Abstract
Introduction
COVID-19 has led to intricate global challenges, among these, the impact on emergency and elective orthopedic services. Patients with COVID-19 often complain of musculoskeletal symptoms. The subsequent orthopedic consultations require careful assessment of possible inpatient trauma and to rule out any injuries that require active management.
Methods
A retrospective cross-sectional analysis involving 13,580 admitted patients in a national quarantine center between March 2020 and April 2021. All patients with orthopedic consultations were included in the study, and were assessed by orthopedic surgeons in person. Patients were further evaluated for age, sex, presence of trauma, cause for consultation, diagnosis and management.
Results
Seventy-five orthopedic consultations were included, 44% females and 56% males. Of the 75 consultations, 29 (38%) were related to a history of inpatient trauma. Of the 29 cases, 11 sustained fractures of the distal radius, proximal humerus, femoral neck, clavicle and ankle. Four of which were treated operatively.
Discussion and conclusion
Inpatient orthopedic consultations must be assessed carefully to avoid misdiagnoses. Elderly or frail patients are more likely to both; sustain trauma and fractures. Potential limitations of tele-orthopedics may be apparent here, especially in the presence of technological incompetence and high likelihood of fractures.
Keywords: Orthopedic consultation, Telemedicine, COVID-19, Trauma, Fractures
Highlights
-
•
COVID-19 has presented various challenges to orthopedic practice.
-
•
The advent of telemedicine may soon be increasingly utilized in the orthopaedic field.
-
•
Potential implications of tele-orthopaedics must be addressed in order to avoid missed diagnoses.
1. Introduction
While COVID-19 is a predominantly respiratory illness, it has led to intricate global challenges in healthcare. Among these, the impact on emergency and elective orthopedic services across the world [1]. The subsequent delays in elective practice often delays procedures or further, have surgeries deferred indefinitely. While this impact has materialized in various orthopedic services worldwide, there has been scarce data of the impact on inpatient orthopedic services.
Patients with COVID-19 often complain of musculoskeletal symptoms, most commonly myalgia and arthralgia [2]. Frequent and variable complaints among inpatients, has led to the use of telemedicine as a solution in effort to avoid unnecessary repeated exposure to COVID-19 patients [3]. Yet there are unlikely events in which symptomatic inpatients require orthopedic consultations.
In this study, we describe the prevalence and outcomes of orthopedic consultations in symptomatic patients admitted to a national quarantine center that is equipped with orthopedic services. Further, we highlight the potential concerns with telemedicine and missed diagnoses. To our knowledge, no previous studies similarly assessed the outcomes and clinical significance of traumatic orthopedic consultations among symptomatic COVID-19 inpatients. This article has been submitted in line with the STROCCSS statement [10]. This study has been registered with the Research Registry with a (UID: 7392).
2. Methods
A total of 13,580 admitted patients were retrospectively identified from a national quarantine center between March 2020 and April 2021. Admission criteria included; positive COVID-19 PCR, moderate to severe symptoms, positive chest radiological findings. We included a total of 75 official orthopedic consultations. All orthopedic consultations were included in the study, no patients were excluded from the list of consultations. This was done to accurately assess the prevalence of consultations requiring active management. Ethical approval was obtained from our local ethical committee. Where possible, written consent was obtained from patients and/or their family.
Patients were evaluated according to age, gender, presence of trauma, cause for consultation, diagnosis and management. All patients were assessed and examined by experienced orthopedic surgeons following consultations. Further, patients were followed up for their entire length of stay in hospital. Data was entered into a secure study-specific database. Using Minitab 19 (Minitab LLC, PA USA), descriptive analyses including frequencies and percentages were calculated, along with means and standard deviations.
3. Results
Demographic data is shown in (Table 1.), from seventy-five consultations, 44% were male and 56% female. Trauma was the primary reason for consultation in 38% of our patients. The mean age of the patients was 60.7 (range of 19–66).
Table 1.
