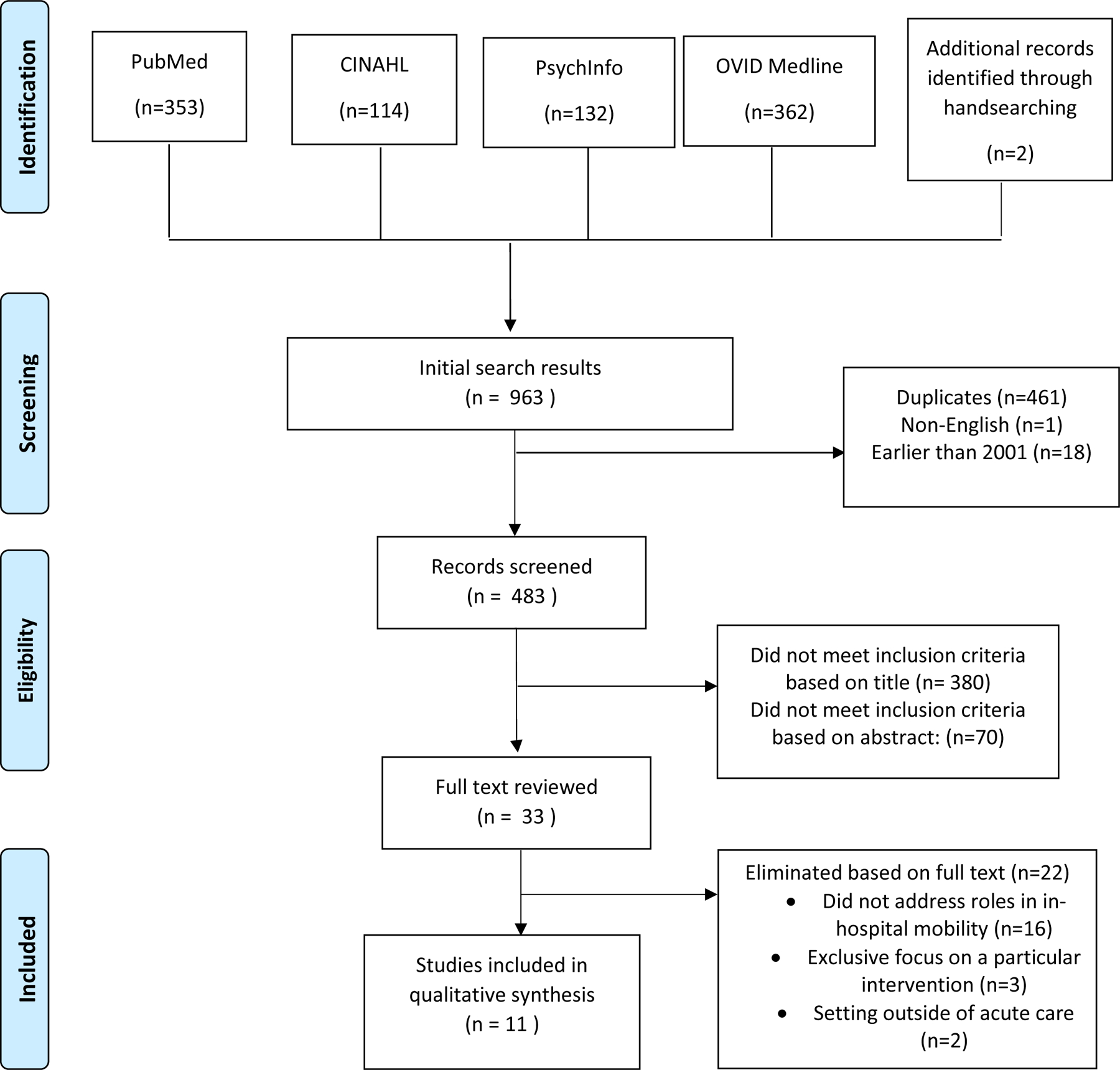
PRISMA Diagram depicting systematic search process for this qualitative systematic review.
Table 1:
Description of studies included in the qualitative metasynthesis.
| Reference number | Authors | Study Purpose | Country | Study Design | Methods | Participants | Summary of Findings |
|---|---|---|---|---|---|---|---|
| 1 | Boltz et al. (2010) | To examine older adults perspectives on physical function during and after a hospital stay | USA | Descriptive | -Focus groups with semi-structured interviews | 24 older adults who had recently experienced a hospitalization | -Participants expected to go home feeling better than when initially hospitalized, but experienced a profound loss of physical function over the course of the hospital stay. -Participants experienced significant barriers to independence, but felt as though strong nursing care facilitated improvement. |
| 2 | Boltz et al. (2011) | To examine organizational factors that influence physical function in hospitalized older adults from the perspectives of nursing staff. | USA | Descriptive | -Focus groups with semi-structured interviews | 55 nurses, nurse supervisors, and personal care assistants from two hospitals | -Nursing staff identified both facilitators and barriers to improving physical function for hospitalized older adults. -Participants identified how older adults are particularly vulnerable to loss of physical function. -Nurses saw promotion of physical function as integral to their professional role. |
| 3 | Brown et al. (2007) | To compare barriers to mobility identified by patients, physicians, and nurses in the hospital setting | USA | Grounded theory | -One on one semi-structured interviews -Content analysis was used to determine perceived barriers to mobility |
10 patients (age 75 or older), 10 nurses, and 9 resident physicians | -All three groups identified barriers such as symptoms (i.e. weakness, pain, fatigue), having an intravenous line or urinary catheter, and concern about falling. -Lack of staff was noted by most nurses and physicians and some patients. -Clinicians identified low patient motivation as a potential barrier, but patients did not. |
| 4 | Chan et al. (2018) | To describe nurses’ perception of facilitators and barriers to older adult’s participation in physical activity during a hospital stay from an Asian context | Singapore | Phenomonology | -Focus group interviews with semi-structured interview guide, reflexivitiy employed throughout the study, theoretical thematic analysis | 30 registered or enrolled nurses from various general wards in a single hospital | -Physical activity was a fundamental aspect of nursing -Facilitators included premorbid functional state, a multidisciplinary approach, family support system -Barriers included adoption of ‘sick role’ behavior, prolonged bed rest, pain and unfamiliar medical devices, fear of falls, safety culture around falls and language differences |
| 5 | Doherty-King & Bowers (2012) | To explore nurses’ expectations around the responsibility for ambulating patients, as well as how this impacts their decision whether to ambulate | USA | Grounded dimensional analysis (grounded theory combined with dimensional analysis) | -Structured focus groups | 25 registered nurses on medical or surgical units from two hospitals | -Some nurses claimed that ambulation of patients was their own responsibility -Nurses who claimed responsibility tended to focus on patient independence and psychosocial well-being, interdisciplinary collaboration, determining appropriateness of activity orders, and adjusting to resource availability -others believed that it was the responsibility of other clinicians |
| 6 | Higgins et al. (2007) | To examine the negative attitudes of nurses towards older adults in their care | Australia | -descriptive qualitative study | -In-depth interviews -Nurses were provided scenarios that demonstrated both positive and negative aspects of care |
-9 nurses participated in this secondary study | -Nurses perceive older adults to be more difficult to work with than other patients -Lack of time for care leads to difficulty caring for this population -Stereotyping older patients was common |
| 7 | Kirk et al. (2019) | To explore how social contextual circumstances impact the mobility of older adults, and how it alters healthcare clinicians decisions whether to mobilize a patient | Denmark | Ethnographic field study | -Study authors followed participants and observed how they talked about mobility, interacted with patients, and how surrounding shaped their actions using an observation guide -Go-along interviews were also conducted |
61 Health professional (PTs, RNs, Nursing assistants) and 18 physicians from six departments in three public hospitals | -Professional roles appeared to be the most important factor for making decisions about mobility. Time pressure contributes to lack of mobility - Environment played a major role in lack of mobility -Encouraging patients was crucial for mobilization -Patients expected nurses to be too busy with other tasks -Mobility improved when connected with ‘transfer value’ (i.e. goals connected to home) |
| 8 | Koenders et al. (2018) | To understand attitudes, beliefs, thoughts and experiences related to physical activity from the perspectives of patients and healthcare clinicians | Norway | Interpretive Phenomono-logical study, | One on one semi-structured interviews, compared patients to health care clinicians | 42 total participants: 18 patients in cardiac care unit, cardiology, orthopedics or traumatology; 24 clinicians (nurses, nursing assistants, PTs, 1 physician assistant and 1 physician) | -Patients/clinicians commonly described physical activity as purposeful activity to achieve a goal -Physical and mental rest is needed to balance physical activity -The hospital environment was not conducive to physical activity -Ability to participate in physical activity was associated with feelings of freedom and autonomy |
| 9 | Masley et al. (2011) | To determine the role of PTs in the acute care setting and describe clinical reasoning processes | USA | Grounded-theory | Semi-structured interviews, used a constant comparative process to determine common themes, which lead to theoretical model | 18 PTs in three academic medical centers | -PTs collect and analyze medical information to determine appropriateness of therapy, apply specialized PT knowledge in mobility, movement dysfunction, and safety in a complex environment -PTs have patients do as much as they can on their own without physical help -PTs communicate with other professions, patients, and families |
| 10 | Ohlsson-Nevo et al. (2019) | To describe how nurses perceive and facilitate physical activity for hospitalized older adults | Sweden | Exploratory/ descriptive | Semi-structured focus group interviews, interaction analysis | 29 nursing staff in three hospitals | -Patients depend on nursing staff for mobility, although nursing staff does not always have time to help -Nurses see physical activity as a fundamental part of their professional role -Understanding patient expectations facilitates physical activity performance -A team approach involving the patient, family, and multiple healthcare professionals facilitates physical activity |
| 11 | So & Pierluissi (2012) | To describe the expectations, facilitators, and barrier around exercise in the hospital | USA | Framework theory/ framework method (familiarization, identifying thematic framework, indexing, charting, mapping and interpretation) | Semi-structured interviews at besides about attitudes/expectations regarding in-hospital exercise | 28 English or Spanish-speaking hospitalized older adults, | -Exercise was equated with walking for most participants -Few participants expected to be exercising -Motivating factors: avoiding negative effects of bed rest, promoting a sense of well-being, being asked to exercise -Barriers included symptoms, institutional barriers, fear of injury |
Critical appraisal
All studies reviewed relevant literature, sampled appropriately, and had a clear research question. Studies varied in quality of trustworthiness and which components (i.e. credibility, transferability, dependability, confirmability)26 were deficient or not reported (Appendix 1).
Analytical themes
Three primary, interrelated themes emerged from this study: (1) Patient, family, and clinician expectations shape roles in in-hospital mobility., (2) Stakeholders’ role in mobility depends on hospital environment, infrastructure, culture and resources., and (3) Teamwork creates successful in-hospital mobility, but lack of coordination and cooperation leads to delay in mobilizing. Table 2 shows these primary themes as well as nineteen subthemes. Primary themes and subthemes were nested within the SEM14 to put our findings into a larger context of hospital culture and to identify potential targets for improvement in mobility culture (Figure 2).
Table 2:
Reciprocal translation table, which depicts synthesis of themes across studies and the primary study themes identified by primary study authors.