Describes the demographic data in our population.
| Variable |
Characteristics |
Frequency |
Percentage |
|---|---|---|---|
| (N = 75) | |||
| Age | Mean | ||
| 60.7 (±2.14) | |||
| (Range 19–66) | |||
| Sex | Male | 33 | 44% |
| Female | 42 | 56% | |
| Consultations for trauma | Yes | 29 | 38% |
| No | 46 | 62% | |
| Fractures | – | 11 | |
| Fractures treated operatively | – | 4 |
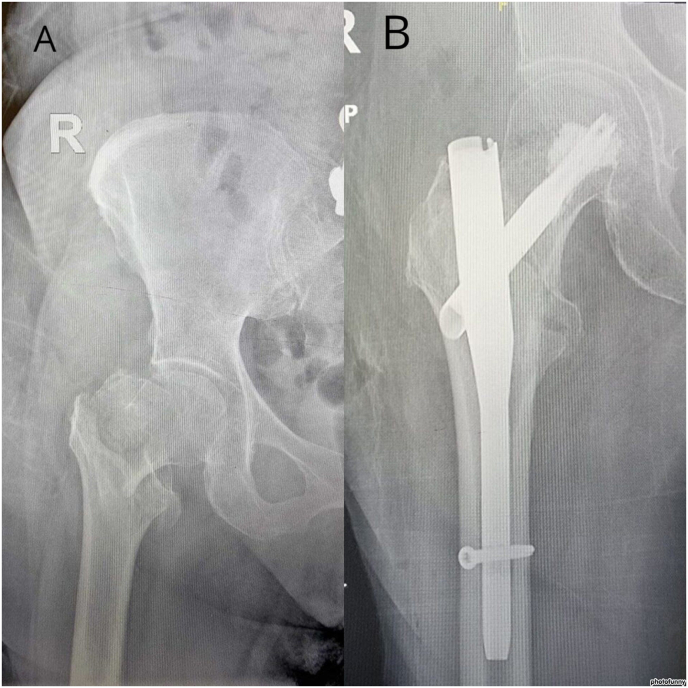
Out of the 29 patients that sustained trauma, eleven patients sustained fractures. These fractures were; ankle (n = 4), proximal humerus (n = 2), proximal femur (n = 4) and clavicle fractures (n = 1). Four of which were treated operatively and all of which were due to fall from standing height. Proximal femoral fractures included; 3 intertrochanteric fractures and 1 femoral neck. All fractures were treated by cement-augmented cephalo-medullary nail (Fig. 2.). We did not experience any cut-out or implant associated complications. One patient died 10-days after fixation of an intertrochanteric fracture; sepsis and widespread gangrene. Another patient died of multi-organ failure after amputation of acute limb ischemia.
Fig. 2.
Pre and postoperative radiographs of a right intertrochanteric femoral fracture. A; Preoperative, B; postoperative fixation with cement-augmented short cephalomedullary device.
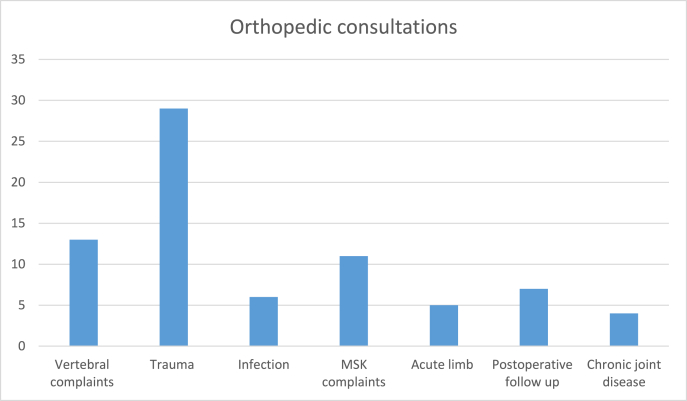
The reasons for orthopedic consultation are displayed in (Fig. 1). Trauma was the most common single cause of consultations in our cohort (38%). The rest of the complaints were mainly non-specific; vertebral complaints, myalgia and arthralgia and pain pertaining to chronic joint disease; osteoarthritis or chronic tendinitis. Other causes for consultation included suspected infection, these were made to rule out possible; septic arthritis, osteomyelitis and localized extremity abscess. Acute limb describes possible acute limb ischemia or compartment syndrome, however, none of which were subsequently diagnosed with acute limb.