| Derived analysis: themes and subthemes | Identified in paper # (Corresponding to Table 1) and page(s) | Primary study themes | Socioecological Model Levels and Interactions |
|---|---|---|---|
| 1. Patient, family, and clinician expectations shape roles in in-hospital mobility. | |||
| Ageism among clinicians lowers expectations around mobility | 2 (pg 218), 3 (pg 310), 6 (pg 231–232), 8 (pg 5), 10 (pg 6) | Walking a tight rope, Marginalization and oppression of older people, lack of patient motivation, stereotypical thinking | Clinician, Patient-Clinician interaction, Clinician-society |
| Clinician uncertainty about prior level of function lowers mobility expectations | 1 (pg 385), 2 (pg 219), 5 (pg 1243) | Constraints to function promotion, Barriers to independence, Attributing responsibility to others | Clinician, clinician-patient interaction, hospital-clinician interaction |
| Management-level expectations drive clinician mobility behaviors | 2 (pg 220), 5 (pg 1244) | Changing actions without changing responsibility | Unit-clinician interaction |
| Many patients take a passive role in their mobility | 1 (pg 383, 386), 2 (pg 218), 3 (pg 308), 6 (pg 231), 8(pg 5), 10 (pg 8), 11 (pg 717), | Barriers to independence, marginalization of older people, better not worse, barriers to exercise | Patient, Clinician-patient interaction, Patient-society |
| Mobility helps patients regain autonomy | 8 (pg 5), 11 (pg 716) | Improved well-being, fundamental feelings | Patient, patient-caregiver/clinician interaction |
| Patient, family, and clinician preconceived notions influence mobility. | 2 (pg 219), 4 (pg 94), 6 (pg 232), 7 (pg 13), 8 (pg 4), 10 (pg 8), 11 (pg 715) | Walking a tight rope, the hospital environment, patient and family-based barriers, meeting the patients’ expectations, stereotyping the older person | Provider-patient and clinician-patient interaction |
| Patients have differential expectations for who provides mobility interventions | 7 (pg 12), 10 (pg 8) | Taking joint responsibility | Patient-clinician interaction |
| The caregiver paradox: optimal care involves promoting mobility, but clinicians may do more for the patient than needed. | 4 (pg 94), 7 (pg 10), 8 (pg 5), 10 (pg 8) | Adoption of ‘sick role’ behaviors, the hospital environment | Clinician, clinician-patient Interaction |
| 2. Stakeholders’ role in mobility depends on hospital environment, infrastructure, culture and resources. | |||
| Among clinicians, competing priorities put mobility low on the task list. | 1 (pg 385), 2 (pg 219), 3 (pg 308), 4 (pg 95), 5 (pg 1243), 6 (pg 232), 8 (pg 4–5), 10 (pg 4–5) | Constraints to function promotion, if only we had time, need for assistance and lack of staff, the hospital environment, attributing responsibility to others, hospital-based barriers, physical activity depends on the external environments | Clinician, unit, hospital, healthcare system; clinician-unit interaction, Unit-hospital interaction, hospital-healthcare system interaction |
| The rhythm of workflow may facilitate mobility, but it is easily disrupted. | 4 (pg 94), 5 (1244), 7 (pg 14), 10 (pg 6) | Integration of physical activity into daily work, adjusting to resource limitations | Clinician-unit interaction, unit-hospital interaction |
| Physical environment of a hospital often hinders realization of professional role surrounding mobility. | 1 (pg 385), 2 (pg 218), 3 (pg 308), 8 (pg 4), 7 (pg 8–9), 10 (pg 6), 11 (pg 716) | Constraints to function promotion, enabling environment, institutional barriers, Medical devices, hospital environment, materialities, physical activity depends on external environment | Clinician-unit interaction, Unit, Hospital |
| Clinicians use motivational strategies to engage patients in mobility. | 1 (pg 384), 2 (pg 219), 4 (pg 94), 5 (pg 1244), 7 (pg 12), 8 (pg 4), 10 (pg 4, pg 7) | Coaching and caring, strong basic nursing care, meaning of inpatient physical activity and rest, professional roles, motivating patients, in the hands of nurses | Clinician, clinician-patient interaction |
| Resilient, experienced clinicians will take charge of mobility-related tasks even in uncertain circumstances | 2 (pg 219), 4 (pg 95), 5 (pg 1242), 7 (pg 11), 10 (pg 4–5), | Constraints to function promotion, nurses claiming responsibility, in the hands of nurses | Clinician-unit interaction, clinician-hospital interaction |
| A culture of fear around falls deters patient mobility | 1 (pg 385), 2 (pg 218, 220), 3 (pg 309), 4 (pg 95), 5 (pg 1243), 11 (pg 717) | Walking a tight rope, barriers to independence, fear of injury, fear of a patient falling, hospital-based barriers, waiting for risk to change | Patient, caregiver, clinician, unit, hospital, patient-clinician interaction, clinician-unit interaction, hospital-healthcare system interaction, society |
| 3. Teamwork creates successful in-hospital mobility, but lack of coordination and cooperation leads to delay in mobilizing. | |||
| A team approach involving patients, families, and clinicians facilitates stakeholder roles surrounding mobility | 4 (pg 63–64), 5 (1243–1244), 8 (pg 6), 10 (pg 7) | Striving for a mutual understanding of patients’ physical activity, healthcare professional-based facilitators, claiming responsibility | Provider and Caregiver-unit interaction |
| Language around mobility differs by stakeholders | 7 (pg 10), 8 (pg 4) | Meaning of inpatient physical activity and rest, professional roles | Patient, Caregiver/clinician |
| PTs and OTs are experts in complex factors around mobility | 4 (pg 94), 7 (9–10), 8 (pg 5), 9 (pg 910), 10 (pg 7), | The hospital environment, application of specialized PT knowledge, engaging a multidisciplinary team approach | Clinician, clinician-unit interaction, clinician-hospital interaction |
| Nurses and patients may wait for PT or physician clearance before mobilizing. | 2 (pg 219), 5 (pg 1243), 7 (pg 10), | Constraints to function promotion, professional roles, attributing responsibility to others | Clinician interaction, clinician-unit interaction, clinician-hospital interaction |
| There is disagreement around who is responsible for mobility tasks. | 2 (pg 219), 5 (1243), 7 (pg 10–11), 9 (pg 910) | Constraints to function promotion, attributing responsibility, professional roles | Clinician, Clinician-unit interaction, clinician-hospital interaction |
Figure 2:
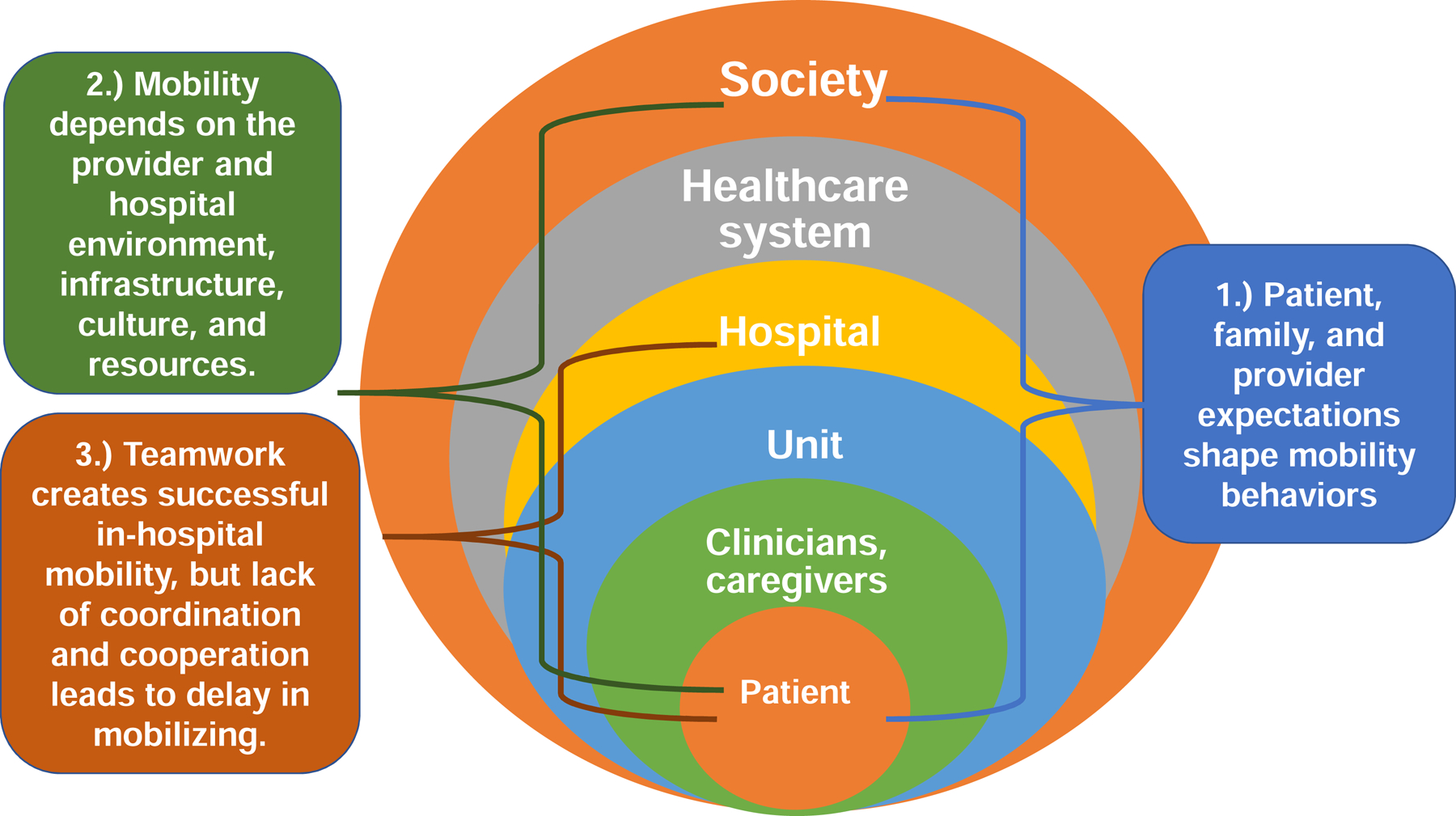
Revision of the SEM to fit in hospital mobility and depiction of three primary themes nested with the healthcare system in the SEM.
1. Patient, family, and clinician expectations shape roles in in-hospital mobility.
Patients often do not expect to be active in the hospital,13 and clinicians generally had low expectations for their older patients. Five studies noted that ageism among clinicians lowers expectations around mobility.10,12,28–30 Many staff expected that their patients who were older were less motivated and willing to move, more stubborn, and less capable. For example: “I don’t know if it is because it is the elderly or because they just seem more stubborn. They are sometimes more content to stay in the bed, and you have to really stress to them to get up.”12 These stereotypes clearly had an impact on clinician behavior. One nurse said “Perhaps you would probably work a little bit harder to get, say, a sixty-year-old up and moving and to become more independent. You wouldn’t necessarily spend as much time on an elderly patient that you know is going back to a nursing home that probably wasn’t walking very well before.”28
Additionally, the theme clinician uncertainty around the prior level of function lowers mobility expectations emerged from interviews with nursing11,29 and patients.31 Staff did not understand how active older patients were before the hospitalization; When patients began to improve medically, the staff still expected them to “take it easy,”31 implying that the patient should limit movement. Nursing staff expressed that if they were not aware of a patients’ mobility level before the hospital stay, they were more fearful of injury to the patient or themselves.11 Conversely, if they received information that the patient was active before the hospitalization, nursing staff were more likely to promote mobility.11
The unit and hospital level of the SEM also played a role in how much clinicians incorporated mobility into patient care as management-level expectations drive clinician mobility behaviors.11,29 Management can elevate the role of the nurse in providing mobility interventions, particularly by auditing documentation for ambulation and activity. Higher management expectations would increase staff compliance with mobility related tasks, even for staff who would normally attribute responsibility for ambulating patients to others.29
Seven of the studies suggested that many patients take a passive role in their mobility.10,12,13,28–31 For example one nurse indicated, “older adults are quieter, more passive.”29 Patients expressed that they wanted to move more throughout the day, but that they didn’t want to bother the nursing staff, who seemed very busy.12,31 Patients were mobile with PT, but PT was only present for a small portion of the day.32 In addition, PTs do not spend their entire session on mobility,32,33 meaning that patients received overall a small dosage of mobility from PTs. This was not the case across all patients: some did take a more proactive role and advocate for themselves to be more mobile.32 Patients also indicated a stressful experience in the hospital and a loss of independence. Importantly, however, mobility helps patients regain autonomy.10,13 For example, “When I was finally able to move again, a sparkle of freedom returned on me. It feels liberated to not be attached to a bed, you know.”10 Mobility had additional benefits for fighting boredom in the hospital.10,13
The theme patient, family, and clinician preconceived notions influence mobility emerged from many of the studies.10,28–30,32,34 Patients who expected to be active (sometimes from previous contact with physical therapy in a prior hospitalization) appeared more likely to take a proactive role in mobility.13,32 Family expectations also played a significant role. Usually, family involvement increased expectations around mobility, and motivated clinicians to deliver mobility interventions.32 However, families sometimes had expectations that the patient should be resting in bed, which could interfere with clinicians’ role in facilitating mobility.10,34 Patients have differential expectations around who provides mobility interventions. Primarily, patients indicated that they would expect to be more active during their PT time,32 while nurses indicated that patients were less willing to move for nurses than for PTs.30,32
Staff could also feel conflicted around their role in mobility. Four studies identified the caregiver paradox: optimal care involves promoting mobility, but clinicians may do more for the patient than needed.10,30,32,34 Clinicians would often perform tasks that patients might be able to do for themselves, which could interfere with mobility. Moreover, clinicians perceived that some patients expected to be served while in the hospital. For instance, “I suppose they find it troublesome to be independent. After all, they have been attended to and served during their whole hospitalization. So when someone suddenly comes and ask them to perform physical activity, they will be like, ‘No, I want to go back to being assisted.’” 34
2. Stakeholders’ role in mobility depends on the clinician and hospital environment, infrastructure, culture, and resources.