Fig. 1.
Displays the various reasons for orthopedic consultations among inpatients. MSK; musculoskeletal.
4. Discussion
Our study aimed to assess the various causes for consultation among inpatients with COVID-19. The comparison may provide insight into the feasibility of telemedicine around specific complaints. In our cohort, consultations that stemmed from trauma were more likely to yield specific findings requiring active management. Inpatients that are unwell are likely more susceptible to injury and falls if precautions are not taken to avoid these in the first place.
There are other diagnoses that must be approached with a high index of suspicion; acute limb ischemia, compartment syndrome and possible infective processes. The patients who sustained proximal femoral fractures were treated with cement-augmented short cephalomedullary devices. These procedures are usually performed quickly, associated with minimal soft tissue disruption and are stable. Of course, patients who underwent surgery required daily in-person postoperative assessments in order to ensure no complications arose.
While our results provide insight into inpatient orthopedic consultations, the study included a relatively small sample size. In addition, the retrospective nature of the study did not allow for an accurate assessment of the temporal association between COVID-19 severity and the cause for consultation. For instance, there was difficulty in attempting to gauge the underlying cause of falls in our cohort. There is a question of whether the large scale application of tele-orthopedics among relatively unwell inpatients is feasible when considering the grim risk of complications if patients are misdiagnosed.
5. Inpatient consultations
The principal concern of orthopedic surgeons attending to consultations electronically is by the potential risk of misdiagnosis. Inpatients often differ in health status compared to patients in the outpatient setting. There are various patient factors that contribute to the plausibility of assessing inpatients through telemedicine; factors that contribute to the frailty of the patient, the patients’ technological competence and the suspected gravity of the injury [9]. Further, resistance to utilize tele-medicine may stem from the implication of professional liability.
6. Outpatient consultations
The variety in orthopedic outpatient consultations may prove challenging in telemedicine. For first-time complaints, virtual examinations may be difficult and providers are often tentative when using the technology [4]. Thus applying teleorthopedics to certain subset of patients; follow up for non-surgical fractures, mild trauma and non-urgent consultations for geographically distant patients.
7. Postoperative follow up
There have been positive implementations of teleorthopedics for follow up of patients in the postoperative period. Marsh et al. reported lower costs, shorter consultations and less travelling distances for patients being followed up after arthroplasty [6]. Further, an assessment of rehabilitation, functional outcomes and home environment is possible in video consultations [7]. However, an in person assessment of wounds, range of motion and the application of dressing is likely more accurate. Perhaps an in-person assessment in the immediate postoperative period is warranted, whereas video consultations may provide similar yields down the recovery period.
8. Specific patient cohorts
Telemedicine has been positively implemented in certain scenarios, particularly to avoid long-distance transportation in rural populations [8]. Further, assessment of patients in the postoperative period may prove convenient; especially when assessing wounds and range of motion. Multiple resources have cited lower costs using the web-based consultations, avoiding the need to travel and consult in person [3,5,6].
9. Conclusion
Inpatient orthopedic consultations must be assessed carefully to avoid misdiagnoses. Elderly or frail patients are more likely to both; sustain trauma and fractures. Potential limitations of tele-orthopedics may be apparent here, especially in the presence of technological incompetence and high likelihood of fractures. The number of fractures in inpatient COVID-19 patients warrants careful examination and high suspicion of fractures.
Source of funding
This study received no funding
Author contributions
Jarragh A – Manuscript, conceptualization, review, editing. Lari A – Manuscript preparation, review, editing. AlShatti A – Data collection, draft. AlLoughani E − Data collection, draft. AlAwadhi K – Data collection, draf.
Ethical approval
Ethical approval was obtained from our local ethical committee.
Registration of research studies
-
1.
Name of the registry: Research Registry
-
2.
Unique Identifying number or registration ID: 7739
-
3.