The ability of stakeholders to realize their role in mobility is highly context dependent. For example, nine of the eleven studies identified that among clinicians competing priorities put mobility low on the task list.10–12,28–32,34 Nursing staff were generally aware of the importance of mobility but needed to prioritize other tasks. Nurses indicated a lack of time and/or support staff could hinder the realization of their professional role in providing mobility, particularly when units were busy.11,29,30 For example: “If it is really busy on the unit, getting the patient up to walk is the last thing on my mind.”11 PTs also voiced competing priorities such as care plans, patient education, and respiratory exercises.32 Furthermore, the rhythm of workflow may facilitate mobility, but it is easily disrupted.11,30,32,34 Clinicians indicated that planning for physical activity, which included coordinating with other staff members, could help to make sure that the patient received mobility. Having patients perform tasks for themselves helps to save time with more mobile patients.34 However, disruptions to workflow such as testing and call bells would often interfere with providing mobility.10,32
The physical environment of a hospital often hinders realization of professional role surrounding mobility.10,12,13,29–32 Medical care tends to be centered around the bed of the patient,10 patient rooms and hallways were often cluttered and difficult to navigate,32 and patients infrequently used common spaces.32 While hallways were often identified as a potential space for mobility, an ethnographic study observed very infrequent use of the hallways for mobility activities.32 Staff transport patients in wheelchairs or gurneys throughout the hospital when needed for testing, leading to less opportunity for mobility.29 These environmental factors, coupled with competing priorities, created an environment where patients and clinicians faced considerable difficulty in realizing their ideal role in promoting mobility.
The interpersonal clinician environment also played a major role in in-hospital mobility. Clinicians use motivational strategies to engage patients in mobility, such as connecting physical activity to functional goals to ensure that the activity has transfer value,10,29,30 rewards,32 engaging family members,29 and praise.10 Motivational strategies facilitated clinicians’ ability to fulfill their role in in-hospital mobility. In addition, the theme resilient, experienced clinicians will take charge of mobility-related tasks even in uncertain circumstances11,29,30,32,34 became evident in nursing interviews. Some nursing staff frequently waited for PT or physician clearance before getting a patient up and moving; however, others would challenge orders that they thought were inappropriate or took the initiative to get patients up if PT was busy. For example, “PT didn’t come to see them, so I just got them up and walked them. Some nurses were appalled that they weren’t evaluated by PT first.”
A culture of fear around falls deters patient mobility was present in six of the studies.11–13,29,31,34 Some patients reported that they were told not to get out of bed for fear of a fall, and some were afraid to get out of bed themselves. For example, “As old as I am, your legs don’t last long, and they give away. It would be dangerous because I haven’t got the strength. Now, since I’ve fallen, yes, I have to be careful.”12 Many staff indicated that hospitals had a culture of safety when it came to falling, which made them hesitate to get patients out of bed.10–12,32 Staff made patients well-aware of their risk of falls, which even drove some patients to choose to wear adult briefs or use a bedside commode although they could ambulate.34
3. Teamwork creates successful in-hospital mobility, but lack of coordination and cooperation leads to delay in mobilizing.
One important theme suggested by many clinicians was a team approach involving patients, families, and their clinicians facilitates stakeholder roles surrounding mobility.10,11,30,34 Communication and collaboration among PTs, nurses, and physicians34 was thought to facilitate an environment of mobility. Reinforcing the importance of mobility from multiple clinicians,30 timing PT sessions to assist with nursing workflow,11 communicating about functional status, and giving patients adequate time to rest10 all facilitated stakeholders’ role in mobility. However, teamwork was often difficult to execute; as hospitals became busier, coordinating different schedules becomes a significant barrier, and a mobility plan might become lost over the course of a shift change.28,29 Moreover, patients identified that clinicians such as doctors and nurses did not emphasize the importance of physical activity during their stay. For example: “I didn’t realize this until now, but there should be more attention paid by nurses to help people walk and take care of themselves. The doctors don’t focus on this. The physical therapist is only with you a short time. The nurses are with the patient and can see how the patient is progressing. I did have a nurse who would say, ‘I’ll help you walk to the bathroom. You won’t use a urinal at home.’ It was an inconvenience but he (the nurse) was doing the right thing.”31
Language around mobility differed by stakeholders:10,32
PTs talked primarily about exercises, nurses and physicians talked about mobilization, transfers, and being physically active, and patients talked about rehabilitation, therapy, and recovery.10,32 Language also mattered in determining responsibility: PTs were generally responsible for exercise, while nurses might be responsible for mobility.32 However, distinctions between exercise and mobility were unclear.
Professional roles and work patterns highly influence the timing and implementation of mobility tasks. Five of the studies commented on how PTs and OTs are experts in complex factors around mobility. This expertise was highly ingrained in the professional identity of PTs. Some nurses often deferred to PT or OT for mobility tasks, because they were not comfortable completing mobility tasks for patients with complex needs such as assistive device prescription or a high degree of physical dependency.30,32 For instance, “PT comes and assesses them… we hear from them whether it is safe.”11 PTs would also help with training nursing staff on safe patient handling techniques to reduce risk of injury to both patients and staff members. However, nurses and patients may wait for PT or physician clearance before mobilizing.11,29,32 Nursing staff did not universally express a tendency to wait, but waiting appeared to be more common for nurses with limited professional experience.11 PTs often could not quickly assess a particular patient, creating even more time for physical deconditioning to occur.11,28 In an environment of waiting, some staff did not ambulate patients until just before discharge, which could be quite problematic. For example: “The elderly often have pain and are slower moving to begin with. They come to the hospital, stay in bed, and when it’s time to go home, guess what? We find out they can’t walk anymore.”29
While coordination and communication could help facilitate mobility, there is often disagreement over who is responsible for mobility tasks.11,29,32,33 Some nurses saw physical activity or exercise as rehabilitation tasks and, therefore not in their scope of responsibility. The ethnographic study demonstrated that nurses’ primary mobilization task was transfers from the bed to the chair, often in pursuit of a secondary task.32 Other nurses saw mobility as central to their professional identity, although they still face significant barriers to fulfilling this role.30 Many PTs took ownership of the complexities surrounding mobility assessment,10,33 however generally did not spend enough time with patients to execute a mobility program with substantial volume. Other PTs did not see mobility as a core task. For example: “Exercise is part of the treatment. The nurses’ or the physicians’ can send a request for exercise, but when we receive a requisition for mobilization; we call the department and tell them, that mobilization is not one of our tasks.”32 In contrast, a PT in a different study said: “We’re the experts in mobility and safety from a mobility standpoint. So, we’re consulted in order to give our opinion on a patient’s ability to move and function.”33
Discussion
To our knowledge, this is the first study to systematically review the qualitative literature regarding patient and clinician perception of their roles related to in-hospital mobility. Given the importance of mobility in preventing costly adverse events including reshopitalization,5 loss of independence,35 and death,6 there is a concerted effort in the rehabilitation community to improve mobility in the hospital. While all stakeholders saw themselves as having a significant role in mobility, their ability to carry out their professional role was highly dependent on the hospital’s physical and cultural environment, as well as their own expectations and preconceived notions. Three primary analytic themes emerged from this study: 1) Patient, family, and clinician expectations shape roles in in-hospital mobility; 2) Stakeholders’ role in mobility depends on hospital environment, infrastructure, culture and resources; and 3) teamwork creates successful in-hospital mobility, but lack of coordination and cooperation leads to delay in mobilization.