Hyperlink to your specific registration (must be publicly accessible and will be checked): https://www.researchregistry.com/browse-the-registry#home/registrationdetails/619d0e5bb3ee81001e1ba0f5/
Guarantor
The Guarantor is the one or more people who accept full responsibility for the work and/or the conduct of the study, had access to the data, and controlled the decision to publish.
Consent
Written consent was obtained from patients where possible. A copy of the written consent is available for review by the Editor in Chief of this journal on request.
Declaration of competing interest
The authors declare no conflict of interest.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.amsu.2021.103155.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Uimonen M., Kuitunen I., Paloneva J., Launonen A.P., Ponkilainen V., Mattila V.M. The impact of the COVID-19 pandemic on waiting times for elective surgery patients: a multicenter study. PLoS One. 2021 Jul 6;16(7) doi: 10.1371/journal.pone.0253875. PMID: 34228727; PMCID: PMC8259989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Vaishya R., Jain V.K., Iyengar K.P. Musculoskeletal manifestations of COVID-19. J Clin Orthop Trauma. 2021;17:280–281. doi: 10.1016/j.jcot.2021.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ajrawat P., Young Shin D., Dryan D., Khan M., Ravi B., Veillette C., Leroux T. The use of telehealth for orthopedic consultations and assessments: a systematic review. Orthopedics. 2021 Jul-Aug;44(4):198–206. doi: 10.3928/01477447-20210621-08. Epub 2021 Jul 1. PMID: 34292815. [DOI] [PubMed] [Google Scholar]
- 4.Caffery L.J., Taylor M., North J.B., Smith A.C. Tele-orthopaedics: a snapshot of services in Australia. J. Telemed. Telecare. 2017 Dec;23(10):835–841. doi: 10.1177/1357633X17732800. Epub 2017 Sep 26. PMID: 28950754. [DOI] [PubMed] [Google Scholar]
- 5.Moisan P., Barimani B., Antoniou J. Orthopedic surgery and telemedicine in times of COVID-19 and beyond: a review. Curr Rev Musculoskelet Med. 2021 Apr;14(2):155–159. doi: 10.1007/s12178-021-09693-9. Epub 2021 Jan 18. PMID: 33460020; PMCID: PMC7812031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Marsh J., Hoch J.S., Bryant D., MacDonald S.J., Naudie D., McCalden R., Howard J., Bourne R., McAuley J. Economic evaluation of web-based compared with in-person follow-up after total joint arthroplasty. J Bone Joint Surg Am. 2014 Nov 19;96(22):1910–1916. doi: 10.2106/JBJS.M.01558. PMID: 25410510. [DOI] [PubMed] [Google Scholar]
- 7.Sathiyakumar V., Apfeld J.C., Obremskey W.T., Thakore R.V., Sethi M.K. Prospective randomized controlled trial using telemedicine for follow-ups in an orthopedic trauma population: a pilot study. J. Orthop. Trauma. 2015 Mar;29(3):e139–e145. doi: 10.1097/BOT.0000000000000189. PMID: 24983434. [DOI] [PubMed] [Google Scholar]
- 8.DeNino W.F., Osler T., Evans E.G., Forgione P.M. Travel distance as factor in follow-up visit compliance in postlaparoscopic adjustable gastric banding population. Surg. Obes. Relat. Dis. 2010 Nov-Dec;6(6):597–600. doi: 10.1016/j.soard.2010.09.008. Epub 2010 Sep 17. PMID: 21111380. [DOI] [PubMed] [Google Scholar]
- 9.McLiesh P. Telehealth in contemporary orthopaedic nursing. Int J Orthop Trauma Nurs. 2019 May;33:1–3. doi: 10.1016/j.ijotn.2019.02.003. Epub 2019 Mar 13. PMID: 30910467. [DOI] [PubMed] [Google Scholar]
- 10.Agha R.A., Borrelli M.R., Vella-Baldacchino M., Thavayogan R., Orgill D.P., STROCSS Group The STROCSS statement: strengthening the reporting of cohort studies in surgery. Int. J. Surg. 2017 Oct;46:198–202. doi: 10.1016/j.ijsu.2017.08.586. Epub 2017 Sep 7. PMID: 28890409; PMCID: PMC6040889. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.