We used our synthesis of stakeholder perspectives (Table 2) to revise the SEM framework (Figure 2) to provide a comprehensive examination of the factors surrounding providers’ roles in in-hospital mobility. All primary analytic themes spanned multiple levels of the SEM, indicating that interventions may need to target higher levels of the model to have sustainable impact. Different levels of the SEM are more amenable to change than others: it is far more difficult to challenge a societal norm around ageism than it is to change a clinicians’ perspective. However, many themes spanned the unit and hospital, indicating that intervening on these levels could still have a major impact on improving in-hospital mobility. Showing the effectiveness and importance of mobility with those interventions can demonstrate to policymakers that reform is needed to improve in-hospital mobility and consequently, patient outcomes. Using the results of our metasynthesis and the SEM as a guide, we recommend strategies for improving mobility in the hospital (Table 3).
Table 3:
Recommendations for initiatives to support stakeholder role in in-hospital mobility based on results of qualitative metasynthesis.
| Recommendation | Metasynthesis supporting results | Target socioecological model level |
|---|---|---|
| Improve clarity about responsibility for mobility-related tasks | There is often uncertainty over who has responsibility for mobility tasks | Clinician, unit, hospital |
| Environmental changes: reconstruct patient rooms to encourage out of bed activities | The physical environment can hinder stakeholders from fulfilling their roles in in-hospital mobility. | Hospital |
| Balance fall risk with benefits of mobility, and consider measuring physical activity and physical function as quality metrics for hospitals. | Fear of falling hinders mobility | Hospital, healthcare system |
| Routinely assess prior level of function | Uncertainty surrounding prior level of function can hinder mobility. | Hospital, healthcare system |
| Challenge stereotypes around aging | Ageism lowers expectations surrounding mobility | Hospital, unit, clinician |
| Staff support and training, integration of mobility into existing tasks and workflow | While some clinicians can facilitate mobility in uncertain circumstances, many have trouble including mobility into workflow, which can be easily interrupted | Clinician, unit, hospital |
| Increase expectations for mobility in the hospital | Patients often to do not expect to be mobile in the hospital, while clinicians often have low expectations for their older patients. | Patient, clinician, caregiver, hospital |
Many staff members and some patients perceived that hospitalized, older patients took a passive role in their mobility. This finding is consistent with previous research suggesting hospitalized older adults often feel as though the hospital is a powerful institution, and that they do not expect to be involved in medical decisions.36 Hospitalized older adults report feeling overwhelmed, confused, and experiencing a loss of sense of control.37 Moreover, the hospital environment tends to center around the bed, which promotes more time in bed, and is inactivating for the patient.10 Mobility interventions in the hospital may want to consider reconstructing patient rooms so that daily activities are not centered around patient beds, which will require concerted effort on the hospital level. Passive behaviors in the hospital may not stem from lack of intrinsic motivation, but rather might be a result of clinician and hospital level expectations around safety that encourage patients to be passive.
However, patients may have higher expectations surrounding care than clinicians perceive. Clinicians noted that older adults do not expect much from their clinicians,29 but patients expressed high expectations for quality care, which were not always met.31 No clinicians mentioned teaching patients to advocate for themselves, a key component of patient-centered care and shared decision-making.38 However, studies also indicated that mobility helps patients to regain a sense of autonomy and independence.10 Therefore, interventions designed to improve mobility should elevate expectations around patient engagement in their mobility, which may have greater uptake if the recommendation comes from hospital policies.
Importantly, stereotypical thinking about age and mobility pervaded in many studies, at both the patient and clinician level. Stakeholders saw older adults as inherently inactive, needing more rest, and less motivated. Misperceptions around aging have important implications at the patient, clinician, organizational, and system levels. The World Health Organization has recognized stereotypes about aging as a major barrier to healthy and active aging39 and positive self-perceptions of aging have been associated with a 7.5 year longer life-span.40 In the hospital environment, stereotypes about aging may cause clinicians to expect less of their patients, and for patients to expect less of themselves.
System-level implications
Several of these findings relate to system level problems that can detract from optimal patient care. Competing priorities were obvious to both patients and clinicians and came from the hospital and healthcare system level. Particularly when units were busy, staff were unable to assist patients out of bed, and patients were afraid to ask for help since they did not want to bother nursing staff. Stress levels were high, and staff commented that standards of care could slip in those situations. High nursing staff to patient ratios are associated with a shorter length of stay, less clinician burnout, fewer pressure ulcers, and lower mortality.41 Healthcare-system policies that incentivize higher nurse to patient ratios or hospital-level policies that optimize staff to patient ratios would likely improve mobility and overall quality of patient care.
Both clinicians and patients felt system-level expectations around fall prevention contributed to fear of movement. A culture of safety was particularly present from clinicians’ perspectives, which is not surprising given previous research demonstrating clinician stress associated with inpatient falls,42 and the punitive culture often surrounding a fall event on a healthcare system-level.43 This study demonstrated that patients were often prescribed immobility to prevent falls, despite previous research indicating that interventions designed to reduce independent mobility such as bed alarms44 and low-low beds45 do not decrease the risk of falls, and interventions designed to improve mobility can actually prevent falls.46 Falls are easy to measure while physical activity and physical function are not as intuitive. However, measuring physical activity and physical function as determinants of hospital outcomes on a healthcare system level may lead to improvements in mobility.
In-hospital mobility suffers from a knowledge-translation gap
Most of the clinicians in these studies recognized the benefits of in-hospital mobility and saw themselves as playing a role in facilitating mobility. However, the ability to mobilize patients depended on unit, hospital, and healthcare system factors that limited time clinicians may have to help mobilize their patients. Mobility interventions should consider adequate staff support and training as well as integration of mobility into existing tasks as essential components to overcome the barriers to mobility.
It appeared from both patients and clinicians that uncertainty surrounding prior level of function would lower expectations around mobility, and that when patients’ medical condition improved, mobility would lag. Systematically assessing the patient’s prior level of physical function could help clinicians understand achievable goals for mobility during a hospital stay. One study noted that nurses who did not see mobility as a core task would be more likely to complete mobility tasks if management had high expectations for mobility.11 This finding indicates that interventions that stem from a higher level on the SEM may overcome major interpersonal barriers to improving mobility.
Limitations
While we attempted to be inclusive of different stakeholders’ perspectives, none of the studies interviewed hospital administrators, who could provide a valuable perspective on hospital and healthcare-system related factors that may alter professional roles surrounding mobility. In addition, the studies came from a variety of geographic settings with different healthcare cultures, which might limit the ability of some studies to relate to each other. However, the diversity of perspectives provided by this approach enriches the data set, and the qualitative metasynthesis methodology allowed for us to include a large sample size.
Conclusion
In summary, the results of this qualitative metasynthesis on stakeholder perspectives surrounding in-hospital mobility informed a revision of the SEM framework, which led to recommendations to improve in-hospital mobility that represent important avenues for future research. While many previous studies on in-hospital mobility have focused on lower levels of the SEM (i.e. patient and clinician), our study indicates that in-hospital mobility is a complex phenomenon influenced by multiple levels of the healthcare system that might be better addressed with a systems approach. Our interpretation of stakeholder perspectives suggest that interventions designed to improve mobility should consider challenging low expectations for in-hospital mobility, account for the fluid nature of professional roles, create infrastructure for successful teamwork, and address the organizational, cultural, and physical environment. The complexities of the acute-care hospital system could be considered analogous to the post-acute care system, and future qualitative studies should examine factors surrounding mobility in settings such as skilled nursing facilities, home health, and inpatient rehabilitation facilities.
Acknowledgement of presentation:
This work has not been presented.
Acknowledgement of financial support:
This work was supported by the Foundation for Physical Therapy PODS I Award and NIH T32 AG000279
Abbreviations:
- OT
occupational therapist
- PT
physical therapist
- ICU
intensive care unit
- SEM
socioecological model
Appendix 1: Results of critical appraisal analysis for included studies using the McMaster tool.30
| Rigor criteria30 | Credibility: Are the descriptions and interpretations of participants’ experiences recognizable? | Transferability: Can the findings be transferred to other situations? | Dependability: Is there consistency between the data and the findings? | Confirmability: Have strategies been used to limit biases in the research? |
|---|---|---|---|---|
| Boltz et al. 2010 | Yes | No | Yes | Yes |
| Boltz et al. 2011 | Yes | Yes | Yes | Yes |
| Brown et al. (2007) | No | No | No | No |
| Chan et al. (2018) | Yes | Yes | Yes | Yes |
| Doherty-King & Bowers (2012) | No | Yes | No | No |
| Higgins et al. (2007) | No | Yes | No | No |
| Kirk et al. (2019) | Yes | Yes | Yes | Yes |
| Koenders et al. (2018) | Yes | Yes | Yes | Yes |
| Masley et al. (2011) | Yes | Yes | Yes | Yes |
| Ohlsson-Nevo et al. (2019) | Yes | Yes | Yes | Yes |
| So & Pierluissi (2012) | Yes | Yes | Yes | Yes |
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
There are no conflicts of interest reported by any authors.
References
- 1.Lucas JWBV. Tables of Summary Health Statistics for the U.S. Population: 2018 National Health Interview Survey. National Center for Health Statistics Available from: https://www.cdc.gov/nchs/nhis/SHS/tableshtm. 2019.
- 2.Kortebein P Rehabilitation for hospital-associated deconditioning. Am J Phys Med Rehabil 2009;88(1):66–77. [DOI] [PubMed] [Google Scholar]
- 3.Gill TM, Allore HG, Holford TR, Guo Z. Hospitalization, restricted activity, and the development of disability among older persons. Jama 2004;292(17):2115–2124. [DOI] [PubMed] [Google Scholar]
- 4.Pavon JM, Sloane RJ, Pieper CF, et al. Accelerometer-Measured Hospital Physical Activity and Hospital-Acquired Disability in Older Adults. Journal of the American Geriatrics Society. 2020;68(2):261–265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fisher SR, Kuo Y-F, Sharma G, et al. Mobility after hospital discharge as a marker for 30-day readmission. Journals of Gerontology Series A: Biomedical Sciences and Medical Sciences. 2016;68(7):805–810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ostir GV, Berges IM, Kuo YF, Goodwin JS, Fisher SR, Guralnik JM. Mobility activity and its value as a prognostic indicator of survival in hospitalized older adults. Journal of the American Geriatrics Society. 2013;61(4):551–557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fisher SR, Goodwin JS, Protas EJ, et al. Ambulatory activity of older adults hospitalized with acute medical illness. Journal of the American Geriatrics Society. 2011;59(1):91–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tudor-Locke C, Craig CL, Aoyagi Y, et al. How many steps/day are enough? For older adults and special populations. International Journal of Behavioral Nutrition and Physical Activity. 2011;8(1):80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chawla H, Bulathsinghala C, Tejada JP, Wakefield D, ZuWallack R. Physical activity as a predictor of thirty-day hospital readmission after a discharge for a clinical exacerbation of chronic obstructive pulmonary disease. Annals of the American Thoracic Society. 2014;11(8):1203–1209. [DOI] [PubMed] [Google Scholar]
- 10.Koenders N, van Oorsouw R, Seeger JP, Nijhuis–van der Sanden MW, van de Glind I, Hoogeboom TJ. “I’m not going to walk, just for the sake of walking…”: a qualitative, phenomenological study on physical activity during hospital stay. Disability and rehabilitation. 2018:1–8. [DOI] [PubMed] [Google Scholar]
- 11.Doherty-King B, Bowers BJ. Attributing the responsibility for ambulating patients: a qualitative study. International journal of nursing studies. 2013;50(9):1240–1246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Brown CJ, Williams BR, Woodby LL, Davis LL, Allman RM. Barriers to mobility during hospitalization from the perspectives of older patients and their nurses and physicians. Journal of Hospital Medicine: An Official Publication of the Society of Hospital Medicine. 2007;2(5):305–313. [DOI] [PubMed] [Google Scholar]
- 13.So C, Pierluissi E. Attitudes and expectations regarding exercise in the hospital of hospitalized older adults: a qualitative study. Journal of the American Geriatrics Society. 2012;60(4):713–718. [DOI] [PubMed] [Google Scholar]
- 14.Bronfenbrenner U Ecological systems theory. Jessica Kingsley Publishers; 1992. [Google Scholar]
- 15.Richard L, Gauvin L, Raine K. Ecological models revisited: their uses and evolution in health promotion over two decades. Annual review of public health. 2011;32:307–326. [DOI] [PubMed] [Google Scholar]
- 16.Fehlberg EA, Lucero RJ, Weaver MT, et al. Impact of the CMS no-pay policy on hospital-acquired fall prevention related practice patterns. Innovation in aging. 2017;1(3):igx036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Walsh D, Downe S. Meta-synthesis method for qualitative research: a literature review. Journal of advanced nursing. 2005;50(2):204–211. [DOI] [PubMed] [Google Scholar]
- 18.Smith B, Sparkes AC. Routledge handbook of qualitative research in sport and exercise. Taylor & Francis; 2016. [Google Scholar]
- 19.McCormick J, Rodney P, Varcoe C. Reinterpretations across studies: An approach to meta-analysis. Qualitative health research. 2003;13(7):933–944. [DOI] [PubMed] [Google Scholar]
- 20.Parry SM, Knight LD, Connolly B, et al. Factors influencing physical activity and rehabilitation in survivors of critical illness: a systematic review of quantitative and qualitative studies. Intensive care medicine. 2017;43(4):531–542. [DOI] [PubMed] [Google Scholar]
- 21.Miller MJ, Jones J, Anderson CB, Christiansen CL. Factors influencing participation in physical activity after dysvascular amputation: a qualitative meta-synthesis. Disability and rehabilitation. 2018:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Luker J, Lynch E, Bernhardsson S, Bennett L, Bernhardt J. Stroke survivors’ experiences of physical rehabilitation: a systematic review of qualitative studies. Archives of physical medicine and rehabilitation. 2015;96(9):1698–1708. e1610. [DOI] [PubMed] [Google Scholar]
- 23.Thomas J, Harden A. Methods for the thematic synthesis of qualitative research in systematic reviews. BMC medical research methodology. 2008;8(1):45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Noblit GW, Hare RD. Meta-ethnography: Synthesizing qualitative studies. Vol 11: sage; 1988. [Google Scholar]
- 25.Tong A, Flemming K, McInnes E, Oliver S, Craig J. Enhancing transparency in reporting the synthesis of qualitative research: ENTREQ. BMC medical research methodology. 2012;12(1):181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Letts L, Wilkins S, Law M, Stewart D, Bosch J, Westmorland M. Guidelines for critical review form: Qualitative studies (Version 2.0). McMaster University Occupational Therapy Evidence-Based Practice Research Group. 2007.
- 27.Barnett-Page E, Thomas J. Methods for the synthesis of qualitative research: a critical review. BMC medical research methodology. 2009;9(1):59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Higgins I, Der Riet PV, Slater L, Peek C. The negative attitudes of nurses towards older patients in the acute hospital setting: A qualitative descriptive study. Contemporary Nurse. 2007;26(2):225–237. [DOI] [PubMed] [Google Scholar]
- 29.Boltz M, Capezuti E, Shabbat N. Nursing staff perceptions of physical function in hospitalized older adults. Applied Nursing Research. 2011;24(4):215–222. [DOI] [PubMed] [Google Scholar]
- 30.Ohlsson-Nevo E, Andersson G, Strid EN. In the hands of nurses: A focus group study of how nurses perceive and promote inpatients’ needs for physical activity. Nursing Open. 2019. [DOI] [PMC free article] [PubMed]
- 31.Boltz M, Capezuti E, Shabbat N, Hall K. Going home better not worse: older adults’ views on physical function during hospitalization. International journal of nursing practice. 2010;16(4):381–388. [DOI] [PubMed] [Google Scholar]
- 32.Kirk JW, Bodilsen AC, Sivertsen DM, Husted RS, Nilsen P, Tjornhoj-Thomsen T. Disentangling the complexity of mobility of older medical patients in routine practice: An ethnographic study in Denmark. PLoS One. 2019;14(4):e0214271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Masley PM, Havrilko CL, Mahnensmith MR, Aubert M, Jette DU. Physical therapist practice in the acute care setting: a qualitative study. Phys Ther 2011;91(6):906–919. [DOI] [PubMed] [Google Scholar]
- 34.Chan DE, Hong MLI, Tan MYG, Chua WL. Older patients’ participation in physical activity during hospitalization: A qualitative study of ward nurses’ perceptions in an Asian context. Geriatric nursing (New York, NY). 2019;40(1):91–98. [DOI] [PubMed] [Google Scholar]
- 35.Covinsky KE, Palmer RM, Fortinsky RH, et al. Loss of independence in activities of daily living in older adults hospitalized with medical illnesses: increased vulnerability with age. Journal of the American Geriatrics Society. 2003;51(4):451–458. [DOI] [PubMed] [Google Scholar]
- 36.Ekdahl AW, Andersson L, Friedrichsen M. “They do what they think is the best for me.” Frail elderly patients’ preferences for participation in their care during hospitalization. Patient education and counseling. 2010;80(2):233–240. [DOI] [PubMed] [Google Scholar]
- 37.Bridges J, Flatley M, Meyer J. Older people’s and relatives’ experiences in acute care settings: Systematic review and synthesis of qualitative studies. International journal of nursing studies. 2010;47(1):89–107. [DOI] [PubMed] [Google Scholar]
- 38.Adams JR, Drake RE. Shared decision-making and evidence-based practice. Community mental health journal. 2006;42(1):87–105. [DOI] [PubMed] [Google Scholar]
- 39.Organization WH. World report on ageing and health. World Health Organization; 2015. [Google Scholar]
- 40.Levy BR, Slade MD, Kunkel SR, Kasl SV. Longevity increased by positive self-perceptions of aging. Journal of personality and social psychology. 2002;83(2):261–270. [DOI] [PubMed] [Google Scholar]
- 41.Lang TA, Hodge M, Olson V, Romano PS, Kravitz RL. Nurse–patient ratios: a systematic review on the effects of nurse staffing on patient, nurse employee, and hospital outcomes. JONA: The Journal of Nursing Administration. 2004;34(7):326–337. [DOI] [PubMed] [Google Scholar]
- 42.Rush KL, Robey-Williams C, Patton LM, Chamberlain D, Bendyk H, Sparks T. Patient falls: acute care nurses’ experiences. Journal of clinical nursing. 2009;18(3):357–365. [DOI] [PubMed] [Google Scholar]
- 43.Cozart H-CT, Cesario SK. Falls aren’t us: state of the science. Critical care nursing quarterly. 2009;32(2):116–127. [DOI] [PubMed] [Google Scholar]
- 44.Shorr RI, Chandler AM, Mion LC, et al. Effects of an intervention to increase bed alarm use to prevent falls in hospitalized patients: a cluster randomized trial. Annals of internal medicine. 2012;157(10):692–699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Haines TP, Bell RA, Varghese PN. Pragmatic, cluster randomized trial of a policy to introduce low-low beds to hospital wards for the prevention of falls and fall injuries. Journal of the American Geriatrics Society. 2010;58(3):435–441. [DOI] [PubMed] [Google Scholar]
- 46.Brown CJ, Foley KT, Lowman JD, et al. Comparison of posthospitalization function and community mobility in hospital mobility program and usual care patients: a randomized clinical trial. JAMA internal medicine. 2016;176(7):921–927. [DOI] [PubMed] [Google Scholar]


